Abstract
Analytical and clinical performance validation is essential before introduction of a new human papillomavirus (HPV) assay into clinical practice. This study compares the new BD Onclarity HPV assay, which detects E6/E7 DNA from 14 high-risk HPV types, to the Hybrid Capture II (HC2) HPV DNA test, to concurrent cytology and histology results, in order to evaluate its performance in detecting high-grade cervical lesions. A population of 567 women, including 325 with ≥ASCUS (where ASCUS stands for atypical cells of undetermined significance) and any HC2 result and 242 with both negative cytology and negative HC2 results, were prospectively enrolled for the study. The overall agreement between Onclarity and HC2 was 94.6% (95% confidence intervals [CI], 92.3% to 96.2%). In this population with a high prevalence of disease, the relative sensitivities (versus adjudicated cervical intraepithelial neoplasia grades 2 and 3 [CIN2+] histology endpoints) of the Onclarity and HC2 tests were 95.2% (95% CI, 90.7% to 97.5%) and 96.9% (95% CI, 92.9% to 98.7%), respectively, and the relative specificities were 50.3% (95% CI, 43.2% to 57.4%) for BD and 40.8% (95% CI, 33.9%, 48.1%) for HC2. These results indicate that the BD Onclarity HPV assay has sensitivity comparable to that of the HC2 assay, with a trend to an increased specificity. Moreover, as Onclarity gives the chance to discriminate between the different genotypes, we calculated the genotype prevalence and the absolute risk of CIN2+: HPV 16 was the most prevalent genotype (19.8%) with an absolute risk of CIN2+ of 77.1%.
INTRODUCTION
Human papillomavirus (HPV) is the etiological agent for the development of cervical cancer and its precursor lesions (1): a persistent infection with high-risk (HR) HPV types has been established as a necessary step in the progression from precancerous to neoplastic disease (2). It is widely recognized that different HR HPV genotypes have different oncogenic potential, with genotype 16 being the most oncogenic of the cancer-causing HPV genotypes (3, 4).
For decades, the test of choice for the detection of cervical intraepithelial neoplasia (CIN) was the Pap smear (5). However, the Pap test has severe limitations: a relatively low sensitivity for detection of disease (range, 51 to 74%, depending on the study), limited reproducibility, interobserver variability, and finally the occurrence of equivocal results (6). The advent of HPV testing has introduced an epochal change in cervical cancer screening: in recent years, we observed a gradual shift in the use of HPV test from a “triage test,” in case of equivocal cytology, or as an adjunct test to cytology in women older than 30 years, to a primary screening test. This introduction of molecular HPV testing is slowly changing the premise of cervical screening, promising better performance than cytology-based screening but also posing new challenges (7). Over the last 7 years, HPV testing has gained a foothold in a number of national screening programs, most notably in triage of equivocal cytology or as an adjunct test to cytology in women older than 30 years, as well as more recently as a primary screening modality. Four European randomized control trials (RCTs), as recently summarized by Ronco and colleagues, clearly demonstrate the benefit of HPV testing over the use of the Pap smear (8). In this scenario, the performance of the HPV testing system of choice is crucial: the key is for an HPV assay to have an optimal balance between sensitivity and specificity for detection of CIN grade 2 or 3 (CIN2+) lesions in order to identify virtually all women with immediate precursors or in rare cases cervical cancer, and at the same time not to result in too many screening false-positive samples (9, 10). The advantage of HPV testing relies on its high sensitivity, ≥95% for CIN2+ lesions, which translates into a high negative predictive value (NPV) allowing for extended screening intervals without increased risk of cervical cancer: HPV-negative women have a reduced risk for CIN2/3 lesions and cancer in the subsequent screening round as demonstrated by the European RCTs (8).
Several in-house HPV DNA detection methods have been successfully used in research laboratories worldwide for more than 2 decades, and some have been employed for diagnostic purposes in countries where “nonapproved” tests for routine clinical testing are allowed (11). Recently, new tests using microarrays or real-time PCRs have been developed: the majority of them have been designed to detect the entire genome or a region thereof (usually within L1 region) with different grades of automation. Some of these tests are also able to provide genotyping (single or pooled), possibly allowing a stratification of the risk of cervical high-grade lesions (12).
Becton Dickinson (BD) has recently developed a new assay for the detection of HR HPV: the BD Onclarity HPV assay. It is based on type-specific E6/E7 DNA target detection using the BD Viper LT platform (BD Diagnostics, Sparks, MD, USA). The assay simultaneously detects 13 high-risk genotypes and one possibly carcinogenic HPV genotype (HPV66) (13); it provides genotyping information on six individual genotypes (16, 18, 31, 45, 51, and 52) and reports the remaining eight HPV genotypes in three distinct groups (33/58, 56/59/66, and 35/39/68). The assay has an internal human beta globin (HBB) gene control for sample sufficiency and assay performance.
This study was aimed at an explorative analytical evaluation of the Onclarity assay in a referral colposcopy center, with a high prevalence of cervical high-grade lesions, to evaluate the relative sensitivity and specificity of the assay in this setting. We compared the results of the BD Onclarity TM HPV assay (i) to those of the Qiagen HC2 HPV DNA test (HC2; Qiagen GmbH, Hilden, Germany) and (ii) to reference cytology and histology results.
MATERIALS AND METHODS
Population.
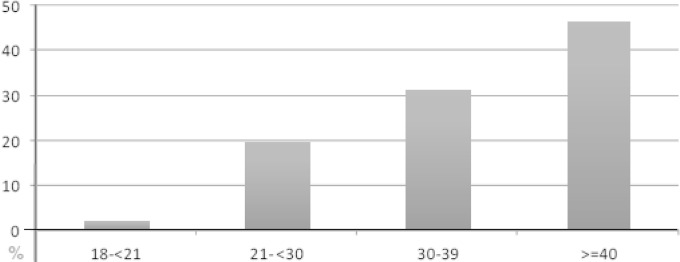
Women (n = 567, ranging in age from 18 to 81 years) (Fig. 1) attending the European Institute of Oncology in Milan referred for cervical conization, for colposcopy, or for screening purposes were enrolled in the study. For each woman a ThinPrep PreservCyt (Hologic, Inc. Bedford, MA) cervical sample was collected for Onclarity, HC2, and the Roche Diagnostics linear array (LA) test for genotyping and cytology. Cytological diagnoses were reported according to the 2001 Bethesda system terminology (14). Histology was performed for all women with positive cytology (≥ASCUS, where ASCUS stands for atypical cells of undetermined significance) and/or a positive HPV test. Histology was performed either from a specimen obtained by colposcopy with biopsy or from the evaluation of a conization specimen, and in the case of high-grade lesions a conservative surgical procedure was performed with histology evaluation of the tissue. Informed consent was obtained from all study women according to local ethical approval (IEO S689/212 study approved 28 March 2012).
FIG 1.
Age distribution of women enrolled.
Laboratory test.
After vortexing, each sample was aliquoted for cytological analysis, HC2, LA, and Onclarity assays.
HC2.
The Qiagen HC2 test is a sandwich capture molecular hybridization assay: it is a signal amplification detection method based on chemiluminescence that detects 13 HR HPV types (HPV 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, and 68). The DNA-RNA hybrids are captured on a microplate, and the emitted light is measured in a luminometer as relative light units (RLU). Samples were considered positive if the RLU/cutoff ratio was >1.0 (equivalent to 1.0 pg HPV DNA/ml). All samples with RLU between 1 and 2.5 should be retested as requested in the package insert instructions, but the residual material volume was not sufficient: these samples were discarded from the analysis.
Linear array test.
The Roche Diagnostics LA test uses biotinylated PGMY09/11 consensus primers to amplify a 450-bp region of the L1 gene: it is capable of detecting 37 HPV genotypes (6, 11, 16, 18, 26, 31, 33, 35, 39, 40, 42, 45, 51, 52, 53, 54, 55, 56, 58, 59, 61, 62, 64, 66, 67, 68, 69, 70, 71, 72, 73 [MM9], 81, 82 [MM4], 83 [MM7], 84 [MM8], IS39, and CP6108). The denatured PCR products were then hybridized to an array strip containing immobilized oligonucleotide probes. The results were visually interpreted by using the provided reference guide according to the manufacturer's protocol by two independent operators, and then the results were compared to reach a consensus.
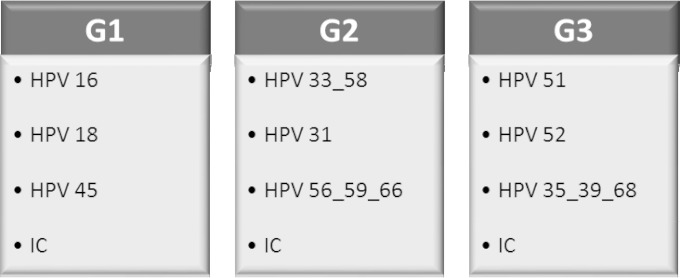
BD Onclarity.
The BD Onclarity HPV assay detects 14 HPV genotypes and coamplifies a beta-globin internal control (IC), which acts as a processing control. The primers for the 14 HPV genotypes are designed to target a region of 79 to 137 bases in the E6/E7 genome, whereas the IC primers amplify a 75-base region in the human beta-globin gene. The assay consists of three PCR assay tubes (G1, G2, and G3) and four optical channels for the detection of the 14 HPV genotypes (16, 18, 31, 45, 51, 52 as single infections and the remaining eight genotypes in three groups [33/58, 56/59/66, and 35/39/68]) and the IC (Fig. 2).
FIG 2.
BD Onclarity HPV assay design. The assay is comprised of 3 wells, designated G1 to G3, each of which has a beta-globin internal control (IC) on one channel. The 14 high-risk HPV types are read out on the other 3 channels of each well as an individual genotype or as a group of 2 or 3 pooled HPV types as shown.
Cytology and histology.
Pap tests were all liquid based and prepared with the ThinPrep 5000 slide processor (Hologic, Inc., Bedford, MA). The final diagnosis of women with abnormal cytology (>ASCUS) was made by histological evaluation of colposcopically directed biopsy specimens (at least 2 punches of the transformation zone alone or with endocervical curettage [ECC]) or on surgical tissue. Histology was adjudicated by two independent pathologists. Discrepancies were further adjudicated by a third independent pathologist.
Data analysis and statistics.
The data were recorded on case report forms and analyzed using standard statistical techniques.
We compared the results of Onclarity HPV assay with those of the HC2 HPV assay using the McNemar test.
Sensitivity and specificity were calculated for these two tests in relationship to cytology category. Positive predictive value and negative predictive value were evaluated. The results of HC2, Linear Array (Roche), and LBC Onclarity HPV assays were summarized and cross-tabulated.
All tests were considered statistically significant at α values of <0.05. All statistical analyses were performed using SAS 9.3 (SAS Institute Inc., Cary, NC).
RESULTS
We prospectively enrolled 567 women. The median age was 39 years (range, 18 to 81 years). The majority of women were found in the category of ≥30 years (78.1%) (Fig. 1).
Subsequent histology was available for 352 women, with 46.9% of them showing samples determined as ≥CIN2 and 25% with ≥CIN3. Women with no histological evaluation were considered negative if they fulfilled the combination of being cytology negative, HPV negative, and cytology negative at the previous round of screening.
Overall, we collected 567 cervical samples: 15 samples were not analyzed because they gave an HC2 result with an RLU between 1.0 to 2.5 and the volume was insufficient for retesting. Concordance between the BD Onclarity HPV and the Qiagen HC2 assays was 94.6% (522/552), with 30 discordant samples (5.4%). Percent agreements subcategorized into cytology results and combined results are shown in Table 1. Onclarity and HC2 results were significantly different for overall cytology categories (P = 0.03); however, these differences occurred only for samples with a concurrent cytology showing >ASCUS (P = 0.008, Table 1). Nine samples were found to be HC2 negative and Onclarity positive; of these, 4 tested HR HPV positive with LA while 5 were LA negative (Table 2). Resulting histology was available in 4 cases, and 1 ≥CIN3 sample was detected. Twenty-one samples were HC2 positive and Onclarity negative; 11 were concordantly HR HPV negative with LA, and the resulting histology showed 1 sample to be ≥CIN3 and 10 samples to be <CIN2. Ten patients showed discrepant genotype findings between Onclarity and LA whether in single or multiple infections. Histology of these patients revealed that 2 were ≥CIN2 and 8 were <CIN2 (Table 3).
TABLE 1.
Percent agreement of BD HPV and Qiagen HC2 HPV assays by each cytology category (NILM, ASCUS, >ASCUS) and all categories combined for PreservCyt samplesa
| Cytology category | Onclarity HPV assay result | No. of samples with indicated HC2 HPV assay result |
Total no. of samples | P value | % agreement (95% CI) |
||||
|---|---|---|---|---|---|---|---|---|---|
| Positive | Negative | NAb | Positive | Negative | Overall | ||||
| NILM | Positive | 15 | 5 | 4 | 24 | 71.4 (50.0–86.2) | 98.0 (95.3–99.1) | 95.9 (92.8–97.7) | |
| Negative | 6 | 242 | 6 | 254 | 0.76 | ||||
| Total | 21 | 247 | 10 | 278 | |||||
| ASCUS | Positive | 13 | 1 | 1 | 15 | 92.9 (68.5–98.7) | 95.2 (77.3–99.2) | 94.3 (81.4–98.4) | |
| Negative | 1 | 20 | 0 | 21 | 1.00 | ||||
| Total | 14 | 21 | 1 | 36 | |||||
| >ASCUS | Positive | 219 | 3 | 1 | 223 | 94.0 (90.2–96.4) | 81.3 (57.0–93.4) | 93.2 (89.3–95.7) | |
| Negative | 14 | 13 | 3 | 30 | 0.008 | ||||
| Total | 233 | 16 | 4 | 253 | |||||
| Overall | Positive | 247 | 9 | 6 | 262 | 92.2% (88.3–94.8) | 96.8 (94.1–98.3) | 94.6 (92.3–96.2) | |
| Negative | 21 | 275 | 9 | 305 | 0.03 | ||||
| Total | 268 | 284 | 15 | 567 | |||||
The McNemar test was used to compare results.
NA, not available.
TABLE 2.
Discordant results between HC2 assay (negative results) and Onclarity assay (positive results) compared to cytology, histology, and linear array
| Subject ID | Result by: |
Onclarity HPV genotype(s) | LA result or HPV genotype(s) |
||||
|---|---|---|---|---|---|---|---|
| Cytology | Lab histology | HC2 | Onclarity | HR HPV | Other HPV | ||
| MIL1091 | NILM | NEG | NEG | POS | 31 | 31 | NEG |
| MIL1372 | NILM | NAa | NEG | POS | 59/56/66 | NEG | NEG |
| MIL1375 | NILM | NA | NEG | POS | 16 | NEG | NEG |
| MIL1617 | NILM | NA | NEG | POS | 33/58 | NEG | NEG |
| MIL1563 | >ASCUS | NA | NEG | POS | 16 | NEG | NEG |
| MIL1326 | NILM | CIN1 | NEG | POS | 16 | 16 | NEG |
| MIL1125 | ASCUS | CIN1 | NEG | POS | 16 | 16 | NEG |
| MIL1128 | >ASCUS | CIN2 | NEG | POS | 52 | NEG | NEG |
| MIL1248 | >ASCUS | ≥CIN3 | NEG | POS | 52 | 52 | 6, 53 |
NA, not available.
TABLE 3.
Discordant results between HC2 assay (positive results) and Onclarity assay (negative results) compared to cytology, histology, and linear array
| Subject ID | Result by: |
LA result or HPV genotype(s) |
||||
|---|---|---|---|---|---|---|
| Cytology | Lab histology | HC2 | Onclarity | HR HPV | Other HPV | |
| MIL1084 | NILM | NEG | POS | Negative | Negative | Negative |
| MIL1232 | NILM | NEG | POS | Negative | Negative | Negative |
| MIL1561 | NILM | NEG | POS | Negative | Negative | Negative |
| MIL1043 | NILM | NEG | POS | Negative | HPV58 | HPV53 |
| MIL1068 | NILM | NEG | POS | Negative | HPV58 | HPV42 |
| MIL1235 | NILM | NEG | POS | Negative | HPV16 | Negative |
| MIL1030 | ASCUS | CIN1 | POS | Negative | Negative | HPV70 |
| MIL1118 | >ASCUS | NEG | POS | Negative | HPV51 | HPV42 |
| MIL1049 | >ASCUS | NEG | POS | Negative | HPV45, HPV51 | HPV42, HPV53, HPV70, HPV83 |
| MIL1152 | >ASCUS | NEG | POS | Negative | HPV45, HPV51, HPV66 | HPV42, HPV67 |
| MIL1024 | >ASCUS | CIN1 | POS | Negative | Negative | Negative |
| MIL1361 | >ASCUS | CIN1 | POS | Negative | Negative | HPV53 |
| MIL1485 | >ASCUS | CIN1 | POS | Negative | Negative | HPV70 |
| MIL1192 | >ASCUS | CIN1 | POS | Negative | Negative | HPV54, HPV70 |
| MIL1116 | >ASCUS | CIN1 | POS | Negative | Negative | HPV53, HPV54, HPV84, CP6108 |
| MIL1079 | >ASCUS | CIN1 | POS | Negative | Negative | HPV53, HPV67 |
| MIL1051 | >ASCUS | CIN1 | POS | Negative | HPV16, HPV59 | Negative |
| MIL1041 | >ASCUS | CIN1 | POS | Negative | HPV31, HPV45, HPV51 | HPV61 |
| MIL1106 | >ASCUS | CIN2 | POS | Negative | HPV33, HPV39 | Negative |
| MIL1087 | >ASCUS | ≥CIN3 | POS | Negative | Negative | HPV67 |
| MIL1006 | >ASCUS | ≥CIN3 | POS | Negative | HPV16 | HPV53, HPV61 |
We analyzed the data coming from genotyping and calculated the prevalence and the absolute risk of CIN2+: HPV16 was the most prevalent genotype (19.8%) with an absolute risk of CIN2+ of 77.1%. The second-most-frequent genotype was HPV31 (10.6%) with an associated absolute risk of CIN2+ of 66.7%. HPV18 was found in 4.2%, with an absolute risk of 52.2%.
A comparison of the performance of BD Onclarity HPV assay with that of HC2 stratified according to histology results (≥CIN2 versus <CIN2) by each cytology category (negative for intraepithelial lesion or malignancy [NILM], ASCUS, or >ASCUS) is shown in Table 3. Overall sensitivity was 95.2% (95% confidence intervals [CI], 90.7% to 97.5%) for BD and 96.9% (95% CI, 92.9% to 98.7%) for HC2 HPV, and overall specificity was 50.3% (95% CI, 43.2% to 57.4%) for BD and 40.8 (95% CI, 33.9% to 48.1%) for HC2 HPV (Table 4).
TABLE 4.
Performance comparison of BD Onclarity HPV and Qiagen HC2 assays with histology results (≥CIN2 versus <CIN2) for PreservCyt samples by each cytology category (NILM, ASCUS, >ASCUS) and all categories combined
| Cytology category | Performance measure | BD Onclarity HPV assay |
Qiagen HC2 HPV assay |
||
|---|---|---|---|---|---|
| Value %a | 95% CI | Value % | 95% CI | ||
| NILM | Sensitivity | 50.0 (2/4) | 15.0–85.0 | 50.0 (1/2) | 9.5–90.5 |
| Specificity | 79.1 (53/67) | 67.9–87.1 | 72.6 (45/62) | 60.4–82.1 | |
| ASCUS | Sensitivity | 100.0 (7/7) | 64.6–100.0 | 100.0 (7/7) | 64.6–100.0 |
| Specificity | 72.0 (18/25) | 52.4–85.7 | 75.0 (18/24) | 55.1–88.0 | |
| >ASCUS | Sensitivity | 96.1 (148/154) | 91.8–98.2 | 97.4 (148/152) | 93.4–99.0 |
| Specificity | 24.2 (23/95) | 16.7–33.7 | 10.8 (10/93) | 5.9–18.7 | |
| Overall | Sensitivity | 95.2 (157/165) | 90.7–97.5 | 96.9 (156/161) | 92.9–98.7 |
| Specificity | 50.3 (94/187) | 43.2–57.4 | 40.8 (73/179) | 33.9–48.1 | |
| Positive predictive value | 62.8 (157/250) | 59.5–66.4 | 59.5 (156/262) | 56.7–62.7 | |
| Negative predictive value | 92.2 (94/102) | 85.8–95.9 | 93.6 (73/78) | 86.3–97.2 | |
Values are percentages relatives to the CIN2+ endpoints determined by histology; fractions in parentheses represent the number of samples with results agreeing with histology/total number of samples.
DISCUSSION
The aim of the current study was to evaluate the analytical performance of the BD Onclarity HPV assay against that of the HC2 assay for the detection of HR HPV in cervical samples from a referral population attending our institution. Overall, the two assays showed good agreement using ThinPrep stored samples (94.6%), with similar sensitivity and specificity between the assays in this setting with high prevalence of disease.
HPV testing is becoming more and more recognized as the test of choice for primary screening and management of cervical disease, and recently released guidelines propose HPV testing as the primary screening test, replacing cytology (8, 9, 15). A shift to primary HPV screening can be implemented only if the test used has undergone a fully analytical and clinical validation. Yet a number of different systems are available and used today (12, 16), with large differences in analytical and clinical performance. This represents a serious challenge, as decisions are taken by the clinicians on the basis of a result that may not be completely correct from a clinical perspective. In fact, at present only few systems have been fully validated.
In this study, we focused primarily on the evaluation of Onclarity in a referral population, associating the Onclarity HPV result with underlying clinical disease and comparing the outcomes in a split-sample fashion to results obtained with the HC2 test. The agreement was found to be very high, even though the Onclarity test, with its extended genotype readout, represents a more complex diagnostic system than does the HC2. These findings are in line with the conclusions previously reported by Wright et al. and Ejegod et al. (17, 18). Onclarity offers substantial advantages over “yes/no” assays like HC2 in terms of automation, reduced hands-on time, and the presence of an internal control based on a human housekeeping gene, the positivity of which confirms the adequacy of the specimen.
Looking at the discordant samples, HC2-positive/Onclarity-negative results dominated, constituting 70% of the discordant samples. The HR HPV result of HC2 was not confirmed by LA genotyping in one half of these samples, while for the other half the LA detected the presence of different low-risk genotypes. We found only 3 of 21 patients HC2 positive/Onclarity negative with a lesion ≥CIN2. The remaining HC2-positive/Onclarity-discordant samples showed mainly LR HPV types, thereby representing a “false-positive” HC2 test result, using LA HR HPV negativity as the adjudicator. On the other hand, 9 patients were HC2 negative/Onclarity positive; 4 patients were positive for HR HPV by LA, and 1 patient was negative for any HPV. Histology was available for only 6 of these patients, with 2 patients bearing a ≥CIN2, both with HPV genotype 52. It should be noted that LA does not have an established clinical cutoff and would be expected to detect some analytically positive samples that are below the clinical cutoff in the Onclarity assay. Overall, our data corroborate already published data showing that a substantial cross-reactivity to LR HPV types damages the HC2 specificity (19, 20, 21). In conclusion, these data show that Onclarity not only performs as well as HC2 from a clinical sensitivity perspective but also offers some advantage in terms of specificity, although the comparison, though showing a trend, did not reach a statistical significance overall.
One interesting point is that, differently from other recently introduced systems, Onclarity is a PCR-based assay in which the target region is within the E6 and E7 regions of the HR HPV genome. This could be of help in the case of cervical cancer, in which the L1 part of the genome has been disrupted and therefore these lesions may give a negative HPV test result when systems based on L1 consensus primers PCR are used (22, 23). Moreover, the test is designed so that different genotypes can be distinguished: HPV genotypes 16, 18, 45, 31, 51, 52, 33, 58, 56, 59, 66, 35, 39, and 68 can be identified in single or multiple infections. This can be of help, both for the risk stratification of the patients, as HPV16 detection can refer the women to a different clinical approach, and for the follow-up of patients with a CIN lesion, after treatment, to evaluate the clearance or the persistence of a specific HPV type (4). One strength of this study is that women were prospectively enrolled, samples were stored and tested in batches with Onclarity, and we had a high percentage of specimens taken from patients with a cervical lesion. On the other hand, one limitation related to the inclusion criteria is that we could not have a histological diagnosis in case of both HC2 negativity and cytology negativity, in particular for those cases testing positive with Onclarity.
In conclusion, the BD Onclarity assay is an accurate HPV assay for the detection and genotyping of HR HPV infections. Further studies are ongoing to validate its clinical performance outside high-prevalence, high-risk referral populations like those used in this study.
ACKNOWLEDGMENTS
The BD Onclarity HPV assay, Qiagen HC2, and Roche Diagnostics Linear Array tests performed in this study were funded entirely by BD Diagnostics, Sparks, MD, USA.
REFERENCES
- 1.zur Hausen H. 2009. Papillomaviruses in the causation of human cancers—a brief historical account. Virology 384:260–265. doi: 10.1016/j.virol.2008.11.046. [DOI] [PubMed] [Google Scholar]
- 2.Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, Snijders PJ, Peto J, Meijer CJ, Muñoz N. 1999. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol 189:12–19. doi:. [DOI] [PubMed] [Google Scholar]
- 3.Castle PE, Solomon D, Schiffman M, Wheeler CM. 2005. Human papillomavirus type 16 infections and 2-year absolute risk of cervical precancer in women with equivocal or mild cytologic abnormalities. J Natl Cancer Inst 97:1066–1071. doi: 10.1093/jnci/dji186. [DOI] [PubMed] [Google Scholar]
- 4.Kjær SK, Frederiksen K, Munk C, Iftner T. 2010. Long-term absolute risk of cervical intraepithelial neoplasia grade 3 or worse following human papillomavirus infection: role of persistence. J Natl Cancer Inst 102:1478–1488. doi: 10.1093/jnci/djq356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cox JT. 2009. History of the use of HPV testing in cervical screening and in the management of abnormal cervical screening results. J Clin Virol 45(Suppl 1):S3–S12. doi: 10.1016/S1386-6532(09)70002-2. [DOI] [PubMed] [Google Scholar]
- 6.Cuzick J, Arbyn M, Sankaranarayanan R, Tsu V, Ronco G, Mayrand MH, Dillner J, Meijer CJ. 2008. Overview of human papillomavirus-based and other novel options for cervical cancer screening in developed and developing countries. Vaccine 26(Suppl 10):K29–K41. doi: 10.1016/j.vaccine.2008.06.019. [DOI] [PubMed] [Google Scholar]
- 7.Lynge E, Rygaard C, Baillet MV, Dugué PA, Sander BB, Bonde J, Rebolj M. 2014. Cervical cancer screening at crossroads. APMIS 122:667–673. doi: 10.1111/apm.12279. [DOI] [PubMed] [Google Scholar]
- 8.Ronco G, Dillner J, Elfström KM, Tunesi S, Snijders PJ, Arbyn M, Kitchener H, Segnan N, Gilham C, Giorgi-Rossi P, Berkhof J, Peto J, Meijer CJ, International HPV screening working group. 2014. Efficacy of HPV-based screening for prevention of invasive cervical cancer: follow-up of four European randomised controlled trials. Lancet 383:524–532. doi: 10.1016/S0140-6736(13)62218-7. [DOI] [PubMed] [Google Scholar]
- 9.Meijer CJ, Berkhof J, Castle PE, Hesselink AT, Franco EL, Ronco G, Arbyn M, Bosch FX, Cuzick J, Dillner J, Heideman DA, Snijders PJ. 2009. Guidelines for human papillomavirus DNA test requirements for primary cervical cancer screening in women 30 years and older. Int J Cancer 124:516–520. doi: 10.1002/ijc.24010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stoler MH, Castle PE, Solomon D, Schiffman M. 2007. The expanded use of HPV testing in gynecologic practice per ASCCP-guided management requires the use of well-validated assays. Am J Clin Pathol 127:335–337. doi: 10.1309/RNF3C01JKADQCLKP. [DOI] [PubMed] [Google Scholar]
- 11.Snijders PJ, Heideman DA, Meijer CJ. 2010. Methods for HPV detection in exfoliated cell and tissue specimens. APMIS 118:520–528. doi: 10.1111/j.1600-0463.2010.02621.x. [DOI] [PubMed] [Google Scholar]
- 12.Poljak M, Kocjan BJ. 2010. Commercially available assays for multiplex detection of alpha human papillomaviruses. Expert Rev Anti Infect Ther 8:1139–1162. doi: 10.1586/eri.10.104. [DOI] [PubMed] [Google Scholar]
- 13.Halec G, Alemany L, Lloveras B, Schmitt M, Alejo M, Bosch FX, Tous S, Klaustermeier JE, Guimerà N, Grabe N, Lahrmann B, Gissmann L, Quint W, Bosch FX, de Sanjose S, Pawlita M, Retrospective International Survey and Time Trends Study Group; Retrospective International Survey HPV, Time Trends Study Group HPV. 2014. Pathogenic role of the eight probably/possibly carcinogenic HPV types 26, 53, 66, 67, 68, 70, 73 and 82 in cervical cancer. J Pathol 234:441–451. doi: 10.1002/path.4405. [DOI] [PubMed] [Google Scholar]
- 14.Stoler MH. 2002. New Bethesda terminology and evidence-based management guidelines for cervical cytology findings. JAMA 287:2140–2141. doi: 10.1001/jama.287.16.2140. [DOI] [PubMed] [Google Scholar]
- 15.World Health Organization. 2013. WHO guidelines for screening and treatment of precancerous lesions for cervical cancer prevention. World Health Organization, Geneva, Switzerland. [PubMed] [Google Scholar]
- 16.Cuzick J, Cadman L, Mesher D, Austin J, Ashdown-Barr L, Ho L, Terry G, Liddle S, Wright C, Lyons D, Szarewski A. 2013. Comparing the performance of six human papillomavirus tests in a screening population. Br J Cancer 108:908–913. doi: 10.1038/bjc.2013.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wright TC Jr, Stoler MH, Agreda PM, Beitman GH, Gutierrez EC, Harris JM, Koch KR, Kuebler M, LaViers WD, Legendre BL Jr, Leitch SV, Maus CE, McMillian RA, Nussbaumer WA, Palmer ML, Porter MJ, Richart GA, Schwab RJ, Vaughan LM. 2014. Clinical performance of the BD Onclarity HPV assay using an adjudicated cohort of BD SurePath liquid-based cytology specimens. Am J Clin Pathol 142:43–50. doi: 10.1309/AJCP53KMHNRDICBL. [DOI] [PubMed] [Google Scholar]
- 18.Ejegod DM, Bonde J, Serrano I, Cuschieri KS, Nussbaumer WA, Vaughan LM, Ahmad AS, Cuzick J. 2013. Clinical validation of the BD Onclarity™ HPV assay using a non-inferiority test. J Med Microbiol Diagn S3:003. doi: 10.4172/2161-0703.S3-003. [DOI] [Google Scholar]
- 19.Castle PE, Schiffman M, Burk RD, Wacholder S, Hildesheim A, Herrero R, Bratti MC, Sherman ME, Lorincz A. 2002. Restricted cross-reactivity of hybrid capture 2 with nononcogenic human papillomavirus types. Cancer Epidemiol Biomarkers Prev 11:1394–1399. [PubMed] [Google Scholar]
- 20.Castle PE, Solomon D, Wheeler CM, Gravitt PE, Wacholder S, Schiffman M. 2008. Human papillomavirus genotype specificity of hybrid capture 2. J Clin Microbiol 46:2595–2604. doi: 10.1128/JCM.00824-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Poljak M, Marin IJ, Seme K, Vince A. 2002. Hybrid Capture II HPV Test detects at least 15 human papillomavirus genotypes not included in its current high-risk probe cocktail. J Clin Virol 25(Suppl 3):S89–S97. doi: 10.1016/S1386-6532(02)00187-7. [DOI] [PubMed] [Google Scholar]
- 22.Karlsen F, Kalantari M, Jenkins A, Pettersen E, Kristensen G, Holm R, Johansson B, Hagmar B. 1996. Use of multiple PCR primer sets for optimal detection of human papillomavirus. J Clin Microbiol 34:2095–2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tjalma WA, Depuydt CE. 2013. Cervical cancer screening: which HPV test should be used—L1 or E6/E7. Eur J Obstet Gynecol Reprod Biol 170:45–46. doi: 10.1016/j.ejogrb.2013.06.027. [DOI] [PubMed] [Google Scholar]