Abstract
We describe an outbreak caused by KPC-2- and IMP-10-producing Serratia marcescens isolates in a Brazilian teaching hospital. Tigecycline was the only active antimicrobial agent tested. The blaIMP-10 gene was located in a new class 1 integron, named In990, carried by a nonconjugative plasmid, in contrast to blaKPC-2.
TEXT
Serratia marcescens is a common pathogen involved in nosocomial infections affecting several body sites, with a significant impact on morbidity and mortality (1, 2). The spread of carbapenem-resistant S. marcescens strains in the nosocomial environment is a matter of concern, since this pathogen is intrinsically resistant to polymyxins (3). To date, a few Brazilian studies have reported the production of KPC-2 in carbapenem-resistant S. marcescens isolates from hospitals located in southern and northeastern Brazilian regions (4, 5). We describe herein the microbiological characterization of an outbreak caused by a KPC-2- and IMP-10-producing S. marcescens clone in a tertiary teaching hospital located in mid-western Brazil. (This study was presented in part at the 24th European Congress of Clinical Microbiology and Infectious Diseases [ECCMID], in Barcelona, Spain, 10 to 13 May 2014.)
A total of 30 carbapenem-resistant S. marcescens isolates, collected on different days and from different body site infections, between September 2011 and February 2013, were recovered from 23 patients hospitalized in intensive care units (ICUs) at a tertiary teaching hospital located in the city of Dourados in Mato Grosso do Sul state. Patients' identification and demographic data were recorded, and all clinical data were entered into a research electronic data capture (Redcap) database. Species identification was performed by Vitek2 (bioMérieux, Hazelwood, MO), and confirmed by matrix-assisted laser desorption ionization−time of flight mass spectrometry (MALDI-TOF MS), using a Microflex LT spectrometer (Bruker Daltonics, MA, USA) (6). The MICs of antimicrobials were determined by broth microdilution according to the Clinical and Laboratory Standards Institute (CLSI) guidelines (7), except for tigecycline, for which they were determined using Etest strips (bioMérieux, Marcy l'Étoile, France), according to the manufacturer's recommendations. All S. marcescens isolates were resistant to ertapenem (MIC50, >16 mg/liter), imipenem (MIC50, >8 mg/liter), and meropenem (MIC50, >8 mg/liter). Preliminary screening for the presence of carbapenemase was performed by the modified Hodge test (MHT) (7), and positive results were confirmed by ertapenem hydrolysis using MALDI-TOF MS (8). The presence of β-lactamase genes was evaluated by PCR followed by sequencing, using specific primers (9, 10). Of the 30 isolates, 24 were classified as carbapenemase producers by the MHT and MALDI-TOF MS and shown to codify blaKPC-2. The blaIMP-10 gene was also detected in 6/24 isolates (Table 1). The genetic relationships among the KPC-2-producing S. marcescens strains were determined by pulsed-field gel electrophoresis (PFGE), using SpeI (New England BioLabs, Ipswich, MA, USA) and analyzed with BioNumerics software v.3.0 (Applied Maths, Sint-Martens-Latem, Belgium). The percentage of similarity between fingerprints was scored by the Dice coefficient (11). All 24 KPC-2-producing strains, including those that coproduced IMP-10, exhibited >94.1% similarity (Fig. 1). The results of the susceptibility tests for the six isolates coproducing KPC-2 and IMP-10 show that tigecycline was the only antimicrobial agent tested with activity against these strains (Table 2). The sequencing analysis of the blaIMP-10 genetic context (12, 13) demonstrated that it was inserted in a new class 1 integron cassette arrangement, named In990. The blaIMP-10 gene was arranged as the first gene cassette of In990, immediately downstream of the 5′-conserved sequence (CS), followed by 2 genes (aacA31 and aadA1) encoding aminoglycoside-modifying enzymes (AMEs). The 3′-CS contained the qacEΔ1-sul1 genes encoding resistance to a disinfectant determinant and sulfonamide, respectively. The plasmid DNA extraction was performed using the Kieser protocol (14) and DNA-DNA hybridization was assessed by Southern blotting with a Hybond-N+ nylon transfer membrane (GE Healthcare, Little Chalfont, United Kingdom). Digoxigenin (DIG) labeling of the blaKPC-2 and blaIMP-10 specific probes and signal detection were carried out using the DIG DNA labeling and detection kit (Roche Diagnostics GmbH, Penzberg, Germany). Conjugation assays were performed as described previously (15). The blaKPC-2 gene was inserted into a 100-kb conjugative plasmid in all 24 carbapenem-resistant S. marcescens isolates and was successfully transferred to the Escherichia coli J53 strain by conjugation, while the blaIMP-10 gene was located in a nonconjugative plasmid of approximately 150 kb in all six isolates (Table 2). Numerous attempts to transfer the plasmid harboring blaIMP-10 failed.
TABLE 1.
Clinical characteristics of the 23 patients involved in the ICU outbreaks caused by an epidemic of a KPC-2-producing S. marcescens strain
| Patient no. | Age (yr), sexa | Clinical isolate(s) | Strainb | Date of admission (mo/day/yr) | Date of isolation (mo/day/yr) | Hospital unitc | Length of stay (days) | Place prior to admission | Outcome | Antibiotic exposure | Carbapenemase gene(s) | Treatment (dosage)/days of therapyd |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 60, F | Tracheal aspirates | P | 9/26/2011 | 10/3/2011 | ICU | 65 | Another hospital | Death | Carbapenems | blaKPC-2 | AMI (500 mg) + CST-PMB (500 mg)/13 |
| 2 | 63, F | Tracheal aspirates | P | 9/25/2011 | 10/12/2011 | ICU | 15 | Home | RHe | Cephalosporins | blaKPC-2 | AMI (250 mg) + CST-PMB (500 mg)/14 |
| 2 | 63, F | Tracheal aspirates | P | 9/25/2011 | 11/12/2011 | ICU | 15 | Home | Recovery | Cephalosporins | blaKPC-2 | AMI (250 mg) + CST-PMB (500 mg)/17 |
| 3f | 82, M | Urine culture | P | 10/24/2011 | 10/28/2011 | ICU | 180 | Another hospital | RH | Carbapenems/cephalosporins | blaKPC-2/blaIMP-10 | AMP-SAM (4 g) + CST-PMB (500 mg)/20 |
| 3 | 82, M | Urine culture | P | 10/24/2011 | 4/3/2012 | ICU | 180 | Another hospital | Death | Carbapenems/cephalosporins | blaKPC-2/blaIMP-10 | AMP-SAM (4 g) + CST-PMB (500 mg)/14 |
| 4 | 1, M | Rectal swab | C | 11/20/2011 | 11/25/2011 | ICUneo | 29 | Home | Recovery | Cephalosporins | blaKPC-2 | AMI (50 mg) + CST-PMB (500 mg)/17 |
| 5 | 75, F | Scar | C | 9/26/2011 | 11/29/2011 | ICU | 24 | Another hospital | RH | Carbapenems/cephalosporins | blaKPC-2 | AMI (250 mg) + CST-PMB (500 mg)/7 |
| 5 | 75, F | Nasal swab | C | 09/26/2011 | 12/27/2011 | ICU | 24 | Another hospital | RH | Carbapenems/cephalosporins | blaKPC-2 | AMI (250 mg) + CST-PMB (500 mg)/10 |
| 5f | 75, F | Tracheal aspirates | P | 09/26/2011 | 12/28/2011 | ICU | 24 | Another hospital | Death | Carbapenems/cephalosporins | blaKPC-2/blaIMP-10 | AMP-SAM (4 g) + CST-PMB (500 mg)/10 |
| 6 | 76, F | Tracheal aspirates | P | 12/6/2011 | 12/21/2011 | ICU | 28 | Home | RH | Aminoglycosides/cephalosporins | blaKPC-2 | AMP-SAM (4 g) + CST-PMB (500 mg)/10 |
| 6 | 76, F | Blood culture | P | 12/6/2011 | 01/5/2012 | ICU | 28 | Home | Death | Aminoglycosides/cephalosporins | blaKPC-2 | FLU (750 mg) + CAR (500 mg)/18 |
| 7 | 2, M | Catheter | C | 12/10/2011 | 12/26/2011 | ICUped | 90 | Home | Recovery | Penicillins | NDg | AMI (250 mg) + CAR (500 mg)/22 |
| 8 | 25, M | Scar | C | 1/2/2012 | 1/7/2012 | ICU | 30 | Another hospital | Recovery | Fluoroquinolone | blaKPC-2 | AMI (250 mg) + CST-PMB (500 mg)/20 |
| 9 | 1, M | Urine culture | P | 1/10/2012 | 1/14/2012 | ICUneo | 15 | Home | Recovery | Cephalosporins | ND | CEPH (50 mg) + CAR (500 mg)/10 |
| 10 | 62, M | Tracheal aspirates | P | 1/05/2012 | 1/16/2012 | ICU | 80 | Home | Recovery | Carbapenems/cephalosporins | blaKPC-2 | AMI (500 mg) + CST-PMB (500 mg)/17 |
| 11 | 1, F | Blood culture | P | 12/29/2011 | 2/9/2012 | ICUped | 90 | Home | Death | Cephalosporins | blaKPC-2 | AMI (250 mg) + CST-PMB (500 mg)/17 |
| 12f | 52, M | Urine culture | P | 1/31/2012 | 2/13/2012 | ICU | 90 | Another hospital | Death | Aminoglycosides/carbapenems | blaKPC-2/blaIMP-10 | AMI (500 mg) + CST-PMB (500 mg)/20 |
| 13 | 62, M | Urine culture | P | 2/6/2012 | 2/16/2012 | ICU | 23 | Another hospital | RH | Aminoglycosides/carbapenems | ND | AMI (250 mg) + CAR (500 mg)/8 |
| 13 | 62, M | Tracheal aspirates | P | 2/6/2012 | 3/18/2012 | ICU | 23 | Another hospital | Recovery | Aminoglycosides/carbapenems | blaKPC-2 | AMP-SAM (4 g) + CST-PMB (500 mg)/10 |
| 14 | 56, M | Tracheal aspirates | C | 2/8/2012 | 2/16/2012 | ICU | 31 | Home | RH | Aminoglycosides/carbapenems/fluoroquinolone | blaKPC-2 | AMP-SAM (4 g) + CST-PMB (500 mg)/10 |
| 14 | 56, M | Urine culture | P | 2/8/2012 | 3/19/2012 | ICU | 31 | Home | Recovery | Aminoglycosides/carbapenems/fluoroquinolones | blaKPC-2 | AMI (500 mg) + CST-PMB (500 mg)/14 |
| 15 | 82, M | Nasal swab | C | 2/8/2012 | 2/17/2012 | ICU | 33 | Another hospital | Recovery | Carbapenems/cephalosporins | blaKPC-2 | AMI (250 mg) + CST-PMB (500 mg)/17 |
| 16 | 62, M | Tracheal aspirates | P | 2/6/2012 | 2/27/2012 | ICU | 47 | Another hospital | Recovery | Aminoglycosides/carbapenems | blaKPC-2 | AMI (500 mg) + CST-PMB (500 mg)/12 |
| 17f | 67, M | Tracheal aspirates | P | 3/31/2012 | 4/16/2012 | ICU | 90 | Another hospital | Death | Aminoglycosides/carbapenems | blaKPC-2/blaIMP-10 | AMP-SAM (4 g) + CST-PMB (500 mg)/10 |
| 18 | 45, M | Rectal swab | C | 3/15/2012 | 4/20/2012 | ICU | 28 | Another hospital | Death | Carbapenems/cephalosporins | blaKPC-2 | AMI (250 mg) + CST-PMB (500 mg)/12 |
| 19f | 85, F | Tracheal aspirates | P | 4/17/2012 | 4/23/2012 | ICU | 43 | Another hospital | Death | Aminoglycosides/carbapenems | blaKPC-2/blaIMP-10 | AMP-SAM (4 g + CST-PMB (500 mg)/10 |
| 20 | 75, F | Blood culture | P | 6/8/2012 | 6/13/2012 | ICU | 30 | Home | Recovery | Penicillins/carbapenems | ND | AMI (250 mg) + CAR (500 mg)/14 |
| 21 | 83, F | Tracheal aspirates | P | 6/30/2012 | 7/4/2012 | ICU | 27 | Home | Recovery | Cephalosporins | blaKPC-2 | AMI (500 mg) + CAR (500 mg)/16 |
| 22 | 2, F | Catheter | C | 10/09/2012 | 11/4/2012 | ICU | 90 | Home | Recovery | Cephalosporins | ND | AMI (250 mg) + CAR (500 mg)/15 |
| 23 | 1, M | Catheter | C | 1/29/2013 | 2/9/2013 | ICUneo | 30 | Home | Recovery | Cephalosporins | ND | AMI (250 mg) + CAR (250 mg)/20 |
F, female; M, male.
P, pathogen; C, colonizer.
ICU, general intensive care unit; ICUneo, neonatal intensive care unit; ICUped, pediatric intensive care unit.
AMI, aminoglycosides; CST, colistin; PMB, polymyxin B; AMP-SAM, ampicillin-sulbactam; FLU, fluoroquinolones; CAR, carbapenems; CEPH, cephalosporins.
RH, remained hospitalized.
The patient was admitted after previously hospitalization in the same hospital.
ND, not detected.
FIG 1.
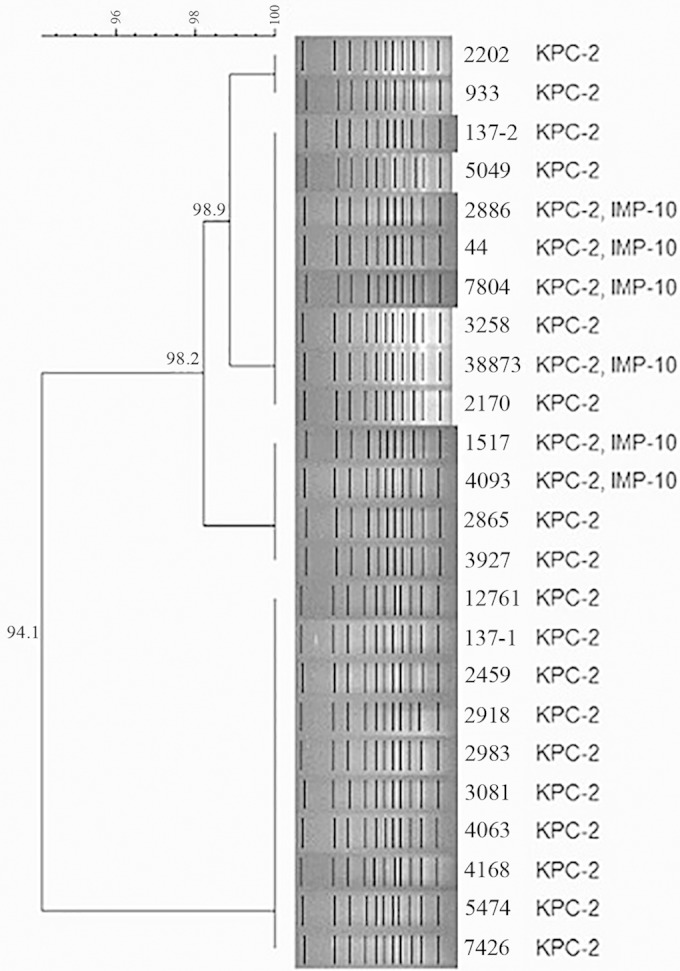
Dendrogram displaying the genetic relatedness of 24 carbapenem-resistant S. marcescens isolates recovered during an outbreak in the ICUs of a Brazilian teaching hospital according to the PFGE data and carbapenemase content.
TABLE 2.
Antimicrobial susceptibility patterns, genetic similarity, and carbapenemase content of the 6 KPC-2- and IMP-10-producing S. marcescens isolates
| Strain | PFGEc | MIC (mg/liter)a |
Gene location (kb)b |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CAZ | CTX | CRO | FEP | ATM | IPM | MEM | ETP | AMK | GEN | CIP | LVX | TGC | PMB | blaKPC-2 | blaIMP-10 | ||
| 44 | A | >256 | >256 | >256 | >256 | >32 | >8 | >16 | >32 | 64 | >64 | 16 | 8 | 0.5 | >64 | P+ (100) | P− (150) |
| 1517 | A | >256 | >256 | >256 | 128 | >32 | >8 | >16 | >32 | 64 | 32 | 4 | 8 | 0.5 | >64 | P+ (100) | P− (150) |
| 2886 | A | >256 | >256 | >256 | >256 | >32 | >8 | >16 | >32 | 64 | >64 | 4 | 4 | 0.5 | >64 | P+ (100) | P− (150) |
| 4093 | A | >256 | >256 | >256 | >256 | >32 | >8 | >16 | >32 | 64 | >64 | 4 | 4 | 0.5 | >64 | P+ (100) | P− (150) |
| 7804 | A | 128 | >256 | 128 | >256 | >32 | >8 | >16 | >32 | 32 | 2 | 2 | 4 | 0.5 | >64 | P+ (100) | P− (150) |
| 37510 | A | >256 | >256 | >256 | >256 | >32 | >8 | >16 | >32 | 64 | 2 | 4 | 4 | 0.5 | >64 | P+ (100) | P− (150) |
CAZ, ceftazidime; CTX, cefotaxime; CRO, ceftriaxone; FEP, cefepime; ATM, aztreonam; IMP, imipenem; MEM, meropenem; ETP, ertapenem; AMK, amikacin; GEN, gentamicin; CIP, ciprofloxacin; LVX, levofloxacin; TGC, tigecycline; PMB, polymyxin B.
P+, conjugative plasmid; P−, nonconjugative plasmid.
A, genetic profiles.
This study was conducted with the approval of the research ethics committee from the Universidade Federal da Grande Dourados (no. 039439/2012).
Since May 2011, the hospital has observed the dissemination of KPC-2-producing isolates, mainly in Klebsiella pneumoniae and Enterobacter spp. As part of the control measures, surveillance cultures were obtained weekly from nasal and rectal swabs from ICU patients for detection of methicillin-resistant Staphylococcus aureus and carbapenem-resistant Enterobacteriaceae, respectively. The carbapenem-resistant S. marcescens index strain was isolated from the tracheal aspirate of an ICU patient on 25 September 2011. The following 29 carbapenem-resistant S. marcescens isolates were recovered from 23 patients hospitalized in different ICUs during the study period. Among them, 60.9% were from male patients (n = 14). The patients' ages ranged from 1 to 85 years, and the median length of their hospital stay was 66 days (range, 15 to 180 days). Prior to the isolation of carbapenem-resistant S. marcescens, all patients had received antimicrobial therapy, including penicillins, fluoroquinolones, aminoglycosides, and/or mainly broad-spectrum cephalosporins and carbapenems (n = 21; 91.3%), except for a single patient who had received monotherapy with a fluoroquinolone. After the first positive culture, most patients received combination therapy of colistin or polymyxin B combined with an aminoglycoside or ampicillin-sulbactam, based on susceptibility testing. Although tigecycline was the only antimicrobial agent tested with activity against KPC-2 and IMP-10-coproducing strains, the patients infected did not receive this therapy because it was not available in the hospital during the study time. Among the 30 isolates studied, 20 were considered true pathogens and 10 were considered colonizers (Table 1). Colonization was defined as the isolation of strains without clinical manifestation of infection. Clinical infection was defined by a medical diagnosis according to clinical criteria (sepsis, fever, changes in frequency or color of the secretion, or new radiological findings) associated with the decision to initiate antibiotic therapy and the isolation of one strain (16). The patients who were infected by KPC-2 and IMP-10-coproducing S. marcescens showed a higher mortality rate (100%) than those infected by isolates that produced KPC-2 alone (22% mortality rate; P ≤ 0.01).
S. marcescens shows intrinsic resistance to several antimicrobial agents (3, 17) and is capable of acquiring multiple drug resistance mechanisms during antimicrobial therapy (1, 2). In Brazil, resistance to carbapenems in S. marcescens strains has rarely been reported and is associated exclusively with KPC-2 production (4, 5, 18). Outbreaks of S. marcescens infections in ICUs are frequently associated with considerable mortality rates, ranging from 14% to 60% (18, 19). This observation is in accordance with our findings, as the overall mortality rate was 39%. Interestingly, six KPC-2-producing S. marcescens isolates described in the present study also produced the metallo-β-lactamase (MBL) IMP-10 and were recovered from five patients over the course of 6 months. These patients were ≥50 years old, were previously hospitalized in the ICU for 30 to 90 days, and displayed several comorbidities. During hospitalization, they were subjected to central venous catheterization, mechanical ventilation, or surgical procedures and received more than five different antibiotics prior to the isolation of S. marcescens strains. Therefore, the high mortality rate (100%) among this group of patients could not be attributed solely to the presence of KPC-2 and IMP-10-coproducing S. marcescens isolates but could also be related to unfavorable clinical conditions. All patients infected by an S. marcescens strain producing both KPC-2 and IMP-10 were previously hospitalized in another hospital. The first patient was admitted to our hospital and remained colonized by IMP-10- and KPC-2-producing S. marcescens for 6 months, demonstrating the ability of this strain to persist. The clinical evidence suggests that this clonal strain was introduced into our hospital by colonized patients who previously had been hospitalized elsewhere. This observation is highly indicative of former dissemination and ineffective detection and isolation of such strains. Following the initial detection and characterization of this clone, infection control measures were reinforced and rectal surveillance swabs were collected from all patients in the standard care wards and ICUs. No new KPC-2 and/or IMP-10-coproducing strains have been found so far.
Both carbapenemase-encoding genes were found to be located in two different plasmids. Although the blaKPC-2 gene was transferred to the recipient E. coli J53 strain, the blaIMP-10 gene was not, a finding that differed from that observed by Hu and Zhao (20). This finding may explain why the blaIMP-10 gene was identified in only 6 out of 24 KPC-2-producing S. marcescens isolates.
In conclusion, to our knowledge, we report for the first time the production of IMP-10 in Brazil as well as the coproduction of KPC-2 and IMP-10 in S. marcescens isolates causing an outbreak associated with high mortality in ICUs at a Brazilian teaching hospital. The production of both carbapenemases by the same strain is a matter of great concern, since this pathogen exhibits intrinsic resistance to polymyxins, and carbapenems are often the drugs of the last resort for treatment. Our findings highlight the urgent need for development of efficacious strategies for the prevention and control of multidrug-resistant Gram-negative bacilli.
Nucleotide sequence accession number.
The sequencing analysis of a new class 1 integron cassette arrangement, named In990, was submitted to GenBank under accession number KP177456.
ACKNOWLEDGMENTS
We thank Thomas Jové from the Integrall database (http://integrall.bio.ua.pt/) for helping us with the integron structure analysis.
This work was partially supported by the Brazilian National Research Council (CNPq grants 480949/2013-1) and the Support Foundation for the Development of Education, Science and Technology in the State of Mato Grosso do Sul (FUNDECT grants 05/2011 and 04/2012). K.E.S. received a scholarship from Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES). We are grateful to the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP) for providing a postdoctoral grant to R.C. (protocol 2012/15459-6). A.C.G. is a researcher from the National Council for Science and Technological Development (CNPq), Ministry of Science and Technology, Brazil (process number 307816/2009-5).
A.C.G. has recently received research funding and/or consultation fees AstraZeneca, MSD, Novartis, Thermo Fisher Scientific and bioMérieux. The other authors declare no conflicts of interest.
REFERENCES
- 1.Iosifidis E, Farmaki E, Nedelkopoulou N, Tsivitanidou M, Kaperoni M, Pentsoglou V, Pournaras S, Athanasiou-Metaxa M, Roilides E. 2012. Outbreak of bloodstream infections because of Serratia marcescens in a pediatric department. Am J Infect Control 40:11–15. doi: 10.1016/j.ajic.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 2.de Vries JJ, Baas WH, van der Ploeg K, Heesink A, Degener JE, Arends JP. 2006. Outbreak of Serratia marcescens colonization and infection traced to a healthcare worker with long-term carriage on the hands. Infect Control Hosp Epidemiol 27:1153–1158. doi: 10.1086/508818. [DOI] [PubMed] [Google Scholar]
- 3.Samonis G, Korbila IP, Maraki S, Michailidou I, Vardakas KZ, Kofteridis D, Dimopoulou D, Gkogkozotou VK, Falagas ME. 2014. Trends of isolation of intrinsically resistant to colistin Enterobacteriaceae and association with colistin use in a tertiary hospital. Eur J Clin Microbiol Infect Dis 33:1505–1510. doi: 10.1007/s10096-014-2097-8. [DOI] [PubMed] [Google Scholar]
- 4.Ribeiro VB, Andrade LN, Linhares AR, Barin J, Darini AL, Zavascki AP, Barth AL. 2013. Molecular characterization of Klebsiella pneumoniae carbapenemase-producing isolates in southern Brazil. J Med Microbiol 62:1721–1727. doi: 10.1099/jmm.0.062141-0. [DOI] [PubMed] [Google Scholar]
- 5.da Costa Guimarães AC, Almeida AC, Nicoletti AG, Vilela MA, Gales AC, de Morais MM. 2013. Clonal spread of carbapenem-resistant Serratia marcescens isolates sharing an IncK plasmid containing blaKPC-2. Int J Antimicrob Agents 42:369–370. doi: 10.1016/j.ijantimicag.2013.05.017. [DOI] [PubMed] [Google Scholar]
- 6.Fehlberg LC, Andrade LH, Assis DM, Pereira RH, Gales AC. 2013. Performance of MALDI-TOF MS for species identification of Burkholderia cepacia complex clinical isolates. Diagn Microbiol Infect Dis 77:126–128. doi: 10.1016/j.diagmicrobio.2013.06.011. [DOI] [PubMed] [Google Scholar]
- 7.Clinical Laboratory Standard Institute. 2014. Performance standards for antimicrobial susceptibility testing; 24th informational supplement. CLSI document M100-S24 Clinical Laboratory Standard Institute, Wayne, PA. [Google Scholar]
- 8.Carvalhaes CG, Cayô R, Assis DM, Martins ER, Juliano L, Juliano MA, Gales AC. 2013. Detection of SPM-1-producing Pseudomonas aeruginosa and class D β-lactamase-producing Acinetobacter baumannii isolates by use of liquid chromatography-mass spectrometry and matrix-assisted laser desorption ionization−time of flight mass spectrometry. J Clin Microbiol 51:287–290. doi: 10.1128/JCM.02365-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Poirel L, Héritier C, Tolün V, Nordmann P. 2004. Emergence of oxacillinase-mediated resistance to imipenem in Klebsiella pneumoniae. Antimicrob Agents Chemother 48:15–22. doi: 10.1128/AAC.48.1.15-22.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fehlberg LC, da Silva Nogueira K, Cayô da Silva R, Nicoletti AG, Palmeiro JK, Gales AC, Dalla-Costa LM. 2014. Detection of PER-2-producing Enterobacter cloacae in a Brazilian liver transplantation unit. Antimicrob Agents Chemother 58:1831–1832. doi: 10.1128/AAC.01260-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dice LR. 1945. Measures of the amount of ecological association between species. Ecology 26:297–302. doi: 10.2307/1932409. [DOI] [Google Scholar]
- 12.Mendes RE, Toleman MA, Ribeiro J, Sader HS, Jones RN, Walsh TR. 2004. Integron carrying a novel metallo-beta-lactamase gene, blaIMP-16, and a fused form of aminoglycoside-resistant gene aac(6′)-30/aac(6′)-Ib′: report from the SENTRY Antimicrobial Surveillance Program. Antimicrob Agents Chemother 48:4693–4702. doi: 10.1128/AAC.48.12.4693-4702.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mendes RE, Castanheira M, Toleman MA, Sader HS, Jones RN, Walsh TR. 2007. Characterization of an integron carrying blaIMP-1 and a new aminoglycoside resistance gene, aac(6′)-31, and its dissemination among genetically unrelated clinical isolates in a Brazilian hospital. Antimicrob Agents Chemother 51:2611–2614. doi: 10.1128/AAC.00838-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kieser T. 1984. Factors affecting the isolation of CCC DNA from Streptomyces lividans and Escherichia coli. Plasmid 12:19–36. doi: 10.1016/0147-619X(84)90063-5. [DOI] [PubMed] [Google Scholar]
- 15.Andrade LM, Vitali L, Gaspar GG, Bellissimo-Rodrigues F, Martinez R, Darini ALC. 2014. Expansion and evolution of a virulent, extensively drug-resistant (polymyxin B-resistant), QnrS1-, CTX-M-2-, and KPC-2-producing Klebsiella pneumoniae ST11 international high-risk clone. J Clin Microbiol 52:2530–2535. doi: 10.1128/JCM.00088-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Casadevall A, Pirofisk LA. 2000. Host-pathogen interactions: basic concepts of microbial commensalism, colonization, infection, and disease. Infect Immun 68:6511–6518. doi: 10.1128/IAI.68.12.6511-6518.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mahlen SD. 2011. Serratia infections: from military experiments to current practice. Clin Microbiol Rev 24:755–791. doi: 10.1128/CMR.00017-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Milisavljevic V, Wu F, Larson E, Rubenstein D, Ross B, Drusin LM, Della-Latta P, Saiman L. 2004. Molecular epidemiology of Serratia marcescens outbreaks in two neonatal intensive care units. Infect Control Hosp Epidemiol 25:719–721. doi: 10.1086/502466. [DOI] [PubMed] [Google Scholar]
- 19.Arslan U, Erayman I, Kirdar S, Yuksekkaya S, Cimen O, Tuncer I, Bozdogan B. 2010. Serratia marcescens sepsis outbreak in a neonatal intensive care unit. Pediatr Int 52:208–212. doi: 10.1111/j.1442-200X.2009.02934.x. [DOI] [PubMed] [Google Scholar]
- 20.Hu Z, Zhao WH. 2009. Identification of plasmid- and integron-borne blaIMP-1 and blaIMP-10 in clinical isolates of Serratia marcescens. J Med Microbiol 58:217–221. doi: 10.1099/jmm.0.006874-0. [DOI] [PubMed] [Google Scholar]


