Abstract
Background
The heaviest period of cannabis use coincides with ongoing white matter (WM) maturation. Further, cannabis-related changes may be moderated by FAAH genotype (rs324420). We examined the association between cannabis use and FAAH genotype on frontolimbic WM integrity in adolescents and emerging adults. We then tested whether observed WM abnormalities were linked with depressive or apathy symptoms.
Methods
Participants included 37 cannabis users and 37 healthy controls (33 female; ages 18–25). Multiple regressions examined the independent and interactive effects of variables on WM integrity.
Results
Regular cannabis users demonstrated reduced WM integrity in the bilateral uncinate fasciculus (UNC) (MD, right: p = .009 and left: p = .009; FA, right: p = .04 and left: p = .03) and forceps minor (fMinor) (MD, p = .03) compared to healthy controls. Marginally reduced WM integrity in the cannabis users was found in the left anterior thalamic radiation (ATR) (FA, p = .08). Cannabis group ∗ FAAH genotype interaction predicted WM integrity in bilateral ATR (FA, right: p = .05 and left: p = .001) and fMinor (FA, p = .02). In cannabis users, poorer WM integrity was correlated with increased symptoms of depression and apathy in bilateral ATR and UNC.
Conclusions
Consistent with prior findings, cannabis use was associated with reduced frontolimbic WM integrity. WM integrity was also moderated by FAAH genotype, in that cannabis-using FAAH C/C carriers and A carrying controls had reduced WM integrity compared to control C/C carriers. Observed frontolimbic white matter abnormalities were linked with increased depressive and apathy symptoms in the cannabis users.
Keywords: Diffusion tensor imaging, Cannabis, Frontolimbic, FAAH, Emerging adults, Depression
Highlights
-
•
We compare frontolimbic white matter (WM) integrity in young cannabis users to controls in an otherwise healthy sample.
-
•
We examine the moderating influence of FAAH genotype on frontolimbic WM integrity.
-
•
Frequent cannabis use was associated with reduced WM integrity and FAAH genotype moderated integrity.
-
•
Reduced WM integrity in cannabis users was associated with increased symptoms of depression and apathy.
-
•
Results indicate that sensitive periods during neurodevelopment may be affected by frequent cannabis use.
1. Introduction
Cannabis use remains the most popular illicit substance among youth, with 22.7% of high school seniors and roughly 20% of college students reporting past month use (Johnston et al., 2014). Considering the decline in perceived risk of use (Johnston et al., 2013), understanding the neurocognitive consequences of regular cannabis use in youth is a significant public health priority.
Consistent with high cannabinoid receptor 1 (CB1) frontolimbic receptor density, the endogenous endocannabinoid system is thought to regulate emotion-related memory, affective processing, stress response, and executive functioning (see Egerton et al., 2006; Horder et al., 2009; Marco and Lavioloa, 2012). Adult daily cannabis users demonstrate significant downregulation of CB1 density, especially within frontolimbic regions (Hirvonen et al., 2012). CB1 receptors are localized on axons in high concentrations as well as oligodendrocytes, which myelinate axons (see Mackie, 2005; Molina-Holgado et al., 2002; Moldrich and Wenger, 2000). Diffusion tensor imaging (DTI) provides in-vivo analysis of WM integrity, measured by fractional anisotropy (FA), and mean diffusivity (MD), quantifying the direction and coherence of WM fibers. In general, greater FA and lower MD values indicate highly cohesive WM bundles (see Johansen-Berg and Behrens, 2009). Adolescence and early adulthood are characterized by substantial increases in white matter (WM) volume, consisting of axons and oligodendrocytes, and improved cohesion in the frontal and limbic networks (Ashtari et al., 2007; Barnea-Goraly et al., 2005; Bava et al., 2010a; Giorgio et al., 2008; Giorgio et al., 2010; Simmonds et al., 2014; Toga et al., 2006), which is associated with improved cognitive efficiency, especially in affective processing and complex executive functioning (Bava et al., 2010a; Blakemore and Choudhury, 2006; Nagy et al., 2004; Steinberg, 2005; Yurgelun-Todd, 2007). Further, this WM neurodevelopment coincides with increases in CB1 receptor density, especially in frontolimbic areas (Terry et al., 2009).
Therefore, chronic cannabis exposure during adolescence and young adulthood may significantly disrupt frontolimbic WM integrity. However, to date, most studies examining white matter integrity in cannabis users have focused on the corpus callosum (fMinor), memory and sensory-motor relays, finding poorer integrity in the genu (Abou-Saleh, 2010; Arnone et al., 2008; Gruber et al., 2011; Gruber et al., 2014), internal capsule (Gruber et al., 2014), arcuate fasciculi (Ashtari et al., 2009), and tracts within the hippocampus (Yücel et al., 2010; Zalesky et al., 2012), but not the corona radiata (Gruber et al., 2014). Only a few studies have specifically examined WM integrity in frontal projecting fibers that underlie emotional regulation (such as the uncinate fasciculus, anterior thalamic radiation, and forceps minor; Blumenfeld, 2002) in cannabis users. For example, Clark et al. (2012) found lowered FA in PFC WM in adolescents with polysubstance use disorders (89% cannabis use disorder), including the frontal pole, frontal superior, frontal caudal middle, frontal rostral middle, and inferior frontal gyrus. In contrast, another study found increased apparent diffusivity coefficient in PFC regions in cannabis users and controls, with no differences in FA (DeLisi et al., 2006). Filbey et al. (2014) found increased FA in the forceps minor in heavy cannabis users, although this sample was on average 28 years old; therefore, results may be unique to this age group. Perhaps most relevant to the current study, Jacobus et al. (2013b) found reductions in white matter in cannabis users with comorbid alcohol use in a 3-year longitudinal investigation, with significant group by time interactions revealing decreased FA with cannabis use in the left anterior internal capsule and uncinate fasciculus.
Inconsistent findings in this literature may be related to methodological differences including decreased power associated with whole-brain analysis (DeLisi et al., 2006; Jacobus et al., 2013b) and sample age (Filbey et al., 2014). Alternatively, genes that regulate endocannabinoid signaling (ECS) may clarify variability in cannabis-related WM findings. An enzyme called fatty acid amide hydrolase (FAAH) is involved in decreasing CB1 receptor activation by degrading the naturally occurring agonist anandamide (AEA; see Ho and Hillard, 2005). As the PFC continues to develop during adolescence, persistent increases in the reliance of FAAH activity have been noted (Long et al., 2012), suggesting that variation in FAAH signaling may regulate white matter integrity in young cannabis users. The most common single nucleotide polymorphism (SNP) results in a missense from C to A at position 385 (rs324420) for the gene encoding for the enzyme FAAH (FAAH) with C/C representing the most common genotype and A/A representing the least common (Sipe et al., 2002; Sipe et al., 2010). Carriers of the A nucleotide have increased levels of AEA thought to be attributed to a less stable form of FAAH (Sipe et al., 2010). The FAAH genotype has been linked with behavioral phenotypes (Conzelmann et al., 2012; Filbey et al., 2010; Flanagan et al., 2006; see Gunduz-Cinar et al., 2013; Hariri et al., 2009; Haughey et al., 2008; Schatch et al., 2009; Sipe et al., 2002; Sipe et al., 2010; Tyndale et al., 2007). Functional relationships have been reported between FAAH and frontolimbic behavioral phenotypes in young adult cannabis users. Haughey et al. (2008) examined self-report assessments of subjective experience and found that individuals with the C/C genotype reported significantly greater craving following abstinence compared to A carriers and A homozygotes may be at reduced risk for developing THC dependence (Tyndale et al., 2007). A follow-up study indicated that the C/C genotype individuals reported greater withdrawal symptoms post-abstinence and increased happiness after smoking relative to A carriers (Schatch et al., 2009). On balance, in non-using controls, those with A allele status have been found to have an increase in startle response toward unpleasant stimuli coupled with reduced reactivity toward pleasant stimuli (Conzelmann et al., 2012). In contrast, previous studies reported the opposite with C/C carriers demonstrating increased amygdala or threat-related reactivity and decreased ventral striatal or reward reactivity (Hariri et al., 2009); yet, Filbey et al. (2010) noted enhanced reward-related activation in orbitofrontal and anterior cingulate regions within the PFC among cannabis users with the C/C genotype. No studies to date examined whether the FAAH genotype interacts with cannabis exposure to predict frontolimbic WM integrity in youth.
The primary aim of the current study was to measure whether cannabis use and the FAAH genotype are independently or interactively associated with frontolimbic WM integrity in a sample of adolescents and emerging adults (ages 18–25). Our secondary aim was to examine whether observed abnormalities in WM integrity were associated with mood and/or apathy symptoms in the cannabis users. Based on previous findings, we hypothesized that cannabis users would demonstrate poorer WM integrity (increased MD or decreased FA values) in frontolimbic tracts compared to controls; ROIs included the forceps minor (fMinor), UNC, and ATR (Abou-Saleh, 2010; Arnone et al., 2008; Ashtari et al., 2009; Gruber et al., 2011; Gruber et al., 2014; Houenou et al., 2007; see Mahon et al., 2010; Oertel-Knöchel et al., 2014; Simmonds et al., 2014; Steffens et al., 2011; Wang et al., 2008; Yücel et al., 2010; Zalesky et al., 2012). On the basis of previous FAAH findings (Filbey et al., 2010; Haughey et al., 2008; Schacht et al., 2009; Tyndale et al., 2007), we hypothesized a significant group by genotype interaction such that cannabis users with the FAAH C/C genotype will demonstrate the lowest WM integrity compared to controls and cannabis A carriers. Finally, it was hypothesized that significant correlations would exist between poorer white matter integrity and increased depressive and apathy symptoms in the cannabis users (Bloomfield et al., 2014; Degenhardt et al., 2003; Hayatbakhsh et al., 2007; Medina et al., 2007a; Medina et al., 2007b; Verdejo-García et al., 2006).
2. Methods and materials
2.1. Participants
Participants included 67 (33 cannabis-users) right-handed adolescents and emerging adults from a larger imaging genetics study (PI: Lisdahl, NIDA R03 DA027457; see Lisdahl and Price, 2012 for additional details). Participants were between the ages 18–25 (35 males; see Table 1). The exclusions included current or past history of major neurologic, medical or Axis I disorders with the exception of substance use disorders; history of LD or special education; current psychoactive medication use; MRI contraindications; and failure to maintain abstinence for 7 days (for the detailed exclusion criteria see Lisdahl and Price, 2012). The eligible cannabis use criteria included more than 50 lifetime joints and more than 25 past year joints (on average, the group used 548 joints in the past year). Control status included less than or equal to 5 past year and 10 lifetime joints. Groups were matched as closely as possible on gender, age, education, verbal IQ, and ethnicity. Participants reporting >8 standard drinks per week on average as indicated in the Cahalan criteria as “very heavy drinkers” were excluded from the analyses.
Table 1.
Demographic & substance use information according to group & genotype.
| Cannabis users (N = 33) | Controls (N = 34) | FAAH carrier of A (N = 24) | FAAH C/C (N = 43) | |
|---|---|---|---|---|
| Age | 21.21 [18–25] | 21.12 [18–25] | 21.92* [18–25] | 20.74* [18–25] |
| % Male | 63.64% | 41.18% | 45.83% | 55.81% |
| % ethnic minority | 33.33% | 32.35% | 54.17%** | 20.93%** |
| % FAAH C/C carriers | 54.55% | 73.53% | ||
| WRAT-4 Reading, standard score | 103.36 [73–134] | 100.97 [81–120] | 98.08* [81–120] | 104.42* [73–134] |
| Education | 13.12 [9–17] | 13.88 [11–18] | 13.54 [9–17] | 13.49 [11–18] |
| Beck Depression, Inventory Total-2 | 5.12* [0–17] | 3.38* [0–14] | 2.96* [0–8] | 4.95* [0–17] |
| FrSBE apathy T scores | 52.97 [28–84] | 51.88 [25–87] | 50.54 [28–84] | 53.47 [25–87] |
| Past year nicotine use | 1788.67** [0–7350] | 469.26** [0–3680] | 719.17 [0–3680] | 1342.35 [0–7350] |
| Cotinine levels | 3.89** [0–6] | 1.32** [0–6] | 3.04 [0–6] | 2.33 [0–6] |
| Past year alcohol use | 282.91* [0–1724] | 104.26* [0–878] | 193.25 [2–1724] | 191.70 [0–1238] |
| Past year cannabis use | 548.36** [26–3895] | .41** [0–5] | 339.83 [0–1662] | 231.49 [0–3895] |
| Past year other drug use | 9.82 [0–171] | .12 [0–3] | 1.0 [0–12] | 7.07 [0–171] |
Drug use categories were as follows: alcohol, cannabis, nicotine: cigarettes, chewing tobacco/snuff/pipe, cigars/hookah, and ‘other’ drug use, which was a total including all of the following categories: sedatives, ecstasy, stimulants, opioids, hallucinogens, inhalants, and other (anything else not mentioned). For this particular study, other was a sum of the following: stimulants, ecstasy, inhalants, hallucinogens, sedatives, and opioids.
p < .05.
p < .01.
2.2. Procedures
All aspects of the study were approved by the University of Cincinnati Institutional Review Board. Recruitment included advertisements in fliers and newspapers. Interested participants were phoned to assess the eligibility criteria. This included a semi-structured interview based on the DSM-IV-TR criteria for Axis I anxiety, mood, and psychotic disorders (determined by Dr. Lisdahl; First et al., 2001). Eligible participants then completed either one or two sessions. Those with considerable substance use completed the questionnaires, drug use interview, neuropsychological battery and MRI scan in two sessions in order to ensure abstinence. Participants were paid $160 for two sessions and $110 for completing one session. They also received reimbursement for parking, images of their brain, and local substance treatment resource literature.
2.3. Screening inventories and questionnaires
2.3.1. Demographic information.
Demographic variables were collected via a Background Questionnaire (see Table 1).
2.3.2. Biological samples
Participants completed a breathalyzer test and provided urine samples for assessing recent substance use and pregnancy testing. Individuals with positive drug and/or alcohol tests with the exception of cannabis and nicotine were not included in these analyses. THC metabolite levels were assessed via mass spectrometry testing in participants that tested positive; abstinence was ensured by subtracting the session 2 total from the session 1 THC metabolite ratio totals while controlling for creatinine.
2.3.3. Drug use
The Time-line Follow-back (Sobell et al., 1979) assessed past year substance use in standard units (standard drinks for alcohol; cigarettes or cigars for nicotine; joints for cannabis; grams for stimulants; tablets for ecstasy; hits or pills for: inhalants, hallucinogens, opioids, and sedatives; see Table 1). The Customary Drinking and Drug Use Record (CDDR) estimated past 3-month and lifetime substance use and assessed withdrawal, abuse and dependence criteria (DSM-IV), and difficulties related to substance use (Brown et al., 1998; Stewart and Brown, 1995).
2.3.4. Self-report measures
Current depressive symptoms were measured by the Beck Depression Inventory-II (Beck et al., 1996). Greater cannabis use has previously been associated with greater apathy scores on the Frontal Systems Behavioral Scale (FrSBE) (Verdejo-García et al., 2006), thus current symptoms of apathy were measured by the FrSBE, and age, gender, and education-normed T scores were used in all analyses (Grace and Malloy, 2001).
2.4. Neuropsychological assessment
2.4.1. Premorbid intelligence
Estimates of verbal intelligence were measured by The Wide Range Achievement Test-4th Edition (WRAT-4) Reading subtest (Wilkinson, 2006), which may be sensitive to quality of education (see Manly et al., 2002). We controlled for this estimate in the analyses in order to reduce any pre-existing differences between groups.
2.5. Genotyping
2.5.1. FAAH
The FAAH variant was genotyped by a trained geneticist using the TaqMan (fluorogenic 5′ nuclease) assay (for an example see Egan et al., 2003). The primers and the probes were obtained from Applied Biosystems, and PCR was conducted via an ABI 9700 thermocycler. Endpoint results were scored using the ABI 7900HT Sequence Detection System. For these analyses, individuals fit into one of two FAAH genotype groups: C/C genotype or A carrier (e.g., C/A or A/A genotype).
2.6. MRI data acquisition
2.6.1. Parameters
Images were obtained from a 4 T Varian, Unity MRI scanner. T1-weighted, 3-D SPGR anatomical brain scan was obtained using a modified driven equilibrium Fourier transform (MDEFT) sequence (FOV = 25.6 cm, 256 × 256 × 192 matrix, slice thickness = 1 mm, in-plane resolution= 1 × 1 mm, TR = 13 ms, TE = 5.3 ms, flip angle = 22°). Diffusion tensor imaging (DTI) was obtained using 12 diffusion directions with b ≈ 600 s/mm2 (FOV = 25.6 cm, 64 × 64 × 30 matrix, resolution = 4 × 4 × 4 mm3, TR = 8000 ms, TE = 88.8 ms, flip angle 90°). A neuroradiologist at CIR reviewed anatomical scans, and participants with noted abnormalities were excluded from this sample.
2.7. MRI processing
2.7.1. PFC underlying WM integrity
The WM pathways were reconstructed using voxel based 3 × 3 symmetric tensor matrices. ROI-based comparison was computed through FreeSurfer version 5.3 tractography software TRACULA providing both measures of average weighted fractional anisotropy (FA) and mean diffusivity (MD) (Yendiki et al., 2011) for the following tracts: the corpus callosum forceps minor (fMinor), and bilateral: anterior thalamic radiation (ATR), and uncinate fasciculus (UNC) (see Fig. 1).
Fig. 1.
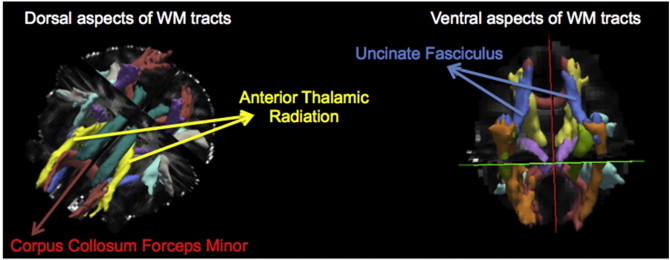
White matter (WM) regions of interest.
2.8. Data analysis
All analyses were conducted using SPSS. ANOVAs and Chi-square tests were run to examine potential demographic differences as well as differences in past year drug use histories between the drug and genotype groups. For the primary aim, general linear modeling (GLM) in SPSS was used to examine whether group, FAAH genotype, or a group ∗ FAAH genotype interaction were significantly associated with average weighted FA and MD for each ROI. Standard least squares multiple regression was used; block one included covariates (WRAT-4 Reading score, age, gender, ethnicity, past year alcohol use, cotinine levels), group, and genotype; block two included the interaction between group and FAAH genotype. If the interaction (cannabis ∗ FAAH genotype) was not significant, only block one was interpreted. All dependent variables were normally distributed and there was no evidence of multicollinearity. For the secondary analysis, Pearson correlations were run in the cannabis users between BDI-II depressive symptoms, FrSBE apathy symptoms, and WM ROIs that significantly differed between groups or by genotype × group interactions. Significance was determined if p < .05 for all analyses.
3. Results
3.1. Demographic & mood information
3.1.1. Demographics: drug group
ANOVAs and Chi-square tests revealed that groups did not differ in gender [χ2(1)3.39, p = .07], ethnicity [66.67% Caucasian for cannabis users and 67.65% controls], [χ2(1).007, p = .93], WRAT-4 Reading standard score [F(1,65) = .55, p = .46], age [F(1,65) = .03, p = .87], education [F(1,65) = 3.2, p = .08], annual income [F(1,65) = .05, p = .83], body mass index [F(1,64) = .43, p = .52], or FrSBe apathy T scores [F(1,65) = .17, p = .72]. As reported previously, cannabis users and controls significantly differed in BDI-II depressive symptoms [F(1,65) = 3.84, p = .05], with cannabis users reporting more symptoms than controls (primarily in irritability and self-criticalness). Cannabis users reported an average BDI-II total of 5, which is consistent with minimal depressive symptoms (see Table 1).
3.1.2. Demographics: FAAH genotype
ANOVAs and Chi-square tests noted significant differences between C/C and A carriers in ethnicity [χ2(1)7.72, p = .005], (22.93% of C/C individuals and 54.17% of A carriers identified as an ethnic minority); this is consistent with rates in the general population, as African Americans have previously been reported to have greater levels of P129T haplotype diversity compared to Caucasians (Flanagan et al., 2006). There were also significant differences between genotypes in age [F(1,65) = 4.07, p = .05], and BDI-II depressive symptoms [F(1,65) = 4.71, p = .03] (see Table 1). No differences were found between genotypes in the WRAT-4 Reading standard score [F(1,65) = 3.71, p = .06], body mass index [F(1,64) = .45, p = .5], gender [χ2(1).62, p = .43], education [F(1,65) = .01, p = .91], income [F(1,65) = 3.1, p = .08], or FrSBe apathy T scores [F(1,65) = .85, p = .36].
3.2. Allele frequencies
3.2.1. FAAH genotype
FAAH allele frequencies for 67 subjects were: 24 A carriers and 43 C/C genotype (11 A carrying and 24 C/C males; 13 A carrying and 19 C/C females; see Table 1). There were no significant differences between cannabis users and controls in the FAAH genotype [χ2(1)2.63, p = .11].
3.3. Drug use
3.3.1. Cannabis group
Cannabis users differed from controls in past year uses of nicotine [F(1,65) = 7.7, p = .007], alcohol [F(1,65) = 6.2, p = .02] and cannabis [F(1,65) = 17.18, p < .001] and recent nicotine use measured by cotinine level [F(1,65) = 22.33, p < .001] (see Table 1). There was no difference between past year other drug use [F(1,65) = 3.48, p = .07] and past year drinking patterns [χ2(5)3.84, p = .57] between the groups. The cannabis group had an average age of regular (at least weekly for 6 months) cannabis use onset of 17.9 (range 10–24).
3.3.2. FAAH group
No differences in any drug use variable were noted between C/C carriers and A carriers.
3.4. Primary results
3.4.1. Primary aim: white matter integrity: cannabis group status
After controlling for the WRAT-4 Reading score, age, gender, ethnicity, past year alcohol use and cotinine levels, cannabis users demonstrated increased MD in fMinor (MD, [t(58) = 2.17, beta = .30, p = .03]), and bilateral UNC (MD, right: [t(58) = 2.69, beta = .39, p = .009]); left: [t(58) = 2.69, beta = .39, p = .009]. Likewise, cannabis users demonstrated decreased FA in bilateral UNC (FA, right: [t(58) = −2.07, beta = −.32, p = .04]; left: [t(58) = −2.27, beta = −.34, p = .03]) WM tracts. Cannabis users also demonstrated marginal reductions in WM integrity in the left ATR (increased MD, t(58) = 1.79, beta = .26, p = .08).
3.4.1.1. FAAH genotype
FAAH genotype did not independently predict WM integrity.
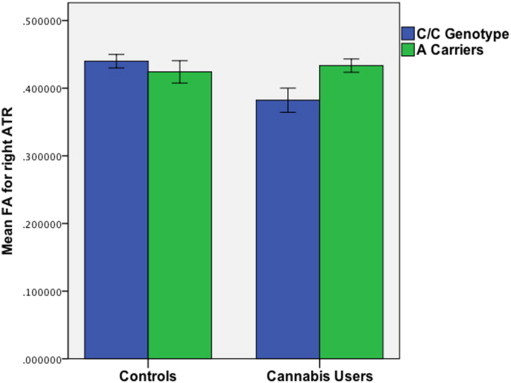
3.4.1.2. Cannabis ∗ FAAH interaction
FAAH genotype interacted with cannabis group status to significantly predict FA in fMinor and bilateral ATR. C/C cannabis users and A carrier controls demonstrated reduced FA in fMinor [t(57) = 2.43, beta = .31, p = .02], and C/C cannabis users demonstrated reduced bilateral ATR (FA, right [t(57) = 1.99, beta = .25, p = .05]; left: [t(57) = 3.53, beta = .41, p = .001]) (see Figs. 2, 3 & 4).
Fig. 2.
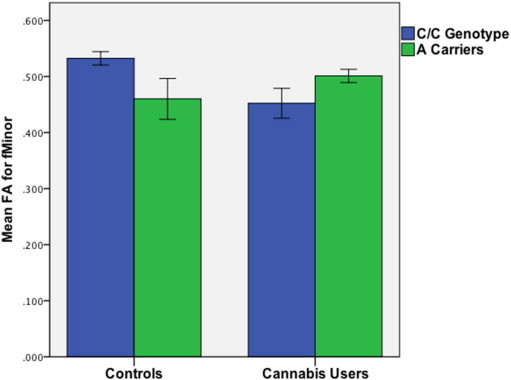
Mean FA for fMinor varies by group and FAAH genotype.
Fig. 3.
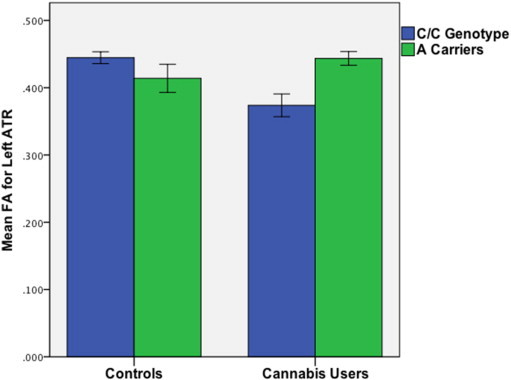
Mean FA for right ATR varies by FAAH genotype in cannabis users.
Fig. 4.
Mean FA for left ATR varies by FAAH genotype in cannabis users.
3.4.1.3. Covariates
Lower WRAT-4 Reading score [t(58) = −2.42, beta = −.32, p = .02], Caucasian ethnicity [t(58) = −2.55, beta = −.32, p = .01], and greater cotinine level [t(58) = 2.1, beta = .27, p = .04] predicted increased MD in the right ATR. Lower WRAT-4 Reading score [t(58) = −2.69, beta = −.37, p = .009] and Caucasian ethnicity [t(58) = −2.0, beta = −.26, p = .05] predicted increased MD in the left ATR. Caucasian ethnicity [t(58) = −1.97, beta = −.26, p = .05] predicted increased MD in the left UNC. Lower WRAT-4 Reading score [t(58) = −2.15, beta = −.28, p = .04] and Caucasian ethnicity [t(61) = −2.2, beta = −.28, p = .03] predicted increased MD in fMinor.
3.4.2. Secondary aim: brain–behavior relationships in cannabis users (n = 33)
Greater symptoms of depression were associated with decreased FA in bilateral ATR (right: [r = −.36, p = .04]; left: [r = −.35, p = .04]) and FA in the right UNC [r = −.34, p = .05], and increased MD in the left ATR [r = .45, p = .009]. Increased self-reported apathy symptoms were associated with decreased FA in bilateral UNC (right: [r = −.52, p = .002]; left: [r = −.59, p < .001] see Fig. 5).
Fig. 5.
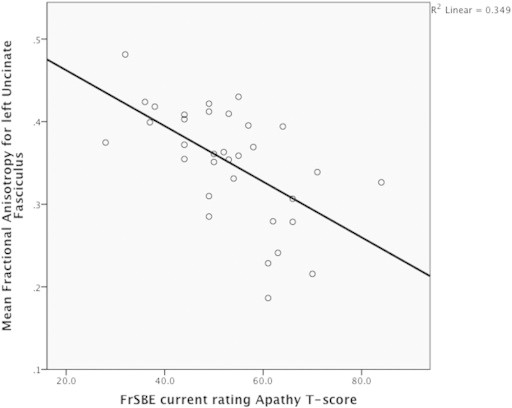
Scatter Plot — mean FA for the left UNC & apathy T score in cannabis users.
4. Discussion
The current study measured the relationship between cannabis group status, FAAH genotype, and frontolimbic WM integrity in a sample of adolescents and emerging adults (18–25 years old) without comorbid psychiatric disorders. Consistent with the predicted hypotheses, cannabis users had poorer WM integrity in fMinor and bilateral uncinate fasciculi (UNC) compared to controls. Further, consistent with proposed direction, cannabis users with the C/C genotype had reduced WM integrity in bilateral anterior thalamic radiation (ATR) compared to cannabis A carriers and controls. Examination of brain–behavior relationships noted that in cannabis users, greater self-reported depressive symptoms were significantly associated with poorer integrity in bilateral ATR and right UNC, while greater apathy scores were associated with poorer integrity in bilateral UNC, demonstrating a negative impact on affective processing.
The present findings are consistent with previous research examining regions of the fMinor, hippocampal, and internal capsule in young cannabis users (Abou-Saleh, 2010; Arnone et al., 2008; Gruber et al., 2011; Gruber et al., 2014; Jacobus et al., 2013b; Yücel et al., 2010; Zalesky et al., 2012). The PFC, especially the medial and orbital PFC, plays a vital role in regulating emotional, cognitive and behavioral functions (see Casey and Caudle, 2013; see Davidson, 2002), and such processes are fine-tuned with ongoing neurodevelopment, such that frontal regions exert greater top-down control over subcortical limbic regions (Phan et al., 2005). It has been previously proposed that the UNC has a bidirectional role in relaying associated memories of stimuli and emotions from the temporal lobes to the orbital frontal regions responsible for evaluating stimuli and rewards for the purpose of modifying behavior (see Von Der Heide et al., 2013). On balance, fMinor is composed of a collection of fibers that allow the exchange of both inhibitory and excitatory influences on the homologous region of the contralateral hemisphere within the PFC (see Bloom and Hynd, 2005; see van der Knaap and van der Ham, 2011). Thus, the observed reductions in fMinor and UNC integrity, tracts that connect the PFC to the limbic regions, may provide insight into mood and apathy symptoms related to cannabis use during this developmental period, perhaps influencing top-down abilities and affective processing in users (Bolla et al., 2005; Dorard et al., 2008; Gruber et al., 2009; Patton et al., 2002; Platt et al., 2010). As cortico-limbic tracts are one of the last to develop (Simmonds et al., 2014), the present findings demonstrated compromise in these particular bundles, suggesting disruption of neurodevelopmental processes among cannabis using youth.
We also found moderations of WM integrity in cannabis users by FAAH genotype. Consistent with previous research suggesting greater risk associated with C/C genotype (Filbey et al., 2010; Haughey et al., 2008; Schacht et al., 2009; Tyndale et al., 2007), C/C status in cannabis users was associated with reduced WM integrity in bundles terminating on the prefrontal regions including the anterior cingulate and orbital frontal cortices, and previous studies have highlighted the role of such pathways in emotion processing, mood disorders, and reward-related behavior (Coenen et al., 2012; Lai and Wu, 2014; Paul et al., 2006). Filbey et al. (2010) examined functional changes between C/C and A carriers and found heightened activation in reward circuitry regions, including both anterior cingulate and orbital frontal cortex, among cannabis users with C/C genotype. Such findings suggest over-activation of limbic regions, which may be at the expense of reduced inhibitory response in the control regions of the PFC, and such patterns may occur in concert with poorer WM integrity in fMinor and ATR in cannabis using C/C carriers as observed in this study. In controls, the opposite pattern was observed, with those carrying at least one A allele demonstrating a pattern in reduced FA in the fMinor. Endocannabinoid signaling may impact myelination with evidence of communication between oligodendrocytes and neurons (Simons and Trajkovic, 2006). Therefore, the relationship between endocannabinoid signaling and neuronal health may be an inverse-U shaped curve, with too much or too little endocannabinoid involvement being associated with poorer WM integrity. Additional longitudinal studies characterizing the differences and influences of endocannabinoid signaling on WM development are needed.
We found that poorer WM integrity was significantly associated with increased self-reported symptoms of depression and apathy in the cannabis users. These brain–behavior findings are consistent with our previous finding that reduced WM volume was associated with increased depressive symptoms in adolescent cannabis users (Medina et al., 2007b), longitudinal studies linking cannabis use with depressive disorders (Patton et al., 2002), and studies linking white matter integrity with apathy in individuals with HIV (Kamat et al., 2014). Consistent with our previous findings (Medina et al., 2007a), cannabis users as a group did not significantly differ from controls in symptoms of apathy; however, cannabis users with poorer white matter integrity did demonstrate increased apathy symptoms. Therefore, white matter integrity in frontolimbic pathways may mediate apathy symptoms in cannabis users. The reward system may also be involved, as cannabis-using youth demonstrated a relationship between increased apathy and decreased dopamine production in the striatum (Bloomfield et al., 2014), a subcortical region high in CB1 density (Terry et al., 2009). These WM pathways have been shown to impart top-down executive control (see Davison, 2002; Phan et al., 2005) and previous studies in adolescents highlight the influence they have on affective activation (Swartz et al., 2014); thus, frontal regions may not effectively regulate affective processing in young cannabis users. Future studies may want to examine frontolimbic functional connectivity differences in affective processing between young cannabis users and non-users.
There are limitations to the present study. Alcohol and cannabis are the most frequently used substances among youth (Johnston et al., 2014). The current study excluded individuals meeting the Cahalan criteria for “very heavy” alcohol use, and we statistically controlled for alcohol in the main analyses; however, it is possible that the effects of simultaneous or combined cannabis and alcohol use on WM may be influencing the observed results. For example, studies comparing non-using controls with groups reporting alcohol only or combined alcohol and cannabis use suggest that alcohol does indeed have damaging effects on WM in the frontal and temporal regions (Bava et al., 2009; Bava et al., 2010b; Bava et al., 2013; Jacobus et al., 2009; Jacobus et al., 2013a), though those transitioning to combined use may have greater WM abnormalities (Jacobus et al., 2013b). Jacobus et al. (2013b) examined WM quality in youth prior to initiation of heavy cannabis and/or heavy alcohol use and found significant reductions in WM integrity in those with combined alcohol and cannabis use compared to those that initiated heavy alcohol use alone. Thus, combined cannabis and alcohol use appears to be detrimental to WM health in youth. Similarly, cannabis users indicated greater nicotine use than controls, consistent with reported rates of co-use in youth, and associated with mood symptomatology (see Ramo et al., 2012). We also found that recent nicotine use measured by saliva cotinine levels predicted WM integrity in the right ATR, such that higher levels were associated with reduced integrity. Because this is a cross-sectional study, it is not possible to determine whether results are due to premorbid differences. A longitudinal study found that weekly or greater cannabis use during the teenage years doubled the risk of later depression and anxiety, whereas depression and anxiety as a teenager did not predict later cannabis use (Patton et al., 2002), suggesting that mood symptoms may be related to long-term regular use with earlier onset. Therefore, prospective, longitudinal studies are needed to disentangle potential causal influences on findings from cross-sectional datasets. Additionally, despite lack of differences observed in genotype between cannabis users and controls, there were significant differences in age between C/C genotype and A carriers. Although age was statistically controlled for, this may have important implications related to the degree of development reached between genotypes. Finally, ethnicity (coded as Caucasian or not) significantly predicted white matter when the FAAH genotype was included in regressions; due to power, we were not able to examine ethnicities separately. Larger cohorts may remedy this and address developmental differences between genotypes.
5. Conclusions
In conclusion, this study found that regular cannabis use is associated with poorer frontolimbic WM integrity, and these findings were moderated by the FAAH genotype. This reduced WM integrity was associated with negative mood and greater apathy symptoms in cannabis users. As use is predicted to rise in youth (Caulkins et al., 2012) in the context of decreases in perceived risk (Johnston et al., 2013), it remains an important public health priority to delay the onset of regular cannabis use until neuronal maturation has been reached (see Lisdahl et al., 2013).
Conflict of interest
None.
Acknowledgments
This research was funded by the National Institute on Drug Abuse (NIDA; R03 DA027457) and the University of Cincinnati Center for Environmental Genetics Pilot Program (P30 ES06096). Dr. Lisdahl was also funded by NIDA (R01 DA030354) during the manuscript preparation.
Contributor Information
Skyler G. Shollenbarger, Email: Skyler.Shollenbarger@gmail.com.
Jenessa Price, Email: JenessaPrice@gmail.com.
Jon Wieser, Email: JonWieser@netzero.com.
Krista Lisdahl, Email: Krista.Medina@gmail.com.
References
- Abou-Saleh M. P03-237 — corpus callosum damage in heavy marijuana use: preliminary evidence from diffusion tensor tractography and tract-based spatial statistics. Eur. Psychiatry. 2010;25:1304. doi: 10.1016/j.neuroimage.2008.02.064. [DOI] [PubMed] [Google Scholar]
- Arnone D., Barrick T.R., Chengappa S., Mackay C.E., Clark C.A., Abou-Saleh M.T. Corpus callosum damage in heavy marijuana use: preliminary evidence from diffusion tensor tractography and tract-based spatial statistics. Neuroimage. 2008;41(3):1067–1074. doi: 10.1016/j.neuroimage.2008.02.064. 18424082 [DOI] [PubMed] [Google Scholar]
- Ashtari M., Cervellione K., Cottone J., Ardekani B.A., Sevy S., Kumra S. Diffusion abnormalities in adolescents and young adults with a history of heavy cannabis use. J. Psychiatr. Res. 2009;43(3):189–204. doi: 10.1016/j.jpsychires.2008.12.002. 19111160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ashtari M., Cervellione K.L., Hasan K.M., Wu J., McIlree C., Kester H., Ardekani B.A., Roofeh D., Szeszko P.R., Kumra S. White matter development during late adolescence in healthy males: a cross-sectional diffusion tensor imaging study. Neuroimage. 2007;35(2):501–510. doi: 10.1016/j.neuroimage.2006.10.047. 17258911 [DOI] [PubMed] [Google Scholar]
- Barnea-Goraly N., Menon V., Eckert M., Tamm L., Bammer R., Karchemskiy A., Dant C.C., Reiss A.L. White matter development during childhood and adolescence: a cross-sectional diffusion tensor imaging study. Cereb. Cortex. 2005;15(12):1848–1854. doi: 10.1093/cercor/bhi062. 15758200 [DOI] [PubMed] [Google Scholar]
- Bava S., Frank L.R., McQueeny T., Schweinsburg B.C., Schweinsburg A.D., Tapert S.F. Altered white matter microstructure in adolescent substance users. Psychiatry Res. 2009;173(3):228–237. doi: 10.1016/j.pscychresns.2009.04.005. 19699064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bava S., Jacobus J., Mahmood O., Yang T.T., Tapert S.F. Neurocognitive correlates of white matter quality in adolescent substance users. Brain Cogn. 2010;72(3):347–354. doi: 10.1016/j.bandc.2009.10.012. 19932550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bava S., Jacobus J., Thayer R.E., Tapert S.F. Longitudinal changes in white matter integrity among adolescent substance users. Alcohol. Clin. Exp. Res. 2013;37(Suppl. 1):E181–E189. doi: 10.1111/j.1530-0277.2012.01920.x. 23240741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bava S., Thayer R., Jacobus J., Ward M., Jernigan T.L., Tapert S.F. Longitudinal characterization of white matter maturation during adolescence. Brain Res. 2010;1327:38–46. doi: 10.1016/j.brainres.2010.02.066. 20206151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A.T., Steer R.A., Brown G.K. Beck Depression Inventory—II. Psychological Corporation; San Antonio, TX.: 1996. [Google Scholar]
- Blakemore S.J., Choudhury S. Development of the adolescent brain: implications for executive function and social cognition. J. Child Psychol. Psychiatry. 2006;47(3–4):296–312. doi: 10.1111/j.1469-7610.2006.01611.x. 16492261 [DOI] [PubMed] [Google Scholar]
- Bloom J.S., Hynd G.W. The role of the corpus callosum in interhemispheric transfer of information: excitation or inhibition? Neuropsychol. Rev. 2005;15(2):59–71. doi: 10.1007/s11065-005-6252-y. 16211466 [DOI] [PubMed] [Google Scholar]
- Bloomfield M.A., Morgan C.J., Kapur S., Curran H.V., Howes O.D. The link between dopamine function and apathy in cannabis users: an [18F]-DOPA PET imaging study. Psychopharmacology (Berl.) 2014;231(11):2251–2259. doi: 10.1007/s00213-014-3523-4. 24696078 [DOI] [PubMed] [Google Scholar]
- Blumenfeld H. Neuroanatomy Through Clinical Cases. Sinauer Associates, Inc.; Sunderland, MA: 2002. [Google Scholar]
- Bolla K.I., Eldreth D.A., Matochik J.A., Cadet J.L. Neural substrates of faulty decision-making in abstinent marijuana users. Neuroimage. 2005;26(2):480–492. doi: 10.1016/j.neuroimage.2005.02.012. 15907305 [DOI] [PubMed] [Google Scholar]
- Brown S.A., Myers M.G., Lippke L., Tapert S.F., Stewart D.G., Vik P.W. Psychometric evaluation of the Customary Drinking and Drug Use Record (CDDR): a measure of adolescent alcohol and drug involvement. J. Stud. Alcohol. 1998;59(4):427–438. doi: 10.15288/jsa.1998.59.427. 9647425 [DOI] [PubMed] [Google Scholar]
- Casey B., Caudle K. The teenage brain: self control. Curr Dir Psychol Sci. 2013;22(2):82–87. doi: 10.1177/0963721413480170. 25284961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caulkins J.P., Kilmer B., MacCoun R.J., Pacula R.L., Reuter P. Design considerations for legalizing cannabis: lessons inspired by analysis of California's Proposition 19. Addiction. 2012;107(5):865–871. doi: 10.1111/j.1360-0443.2011.03561.x. 21985069 [DOI] [PubMed] [Google Scholar]
- Clark D.B., Chung T., Thatcher D.L., Pajtek S., Long E.C. Psychological dysregulation, white matter disorganization and substance use disorders in adolescence. Addiction. 2012;107(1):206–214. doi: 10.1111/j.1360-0443.2011.03566.x. 21752141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coenen V.A., Panksepp J., Hurwitz T.A., Urbach H., Mädler B. Human medial forebrain bundle (MFB) and anterior thalamic radiation (ATR): imaging of two major subcortical pathways and the dynamic balance of opposite affects in understanding depression. JNP. 2012;24(2):223–236. doi: 10.1176/appi.neuropsych.11080180. [DOI] [PubMed] [Google Scholar]
- Conzelmann A., Reif A., Jacob C., Weyers P., Lesch K.P., Lutz B., Pauli P. A polymorphism in the gene of the endocannabinoid-degrading enzyme FAAH (FAAH C385A) is associated with emotional–motivational reactivity. Psychopharmacology. 2012;224(4):573–579. doi: 10.1007/s00213-012-2785-y. 22776995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson R.J. Anxiety and affective style: role of prefrontal cortex and amygdala. Biol. Psychiatry. 2002;51(1):68–80. doi: 10.1016/s0006-3223(01)01328-2. 11801232 [DOI] [PubMed] [Google Scholar]
- Degenhardt L., Hall W., Lynskey M. Exploring the association between cannabis use and depression. Addiction. 2003;98(11):1493–1504. doi: 10.1046/j.1360-0443.2003.00437.x. 14616175 [DOI] [PubMed] [Google Scholar]
- DeLisi L.E., Bertisch H.C., Szulc K.U., Majcher M., Brown K., Bappal A., Ardekani B.A. A preliminary DTI study showing no brain structural change associated with adolescent cannabis use. Harm Reduction J. 2006;3(1):17. doi: 10.1186/1477-7517-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorard G., Berthoz S., Phan O., Corcos M., Bungener C. Affect dysregulation in cannabis abusers: a study in adolescents and young adults. Eur. Child Adolesc. Psychiatry. 2008;17(5):274–282. doi: 10.1007/s00787-007-0663-7. 18301941 [DOI] [PubMed] [Google Scholar]
- Egan M.F., Kojima M., Callicott J.H., Goldberg T.E., Kolachana B.S., Bertolino A., Zaitsev E., Gold B., Goldman D., Dean M., Lu B., Weinberger D.R. The BDNF val66met polymorphism affects activity-dependent secretion of BDNF and human memory and hippocampal function. Cell. 2003;112(2):257–269. doi: 10.1016/s0092-8674(03)00035-7. 12553913 [DOI] [PubMed] [Google Scholar]
- Egerton A., Allison C., Brett R.R., Pratt J.A. Cannabinoids and prefrontal cortical function: insights from preclinical studies. Neurosci. Biobehav. Rev. 2006;30(5):680–695. doi: 10.1016/j.neubiorev.2005.12.002. 16574226 [DOI] [PubMed] [Google Scholar]
- Filbey F.M., Aslan S., Calhoun V.D., Spence J.S., Damaraju E., Caprihan A., Segall J. Long-term Effects of Marijuana Use on the Brain. PNAS; 2014. 25385625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filbey F.M., Schacht J.P., Myers U.S., Chavez R.S., Hutchison K.E. Individual and additive effects of the CNR1 and FAAH genes on brain response to marijuana cues. Neuropsychopharmacology. 2010;35(4):967–975. doi: 10.1038/npp.2009.200. 20010552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- First M.B., Spitzer R.L., Gibbon M., Williams J.B.W. Clinical Interview for DSM-IVTR (SCID-I): User's Guide and Interview—Research Version. New York Psychiatric Institute Biometrics Research Department; New York: 2001. [Google Scholar]
- Flanagan J.M., Gerber A.L., Cadet J.L., Beutler E., Sipe J.C. The fatty acid amide hydrolase 385 A/A (P129T) variant: haplotype analysis of an ancient missense mutation and validation of risk for drug addiction. Hum. Genet. 2006;120(4):581–588. doi: 10.1007/s00439-006-0250-x. 16972078 [DOI] [PubMed] [Google Scholar]
- Giorgio A., Watkins K.E., Chadwick M., James S., Winmill L., Douaud G., De Stefano N., Matthews P.M., Smith S.M., Johansen-Berg H., James A.C. Longitudinal changes in grey and white matter during adolescence. Neuroimage. 2010;49(1):94–103. doi: 10.1016/j.neuroimage.2009.08.003. 19679191 [DOI] [PubMed] [Google Scholar]
- Giorgio A., Watkins K.E., Douaud G., James A.C., James S., De Stefano N., Matthews P.M., Smith S.M., Johansen-Berg H. Changes in white matter microstructure during adolescence. Neuroimage. 2008;39(1):52–61. doi: 10.1016/j.neuroimage.2007.07.043. 17919933 [DOI] [PubMed] [Google Scholar]
- Grace J., Malloy P.F. Professional manual. Lutz; Psychological Assessment Resources, FL: 2001. Frontal systems behavior scale. [Google Scholar]
- Gruber S.A., Rogowska J., Yurgelun-Todd D.A. Altered affective response in marijuana smokers: an fMRI study. Drug Alcohol Depend. 2009;105(1–2):139–153. doi: 10.1016/j.drugalcdep.2009.06.019. 19656642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber S.A., Dahlgren M.K., Sagar K.A., Gönenc A., Lukas S.E. Worth the wait: effects of age of onset of marijuana use on white matter and impulsivity. Psychopharmacology (Berl.) 2014;231(8):1455–1465. doi: 10.1007/s00213-013-3326-z. 24190588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruber S.A., Silveri M.M., Dahlgren M.K., Yurgelun-Todd D. Why so impulsive? White matter alterations are associated with impulsivity in chronic marijuana smokers. Exp. Clin. Psychopharmacol. 2011;19(3):231–242. doi: 10.1037/a0023034. 21480730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunduz-Cinar O., Hill M.N., McEwen B.S., Holmes A. Amygdala FAAH and anandamide: mediating protection and recovery from stress. Trends Pharmacol. Sci. 2013;34(11):637–644. doi: 10.1016/j.tips.2013.08.008. 24325918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hariri A.R., Gorka A., Hyde L.W., Kimak M., Halder I., Ducci F., Ferrell R.E., Goldman D., Manuck S.B. Divergent effects of genetic variation in endocannabinoid signaling on human threat- and reward-related brain function. Biol. Psychiatry. 2009;66(1):9–16. doi: 10.1016/j.biopsych.2008.10.047. 19103437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haughey H.M., Marshall E., Schacht J.P., Louis A., Hutchison K.E. Marijuana withdrawal and craving: influence of the cannabinoid receptor 1 (CNR1) and fatty acid amide hydrolase (FAAH) genes. Addiction. 2008;103(10):1678–1686. doi: 10.1111/j.1360-0443.2008.02292.x. 18705688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayatbakhsh M.R., Najman J.M., Jamrozik K., Mamun A.A., Alati R., Bor W. Cannabis and anxiety and depression in young adults: a large prospective study. J. Am. Acad. Child Adolesc. Psychiatry. 2007;46(3):408–417. doi: 10.1097/chi.0b013e31802dc54d. 17314727 [DOI] [PubMed] [Google Scholar]
- Hirvonen J., Goodwin R.S., Li C.T., Terry G.E., Zoghbi S.S., Morse C., Pike V.W., Volkow N.D., Huestis M.A., Innis R.B. Reversible and regionally selective downregulation of brain cannabinoid CB1 receptors in chronic daily cannabis smokers. Mol. Psychiatry. 2012;17(6):642–649. doi: 10.1038/mp.2011.82. 21747398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho W.S., Hillard C.J. Modulators of endocannabinoid enzymic hydrolysis and membrane transport. In: Pertwee R., editor. Cannabinoids, 168. Springer; Freiburg: 2005. pp. 187–207. [DOI] [PubMed] [Google Scholar]
- Horder J., Cowen P.J., Di Simplicio M., Browning M., Harmer C.J. Acute administration of the cannabinoid CB1 antagonist rimonabant impairs positive affective memory in healthy volunteers. Psychopharmacology. 2009;205(1):85–91. doi: 10.1007/s00213-009-1517-4. 19337726 [DOI] [PubMed] [Google Scholar]
- Houenou J., Wessa M., Douaud G., Leboyer M., Chanraud S., Perrin M., Poupon C., Martinot J.L., Paillere-Martinot M.L. Increased white matter connectivity in euthymic bipolar patients: diffusion tensor tractography between the subgenual cingulate and the amygdalo–hippocampal complex. Mol. Psychiatry. 2007;12(11):1001–1010. doi: 10.1038/sj.mp.4002010. 17471288 [DOI] [PubMed] [Google Scholar]
- Jacobus J., McQueeny T., Bava S., Schweinsburg B.C., Frank L.R., Yang T.T., Tapert S.F. White matter integrity in adolescents with histories of marijuana use and binge drinking. Neurotoxicol. Teratol. 2009;31(6):349–355. doi: 10.1016/j.ntt.2009.07.006. 19631736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobus J., Squeglia L.M., Infante M.A., Bava S., Tapert S.F. White matter integrity pre- and postmarijuana and alcohol initiation in adolescence. Brain Sciences. 2013;3(1):396–414. doi: 10.3390/brainsci3010396. 23914300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobus J., Thayer R.E., Trim R.S., Bava S., Frank L.R., Tapert S.F. White matter integrity, substance use, and risk taking in adolescence. Psychol. Addict Behav. 2013;27(2):431–442. doi: 10.1037/a0028235. 22564204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansen-Berg H., Behrens T.E.J. Diffusion MRI. From Quantitative Measurement to In Vivo Neuroanatomy. Elsevier; Burlington, MA: 2009. [Google Scholar]
- Johnston L.D., O’Malley P.M., Bachman J.G., Schulenburg J.E., Miech R.A. II. Institute for Social Research, The University of Michigan; Ann Arbor: 2014. p. 424. (Monitoring the Future: National Survey Results on Drug Use, 1975–2011: College Students and Adults Ages 19–55). [Google Scholar]
- Johnston L.D., O’Malley P.M., Bachman J.G., Schulenberg J.E. II. Institute for Social Research, University of Michigan; Ann Arbor: 2013. p. 400. (Monitoring the Future National Survey Results on Drug Use, 1975–2012: College Students and Adults Ages 19–50). [Google Scholar]
- Kamat R., Brown G.G., Bolden K., Fennema-Notestein C., Archibald S., Marcotte T.D., Letendre S.L., Ellis R.J., Woods S.P., Grant I., Heaton R.K., TMARC Group Apathy is associated with white matter abnormalities in anterior, medial brain regions in persons with HIV infection. J. Clin. Exp. Neuropsychol. 2014;36(8):854–866. doi: 10.1080/13803395.2014.950636. 25275424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai C.H., Wu Y.T. Alterations in white matter micro-integrity of the superior longitudinal fasciculus and anterior thalamic radiation of young adult patients with depression. Psychol. Med. 2014;44(13):2825–2832. doi: 10.1017/S0033291714000440. 25065445 [DOI] [PubMed] [Google Scholar]
- Lisdahl K.M., Gilbart E.R., Wright N.E., Shollenbarger S., Tapert S.F. Dare to delay? The impacts of adolescent alcohol and marijuana use onset on cognition, brain structure, and function. Front. Psychiatry. 2013;4:53. doi: 10.3389/fpsyt.2013.00053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lisdahl K.M., Price J.S. Increased marijuana use and gender predict poorer cognitive functioning in adolescents and emerging adults. J. Int. Neuropsychol. Soc. 2012;18(4):678–688. doi: 10.1017/S1355617712000276. 22613255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long L.E., Lind J., Webster M., Weickert C.S. Developmental trajectory of the endocannabinoid system in human dorsolateral prefrontal cortex. B.M.C. Neurosci. 2012;13(1):87–100. doi: 10.1186/1471-2202-13-87. 22827915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackie K. Distribution of cannabinoid receptors in the central and peripheral nervous system. Handb. Exp. Pharmacol. 2005;168(168):299–325. doi: 10.1007/3-540-26573-2_10. 16596779 [DOI] [PubMed] [Google Scholar]
- Mahon K., Burdick K.E., Szeszko P.R. A role for white matter abnormalities in the pathophysiology of bipolar disorder. Neurosci. Biobehav. Rev. 2010;34(4):533–554. doi: 10.1016/j.neubiorev.2009.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manly J.J., Jacobs D.M., Touradji P., Small S.A., Stern Y. Reading level attenuates differences in neuropsychological test performance between African American and White elders. J. Int. Neuropsychol. Soc. 2002;8(3):341–348. doi: 10.1017/s1355617702813157. 11939693 [DOI] [PubMed] [Google Scholar]
- Marco E.M., Laviola G. The endocannabinoid system in the regulation of emotions throughout lifespan: a discussion on therapeutic perspectives. J. Psychopharmacol. 2012;26(1):150–163. doi: 10.1177/0269881111408459. 21693551 [DOI] [PubMed] [Google Scholar]
- Medina K.L., Hanson K.L., Schweinsburg A.D., Cohen-Zion M., Nagel B.J., Tapert S.F. Neuropsychological functioning in adolescent marijuana users: subtle deficits detectable after a month of abstinence. J. Int. Neuropsychol. Soc. 2007;13(5):807–820. doi: 10.1017/S1355617707071032. 17697412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medina K.L., Nagel B.J., Park A., McQueeny T., Tapert S.F. Depressive symptoms in adolescents: associations with white matter volume and marijuana use. J. Child Psychol. Psychiatry. 2007;48(6):592–600. doi: 10.1111/j.1469-7610.2007.01728.x. 17537075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moldrich G., Wenger T. Localization of the CB1 cannabinoid receptor in the rat brain. An immunohistochemical study. Peptides. 2000;21(11):1735–1742. doi: 10.1016/s0196-9781(00)00324-7. 11090929 [DOI] [PubMed] [Google Scholar]
- Molina-Holgado E., Vela J.M., Arévalo-Martín A., Almazán G., Molina-Holgado F., Borrell J., Guaza C. Cannabinoids promote oligodendrocyte progenitor survival: involvement of cannabinoid receptors and phosphatidylinositol-3 kinase/Akt signaling. J. Neurosci. 2002;22(22):9742–9753. doi: 10.1523/JNEUROSCI.22-22-09742.2002. 12427829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagy Z., Westerberg H., Klingberg T. Maturation of White matter is associated with the development of cognitive functions during childhood. J. Cogn. Neurosci. 2004;16(7):1227–1233. doi: 10.1162/0898929041920441. 15453975 [DOI] [PubMed] [Google Scholar]
- Oertel-Knöchel V., Reinke B., Alves G., Jurcoane A., Wenzler S., Prvulovic D., Linden D., Knöchel C. Frontal white matter alterations are associated with executive cognitive function in euthymic bipolar patients. J. Affect. Disord. 2014;155:223–233. doi: 10.1016/j.jad.2013.11.004. 24295601 [DOI] [PubMed] [Google Scholar]
- Patton G.C., Coffey C., Carlin J.B., Degenhardt L., Lynskey M., Hall W. Cannabis use and mental health in young people: cohort study. BMJ. 2002;325(7374):1195–1198. doi: 10.1136/bmj.325.7374.1195. 12446533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul L.K., Lautzenhiser A., Brown W.S., Hart A., Neumann D., Spezio M., Adolphs R. Emotional arousal in agenesis of the corpus callosum. Int. J. Psychophysiol. 2006;61(1):47–56. doi: 10.1016/j.ijpsycho.2005.10.017. 16759726 [DOI] [PubMed] [Google Scholar]
- Phan K.L., Fitzgerald D.A., Nathan P.J., Moore G.J., Uhde T.W., Tancer M.E. Neural substrates for voluntary suppression of negative affect: a functional magnetic resonance imaging study. Biol. Psychiatry. 2005;57(3):210–219. doi: 10.1016/j.biopsych.2004.10.030. 15691521 [DOI] [PubMed] [Google Scholar]
- Platt B., Kamboj S., Morgan C.J., Curran H.V. Processing dynamic facial affect in frequent cannabis-users: evidence of deficits in the speed of identifying emotional expressions. Drug Alcohol Depend. 2010;112(1–2):27–32. doi: 10.1016/j.drugalcdep.2010.05.004. 21036306 [DOI] [PubMed] [Google Scholar]
- Ramo D.E., Liu H., Prochaska J.J. Tobacco and marijuana use among adolescents and young adults: a systematic review of their co-use. Clin. Psychol. Rev. 2012;32(2):105–121. doi: 10.1016/j.cpr.2011.12.002. 22245559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schacht J.P., Selling R.E., Hutchison K.E. Intermediate cannabis dependence phenotypes and the FAAH C385A variant: an exploratory analysis. Psychopharmacology. 2009;203(3):511–517. doi: 10.1007/s00213-008-1397-z. 19002671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simmonds D.J., Hallquist M.N., Asato M., Luna B. Developmental stages and sex differences of white matter and behavioral development through adolescence: a longitudinal diffusion tensor imaging (DTI) study. Neuroimage. 2014;92:356–368. doi: 10.1016/j.neuroimage.2013.12.044. 24384150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons M., Trajkovic K. Neuron–glia communication in the control of oligodendrocyte function and myelin biogenesis. J. Cell Sci. 2006;119(21):4381–4389. doi: 10.1242/jcs.03242. 17074832 [DOI] [PubMed] [Google Scholar]
- Sipe J.C., Chiang K., Gerber A.L., Beutler E., Cravatt B.F. A missense mutation in human fatty acid amide hydrolase associated with problem drug use. Proc. Natl. Acad. Sci. U. S. A. 2002;99(12):8394–8399. doi: 10.1073/pnas.082235799. 12060782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sipe J.C., Scott T.M., Murray S., Harismendy O., Simon G.M., Cravatt B.F., Waalen J. Biomarkers of endocannabinoid system activation in severe obesity. P.L.O.S. ONE. 2010;5(1):e8792. doi: 10.1371/journal.pone.0008792. 20098695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell L.C., Maisto S.A., Sobell M.B., Cooper A.M. Reliability of alcohol abusers' self-reports of drinking behavior. Behav. Res. Ther. 1979;17(2):157–160. doi: 10.1016/0005-7967(79)90025-1. 426744 [DOI] [PubMed] [Google Scholar]
- Steffens D.C., Taylor W.D., Denny K.L., Bergman S.R., Wang L. Structural integrity of the uncinate fasciculus and resting state functional connectivity of the ventral prefrontal cortex in late life depression. P.L.O.S. ONE. 2011;6(7):e22697. doi: 10.1371/journal.pone.0022697. 21799934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg L. Cognitive and affective development in adolescence. Trends Cogn. Sci. 2005;9(2):69–74. doi: 10.1016/j.tics.2004.12.005. 15668099 [DOI] [PubMed] [Google Scholar]
- Stewart D.G., Brown S.A. Withdrawal and dependency symptoms among adolescent alcohol and drug abusers. Addiction. 1995;90(5):627–635. doi: 10.1046/j.1360-0443.1995.9056274.x. 7795499 [DOI] [PubMed] [Google Scholar]
- Swartz J.R., Carrasco M., Wiggins J.L., Thomason M.E., Monk C.S. Age-related changes in the structure and function of prefrontal cortex–amygdala circuitry in children and adolescents: a multi-modal imaging approach. Neuroimage. 2014;86:212–220. doi: 10.1016/j.neuroimage.2013.08.018. 23959199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terry G.E., Liow J.S., Zoghbi S.S., Hirvonen J., Farris A.G., Lerner A., Tauscher J.T., Schaus J.M., Phebus L., Felder C.C., Morse C.L., Hong J.S., Pike V.W., Halldin C., Innis R.B. Quantitation of cannabinoid CB1 receptors in healthy human brain using positron emission tomography and an inverse agonist radioligand. Neuroimage. 2009;48(2):362–370. doi: 10.1016/j.neuroimage.2009.06.059. 19573609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toga A.W., Thompson P.M., Sowell E.R. Mapping brain maturation. Trends Neurosci. 2006;29(3):148–159. doi: 10.1016/j.tins.2006.01.007. 16472876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tyndale R.F., Payne J.I., Gerber A.L., Sipe J.C. The fatty acid amide hydrolase C385A (P129T) missense variant in cannabis users: studies of drug use and dependence in Caucasians. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2007;144B(5):660–666. doi: 10.1002/ajmg.b.30491. 17290447 [DOI] [PubMed] [Google Scholar]
- Van der Knaap L.J., van der Ham I.J. How does the corpus callosum mediate interhemispheric transfer? A review. Behav. Brain Res. 2011;223(1):211–221. doi: 10.1016/j.bbr.2011.04.018. 21530590 [DOI] [PubMed] [Google Scholar]
- Verdejo-García A., Rivas-Pérez C., López-Torrecillas F., Pérez-García M. Differential impact of severity of drug use on frontal behavioral symptoms. Addict Behav. 2006;31(8):1373–1382. doi: 10.1016/j.addbeh.2005.11.003. 16326022 [DOI] [PubMed] [Google Scholar]
- Von Der Heide R.J., Skipper L.M., Klobusicky E., Olson I.R. Dissecting the uncinate fasciculus: disorders, controversies and a hypothesis. Brain J. Neurol. 2013;136(6):1692–1707. doi: 10.1093/brain/awt094. 23649697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang F., Kalmar J.H., Edmiston E., Chepenik L.G., Bhagwagar Z., Spencer L., Pittman B., Jackowski M., Papademetris X., Constable R.T., Blumberg H.P. Abnormal corpus callosum integrity in bipolar disorder: a diffusion tensor imaging study. Biol. Psychiatry. 2008;64(8):730–733. doi: 10.1016/j.biopsych.2008.06.001. 18620337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson G. Wide Range Achievement Test (WRAT-4) fourth edition. Wide Range, Wilmington, DE; 2006. [Google Scholar]
- Yendiki A., Panneck P., Srinivasan P., Stevens A., Zöllei L., Augustinack J., Wang R., Salat D., Ehrlich S., Behrens T., Jbabdi S., Gollub R., Fischl B. Automated probabilistic reconstruction of white-matter pathways in health and disease using an atlas of the underlying anatomy. Front. Neuroinform. 2011;5:23. doi: 10.3389/fninf.2011.00023. 22016733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yücel M., Zalesky A., Takagi M.J., Bora E., Fornito A., Ditchfield M., Egan G.F., Pantelis C., Lubman D.I. White-matter abnormalities in adolescents with long-term inhalant and cannabis use: a diffusion magnetic resonance imaging study. J. Psychiatry Neurosci. 2010;35(6):409–412. doi: 10.1503/jpn.090177. 20731960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yurgelun-Todd D. Emotional and cognitive changes during adolescence. Curr. Opin. Neurobiol. 2007;17(2):251–257. doi: 10.1016/j.conb.2007.03.009. 17383865 [DOI] [PubMed] [Google Scholar]
- Zalesky A., Solowij N., Yücel M., Lubman D.I., Takagi M., Harding I.H., Lorenzetti V., Wang R., Searle K., Pantelis C., Seal M. Effect of long-term cannabis use on axonal fibre connectivity. Brain. 2012;135(7):2245–2255. doi: 10.1093/brain/aws136. 22669080 [DOI] [PubMed] [Google Scholar]


