Abstract
The aim of this meta-analysis was to determine the efficacy of corticosteroid versus placebo injection for the treatment of plantar fasciitis. Databases (Medline, Embase, the Cochrane Library and Google Scholar) and study references were searched for randomized controlled trials comparing corticosteroid with placebo injection for plantar fasciitis. Studies that met the inclusion criteria were selected for the analysis. The risk of bias tool was used for the methodological assessment. Outcomes including visual analogue score (VAS) and plantar fascia thickness (PFT) were extracted and pooled. Egger's test was used to detect publication bias. The evidence quality was assessed by the Grading of Recommendations Assessment, Development and Evaluation system. Statistical analysis was performed using RevMan 5.2. A total of four studies with 289 patients were included in the analysis. Compared with the placebo, corticosteroid injection provided better pain relief after one month [standardized mean difference (SMD), −0.32; 95% confidence interval (CI), −0.59--0.06); P=0.02). No difference was detected with respect to the VAS after two months (SMD, −0.04; 95% CI, −0.35–0.27; P=0.79) or three months (SMD, −0.42; 95% CI, −1.00–0.16; P=0.15) or to the PFT (MD, 0.70; 95% CI, −1.77–0.38; P=0.20), although a tendency of favoring corticosteroid injection was observed. No obvious publication bias was detected. In conclusion, corticosteroid injection may provide pain relief for a short period of time, but the efficacy may disappear with the progression of time.
Keywords: corticosteroid injection, plantar fasciitis, meta-analysis, randomized controlled trial
Introduction
Plantar fasciitis is the most common cause of heel pain (1). It has been estimated to affect overweight individuals who spend long periods standing (1) and ∼10% of runners (2). The patients feel initial pain on the first step out of bed in the morning. The pain is relieved with gradually increased activity and worsens during long periods of standing (3). There are various treatments for plantar fasciitis, including physical therapy, orthotic devices, splinting and walking casts (4). Corticosteroid injection is usually one of the first-line treatments for plantar fasciitis. Owing to its anti-inflammatory effect, this treatment may relieve both acute and chronic pain of the heel (4); however, histological examination has shown that plantar fasciitis is not an inflammatory response but a degenerative process with microtears of the fascia and collagen necrosis, and a number of investigators have recommended that plantar fasciitis should be more exactly termed plantar fibrosis (2,5). As a result, the efficacy of corticosteroid injection has been brought into question. Corticosteroid injection is believed to provide only short-term pain relief or even no benefit (3,4). Furthermore, the patient may suffer from an increased risk of plantar fascia rupture following the treatment (6).
At present, several published randomized controlled trials (RCTs) (7–10) have compared the efficacy of corticosteroid injection with that of placebo injection for the management of plantar fasciitis; however, the efficacy of corticosteroid injection remains controversial. The present meta-analysis was performed to determine the efficacy of corticosteroid versus placebo injection for the treatment of plantar fasciitis.
Materials and methods
Search strategy
Databases, including Medline, the Cochrane Library, Google Scholar and Embase, were systematically searched for RCTs comparing the efficacy of corticosteroid and placebo injection for plantar fasciitis. The time limitation was set from the establishment of the databases to January 1, 2014. The free terms ‘plantar fasciitis’, ‘plantar fibrosis’, ‘heel pain’, ‘painful heel’, ‘corticosteroid’ and ‘steroid’ and corresponding Medical Subject Headings in different combinations were used for the literature search. The citations and reference lists of relevant articles were checked in a series for additional studies.
Inclusion criteria
The full texts of potentially relevant studies were retrieved and reviewed. Studies that met the inclusion criteria were eligible. The inclusion criteria were developed based on the PICOS framework (patient, intervention, comparison, outcome and study design) as follows: i) P, patients who felt pain in the heel and had a point of tenderness over the calcaneal medial tubercle and who were definitely diagnosed with plantar fasciitis; ii) I and C, corticosteroid injection and placebo injection were compared; iii) O, outcomes, including visual analogue score (VAS) and plantar fascial thickness (PFT), were described; iv) S, studies of an RCT design were included. Eligible studies were accepted for inclusion without language restriction.
Data extraction
Two reviewers independently extracted the demographic characteristics and outcomes. The demographic characteristics included the first author, year of publication, location, sample size, average age, male/female ratio, intervention, comparison, study design and follow-up duration.
Quality assessment
The risk of bias tool (11) was used to assess the methodological quality. All included studies were assessed in seven aspects: Random sequence generation, allocation concealment, blinding of patients, blinding of therapists, incomplete outcome data, selective reporting and other bias.
Evidence grading
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) system (12) was used to grade the evidence quality for all outcomes. Outcomes based on RCTs were of high quality. Five factors (risk of bias, inconsistency, indirectness, imprecision and publication bias) had the potential to downgrade the evidence level. Finally, four evidence levels (high, moderate, low and very low) were determined.
Statistical analysis
The outcomes were VAS and PFT. The relative risk with 95% confidence interval (CI) was calculated for dichotomous data, while the standardized mean difference (SMD) or MD with 95% CI was adopted to analyze continuous variables. The statistical heterogeneity across trials was estimated using the I2 value. A fixed-effects model was adopted when heterogeneity could be ignored (I2<50%); otherwise the randomized-effects model was used. Statistical analysis was performed with RevMan software, version 5.2 (The Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen, Denmark), and P<0.05 was considered to be statistically significant.
Results
Characteristics of the included studies
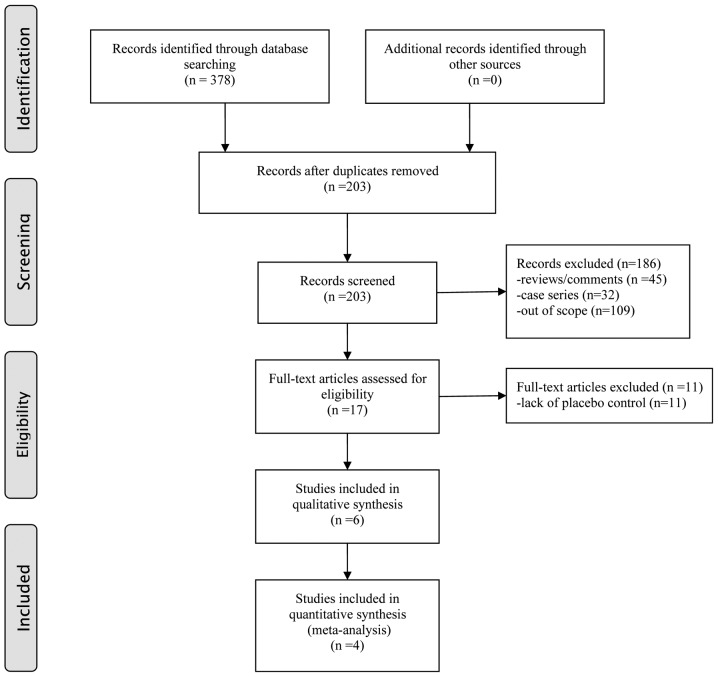
The flow diagram of the literature search is shown in Fig. 1. Four RCTs (7–10) with a total of 289 patients were ultimately considered to be eligible according to the inclusion criteria. The characteristics of the included studies are presented in Table I. All of the included studies compared corticosteroid injection and placebo injection in the treatment of plantar fasciitis. Two studies were performed in UK (7,10), one in Australia (8) and one in Kenya (9). The patients in the included studies were middle-aged and elderly, with an average age of between 43.1 and 58.2 years. The follow up duration was between two and six months.
Figure 1.
Flow diagram of literature screening process.
Table I.
General characteristics of the included studies.
| First author, year (ref.) | Location | Sample size (n) | Average age (years) | Gender (M/F) | BMI in kg/m2 (C/P) | Intervention | Comparison | Study design | Outcomes | Follow-up |
|---|---|---|---|---|---|---|---|---|---|---|
| Crawford, 1999 (7) | UK | 54 | 58.2 | - | - | 1 ml 2% lignocaine with 25 mg prednisolone acetate | 2 ml 1% lignocaine hydrochloride | RCT | VAS | 6 months |
| McMillan, 2012 (8) | Australia | 82 | 52.7 | 43/39 | 31.4/30.9 | 1 ml 4 mg/ml dexamethasone sodium phosphate | 1 ml normal saline | RCT | VAS, PFT | 12 weeks |
| Abdihakin, 2012 (9) | Kenya | 88 | 43.1 | 42/46 | 31.7 | Methylprednisolone acetate 40 mg plus conservative treatment | Saline and lidocaine plus conservative treatment | RCT | VAS | 2 months |
| Ball, 2013 (10) | UK | 65 | 49.4 | 29/36 | 31.3/32.4 | 0.5 ml (20 mg) methylprednisolone acetate and 0.5 ml saline | 1 ml 0.9% saline | RCT | VAS, PFT | 12 weeks |
(9) BMI is the overall value of the two groups. M/F, male/female; BMI, body mass index; C/P, corticosteroid/placebo; RCT, randomized controlled trial; VAS, visual analogue score; PFT, plantar fascia thickness.
Quality assessment
The results of the quality assessment are shown in Table II. Randomization was mentioned in all the studies but one study did not report the randomized sequence generation. Allocation concealment was reported in two studies. Blinding of patients was used in all studies and blinding of therapists was used in all studies. Incomplete outcome data and selective reporting were generally of low risk. The remaining items were of unclear risk.
Table II.
Risk of bias of the included studies.
| First author, year (ref.) | Random sequence generation | Allocation concealment | Blinding of patients | Blinding of therapists | Incomplete outcome data | Selective reporting | Other bias |
|---|---|---|---|---|---|---|---|
| Crawford, 1999 (7) | Low | Low | Low | Low | High | Low | Unclear |
| McMillan, 2012 (8) | Low | Low | Low | Low | Low | Low | Unclear |
| Abdihakin, 2012 (9) | Low | Unclear | Low | Low | Low | Low | Unclear |
| Ball, 2013 (10) | Low | Unclear | Low | Low | Low | Low | Unclear |
Outcome measurements
The follow-up duration varied among the included studies, and the results were pooled based on different follow-up durations. The VAS scores after one, two and three month(s) were reported in three (7–9), two (8,9) and three (7,8,10) studies, respectively. The results showed that pain relief was achieved after one month by corticosteroid injection (SMD, −0.32; 95% CI, −0.59--0.06; P=0.02) (Fig. 2); however, no difference was detected with respect to VAS score after two months (SMD, −0.04; 95% CI, −0.35–0.27; P=0.79) (Fig. 3) or three months (SMD, −0.42; 95% CI, −1.00–0.16; P=0.15) (Fig. 4), although the corticosteroid injection group tended to have a lower VAS score. The PFT was recorded in two studies (8,10) with a total of 147 patients. The patients treated with corticosteroid injection showed a tendency of a thinner PFT, although no significant difference was found (MD, −0.70; 95% CI, −1.77–0.38; P=0.20) (Fig. 5).
Figure 2.
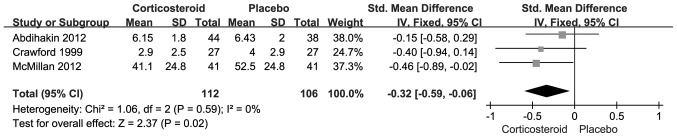
Forest plot for visual analogue score at one month between corticosteroid and placebo injection. SD, standard deviation; CI, confidence interval.
Figure 3.
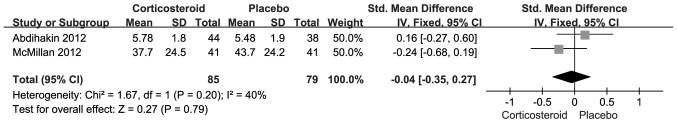
Forest plot for visual analogue score at two months between corticosteroid and placebo injection. SD, standard deviation; CI, confidence interval.
Figure 4.
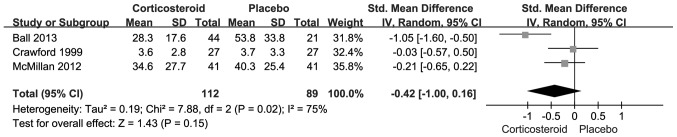
Forest plot for visual analogue score at three months between corticosteroid and placebo injection. SD, standard deviation; CI, confidence interval.
Figure 5.
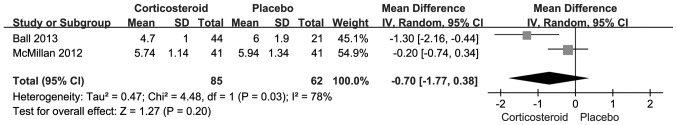
Forest plot for plantar fascia thickness between corticosteroid and placebo injection. SD, standard deviation; CI, confidence interval.
Evidence grading
Evidence grading according to the GRADE system is shown in Table III. Four outcomes in this meta-analysis were analyzed. The quality of evidence was high for the VAS after one and two months, and moderate for the VAS after three months and the PFT (Table III).
Table III.
GRADE assessment of outcomes.
| Outcome | Quality assessment | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| No. of studies | Design | Risk of bias | Inconsistency | Indirectness | Imprecision | Publication bias | Quality | Importance | |
| VAS-1 | 3 | RCT | Not serious | No serious inconsistenc | No serious indirectness | No serious imprecision | Undetected | High | Critical |
| VAS-2 | 2 | RCT | Not serious | No serious inconsistency | No serious indirectness | No serious imprecision | Undetected | High | Critical |
| VAS-3 | 3 | RCT | Not serious | Seriousa | No serious indirectness | No serious imprecision | Undetected | Moderate | Critical |
| PFT | 2 | RCT | Not serious | Seriousa | No serious indirectness | No serious imprecision | Undetected | Moderate | Important |
The heterogeneity among included studies was not negligible. RCT, randomization controlled trial; VAS-1, visual analogue score at one month; PFT, plantar fascia thickness; GRADE, Grading of Recommendations Assessment, Development and Evaluation.
Discussion
Local corticosteroid injection is a commonly used treatment for patients with plantar fasciitis. At present, several RCTs have compared corticosteroid injection with placebo injection; however, the conclusions remain controversial. This meta-analysis was therefore conducted to determine whether corticosteroid injection is superior to placebo injection. The results showed that patients benefit from corticosteroid injection in terms of the VAS after one month. No notable improvement was observed with respect to the VAS after two or months or the PFT.
The etiology of plantar fasciitis is not fully understood and may be multifactorial (2,4,13). Evidence has suggested that gender, age and weight contribute to the disease process (13). The association between plantar fasciitis and gender is controversial. No difference was detected with respect to the male/female ratio in this study. Despite a study finding the incidence rates for men and women to be 9.2 and 18.0 per 1,000 person-years, respectively (13), another retrospective analysis suggested that men are more likely to suffer plantar fasciitis than women (14). The average age of patients in the present study ranged between 43.1 and 58.2 years. It has previously been demonstrated that plantar fasciitis is a chronic degenerative process caused by repetitive microtrauma of the plantar fascia (15). The incidence rate of the condition increases with age (13). In the present study, the average body mass index was mentioned in three studies (8–10) and ranged from 30.9 to 32.4 kg/m2. The incidence of plantar fasciitis in obese individuals has been found to be 5.6-fold higher than that in the non-obese (16). Other potential risk factors, including limited ankle dorsiflexion and prolonged weight bearing, may also contribute to the disease development (13); however, these risk factors were not reported in the included studies.
In the present study, pain relief was gained with corticosteroid injection after one month but not after two or three months. Furthermore, no difference was detected with respect to the PFT. The short-term efficacy of corticosteroid injection has been previously confirmed, and was in accordance with the present results; however, this modality was primarily used for shoulder and elbow tendinitis (17). The plantar fascia is a different structure and the results may not be exactly the same. Considering the observation that corticosteroid injection tended to produce more favorable results than placebo, without significant difference, we speculated that it was due to the illusion of small sample size. Thus, the power for each outcome was calculated. The results showed that the power for PFT was 0.91, while that for the remaining outcomes was <0.8, which confirmed our speculation.
Plantar fasciitis causes heel pain and disables activity. In the present analysis, foot function was meaningful during the follow-up. Abdihakin et al (9) treated patients with plantar fasciitis with steroid injection and the Foot Function Index scores were recorded at study entry and at one and two months. The results showed that steroid injection did not improve function compared with the control group. Another RCT (18) compared corticosteroid and placebo therapy for plantar fasciitis, and foot function was assessed using the Maryland Foot Score. Compared with the placebo, corticosteroid injection improved the function score at the end of treatment but not at the one-month time-point.
Corticosteroid injection for the treatment of plantar fasciitis can significantly improve the heel pain, particularly in the short term; however, it can also cause serious complications, including plantar fascia rupture, fat pad atrophy, plantar fascia calcification, nerve injury, sterile abscess, calcaneal osteomyelitis and even impaired vision (19–22). In the present analysis, two studies (8,10) reported that no adverse event occurred. This was not mentioned in two other studies (7,9).
Plantar fasciitis is generally a self-limiting disease, and the majority of patients report spontaneous heel pain relief within one year, even without treatment (2,23); however, ∼10% of patients seek care from the physician due to unrelieved pain and disabled daily activities (2). Corticosteroid injection is considered to be one of the first-line treatments and has been found to produce satisfactory short-term results by blockading the inflammatory response and improving local edema, swelling, pain and foot function. Despite this, it has been revealed that inflammatory cells are rarely present within the lesion and that plantar fasciitis is therefore essentially a degenerative disease (5). This finding has led to the efficacy of corticosteroid injection being questioned and to the suggestion that there could be an increased risk of certain adverse events with this method. The treatment should therefore not be used until it has been confirmed to be effective.
The present meta-analysis was a secondary research based on published studies and was certainly flawed. Firstly, only four studies with a total of 289 patients were finally included; thus, the power for all outcomes may be limited by the small sample size. Secondly, the heterogeneity between the included studies cannot be ignored. This heterogeneity may have been caused by a number of factors, including different treatment algorithms, clinical skills and physician experience. A physician with more experience and skills would be considerably more likely to administer an accurate injection with few adverse events. Furthermore, the outcomes were mainly VAS, which is somewhat subjective. Other objective changes included tenderness threshold, heel tenderness index and heel pad thickness, which were not reported in all the included studies. In addition, measurements on safety, economy and quality of life were seldom provided. Despite the weaknesses, the present meta-analysis did reveal that patients with plantar fasciitis may benefit from local corticosteroid injection with respect to the pain symptoms, at least in the short term.
In conclusion, the present meta-analysis has found that corticosteroid injection may provide short-term pain relief; however, the effect may vanish with the progression of time. Further studies are required to confirm the present findings.
References
- 1.Schwartz EN, Su J. Plantar fasciitis: A concise review. Perm J. 2014;18:e105–e107. doi: 10.7812/TPP/13-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Martinelli N, Bonifacini C, Romeo G. Current therapeutic approaches for plantar fasciitis. Orthop Res Rev. 2014;6:33. doi: 10.2147/ORR.S43126. [DOI] [Google Scholar]
- 3.Buchbinder R. Clinical practice. Plantar fasciitis. N Engl J Med. 2004;350:2159–2166. doi: 10.1056/NEJMcp032745. [DOI] [PubMed] [Google Scholar]
- 4.Kirkland P, Beeson P. Use of primary corticosteroid injection in the management of plantar fasciopathy: Is it time to challenge existing practice? J Am Podiatr Med Assoc. 2013;103:418–429. doi: 10.7547/1030418. [DOI] [PubMed] [Google Scholar]
- 5.Lemont H, Ammirati KM, Usen N. Plantar fasciitis: A degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc. 2003;93:234–237. doi: 10.7547/87507315-93-3-234. [DOI] [PubMed] [Google Scholar]
- 6.Tatli YZ, Kapasi S. The real risks of steroid injection for plantar fasciitis, with a review of conservative therapies. Curr Rev Musculoskelet Med. 2009;2:3–9. doi: 10.1007/s12178-008-9036-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crawford F, Atkins D, Young P, Edwards J. Steroid injection for heel pain: Evidence of short-term effectiveness. A randomized controlled trial. Rheumatology (Oxford) 1999;38:974–977. doi: 10.1093/rheumatology/38.10.974. [DOI] [PubMed] [Google Scholar]
- 8.McMillan AM, Landorf KB, Gilheany MF, Bird AR, Morrow AD, Menz HB. Ultrasound guided corticosteroid injection for plantar fasciitis: Randomised controlled trial. BMJ. 2012;344:e3260. doi: 10.1136/bmj.e3260. [DOI] [PubMed] [Google Scholar]
- 9.Abdihakin M, Wafula K, Hasan S, MacLeod J. A randomised controlled trial of steroid injection in the management of plantar fasciitis. SA Orthop J. 2012;11:33–38. [Google Scholar]
- 10.Ball EM, McKeeman HM, Patterson C, et al. Steroid injection for inferior heel pain: A randomised controlled trial. Ann Rheum Dis. 2013;72:996–1002. doi: 10.1136/annrheumdis-2012-201508. [DOI] [PubMed] [Google Scholar]
- 11.Higgins JP, Altman DG, Gøtzsche PC, et al. Cochrane Bias Methods Group; Cochrane Statistical Methods Group: The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Atkins D, Best D, Briss PA, et al. GRADE Working Group: Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beeson P. Plantar fasciopathy: Revisiting the risk factors. Foot Ankle Surg. 2014;20:160–165. doi: 10.1016/j.fas.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 14.Taunton JE, Ryan MB, Clement DB, McKenzie DC, Lloyd-Smith DR, Zumbo BD. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med. 2002;36:95–101. doi: 10.1136/bjsm.36.2.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosenbaum AJ, DiPreta JA, Misener D. Plantar heel pain. Med Clin North Am. 2014;98:339–352. doi: 10.1016/j.mcna.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 16.Riddle DL, Pulisic M, Pidcoe P, Johnson RE. Risk factors for Plantar fasciitis: A matched case-control study. J Bone Joint Surg Am. 2003;85-A:872–877. doi: 10.2106/00004623-200305000-00015. [DOI] [PubMed] [Google Scholar]
- 17.Gaujoux-Viala C, Dougados M, Gossec L. Efficacy and safety of steroid injections for shoulder and elbow tendonitis: A meta-analysis of randomised controlled trials. Ann Rheum Dis. 2009;68:1843–1849. doi: 10.1136/ard.2008.099572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gudeman SD, Eisele SA, Heidt RJ, Colosimo AJ, Stroupe AL. Treatment of plantar fasciitis by iontophoresis of 0.4% dexamethasone. A randomized, double-blind, placebo-controlled study. Am J Sports Med. 1997;25:312–316. doi: 10.1177/036354659702500307. [DOI] [PubMed] [Google Scholar]
- 19.Molloy LA. Managing chronic plantar fasciitis: when conservative strategies fail. JAAPA. 2012;25:52–53. doi: 10.1097/01720610-201211000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Gidumal R, Evanski P. Calcaneal osteomyelitis following steroid injection: a case report. Foot Ankle. 1985;6:44–46. doi: 10.1177/107110078500600109. [DOI] [PubMed] [Google Scholar]
- 21.Buccilli Ta, Jr, Hall HR, Solmen JD. Sterile abscess formation following a corticosteroid injection for the treatment of plantar fasciitis. J Foot Ankle Surg. 2005;44:466–468. doi: 10.1053/j.jfas.2005.07.020. [DOI] [PubMed] [Google Scholar]
- 22.Anupama B, Puthran N, Hegde V, Andrews S. Plantar fasciitis and impaired vision: A case report. Foot (Edinb) 2010;20:151–153. doi: 10.1016/j.foot.2010.09.001. [DOI] [PubMed] [Google Scholar]
- 23.Goff JD, Crawford R. Diagnosis and treatment of plantar fasciitis. Am Fam Physician. 2011;84:676–682. [PubMed] [Google Scholar]