Abstract
Background
Extensive evidence shows that well over 50% of people prefer to be cared for and to die at home provided circumstances allow choice. Despite best efforts and policies, one‐third or less of all deaths take place at home in many countries of the world.
Objectives
1. To quantify the effect of home palliative care services for adult patients with advanced illness and their family caregivers on patients' odds of dying at home; 2. to examine the clinical effectiveness of home palliative care services on other outcomes for patients and their caregivers such as symptom control, quality of life, caregiver distress and satisfaction with care; 3. to compare the resource use and costs associated with these services; 4. to critically appraise and summarise the current evidence on cost‐effectiveness.
Search methods
We searched 12 electronic databases up to November 2012. We checked the reference lists of all included studies, 49 relevant systematic reviews, four key textbooks and recent conference abstracts. We contacted 17 experts and researchers for unpublished data.
Selection criteria
We included randomised controlled trials (RCTs), controlled clinical trials (CCTs), controlled before and after studies (CBAs) and interrupted time series (ITSs) evaluating the impact of home palliative care services on outcomes for adults with advanced illness or their family caregivers, or both.
Data collection and analysis
One review author assessed the identified titles and abstracts. Two independent reviewers performed assessment of all potentially relevant studies, data extraction and assessment of methodological quality. We carried out meta‐analysis where appropriate and calculated numbers needed to treat to benefit (NNTBs) for the primary outcome (death at home).
Main results
We identified 23 studies (16 RCTs, 6 of high quality), including 37,561 participants and 4042 family caregivers, largely with advanced cancer but also congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD), HIV/AIDS and multiple sclerosis (MS), among other conditions. Meta‐analysis showed increased odds of dying at home (odds ratio (OR) 2.21, 95% CI 1.31 to 3.71; Z = 2.98, P value = 0.003; Chi2 = 20.57, degrees of freedom (df) = 6, P value = 0.002; I2 = 71%; NNTB 5, 95% CI 3 to 14 (seven trials with 1222 participants, three of high quality)). In addition, narrative synthesis showed evidence of small but statistically significant beneficial effects of home palliative care services compared to usual care on reducing symptom burden for patients (three trials, two of high quality, and one CBA with 2107 participants) and of no effect on caregiver grief (three RCTs, two of high quality, and one CBA with 2113 caregivers). Evidence on cost‐effectiveness (six studies) is inconclusive.
Authors' conclusions
The results provide clear and reliable evidence that home palliative care increases the chance of dying at home and reduces symptom burden in particular for patients with cancer, without impacting on caregiver grief. This justifies providing home palliative care for patients who wish to die at home. More work is needed to study cost‐effectiveness especially for people with non‐malignant conditions, assessing place of death and appropriate outcomes that are sensitive to change and valid in these populations, and to compare different models of home palliative care, in powered studies.
Keywords: Adult, Female, Humans, Male, Attitude to Death, Caregivers, Cost-Benefit Analysis, Critical Illness, Critical Illness/nursing, Home Care Services, Home Care Services/economics, Palliative Care, Palliative Care/economics, Palliative Care/methods, Patient Preference, Randomized Controlled Trials as Topic, Treatment Outcome
Plain language summary
Effectiveness and cost‐effectiveness of home‐based palliative care services for adults with advanced illness and their caregivers
When faced with the prospect of dying with an advanced illness, the majority of people prefer to die at home, yet in many countries around the world they are most likely to die in hospital. We reviewed all known studies that evaluated home palliative care services, i.e. experienced home care teams of health professionals specialised in the control of a wide range of problems associated with advanced illness – physical, psychological, social, spiritual. We wanted to see how much of a difference these services make to people's chances of dying at home, but also to other important aspects for patients towards the end of life, such as symptoms (e.g. pain) and family distress. We also compared the impact on the costs with care. On the basis of 23 studies including 37,561 patients and 4042 family caregivers, we found that when someone with an advanced illness gets home palliative care, their chances of dying at home more than double. Home palliative care services also help reduce the symptom burden people may experience as a result of advanced illness, without increasing grief for family caregivers after the patient dies. In these circumstances, patients who wish to die at home should be offered home palliative care. There is still scope to improve home palliative care services and increase the benefits for patients and families without raising costs.
Summary of findings
Summary of findings 1. Summary of findings.
| Outcomes: home palliative care vs. usual care | |||||
|
Patient or population: adult patients with a severe or advanced disease (malignant or non‐malignant) Settings: Canada, Italy, Norway, Sweden, UK, US Intervention: home palliative care Comparison: usual care, which could include community care (primary or specialist care at home and in nursing homes), hospital care (inpatient and outpatient) and in some instances palliative or hospice care (or both) | |||||
| Outcomes | Number needed to treat to benefit (NNTB)a (95% CI) | Odds ratio (95% CI) | No of participants (studies) |
Level of evidenceb (adapted fromVan Tulder 2003) |
Comments |
|
Home death follow‐up: 3 to 24 months Analysis 1.1 and Analysis 1.2 |
With study population control risk (307 home deaths/1000 deaths) NNTB 5 (3 to 14), meaning that for one additional patient to die at home five more would need to receive home palliative care as opposed to usual care With low home death population assumed control risk (ACR) (128 home deaths/1000 deaths) NNTB 9 (5 to 26) With medium home death population ACR (278 home deaths/1000 deaths) NNTB 6 (3 to 15) With high home death population ACR (454 home deaths/1000 deaths) NNTB 5 (3 to 13) |
OR 2.21 (1.31 to 3.71) |
1222 (7 studies, 3 of high quality; 5 RCTs and 2 CCTs) |
Strong | The majority of patients had cancer but 3 trials also included non‐cancer conditions. 3 interventions provided specialist palliative care and 4 provided intermediate palliative care The direction of the effect was consistent across all studies but did not reach statistical significance in 3; ORs ranged from 1.36 (95% CI 0.80 to 2.31) to 2.86 (95% CI 0.78 to 10.53) Sensitivity analyses showed that exclusion of the 2 CCTs (both of Swedish hospital‐based services with a pooled OR 3.44, 95% CI 0.60 to 19.57) and inclusion of only high quality RCTs resulted in a reduction of the OR to 1.28 (95% CI 1.28 to 2.33) and 1.75 (95% CI 1.24 to 2.47) respectively, with more precision and less heterogeneity |
|
Symptom burden follow‐up: 1 month from enrolment to the week of death Table 2 |
Not calculated, data were not pooled due to the high degree of heterogeneity. See comments | 2107 (4 studies, 2 of high quality; 3 RCTs and 1 CBA) |
Strong | Strong evidence of a positive effect on symptom burden: statistically significant reduction of symptom burden in 3 studies (one UK RCT of high quality) further to marginally significant positive effect among 209 patients in Bakitas 2009 (US RCT of high quality; P value = 0.06) Effect sizes were small (ranging from difference in mean scores of 0.08 in a 0 to 7 scale to a difference of 2.1 in a 0 to 20 scale). All studies used different measures 1 study evaluated a specialist palliative care intervention for patients with MS. The other 3 included only patients with cancer (1 evaluated a specialist service and 2 evaluated intermediate palliative care) |
|
|
Pain follow‐up: 1 week from enrolment to week of death Table 3 |
Not calculated, data were not pooled due to the high degree of heterogeneity. See comments | 2735 (9 studies; 4 high quality; 8 RCTs and 1 CBA) |
Conflicting | 2 UK RCTs (one of high quality) and Greer 1986 found statistically significant positive effects (the latter favouring the hospital‐based intervention); a marginally significant positive effect was found among 83 patients in McKegney 1981 in the last month before death (high quality RCT; P value = 0.06). The remaining 6 trials (including 1 high quality RCT) found no statistically significant group differences High variability in outcome measures (only the McGill‐Melzack Pain Questionnaire was used more than once) |
|
|
Physical function follow‐up: 1 month from enrolment to week of death Table 4 |
Not calculated, data were not pooled due to the high degree of heterogeneity. See comments | 2408 (7 studies, 3 high quality; 6 RCTs and 1 CBA) |
Inconclusive | Statistical significance unknown in 2 out of 7 studies hence the evidence was deemed inconclusive 3 RCTs in the UK, Norway and the US (all of high quality) found no statistically significant group differences, while two RCTs of intermediate palliative care services in the US (McCorkle 1989; Aiken 2006) detected significantly better physical functioning trajectories in the intervention group through longitudinal analysis up to 9 months following enrolment |
|
|
Quality of life follow‐up: 1 month from enrolment to week of death Table 5 |
Not calculated, data were not pooled due to the high degree of heterogeneity. See comments | 2487 (7 studies; 3 of high quality; 6 RCTs and 1 CBA) |
Inconclusive | Statistical significance unknown in 2 out of 7 studies hence the evidence was deemed inconclusive. 3 RCTs (2 of high quality) found no statistically significant group differences 2 US RCTs, 1 of a specialist service (high quality; Bakitas 2009) and 1 of an intermediate service (Aiken 2006) detected significantly better quality of life through longitudinal analysis up to the month of death Effects were statistically significant both forwards from enrolment and backwards from death in analyses by Bakitas 2009; they were statistically significant in physical functioning, general health and vitality but not in pain‐related, social, emotional and mental health dimensions of quality of life in Aiken 2006 |
|
|
Caregiver burden follow‐up: 1 month from enrolment to the patients' "last weeks of life" Table 6 |
Not calculated, data were not pooled due to the high degree of heterogeneity. See comments | 1888 (3 studies; 2 of high quality; 2 RCTs and 1 CBA) |
Conflicting | Conflicting findings from 2 high quality RCTs of specialist home palliative care interventions, 1 in the US with cancer patients (Bakitas 2009 reported no group main effects or group by time interactions 1‐10 months after enrolment) and 1 in the UK with MS patients (Higginson 2009 found differences in change scores from baseline at 12 weeks' follow‐up (P value = 0.01) Greer 1986 found a small but significant difference in the last weeks of the patient's life, with higher caregiver burden in the community‐based intervention |
|
|
Caregiver grief follow‐up: from moment the patient died to 13 months after Table 7 |
Not calculated, data were not pooled due to the high degree of heterogeneity. See comments | 2113 (4 studies, 2 of high quality; 3 RCTs and 1 CBA) | Strong | Strong evidence of no effect on caregiver grief: no statistically significant differences in three RCTs in the UK and the US (two of high quality) Outcome measures varied (only the Texas Revised Inventory of Grief was used more than once but scored in different ways) Greer 1986 found significant higher emotional distress as measured by the modified Grief Experience Inventory among caregivers in the community‐based intervention assessed 90 to 120 days after the patient died |
|
|
Satisfaction with care follow‐up: 1 month from enrolment to approximately 4‐6 months after the patient died(caregiver report) Table 8 |
Not calculated, data were not pooled due to the high degree of heterogeneity. See comments | 2497 (6 studies; 4 of high quality; 5 RCTs and 1 CBA) |
Conflicting | 3 RCTs (2 of high quality) found statistically significant positive effects; the other 2 RCTs (bothhigh quality studies in the US) reported no statistically significant differences. Positive effects were related to a hospital‐based specialist service in Norway (Jordhøy 2000) and 2 intermediate services in the US (Brumley 2007; Hughes 1992) Greer 1986 found significant higher satisfaction with care among caregivers in the hospital‐based intervention assessed 90‐120 days after the patient died |
|
CBA: controlled before and after study; CCT: controlled clinical trial; CI: confidence interval; MS: multiple sclerosis; OR: odds ratio; RCT: randomised controlled trial. aNumbers needed to treat to benefit (NNTBs) were calculated for the study population control risk and for three other assumed control risks (ACR). These were based on recent cancer home deaths rates from a population‐based study across six European countries (Cohen 2010): 1) low home death population assumed the lowest rate of 128 deaths at home per 1000 cancer deaths (Norway); 2) medium home death population assumed the mean across the six European countries (278 deaths at home per 1000 cancer deaths); 3) high home death population assumed the highest rate of 454 deaths at home per 1000 cancer deaths (the Netherlands). We applied rates related to cancer as the included studies involved largely cancer patients. bLevels of evidence: Strong: findings from meta‐analysis or consistent findings across all studies including at least two high quality RCTs Moderate: consistent findings across all studies including at least two low quality RCTs/CCTs or one high quality RCT Limited: one RCT/CCT not reaching high quality Conflicting: inconsistent findings among at least two studies with at least one RCT/CCT Inconclusive: statistical significance of differences unknown in > 25% of all studies No evidence from trials: no RCTs or CCTs Consistent (conflates assessment of direction and precision): statistically significant effect in same direction in ≥ 75% of all studies High quality RCTs/CCTs: ≥ 3.5 methodological quality score (ranging from zero to six)
1.1. Analysis.

Comparison 1: Home palliative care versus usual care, Outcome 1: Death at home
1.2. Analysis.

Comparison 1: Home palliative care versus usual care, Outcome 2: death at home with only high quality RCTs
1. Symptom burden: home palliative care versus usual care.
| Study and country | Measure |
Analysis |
Follow‐up | Significance and direction | Details |
|
Bakitas 2009 US (high quality) |
Edmonton Symptom Assessment Scale (ESAS) measure of 9 symptoms (rated from 0 to 9): pain, activity, nausea, depression, anxiety, drowsiness, appetite, sense of well‐being, shortness of breath; scores: from 0 to 900, higher scores equal greater symptom intensity; patient report |
Forwards from enrolment | 1 month | Marginally significant difference favours interventiona Mean treatment effect (intervention‐control) −27.8 (SE 5); P value = 0.06 |
Intervention (n = 109): LSM 241.81 (95% CI 216.35 to 267.28) Control (n = 100): LSM 288.53 (95% CI 262.03 to 315.03) |
| 4 months | Intervention (n = 73): LSM 254.67 (95% CI 224.55 to 284.78) Control (n = 76): LSM 271.87 (95% CI 242.11 to 301.64) |
||||
| 7 months | Intervention (n = 62): LSM 238.77 (95% CI 206.60 to 270.95) Control (n = 54): LSM 268.59 (95% CI 234.34 to 302.83) |
||||
| 10 months | Intervention (n = 48): LSM 271.57 (95% CI 235.83 to 307.31) Control (n = 45): LSM 294.20 (95% CI 257.27 to 331.12) |
||||
| 13 months | Intervention (n = 28): LSM 295.56 (95% CI 250.65 to 340.47) Control (n = 31): LSM 251.66 (95% CI 208.51 to 294.82) |
||||
| Backwards from death | Third last assessment | n.s.a Mean treatment effect (intervention‐control) −24.2 (SE 20.5) P value = 0.24 |
Intervention (n = 52): LSM 262.76 (95% CI 222.61 to 302.91) Control (n = 48): LSM 263.90 (95% CI 222.13 to 305.68) |
||
| Second last assessment | Intervention (n = 81): LSM 274.69 (95% CI 240.63 to 308.76) Control (n = 75): LSM 304.93 (95% CI 269.53 to 340.33) |
||||
| Last assessment | Intervention (n = 80): LSM 322.29 (95% CI 288.08 to 356.51) Control (n = 74): LSM 353.90 (95% CI 318.33 to 389.47) |
||||
|
Higginson 2009 UK (high quality) |
Palliative care Outcome Scale MS Symptoms subscale(POS‐MS‐S5) measure of 5 symptoms (rated from 0 to 4): pain, nausea, vomiting, mouth problems and sleeping difficulty; scores: from 0 to 20, higher scores equal greater symptom intensity; patient report |
Forwards from enrolment | 6 weeks | n.s.b ES ‐0.5 F = 1.08 P value = 0.31 |
M change from baseline Intervention (n = 24): M ‐0.7 (SD 2.3; 95% CI ‐1.7 to 0.3) Control (n = 20): M 0.6 (SD 3.2; 95% CI ‐1.0 to 2.1) |
| 12 weeks | Favours interventionb ES ‐0.8 F = 4.75 P value = 0.04 |
M change from baseline Intervention (n = 25): M ‐1.0 (SD 2.7; 95% CI ‐2.1 to 0.1) Control (n = 21): M 1.1 (SD 2.8; 95% CI ‐0.2 to 2.4) |
|||
|
McCorkle 1989 US |
Symptom Distress Scale measure of 13 symptoms (not stated which); scores: from 13 to 65, higher scores equal greater symptom distress; patient report |
Forwards from enrolment |
6 weeks | Favours interventionc F = 5.01 P value = 0.03 Graphs showed that the entire sample experienced increased symptom distress over time but control2 (i.e. those receiving usual outpatient care) experienced elevated distress 1 occasion sooner (at 6 weeks) than the intervention and control1 (i.e. those receiving cancer home care) |
Adjusted estimates Intervention: M 26.1 Control1 (cancer home care): M 24.88 Control2, (usual outpatient care): M 24.32 |
| 12 weeks | Adjusted estimates Intervention: M 24.23 Control1 (cancer home care): M 24.71 Control2 (usual outpatient care): M 26.79 |
||||
| 18 weeks | Adjusted estimates Intervention: M 25.42 Control1 (cancer home care): M 26.14 Control2 (usual outpatient care): M 26.70 |
||||
| Greer 1986 (CBA) |
Composite symptom severity scale modified from Melzack‐McGill Questionnaire measure of symptoms including nausea or vomiting, constipation, dizziness, fever or chills, dry mouth, breathlessness; scores: from 0 to 7, higher scores equal greater symptom severity; caregiver report |
Backwards from death |
3 weeks | Favours hospital‐based interventiond "patients in HB hospices were likely to experience fewer symptoms than HC or CC patients, although at one week prior to death this difference was statistically significant only in the HB‐CC comparison. Subgroup analyses revealed that statistically significant differences persisted regardless of the level of symptoms at intake" (Greer 1986) |
Adjusted estimatesd Community‐based intervention: M 2.89 (SE 0.09) Hospital‐based intervention: M 2.46 (SE 0.13) Control (conventional care): M 2.97 (SE 0.16) |
| 1 week | Favours intervention regardless service basedd see comment above |
Adjusted estimatesd Community‐based intervention: M 3.05 (SE 0.08) Hospital‐based intervention: M 2.78 (SE 0.12) Control (conventional care): M 3.38 (SE 0.15) |
ANCOVA: analysis of covariance; CBA: controlled before and after study; CC: conventional care (control); CI: confidence interval; ES: estimated effect size; HB: hospital‐based (hospital‐based intervention); HC: home care (community‐based intervention); LSM: estimated least mean square; M: mean; n.s.: not significant; SD: standard deviation; SE: standard error. aResults from repeated measures analysis of covariance (mixed‐effects model applied to longitudinal data using random‐subject effects to account for correlation between repeated outcome measurements on same individual). bResults from F‐tests of non‐imputed data; authors stated that imputed data gave similar results. cThe authors used repeated measures analysis and analysis of variance; analysis included 78 patients who completed the three follow‐up interviews (i.e. up to 18 weeks after enrolment); adjusted means were used due to baseline differences despite randomisation. dThe authors undertook hypothesis testing on adjusted estimates of outcomes in each of the groups derived through linear regression; estimates adjusted for sample differences; standard errors based on the linear regression equation.
2. Pain: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Higginson 2009 UK (high quality) |
Palliative care Outcome Scale (POS) pain item score: from 0 to 4, higher score equals greater pain; negative change equals reduction; patient report |
Forwards from enrolment |
6 weeks | n.s. | Mean change from baseline Intervention (n = 25): ‐0.23 (95% CI ‐0.66 to 0.20) Control (n = 23): 0.09 (95% CI ‐0.36 to 0.54) |
| 12 weeks | Favours intervention F = 5.15; P value = 0.028 |
Mean change from baseline Intervention (n = 26): ‐0.46 (95% CI ‐0.98 to 0.05) Control (n = 24): 0.30 (95% CI ‐0.16 to 0.76) Adjusted for baseline scores, the difference between scores was 0.56 (95% CI ‐ 0.75 to 1.19) |
|||
|
Jordhøy 2000 Norway (high quality) |
EORTC QLQ‐C30 2‐item pain scale transformed score: from 0 to 100, higher score equals greater pain; patient report |
Forwards from enrolment |
1 month | n.s.a P value = 0.35 |
Intervention (n = 153): M 36 Control (n = 116): M 36 |
| 2 months | Intervention (n = 108): M 38 Control (n = 93): M 37 |
||||
| 4 months | Intervention (n = 71): M 41 Control (n = 65): M 37 |
||||
| 6 months | Differences and statistical significance not stated | Intervention (n = 56): M 39 Control (n = 52): M 34 |
|||
|
McKegney 1981 US (high quality) |
Sternbach Pain Estimate score score: from 0 to 100; higher score equals greater pain; patient report |
Backwards from death | 180 to 150 days | Authors stated there were no differences but statistical significance was not stated |
"The two groups had essentially the same mean pain scores until the last 90 days before death." (McKegney 1981); this statement is corroborated by graph of mean pain scores in the 2 groups |
| 150 to 120 days | |||||
| 120 to 90 days | |||||
| 90 to 60 days | Authors stated there were differences but statistical significance was not stated | "The 'Intensive' group of patients has lower mean pain scores than the 'non‐intensive' group over the last 90 days before death. In these last 90 days, the mean pain scores in the non‐intensive group of patients continued to rise until death, whereas the mean pain scores in the intensive group of patients plateaued" (McKegney 1981). The difference in the 30 to 0 days period was marginally significant (P value = 0.06) | |||
| 60 to 30 days | |||||
| 30 to 0 days | Marginally significant difference favours intervention P value = 0.06 |
||||
|
Rabow 2004 US (high quality) |
Brief Pain Inventory measure with 6 items: worst pain, least pain and "average" pain in last 24 hours (from 0 to 10); 'right now' pain (from 0 to 10); relief (from 0 to 100); interference with activities (from 0 to 70); higher scores equal greater pain; patient report |
Forwards from enrolment |
6 months | n.s.b P values ranged from 0.94 (ANCOVA between groups for interference with activities) to 0.10 (ANCOVA between groups for least pain in last 24 hours) |
Mean adjusted for baseline differences Intervention (n = 50) vs. control (n = 40)
|
| 12 months | Mean adjusted for baseline differences Intervention (n = 50) vs. control (n = 40)
|
||||
|
Aiken 2006 US |
SF‐36 2‐item bodily pain subscale transformed score: from 0 to 100; lower score equal greater pain; negative slope equals reduction; patient report |
Forwards from enrolment |
3 months | n.s.c | Growth modelling analysis (separate for COPD and CHF patients) COPD slope: intervention: 2.98 vs. control: ‐0.45 CHF slope: intervention: ‐0.57 vs. control: ‐0.45 |
| 6 months | |||||
| 9 months | |||||
|
Grande 1999 UK |
Cartwright/Addington Hall surveys pain item 4‐point item, score range not stated; higher score equal greater pain; caregiver report 6 weeks after death |
Backwards from death |
Last 2 weeks | Favours intervention P value < 0.05 |
Intervention (n = 107): M 2.52 (SD 0.93) Control (n = 21): M 3.00 (SD 1.10) Although analysis used Mann–Whitney U‐tests, authors reported Ms and SDs for clarity |
|
McCorkle 1989 US |
McGill‐Melzack Pain Questionnaire score: range not stated; higher score equal greater pain; patient report |
Forwards from enrolment |
6 weeks | n.s. |
"The three groups did not differ significantly with respect to McGill‐Melzack Pain Questionnaire" (McCorkle 1989); no data provided to support this statement |
| 12 weeks | |||||
| 6 months | |||||
|
McWhinney 1994 Canada |
McGill‐Melzack Pain Questionnaire score: range not stated; higher score equals greater pain; patient/caregiver report through diary |
Forwards from enrolment |
1 month | n.s. | "There were no clinically or statistically significant differences between the experimental and control groups on any of the measures at one month" (McWhinney 1994); no data provided to support this statement High attrition (53 /146) mainly due to death; 2 months data not analysed due to further attrition |
|
Greer 1986 (CBA) |
McGill‐Melzack Pain Questionnaire score range not stated; higher score equals greater pain; patient report |
Forwards from enrolment |
1 week | n.s.d | "the average level of pain for all three patient groups was between mild and discomforting with no statistically significant differences among the groups" (Morris 1986, Greer 1986); no data provided to support this statement |
| 5 weeks | |||||
| 1) Composite pain index modified from Spitzer Quality of Life Index score: from 0 to 4; higher score equals greater pain; caregiver report 2) Item on being pain‐free score: yes/no; caregiver report 3) Item on persistent pain score: yes/no; caregiver report |
Backwards from death |
3 weeks |
Composite pain index n.s.d Pain‐free n.s.d Persistent pain favours hospital‐based interventiond P value < 0.01 |
Adjusted estimatesd Composite pain index Community‐based intervention: M 1.41 (SE 0.08) Hospital‐based intervention: M 1.10 (SE 0.10) Control (conventional care): M 1.53 (SE 0.16) Patients pain‐free Community‐based intervention: 7% (SE 0.02) Hospital‐based intervention: 12% (SE 0.02) Control (conventional care): 9% (SE 0.04) Patients with persistent pain Community‐based intervention: 7% (SE 0.02) Hospital‐based intervention: 3% (SE 0.02) Control (conventional care): 14% (SE 0.04) |
|
| 1 week |
Composite pain index n.s.d Pain‐free n.s.d Persistent pain favours hospital‐based interventiond P value < 0.001 |
Adjusted estimatesd Composite pain index Community‐based intervention: M 1.61 (SE 0.06) Hospital‐based intervention: M 1.48 (SE 0.07) Control (conventional care): M 1.65 (SE 0.12) Patients pain‐free Community‐based intervention: 9% (SE 0.01) Hospital‐based intervention: 10% (SE 0.02) Control (conventional care): 16% (SE 0.04) Patients with persistent pain Community‐based intervention: 13% (SE 0.02) Hospital‐based intervention: 5% (SE 0.02) Control (conventional care): 22% (SE 0.05) Patient self reports failed to confirm these findings, but at 1 week to death 80% patients could not report |
ANCOVA: analysis of covariance; CBA: controlled before and after study; CHF: congestive heart failure; CI: confidence interval; COPD: chronic obstructive pulmonary disease; M: mean; n.s.: not significant; SD: standard deviation; SE: standard error.
aThe authors calculated mean changes from baseline at one to four months after enrolment by dividing the area under the curve scores by time; differences between groups were tested by bootstrap estimation to fit regression models allowing for clustering and predictive factors. bANCOVAs tested for differences between groups and for group by time interaction, controlling for baseline differences in pain but not for clustering. cThe authors used growth modelling analysis, calculated slopes of "average" linear trajectory within a group, averaged across slopes of individual linear trajectories of individual within the group and compared intercepts at each time point and slopes for COPD and CHF patients separately. dThe authors undertook hypothesis testing on adjusted estimates of outcomes in each of the groups derived through linear regression; estimates adjusted for sample differences; standard errors based on the linear regression equation for continuous variables and on logistic regression equation for dichotomous variables.
3. Physical function: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Higginson 2009 UK (high quality) |
MS Impact Scale (MSIS) Physical subscale score: range not stated; higher scores equal greater physical impact; patient report |
Forwards from enrolment | 6 weeks |
n.s.a ES 0.2 F = 0.15 P value = 0.70 |
M change from baseline Intervention (n = 16): M 1.3 (SD 17.0; 95% CI ‐7.7 to 10.4) Control (n = 7): M ‐1.7 (SD 17.5; 95% CI ‐17.9 to 10.4) |
| 12 weeks | n.s.a ES 0.4 F = 0.37 P value = 0.55 |
M change from baseline Intervention (n = 16): M ‐0.3 (SD 17.5; 95% CI ‐9.7 to 9.0) Control (n = 7): M ‐7.1 (SD 21.3; 95% CI ‐26.8 to 12.5) |
|||
|
Jordhøy 2000 Norway (high quality) |
EORTC‐QLQ‐C30 Physical functioning scale (5 items) transformed score: from 0 to 100; higher scores equal better functioning; patient report |
Forwards from enrolment | 1 month |
n.s.b SAUC intervention ‐8.9 vs. SAUC control ‐6.4 P value = 0.42 |
Intervention: M 47 Control: M 49 |
| 2 months |
Intervention: M 51 Control: M 52 |
||||
| 4 months |
Intervention: M 49 Control: M 54 |
||||
| 6 months | Differences and statistically significance not stated | Intervention: M 53 Control: M 56 |
|||
|
McKegney 1981 US (high quality) |
Karnofsky Performance Status (KPS) score: from 0 to 100; higher scores equal better performance status; patient report |
Backwards from death |
180 to 150 days | Authors stated there were no differences but statistical significance was not stated |
"It should be briefly noted that the intensive and non‐intensive patients did not differ in (...) overall health status as defined by the KPS" (McKegney 1981); no data provided to support this statement |
| 150 to 120 days | |||||
| 120 to 90 days | |||||
| 90 to 60 days | |||||
| 60 to 30 days | |||||
| 30 to 0 days | |||||
|
Aiken 2006 US |
SF‐36 2 subscales: physical functioning and role‐physical transformed score: from 0 to 100; lower scores equal lower physical functioning; negative slope equal reduction; patient report |
Forwards from enrolment | 3 months |
Physical functioning Favours intervention slope: z 2.50; P value < 0.05 Intercept at 9 months: z 2.16; P value < 0.05; g 0.41 Role‐physical n.s. |
Growth modelling analysis (separate for COPD and CHF patients) Physical functioning COPD slope: intervention: 1.00 vs. control: ‐0.95 CHF slope: intervention: 0.18 vs. control: ‐1.39 Control slope declined while intervention slope rose Role‐physical COPD slope: intervention: 0.57 vs. control: ‐0.14 CHF slope: intervention: ‐0.51 vs. control: 1.60 |
| 6 months | |||||
| 9 months | |||||
|
Hughes 1992 US |
Barthels Self Care Index score: range not stated; higher scores equal greater dependency; patient report |
Forwards from enrolment | 1 month |
n.s. Beta ‐0.58 t ‐0.11 P value = 0.92 |
ANCOVA (age, education, race, marital status, retirement due to health, prior private sector hospital use, living arrangement, and baseline care satisfaction scores – none of these factors were predictive of outcomes); descriptive data not provided |
| 6 months | n.s. t < 1 |
Intervention (n = 18): M 72.00 Control (n = 16): M 69.31 Data were analysed using t‐tests because the sample did not support regression models |
|||
|
McCorkle 1989 US |
Enforced Social Dependency Scale (10 items) score: from 10 to 54; higher scores equal greater functional dependency on others; patient report |
Forwards from enrolment |
6 weeks | Favours interventionc F = 5.72; P value = 0.02 Graphs showed that social dependency worsens in the control2 group (i.e. those receiving usual outpatient care) 6 weeks earlier than in the 2 treatment groups |
Adjusted estimates Intervention: M 22.33 Control1 (home cancer care): M 21.68 Control2 (usual outpatient care): M 21.74 |
| 12 weeks | Adjusted estimates Intervention: M 22.67 Control1 (home cancer care): M 20.97 Control2 (usual outpatient care): M 24.85 |
||||
| 18 weeks | Adjusted estimates Intervention: M 24.57 Control1 (home cancer care): M 24.90 Control2 (usual outpatient care): M 25.17 |
||||
|
Greer 1986 (CBA) |
Karnofsky Performance Status (KPS) score: from 0 to 100; higher scores equal better performance status; caregiver report |
Backwards from death | 3 weeks | Authors stated there were no differences but statistical significance was not stated "the three samples exhibited similar decreases in functional performance as measured by the Karnofsky Performance Status" (Greer 1986) |
Adjusted estimates Community‐based intervention: M 29.52 (SE 0.64) Hospital‐based intervention: M 31.05 (SE 0.79), Control (conventional care): M 28.84 (SE 1.06) |
| 1 week | Adjusted estimates Community‐based intervention: M 23.72 (SE 0.54) Hospital‐based intervention: M 25.39 (SE 0.57) Control (conventional care): M 23.83 (SE 0.84) |
ANCOVA: analysis of covariance; CHF: congestive heart failure; CI: confidence interval; COPD: chronic obstructive pulmonary disease; ES: estimated effect size; M: mean; n.s.: not significant; SAUC: standardised area under the curve; SD: standard deviation; SE: standard error.
aResults from F‐tests of non‐imputed data; authors stated that imputed data gave similar results bThe authors calculated mean changes from baseline at one to four months after enrolment by dividing the area under the curve scores by time; differences between groups were tested by bootstrap estimation to fit regression models allowing for clustering and predictive factors. cThe authors used repeated measures analysis and analysis of variance; analysis included 78 patients who completed the three follow‐up interviews (i.e. up to 18 weeks after enrolment); adjusted means were used due to baseline differences despite randomisation.
4. Quality of life: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Rabow 2004 US (high quality) |
Multidimensional Quality of Life Scale – Cancer Version scores: single item (from 0 to 10) and total scale score from 17 items (from 0 to 100); higher scores equal better quality of life; patient report |
Forwards from enrolment | 6 months | n.s.a P values ranged from 0.32 (ANCOVA group by time interaction for total scale score) to 0.72 (ANCOVA group main effect for total scale score) |
Adjusted estimatesa Single item Intervention (n = 50): M 7.6 Control (n = 40): M 7.0 Total scale score Intervention (n = 50): M 69.7 Control (n = 40): M 65.4 |
| 12 months | Adjusted estimatesa Single item Intervention (n = 50): M 7.5 Control (n = 40): M 7.1 Total scale score Intervention (n = 50): M 69.3 Control (n = 40): M 67.7 |
||||
|
Jordhøy 2000 Norway (high quality) |
EORTC‐QLQ‐C30 9 scales and 6 single items transformed scores: from 0 to 100; higher scores on functioning scales equal better functioning; higher scores on symptom scales equal more symptomatology; patient report |
Forwards from enrolment | 1 month | n.s.b P values ranged from 0.95 for the dyspnoea item to 0.10 for the social functioning scale and the financial impact item |
Mean ratings at each assessment point for each group and SAUCs for the various scores provided in Jordhoy 2001a (Jordhøy 2000) |
| 2 months | |||||
| 4 months | |||||
| 6 months | Differences and statistical significance not stated | ||||
|
Bakitas 2009 US (high quality) |
Functional Assessment of Chronic Illness Therapy for Palliative Care (FACIT‐Pal) score: from 0 to 184, higher scores equal better quality of life; patient report |
Forwards from enrolment | 1 month | Favours interventionc M treatment effect (intervention‐control) 4.6 (SE 2); P value = 0.02 |
Intervention (n = 108): LSM 137.25 (95% CI 133.91 to 140.59) Control (n = 97): LSM 135.34 (95% CI 131.83 to 138.86) |
| 4 months | Intervention (n = 69):LSM 137.50 (95% CI 133.50 to 141.49) Control (n = 74): LSM 133.40 (95% CI 129.43 to 137.36) |
||||
| 7 months | Intervention (n = 59): LSM 141.27 (95% CI 136.98 to 145.55) Control (n = 54): LSM 131.14 (95% CI 126.63 to 135.66) |
||||
| 10 months | Intervention (n = 48): LSM 136.33 (95% CI 131.66 to 141.00) Control (n = 44): LSM 128.78 (95% CI 123.85 to 133.70) |
||||
| 13 months | Intervention (n = 27):LSM 138.12 (95% CI 132.20 to 144.03) Control (n = 31): LSM 133.44 (95% CI 127.68 to 139.20) |
||||
| Backwards from death | Third last assessment | Favours interventionc M treatment effect (intervention‐control) 8.6 (SE 3.6); P value = 0.02 |
Intervention (n = 51): LSM 139.48 (95% CI 133.34 to 145.61) Control (n = 47): LSM 130.58 (95% CI 124.20 to 136.97) |
||
| Second last assessment | Intervention (n = 79):LSM 134.19 (95% CI 128.70 to 139.67) Control (n = 75): LSM 127.79 (95% CI 122.13 to 133.46) |
||||
| Last assessment | Intervention (n = 78): LSM 130.13 (95% CI 124.63 to 135.63) Control (n = 72): LSM 119.74 (95% CI 113.74 to 125.18) |
||||
|
McWhinney 1994 Canada |
Functional Living Index – Cancer score: range and interpretation not stated; patient/caregiver report |
Forwards from enrolment | 1 month | n.s. | "There were no clinically or statistically significant differences between the experimental and control groups on any of the measures at one month" (McWhinney 1994); no data provided to support this statement High attrition (53/146) mainly due to death; 2 month data not analysed due to further attrition |
|
Aiken 2006 US |
SF‐36 8 subscales transformed score from 0 to 100; higher scores equal better functioning; patient report |
Forwards from enrolment | 3 months |
Physical functioning favours intervention (slope: z 2.50, P value < 0.05; intercept at 9 months: z 2.16, P value < 0.05, g 0.41) General health favours intervention (slope: z 2.16, P value < 0.05; intercept at 9 months: z 2.51, P value < 0.05, g 0.47) Vitality favours intervention (intercept at 3 months for COPD only: z 2.36, P value < 0.05, g 0.76) Social functioning, role‐physical, bodily pain, role‐emotional, mental health subscales n.s. |
Growth modelling analysis (separate for COPD and CHF patients) Slopes of "average" linear trajectory within COPD and CHF groups ("averaged across slopes of individual linear trajectories of individual within the group") provided in Aiken 2006 Physical functioning: intervention patients in both diagnoses remained the same over time (CHF) or improved (COPD) over time, while control patients declined over time. At the 9‐month point, intervention patients' physical functioning exceeded that of controls General health: the "average" slope for intervention patients was higher than for controls and the intervention intercept exceeded that of controls at 9 months Vitality: there was an intercept difference for COPD at 3 months, with intervention patients having higher vitality scores than controls; no difference between conditions was observed for CHF |
| 6 months | |||||
| 9 months | |||||
|
Tramarin 1992 Italy |
Quality Well‐Being (QWB) Scale score: from 0 (death) to 1.0 (asymptomatic optimal functioning); higher scores equal better health; patient report |
Forwards from enrolment |
Weekly time points (authors plotted data from 6 to 12 months after enrolment) | Authors stated there were differences but statistical significance was not stated |
"Although QWB scores declined progressively in both groups, an increment in well‐being was detectable in the HC group shortly after the beginning of care" (Tramarin 1992); graph showed the increase in the intervention group occurred shortly before month 7 to month 8 (followed by a plateau at around a mean score of 0.54), while controls decreased from same initial level to mean score of around 0.44 at month 8) |
|
Greer 1986 (CBA) |
1) HRCA Quality of Life Index modified from Spitzer's Quality of Life Index Score: from 0 to 10; higher scores equal better quality of life; patient report 2) Uniscale A Unidimensional Q‐L score: from 0 to 14; higher scores equal better quality of life; patient report |
Backwards from death | 3 weeks | Authors stated there were no differences but statistical significance was not stated "Other measures, such as the HRCA Quality of Life Index (...) were comparable in the three systems of care"; "the three samples exhibited similar decreases in functional performance as measured by the (...) Uniscale" (Greer 1986) |
Adjusted estimatesd HRCA Community‐based intervention: M 3.90 (SE 0.13) Hospital‐based intervention: M 4.15 (SE 0.16) Control (conventional care): M 3.64 (SE 0.27) Uniscale Community‐based intervention: M 3.31 (SE 0.09) Hospital‐based intervention: M 3.51 (SE 0.12) Control (conventional care): M 3.60 (SE 0.19) |
| 1 week | Adjusted estimatesd HRCA Community‐based intervention: M 2.99 (SE 0.08) Hospital‐based intervention: M 3.04 (SE 0.10) Control (conventional care): M 3.24 (SE 0.16) Uniscale Community‐based intervention: M 2.92 (SE 0.07) Hospital‐based intervention: M 3.10 (SE 0.07) Control (conventional care): M 3.09 (SE 0.11) |
ANCOVA: analysis of covariance; CHF: congestive health failure; CI: confidence interval; COPD: chronic obstructive pulmonary disease; EORTC‐QLQ‐C30: European Organisation for Research and Treatment of Cancer Quality of Life questionnaire; LSM: estimated least mean square; M: mean; n.s.: not significant; SAUC: standardised area under the curve; SE: standard error. aANCOVAs tested for differences between groups and for group by time interaction, controlling for baseline differences in pain but not for clustering; means adjusted for baseline scores. bThe authors calculated mean changes from baseline at one to four months after enrolment by dividing the area under the curve scores by time; differences between groups were tested by bootstrap estimation to fit regression models allowing for clustering and predictive factors. cResults from repeated measures analysis of covariance (mixed‐effects model applied to longitudinal data using random‐subject effects to account for correlation between repeated outcome measurements on same individual). dEstimates adjusted for sample differences; standard errors based on the linear regression equation.
5. Caregiver burden: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Higginson 2009 UK (high quality) |
Zarit Burden Inventory (12 items) score: from 0 to 48, higher scores equal greater burden); caregiver report |
Forwards from enrolment | 6 weeks | n.s. |
M change from baseline Intervention (n = 24): 1.10 (95% CI ‐3.43 to 5.63) Control (n = 20): ‐1.13 (95% CI ‐3.41 to 1.14) |
| 12 weeks | Favours intervention F = 7.96 P value = 0.011 |
M change from baseline Intervention (n = 25): ‐2.88 (95% CI ‐5.99 to 0.24) Control (n = 23): 1.58 (95% CI ‐0.51 to 3.67) |
|||
|
Bakitas 2009 US (high quality) |
Montgomery Borgatta Caregiver Burden Scale (14 items, 3 subscales: objective burden, stress burden and demand burden) scores: range not stated; caregiver report |
Forwards from enrolment | 1 month | n.s.a P value > 0.05 |
"There were no significant main effects or interactions for Time, Condition, or Patient Gender for any of the measures of caregiver burden (all P values > 0.05)" (O'Hara 2010, Bakitas 2009); no data provided to support this statement |
| 4 months | |||||
| 7 months | |||||
| 10 months | |||||
| Greer 1986 (CBA) |
Study‐specific perceived caregiving burden measure score: from 0 to 6; higher scores equal greater burden; caregiver report |
Backwards from death | not clear: 'last weeks of life' |
Caregiver burden significantly higher in community‐based interventionb (not clear if against hospital‐based intervention, control or both) |
Adjusted estimatesb Community‐based intervention: M 3.32 (SE 0.07) Hospital‐based intervention: M 2.91 (SE 0.09) Control (conventional care): M 3.13 (SE 0.16) "Although one might expect the burden reported by HC PCPs to be much higher, given the greater level of instrumental care provided by HC PCPs in the last weeks of life, the differences observed were small, although statistically significant" (Greer 1986) |
CBA: controlled before and after study; CI: confidence interval; HC: home care (community‐based intervention); M: mean; n.s.: not significant; PCP; primary care person; SE: standard error. aThe authors used mixed effects modelling for repeated measures and adopted a factorial design of time, condition (intervention vs. control), and patient gender (male, female) with an unstructured covariance matrix. The contribution of each independent variable was tested as a main effect and in interaction with the other independent variables for each of the three caregiver burden subscales. bThe authors undertook hypothesis testing on adjusted estimates of outcomes in each of the groups derived through linear regression. Although statistical significance was stated in the text, no details of the test results were given; estimates adjusted for sample differences; standard errors based on the linear regression equation.
6. Caregiver grief: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details | |
|
Bakitas 2009 US (high quality) |
Measure not stated score: total score (sum G1‐G15 items; from 0 to 60; higher scores equal greater grief); binary score for complicated grief (present if at least 3 items from G1 to G4 and G5 to G15 whose values were no less than 4 (often or always) separately); caregiver report |
Forwards from death | Approximately 4 to 6 months |
Grief total score n.s. t‐test P value = 0.56 Complicated grief n.s. P value = 1.0 |
Grief total score Intervention (n = 50): M 22.24 (SD 11.22) Control (n = 36): M 20.72 (SD 12.39) Complicated grief Intervention: 8/50 (16%) Control: 6/36 (17%) |
|
|
Jordhøy 2000 Norway (high quality) |
13‐item scale developed from the 21‐item Texas Revised Inventory of Grief (new scale called ‘TRIG100') transformed scores: from 0 to 100; higher scores equal high grief reactions; caregiver report |
Forwards from death | 1 month | n.s.a group by time interaction F = 0.348 P value = 0.790 (power 0.131) |
n.s. t‐test ‐0.05 P value = 0.959 |
Intervention: M 70.86 (SD 2.76) Control: M 71.11 (SD 4.41) |
| 3 months | n.s. t‐test 0.14 P value = 0.888 |
Intervention: M 71.71 (SD 2.76) Control: M 71.06 (SD 3.89) |
||||
| 6 months | n.s. t‐test ‐0.08 P value = 0.935 |
Intervention: M 67.23 (SD 3.08) Control: M 67.64 (SD 3.98) |
||||
| 13 months | n.s. t‐test 0.44 P value = 0.659 |
Intervention: M 67.20 (SD 2.95) Control: M 64.97 (SD 4.28) |
||||
|
Grande 1999 UK |
Texas Revised Inventory of Grief (TRIG): Scale 1 ‐ grief at time of death (8 items) and Scale 2 ‐ grief at time of scale completion (13 items) scores: range not stated; higher scores equal worse outcome; caregiver report |
Forwards from death | 6 months | 2 TRIG scales n.s. |
TRIG Scale 1 (at time of death) Intervention (n = 74): M 19.1 (SD 6.9) Control (n = 16): M 20.1 (SD 8.7) TRIG Scale 2 (6 months after death) Intervention (n = 70): M 46.5 (SD 12.9) Control (n = 15): M 46.8 (SD 11.8) Comparisons of scores of people who received and did not receive the intervention (27 people in intervention group did not receive the service) showed no differences |
|
|
Greer 1986 (CBA) |
Modified Grief Experience Inventory score: from 0 to 10; higher scores equal greater grief; caregiver report |
Forwards from death | 90 to 120 days | Comparison between intervention and control not stated (authors only referred to significant differences between hospital‐based vs. community‐based intervention favouring the former) "HC PCPs reported significantly greater emotional distress, as measured by a modified Grief Experience Inventory, than did HB PCPs" (Greer 1986) |
Adjusted estimatesb Community‐based intervention: M 5.06 (SE 0.11) Hospital‐based intervention: M 4.49 (SE 0.13) Control (conventional care): M 4.82 (SE 0.19) |
|
HC: home care; M: mean; n.s.: non‐significant; PCP: primary care person; SD: standard deviation; SE: standard error. aLongitudinal analysis of 92 caregivers who turned the four questionnaires (months since death of patient was the within subject factor in MANOVA and group was the between subject factor). MANOVA analysis also showed that grief reactions changed significantly over time (F = 8.145; P value < 0.001; power 0.997) but the pattern of change did not differ significantly between intervention and control groups. bEstimates adjusted for sample differences; standard errors based on the linear regression equation.
7. Satisfaction with care: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Jordhøy 2000 Norway (high quality) |
FAMCARE (20 5‐point items) transformed score from 0 to 100; higher scores equal greater satisfaction; caregiver report Note: item scores are presented in inverse scale, i.e. lower scores equal greater satisfaction |
Backwards from death | 1 month after death | Favours intervention F = 7.11 P value = 0.008 Eta2 0.040 b 7.68 (SE 3.15) t 2.44 P value = 0.016 (adjusted for relationship to deceased, sex and age of caregiver, cancer, sex of patient, time since inclusion in the study, place of death) |
Intervention (n = 112): M 71.68 (SD 20.03) Control (n = 68): M 63.08 (SD 22.43) Difference (intervention minus control) of 8.60 points reduced to 7.7 controlling for others variables Item analyses using t‐test showed 10 items with P value < 0.05; 3 items P value ≥ 0.05 and < 0.10; 7 items P value ≥ 0.01 (details in Ringdal 2002, Jordhøy 2000) |
|
Rabow 2004 US (high quality) |
25 items (5‐point Likert scale) from the Group Health Association of America Consumer Satisfaction Survey score: from 20 to 100; higher scores equal greater satisfaction; patient report |
Forwards from enrolment | 6 months | ANCOVA group main effect: n.s. F = 1.31 P value = 0.26 ANCOVA group by time interaction: n.s. F = 0.61 P value = 0.44 |
Adjusted estimates Intervention (n = 50): M 69.6 Control (n = 40): M 74.5 |
| 12 months | Adjusted estimates Intervention (n = 50): M 70.1 Control (n = 40): M 72.4 |
||||
|
Bakitas 2009 US (high quality) |
Revised version of Teno's After Death Bereaved Family Member Interview overall rating item: range not stated; higher scores equal greater satisfaction; caregiver report |
Backwards from death | Approximately 4‐6 months after death |
Overall rating n.s. P value = 0.91 |
Overall rating Intervention (n = 50): M 41.08 (SD 12.26) Control (n = 36): M 40.78 (SD 11.61) Note: authors also measured a number of different dimensions of care satisfaction but found no statistically significant differences and only 1 marginally significant difference (P value = 0.06) in how the services responded to caregiver distress (rated better in the intervention group; M 4.5 score, SD 3.16 vs. M 3.28, SD 2.72 in the control group). Other dimensions of care examined included provision of family support, patient spiritual support, co‐ordination of care, shared decision‐making, information about symptoms and response to unmet needs and preferences, respect and individual‐focused care and quality of pre‐palliative cancer care |
|
Brumley 2007 US (high quality) |
Reid‐Gundlach Satisfaction with Services instrument (12 items) score: unknown to 48; higher scores equal greater satisfaction; dichotomised for analysis ≥ 37 very satisfied)a; patient report (or caregiver if the patient was unable to take part in telephone interview) |
Forwards from enrolment | 30 days | Favours intervention logistic regression OR 3.37 (95% CI 1.42 to 8.10); P value = 0.006 |
n = 216 Intervention: 93.1% very satisfied Control: 80.0% very satisfied |
| 60 days | n.s. logistic regression OR 1.79 (95% CI 0.65 to 4.96); P value = 0.26 |
n = 168 Intervention: 92.3% very satisfied Control: 87.0% very satisfied |
|||
| 90 days | Favours interventionb log regression OR 3.37 (95% CI 0.65 to 4.96); P value = 0.03 |
n = 149 Intervention: 93.4% very satisfied Control: 80.8% very satisfied |
|||
|
Hughes 1992 US |
Adapted US hospice study scale (17 items) score: from 1 to 3, higher scores equal greater satisfaction; patient report |
Forwards from enrolment | 1 month | Favours intervention Beta 0.13 t 2.15 P value = 0.04 |
ANCOVA (age, education, race, marital status, retirement due to health, prior private sector hospital use, living arrangement, and baseline care satisfaction scores – none of these factors were predictive of outcomes); descriptive data not provided |
| 6 months | Marginally significant difference favouring intervention t ‐1.98 P value = 0.06 |
Intervention (n = 17): M 2.72 Control (n = 14): M 2.45 Data were analysed using t‐tests because the sample did not support regression models |
|||
|
Adapted US hospice study scale (17 items) score: from 1 to 3, higher scores equal greater satisfaction; caregiver report |
1 month | Favours intervention Beta 0.18 t 3.46 P value = 0.0007 |
ANCOVA (caregiver age, race, education, relationship to patient, care satisfaction baseline score); descriptive data not provided | ||
| 6 months | n.s. Beta 0.12 t 1.59 P value = 0.12 |
ANCOVA (caregiver age, race, education, relationship to patient, care satisfaction baseline score); descriptive data not provided | |||
| Greer 1986 (CBA) |
Modified Medical Interview Satisfaction Scale score: from 1 to 5; higher scores equal greater satisfaction; patient report |
Forwards from enrolment | 3 weeks | n.s.c "No significant differences were observed in patient‐reported levels of satisfaction, which were uniformly high in all settings" (Greer 1986) |
Adjusted estimatesc Community‐based intervention: M 4.87 (SE 0.51) Hospital‐based intervention: M 3.76 (SE 0.98) Control (conventional care): M 4.20 (SE 0.71) |
| 1 week | Adjusted estimatesc Community‐based intervention: M 3.56 (SE 0.44) Hospital‐based intervention: M 4.60 (SE 0.72) Control (conventional care): M 5.20 (SE 0.75) |
||||
| 1) Modified Medical Interview Satisfaction Scale score: from 1 to 5; higher scores equal greater satisfaction; caregiver report pre and after death 2) Item on caregiver regret concerning the medical treatment the patient received (yes/no; caregiver report after death only) |
Pre death (time point not stated) |
Adjusted estimatesc Community‐based intervention: M 4.39 (SE 0.04), Hospital‐based intervention: M 4.54 (SE 0.05) Control (conventional care): M 4.38 (SE 0.09) |
|||
| Backwards from death | 90‐120 days after death |
Modified Medical Interview Satisfaction Scale favours hospital‐based interventionc "HB [hospital‐based] PCPs [primary care person], both before and after the patient's death, reported higher satisfaction with the patient's care than CC [conventional care] PCPs"; "small but significantly higher level of satisfaction reported by HB family members" (Greer 1986) Regret concerning patient medical treatment n.s. "Few PCPs (...) reported increased (...) regret concerning the medical treatment the patient received (11%), with no statistically significant differences among settings" (Greer 1986) |
Adjusted estimatesc Modified Medical Interview Satisfaction Scale Community‐based intervention: M 4.36 (SE 0.04) Hospital‐based intervention: M 4.48 (SE 0.05) Control (conventional care): M 4.33 (SE 0.08) Regret concerning patient medical treatment Descriptive data by group not provided |
ANCOVA: analysis of covariance; b: metric regression coefficient; CI: confidence interval; M: mean; n.s.: non‐significant; OR: odds ratio; SD: standard deviation; SE: standard error. aThere were no differences in the dichotomised variable at baseline but there were statistically significant differences in the continuous variable favouring the intervention over control (M 39.3 (SD 6.2) vs. 40.8 (SD 5.2); P value = 0.03). bLast point of analysis because reduction in sample size at 120 days (n = 136) resulted in the exclusion of this data in analyses. cThe authors undertook hypothesis testing on adjusted estimates of outcomes in each of the groups derived through linear regression. Although statistical significance was stated in the text, no details of the test results were given; estimates adjusted for sample differences; standard errors based on the linear regression equation for continuous variables and on logistic regression equation for dichotomous variables.
Summary of findings 2. Summary of findings.
| Economic data: home palliative care vs. usual care | |||
|
Patient or population: adult patients with a severe or advanced disease (malignant /or non‐malignant) Settings: Italy, UK, US Intervention: home palliative care Comparison: usual care, which could include community care (primary or specialist care at home and in nursing homes), hospital care (inpatient and outpatient) and in some instances palliative or hospice care (or both) | |||
| Economic data | No of participants (studies) |
Level of evidencea (adapted fromVan Tulder 2003) |
Comments |
|
ED visits Time horizon: 6 months following enrolment; from enrolment to death, transfer to hospice care or study end; last 2 weeks before death Table 10 |
1103 (6 RCTs; 3 high quality) |
Moderate | Moderate evidence of no statistically significant effect on ED visits: consistent across 4 RCTs. In addition, subanalysis of last 2 weeks of life for 33 patients that died in Zimmer 1985 found no ED visits in either group A significant reduction in ED use as a result of receiving home palliative care was found only in Brumley 2007 (high quality RCT conducted with patients with cancer, CHF and COPD in the US), where 20% of intervention patients had ED visits during the study period as opposed to 33% of those in usual care (P value = 0.01) |
|
Total care costs time horizon: 12 weeks or 6 months following enrolment; from enrolment to death, transfer to hospice care or study end; last 2 weeks before death Table 11 |
2047 (6 studies; all high quality economic evaluations; 5 RCTs and 1 CBA) |
Inconclusive | All studies reported lower costs in the intervention group with differences ranging from 18% to 35% (in Greer 1986 costs under the hospital‐based intervention were 2% lower than usual care as opposed to 32% lower under community‐based intervention). However, differences were statistically significant only in Brumley 2007 (the study with the largest sample size and only slightly underpowered by 3 patients as planned by authors to detect cost differences) Statistical significance not reported in 3 RCTs |
|
Cost‐effectiveness time horizon: 6 months following enrolment; from enrolment to death, transfer to hospice care or study end; last 2 weeks before death Table 11 |
2047 patients and 1678 caregivers (6 studies; all high‐quality economic evaluations; 5 RCTs and 1 CBA) |
inconclusive | Home palliative care were cost‐effective compared to usual care in Brumley 2007 (297 people with cancer, CHF and COPD) and Higginson 2009 (50 people with MS and their caregivers). However, cost‐effectiveness is unclear in the other 4 studies, as there were positive, null and negative clinical effectiveness results while costs did not differ (Hughes 1992) and the statistical significance of differences in outcomes or costs, or both, was not reported (2 trials and Greer 1986) Only Tramarin 1992 calculated a summary cost‐effectiveness measure ("average" cost‐effectiveness ratio reported in 1990 USD was USD482 per well‐week in intervention group and USD791 in control group) but with unknown statistical significance of difference or uncertainty around the estimates. In addition, Higginson 2009 plotted cost‐effectiveness planes for 2 of their outcomes. The plane for overall palliative care outcomes showed 33.8% replications in the quadrant indicating better outcomes and lower costs in the intervention group, and 54.9% in the quadrant indicating worse outcomes but lower costs. In contrast, the plane on caregiver burden showed 47.3% replications in the quadrant indicating lower costs and better outcomes and 48.0% in the quadrant showing higher costs and better outcomes |
CBA: controlled before and after study; CCT: controlled clinical trial; CHF: congestive heart failure; COPD: chronic obstructive pulmonary disease; ED: emergency department; MS: multiple sclerosis; RCT: randomised controlled trial
aLevels of evidence: Strong: findings from meta‐analysis or consistent findings across all studies including at least two high quality RCTs Moderate: consistent findings across all studies including at least two low quality RCTs/CCTs or one high quality RCT Limited: one RCT/CCT not reaching high quality Conflicting: inconsistent findings among at least two studies with at least one RCT/CCT Inconclusive: statistical significance of differences unknown in > 25% of all studies No evidence from trials: No RCTs or CCTs Consistent (conflates assessment of direction and precision): statistically significant effect in same direction in ≥ 75% of all studies High quality RCTs/CCTs: ≥ 3.5 methodological quality score (ranging from zero to six)
8. Emergency department use.
| Study | Analysis | Time horizon | Significance and direction | Details |
|
Bakitas 2009 US (high quality) |
Forwards from enrolment |
During study period | n.s. Wilcoxon rank sum test P value = 0.53 |
Intervention: 0.86 visits Control: 0.63 visits Note: not clear if the figures are means or medians |
|
Brumley 2007 US (high quality) |
Forwards from enrolment |
During study period |
Reduced ED use in intervention group Cramer's V 0.15; P value = 0.01 linear regression adjusted for survival, age and severity of illness showed intervention reduced ED visits by 0.35 (P value = 0.02) |
Intervention: 20% had ED visits Control: 33% had ED visits |
|
Rabow 2004 US (high quality) |
Forwards from enrolment | During study period | n.s. t ‐0.24 P value = 0.81 |
Intervention (n = 50): M 1.6 visits (SD 2.2) Control (n = 40): M 1.7 visits (SD 2.8) |
|
Aiken 2006 US |
Forwards from enrolment |
During study period | n.s. overdispersed Poisson regression model predicted number of ED visits during enrolment from group, diagnosis and their interaction, controlling for total number of days in study and number of pre‐enrolment ED visits; authors stated there was no significant intervention effect. Neither was there an effect on ED visits for a subgroup of participants identified as being at high risk for ED utilisation |
Intervention: M visits/month 0.11 (SD 0.34) Control: M visits/month 0.10 (SD 0.31) Note: authors stated the number of ED visits per month remained "essentially unchanged" from 6 months prior to enrolment to period from then until the end of study |
|
Hughes 1992 US |
Forwards from enrolment |
6 months following enrolment |
VA ED visits "n.s." t 1.14 Non‐VA ED visits "n.s" t < 1 |
VA ED Intervention (n = 86): M 0.57 visits (SD 0.8) control (n = 85): M 0.72 visits (SD 0.9) non‐VA ED Intervention (n = 86): M 0.10 visits (SD 0.3) control (n = 85): M 0.08 visits (SD 0.3) |
|
Zimmer 1985 US |
Backwards from death | Last 2 weeks before death | No differences (there were no ED visits in either group) | Intervention (n = 21): 0 visits Control (n = 12): 0 visits |
ED: emergency department; M: mean; n.s.: non‐significant; SD: standard deviation; VA: Veteran Affairs.
9. Cost‐effectiveness analyses with total care costs.
| Study and sample analysed | Clinical effectiveness | Impact on resource use | Impact on total care costs | Cost‐effectiveness |
|
Brumley 2007 US N intervention = 145 N control = 152 high quality economic evaluation (mean score 0.7) |
+ death at homea + death in hospitala + patient satisfaction with care at 30 days + patient satisfaction with care at 90 days Ø patient satisfaction with care at 60 days Ø death in nursing homea Ø death in inpatient hospicea Ø survivalb |
↓ ED visits ↓ hospital admission ↓ hospital inpatient days Ø referral to hospice care |
↓ total adjusted mean costs per patientc USD7552 lower in intervention group (33% lower; 95% CI ‐ USD12,411 to ‐ USD780; P value = 0.03; R2 0.16) unadjusted difference: t 3.63; P value < 0.001 time horizon: from enrolment to death, transfer to hospice care or study end (mean survival of 196 days in intervention group and 242 days in control group; 73% patients died) currency: 2002 USD Adjusted mean costs per patientc Intervention USD2670 ± 12,523 Control USD20,222 ± 30,026 Adjusted mean costs per patient per dayc Intervention USD95.30 Control USD212.80 t ‐ 2.417; P value = 0.02 Total costs included those associated with physician visits, ED visits, hospital days, skilled nursing facility days, and home health or palliative days |
+ no summary measure, but the intervention was cost‐effective as it resulted in statistically significant improved outcomes (no negative findings), reduced resource use (no negative findings) and a statistically significant reduction in total costs |
|
Higginson 2009 UK N intervention = 26 N control = 24 high quality economic evaluation (mean score 0.8) |
+ symptom burden at 12 weeks + pain at 12 weeks + caregiver burden at 12 weeks Ø palliative care outcomes (primary outcome; at 6 and 12 weeks) Ø symptom burden 6 weeks Ø pain at 6 weeks Ø MS psychological impact at 6 and 12 weeks Ø MS physical impact at 6 and 12 weeks Ø caregiver burden 6 weeks Ø caregiver mastery (learning new skills) at 6 and 12 weeks Ø caregiver positivity at 6 and 12 weeks |
? authors reported the use of a range of health, social and voluntary services but the statistical significance of differences was not stated | Ø total mean costs per patient GBP1789 lower in intervention group (29% lower; bootstrapped 95% CI ‐ GBP5224 to GBP1902; n.s.); excluding inpatient care and informal care, mean service costs were GBP1195 lower in the intervention group (50% lower; bootstrapped 95% CI ‐ GBP2916 to GBP178; n.s.)d time horizon: 12 weeks from enrolment (only 4 deaths) currency: 2005 GBP Mean costs per patient Intervention GBP4294 Control GBP6084 Total costs included those associated with a range of health, social, and voluntary services (inpatient care, respite care, day centre, contacts with district/practice nurse, MS nurse, palliative care nurse, other nurse, general practice, specialist at home, in hospital, in a ward and in other places, occupational therapist, physiotherapist, dietician, chiropodist, dentist, speech therapist, social services) and informal care |
+ the intervention was cost‐effective as it improved caregiver burden (ZBI) with no statistically significant differences in palliative care outcomes (POS‐8) and total costs The authors plotted cost‐effectiveness planes for the two above‐mentioned outcomes (ZBI and POS‐8). These planes plot costs against outcomes forming four‐quadrants to visualise if the intervention has better outcomes and higher costs, better outcomes at lower costs, worse outcomes at higher costs or worse outcomes but at lower costs. The authors accounted for uncertainty around the cost‐effectiveness estimates by generating 1000 resamples using bootstrapping and computing cost and outcome differences for each, which were then plotted on the cost‐effectiveness planes. The point estimates in cost‐effectiveness planes suggest that the intervention was cost saving, with equivalent outcomes on overall palliative outcomes and improved outcomes for caregiver burden. The POS‐8 plane showed 33.8% replications in the lower right quadrant, indicating that intervention patients had better outcomes and lower costs than controls, and 54.9% in the quadrant indicating worse outcomes but lower costs. By contrast, in the ZBI plane, 47.3% replications were in the quadrant showing lower costs and better outcomes and 48.0% in the quadrant showing higher costs and better outcomes The authors also conducted a sensitivity analysis testing different imputation methods for dealing with missing data (last value carried, forward, next value carried backwards, and mean value), reporting similar results in nonimputed and imputed data, for all imputation methods |
|
Zimmer 1985 US N intervention = 21 N control = 12 high quality economic evaluation (mean score 0.7) |
Ø death at homea Ø survival |
? authors reported the use of a range of out‐of‐home and in‐home services but the statistical significance of differences was not stated |
? total mean costs USD716 lower in intervention group (31% lower; statistical significance and/or uncertainty not reported) time horizon: last 2 weeks before death (subanalysis of deaths within the study) currency: USD, date not stated (study conducted in 1979‐1982) Mean costs of last 2 weeks before death per patient Intervention USD1577 Control USD2293 Total costs included out‐of‐home costs (hospital days, clinic visits, nursing home days, MD office or ED visits, ambulance or chairmobile rides) and in‐home costs (MD visits, nurse visits, RN/LPN hours, aide/homemaker visits, social worker visits, laboratory technician visits, meals‐on‐wheels visits) |
? no summary measure, and it is unclear if the intervention was cost‐effective as there were no statistically significant differences in outcomes, and although total costs were lower in the intervention group, the statistical significance of this difference was not reported |
|
Hughes 1992 US N intervention = 85 N control = 86 high quality economic evaluation (mean score 0.7) |
+ patient satisfaction with care at 1 month + caregiver satisfaction with care at 1 month ‐ caregiver morale at 6 months Ø patient satisfaction with care at 6 monthse Ø caregiver satisfaction with care at 6 months Ø caregiver morale at 1 month Ø morale Ø cognitive functioning Ø physical function Ø survival |
↓ hospital inpatient daysf ↓ VA outpatient clinic visits ↓ non‐VA community nursing visits Ø ED visits (VA and non‐VA) Ø ICU days Ø nursing home days Ø hospital admission Ø non‐VA community nursing visits Ø non‐VA private home care visits Ø extended care days ? length of last hospital admission before death |
Ø total mean costs per patient USD769 lower in intervention group (18% lower; t 1.05; "n.s.") time horizon: 6 months from enrolment (mean survival was 76.2 days in intervention group and 67.1 days in control group; 79% and 78% patients died within the study, respectively) currency: 1985 USD Mean costs of 6 months following enrolment per patient Intervention USD3479.36 Control USD4248.68 Total costs included those associated with institutional care (VA and private hospitals, nursing homes) and non‐institutional (outpatient clinic visits, intervention team's visits, community nursing) |
? no summary measure, and it is unclear if the intervention was cost‐effective as there were positive and negative results in clinical outcomes and the difference in total costs was not statistically significant |
|
Tramarin 1992 Italy N intervention = 9 N control = 30 high quality economic evaluation (mean score 0.8) |
? quality of life |
? authors reported on hospital admission, length of hospital admission, hospital inpatient days and outpatient clinic visits but the statistical significance of differences was not stated | ? total '"average" costs per person‐year USD7595 lower (35% lower; statistical significance or uncertainty, or both, not reported) time horizon: costs per person‐year (6 months from enrolment multiplied by 2; 22 deaths within the study) currency: 1990 USD (converted from 1990 ITL using healthcare‐specific purchasing power parities) "Average" total costs per person‐year Intervention stage 2/3 patients USD 14, 259 stage 2 patients only USD 11,321 stage 3 patients only USD 17,237 Control stage 2/3 patients USD 21,854 stage 2 patients only USD 15,944 stage 3 patients only USD 27,764 Total costs included more than 500 items including inpatient, outpatient clinics and home care (including intervention service), hotel and general services, diagnostic examinations and therapy, treatment items, medication and personnel salaries |
? cost‐utility ratios calculated only for stage 3 patients ("average" cost‐effectiveness ratio of USD482 per well‐week in intervention group and USD791 in control group; statistical significance or uncertainty, or both, around estimates not reported) and more appropriate incremental ratios could not be calculated from the data; hence it is unclear if the intervention was cost‐effective |
|
Greer 1986 (CBA) N intervention = 1457 (833 in community‐based intervention, 624 in hospital‐based intervention) N control = 297 (conventional care) high quality economic evaluation (mean score 0.7) |
+ patient at home as long as wanted (favours community‐based intervention vs. other groups) + symptom severity at 3 weeks to death (favours hospital‐based intervention vs. other groups) + symptom severity at 1 week to death + persistent pain at 3 and 1 week to death (favours hospital‐based intervention vs. other groups) + hours of social visiting at 3 weeks to death + caregiver satisfaction with care 90 to 120 after death (favours hospital‐based intervention vs. control) + quality of death referring to 3 days before death ‐ social quality of life at 1 week to death ‐ caregiver burden in last weeks before death (higher in community‐based intervention vs. other groups) Ø patient report of pain at 1 and 5 weeks Ø survival Ø physical function at 3 and 1 week to death Ø social quality of life at 3 weeks to death Ø hours of social visiting at 1 week to death Ø hours of chatting with household members at 3 weeks to death Ø caregiver pre‐bereavement psychological well‐being (distress, use of medication for anxiety and depression, increased drinking) Ø patient satisfaction with care at 3 and 1 week to death Ø caregiver regret at 90 to 120 days after death concerning the medical care the patient received ? death at home ? caregiver satisfaction with place of death ? caregiver report of patient pain at 3 and 1 week to death (composite pain and pain‐free) ? quality of life at 3 and 1 week to death ? emotional quality of life at 3 and 1 week to death ? hours of chatting with household members at 3 weeks to death ? spiritual well‐being in the 3 days before death ? patient awareness at 3 and 1 week to death ? grief at 90 to 120 days after death ? caregiver post bereavement psychological well‐being in first 90 to 120 days after death (use of medication for anxiety and depression, increased drinking) |
↑ receipt of social services ↑ general counselling in study period ↑ paperwork assistance ↑ analgesics prescribed and taken at 1 week to death (increased in hospital‐based intervention vs. other groups) ↑ oral route of analgesics ↓ analgesic consumption on a pro order ↓ aggressive interventions (radiotherapy, surgery, chemo or hormonal therapy) ↓ diagnostic tests (blood tests, x‐rays, scans) ↓ respiratory support interventions (oxygen, respiratory therapy) ↓ radiotherapy for patients with primary brain cancer or brain metastases 0 general counselling in last 2 weeks before death Ø legal/financial counselling Ø help getting services Ø self care training Ø caregiver post‐bereavement absenteeism from work in first 90‐120 days after death Ø analgesics prescribed and taken at 3 weeks to death Ø level of analgesics used Ø mean daily OME consumption Ø thoracentesis Ø palliative radiation therapy for patients with bone metastases with bone pain ? institutional days ? physician and outpatient visits ? home nursing visits ? home health/home worker visits ? hours of direct informal care caregiver post‐bereavement healthcare use (physician visits, hospitalisation in first 90 to 120 days after death) |
? total costs per study day USD48 lower in community‐based intervention (32% lower) and USD3 lower in hospital‐based intervention (2% lower) compared to the control group (conventional care); statistical significance not reported) time horizon: from enrolment to death or study end (length of survival not stated; all patients died within the study) currency: 1982 USD Total costs per study day Community‐based intervention USD101 (SE 9.1)g Hospital‐based intervention USD146 (SE 10.0)g Control (conventional care) USD149 (SE 11.7)g Note: not clear if the figures are means or medians Authors stated that total costs per study day were "substantially lower" in the community‐based intervention group than in the hospital‐based or control groups and that total costs were "comparable" for the first 2. Statistical significance was not stated Total costs included those associated with inpatient and home care, physician visits, outpatient clinic visits, drugs, supplies and equipment expenditures. Total costs combine "costs" and "charges" since only charges were available for physician services, drugs, supplies, and equipment purchased at home |
? no summary measure, and it is unclear if the intervention was cost‐effective as there were positive and negative results in outcomes but also others where statistical significance was not reported; in addition, it is unclear if differences in costs were statistically significant between intervention groups and the control (conventional care) |
+: statistically significant positive effect (favouring intervention); ‐: statistically significant negative effect (favouring control); Ø: effect not statistically significant; ?: statistical significance of effect not stated; ↑: statistically significant increase in intervention group; ↓: statistically significant decreased in intervention group; CI: confidence interval; ED: emergency department; GBP: British pound; ICU: intensive care unit; ITL: Italian lira; LPN: licensed practical nurse; M: mean; MS: multiple sclerosis; MD: medical doctor; n.s.: non‐significant; OME: oral morphine equivalent; RN: registered nurse; SE: standard error; USD: United States dollar; VA: Veterans Affairs; ZBI: Zarit Burden Interview. aResults as examined in meta‐analysis. bNo statistically significant difference in survival (log rank test P value = 0.08). cAdjusted in linear regression for differences in age, survival, severity of illness and diagnosis; the authors stated they used ordinary least squares regression in the final analysis to account for the right‐skewness in the cost data dThe authors used bootstrapping to produce 95% CIs around the cost differences between the groups eMarginally significant difference in t‐test favouring intervention group (i.e. greater satisfaction with care in intervention group; P value = 0.06). fStatistically significant differences for total VA hospital days and VA general hospital beds; not significant for inpatient days in VA hospital rehabilitation or intermediate beds or non‐VA private hospitals gStandard errors of estimates were based upon multiple regression equation.
Background
Extensive evidence shows that well over 50% of people prefer to be cared for and to die at home (Gomes 2013; Bell 2009; Higginson 2000). Most patients and caregivers facing advanced illness also prefer this. However, their choices depend on the problems experienced and the quality of the care received (Choi 2005; Thomas 2004). At present, in many countries of the world, most people have their wishes for home death unfulfilled. Despite efforts and policies to enable more to die at home only a minority of deaths take place at home, for example 17% in Norway in 2008, 21% in England in 2010, 23% in Belgium in 2007, 30% in Canada in 2004, 33% in Portugal in 2005, 34% in Italy in 2002 and 34% in the Netherlands in 2003 (Cohen 2010; Gomes 2012a; Houttekier 2011; WHO 2011; Wilson 2009).
The importance of providing optimal palliative care that supports patients with advanced illness and caregivers who wish to stay at home is particularly topical in ageing populations (Khaw 1999; WHO 2011). With the number of deaths predicted to rise dramatically in the future due to longer life expectancy and large cohorts of 'baby‐boom' generations reaching older age, high numbers of hospital deaths are difficult to sustain and an expansion of palliative care provision will need to happen in all settings – in hospitals, hospices, nursing and residential homes, and importantly at home (Gomes 2008; Gomes 2011). Already in a few countries such as the UK, Canada and the US, there has been a reversal of secular trends towards institutionalised dying and increasingly more people die at home (Gomes 2012a; Gao 2013; Wilson 2009;Teno 2013; Flory 2004).
In order to care well for more people at home and thus meet the preferences of more patients and caregivers, the effect of home palliative care services on death at home needs to be quantified. This will help estimate the extent to which current services need expansion or improvement, or both, according to need and preference. Furthermore, it is crucial to ascertain the effect of these services on outcomes other than death at home, such as symptom control, quality of life, caregiver distress and satisfaction with care. These outcomes are often as important or more important to patients than to die at home (Heyland 2006Steinhauser 2000). Finally, from a service planning perspective, home palliative care may save costs elsewhere in a healthcare system, in particular hospital costs, but whether or not these services are a cost‐effective addition or alternative to usual care is still a question.
Why it is important to do this review
Existing reviews of the effectiveness of home palliative care services (including home care teams attached to inpatient hospices, community hospice care agencies, hospital‐based community support teams and hospital at home services) have often been part of wider reviews of the effectiveness of palliative care models or have referred to populations of patients with cancer only (Smeenk 1998b). However, palliative care has expanded beyond cancer (Addington‐Hall 2001a). Two systematic reviews have looked at palliative care services regardless of patient diagnosis and included economic studies (Higginson 2003Zimmermann 2008); only one full economic evaluation, conducted as part of a pilot study in Italy in the 1990s, was found (Tramarin 1992). Furthermore, findings on outcomes varied, with the exception of an increased probability of death at home resulting from one model of home palliative care – hospital at home – as found in a Cochrane review (Shepperd 2011). A wider examination of home palliative care models and a critical appraisal of the variation in findings will help improve the evidence‐base for the development, implementation and evaluation of home palliative care services in the future.
Objectives
The objectives of this review were:
to quantify the effect of home palliative care services for adults with advanced illness and their family caregivers on patients' odds of dying at home;
to examine the clinical effectiveness of home palliative care services on other outcomes for patients and their caregivers such as symptom control, quality of life, caregiver distress and satisfaction with care;
to compare the resource use and costs associated with these services;
to critically appraise and summarise the current evidence on cost‐effectiveness.
Additional objectives were to examine sources of heterogeneity in the findings and to ascertain the appropriateness for meta‐analysis.
Methods
Criteria for considering studies for this review
Types of studies
Patient or cluster randomised controlled trials (RCTs)
Patient or cluster controlled clinical trials (CCTs)
Controlled before and after studies (CBAs)
Interrupted time series analyses (ITSs)
We defined 'randomised' as studies that were described by the authors as 'randomised' anywhere in the manuscript except in cases where the term was misused (e.g. referring to a random sample). We included CBAs that had at least two intervention sites and two control sites. We included ITSs with a defined point in time when the intervention started and at least three data points before and three after the intervention.
The economic component of the review was restricted to economic analyses conducted alongside the studies meeting eligibility criteria for the effectiveness component of the review. The following types of economic analyses were included:
full economic evaluations;
partial economic evaluations;
analyses reporting more limited resource use/cost information.
Types of participants
Participants aged 18 years or older in receipt of a home palliative care service (as described below), their family caregivers, or both. For a study to be included, the majority of patients had to have a severe or advanced disease (malignant or non‐malignant), no longer responding to curative/maintenance treatment or symptomatic, or both (e.g. lung/brain tumours or metastatic cancers, chronic obstructive pulmonary disease (COPD)).
Types of interventions
A team delivering home palliative care with the presence of the following four elements.
1. Primarily for patients with a severe or advanced disease (malignant or non‐malignant), no longer responding to curative/maintenance treatment or symptomatic (or both), or their family caregivers, or both
Interventions that did not directly deliver care to patients or caregivers were excluded. This included staff education/training programmes, teams operating only in a staff advisory capacity or co‐ordinating services, interventions conducting assessment only thus no direct management (e.g. screening tool), new policies (e.g. introduction of benefit scheme) and national policies/strategies were excluded. These do not necessarily and directly translate into care to patients or caregivers.
2. Aiming to support patients or family caregivers, or both, outside hospital and other institutional settings as far as possible and to enable patients to stay at home
While conducting the review we have also included interventions in which it was clear the majority of service contacts were established while the patients were at home. Services delivered in skilled nursing facilities, day care centres, residential homes or prisons were excluded.
3. Providing either specialist or intermediate palliative/hospice care, as defined in a previous systematic review
i) specialist palliative/hospice care was defined as health and social care provided by:
a) one or more doctors who have undergone higher specialist training in palliative medicine, and
b) one or more nurses who have undergone higher specialist training, and
c) one or more professionals attached to the team from a profession allied to medicine who have had further training in palliative care.
We accepted the presence of higher specialist training in palliative/hospice care if the authors described the professionals as palliative care specialists or experts (e.g. 'palliative care physician'). Training in 'care of the dying' (or described using equivalent terms) or comprising different physical and psychosocial components of palliative care were accepted. We also considered an intervention specialist palliative/hospice care if stated as such by the authors.
ii) intermediate palliative/hospice care was defined as health and social care provided by:
a) professionals from differing clinical disciplines working full‐time or most of the time in palliative/hospice care, who have not undergone any higher specialist training but developed much clinical experience over the years and had in‐service training for their job, or
b) a uni‐disciplinary team of professionals (e.g. nurses) working full‐time or most of the time in palliative care, in which one or more members may have had some further training.
We accepted that a team of professionals with years of existence or largely caring for patients with advanced illness is likely to work most of the time in the field and have some form of in‐house training, thus this was considered as intermediate palliative/hospice care. We also considered an intervention intermediate palliative/hospice care if the authors described it as 'palliative care' or ‘'hospice care' but when it was unclear whether the criteria for specialist (point 'i' above) were met.
4. Providing comprehensive care and aiming at different physical and psychosocial components of palliative care
Evaluations of interventions delivering only one component of palliative care (e.g. pain medication, home parenteral nutrition, home oxygen, home yoga, psychotherapy, social work, bereavement support, respite care, physical exercise, assistance with living wills) were excluded as they do not encompass the holistic nature of palliative care. Studies that compared forms of home palliative care differing in only one component of care (e.g. medication regimen) were also excluded. Excluding these, we accepted the delivery of comprehensive care if the authors stated the team offered 'palliative care' or 'hospice care', or if it was clear its professionals had training or experience in providing different physical and psychosocial components of palliative care.
Types of outcome measures
Primary outcomes
Death at home.
Secondary outcomes
According to our protocol (Gomes 2009), these included:
time the patient spent at home,
satisfaction with care,
pain,
other symptoms,
physical function,
quality of life,
caregiver pre‐ and post‐bereavement outcomes.
Economic data
These included:
hospital costs,
other institutional care costs,
community care costs,
informal care costs,
equipment and medication prescribed.
Measures of cost‐effectiveness included incremental cost‐effectiveness ratios (ICERs) using condition specific outcome measures and ICERs using quality‐adjusted life years (QALYs) as outcome measures.
Search methods for identification of studies
Electronic searches
We identified studies from a search of 12 databases:
Cochrane Central Register of Controlled Trials (CENTRAL) (21 November 2012);
EMBASE (1980 to 21 November 2012);
MEDLINE (1950 to 21 November 2012);
Cochrane Pain, Palliative and Supportive Care (PaPaS) Trials Register (11 May 2010);
Cochrane Effective Practice and Organisation of Care (EPOC) Trials Register (11 May 2010);
CINAHL (1981 to 13 April 2010);
EURONHEED (1980 to 13 April 2010);
PsycINFO (1806 to 13 April 2010);
Cochrane Database of Systematic Reviews (CDSR) (7 April 2010);
Database of Abstracts of Reviews of Effectiveness (DARE) (7 April 2010);
Health Technology Assessment (HTA) Database (7 April 2010);
NHS Economic Evaluation Database (NHS EED) (7 April 2010).
Search strategies were refined with input from the Trials Search Co‐ordinator of our Review Group (Cochrane PaPaS Review Group). Please see Appendix 1 for the MEDLINE search strategy in OVID and Appendix 2, Appendix 3, Appendix 4, Appendix 5, Appendix 6, Appendix 7 and Appendix 8 for all other search strategies. Results from searches in Cochrane databases, DARE, HTA and NHS EED were provided by the Trials Search Co‐ordinator. The remaining searches and last update in November 2012 were conducted by BG/NC.
Searching other resources
Handsearching
We handsearched the reference lists of the following four textbooks: Textbook of Palliative Medicine (Bruera 2006); Palliative Medicine (Walsh 2009); Oxford Textbook of Palliative Medicine (Hanks 2009) and Oxford Textbook of Palliative Nursing (Ferrell 2010). We also checked conference proceedings of the biennial Research Congress of the European Association for Palliative Care (EAPC 2008 and EAPC 2010).
Reference lists
We checked the reference lists of 49 relevant reviews (references in Appendix 9) and all included studies.
Correspondence
We contacted 17 authors of the main studies and investigators who were known to be carrying out research in this area for further studies and unpublished data: Amy Abernethy, Charles Normand, Sydney Dy, Ilora Finlay, Richard Harding, Chris Salisbury, Lidia Garcia Perez, Susan L Hughes, Bruce E Robinson, Donna Wilson, Tim Whelan, Frank Smeenk, Franco Toscani, Stein Kaasa, Camilla Zimmerman, Sasha Shepperd and Taryn Young.
Language
There was no language restriction in the selection of studies.
Data collection and analysis
Selection of studies
One review author (BG) screened the titles and abstracts for relevance, to judge eligibility and to remove duplicates. Full text of all potentially relevant studies was assessed by BG and NC. Disagreements were resolved by consensus and with a third review author (IJH) when needed.
Data extraction and management
Data from each selected study were entered on a data extraction form; the content is described in the protocol (Gomes 2009). Two reviewers extracted data independently for each study (two of BG/NC/BA/KS). Disagreements were resolved by consensus and with a third review author when needed. We contacted authors of studies to provide unpublished data for meta‐analysis where required.
Assessment of methodological quality of included studies
Two independent reviewers (two of BG/NC/BA/KS) assessed all included studies for methodological quality. We used the standard criteria developed by the Cochrane EPOC Review Group for RCTs/CCTs, CBAs and ITSs (see methods used in reviews under editorial information in Group Details). The checklist for RCTs/CCTs contains seven items qualified as done, unclear and not done for concealment of allocation, follow‐up of professionals, follow‐up of patients or episodes of care, blinded assessment of primary outcome(s), baseline assessment, reliable primary outcome measure(s) and protection against contamination. We assessed blinding and reliability of all outcomes (rather than just the primary). Also, one of the criteria (follow‐up of professionals) was not relevant to the studies in review; the remaining six were used. Each criterion was scored zero (not done), 0.5 (not clear or when scores varied across outcomes) and one (done). Total scores for RCTs/CCTs ranged from zero to six; studies with a score of 3.5 or above were considered of high quality.
Two independent review authors (BG/PMcC) assessed the methodological quality of all economic evaluations comparing total costs alongside outcomes (i.e. those enabling an appraisal of cost‐effectiveness). We used the BMJ's 35‐item checklist for authors and peer reviewers of economic submissions (Drummond 1996). An existing scoring system was applied to the checklist to distinguish high quality economic evaluations. We calculated a mean score with all items weighted equally (Gonzalez‐Perez 2002). Each item was scored zero (no), 0.5 (not clear or when scores varied across resource care/cost items) and one (yes); evaluations with a mean score of 0.6 or above were considered of high quality (Gonzalez‐Perez 2002). Not applicable items were omitted from the calculation of the mean.
We integrated the results of the quality assessment in data analysis and conducted meta‐analyses with sensitivity analyses including only high quality studies.
Measures of treatment effect
We combined studies using Review Manager (Version 5.1) (RevMan 2011). When sample size and proportions were missing we did not impute or estimate them for meta‐analysis because none of the suggested imputations in the Cochrane Handbook for Systematic Review of Interventions were considered reliable (following procedures in previous Cochrane reviews under advice from the statistician of our Cochrane Review Group) (Higgins 2011). We therefore contacted the authors to request additional data.
We combined data from trials for the primary outcome (death at home vs. elsewhere, dichotomous outcome) using a random‐effects model to account for the heterogeneity in populations and interventions (DerSimonian 1986). We used the Mantel‐Haenszel (M‐H) method; this estimates the amount of between‐study variation by comparing each study's result with a M‐H fixed‐effect meta‐analysis result (Higgins 2011). The pooled effect is expressed as an odds ratio (OR) for home palliative care compared with usual care; values greater than 1 indicate increased odds of death at home with home palliative care, and less than 1 for decreased odds. A P value of 0.05 was used as the cut‐off value to determine statistical significance and data are presented as the estimated effect with 95% confidence intervals (CIs). We conducted similar meta‐analyses for death in hospital, in nursing homes and in inpatient hospices/palliative care units. One study was a cluster RCT where three pairs of clusters (health regions) were randomised to the intervention or control. We adjusted the data for meta‐analysis using the 0.02 estimate of intracorrelation coefficient for this study used in Shepperd's Cochrane review (Shepperd 2011). This reduced the sample size in meta‐analysis both for number of events (e.g. death at home) and total in each of the groups.
We calculated the number needed to treat to benefit (NNTB) for the primary outcome, that is the expected number of people who would need to receive home palliative care rather than usual care for one additional person to die at home. NNTBs were calculated for the study population control risk and for three other assumed control risks (ACR). These were based on cancer home deaths rates from a population‐based study across six European countries (Cohen 2010):
low home death population assumed the lowest rate of 128 deaths at home per 1000 cancer deaths (Norway);
medium home death population assumed the mean across the six European countries (278 deaths at home per 1000 cancer deaths);
high home death population assumed the highest rate of 454 deaths at home per 1000 cancer deaths (the Netherlands).
We applied rates related to cancer as the included studies involved largely people with cancer.
Combining data on other outcomes, resource use and costs was not possible due to differences in the measurement and reporting (e.g. tools used, follow‐up and assessment time points or time horizon, type of analysis and statistics reported). We present the data in narrative summary tables. We summarised the results related to cost‐effectiveness based on studies examining the total costs of care. The evidence was graded (strong, moderate, limited, conflicting, inconclusive or no evidence from trials) adapting criteria developed by the Cochrane Collaboration Back Review Group (Table 12; Van Tulder 2003).
10. Levels of evidencea.
| Strong | Findings from meta‐analysis or consistent findings across all studies including at least 2 high‐quality RCTs |
| Moderate | Consistent findings across all studies including at least 2 low‐quality RCTs/CCTs or 1 high‐quality RCT |
| Limited | 1 RCT/CCT not reaching high quality |
| Conflicting | Inconsistent findings among at least 2 studies with at least 1 RCT/CCT |
| Inconclusive | Statistical significance of differences unknown in > 25% of all studies |
| No evidence from trials | No RCTs or CCTs |
| Consistent (conflates assessment of direction and precision): statistically significant effect in same direction in ≥ 75% of all studies High‐quality RCTs/CCTs: ≥ 3.5 methodological quality score (ranging from 0 to 6) | |
aadapted from Van Tulder 2003.
CCT: controlled clinical trial; RCT: randomised controlled trial.
Dealing with missing data
Cases with missing data regarding place of death and people who were still alive at the end of the study were excluded from the meta‐analyses.
Assessment of heterogeneity
We quantified heterogeneity using Chi2 and the I2 statistic, the latter quantifying the percentage of the variability in effect estimates that is due to heterogeneity rather than to chance (Higgins 2011); higher percentages suggest more observed heterogeneity.
Assessment of reporting biases
We examined the funnel plot for our primary outcome (death at home), to explore heterogeneity and publication bias. As the number of studies was less than 10 and only three were of high quality, we did not perform statistical tests for funnel plot asymmetry (in these conditions the power of the tests is considered too low to distinguish chance from real asymmetry; Higgins 2011).
Results
Description of studies
Also see the Characteristics of included studies, Characteristics of excluded studies, Characteristics of studies awaiting classification and Characteristics of ongoing studies tables.
Results of the search
We identified 7594 records through searches of databases, excluding duplicates. After screening the titles and abstracts, we excluded 6986 (see reasons in Figure 1). We reviewed the full text of the remaining 608 records for a more detailed evaluation. Of these, 53 reports (of 23 studies) met our inclusion criteria and were included in the review.
1.
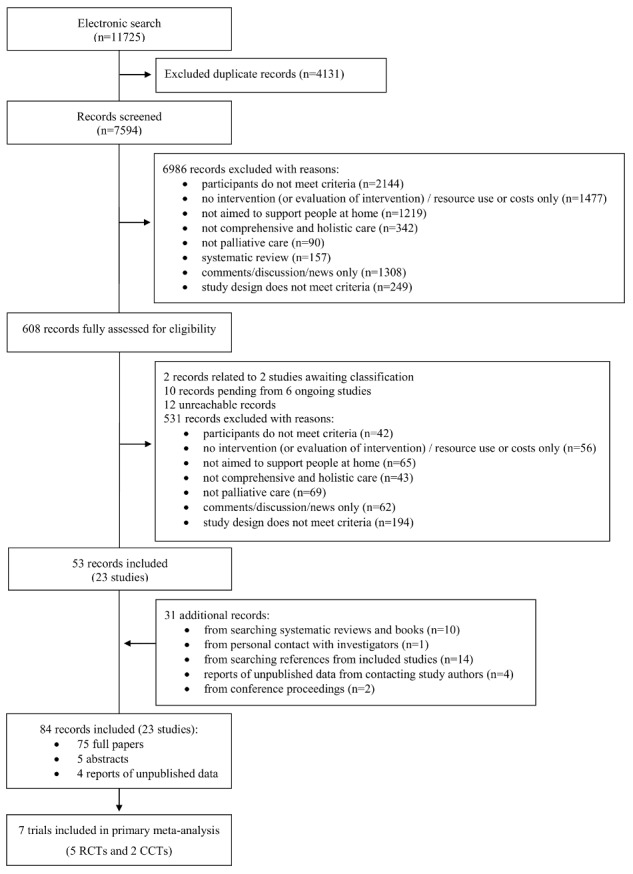
PRISMA flowchart
The search of reviews and textbooks identified no new studies but found 10 additional references reporting on the already included studies. Searches of conference proceedings added two records to an already included study (one conference abstract and one paper). Personal contact with investigators added no new studies (yet identified one additional reference on an already included study). These additional 13 records were included in the review.
We screened the reference lists from the 23 included studies but no further eligible studies were found (yet another 14 records on the included studies were added, one of them a pooled analysis of two included studies). Personal contact with study authors added four reports of unpublished data. These 18 records were also included in the review.
In summary, the review included 23 studies reported in 84 records (75 full papers, five abstracts and four reports of unpublished data), ranging from one to 16 records per study.
Included studies
Design
Sixteen studies were RCTs (including three cluster RCTs and two fast‐track trials). Four studies were CCTs (including two cluster CCTs). Two studies were CBAs: Gómez‐Batiste 2010 compared 62 home support palliative care teams with 43 hospital palliative care teams and Greer 1986 compared 39 home hospice care sites (20 community‐based and 19 hospital‐based) with 14 conventional care sites. One study was an ITS with a nested CBA, comparing the three years before and three years after the introduction of eight Macmillan home nursing services in the UK (four attached to inpatient hospices). For two of these services, the authors could only provide two or one year data prior to their introduction; as this did not meet our ITS inclusion criteria we analysed data only for the remaining six services (Ward 1987).
Sample sizes
The studies' sample sizes varied between 42 and 747 participants, except for two non‐randomised studies (Greer 1986 with 1754 cancer patients and their caregivers and Ward 1987 with 31,890 cancer deaths). Excluding the latter study, which covered a period of six years, recruitment length ranged from 1 to 50 months. In total, we analysed data from studies involving 41,603 participants (37,561 patients and 4042 caregivers).
Eleven studies were guided by power calculations (details in 'Characteristics of included studies'): three powered the study on quality of life (one also performed calculations on care costs and one on symptom intensity and depression), two on place of death, two on pain (one also performed calculations on nausea), one on overall palliative care outcomes, one on caregiver general health and one on care costs. In one study (McMillan 2007), the authors performed power calculations but provided no details.
Seven of these 11 studies were underpowered at recruitment stage (i.e. participants enrolled) – by 3, 7, 10, 78, 54, 151 and 319 participants. Reasons included lower than expected referrals and proportion of eligible patients, and early deaths. The remaining four studies recruited the planned number of participants but none had the planned numbers at the first time point for analysis of the primary outcome (following baseline assessment and after receiving the intervention or control). At that point, they were underpowered by three participants (Brumley 2007), four participants (Higginson 2009), 57 participants (Walsh 2007) and 131 participants (Jordhøy 2000). Four RCTs published methodological papers discussing challenges and solutions in recruitment, attrition and compliance (Higginson 2009; Jordhøy 2000; McMillan 2007; McWhinney 1994).
Two trials conducted post‐hoc power calculations. Aiken 2006 was underpowered (power fell from 0.93 at baseline to 0.74 at first point for analysis after receiving the intervention or control); Hudson 2005 achieved power values ranging from 0.70 (t‐test for independent samples) to 0.99 (t‐test for related samples). Overall, most studies (12 out of 23) examined post‐intervention assessments of fewer than 120 participants.
Setting
Eleven studies were conducted in the US (seven in metropolitan areas, two in rural areas and two in mixed areas including Greer 1986 across areas in Southern New England, Northern Midwest and Southern California). Five studies took place in the UK (three in the London metropolitan area, two in more mixed areas of the country). Three studies were conducted in Northern Europe (two in metropolitan areas in Sweden and one across six metropolitan and two rural areas in Norway). Two studies were conducted in Southern Europe (one in the Vicenza mixed urban and rural health district in Italy and one nationwide study in Spain). One study took place in the city of London in Ontario, Canada (McWhinney 1994) and one in the city of Melbourne, Australia (Hudson 2005).
The first studies were conducted in the US – one in New Haven (1975 to 1977, Buckingham 1978) and one in Vermont (four‐year study published in 1979, McKegney 1981); 10 studies were conducted or first published from 2000 onwards (see 'Characteristics of included studies' for details on dates).
Seven studies recruited mainly from departments in general hospitals and four recruited mainly from primary care (including community services and US health management organisations). One study recruited only from an US Veteran Affairs (VA) hospital, with a population of largely male veterans (Hughes 1992). Three studies recruited from cancer centres or secondary care professionals (e.g. oncologists). One study used a variety of referral sources including community agencies, hospitals, managed care organisations, physicians, family/friends and self referrals (the latter were also accepted in three other studies) (Aiken 2006). Four studies were undertaken within existing specialist home palliative or hospice care teams. Ward 1987 was population‐based (ITS drawing on death certificate data). Greer 1986 recruited from 39 home hospice care sites and 14 conventional care sites. Gómez‐Batiste 2010 recruited from 62 home support palliative care teams and 43 hospital palliative care teams. Intervention and control groups were recruited from the same setting in all but Gómez‐Batiste 2010 and Greer 1986.
Participants
Fourteen studies were exclusively conducted with patients with advanced cancer or their caregivers, or both. Six studies included both cancer and non‐cancer conditions (in three studies the majority of patients had cancer). Three studies included only non‐cancer conditions: multiple sclerosis (MS) in one study (Higginson 2009), congestive heart failure (CHF) and COPD in one study (Rabow 2004) and AIDS in one study (Tramarin 1992). Median/mean age ranged from 53 to 77 years, except in Tramarin 1992 (approximate median was 30 years old). Approximately equal numbers of male and female patients were included, except in four studies where between 60% and 69% were women and in four studies where more than 60% were men (Gómez‐Batiste 2010 with 61% male patients, McCorkle 1989 with 63% male patients, Tramarin 1992 with 79% male patients and Hughes 1992 with largely male veterans). Across eight studies, between 12% and 43% of patients lived alone. Nine out of 14 studies involving caregivers described their characteristics; these were mostly spouses and women (median/mean age ranged from 56 to 63 years).
Fifteen studies used participants' expected survival as a criterion for study inclusion. Minimum life expectancy (estimated at recruitment usually by physicians) ranged from two weeks to three months, whereas maximum values ranged from two weeks to five years. Actual median/mean survival from enrolment was less than three months in five studies, between three and five months in two studies, and between six months and approximately one year in three studies.
Two studies were conducted with newly diagnosed patients (within 8 to 10 weeks in McCorkle 1989 and 8 to 12 weeks in Bakitas 2009). Exclusion criteria included enrolment in or transfer to hospice care in two studies (Brumley 2007; Rabow 2004), enrolment in a home health agency (McCorkle 1989), and admission to an inpatient hospice, assisted‐living facility or nursing home in one study (McMillan 2007). Ten studies excluded patients with no caregiver.
Intervention
Home palliative care
Nineteen different models of home palliative care were examined (Table 13). Some were new interventions, evaluated through pilot studies, demonstration projects or early phase trials (e.g. Tramarin 1992Rabow 2004 and Higginson 2009, respectively); others existed for some time (e.g. the palliative care home support team in McWhinney 1994 existed for 18 months, the hospital‐based home care (HBHC) team in Hughes 1992 existed for 13 years).
11. Nineteen models of specialist and intermediate home palliative care.
| Study, country, setting | Type of care |
Service base |
Core team, responsibility | Theoretical framework | Intervention | Contacts, duration |
| Axelsson 1998Sweden, Östersund, county of Jämtland, metropolitan (sparsely populated region) | Specialist | Department of General Surgery at County Hospital of Östersund | Full‐time nurse (weekdays from 8 a.m. to 5 p.m., equipped with leasing care and phone) with 15 years' experience of practical cancer care in a surgical ward, trained in pain relief and symptom control, surgeon (half‐day per week); responsibility not stated but service worked with primary care centres; weekly review meetings | — | "Palliative Support Service" new programme * nurse role ‐ link between home and hospital; patient, caregiver and staff support; district nurse education on care management; administration of blood transfusions, low‐dose chemotherapy and parenteral nutrition at home * surgeon role ‐ screening of referrals; case review with nurse at weekly conference; occasional home visits * dossier given to patient at discharge |
Median 14.5 hours of contact with nurse and 2 hours of contact with surgeon; 70 days median length of stay in intervention; all intervention patients analysed died within study period |
|
Bakitas 2009 US, New Hampshire and Vermont, rural |
Specialist | Palliative care programme, Dartmouth‐Hitchcock Medical Center (National Cancer Institute‐designated comprehensive cancer centre) | Palliative care physician, advanced practice nurses with high specialty training in palliative care; nurses acted as case managers but primary team held final responsibility for medical decisions; 12‐20 hours of staff training (materials available from authors); biweekly reviews of audio‐taped sessions and feedback on difficult patient management issues | Chronic care model | "Project ENABLE II" followed a demonstration project * without forgoing curative care * needs assessment using Distress Thermometer * case management * crisis prevention * patient and caregiver education * education manual (available from authors) * monthly group shared medical appointments * referral to other resources (e.g. palliative care team, hospice, spiritual counsellor) * nurse readily available by phone * follow‐up call in bereavement * intervention manual (available from authors) |
Telephone‐based format, 4 sessions (31‐40 min), at least monthly telephone follow‐ups (14 months median survival in intervention group, 112/161 deaths in intervention group during mean 14.6 months' follow‐up), bereavement follow‐up call |
| Gómez‐Batiste 2010Spain, all 19 regions, mix of metropolitan and rural | Specialist | 63 teams, base not stated | Teams typically included doctor, 2 or 3 nurses, psychosocial worker (social worker or psychologist) with advanced training in palliative care; not stated who held responsibility but services aimed to advise other conventional teams in the community | — | Existing teams no specific information about intervention components |
According to previous study, teams performed a mean of 9 interventions per patient and telephone calls were second most frequent activity; 42 days median length from day of first clinical visit to death or last monitoring visit; 42 patients died and considered drop‐outs |
|
Higginson 2009 UK, London, metropolitan |
Specialist | Intra‐hospital palliative care team at King's College Hospital (general public teaching hospital) | part‐time palliative medicine consultant with training in neurology and interest in MS, part‐time clinical nurse specialist working in neurology and with some palliative care training, full‐time administrator; responsibility not stated but service aimed to complement and not to replace existing services; weekly review meetings for consultant to input into management of all patients | — | Phase II study followed previous steps of MRC framework for the evaluation of complex interventions * service referrals used standard form * initial needs assessment * action plan and follow‐up (communicated to primary team and other professionals) * joint review with neurologist and other professionals in weekly multi‐professional MS clinics (in addition to phone and email contact) * crisis prevention * welfare benefits advice * bereavement support * staff education and support * referral to longer‐term specialist home palliative care services based on need (WHO definition) |
Short‐term: 1‐3 contacts (initial needs assessment with "average" 110 min direct contact and 90‐min liaison/administration; further visits or telephone calls, or both); patients seen in their place of choice (often home, sometimes outpatient clinics, nursing home, hospital); 4/52 patients died during study period |
| Jordhøy 2000Norway, Trondheim, 6 metropolitan and 2 rural areas | Specialist | Palliative medicine unit at University Hospital of Trondheim (unit with 12 beds, outpatient clinic and consultant team in and out of hospital) | Full‐time physician; 2 palliative care nurses, social worker, priest, nutritionist, part‐time physiotherapist (all worked day hours only); nurse acted as care co‐ordinator but primary family physician and community nurse remained main professional carers; weekly review meetings | "Grounded on holistic philosophy" | New intervention * multidisciplinary approach to patient's needs * care co‐ordination * link between palliative medicine unit and community services under predefined guidelines * initial care plan set up in meeting with patient, caregivers, family physician, community nurse * follow‐ups by community staff supervised by team (available for joint home visits) * staff education programme (bedside training, 6‐12 hours of lecturers every 6 months on symptoms and difficulties in palliative care) * inpatient and outpatient services provided at unit except when required for medical reasons * no out of hours or on‐call service |
Contacts and duration not described; 99 days' median survival in intervention group; 219/235 intervention patients died during study period |
| McWhinney 1994Canada, London, Ontario, metropolitan | Specialist | 14‐bed palliative care unit (host organisation not stated) | Physician, 2 experienced palliative care nurses (working 1 week on, 1 off) and a part‐time social worker; responsibility remained with family physician and home care nurses (consulting and support service only) | — | "Palliative care home support team" service existed for 18 months * nurse assessment within 3 days of referral * care plan with team's physician, copies sent to family physician, home nurse and case manager * follow‐ups varied from no further contact to monitoring phone calls to periodic visits (as per wishes of patient and family and negotiation with family physician and home nurse) * 24 hours on‐call nursing with physician back up and contact given (if family physician and home nurse not available) |
Initial nurse assessment at home and follow‐ups varied from no contact to periodic visits; duration not described; 36/146 patients died within the first month |
|
Ahlner‐Elmqvist 2008 Sweden, Malmö, metropolitan |
Intermediate | Hospital oncology department at Malmö University Hospital | 9 experienced nurses (day and evening shifts and night emergencies); oncologist, social worker, physiotherapist, secretary (day hours only); priest associated on consultation basis; all with long experience in advanced cancer care with no formal training but attended palliative care training programme prior to service start; weekly meetings | — | "Advanced Home Care ‐ AHC" new 7‐days/week service * symptom treatment, counselling and emotional, social and family support * team home visits planned according to patient's needs and with degree of flexibility * administration of injections, intravenous fluid therapy, blood transfusions, chemotherapy, nasogastric intubation, catheterisation of urine bladder and other forms of technical support * access to on‐call service from service base * 3 'back‐up' beds available (2 at hospice and 1 at the oncology unit) |
Contacts and duration not described; 94 days median survival in intervention group, 117/119 intervention patients died during study period |
|
Aiken 2006 US, Phoenix, Arizona, metropolitan |
Intermediate | Hospice of the Valley (largest community‐based hospice care provider in the US) | Physician (medical director), from 2 or 3 registered nurse case managers, half‐time social worker, half‐time pastoral counsellor; staff training (2 weeks on FairCare communication model and other monthly training); team's nurse responsible for care with primary care physician and HMO case manager; nurse went with patient to physician visits to discuss progress and care options | Patient empowerment model and behaviour change theory | "PhoenixCare Intervention" * without forgoing curative treatment * disease and symptom management, patient/ caregiver education, psychosocial and spiritual support, needs assessment, care co‐ordination, case management * management protocols by phase of illness (initially unstable, stable, unstable following exacerbation) * individualised emergency response plan at home (used in hospice care) with contacts * advance care planning with patient/family * referral to counselling and other resources * patient notebook at home *on‐call nursing |
Nurses contacts ("average" 6, 5, 4, 4, 3 and 3 in first 6 months and stable from then onwards; half calls, half visits); visits from other staff (45% saw social worker, on "average" 6 times); duration from enrolment to death (16% intervention patients died within study period), transfer to hospice care or skilled nursing care facility, or study end |
|
Brumley 2007 US, Hawaii and Colorado, metropolitan |
Intermediate | 2 non‐profit Kaiser Permanente Group HMOs | Physician, nurse, social worker with support from others (spiritual counsellor/chaplain, bereavement co‐ordinator, home health aide, pharmacist, dietician, volunteer, physiotherapist, occupational therapist, speech therapist); patients could maintain primary care provider while receiving home visits team | "Modelled after hospice programs" | "In‐Home Palliative Care – IHPC" * without forgoing curative care * patients assigned to palliative care physician to co‐ordinate care from a variety of healthcare providers * medical care, symptom management, patient and caregiver education, biopsychosocial support, continuous needs assessment, care management * joint care plan to decide frequency of visits * advance directives with patient and family * patient wrist band for emergency department staff to know patient was in home palliative care and had advance directives (1 site only) * physicians home visits, nursing care 24 hours/day |
Contacts not described; duration from enrolment to death or transfer to hospice care; 196 days mean survival in intervention group; 225/310 patients died within study period |
|
Buckingham 1978 US, New Haven, metropolitan |
Intermediate | Not stated | Described as "experienced services"; not stated who held responsibility for care | — | "Hospice home care program" * aimed to provide for many needs that often cannot be met in acute care settings |
Contacts and duration not described |
|
Grande 1999 UK, Cambridge health district |
Intermediate | Marie Curie nursing service and inpatient hospice | 6 qualified nurses, 2 nursing auxiliaries, co‐ordinator, most with Marie Curie nursing experience; not stated who held responsibility for care | — | "Cambridge Hospital At Home ‐ HAH" * practical home palliative nursing care * care available up to 24 hours a day |
Median 18 hours of HAH for a maximum of 2 weeks; 11 days median survival in intervention group |
|
Greer 1986 US, Southern New England, Northern Midwest and Southern California, metropolitan and rural |
Intermediate | 20 community‐based hospices without inpatient beds, 19 hospital‐based hospices with inpatient beds | Medically supervised interdisciplinary teams composed of several individuals with appropriate skills including professionals and volunteers; teams medically supervised but not stated who held responsibility for care | Grounded on hospice and humanistic philosophy of caring for terminally ill patients and their families as per National Hospice Organization's 1979 standards of hospice programme of care | "Hospice care" * palliative, preventive, supportive, less resource‐intensive and with more informal care (family and volunteers) than conventional care * palliative care and control of symptoms, physical, emotional and spiritual distress * emphasis placed upon care in the home * individualised care plan and provision * choices about treatment and place of death * family supportive care during dying process and bereavement (this may include follow‐up visits) * maximum access regardless ability to pay * treating patient and caregivers as a unit * inpatient and home care services closely integrated to ensure continuity and co‐ordination * education programme (for patient, family and team) * availability 24 hours/day |
Contacts not described; "average" 72 days length of stay in intervention for community‐based hospices and 63 days for hospital‐based hospices; half of all patients died within 35 days of admission, nearly 20% stayed ≤ 10 days; all patients analysed died within study period |
|
Hughes 1992 US, Hines, Illinois, metropolitan |
Intermediate | Edward Hines Jr. VA Hospital (department not stated) | Physician‐led team including nurses, social worker, physiotherapist, dietician, health technicians (physician also managed the hospital's inpatient intermediate care unit thus maximised potential for continuity of care across home and hospital); team meetings; not stated who held responsibility for care | — | "Hospital‐based home care ‐ HBHC" service existed for 13 years * emphasis on care to high‐risk patients * comprehensive services based on need * timely communication across team members * involvement and training of informal caregivers in patient care to the maximum extent possible * patient and family as unit of care * education strong service component * goal‐oriented, interdisciplinary care plan * scheduled visits according to individual needs * physician home visits, pharmaceuticals, supplies |
Mean 17.93 team visits in 6 months from enrolment (duration of intervention); 76 days mean survival in intervention group; 79% intervention patients died within study period |
|
McCorkle 1989 US, King County, Washington, metropolitan and rural |
Intermediate | Not stated | Nurses with masters' degrees and trained to give personalised clinical care to people with advanced cancer and their families; other specialised services called upon as needed; nurse was care co‐ordinator but not stated who held responsibility for care | Oncology transition services model | "Specialized Oncology Home Care Program ‐ OHC" * personalised care in home setting * advanced education in symptom management * nurse acting as central care co‐ordinator * 24‐hour access to nursing staff |
Contacts and duration not described; 87/166 patients died during study period |
|
McKegney 1981 US, Vermont, rural |
Intermediate | Vermont Regional Cancer Center (department not stated) | Trained oncology nurse practitioners with extensive experience in care of the patients with advance cancer backed up by usual multidisciplinary team at the cancer centre; formal interdisciplinary training on extended assessment skills; weekly team conferences; nurses acted as link between the multidisciplinary team and as care co‐ordinator responsible for patients through home visits, clinic visits, and hospitalisations to ensure continuity; primary physician informed and collaborated in complex medical problems | — | "Intensive home care" *aimed to improve patient's quality of life and communication between conventional cancer rehabilitation team and patient * patients assigned oncology nurses to closely monitor and co‐ordinate care, anticipate and solve medical and psychosocial problems * initial interdisciplinary assessment followed by care plan build by nurse * home visits focused on patient needs ("incidental interactions with family"), physical care, talking with patient about illness and implications, mobilising family and social resources and co‐ordinating with patient's physician * protocol for pain management, nausea, vomiting, home administration of intravenous chemotherapy drugs (available from authors) * pain killers given regularly for continuous control |
Home visits (35‐40 min) with frequency defined based on prognosis (life expectancy < 3 months biweekly visits; ≥ 3 months monthly visits); duration not stated; 345 days mean survival in intervention group; 139/199 patients died within study period |
|
Rabow 2004 US, San Francisco, California, metropolitan |
Intermediate | General medicine practice at University of California Medical Center (tertiary care) | 3 physicians, nurse, social worker, chaplain, pharmacist, psychologist, art therapist (all with expertise in palliative care), volunteer co‐ordinator, volunteer medical/pharmacy student patient advocates; regular physician‐led meetings; collaboration with other services; social worker responsible for case management; team's physician advised primary physician who retained responsibility for medical care | Social work centred case management approach | "Comprehensive Care Team" demonstration project * without forgoing curative care * 7 components: 1) formal consultations 2) case management 3) caregiver education and support 4) medical chart review 5) spiritual and psychological support 6) patient/caregiver support groups 7) patient support and advocacy |
3 consultations, "average" 3.8 social worker in‐person contacts and 13.0 telephone calls; at least 1 chaplain contact and 1 medical chart review (pharmacist), mean 2.2 hospital visits to hospitalised patients, "average" 6.5 advocates' contacts (telephone calls, home visits, hospital visits); 1‐year duration; 10/50 intervention patients died within study period |
|
Tramarin 1992 Italy, Vicenza health district and surroundings, metropolitan and rural |
Intermediate | Infectious diseases department at San Bortolo Hospital, with 15 beds, outpatient clinic and hospice offering home care | Multidisciplinary team of 4 trained nurses, psychologist, 10 volunteers, social workers (where available), 2 infectious disease specialists; patient's family doctor viewed as part of team; consultant doctors at the department supervised other caregivers (family doctors, volunteers, social care agencies) | "Based on the principles of palliative care (...) in line with National Health AIDS Plan guidelines" (Tramarin 1992) | "Home‐care Assistance" pilot study * integrated package of home care * aimed to improve quality of life whenever possible through symptom control * aimed to limit use of inappropriate inpatient services, substituting with palliative care * chemotherapy, parenteral nutrition, blood transfusion and fluids administered if needed at home using a tunnelled catheter |
"Average" of 33.1 staff hours, 29.1 nurse visits and 4.5 specialist visits in 6 month following enrolment; "average" duration of 74.1 days; 5/10 intervention patients died within study period |
| Ward 1987UK, Trent and Yorkshire health regions, metropolitan and rural | Intermediate | 4 teams based at an inpatient hospice and 4 teams with a non‐hospice base (1 hospital, 1 non‐inpatient hospice, 1 in grounds of future in‐patient hospice, and 1 in primary care team offices) | 7 teams were multidisciplinary and 1 was of nurses only, members ranged from 2 to 8; all teams had nurses, 7 had medical input, 5 had social workers; not clear who held responsibility for care although services' aim was to augment but not replace care from district nursing, GPs and families | — | "Macmillan home care nursing care" services existed for ≥ 18 months * home visits to monitor situation, pain and other symptoms, reassure/support, assess need for community care, inpatient or day unit, give advice, deliver equipment/ medication, practical nursing * out‐of‐hours cover ‐ all teams had 24/7 coverage (e.g. hospice out of hours, bleeps, radio paging, nursing message systems, nurses home number, coverage by inpatient hospice staff for advice) * patients from teams based at inpatient hospices could access hospice beds, day centres, family relief and other hospice services |
Service routine data showed mean home visits per patient/month ranged from 2.3 to 7.7 for hospice‐based services and from 7.9 to 12.5 for non‐hospice based; out‐of‐hours visits ranged from 0 to 9, except in 1 hospice‐based team (40 visits) and in 1 non‐hospice based (81 visits); duration from enrolment to death (median 32 days, range 21.5 to 44.5 days) |
|
Zimmer 1985 US, Rochester, New York, metropolitan |
Intermediate | Ambulatory care unit at University of Rochester Medical Center | Physician, geriatric nurse practitioner (Masters' medical nurse practitioner); social worker; weekly team conferences to assure co‐ordination of patient care; 1 team member designated as primary provider in care plan following initial interdisciplinary assessment |
— | "Home Health Care Team" service existed for 2 years * aimed for home‐bound, chronically or terminally ill, or disabled patients (largely elderly) when attending clinics was too difficult * initial home assessment by each team member * interdisciplinary care plan with designated primary professional care provider * nurse role ‐ physical assessments (routine and emergency), responsible for nursing plan, supported medical care * physician role ‐ evaluation at intake, home visits, follow‐ups as needed, patient's attending physician during hospitalisations * social worker role ‐ help deal with social, financial and emotional problems; caregiver support and education * 24‐hour phone service with physician back‐up |
Contacts not described but authors referred to low number of out‐of‐hours calls (over 70% handled on telephone); duration not stated; by 3 months 23/32 of the terminally ill patients had died |
GP: general practitioner; HMO: health maintenance organisation; MRC: Medical Research Council; MS: multiple sclerosis; VA: Veterans Affairs; WHO: World Health Organization
Intervention services were mostly based in hospices, palliative care departments within hospitals or in other hospital departments; seven were attached to units with beds and four provided bed access to intervention patients when needed. Most served urban and suburban populations. Bakitas 2009 evaluated a telephone‐format intervention for rural populations and McKegney 1981 evaluated an "intensive home care" model in rural Vermont; both were nurse‐led interventions. Others served a mix of metropolitan and rural areas.
Most teams were multidisciplinary, ranging from two to 13 professionals, typically including physicians, nurses and social workers. Three studies evaluated nursing services (Grande 1999; McCorkle 1989; Ward 1987).
The intervention components, format and duration varied. For example, Higginson 2009 evaluated an early short‐term specialist palliative care intervention of one to three contacts from a core clinical team of consultant and nurse, aimed to complement existing local services and not to duplicate or replace them, providing consultation and shared care with other care providers. In contrast, Brumley 2007 was an intermediate palliative care intervention from a larger team with the consultant co‐ordinating care and with 24 hours a day nursing care provided to patients in their last seven months of life.
Four models of care were theoretically grounded (on chronic care model, social work‐centred case management approach, oncology transition services model and patient empowerment model/behaviour change theory). Four stated they were modelled after hospice programmes, followed palliative care principles or adopted a holistic/humanistic philosophy. Ten included arrangements for out‐of‐hours care. Innovative features included the use of the distress thermometer in needs assessment, the use of a patient wrist band for emergency department (ED) staff to know the patient was in home palliative care and had advance directives, individual medical chart review by pharmacist, management protocols by phase of illness (initially unstable, stable and unstable following exacerbation), individualised emergency plan with staff contacts, staff education programmes and patient education manuals/dossiers/ notebooks. Bakitas 2009's intervention was manualised (available from authors).
Reinforced home palliative care
Four models reinforced existing home palliative care with an additional component of caregiver support (Table 14). All were tested within specialist home palliative care teams serving urban and suburban populations (two studies took place in London, UK, one in Melbourne, Australia and one in Tampa, US). The added components were delivered by "carer advisors" with experience in community nursing and social work, nurses, health aides and facilitator‐led multidisciplinary groups of professionals. All were new and brief psychoeducational interventions, with components of advice, support, education, empowering the caregiver for patient care and self care. The "cope intervention" (McMillan 2007) was the only theoretically grounded intervention (drawn on stress process models and problem‐solving training and therapy); however, all others were based in literature and previous research. Innovative features included teaching a problem‐solving method to deal with patients symptoms, caregiver use of assessment scales for pain, breathlessness and constipation with ratings recorded in a symptom diary acting as a foundation for action to call staff, home care guide with 23 patient problems with easy reference for caregivers, telephone format to enable flexibility and to help approach issues difficult to discuss face‐to‐face, provision of transport and patient‐sitting to encourage caregiver participation in group activities. Interventions in Walsh 2007 and McMillan 2007 were manualised (available from authors).
12. Four models of reinforced home palliative care.
| Study, country, setting | Type of care |
Service base |
Core team, responsibility | Theoretical framework | Additional component | Contacts, duration |
|
Harding 2004 UK, London, metropolitan |
Specialist | 2 home palliative care teams (base not stated) | Composition of home palliative care teams not stated; additional component delivered by a facilitator‐led multiprofessional group (1 facilitator per site); weekly facilitators' peer supervision (intervention consistency) | — | "90 Minute Group" new brief caregiver group intervention (research‐based, grounded on literature and qualitative study) * aimed to promote self care * informal teaching * group support (caregiver information and support) * maximum of 12 carers/group (2 at each site) * 4 principles: 1) lack of identification with the label of 'carer', 2) safe and legitimate time/space away from caring, 3) time limited, 4) respectful of existing coping strategies * facilitator introduced multiprofessional input from a changing weekly speaker (welfare benefits advice, occupational and physical therapy, clinical nurse specialist, aromatherapy) and subsequently facilitate group discussion of the weekly themes * group initially focused on patient issues in order to provide legitimacy for attending, and to address the patient‐oriented sources of distress * detailed programmed objectives for each session * transport and patient‐sitting when needed |
Additional component was a 6‐week intervention (6 weekly 90‐minute sessions); survival and mortality not stated |
|
Hudson 2005 Australia, Melbourne, Victoria, metropolitan |
Specialist | 2 home palliative care teams (base not stated) | Home palliative care teams of specialist nurses, doctors, and allied health professionals (including nurses, social workers, medical consultants, pastoral care workers, volunteers, bereavement counsellors); additional component delivered by nurse | — | "Psychoeducational intervention" new brief caregiver psychoeducational support (research‐based, grounded on literature and focus groups with nurses and caregivers) * aimed to enhance support/guidance for caregivers * visits structured around and complemented by audiotape with reflections from caregivers, self care strategies, structured relaxation exercise, and guidebook with information on typical aspects of caring for dying person (link provided in paper) * caregivers read guidebook sections and noted questions prior to visits and call: * first visit ‐ prepared for caregiver role and aspects of caregiving (section 1 and 2 of guidebook) * telephone call ‐ focused on evaluating plans, self care (section 3), new issues and caregiver desire to go on to next section * second visit ‐ focused on evaluating previous strategies, new issues and preparing for dying phase (final section of guidebook) |
Additional component was a 2‐week intervention (2 fortnightly home visits with follow‐up call between visits); survival and mortality not stated |
|
McMillan 2007 US, Tampa, Florida, metropolitan |
Specialist | Large non‐profit community‐based hospice | Composition of home hospice care team not stated (cared for 850 patients/day); additional component delivered by newly hired nurses (1 full‐time, 1 back‐up) and home health aides with hospice experience; 4‐day training on intervention with role play and audiotapes of sessions reviewed monthly to ensure protocols were followed | Additional component grounded on stress process models and problem solving training and therapy | "COPE Intervention" new brief caregiver psychoeducational support * aimed to teach a problem solving method to assess and manage patient symptoms (focus on pain, dyspnoea and constipation) * 4 components: 1) creativity (viewing problems from different perspectives to develop new strategies for solving caregiving problems) 2) optimism (positive but realistic attitude toward problem‐solving process, including communicating realistic optimism to patient) 3) planning (setting reasonable caregiving goals and thinking out, in advance, the steps necessary to reach those goals, e.g. family holiday) 4) expert information (about nature of problem, when and where to get professional help, and what to do on one's own to deal with problem) * Home Care Guide for advanced cancer (for patients and caregivers) with 23 patient problems with easy reference for caregivers * caregiver use of assessment scales for pain, dyspnoea and constipation, findings recorded in symptom diary; ratings were foundation for action to call hospice staff and manage symptoms at home * nurse pager contact * intervention manual (available from authors) |
Additional component was a 9‐day intervention with 3 visits (first 5 min, second and third 30 min) with continued support in between with calls to assess problems, offered support and answer questions; survival and mortality not stated |
|
Walsh 2007 UK, London, metropolitan |
Specialist | 7 home palliative care services covering 3 regional cancer networks (2 hospital‐based, 2 community‐based, 3 inpatient hospice‐based teams) | Home palliative care teams of clinical nurse specialists, specialist medical support and sometimes social work; additional component delivered by 2 part‐time carer advisors experienced in community nursing and social work (1 month's training with fieldwork in palliative care in home, hospice, hospital settings); weekly meetings between advisors and researchers for debriefing, advice on emerging issues and to ensure all domains of need were covered; half‐day training session on intervention after 1 year | — | "Carer advisor" new brief caregiver‐focused intervention (research‐based, grounded on literature and pilot with caregivers on preferred mode of extra support) * aimed to meet caregiver alone (outside home, at workplace, evenings or weekends if needed) * mainly face‐to‐face but sometimes on phone (enabled flexibility and helped approach issues difficult to discuss face‐to‐face) * comprehensive needs assessment, discussion and advice on past, present and future issues * information and emotional support * covered physical and psychological health, need for time away from patient in short and long term and to plan future, relationships and social networks, relationships with services, finances * kept to giving advice and support rather than taking action on behalf of caregivers (advice went as far as helping to calculate benefit entitlements) * bereavement support and advice * intervention manual (available from authors) |
additional component was a 6‐week intervention (6 visits over 6 weeks), introduced at second/third contact with team and if patient died before sixth contact, visits took place after death; mean 5 contacts and mean 3.6 contacts up to death; 13 weeks median survival in intervention group; 47/137 intervention patients died during study period |
Controls
While models of reinforced home palliative care were compared with the care provided by existing specialist home palliative care teams, wider evaluations of home palliative care services (intermediate or specialist) compared it with usual care. The latter varied across studies, reflecting differences in health systems and local service provision. For example, in Jordhøy 2000, usual care was shared among hospital departments and the community including family physicians, home nursing (provided by nurses and nurse‐assistants with 24 hours a day coverage in all but the smallest district) and nursing homes, but with no well‐defined routines and no specialist palliative care provision. In Brumley 2007, on the other hand, controls received various amounts and levels of primary care services, home health services (when Medicare criteria were met), acute care services and hospice care. McCorkle 1989 included two control groups: home care (provided by an interdisciplinary team representing standard Medicare‐reimbursed services available in the community) and traditional outpatient care (provided by the patient's physician and outpatient staff with no general or specialised home nursing care). Gómez‐Batiste 2010 compared home palliative care with hospital palliative care.
Outcomes
Nine studies reported whether the patient died at home or not. Other outcomes related to place of death included death in hospital (six studies), death in a nursing home (five studies), death in an inpatient hospice/palliative care unit (five studies) and time the patient spent at home (five studies). Two studies reported on caregivers' views about the place where the patient died.
Other patient outcomes included symptom burden, physical symptoms (pain, breathlessness, sleep disturbance, nausea/vomiting, constipation, diarrhoea, fatigue and appetite loss), advance care planning, patient self management of illness, patient unmet needs, quality of life, general health, survival, physical function, psychological, social and spiritual well‐being, nutrition and cognitive status.
Caregiver pre‐bereavement outcomes included dimensions of well‐being and quality of life (psychological, social, physical, pain and general health) and caregiving‐related outcomes (burden, mastery, positive aspects of caregiving, unmet needs, coping and distress with patients' symptoms). Post‐bereavement outcomes included grief, and well‐being and quality of life dimensions.
Family outcomes were satisfaction with care and overall palliative care outcomes.
Economic data
Sixteen studies measured the resource use associated with receiving the intervention and the control. This included ED visits; stays in intensive care; admission, days and proportion of time spent in nursing homes and hospitals; length of hospital admissions including the last one before death; overall institutional days; outpatient clinic visits; a range of community services; informal care; medication and other resources; caregiver post‐bereavement healthcare use and absenteeism from work.
Eight of these 16 studies calculated the costs associated with the resources used; six reported on total costs. Higginson 2009 provided cost‐effectiveness planes for the primary outcome (palliative outcomes) and a secondary outcome (caregiver burden). Tramarin 1992 (the only full economic evaluation) calculated cost‐utility ratios.
Risk of bias in included studies
Randomised controlled trials/controlled clinical trials
Six of the 16 RCTs were considered of high quality, while none of the four CCTs reached high quality (Figure 2).
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Random allocation to the intervention was described explicitly and conducted using a centralised scheme in nine trials. In five RCTs the procedures were unclear and in Tramarin 1992 randomisation was contaminated; 25/32 controls were not randomised but allocated to usual care as they failed to meet one or more criteria for service eligibility. Allocation was based on geographical proximity to the intervention in the two cluster CCTs (areas closer to the base were offered the intervention), patient preference in Ahlner‐Elmqvist 2008 and caregiver preference in Harding 2004.
Follow‐up
Only two studies were able to follow‐up 80% or more on all outcomes analysed: Higginson 2009 (46/52 patient and caregiver dyads at the end of the study) and Tramarin 1992 (39/42 patients followed‐up on quality of life, the only outcome analysed). In seven studies follow‐up varied by outcome with some above and others below the 80% threshold required for quality (Ahlner‐Elmqvist 2008; Bakitas 2009; Brumley 2007; Grande 1999; Hughes 1992; Jordhøy 2000; Zimmer 1985). For example, in Grande 1999, although follow‐up was high for the primary outcome (death at home known for 95% of participants randomised) only 53% were followed‐up on pain (measured via caregivers six weeks after death). In two studies, follow‐up was not stated for most outcomes (Buckingham 1978;McKegney 1981). In the remaining nine studies, follow‐up of all outcomes analysed was below 80%. Jordhøy 2000, McMillan 2007 and McWhinney 1994 discussed problems with attrition due to decline, weakness, exhaustion, cognitive impairment, death and caregiving‐related reasons. Attrition rates at one month in these studies were of 36% patients and 49% caregivers, 69% and 38% patient and caregiver dyads, respectively.
Blinding
Although likely to occur due to the nature of the intervention, lack of participant blinding was explicitly mentioned in only four studies (Bakitas 2009; Grande 1999; Higginson 2009; Zimmer 1985). Bakitas 2009 and Zimmer 1985 were double‐blinded at baseline but not in follow‐up. McCorkle 1989 was also double‐blinded at baseline. In five studies (Aiken 2006; Brumley 2007; McMillan 2007; McWhinney 1994; Walsh 2007), researchers who collected outcome data from participants were kept blinded throughout the study.
Baseline measurement
Nine studies (eight RCTs and one CCT) measured participant characteristics and outcomes at baseline and found no substantial differences between intervention and control groups. Baseline differences in other trials involved the intervention group having lower caregiver strain and higher quality of life (Walsh 2007), doing "notably better" in most outcomes (McCorkle 1989), having better social functioning and mental health scores (Aiken 2006), living in a villa/apartment and having greater informal care and less home care (Jordhøy 2000). In addition, 25/32 controls in Tramarin 1992 (those who were not randomised) failed to meet one or more of the following conditions: adequate economic and family support, living within 10 km from hospital and willingness to accept home care.
Baseline differences in CCTs, other than the criteria used for allocation (i.e. preference or geographical proximity to intervention base), were evident in Ahlner‐Elmqvist 2008 where the intervention group had poorer physical function, a longer length of illness and less frequently a diagnosis of lung and gastrointestinal cancer.
Reliability of outcome measurement
Most trials assessed a mix of objective outcomes obtained from automated systems (e.g. place of death) and subjective outcomes collected from participants by the researchers. In three RCTs participants self completed the measures in the absence of researchers using standardised tools (Bakitas 2009; McCorkle 1989; McWhinney 1994). Inter‐rater reliability was examined in two studies. McKegney 1981 found a Pearson correlation coefficient of 0.70 between trained independent professional raters on main scale items in pilot stages of the project. McMillan 2007 found that caregivers overestimated symptom intensity for pain (the difference in mean scores was 1.33 in a 0 to 10 scale), breathlessness (0.78 difference in mean scores in a 0 to 10 scale) and constipation (1.08 difference in mean scores in 0 to 16 scale); all three differences were highly significant (paired t‐tests; P value < 0.001). Pearson correlation coefficients were 0.40, 0.46 and 0.51, respectively.
Protection against contamination
In 15 of the 20 studies, patients/caregivers rather than professionals were allocated to the intervention or control. In four studies, allocation was based on geographical area thus it is unlikely that the controls received the intervention. In Rabow 2004, two general medicine clinic modules within the same medical centre were randomly assigned to the intervention and control. Each comprised separate patients and physicians originally assigned based on space and appointment availability, housed in the same building, but with separate waiting areas and nursing and clerical staff. However, communication between intervention and control professionals could have occurred.
Controlled before and after studies/interrupted time series
Two of the three CBAs were considered high quality, while the ITS undertaken as part of Ward 1987 did not reach high quality (Figure 2).
Economic evaluations with total costs
All the six studies that examined total costs were considered high quality economic evaluations (Figure 3) but were typically small and had varying methods and items of resource use that precluded meta‐analysis. In terms of study design, nearly all studies clarified and justified the research question, its economic importance and the rationale for choosing the intervention and control(s) compared. However, only two stated the form of economic evaluation used (cost‐effectiveness analysis in Higginson 2009 and cost‐utility analysis in Tramarin 1992) and viewpoints(s) of analysis were not always clear or justified. In terms of data collection, nearly all studies were clear about the effectiveness component (source of estimates, measurement methods, results) and quantities of resources were reported separately from their unit costs in all studies except in Brumley 2007. However, two studies provided limited currency and price data (Zimmer 1985 and Greer 1986) and details of currency or price adjustments for inflation or currency conversion were only given in one study (Tramarin 1992). None of the six studies discussed productivity changes (time off work because of illness, therapy or caregiving). In terms of analysis and interpretation of results, all studies were clear about the time horizon of costs and benefits, they all answered to the study question given, and the conclusions followed from the data reported. Downpoints were the lack of detail about statistical tests and confidence intervals, about the ranges over which the variables varied, and about disaggregated outcome data.
3.
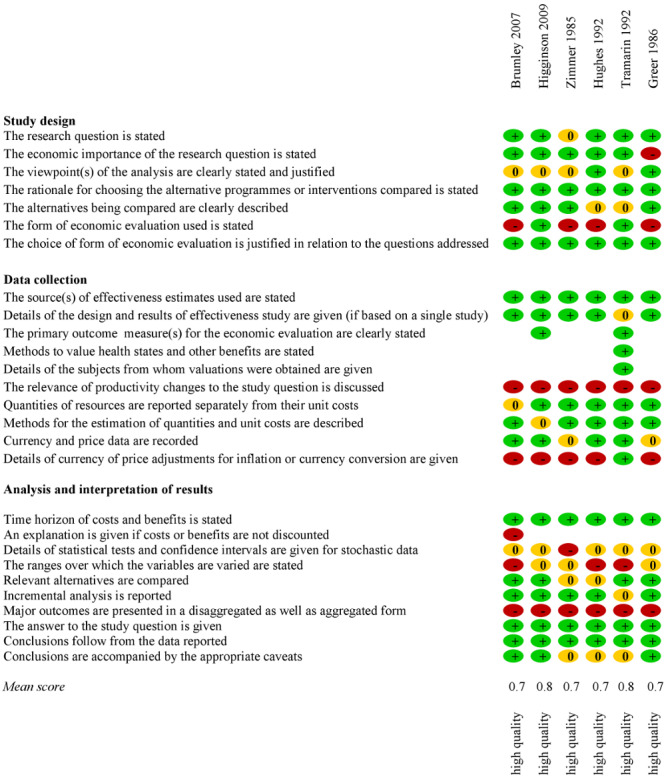
Quality assessment of economic evaluations with total costs.
Effects of interventions
Home palliative care versus usual care
Death at home
Pooled data from seven studies (five RCTs, three of high quality, and two CCTs with 1222 participants) showed that those receiving home palliative care had statistically significantly higher odds of dying at home than those receiving usual care (OR 2.21, 95% CI 1.31 to 3.71; Z = 2.98, P value = 0.003; Chi2 = 20.57, degrees of freedom (df) = 6, P value = 0.002; I2 = 71%) (Analysis 1.1). The study population control risk was of 307 home deaths per 1000 deaths; based on this ACR of 0.307, the NNTB was 5 (95% CI 3 to 14), meaning that for one additional patient to die at home five more would need to receive home palliative care as opposed to usual care. Assuming a medium cancer home death rate population ACR of 0.278 (i.e. 278 home deaths per 1000 cancer deaths), the NNTB was 6 (95% CI 3 to 15). This means that for one additional cancer patient to die at home in a population where there are 278 home deaths per 1000 cancer deaths, six more would need to receive home palliative care. NNTB estimates ranged from 9 patients (95% CI 5 to 16) when applied to a low home death rate population such as the one observed in Norway (128 home deaths per 1000 cancer deaths) to 5 patients (95% CI 3 to 13) when applied to a high home death rate population such as the one observed in the Netherlands (454 home deaths per 1000 cancer deaths) (Cohen 2010).
The funnel plot (Figure 4)suggested some asymmetry but the small number of studies precluded tests to distinguish chance from real asymmetry. The plot also suggested that the largest CCT (Ahlner‐Elmqvist 2008) could be an outlier. Sensitivity analysis excluding this CCT resulted in a reduction of the OR to 1.70 but the effect on death at home remain statistically significant (95% CI 1.27 to 2.28; Z = 3.59, P value = 0.0003; heterogeneity: Tau2 = 0.00; Chi2 = 2.76, df = 5 (P value = 0.74); I2 = 0%). Further sensitivity analysis showed that exclusion of the two CCTs (both of Swedish hospital‐based services with a pooled OR 3.44, 95% CI 0.60 to 19.57) resulted in more precision and less heterogeneity with an OR of 1.73 (95% CI 1.28 to 2.33; Z = 3.60, P value = 0.0003; Chi2 = 2.57, df = 4, P value = 0.63; I2 = 0%). These findings were similar to when only high quality RCTs were considered (OR 1.75, 95% CI 1.24 to 2.47; Z = 3.20, P value = 0.001; Chi2 = 1.71, df = 2, P value = 0.42; I2 = 0%; Analysis 1.2).The direction of the effect was consistent across all seven trials, regardless of statistical significance.
4.

Funnel plot of comparison: 1 Home palliative care versus usual care, outcome: 1.1 Death at home.
Brumley 2007 was the only RCT where differences in death at home reached statistical significance. This trial (of high quality) was conducted with cancer, CHF and COPD patients and evaluated a physician‐led intervention based in integrated healthcare organisations offering physician home visits and 24 hours a day nursing care.
The majority of participants in all seven trials in the meta‐analysis had cancer but three also included non‐cancer conditions (Brumley 2007; Grande 1999; Zimmer 1985). Three interventions provided specialist palliative care and four provided intermediate palliative care. The meta‐analysis excluded Hughes 1992 (data were requested from authors with no answer) and Rabow 2004 (data could not be retrieved due to authors' retirement); however, the number of deaths in the latter study was small (15/90) and the authors reported no differences in place of death (P value = 0.40).
In addition, two large‐scale yet non‐randomised studies, Ward's ITS (Ward 1987) in the UK and Greer's CBA (Greer 1986), examined the effect of home palliative care on death at home. Ward's six‐year data on 31,890 cancer deaths showed that local home death rates reduced after the introduction of six home palliative care services (from 29.4% in the three years prior to 28.7% in the three years after); however, differences between services were noted – home death proportions declined in three districts with services attached to inpatient hospices (from 31.2% to 28.1%) and increased in three districts served by home care only services (from 25.9% to 29.8%). The nested CBA analysis of 957 deaths that took place in each of the services revealed that in those attached to inpatient hospices, 29% of patients died at home, compared with 65% in the home care only services. A report of findings from Greer 1986 on 1754 cancer patients also stated "marked differences" in the proportion dying at home in community‐based sites and hospital‐based intervention sites (both providing home hospice care) and conventional care (62%, 27% and 13%, respectively). Neither of these two studies reported on the statistical significance of the differences observed.
Death in institutions
Pooled data from six trials (four RCTs, three of high quality, and two CCTs with 1179 patients) showed that patients under home palliative care had lower odds of dying in hospital than those receiving usual care; however, the 95% CI increased and statistical significance was lost when the two CCTs were excluded (Analysis 1.3), and in the sensitivity analysis with only high quality RCTs (Analysis 1.4). The direction of the effect was consistent across all trials but ORs varied widely (from 0.02 to 0.99). Statistical significance was reached in three of the six trials: Jordhøy 2000 and Brumley 2007 (both RCTs of high quality), and Ahlner‐Elmqvist 2008 (CCT).
1.3. Analysis.

Comparison 1: Home palliative care versus usual care, Outcome 3: Death in hospital
1.4. Analysis.

Comparison 1: Home palliative care versus usual care, Outcome 4: death in hospital with only high quality RCTs
Pooled data from five trials (four RCTs, three of high quality, and one CCT with 899 patients) showed that although home palliative care patients had lower odds of dying in a nursing home than those under usual care, the difference did not reach statistical significance (OR 0.64, 95% CI 0.40 to 1.03; Z = 1.83, P value = 0.07; Chi2 = 2.77, df = 4, P value = 0.60; I2 = 0%;Analysis 1.5). Excluding Axelsson 1998 and analysing only the high quality RCTs (Analysis 1.6) had minor impact on the OR and 95% CI. The effect reached statistical significance only in Jordhøy 2000 but the direction of the effect was consistent across all RCTs, regardless of statistical significance.
1.5. Analysis.

Comparison 1: Home palliative care versus usual care, Outcome 5: Death in nursing home
1.6. Analysis.

Comparison 1: Home palliative care versus usual care, Outcome 6: death in nursing home with only high quality RCTs
Pooled data from five trials (four RCTs, three of high quality, and one CCT with 1123 patients) showed that although patients under home palliative care were more likely to die in an inpatient hospice/palliative care unit than those receiving usual care, the difference was not statistically significant (OR 1.46, 95% CI 0.51 to 4.19; Z = 0.71, P value = 0.48; Chi2 = 25.82, df = 4, P value < 0.0001; I2 = 85%;Analysis 1.7). Exclusion of the CCT and analysing only high quality RCTs (Analysis 1.8) increased the OR but also the 95% CI. The effect was statistically significant only in Jordhøy 2000, and in a direction opposite to the other three RCTs. This is explained by the fact that 63% of participants in the intervention group died at the hospital palliative care unit (where the intervention service was based), as opposed to none of the controls. The other three RCTs found decreased odds of inpatient hospice death in the intervention group, with ORs varying from 0.70 to 0.82, but none reached statistical significance.
1.7. Analysis.

Comparison 1: Home palliative care versus usual care, Outcome 7: Death in inpatient hospice/palliative care unit
1.8. Analysis.

Comparison 1: Home palliative care versus usual care, Outcome 8: death in inpatient hospice/palliative care unit with only high quality RCTs
Time the patient spent at home
There was conflicting evidence about the effect of home palliative care compared with usual care on the time the patient spent at home (four trials and one CBA, Table 15). In Jordhøy 2000, intervention and control groups spent a mean of 65% and 63% of time at home, respectively, for the entire follow‐up (P value = 0.6; follow‐up of two years with median survival of 99 days for the intervention group and 127 days for controls). Although there was a marginally significant difference in the mean percentage of time spent at home in the last month of life (48% and 41%, respectively; P value = 0.06), this was lost (P value = 0.15) when adjusted for other predictive factors (gender and living with spouse). Twenty‐eight (13%) intervention patients and 11 (6%) controls had no inpatient‐days in institutions in the last month of life (P value = 0.06, adjusted for sex as the only predictive factor). Intervention and control groups in Grande 1999 also did not differ in the proportion of patients who spent time at home during their last two weeks of life (based on retrospective accounts from their primary care team this was 82% and 77%, respectively; P value = 0.46).
13. Time the patient spent at home: home palliative care versus usual care.
| Study | Analysis | Follow‐up | Significance and direction | Details |
|
Jordhøy 2000 Norway (high quality) |
Forwards from enrolment | Entire follow‐up (up to 2 years with mean survival 99 days for intervention patients and 127 days for controls) |
n.s. P value = 0.6 |
M percentage time at home Intervention: 65% Control: 63% |
| Backwards from death | Last month |
Percentage of time at home marginally significant difference favours intervention P value = 0.06 n.s. adjusted for other predictive factors (gender and living with spouse) P value = 0.15 Number of inpatient‐days marginally significant difference favours intervention adjusted for sex as only predictive factor P value = 0.06 |
M percentage time at home Intervention: 48% Control: 41% Percentage of patients with no inpatient‐days Intervention: 28/219 (13%) Control: 11/176 (6%) |
|
|
Grande 1999 UK |
Backwards from death | Last 2 weeks (based on primary care team report 6 weeks after death) |
n.s. Chi2 0.557 P value = 0.455 |
Percentage of patients who spent time at home Intervention: 82% Control: 77% |
|
Buckingham 1978 US |
Not stated | Not stated | Authors stated difference favouring intervention but statistical significance was not stated | "It is estimated that nonhospice patients spent 50 percent more time in either an acute care hospital or some other form of institutional setting than hospice patients" (Buckingham 1978) |
|
Axelsson 1998 Sweden |
Forwards from enrolment | Entire follow‐up (median 70 days for intervention patients and 55 days for controls) | Favours intervention P value < 0.05 |
Median percentage of time spent at home Intervention (n = 41): 86% (range 0% to 100%) Control (n = 15): 72% (range 0% to 100%) |
| Backwards from death | Last 2 months | n.s. |
Median number of days spent at home Intervention (n = 41): 44 days (range 0 to 60) Control (n = 15): 39 days (range 15 to 60) |
|
|
Greer 1986 (CBA) |
Backwards from death | Not stated (based on caregiver report 90‐120 days after death) |
Favours community‐based intervention "HC PCPs were significantly more likely than HB and CC PCPs to report that the patient had been able to remain at home as long as he/she wanted" (Greer 1986) |
Patient able to remain at home as long as she/he wanted (adjusted estimatesa) Community‐based intervention: 82% (SE 0.04) Hospital‐based intervention: 69% (SE 0.05) Control (conventional care): 56% (SE 0.09) |
CC: conventional care (control); HB: hospital‐based (hospital‐based intervention); HC: home care (community‐based intervention); M: mean; n.s.: non‐significant; PCP: primary care person; SE: standard error. aOutcomes adjusted for sample differences; standard errors based on a logistic regression equation.
In contrast, data from two CCTs and one CBA suggested intervention patients spent more time at home than controls. In Axelsson 1998, the median percentage of time spent at home for the entire follow‐up (median 70 days for intervention patients and 55 days for controls) was 86% for intervention patients and 72% for controls (P value = 0.05); the authors also reported that the median number of days spent at home in the last two months of life was higher for the intervention than for the control group (44 and 39 days, respectively), although statistical significance was not reached. In Buckingham 1978, controls spent 50% more time in acute care hospital and other form of institutional setting than intervention patients (statistical significance not stated). Greer 1986 adjusted for sample differences and reported that bereaved caregivers in the community‐based intervention were significantly more likely to say that the patient had been able to remain at home as long as she/he wanted (82% vs. 69% in the hospital‐based intervention and 56% in conventional care).
Caregiver view on place of death
The evidence was inconclusive about the effect of home palliative care compared to usual care on caregivers' views on place of death (one RCT and one CBA, Table 16). Grande 1999 found that only four caregivers rated place of death as "definitely" or "probably inappropriate"; the numbers were too small to analyse. Greer 1986 reported that caregivers of patients who received the community‐based intervention were more satisfied with where the patient died than those in conventional care (91% in community‐based intervention vs. 88% in hospital‐based intervention vs. 74% in conventional care; statistical significance not stated).
14. Caregiver view on place of death: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Grande 1999 UK |
Item on perceived appropriateness of place of death score: definitely yes, probably yes, probably not, definitely not; caregiver report 6 weeks after death |
NA | NA | Not tested | "Only four caregivers rated place of death as 'definitely' or ‘probably inappropriate'. One of these represented a home death, three an inpatient death. Numbers were therefore too small in the 'inappropriate' category to analyze perceived appropriateness of place of death" (Grande 2004, Grande 1999) |
|
Greer 1986 (CBA) |
Item on satisfaction with place of death score: yes/no; caregiver report 90‐100 days after death |
NA | NA | Authors stated there were differences but significance not stated "PCPs in both types of hospices were satisfied with where the patients died; however, both hospice PCP groups were more satisfied with where the patient died than were CC PCPs" (Greer 1986) |
Adjusted estimatesa Community‐based intervention: 91% (SE 0.04) Hospital‐based intervention: 88% (SE 0.06) Control (conventional care): 74% (SE 0.02) |
CC: conventional care (control); NA: not applicable; PCP: primary care person; SE: standard error. aOutcomes adjusted for sample differences; standard errors based on a logistic regression equation.
Symptom burden
There was strong evidence that home palliative care is more effective than usual care on relieving the symptom burden for patients (three RCTs, two of high quality, and one CBA, 2107 patients, Table 2). Three studies (one of high quality) found statistically significant positive effects; in addition, Bakitas 2009 (high quality) reported a marginally significant effect in the same direction. Effect sizes were small (ranging from a difference in mean scores of 0.08 in a 0 to 7 scale to a difference of 2.1 in a 0 to 20 scale), but the findings from two of the RCTs (one of high quality) indicated an inversion of trajectory, with symptom burden reducing in the intervention group while it increased in the control group. All studies used different measures, analysed and reported in different ways, which precluded meta‐analysis.
Higginson 2009 (high quality) reported a one‐point decrease in mean scores of symptom burden (measured using the Palliative care Outcome Scale ‐ MS Symptom subscale; five symptoms; 0 to 20 scale, 20 = worst) from baseline to 12 weeks for 25 intervention patients (baseline mean 3.8) while for 21 controls symptom burden increased 1.1 (baseline mean 2.7). The difference between groups was statistically significant at 12 weeks (P value = 0.04) and observed already at six weeks, although it did not reach statistical significance by then (P value = 0.31). McCorkle 1989 reported different trajectories in symptom distress from 6 to 18 weeks after enrolment (Symptom Distress Scale; 13 symptoms; 13 to 65 scale, 65 = worst) in the intervention group and two controls: home care and usual outpatient care (P value = 0.03). Through repeated measures analysis adjusted for baseline scores, the authors found that while symptom distress decreased from week 6 to 12 by 1.87 points for intervention patients (adjusted mean 26.10 at six weeks) and by 0.17 points for home cancer care patients (adjusted mean 24.88 at six weeks), it increased for those under usual outpatient care by 2.47 points (adjusted mean 24.32 at six weeks). From week 12 to 18, all three groups experienced an increase of symptom distress, particularly those under home care (with an increase in adjusted means of 1.43, as opposed to 1.19 for intervention patients and 0.09 for those under usual outpatient care).
Intervention patients in Greer 1986 were likely to experience fewer symptoms than those in conventional care at one week to death (composite symptom severity scale modified from Melzack‐McGill Questionnaire; seven symptoms; 0 to 7 scale, 7 = worst). Greer reported that statistically significant differences persisted regardless of the level of symptoms at intake and that there was no statistically significant difference between community‐based and hospital‐based intervention groups (adjusted mean scores of 3.05 and 2.78, respectively; 3.38 for patients under conventional care), although at three weeks before death the first group experienced more symptoms than the second (adjusted means of 2.89 and 2.46, respectively; 2.97 for patients under conventional care).
The marginally significant effect favouring the intervention in Bakitas 2009 (mean treatment effect 27.8, standard error (SE) = 15; P value = 0.06; Edmonton Symptom Assessment Scale; nine symptoms; 0 to 900 scale, 900 = worst) was detected in the 13 months following enrolment through repeated measures analysis. Bakitas reported that this difference did not reach statistical significance when the data were analysed backwards from death (i.e. anchoring assessment time points to the date when the patient died; P value = 0.24). Symptom intensity increased for both groups in the last three assessments prior to death (each separated by three months).
Physical symptoms
There was conflicting evidence about the effect of home palliative care compared with usual care on patients' experience of pain, breathlessness and sleep disturbance (Table 3; Table 17; Table 18); other than these three symptoms, there was moderate evidence showing no statistically significant effect on nausea/vomiting (three RCTs, Table 19), constipation (two RCTs, Table 20) and diarrhoea (two RCTs, Table 21). There was also moderate evidence provided by Jordhøy 2000 of no statistically significant effect on fatigue and appetite loss (Table 22; Table 23). No study found statistically significant effects on these five symptoms.
15. Breathlessness: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Jordhøy 2000 Norway (high quality) |
EORTC QLQ‐C30 dyspnoea item score: from 0 to 100, higher scores equal greater dyspnoea; patient report |
Forwards from enrolment |
1 month | n.s.a SAUC intervention 2.8 vs. SAUC control 1.9 P value = 0.95 |
Intervention (n = 153): M 32 Control (n = 116): M 39 |
| 2 months | Intervention (n = 108): M 30 Control (n = 93): M 37 |
||||
| 4 months | Intervention (n = 71): M 38 Control (n = 65): M 37 |
||||
| 6 months | Differences and statistical significance not stated | Intervention (n = 56): M 40 Control (n = 52): M 42 |
|||
|
Rabow 2004 US (high quality) |
University of California San Diego Shortness of Breath Questionnaire measure with 2 subscales: 1) degree to which dyspnoea interference with daily activities (21 items; range 9 to 105) and 2) degree to which dyspnoea limits daily life (3 items; range 0 to 18); higher scores equal greater interference/limitation; patient report |
Forwards from enrolment |
6 months |
Interference with daily activities group main effect: favours intervention F = 7.06 P value = 0.01 group by time interaction: n.s. F = 1.67 P value = 0.21 Limitations to daily life group main effect: marginally significant difference favours intervention F = 3.64 P value = 0.07 group by time interaction: favours intervention F = 6.83 P value = 0.01 Presence of breathlessness favours intervention Controlling for the presence of breathlessness at baseline, the odds of reporting any breathlessness at 12 months were higher for controls than for intervention patients (OR 6.07; 95% CI 1.04 to 35.56) |
Adjusted estimatesb Interference with daily activities Intervention (n = 50): M 32.6 Control (n = 40): M 40.3 Limitations to daily life Intervention (n = 50): M 5.8 Control (n = 40): M 6.5 |
| 12 months | Adjusted estimatesb Interference with daily activities Intervention (n = 50): M 25.4 Control (n = 40): M 32.6 Limitations to daily life Intervention (n = 50): M 3.6 Control (n = 40): M 7.1 |
||||
|
Grande 1999 UK |
Cartwright/Addington Hall surveys breathlessness item 4‐point item, range not stated; higher scores equal greater breathlessness; caregiver report 6 weeks after death |
Backwards from death |
Last 2 weeks |
n.s. P value ≥ 0.05 |
Intervention (n = 107): M 2.43 (SD 1.17) Control (n = 18): M 2.17 (SD 1.15) Although analysis used Mann–Whitney U‐tests, authors reported Ms and SDs for clarity |
CI: confidence interval; EORTC QLQ‐C30: European Organisation for Research and Treatment of Cancer Quality of Life questionnaire; M: mean; n.s.: non‐significant; OR: odds ratio; SAUC: standardised area under the curve; SD: standard deviation. aThe authors calculated mean changes from baseline at one to four months after enrolment by dividing the area under the curve scores by time; differences between groups were tested by bootstrap estimation to fit regression models allowing for clustering and predictive factors. bMeans adjusted for baseline scores.
16. Sleep disturbance: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Jordhøy 2000 Norway (high quality) |
EORTC QLQ‐C30 sleep disturbances item score: from 0 to 100, higher scores equal greater sleep disturbances; patient report |
Forwards from enrolment |
1 month | n.s.a SAUC intervention ‐4.7 vs. SAUC control ‐2.2 P value = 0.56 |
Intervention (n = 153): M 32 Control (n = 116): M 34 |
| 2 months | Intervention (n = 108): M 33 Control (n = 93): M 33 |
||||
| 4 months | Intervention (n = 71): M 32 Control (n = 65): M 28 |
||||
| 6 months | Differences and statistical significance not stated | Intervention (n = 56): M 28 Control (n = 52): M 32 |
|||
|
Rabow 2004 US (high quality) |
Medical Outcomes Study 6 sleep items measure of sleep quality and duration in preceding 4 weeks; scores: sleep quality (from 6 to 24); higher scores equal better sleep; sleep duration (0‐24 hours); patient report |
Forwards from enrolment |
6 months |
Sleep quality group main effect: favours intervention F = 4.05 P value = 0.05 group by time interaction: n.s. F = 0.14 P value = 0.71 Sleep duration group main effect: n.s. F = 2.43 P value = 0.13 group by time interaction: n.s. F = 1.98 P value = 0.17 |
Adjusted estimatesb Sleep quality Intervention (n = 50): M 11.9 Control (n = 40): M 10.0 Sleep duration Intervention (n = 50): M 6.0 Control (n = 40): M 6.3 |
| 12 months | Adjusted estimatesb Sleep quality Intervention (n = 50): M 12.5 Control (n = 40): M 11.0 Sleep duration Intervention (n = 50): M 5.8 Control (n = 40): M 6.6 |
EORTC QLQ‐C30: European Organisation for Research and Treatment of Cancer Quality of Life questionnaire; M: mean; n.s.: non‐significant; SAUC: standardised area under the curve. aThe authors calculated mean changes from baseline at one to four months after enrolment by dividing the area under the curve scores by time; differences between groups were tested by bootstrap estimation to fit regression models allowing for clustering and predictive factors. bMeans adjusted for baseline scores.
17. Nausea/vomiting: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Jordhøy 2000 Norway (high quality) |
EORTC QLQ‐C30 2‐item nausea/vomiting scale score: from 0 to 100, higher scores equal greater nausea/vomiting; patient report |
Forwards from enrolment |
1 month | n.s.a SAUC intervention ‐0.7 vs. SAUC control 2.1 P value = 0.27 |
Intervention (n = 153): M 15 Control (n = 116): M 21 |
| 2 months | Intervention (n = 108): M 17 Control (n = 93): M 20 |
||||
| 4 months | Intervention (n = 71): M 14 Control (n = 65): M 14 |
||||
| 6 months | Differences and statistical significance not stated | Intervention (n = 56): M 21 Control (n = 52): M 15 |
|||
|
Grande 1999 UK |
Cartwright/Addington Hall surveys nausea/vomiting item 4‐point item, range not stated; higher scores equal greater nausea/vomiting; caregiver report 6 weeks after death |
Backwards from death |
Last 2 weeks |
n.s. P value ≥ 0.05 |
Intervention (n = 105): M 1.91 (SD 0.90) Control (n = 21): M 2.33 (SD 1.06) Although analysis used Mann–Whitney U‐tests, authors reported Ms and SDs for clarity |
|
McWhinney 1994 Canada |
Melzack nausea questionnaire score: range and interpretation not stated; patient/caregiver report through diary |
Forwards from enrolment |
1 month | n.s. | "There were no clinically or statistically significant differences between the experimental and control groups on any of the measures at one month" (McWhinney 1994); no data provided to support this statement High attrition (53/146) mainly due to death; 2 month data not analysed due to further attrition |
EORTC QLQ‐C30: European Organisation for Research and Treatment of Cancer Quality of Life questionnaire; M: mean; n.s.: non‐significant; SAUC: standardised area under the curve; SD: standard deviation. aThe authors calculated mean changes from baseline at one to four months after enrolment by dividing the area under the curve scores by time; differences between groups were tested by bootstrap estimation to fit regression models allowing for clustering and predictive factors.
18. Constipation: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Jordhøy 2000 Norway (high quality) |
EORTC QLQ‐C30 constipation item score: from 0 to 100, higher scores equal greater constipation; patient report |
Forwards from enrolment |
1 month | n.s.a SAUC intervention ‐6.7 vs. SAUC control ‐0.5 P value = 0.12 |
Intervention (n = 153): M 33 Control (n = 116): M 37 |
| 2 months | Intervention (n = 108): M 31 Control (n = 93): M 32 |
||||
| 4 months | Intervention (n = 71): M 34 Control (n = 65): M 30 |
||||
| 6 months | Differences and significance not stated | Intervention (n = 56): M 37 Control (n = 52): M 31 |
|||
|
Grande 1999 UK |
Cartwright/Addington Hall surveys constipation item 4‐point item, range not stated; higher scores equal greater constipation; caregiver report 6 weeks after death |
Backwards from death |
last 2 weeks |
n.s. P value ≥ 0.05 |
Intervention (n = 102): M 2.24 (SD 1.10) Control (n = 21): M 2.62 (SD 0.97) Although analysis used Mann–Whitney U‐tests, authors reported Ms and SDs for clarity |
EORTC QLQ‐C30: European Organisation for Research and Treatment of Cancer Quality of Life questionnaire; M: mean; n.s.: non‐significant; SAUC: standardised area under the curve; SD: standard deviation. aThe authors calculated mean changes from baseline at one to four months after enrolment by dividing the area under the curve scores by time; differences between groups were tested by bootstrap estimation to fit regression models allowing for clustering and predictive factors.
19. Diarrhoea: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Jordhøy 2000 Norway (high quality) |
EORTC QLQ‐C30 diarrhoea item score: from 0 to 100, higher scores equal greater diarrhoea; patient report |
Forwards from enrolment |
1 month | n.s.a SAUC intervention ‐0.4 vs. SAUC control ‐2.0 P value = 0.68 |
Intervention (n = 153): M 25 Control (n = 116): M 23 |
| 2 months | Intervention (n = 108): M 20 Control (n = 93): M 23 |
||||
| 4 months | Intervention (n = 71): M 19 Control (n = 65): M 21 |
||||
| 6 months | Differences and statistical significance not stated | Intervention (n = 56): M 19 Control (n = 52): M 22 |
|||
|
Grande 1999 UK |
Cartwright/Addington Hall surveys diarrhoea item 4‐point item, range not stated; higher scores equal greater diarrhoea; caregiver report 6 weeks after death |
Backwards from death |
last 2 weeks | n.s. P value ≥ 0.05 |
Intervention (n = 98): M 1.51 (SD 0.89) Control (n = 20): M 1.55 (SD 0.94) Although analysis used Mann–Whitney U‐tests, authors reported Ms and SDs for clarity |
EORTC QLQ‐C30: European Organisation for Research and Treatment of Cancer Quality of Life questionnaire; M: mean; n.s.: non‐significant; SAUC: standardised area under the curve; SD: standard deviation. aThe authors calculated mean changes from baseline at one to four months after enrolment by dividing the area under the curve scores by time; differences between groups were tested by bootstrap estimation to fit regression models allowing for clustering and predictive factors.
20. Fatigue: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Jordhøy 2000 Norway (high quality) |
EORTC QLQ‐C30 3‐item fatigue scale score: from 0 to 100, higher scores equal greater fatigue; patient report |
Forwards from enrolment |
1 month | n.s.a SAUC intervention 4.6 vs. SAUC control 1.2 P value = 0.23 |
Intervention (n = 153): M 60 Control (n = 116): M 57 |
| 2 months | Intervention (n = 108): M 56 Control (n = 93): M 55 |
||||
| 4 months | Intervention (n = 71): M 54 Control (n = 65): M 53 |
||||
| 6 months | differences and statistical significance not stated | Intervention (n = 56): M 52 Control (n = 52): M 53 |
EORTC QLQ‐C30: European Organisation for Research and Treatment of Cancer Quality of Life questionnaire; M: mean; n.s.: non‐significant; SAUC: standardised area under the curve. aThe authors calculated mean changes from baseline at one to four months after enrolment by dividing the area under the curve scores by time; differences between groups were tested by bootstrap estimation to fit regression models allowing for clustering and predictive factors.
21. Appetite loss: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Jordhøy 2000 Norway (high quality) |
EORTC QLQ‐C30 appetite loss item score: from 0 to 100, higher scores equal greater appetite loss; patient report |
Forwards from enrolment |
1 month | n.s.a SAUC intervention 1.7 vs. SAUC control 3.4 P value = 0.70 |
Intervention (n = 153): M 37 Control (n = 116): M 44 |
| 2 months | Intervention (n = 108): M 34 Control (n = 93): M 36 |
||||
| 4 months | Intervention (n = 71): M 32 Control (n = 65): M 32 |
||||
| 6 months | Differences and statistical significance not stated | Intervention (n = 56): M 33 Control (n = 52): M 33 |
EORTC QLQ‐C30: European Organisation for Research and Treatment of Cancer Quality of Life questionnaire; M: mean; n.s.: non‐significant; SAUC: standardised area under the curve. aThe authors calculated mean changes from baseline at one to four months after enrolment by dividing the area under the curve scores by time; differences between groups were tested by bootstrap estimation to fit regression models allowing for clustering and predictive factors.
Pain
Eight trials (four of high quality) and one CBA (totaling seven studies with 2735 patients) examined the effectiveness of home palliative care compared to usual care in terms of pain relief. Two RCTs (both conducted in the UK, one of high quality) and Greer 1986 found statistically significant positive effects; in addition, a marginally significant positive effect was found among 83 patients in McKegney 1981 in the last month before death (P value = 0.06); pain scores plateaued for intervention patients while for controls pain continued to rise towards death. The remaining six trials found no statistically significant differences. High variability in outcome measures (only the McGill‐Melzack Pain Questionnaire was used more than once) and in the time points of comparisons (ranging from one week following enrolment to the week of death) precluded meta‐analysis (Table 3).
Higginson 2009 reported a 0.46 point mean decrease in pain scores (Palliative care Outcome Scale pain item; 0 to 4 scale, 4 = worst) from baseline to 12 weeks for 26 intervention patients, while for 24 controls pain increased by a 0.30 point. The difference was statistically significant at 12 weeks (P value = 0.03) and observed already at six weeks although it did not reach statistical significance by then. Grande 1999 also found that the mean pain scores in the last two weeks of life for 107 intervention patients were 0.48 points lower than those of 21 controls, according to their bereaved caregivers (mean 2.52 and 3.00, respectively; P value < 0.05; measured using a four‐point item from Cartwright and Addington‐Hall surveys, higher scores = worst). Greer 1986 found that according to caregiver reports there was a significantly lower proportion of patients with persistent pain at three weeks before death (P value < 0.01) and one week before death (P value < 0.001) among those receiving the hospital‐based intervention as opposed to those under the community‐based intervention and those with conventional care (3%, 7% and 14%, respectively at three weeks to death, and 4%, 13% and 22%, respectively at one week to death). This difference did not reach statistical significance when the data were analysed forwards from enrolment and there were no statistically significant differences in composite pain index scores and in the proportion of patients who were pain‐free. Patient self reports did not confirm the findings, but the authors noted that at one week to death 80% of patients could not report.
Breathlessness
Both Jordhøy 2000 (high quality study) and Grande 1999 found no statistically significant differences between home palliative care and usual care on patients' breathlessness (one to six months after enrolment and in the last two weeks of life, respectively). In contrast, Rabow 2004 (high quality study) found that after controlling for the presence of breathlessness at baseline, the odds of reporting any breathlessness at 12 months were higher for 40 controls than for 50 intervention patients under the "comprehensive care team" (OR 6.07, 95% CI 1.04 to 35.56); however, very wide CIs were noted. Intervention patients also reported less breathlessness interfering with daily activities than controls (adjusted mean 32.6 and 40.3, respectively at six months; adjusted mean 25.4 and 40.6, respectively at 12 months; group main effect with P value = 0.01; measured using the University of California‐San Diego Shortness of Breath Questionnaire; 0 to 105 scale, 105 = worst) and there was a group by time interaction, with decreased limitation of activity due to breathlessness for intervention patients and increased limitation over time for controls (P value = 0.01, Table 17).
Sleep disturbance
No statistically significant differences were found in Jordhøy 2000 through longitudinal analysis of sleep disturbances for intervention and control patients one to four months after enrolment (Table 18). In contrast, intervention patients in Rabow 2004 experienced better sleep quality than controls six to 12 months after enrolment (P value = 0.05), after controlling for baseline differences. Rabow reported a difference in mean scores of 1.9 points at six months and of 1.5 points at 12 months (Sleep Quality Score from Medical Outcomes Study; 6 to 24 scale, 6 = worst), with no statistically significant group by time interaction (scores improved slightly from six to 12 months for both groups) or statistically significant differences in sleep quantity.
Advance care planning
There was moderate evidence showing no statistically significant effect of home palliative care compared to usual care on the completion of a medical power of attorney (two RCTs, Table 24). These two trials found, however, effects on other forms of advance care planning. Analysis of 42 patients who had no funeral arrangements in place at the onset of Rabow 2004's study (high quality study) showed that 8/23 in the intervention group (35%) as opposed to 1/19 in the control group (5%) had those arrangements in place 12 months after (P value = 0.03). Also, intervention patients in Aiken 2006 were four times more likely than controls to have completed a living will or advance directive three months after enrolment (OR 4.47, 95% CI 1.10 to 18.18); no statistically significant difference was detected three months after. Differences on completion of plans for disposition of possessions (Rabow 2004) and discussion of legal documents with family/friends and the physician responsible for the care (Aiken 2006) were not statistically significant.
22. Advance care planning: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Rabow 2004 US (high quality) |
3 items on completion of durable power of attorney for health care, funeral plans and plans for disposition of possessions score: yes/no; patient report |
Forwards from enrolment | 12 months |
Durable power of attorney n.s. P value = 0.12 Funeral arrangements favours intervention P value = 0.03 Plans for disposition of possessions n.s. P value = 0.11 |
Subanalysis of patients without advance care planning arrangements at baseline Completion of durable power of attorney Intervention: 12/22 (55%) Control: 5/18 (28%) Completion of funeral arrangements Intervention: 8/23 (35%) Control: 1/19 (5%) Completion of plans for disposition of possessions Intervention: 16/20 (80%) Control: 5/11 (46%) |
|
Aiken 2006 US |
4 items on completion of living will or advance directives, documents such as medical power of attorney and discussion of legal documents with family and friends and physician responsible for care score: yes/no; patient report |
Forwards from enrolment | 3 months |
Living will/advance directive favours intervention adjusted proportions P value < 0.05; h 0.67 OR 4.47 (95% CI 1.10 to 18.18) Items on completion of documents such as medical power of attorney, and discussion of legal documents n.s. |
n = 111 Completion of living will/advance directive Intervention: 71% Control: 65% Completion of documents such as medical power of attorney Intervention: 66% Control: 69% Discussion of legal documents with physician responsible for care Intervention: 48% Control: 59% Discussion of legal documents with family and friends Intervention: 78% Control: 90% |
| 6 months |
All items n.s. P value ≥ 0.05 |
n = 90 Completion of living will/advance directive Intervention: 70% Control: 73% Completion of documents such as medical power of attorney Intervention: 68% Control: 76% Discussion of legal documents with physician responsible for care Intervention: 34% Control: 62% Discussion of legal documents with family and friends Intervention: 82% Control: 94% |
CI: confidence interval; n.s.: non‐significant; OR: odds ratio.
Other patient outcomes
Aiken 2006 provided limited evidence of a positive effect on four aspects related to patient self management of illness: increased receipt of education about community resources at three months from enrolment, increased receipt of sufficient information to handle an illness emergency and about who to talk to about a medical problem at six months, and decreased experience of events for which the patient was unprepared for at both three and six months (Table 25). No statistically significances were found, though, in the receipt of sufficient information to manage the illness at home and about how family and friends could assist. Grande 1999 provided limited evidence of no statistical significant effect on patients' unmet needs in the last two weeks before death (Table 26). In addition, there was conflicting evidence about the effect of home palliative care compared with usual care on patients' quality of life (six RCTs and one CBA, Table 5), general health (three RCTs, Table 27) and survival (nine trials and one CBA, Table 28). The evidence was inconclusive regarding the effect on physical function (six RCTs and one CBA, Table 4); psychological, social and spiritual well‐being (10 trials and one CBA, Table 29; three trials and one CBA, Table 30; one RCT and one CBA, Table 31, respectively); nutrition (one RCT, Table 32) and cognitive status (one RCT and one CBA, Table 33).
23. Self management of illness: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Aiken 2006 US |
2 items on self management of illness, 3 items on knowledge about resources and 1 item on experience of event for which patient was unprepared in last 4 weeks scores: ranged from 1 to 4 except for experience (yes/no); higher scores equal better self management and knowledge of resources; patient report |
Forwards from enrolment | 3 months |
Receipt of sufficient information to manage illness at home n.s. Receipt of sufficient information to handle illness emergency n.s. Receipt of education about community resources favours intervention F = 5.80; P value < 0.05; g 0.45 Receipt of information about how family and friends can assist n.s. Receipt of information about who to talk to about a medical problem n.s. Experience of event for which patient was unprepared for in the last 4 weeks favours intervention logistic regression with group by diagnosis interaction OR 6.07 (95% CI 1.01 to 36.53) |
M adjusted for baseline Receipt of sufficient information to manage illness at home Intervention: 3.73 Control: 3.55 Receipt of sufficient information to handle illness emergency Intervention: 3.72 Control: 3.52 Receipt of education about community resources Intervention: 2.57 Control: 2.02 Receipt of information about how family and friends can assist Intervention: 2.24 Control: 1.98 Receipt of information about who to talk to about a medical problem Intervention: 2.72 Control: 2.45 Experience of event for which patient was unprepared for in the last 4 weeks Intervention: 32% Control: 40% COPD patients: intervention patients were much less likely to have had such an experience they felt unprepared for than were controls; OR 0.23 (95% CI 0.05 to 0.97), 32% and 58% in intervention and control, respectively |
| 6 months |
Receipt of sufficient information to manage illness at home n.s. Receipt of sufficient information to handle illness emergency favours intervention F = 8.19; P value < 0.05; g 0.59 Receipt of education about community resources n.s. Receipt of information about how family and friends can assist n.s. Receipt of information about who to talk to about a medical problem favours intervention F = 5.12; P value < 0.05; g 0.50 Experience of event for which patient was unprepared for in the last 4 weeks favours control logistic regression with group main effect OR 3.22 (95% CI 1.10 to 9.44) |
M adjusted for baseline Receipt of sufficient information to manage illness at home Intervention: 3.75 Control: 3.70 Receipt of sufficient information to handle illness emergency Intervention: 3.90 Control: 3.51 Receipt of education about community resources Intervention: 2.14 Control: 1.74 Receipt of information about how family and friends can assist Intervention: 1.97 Control: 1.94 Receipt of information about who to talk to about a medical problem Intervention: 2.63 Control: 2.19 Experience of event for which patient was unprepared for in the last 4 weeks Intervention: 42% Control: 21% |
CI: confidence interval; COPD: chronic obstructive pulmonary disease; M: mean; n.s.: non‐significant; OR: odds ratio.
24. Patient unmet needs: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Grande 1999 UK |
Cartwright/Addington Hall surveys items on need for more support in 4 areas: night nursing, medical care, personal care and psychological support 3‐point items, range not stated; higher scores equal greater unmet needs; caregiver report 6 weeks after death |
Backwards from death |
last 2 weeks |
n.s. P value ≥ 0.05 |
Night nursing Intervention (n = 108): M 1.42 (SD 0.73) Control (n = 18): M 1.39 (SD 0.70) Medical care Intervention (n = 108): M 1.15 (SD 0.45) Control (n = 21): M 1.29 (SD 0.64) Personal care Intervention (n = 107): M 1.19 (SD 0.52) Control (n = 20): M 1.20 (SD 0.52) Psychological support Intervention (n = 104): M 1.25 (SD 0.54) Control (n = 18): M 1.28 (SD 0.67) Although analysis used Mann–Whitney U‐tests, authors reported Ms and SDs for clarity |
M: mean; n.s.: non‐significant; SD: standard deviation.
25. General health: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Jordhøy 2000 Norway (high quality) |
EORTC‐QLQ‐C30 global health scale (2 items) transformed score: from 0 to 100, higher scores equal better global health; patient report |
Forwards from enrolment |
1 month | n.s.a SAUC intervention ‐1.1 vs. SAUC control 1.1 P value = 0.48 |
Intervention (n = 153): M 49 Control (n = 116): M 48 |
| 2 months | Intervention (n = 108): M 51 Control (n = 93): M 49 |
||||
| 4 months | Intervention (n = 71): M 50 Control (n = 65): M 53 |
||||
| 6 months | Differences and statistical significance not stated | Intervention (n = 56): M 55 Control (n = 52): M 52 |
|||
|
McCorkle 1989 US |
General Health Rating index (22 items) score: from 22 to 110, lower scores equal better health perceptions; patient report |
Forwards from enrolment |
6 weeks | Favours intervention F = 4.06 P value = 0.05 b |
Adjusted estimates Intervention: M 61.11 Control1 (home cancer care): M 61.26 Control2 (usual outpatient care): M 59.05 |
| 12 weeks | Adjusted estimates Intervention: M 59.53 Control1 (home cancer care): M 60.14 Control2 (usual outpatient care): M 59.66 |
||||
| 18 weeks | Adjusted estimates Intervention: M 57.04 Control1 (home cancer care): M 57.84 Control2 (usual outpatient care): M 60.64 |
||||
|
Aiken 2006 US |
SF‐36 general health subscale transformed score: from 0 to 100, higher scores equal better general health, negative slope equal reduction; patient report |
F from enrolment |
9 months | Favours intervention for both COPD and CHFc slope: z 2.16, P value < 0.05 intercept at 9 months: z 2.52; P value < 0.05; g 0.47 |
Growth modelling analysis (separate for COPD and CHF patients) Slope declined for controls while health remained stable for intervention patients, and the intervention intercept exceeded that of controls at 9 months COPD slope: 0.54 intervention vs. ‐1.67 control CHF slope: 0.16 intervention vs. ‐0.17 control |
CHF: congestive heart failure; COPD: chronic obstructive pulmonary disease; EORTC QLQ‐C30: European Organisation for Research and Treatment of Cancer Quality of Life questionnaire; M: mean; n.s.: non‐significant; SAUC: standardised area under the curve. aThe authors calculated mean changes from baseline at one to four months after enrolment by dividing the area under the curve scores by time; differences between groups were tested by bootstrap estimation to fit regression models allowing for clustering and predictive factors. bThe authors used repeated measures analysis and analysis of variance; analysis included 78 patients who completed the three follow‐up interviews (i.e. up to 18 weeks after enrolment); adjusted means were used due to baseline differences despite randomisation; graphs showed that patients receiving the intervention and the control1 (i.e. those receiving cancer home care) experienced better health perceptions over time while control2 patients (i.e. those receiving usual outpatient care) experienced a decrease over time. cThe authors used growth modelling analysis, calculated slopes of "average" linear trajectory within a group, averaged across slopes of individual linear trajectories of individual within the group and compared intercepts at each time point and slopes for COPD and CHF patients separately.
26. Survival: home palliative care versus usual care.
| Study | Measure | Analysis | Significance and direction | Details |
|
Bakitas 2009 US (high quality) |
Months from enrolment to death or study end | Kaplan‐Meier and log rank test (post‐hoc exploratory analysis, patients alive at end of study censored on study last day) | n.s. P value = 0.14 |
Intervention (n = 161): median 14 months (95% CI 10.6 to 18.4 months) Control (n = 161): median 8.5 months (95% CI 7.0 to 11.1 months) |
|
Brumley 2007 US (high quality) |
Days in study | t‐test, Kaplan‐Meier and log rank test (patients alive at end of study censored on study's last day) | n.s. with log rank test 2.98; P = 0.08 (favours control with t‐test P = 0.03) | Intervention: "average" 196 days (± 164) Controls: "average" 242 days (± 200) |
|
Jordhøy 2000 Norway (high quality) |
'Survival' days | Kaplan‐Meier and log‐rank test adjusted for 3 cancer diagnostic groups (not clear how patients alive at end of study were analysed) | n.s. P value = 0.1 (adjusted for diagnosis) |
Intervention: median 99 days (95% CI 79 to 119 days) Control: median 127 days (95% CI 88 to 166 days) |
|
McKegney 1981 US (high quality) |
'Length of survival' | Not stated | No differences stated but significance not stated | "It should be briefly noted that the intensive and non‐intensive patients did not differ in terms of length of survival" (McKegney 1981) |
|
Grande 1999 UK |
Days from referral to death |
MannWhitney U tests | n.s. z 1.666; P value = 0.096 Favours control vs. those who received intervention service (113/186 of intervention) z 3.005; P value = 0.003 |
Intervention (n = 186): median 11 days (quartiles from 4 to 34 days) Control (n = 43): median 11 days (quartiles from 3 to 26 days) Subanalysis of intervention patients Patients who received service (n = 113): median 16 days (quartiles from 5 to 42.5 days) Patients who did not receive service (n = 73): median 8 days (quartiles from 3 to 18 days) |
|
Zimmer 1985 US |
'Survival profiles' | log‐likelihood ratio Chi2 using Aitken and Clayton method assuming exponential survival and adjusting for terminal/ non‐terminal status (unclear how patients alive at end of study were analysed) | n.s. log‐likelihood ratio Chi2 1.4; P value > 0.10 |
No descriptive data provided |
|
Hughes 1992 US |
'Survival days' | Not stated | n.s. (authors stated "n.s.") |
Intervention: M 76.2 days (SD 67.1) Control: M 83.1 days (SD 68.1) Decedents only Intervention: M 48.0 days (SD 43.3) Control: M 54.5 days (SD 47.7) |
|
Ahlner‐Elmqvist 2008 Sweden |
Days after enrolment | Kaplan‐Meier and log‐rank test (patients alive at end of study were excluded) | Favours control log rank 12.04; P value = 0.0005 |
Intervention: median 94 days Control: median 160 days |
|
Axelsson 1998 Sweden |
Months from diagnosis to death |
Wilcoxon signed rank (comparisons included 3 groups: intervention and control groups and a third historical group) | Favours intervention P value = 0.043 |
Intervention: median 23 months (M 35 ± 42) Control: median 6 months (M 16 ± 19) |
|
Greer 1986 (CBA) |
'Survival' | Not stated | n.s. |
"We tested the differences in patient survival in the study groups, controlling for disease, performance status, selected symptoms, as well as the amount of time patients were able to be followed, and found no statistically significant differences" (Greer 1986); no data provided to support this statement |
CI: confidence interval; M: mean; n.s.: non‐significant; SD: standard deviation.
27. Psychological well‐being: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Bakitas 2009 US (high quality) |
Center for Epidemiological Studies Depression (CES‐D) Scale (20 items) score: from 0 to 60; higher scores equal greater depressive symptoms (cut‐off score of ≥ 16 for depression case); patient report |
Forwards from enrolment | 1 month | Favours interventiona M treatment effect (intervention‐control) ‐1.8 (SE 0.81) P value = 0.02 |
Intervention (n = 102): LSM 10.66 (95% CI 9.26 to 12.06) Control (n = 98): LSM 11.87 (95% CI 10.43 to 13.30) |
| 4 months | Intervention (n = 72): LSM 10.67 (95% CI 9.03 to 12.32) Control (n = 76): LSM 13.55 (95% CI 11.71 to 15.38) |
||||
| 7 months | Intervention (n = 60): LSM 10.75 (95% CI 8.98 to 12.53) Control (n = 54): LSM 13.55 (95% CI 11.71 to 15.38) |
||||
| 10 months | Intervention (n = 47): LSM 12.65 (95% CI 10.67 to 14.62) Control (n = 44): LSM 11.68 (95% CI 9.38 to 13.98) |
||||
| 13 months | Intervention (n = 26): LSM 12.89 (95% CI 10.32 to 15.45) Control (n = 31): LSM 11.68 (95% CI 9.38 to 13.98) |
||||
| Backwards from death | third last assessment | Favours interventiona M treatment effect (intervention‐control) ‐2.7 (SE 1.23) P value = 0.03 |
Intervention (n = 49): LSM 10.71 (95% CI 8.43 to 12.98) Control (n = 49): LSM 12.44 (95% CI 10.13 to 14.74) |
||
| second last assessment | Intervention (n = 79): LSM 11.86 (95% CI 9.90 to 13.81) Control (n = 72): LSM 13.24 (95% CI 11.19 to 15.28) |
||||
| last assessment | Intervention (n = 78): LSM 12.88 (95% CI 10.92 to 19.52) Control (n = 73): LSM 17.49 (95% CI 15.46 to 19.52) |
||||
|
Rabow 2004 US (high quality) |
1) Profile of Mood States (POMS) Anxiety Scale (6 items) score: from 0 to 24; higher scores equal greater anxiety; patient report 2) Center for Epidemiological Studies Depression (CES‐D) Scale (20 items) score: from 0 to 60; higher scores equal greater depressive symptoms (cut‐off score of ≥ 16 for depression case); patient report |
Forwards from enrolment | 6 months |
Anxiety ANCOVA group main effect: n.s. F = 0.17 P value = 0.68 ANCOVA group by time interaction: favours intervention F = 4.09 P value = 0.05 Depression ANCOVA group main effect: n.s. F = 1.19 P value = 0.28 ANCOVA group by time interaction: n.s. F = 0.71 P value = 0.40 |
Adjusted estimates Anxiety Intervention (n = 50): M 6.8 Control (n = 40): M 5.5 Depression Intervention (n = 50): M 16.5 Control (n = 40): M 17.5 |
| 12 months | Adjusted estimates Anxiety Intervention (n = 50): M 5.3 Control (n = 40): M 5.9 Depression Intervention (n = 50): M 12.4 Control (n = 40): M 15.3 |
||||
|
Higginson 2009 UK (high quality) |
MS Impact Scale (MSIS) Psychological subscale score: range not stated; higher scores equal greater psychological impact; patient report |
Forwards from enrolment | 6 weeks | n.s.b ES ‐0.6 F = 2.11 P value = 0.16 |
M change from baseline Intervention (n = 19): M 1.3 (SD 5.9; 95% CI ‐1.6 to 4.1) Control (n = 16): M ‐2.3 (SD 5.1; 95% CI ‐5.0 to 0.5) |
| 12 weeks |
n.s.b ES ‐0.1 F = 0.01 P value = 0.91 |
M change from baseline Intervention (n = 21): M 0.1 (SD 6.5; 95% CI ‐2.9 to 3.1) Control (n = 17): M ‐0.8 (SD 6.1; 95% CI ‐3.9 to 2.4) |
|||
|
Jordhøy 2000 Norway (high quality) |
1) EORCT‐QLQ‐C30 emotional functioning scale (4 items) transformed score: from 0 to 100; higher scores equal better functioning; patient report 2) Impact of Event Scale (IES, 15 items) 2 subscales: intrusion and avoidance scores: intrusion subscale (from 0 to 35), avoidance subscale (from 0 to 40); higher scores equal more distress; patient report |
Forwards from enrolment | 1 month |
n.s.c Emotional functioning SAUC intervention ‐1.5 vs. SAUC control 1.7 P value = 0.94 IES intrusion SAUC intervention ‐1.5 vs. SAUC control ‐2.6 P value = 0.29 IES avoidance SAUC intervention ‐1.5 vs. SAUC control ‐2.0 P value = 0.88 |
Emotional functioning Intervention: M 73 vs. control: M 73 IES intrusion Intervention: M 11 vs. control: M 12 IES avoidance Intervention: M 13 vs. control: M 14 |
| 2 months |
Emotional functioning Intervention: M 71 vs. control: M 72 IES intrusion Intervention: M 12 vs. control: M 11 IES avoidance Intervention: M 14 vs. control: M 14 |
||||
| 4 months |
Emotional functioning Intervention: M 71 vs. control: M 75 IES intrusion Intervention: M 9 vs. control: M 9 IES avoidance Intervention: M 13 vs. control: M 13 |
||||
| 6 months | Differences and statistical significance not stated |
Emotional functioning Intervention: M 71 vs. control: M 76 IES intrusion Intervention: M 11 vs. control: M 9 IES avoidance Intervention: M 12 vs. control: M 14 |
|||
|
McKegney 1981 US (high quality) |
Cornell Medical Index (CMI) (51 items) score: range not stated; higher scores equal greater emotional disturbance; patient report |
Backwards from death | 180 to 150 days | Authors stated there were no differences but statistical significance was not stated |
"It should be briefly noted that the intensive and non‐intensive patients did not differ in terms of length of survival, nor did these two groups differ in several other quality of life outcomes such as (...) optimism" (McKegney 1981); no data provided to support this statement |
| 150 to 120 days | |||||
| 120 to 90 days | |||||
| 90 to 60 days | |||||
| 60 to 30 days | |||||
| 30 to 0 days | |||||
|
Grande 1999 UK |
2 items on anxiety and depression from Cartwright/Addington Hall studies 4‐point items, range not stated; higher scores equal greater distress; caregiver report 6 weeks after death |
Backwards from death | last 2 weeks | n.s. P value ≥ 0.05 n.s. P value ≥ 0.05 |
Anxiety Intervention (n = 104): M 2.58 (SD 1.07) Control (n = 21): M 2.62 (SD 1.02) Depression Intervention (n = 103): M 2.23 (SD 1.05) Control (n = 19): M 2.16 (SD 1.07) Although analysis used Mann–Whitney U‐tests, authors reported Ms and SDs for clarity |
|
McCorkle 1989 US |
1) Profile of Mood States (POMS, 65 items) score: range not stated; higher scores equal greater distress; patient report 2) Inventory of Current Concerns (ICC, 72 items) score: range not stated; higher scores equal greater concerns; patient report |
Forwards from enrolment | 6 weeks | n.s. |
"The three groups did not differ significantly with respect to (...) ICC, and POMS scores" (McCorkle 1989); no data provided to support this statement |
| 12 weeks | |||||
| 18 weeks | |||||
|
Aiken 2006 US |
SF‐36 2 subscales: mental health and role‐emotional transformed score: from 0 to 100; lower scores equal lower functioning; negative slope equal reduction; patient report |
Forwards from enrolment | 3 months | n.s. | Growth modelling analysis (separate for COPD and CHF patients) Mental health COPD slope: intervention: ‐0.37 vs. control: ‐0.10 CHF slope: intervention: ‐0.69 vs. control: ‐1.77 Role‐emotional COPD slope: intervention: 1.77 vs. control: 3.08 CHF slope: intervention: 0.00 vs. control: ‐0.24 |
| 6 months | |||||
| 9 months | |||||
|
Hughes 1992 US |
Philadelphia Geriatric Center Morale Scale (short‐version) score: range not stated; higher scores equal lower morale; patient report |
Forwards from enrolment | 1 month | n.s. Beta 0.02 t 0.35 P value = 0.73 |
ANCOVA (age, education, race, marital status, retirement due to health, prior private sector hospital use, living arrangement, and baseline care satisfaction scores; none of these factors were predictive of outcomes); descriptive data not provided |
| 6 months | n.s. t < 1 |
Intervention (n = 17): M 1.54 Control (n = 14): M 1.57 Data were analysed using t‐tests because the sample did not support regression models |
|||
|
Buckingham 1978 US |
1) Symptom checklist‐90 (SCL‐90) measure psychological problems; scoring not stated; patient report 2) Zuckerman and Lubin adjective checklist to measure depression; scoring not stated; patient report |
Not stated | Not stated | Authors stated there were differences but statistical significance was not stated |
"Hospice patients (...) exhibited (...) lower levels of anxiety and depression than nonhospice patients" (Buckingham 1978); no data provided to support this statement |
|
Greer 1986 (CBA) |
Emotional quality of life score from modified Spitzer quality of life index score: from 0 to 14; higher scores equal better emotional quality of life; caregiver report |
Backwards from death | 3 weeks | Authors stated there were no differences but statistical significance was not stated "Other measures, such as (...) Emotional Quality of Life (...) were comparable in the three systems of care" (Greer 1986) |
Adjusted estimatesd Community‐based intervention: M 6.61 (SE 0.31) Hospital‐based intervention: M 7.02 (SE 0.34) Control (conventional care): M 6.47 (SE 0.55) |
| 1 week | Adjusted estimatesd Community‐based intervention: M 5.63 (SE 0.24) Hospital‐based intervention: M 6.12 (SE 0.25) Control (conventional care): M 6.00 (SE 0.43) |
ANCOVA: analysis of covariance; CBA: controlled before and after study; CHF: congestive health failure; CI: confidence interval; COPD: chronic obstructive pulmonary disease; EORTC QLQ‐C30: European Organisation for Research and Treatment of Cancer Quality of Life questionnaire; ES: estimated effect size; IES: Impact of Event Scale; LSM: estimated least mean square; M: mean; n.s.: not significant; SAUC: standardised area under the curve; SD: standard deviation; SE: standard error. aResults from repeated measures analysis of covariance (mixed‐effects model applied to longitudinal data using random‐subject effects to account for correlation between repeated outcome measurements on same individual). bResults from F‐tests of non‐imputed data; authors stated that imputed data gave similar results. cThe authors calculated mean changes from baseline at one to four months after enrolment by dividing the area under the curve scores by time; differences between groups were tested by bootstrap estimation to fit regression models allowing for clustering and predictive factors. dEstimates adjusted for sample differences; standard errors based on the linear regression equation.
28. Social well‐being: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Jordhøy 2000 Norway (high quality) |
EORTC QLQ‐C30 social functioning scale (2 items) score: from 0 to 100, higher scores equal better functioning; patient report |
Forwards from enrolment |
1 month | n.s.a SAUC intervention ‐8.8 vs. SAUC control ‐0.4 P value = 0.10 |
Intervention (n = 153): M 52 Control (n = 116): M 54 |
| 2 months | Intervention (n = 108): M 53 Control (n = 93): M 52 |
||||
| 4 months | Intervention (n = 71): M 61 Control (n = 65): M 58 |
||||
| 6 months | Differences and statistical significance not stated | Intervention (n = 56): M 67 Control (n = 52): M 58 |
|||
|
Aiken 2006 US |
SF‐36 social functioning subscale transformed score: from 0 to 100; higher scores equal better social functioning; negative slope equal reduction; patient report |
Forwards from enrolment |
3 months | n.s.b |
Growth modelling analysis (separate for COPD and CHF patients) COPD slope: intervention: 1.09 vs. control: 3.72 CHF slope: intervention: ‐0.80 vs. control: ‐2.15 |
| 6 months | |||||
| 9 months | |||||
|
Buckingham 1978 US |
Social Adjustment Self Report Questionnaire score: range and interpretation not stated; patient report |
Not stated | Not clear | Authors stated differences favouring the intervention but statistical significance was not stated | "Hospice patients and primary care persons exhibited higher levels of social adjustment than non‐hospice patients and primary care persons" (Buckingham 1978); no data provided to support this statement |
|
Greer 1986 (CBA) |
Social quality of life measure modified from Spitzer quality of life index score: from 1 to 7; higher scores equal better social quality of life; caregiver report |
Backwards from death |
3 weeks | Differences and statistical significance not stated | Adjusted estimatesc Community‐based intervention: 5.09 (SE 0.11) Hospital‐based intervention: 5.26 (SE 0.14) Control: 5.54 (SE 0.20) |
| 1 week | Favours controls "Although ratings were very high in all three samples, PCP judgment of patients' social quality of life at the measure closest to death was statistically higher among CC patients" (Greer 1986) |
Adjusted estimatesc Community‐based intervention: M 5.03 (SE 0.09) Hospital‐based intervention: M 5.09 (SE 0.09) Control: M 5.62 (SE 0.16) |
|||
|
Item on hours of social visiting from people other than the caregiver score: from 0 to 4 (categorised); higher scores equal greater number of hours of social visiting; caregiver report |
Backwards from death |
3 weeks | Favours intervention "Three weeks prior to death, HC patients received significantly more hours of social visiting than CC patients from persons other than their PCP: the difference between HC and HB patients was not statistically significant" (Greer 1986) |
Adjusted estimatesc Community‐based intervention: M 2.56 (SE 0.09) Hospital‐based intervention: M 2.40 (SE 0.11) Control: M 2.16 (SE 0.18) |
|
| 1 week | Differences and statistical significance not stated | Adjusted estimatesc Community‐based intervention: M 2.61 (SE 0.07) Hospital‐based intervention: M 2.55 (SE 0.09) Control: M 2.41 (SE 0.14) |
|||
|
Item on amount of chatting with household members score: from 0 to 7 (categorised); higher scores equal more chatting with household members; caregiver report |
backwards from death |
3 weeks | Differences and statistical significance not stated | Adjusted estimatesc Community‐based intervention: M 2.87 (SE 0.07) Hospital‐based intervention: M 2.87 (SE 0.09) Control: M 2.86 (SE 0.17) |
|
| 1 week | Authors stated difference favouring the community‐based vs. hospital‐based intervention but statistical significance not stated and no comparison was made with control group "The level of chatting with household members was similar in all three patient samples except at the measure closest to death, when HB patients were more active than HC patients" (Greer 1986) |
Adjusted estimatesc Community‐based intervention: M 2.53 (SE 0.05) Hospital‐based intervention: M 2.71 (SE 0.07) Control: M 2.57 (SE 0.12) |
CBA: controlled before and after study; CC: control (conventional care); CHF: congestive heart failure; COPD: chronic obstructive pulmonary disease; HB: hospital‐based (hospital‐based intervention); HC: home care (community‐based intervention); M: mean; n.s. non‐significant; PCP: primary care person; SAUC: standardised area under the curve; SE: standard error. aThe authors calculated mean changes from baseline at one to four months after enrolment by dividing the area under the curve scores by time; differences between groups were tested by bootstrap estimation to fit regression models allowing for clustering and predictive factors. bThe authors used growth modelling analysis, calculated slopes of "average" linear trajectory within a group, averaged across slopes of individual linear trajectories of individual within the group and compared intercepts at each time point and slopes for COPD and CHF patients separately. cEstimates adjusted for sample differences; standard errors based on the linear regression equation for continuous variables and on logistic regression equation for dichotomous variables.
29. Spiritual well‐being: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Rabow 2004 US (high quality) |
Spiritual well‐being scale (20 items, 2 subscales) score: overall (from 20 to 120), religious subscale (from 10 to 60); existential subscale (from 10 to 60), higher score equal greater spiritual well‐being; patient report |
Forwards from enrolment |
6 months |
Overall spirituality ANCOVA group main effect: favours intervention between groups F = 8.21 P value = 0.007 ANCOVA group by time interaction: favours intervention F = 4.24 P value = 0.05 Religious subscale ANCOVA group main effect: favours intervention F = 14.01 P value = 0.001 ANCOVA group by time interaction: n.s. F = 3.12 P value = 0.09 Existential subscale ANCOVA group main effect: n.s. F = 2.08 P value = 0.16 ANCOVA group by time interaction: n.s. F = 0.47 P value = 0.49 |
Adjusted estimates Overall spirituality Intervention (n = 50): M 98.0 Control (n = 40): M 91.2 Religious subscale Intervention (n = 50): M 52.2 Control (n = 40): M 46.4 Existential subscale Intervention (n = 50): M 44.4 Control (n = 40): M 42.5 |
| 12 months | Adjusted estimates Overall spirituality Intervention (n = 50): M 105.5 Control (n = 40): M 92.4 Religious subscale Intervention (n = 50): M 55.6 Control (n = 40): M 46.4 Existential subscale Intervention (n = 50): M 48.2 Control (n = 40): M 44.9 |
||||
|
Greer 1986 (CBA) |
2 items of Quality of Death measure (study‐specific measure): patient felt at peace/ happy and felt at peace with God score: yes/no; caregiver report from 90 to 100 days after death |
Backwards from death |
3 days | No tests performed (descriptive data only) | Subsample analysis (n = 880) Felt at peace 84% intervention vs. 79% control Felt at peace with God 90% intervention vs. 93% control |
ANCOVA: analysis of covariance; CBA: controlled before and after study; M: mean; n.s.: non‐significant.
30. Nutrition: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
McKegney 1981 US (high quality) |
Nutritional status measure in research database assessed by structured interview score: range and interpretation not stated; patient report |
Backwards from death | 180 to 150 days | Authors stated there were no differences but statistical significance was not stated |
"It should be briefly noted that the intensive and non‐intensive patients did not differ in (...) nutrition" (McKegney 1981); no data provided to support this statement |
| 150 to 120 days | |||||
| 120 to 90 days | |||||
| 90 to 60 days | |||||
| 60 to 30 days | |||||
| 30 to 0 days |
31. Cognitive status: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Hughes 1992 US |
Short Portable Mental Status Questionnaire (10 items) score: from 0 to 10; scale recoded so that higher score equal better cognitive functioning; patient report |
Forwards from enrolment | 1 month | n.s. Beta 0.12 t 0.32 P value = 0.75 |
ANCOVA (age, education, race, marital status, retirement due to health, prior private sector hospital use, living arrangement, and baseline care satisfaction scores; none of these factors were predictive of outcomes); descriptive data not provided |
| 6 months | n.s. t < 1 |
Intervention (n = 17): M 8.33 Control (n = 14): M 8.86 Data were analysed using t‐tests because the sample did not support regression models |
|||
|
Greer 1986 (CBA) |
Item on patient awareness score: from 1 to 4; higher scores equal greater awareness; caregiver report |
Backwards from death | 3 weeks | Authors stated there were no differences but statistical significance was not stated "patient awareness was comparable in the three groups" (Greer 1986) |
Adjusted estimatesa Community‐based intervention: M 1.88 (SE 0.05) Hospital‐based intervention: M 1.84 (SE 0.06) Control: M 1.84 (SE 0.08) |
| 1 week | Adjusted estimatesa Community‐based intervention: M 2.28 (SE 0.05) Hospital‐based intervention: M 2.18 (SE 0.05) Control: M 2.23 (SE 0.09) |
ANCOVA: analysis of covariance; CBA: controlled before and after study; M: mean; n.s.: non‐significant; SE: standard error. aEstimates adjusted for sample differences; standard errors based on the linear regression equation.
Caregiver pre‐bereavement outcomes
Longitudinal analysis of pooled data from Jordhøy 2000 (high quality study) and Ahlner‐Elmqvist 2008 (517 caregivers) for SF‐36 subscales measuring physical function, general health and pain provided moderate evidence of no statistically significant differences between home palliative care and usual care in trajectories for these outcomes during the last 44 months before the patient died except for a significant positive effect on physical functioning (Table 34). Findings showed that the intervention group scored five points higher than controls at the first time point, that is 44 to 13 months before the patient died (transformed scores 0 to 100, 100 = better functioning; b = 5.47; P value < 0.05). There was conflicting evidence about the effect of home palliative care on caregiver psychological well‐being (five trials and one CBA, Table 35) and inconclusive evidence about the effect on caregiver social well‐being (three trials, Table 36).
32. Caregiver pre‐bereavement general health, pain and physical dimensions of quality of life: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Jordhøy 2000 Norway (high quality) and Ahlner‐Elmqvist 2008 Sweden |
SF‐36 5 subscales: physical functioning (10 items), role limitation due to physical problems (4 items), bodily pain (2 items), vitality (4 items), and general health perception (5 items). transformed scores: from 0 to 100; higher scores equal better health; caregiver report |
Backwards from death | 44 to 13 months |
Physical functioning subscale Group main effect: favours intervention b 5.47 SE 2.55; P value < 0.05 Group by time interaction: marginally significant difference favouring intervention P value < 0.10 and ≥ 0.05 Other 4 subscales Group main effect and group by time interaction n.s. P value ≥ 0.10 |
Pooled analysis of data from the 2 studies (n = 517); longitudinal analysis of trajectories included pre‐ and post‐bereavement measurements Findings showed that intervention group scored 5 points higher than controls at the first time point (b 5.47); all other observed differences were not statistically significant b values and SEs for each time interval (in group by time analysis) and graphs with descriptive data on trajectories in scores over time provided in Ringdal 2004 (Jordhøy 2000 and Ahlner‐Elmqvist 2008) |
| 12 to 6 months | |||||
| 5 to 0 months | |||||
| Forwards from death | 1 to 2 months | ||||
| 3 to 5 months | |||||
| 6 to 12 months | |||||
| 13 to 17 months |
b: metric regression coefficient; n.s.: non‐significant; SE: standard error.
33. Caregiver pre‐bereavement psychological well‐being: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Jordhøy 2000 Norway (high quality) and Ahlner‐Elmqvist 2008 Sweden |
SF‐36 2 subscales: role limitation due to emotional problems (3 items) and mental health (5 items) transformed scores: from 0 to 100; higher scores equal better health; caregiver report |
Backwards from death | 44 to 13 months | Increased difference over time in scores for the 2 subscales favours intervention Role limitation due to emotional problems group effect: n.s. b ‐6.67 SE 5.36 P value ≥ 0.10 Group by time interaction: favours intervention P value < 0.05 Mental health Group effect: n.s. b ‐5.09 SE 3.02 P value ≥ 0.10 Group by time interaction: favours intervention P value < 0.05 |
Pooled analysis of data from the 2 studies (n = 517); longitudinal analysis of trajectories included pre‐ and post‐bereavement measurements Findings showed a strong decline in scores before the death of the patient, and rising scores thereafter, especially for the intervention group b values and SEs for each time interval (in group by time analysis) and graphs with descriptive data on trajectories in scores over time provided in Ringdal 2004 (Jordhøy 2000 and Ahlner‐Elmqvist 2008) |
| 12 to 6 months | |||||
| 5 to 0 months | |||||
| Forwards from death | 1 to 2 months | ||||
| 3 to 5 months | |||||
| 6 to 12 months | |||||
| 13 to 17 months | |||||
|
McWhinney 1994 US |
Center for Epidemiological Studies Depression (CES‐D) scale score: range and interpretation not stated; caregiver report |
Forwards from enrolment | 1 month | n.s. | "There were no clinically or statistically significant differences between the experimental and control groups on any of the measures at one month" (McWhinney 1994); no data provided High attrition (53/146) mainly due to death; 2 month data not analysed due to further attrition |
|
Hughes 1992 US |
Philadelphia Geriatric Center Morale Scale (short‐version) score: range not stated; higher scores equal lower morale; caregiver report |
Forwards from enrolment | 1 month | n.s. Beta ‐0.02 t 0.57 P value = 0.57 |
ANCOVA (adjusted for age, race, education, relationship to patient and morale baseline score) Intervention (n = 32): M 1.75 (SD 21) Control (n = 27): M 1.58 (SD 0.32) |
| 6 months | Favours control Beta ‐0.12 t ‐2.30 P value = 0.03 |
ANCOVA (adjusted for age, race, education, relationship to patient and morale baseline score); controlling for survival days did not alter findings Intervention (n = 32): M 1.67 (SD 25) Control (n = 27): M 1.62 (SD 0.34) |
|||
|
Buckingham 1978 US |
1) Symptom checklist‐90 (SCL‐90) measure of psychological problems; score range and interpretation not stated; caregiver report 2) Zuckerman and Lubin adjective checklist for the measurement of depression scores: range and interpretation not stated; caregiver report |
Not stated | Not stated | Authors stated differences favouring intervention but statistical significance not stated | "Hospice patients and their primary care persons exhibited (…) lower levels of anxiety and depression than non‐hospice patients and their primary care persons" (Buckingham 1978); no data provided to support this statement |
|
Greer 1986 (CBA) |
1) Profile of Mood States (POMS) score: from 0 to 5; lower scores equal greater psychological distress; caregiver report 2) use of medication for anxiety or depression (yes/no; caregiver report) 3) report of increased drinking (yes/no; caregiver report) |
Not stated | Not stated |
POMS n.s. Use of medication for anxiety or depression n.s. Increased drinking n.s. "There were no significant differences among the three PCP groups on a modified mood state scale measuring anxiety and depression. Similarly, no significant differences among the groups were observed in use of medications for anxiety or depression, and there was no reported increased use of alcohol" (Greer 1986) |
Adjusted estimatesa POMS Community‐based intervention: M 2.96 (SE 0.06) Hospital‐based intervention: M 2.98 (SE 0.08) Control (conventional care): M 3.01 (SE 0.13) Use of medication for anxiety or depression Community‐based intervention: 11% (SE 0.02) Hospital‐based intervention: 10% (SE 0.02) Control (conventional care): 14% (SE 0.04) Increased drinking Community‐based intervention: 4% (SE 0.01) Hospital‐based intervention: 5% (SE 0.01) Control (conventional care): 6% (SE 0.02) |
ANCOVA: analysis of covariance; b: metric regression coefficient; CBA: controlled before and after study; M: mean; n.s.: non‐significant; PCP: primary care person; SD: standard deviation; SE: standard error. aEstimates adjusted for sample differences; standard errors based on the linear regression equation for continuous variables and on logistic regression equation for dichotomous variables.
34. Caregiver pre‐bereavement social well‐being: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Jordhøy 2000 Norway (high quality) and Ahlner‐Elmqvist 2008 Sweden |
SF‐36 social functioning subscale (2 items) transformed scores: from 0 to 100; higher scores equal better health; caregiver report |
Backwards from death | 44 to 13 months | Group main effect: n.s. b ‐4.43 SE 3.85 P value ≥ 0.10 Group by time interaction: n.s. P value ≥ 0.10 |
Pooled analysis of data from the 2 studies (n = 517); longitudinal analysis of trajectories included pre and post bereavement measurements b values and SEs for each time interval (in group by time analysis) and graphs with descriptive data on trajectories in scores over time provided in Ringdal 2004 (Jordhøy 2000; Ahlner‐Elmqvist 2008) |
| 12 to 6 months | |||||
| 5 to 0 months | |||||
| Forwards from death | 1 to 2 months | ||||
| 3 to 5 months | |||||
| 6 to 12 months | |||||
|
Buckingham 1978 US |
Social Adjustment Self Report Questionnaire score: range and interpretation not stated; caregiver report |
Not stated | Not stated | Authors stated differences favouring intervention but statistical significance was not stated | "Hospice patients and primary care persons exhibited higher levels of social adjustment than non‐hospice patients and primary care persons" (Buckingham 1978); no data provided to support this statement |
b: metric regression coefficient; n.s.: non‐significant; SE: standard error.
Caregiving‐related outcomes
There were conflicting findings about the effect of home palliative care compared with usual care on caregiver burden (two RCTs, both of high quality, and one CBA including 1888 caregivers, Table 6). Bakitas 2009 reported no group main effects or group by time interactions for all measures of caregiver burden one to 10 months after enrolment (objective burden, stress burden and demand burden measured by Montgomery Borgatta Caregiver Burden Scale; all P values > 0.05). However, Higginson 2009 found that caregiver burden reduced from baseline to the 12 weeks follow‐up by 2.88 points in the intervention group while it increased 1.58 points for controls (measured by 12‐item Zarit Burden Inventory; 0 to 48 scale; P value = 0.01). Mean change scores at six months showed a difference in the opposite direction but this was not statistically significant. In addition, Greer 1986 reported that caregiver burden in the last weeks of the patient's life was higher in the community‐based intervention; the difference was described by the authors as small but statistically significant. After adjusting for baseline differences, mean scores on a study‐specific measure of perceived caregiving burden (0 to 6 scale; 6 = worst) were 3.32 among those receiving the community‐based intervention, followed by 3.13 among those in conventional care and 2.91 in the hospital‐based intervention group.
Higginson 2009 provided moderate evidence of no statistically significant difference in the learning of new caregiving skills and in a positive appraisal of caregiving 6 and 12 weeks following enrolment for those in home palliative care compared to usual care (Table 37; Table 38). Grande 1999 provided limited evidence of no statistically significant differences in caregivers' unmet needs (for help looking after the patient, practical running of household, information, psychological support and transport) in the two weeks before death (Table 39).
35. Caregiver mastery: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Higginson 2009 UK (high quality) |
Item on learning new caregiving skills from modified Lawton positivity questionnaire "Have you learnt new skills while caring for your relative?" (Edmonds 2010, Higginson 2009); score: yes/no; caregiver report |
Forwards from enrolment | 6 weeks |
n.s. Cochran‐Mantel‐Haenszel test for trend Chi2 2.56; P value = 0.11 |
Intervention: 12/16 (75%; 95% CI 48% to 93%) Control: 12/17 (71%; 95% CI 44% to 90%) |
| 12 weeks | Intervention: 15/16 (94%; 95% CI 70% to 100%) Control: 7/15 (47%; 95% CI 21% to 73%) |
CI: confidence interval; n.s.: non‐significant.
36. Positive aspects of caregiving: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Higginson 2009 UK (high quality) |
Modified Lawton positivity questionnaire (4 items) score: range not stated; higher scores equal more positive views; caregiver report |
Forwards from enrolment | 6 weeks | n.s. ES 0.49 F = 0.50 P value = 0.49 |
M change from baseline Intervention (n = 9): M ‐0.3 (SD 1.7; 95% CI ‐1.7 to 1.0) Control (n = 15): M ‐0.1 (SD ‐0.1; 95% CI ‐1.1 to 1.0) |
| 12 weeks | n.s. ES ‐0.3 F = 0.10 P value = 0.75 |
M change from baseline Intervention (n = 8): M ‐0.3 (SD 1.0; 95% CI ‐1.1 to 0.6) Control (n = 12): M 0.3 (SD 2.0; 95% CI ‐1.0 to 1.5) |
CI: confidence interval; ES: effect size; M: mean; n.s.: non‐significant; SD: standard deviation.
37. Caregiver unmet needs: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Grande 1999 UK |
Cartwright/Addington Hall surveys items on need for more support on 4 areas: looking after patient, practical running of household, information, psychological support and transport 3‐point items, range not stated; higher scores equal greater unmet needs; caregiver report 6 weeks after death |
Backwards from death |
last 2 weeks |
n.s. P value ≥ 0.05 |
Looking after patient Intervention (n = 106): M 1.41 (SD 0.69) Control (n = 21): M 1.52 (SD 0.75) Practical running of household Intervention (n = 107): M 1.24 (SD 0.56) Control (n = 19): M 1.32 (SD 0.67) Information Intervention (n = 104): M 1.44 (SD 0.72) Control (n = 21): M 1.52 (SD 0.81) Psychological support Intervention (n = 103): M 1.36 (SD 0.65) Control (n = 19): M 1.37 (SD 0.76) Transport Intervention (n = 90): M 1.19 (SD 0.56) Control (n = 18): M 1.11 (SD 0.47) Although analysis used Mann–Whitney U‐tests, authors reported Ms and SDs for clarity |
M: mean; n.s.: non‐significant; SD: standard deviation
Caregiver post‐bereavement outcomes
There was strong evidence (three RCTs, two of high quality, and one CBA with 2113 caregivers, Table 7)showing no difference between caregivers who received home palliative care and those who received usual care in terms of the grief intensity they experienced from the moment the patient died to 13 months after. Longitudinal analysis of scores from a 13‐item scale developed from the 21‐item Texas Revised Inventory of Grief (TRIG100) 1 to 13 months into bereavement in Jordhøy 2000, independent t‐tests of mean scores for grief intensity at time of death and approximately four to six months after (Bakitas 2009; Grande 1999), and comparison of the prevalence of complicated grief cases (Bakitas 2009) found no statistically significant differences between intervention and control groups. Samples included 86 caregivers in Bakitas 2009, 183 in Jordhøy 2000 and 90 in Grande 1999. The findings show small differences between intervention and control groups that together with non‐significant test results rule out the existence of clinically significant differences: Bakitas 2009 found a group difference of 1.52 in mean scores approximately four to six months after the patient died (0 to 60 scale, measure not stated, mean in intervention 22.24, mean in control 20.72; P value = 0.56); the authors also reported a 1% difference in the prevalence of complicated grief (16% in intervention and 17% in control group; P value = 1.0). Jordhøy 2000 found group differences of less than two points in mean scores using TRIG100 (0 to 100 scale, 100 = worst) one to 13 months after the patient died (F = 0.348, P value = 0.790). Grande 1999 reported group differences of less than one point in mean scores in both TRIG scales six months after the patient died, also statistically non‐significant (Table 7). The statistical significance of differences between intervention and control groups was not reported in the CBA yet again clinically significant differences can be ruled out (Greer 1986): adjusted mean scores in the modified Grief Experience Inventory 90 to 120 days into bereavement (0 to 10 scale; 10 = worst) were 0.33 point higher in the conventional care group than in the hospital‐based intervention and 0.24 point lower than in the community‐based intervention (Table 7).
Longitudinal analysis of pooled data from Jordhøy 2000 and Ahlner‐Elmqvist 2008 for SF‐36 subscales measuring physical function, social functioning general health and pain provided moderate evidence of no statistically significant differences between home palliative care and usual care in trajectories for these outcomes in the 13 months after the patient died except for a positive effect on physical functioning. This latter finding conflicted with null results from Grande 1999's analysis of SF‐36 physical component summary scores measured six months after the patient died (Table 40). There was also conflicting evidence about the effect of home palliative care compared to usual care on caregiver post‐bereavement psychological well‐being (three RCTs, one CCT and one CBA, Table 41).
38. Caregiver post‐bereavement general health, pain, social and physical dimensions of quality of life: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up |
Significance and direction |
Details |
|
Jordhøy 2000 Norway (high quality) and Ahlner‐Elmqvist 2008 Sweden |
SF‐36 6 subscales: physical functioning (10 items), social functioning (2 items) role limitation due to physical problems (4 items), bodily pain (2 items), vitality (4 items), and general health perception (5 items) transformed scores: from 0 to 100; higher scores equal better health; caregiver report |
Backwards from death | 44 to 13 months |
Physical functioning subscale group main effect: favours intervention b 5.47 SE 2.55 P value < 0.05 group by time interaction: marginally significant difference favouring intervention P value < 0.10 and ≥ 0.05 Other 5 subscales group effect and group by time interaction n.s. P value ≥ 0.10 |
Pooled analysis of data from the 2 studies (n = 517); longitudinal analysis of trajectories included pre‐ and post‐bereavement measurements b values and SEs for each time interval (in group by time analysis) and graphs with descriptive data on trajectories in scores over time provided in Ringdal 2004 (Jordhøy 2000; Ahlner‐Elmqvist 2008) |
| 12 to 6 months | |||||
| 5 to 0 months | |||||
| Forwards from death | 1 to 2 months | ||||
| 3 to 5 months | |||||
| 6 to 12 months | |||||
| 13 to 17 months | |||||
|
Grande 1999 UK |
SF‐36 physical component summary scores score: range not stated; higher scores equal better outcome; caregiver report |
Forwards from death | 6 months | n.s. | Intervention (n = 73): M 45.5 (SD 13.4) Control (n = 16): M 43.6 (SD 13.8) Comparisons of scores of people who received and did not receive the intervention (27 people in intervention group did not receive the service) showed no differences |
b: metric regression coefficient; M: mean; n.s.: non‐significant; SD: standard deviation; SE: standard error.
39. Caregiver post‐bereavement psychological well‐being: home palliative care versus usual care.
| Study | Measure | Analysis | Time point | Significance and direction | Details |
|
Jordhøy 2000 Norway (high quality) and Ahlner‐Elmqvist 2008 Sweden |
SF‐36 2 subscales: role limitation due to emotional problems (3 items) and mental health (5 items) transformed scores: from 0 to 100; higher scores equal better health; caregiver report |
Backwards from death | 44 to 13 months | Increased difference over time in scores for the 2 subscales favours intervention Role limitation due to emotional problems group main effect: n.s. b ‐6.67 SE 5.36 P value ≥ 0.10 group by time interaction: favours intervention P value < 0.05 Mental health group main effect: n.s. b ‐5.09 SE 3.02 P value ≥ 0.10 group by time interaction: favours intervention P value < 0.05 |
Pooled analysis of data from the 2 studies (n = 517); longitudinal analysis of trajectories included pre‐ and post‐bereavement measurements Findings showed rising scores after the patient died, especially for the intervention group b values and SEs for each time interval (in group by time analysis) and graphs with descriptive data on trajectories in scores over time provided in Ringdal 2004 (Jordhøy 2000 and Ahlner‐Elmqvist 2008) |
| 12 to 6 months | |||||
| 5 to 0 months | |||||
| Forwards from death | 1 to 2 months | ||||
| 3 to 5 months | |||||
| 6 to 12 months | |||||
| 13 to 17 months | |||||
|
Grande 1999 UK |
SF‐36 mental component summary scores score: range not stated; higher scores equal better outcome; caregiver report |
Forwards from death | 6 months | n.s. | Intervention (n = 73): M 48.8 (SD 11.0) Control (n = 16): M 49.2 (SD 12.5) Comparisons of scores of people who received and did not receive the intervention (27 people in intervention group did not receive the service) showed no differences |
|
McCorkle 1989 US |
Brief Symptom Inventory global severity index and 10 subscales: somatisation, obsessive‐compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, psychoticism scores: items rated from 0 to 4; range of global severity index and subscales not stated; higher scores equal greater distress; caregiver report |
Forwards from death | 6 weeks |
Global severity index main group effect: n.s. F = 2.56 P value = 0.089 group by time interaction: n.s. F = 1.51 P value = 0.198 Subscales (results with P value < 0.05 below, all described in McCorkle 1998, McCorkle 1989) Depression main group effect: favours intervention F = 4.67 P value = 0.015 Paranoid ideation main group effect: favours intervention F = 3.66 P value = 0.034 group by time interaction: favours intervention F = 3.83 P value = 0.003 |
Post‐hoc t‐tests (results with P value < 0.05) Depression (intervention vs. control2): t 2.22; P value = 0.022 Psychoticism (intervention vs. control2): t 2.70; P value = 0.012 |
| 6 months |
Post‐hoc t‐tests (results with P value < 0.05) Hostility (intervention vs. control2): t 2.54; P value = 0.017 Paranoid ideation (intervention vs. control2): t 2.63; P value = 0.014 Psychoticism (intervention vs. control2): t 2.36; P value = 0.026 |
||||
| 13 months |
Post‐hoc t‐tests (results with P value < 0.05) Global severity index (intervention vs. control2): t 2.39; P value = 0.024 Hostility (intervention vs. control2): t 3.18; P value = 0.004 Paranoid ideation (intervention vs. control2): t 3.57; P value = 0.001 |
||||
| 25 months | Post‐hoc t‐tests all n.s. Descriptive data (Ms and SDs) for global severity index and 10 subscales for each time point provided in McCorkle 1998, McCorkle 1989 |
||||
|
Greer 1986 (CBA) |
1) Use of medication for anxiety/depression (yes/no; caregiver report) 2) Increased drinking (yes/no; caregiver report) |
Forwards from death | 90 to 120 days | Authors stated no differences but statistical significance not stated "no difference in (…) use of medications for depression, or increased alcohol use during the bereavement period" (Greer 1986) |
Adjusted estimatesa Use of medication for anxiety or depression Community‐based intervention: 16% (SE 0.02) Hospital‐based intervention: 12% (SE 0.02) Control (conventional care): 15% (SE 0.03) Increased drinking Community‐based intervention: 4% (SE 0.01) Hospital‐based intervention: 5% (SE 0.01) Control (conventional care): 6% (SE 0.02) |
b: metric regression coefficient; control2: usual outpatient care; n.s.: non‐significant; SD: standard deviation; SE: standard error. aEstimates adjusted for sample differences; standard errors based on the linear regression equation.
Satisfaction with care
Findings were conflicting about the effect of home palliative care compared with usual care on satisfaction with care (five RCTs, four of high quality, and one CBA including 2497 participants, Table 8). While three RCTs (one of high quality) found statistically significant positive effects, the other two (both of high quality; Bakitas 2009; Rabow 2004) reported no statistically significant differences. Two studies measured caregivers' views; three measured caregivers and patients' perspectives; Rabow 2004 (high quality) measured patients' views only. Three studies measured satisfaction with care prospectively; two measured retrospectively; Greer 1986 measured both ways. All studies used different measures.
Jordhøy 2000 reported that satisfaction with care was 8.60 points higher in the intervention group than among controls, measured with caregivers one month after death using the FAMCARE scale (0 to 100 transformed scores; P value = 0.008); the difference reduced to 7.68 points when adjusted for other predictive factors (relationship to patient, sex and age of caregiver, cancer type, sex of patient, time since inclusion in the study, place of death; P value = 0.02). Brumley 2007 reported that intervention patients were three times more likely to be very satisfied with care than controls at 30 days (OR 3.37, 95% CI 1.42 to 8.10; P value = 0.01) and 90 days (OR 3.37, 95% CI 0.65 to 4.96; P value = 0.03) after enrolling in the trial. The difference did not reach statistical significance at 60 days (OR 1.79, 95% CI 0.65 to 4.96; P value = 0.26). Hughes 1992 reported that after adjusting for other factors, satisfaction with care was higher for patients (Beta = 0.13; P value = 0.04) and caregivers (Beta = 0.18; P value < 0.01) in the intervention group at one month's follow‐up. This difference did not reach statistical significance at the six months' follow‐up although there was a marginally significant difference in patients' reports favouring the intervention (P value = 0.06). Greer 1986 found no differences in patients' reports (described as uniformly high across groups) but reported a "small but significantly higher level of satisfaction" among caregivers receiving the hospital‐based intervention compared to those in conventional care, measured both before and after death (90‐120 days after). The authors also reported that few caregivers expressed regret concerning the medical treatment the patient received (11%), with no statistically significant differences between groups.
Overall palliative care outcomes
There was conflicting evidence about the effect of home palliative care compared with usual care on overall palliative care outcomes for patients and their families (one RCT and one CBA, Table 42). Higginson 2009 found no statistically significant difference between intervention and control patients in changes from baseline in total scores from the Palliative care Outcome Scale (POS‐8) at six and 12 weeks after enrolment. In contrast, in a sub‐analysis of 880 patients in Greer 1986, scores from the Quality of Death measure (study‐based measure of 13 items, assessed with caregivers 90‐120 days after death, reporting to the last three days before death) were higher in the two intervention groups than in the control group (P value = 0.03), with differences gaining further significance when adjusted for three predictive factors: age, family income and extent of disease at diagnosis (P value < 0.001). Greer 1986 reported that differences between the two intervention groups (community‐based and hospital‐based home hospice care) were not significant.
40. Overall palliative care outcomes: home palliative care versus usual care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Higginson 2009 UK (high quality) |
8 items from Palliative care Outcome Scale (POS‐8) score: from 0 to 32; higher scores equal greater problems; negative change equal reduction; patient report |
Forwards from enrolment | 6 weeks | n.s. |
M change from baseline Intervention (n = 24): M ‐0.68 (95% CI ‐2.22 to 0.86) Control (n = 20): M ‐0.55 (95% CI ‐2.42 to 1.33) |
| 12 weeks | n.s. |
M change from baseline Intervention (n = 25): M ‐0.42 (95% CI ‐2.50 to 1.67) Control (n = 21): M ‐0.95 (95% CI ‐2.87 to 0.97) |
|||
|
Greer 1986 (CBA) |
Quality of Death measure (study‐specific measure with 13 items) score: items scored yes/no were weighted according to importance for patients to generate final score; higher scores equal better quality of death; caregiver report 90‐120 days after death |
Backwards from death | 3 days (measured retrospectively, 90‐120 days after death) | Favours intervention ANOVA P value < 0.03 ANCOVA F = 7.80 P value < 0.001 (adjusting for age, family income and extent of disease at diagnosis) Newman‐Keuls post‐test on the adjusted mean scores P value < 0.01 |
Subsample analysis (n = 880) Community‐based intervention: M 80.4 Hospital‐based intervention: M 81.5 Control (conventional care): M 72.5 "Adjusted mean scores were not significantly difference from the unadjusted scores" (Wallston 1988, Greer 1986) "Differences between the two types of hospice [i.e. the two intervention groups] were not significant" (Wallston 1988, Greer 1986) |
CI: confidence interval; M: mean; n.s.: non‐significant.
Home versus hospital palliative care
Gómez‐Batiste 2010 evaluated the clinical effectiveness of 105 palliative care teams (62 provided home palliative care) across all 19 autonomous regions in the country. The authors examined clinical outcomes for 265 patients and reported that all symptoms analysed (breakthrough background pain, anorexia, nausea/vomiting, constipation, insomnia, breathlessness at rest and with movement, anxiety and depression; measured using numeric rating scales) improved significantly from baseline to day seven and to day 14 after enrolment with no differences between the different types of palliative care teams.
Reinforced versus standard home palliative care
Patient outcomes
McMillan 2007 provided limited evidence showing that adding a caregiver support component to specialist home palliative care had a beneficial effect on patients' symptom burden during the month after enrolment (Table 43); however, no statistically significant differences were found in experience of pain, breathlessness, constipation and quality of life (Table 44; Table 45; Table 46; Table 47). There was also limited evidence showing no statistically significant effect on physical function eight weeks and five months after enrolment (Table 48; Harding 2004) and inconclusive findings on survival (Table 49; Walsh 2007).
41. Symptom burden: reinforced versus standard home palliative care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
McMillan 2007 US |
Revised version of Memorial Symptom Assessment Scale 24 symptoms (each rated from 0 to 4): lack of energy, pain, dry mouth, shortness of breath, lack of appetite, cough, feeling nervous, worrying, drowsy, feeling sad, feeling bloated, numbness or tingling, nausea, dizziness, difficulty sleeping, feeling irritable, difficulty concentrating, itching, sweats, difficulty swallowing, problems with urination, vomiting, diarrhoea, sexual problems; total score: from 0 to 96, greater scores equal greater symptom burden; patient report |
Forwards from enrolment | 16 days | Group main effecta: n.s. estimate 0.409 (SE 0.875); P value = 0.641 Group by time interactiona: statistically significant differences between the 3 groups estimate ‐0.101 (SE 0.038); P value = 0.009 Graph showed mean scores decreased from around 23 at baseline to 19 at 16 days and 17 at 30 days for the Cope intervention group, while in the standard care group they decreased from around 22 at baseline and at 16 days to around 21 at 30 days (in the supportive visits group they decreased from around 22 at baseline to 19.5 at 16 and 30 days) |
Authors computed separate random‐effects models comparing the standard home palliative care group with the standard plus supportive visits, and the standard plus the Cope intervention Standard home palliative care vs. standard plus Cope intervention group by time interaction: favours Cope intervention estimate ‐0.101 (SE 0.039); P value = 0.013 Standard home palliative care vs. standard plus supportive visits group by time interaction: n.s. estimate ‐0.035 (SE 0.073); P value = 0.633 |
| 30 days |
n.s.: non‐significant; SE: standard error. aUnstandardised estimates from random‐effects model.
42. Pain: reinforced versus standard home palliative care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
McMillan 2007 US |
Pain numeric rating scale score: from 0 to 10, higher scores equal greater pain; patient report |
Forwards from enrolment | 16 days | Group main effecta: n.s. estimate ‐0.039 (SE 0.197); P value = 0.836 Group by time interactiona: n.s. estimate ‐0.012 (SE 0.011); P value = 0.268 |
No descriptive data provided |
| 30 days |
n.s.: non‐significant; SE: standard error. aAuthors used a random‐effects model. Non‐significant group main effects or group by time interaction terms indicated no group differences in pain scores or trajectories of change.
43. Breathlessness: reinforced versus standard home palliative care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
McMillan 2007 US |
Dyspnoea intensity scale score: from 0 to 10; higher scores equal worse dyspnoea; patient report |
Forwards from enrolment | 16 days | Group main effecta: n.s. estimate 0.148 (SE 0.197); P value = 0.453 Group by time interactiona: n.s. estimate ‐0.003 (SE 0.011); P value = 0.771 |
No descriptive data provided |
| 30 days |
n.s.: non‐significant; SE: standard error. aAuthors used a random‐effects model. Non‐significant group main effects or group by time interaction terms indicated no group differences in pain scores or trajectories of change.
44. Constipation: reinforced versus standard home palliative care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
McMillan 2007 US |
Constipation assessment scale score: from 0 to 16, higher scores equal worse constipation; patient report |
Forwards from enrolment | 16 days | Group main effecta: n.s. estimate ‐0.170 (SE 0.208); P value = 0.416 Group by time interactiona: n.s. estimate ‐0.001 (SE 0.012); P value = 0.973 |
No descriptive data provided |
| 30 days |
n.s.; non‐significant; SE: standard error. aAuthors used a random‐effects model. Non‐significant group main effects or group by time interaction terms indicated no group differences in pain scores or trajectories of change.
45. Quality of life: reinforced versus standard home palliative care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
McMillan 2007 US |
Hospice Quality of Life Index (HQLI, 28 items) score: range 0 to 280; higher scores equal greater quality of life; patient report |
Forward from enrolment | 16 days | Group main effecta: n.s. estimate ‐2.994 (SE 2.562); P value = 0.246 Group by time interactiona: n.s. estimate 0.132 (SE 0.113); P value = 0.246 |
No descriptive data provided |
| 30 days |
n.s.: non‐significant; SE: standard error. aUnstandardised estimates from random‐effects model.
46. Physical function: reinforced versus standard home palliative care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Harding 2004 UK |
ECOG Performance Scale score: from 0 to 4, lower scores equal better performance status; caregiver report |
Forwards from enrolment | 8 weeks | n.s.a b (effect) ‐0.24 P value = 0.14 |
Sample at 8 weeks (n = 46) Intervention: M 2.0 (SD 1.3) Control: M 2.1 (SD 1.2) |
| 5 months | n.s.a b (effect) ‐0.34 P value = 0.08 |
Sample at 5 months (n = 26) Intervention: M 1.7 (SD 1.2) Control: M 2.3 (SD 1.3) |
n.s.: non‐significant; SD: standard deviation. aResults from multivariate regression on change scores from baseline.
47. Survival: reinforced versus standard home palliative care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Walsh 2007 UK |
Time from trial entry to death | Not stated | Not stated | Authors reported there were no differences but statistical significance was not stated "There was no difference between trial arms in (...) the patients' life expectancies; median survival time from trial entry was 12 weeks" (Walsh 2007) |
Intervention (n = 118): median 13 weeks (interdecile range 2 to 41.1) Control (n = 113): median 11 weeks (interdecile range 1 to 39.6) |
Caregiver outcomes
There was moderate evidence showing that providing a caregiver support component additional to specialist home palliative care made no statistically significant difference to caregivers' general health (two trials, Table 50), to their psychological well‐being (two trials, Table 51), coping (two trials, Table 52) and sense of mastery (two RCTs, Table 53). There was also limited evidence provided by Walsh 2007 of no statistically significant difference in the intensity of grief experienced by caregivers four months after the patient died (Table 54). However, two trials found beneficial effects for caregivers. Hudson 2005 provided limited evidence that adding a caregiver support component to specialist home palliative care led to caregivers feeling increased rewards from caregiving (Table 55). Statistically significant group by time interactions were found both pre‐ and post‐bereavement, showing that while reported rewards of caregiving decreased for controls, they increased for the intervention group from baseline to five weeks after and to eight weeks after the patient died. There was also limited evidence provided by McMillan 2007 of a beneficial effect on caregiver distress with the patient's symptoms during the month following enrolment (Table 56). The group receiving the "cope intervention" improved by 30% while the control group receiving standard home palliative care only showed a slight increase in scores. There were conflicting findings about the effect on caregiver burden (three studies, Table 57) and quality of life (two studies, Table 58).
48. Caregiver general health: reinforced versus standard home palliative care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Walsh 2007 UK |
General Heath Questionnaire (GHQ‐28) score: range not stated; higher scores equal more psychological distress; analysis used cut‐off of 5/6; caregiver report |
Forwards from enrolment | 4 weeks |
Participants below GHQ‐28 threshold (5/6) at any follow‐up point with no relapse n.s. Intervention: 21/100 (21%) vs. control: 21/91 (23%) Chi2 0.73 P value = 0.73 Participants below GHQ‐28 threshold (5/6) at any follow‐up point n.s. Intervention: 35/100 (35%) vs. control: 29/91 (32%) Chi2 0.65 P value = 0.76 |
Intervention (n = 97): M 10.5 (SD 6.3) Control (n = 85): M 11.9 (SD 6.4) |
| 9 weeks | Intervention (n = 70): M 9.3 (SD 6.5) Control (n = 64): M 10.7 (SD 7.3) |
||||
| 12 weeks | Intervention (n = 69): M 11.3 (SD 7.3) Control (n = 54): M 11.7 (SD 7.8) |
||||
|
Harding 2004 UK |
General Health Questionnaire (GHQ‐12) score: range not stated; higher scores equal higher levels of problems or difficulties; caregiver report |
Forwards from enrolment | 8 weeks | n.s.a b (effect) ‐0.12 P value = 0.42 |
Sample at 8 weeks (n = 41): Intervention: M 12.5 (SD 4.5) Control: M 14.9 (SD 5.7) |
| 5 months | n.s.a b (effect) ‐0.15 P value = 0.45 |
Sample at 5 months (n = 26): Intervention: M 12.3 (SD 4.2) Control: M 16.6 (SD 7.5) |
M: mean; n.s.: non‐significant; SD: standard deviation. aResults from multivariate regression on change scores from baseline.
49. Caregiver psychological well‐being: reinforced versus standard home palliative care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Hudson 2005 Australia |
Hospital Anxiety and Depression Scale (HADS, 14 items) score: range not stated, analysis used cut‐off of 11 points; lower scores equal possible case of anxiety/depression; caregiver report |
Forwards from enrolment | 5 weeks | n.s. "There were no significant effects or trends found with the variables (...) 'anxiety' between the Time 1 [baseline] and Time 2 [5 weeks] assessments" (Hudson 2005) |
n = 75 Intervention (n = 40): M 7.76 (SD 3.56) Control (n = 35): M 8.06 (SD 3.95) |
| Forwards from death | 8 weeks after death | Group main effect: n.s. P value > 0.05 |
n = 45 Intervention (n = 20): M 6.96 (SD 4.02) Control (n = 25): M 6.76 (SD 3.72) "The main effect of the within‐subjects factor 'time' indicated a trend for differences in overall mean scores between the two time points. Specifically, there was an overall decrease in mean anxiety scores between the pre‐intervention and bereavement" (Hudson 2005) (F = 2.77; P value = 0.10) |
||
|
Harding 2004 UK |
State Anxiety Scale (SAI) short‐version (6 items) score: range not stated; higher scores equal higher levels of problems or difficulties; caregiver report |
Forwards from enrolment | 8 weeks | n.s.a b (effect) ‐0.05 P value = 0.78 |
Sample at 8 weeks (n = 41): Intervention: M 43.2 (SD 11.4) Control: M 44.3 (SD 12.4) |
| 5 months | n.s.a b (effect) ‐2.23 P value = 0.29 |
Sample at 5 months (n = 26): Intervention: M 42.2 (SD 12.2) Control: M 53.4 (SD 16.9) |
M: mean; n.s.: non‐significant; SD: standard deviation aResults from multivariate regression on change scores from baseline.
50. Caregiver coping: reinforced versus standard home palliative care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
McMillan 2007 US |
Brief COPE Scale (28 items) measure of problem‐focused and emotion‐focused coping; 5‐point items, subscale score range not stated; caregiver report |
Forwards from enrolment | 16 days |
Problem‐focused coping group main effect: n.s.a estimate 0.05 (SE 0.03); P value = 0.867 group by time interaction: n.s.a estimate 0.02 (SE 0.01); P value = 0.256 Emotion‐focused coping group main effect: n.s.a estimate 0.14 (SE 0.36); P value = 0.694 group by time interaction: n.s.a estimate ‐0.01 (SE 0.02); P value = 0.813 |
Descriptive data not provided |
| 30 days | |||||
|
Harding 2004 UK |
Coping Responses Inventory (CRI, 48 items) measure of different types of coping responses to stressful life situations; scores range not stated; higher scores equal more reported use of coping strategies pertinent to that domain; caregiver report | Forwards from enrolment | 8 weeks | n.s.b CRI problem/approach focused b (effect) 0.16 P value = 0.34 CRI cognitive problem/approachfocused b (effect) 0.19 P value = 0.28 CRI behaviouralproblem/approach focused b (effect) 0.02 P value = 0.93 CRI emotion/avoidance focused b (effect)=0.14; P=0.47 CRI cognitive emotion/avoidance focused b (effect) 0.06 P value = 0.74 CRI behavioural emotion/avoidance focused b (effect) 0.06 P value = 0.75 |
Sample at 8 weeks (n = 41): CRI problem/approach focused Intervention: M 26.4 (SD 9.4) Control: M 26.4 (SD 7.5) CRI cognitive problem/approach focused Intervention: M 8.9 (SD 5.0) Control: M 8.3 (SD 5.2) CRI behavioural problem/approach focused Intervention: M 17.5 (SD 6.9) Control: M 18.1 (SD 5.8) CRI emotion/avoidance focused Intervention: M 37.6 (SD 10.0) Control: M 34.1 (SD 9.0) CRI cognitive emotion/avoidance focused Intervention: M 19.5 (SD 5.5) Control: M 18.5 (SD 6.8) CRI behavioural emotion/avoidance focused Intervention: M 18.1 (SD 6.2) Control: M 15.5 (SD 5.4) |
| 5 months | n.s.b CRI problem/approach focused b (effect) 0.32 P value = 0.75 CRI cognitive problem/approach focused b (effect) 0.17 P value = 0.42 CRI behavioural problem/approach focused b (effect) 0.10 P value = 0.62 CRI emotion/avoidance focused b (effect) 0.02 P value = 0.93 CRI cognitive emotion/avoidance focused b (effect) 0.08 P value = 0.70 CRI behavioural emotion/avoidance focused b (effect) ‐0.06 P value = 0.79 |
Sample at 5 months (n = 26): CRI problem/approach focused Intervention: M 27.0 (SD 7.1) Control: M 24.1 (SD 10.1) CRI cognitive problem/approach focused Intervention: M 8.8 (SD 4.0) Control: M 8.1 (SD 6.1) CRI behavioural problem/approach focused Intervention: M 18.1 (SD 5.8) Control: M 16.0 (SD 6.9) CRI emotion/avoidance focused Intervention: M 40.0 (SD 13.6) Control: M 32.1 (SD 10.8) CRI cognitive emotion/avoidance focused Intervention: M 19.4 (SD 7.8) Control: M 17.0 (SD 5.8) CRI behavioural emotion/avoidance focused Intervention: M 20.6 (SD 7.8) Control: M 15.1 (SD 5.9) |
M: mean; n.s.: non‐significant; SD: standard deviation; SE: standard error. aAuthors used a random‐effects model. Non‐significant group main effects or group by time interaction terms indicated no group differences in scores or trajectories of change. bResults from multivariate regression on change scores from baseline.
51. Caregiver mastery: reinforced versus standard home palliative care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
McMillan 2007 US |
1) General Caregiver Mastery (6 items) measure of caregiver feelings of control and confidence in caregiving; score range and interpretation not stated; caregiver report 2) Caregiver Demands Scale (46 items) measure of burden and mastery specific to caregiving tasks including assistance with meals, intimate care, treatments, and supervision of the patient; caregivers rated both how stressful the task was (burden) and their confidence in their ability to manage their stress related to this task (mastery); score range and interpretation not stated; caregiver report |
Forwards from enrolment | 16 days |
General mastery group main effect: n.s.a estimate 0.33 (SE 0.20); P value = 0.089 group by time interaction: n.s.a estimate 0.01 (SE 0.01); P value = 0.232 Caregiving task mastery group main effect: n.s.a estimate 0.03 (SE 0.05); P value = 0.514 group by time interaction: n.s.a estimate 0.01 (SE 0.01); P value = 0.466 |
"The caregivers' feelings of mastery were not affected by the intervention. Mastery may be difficult to improve in hospice given the very demanding nature of the caregiving involved" (McMillan 2006, McMillan 2007); no descriptive data provided |
| 30 days | |||||
|
Hudson 2005 Australia |
1) Preparedness for Caregiving Scale (8 items) measure of how ready caregivers perceive they are for their role; score range and interpretation not stated; caregiver report 2) Caregiver Competence Scale (4 items) measure of the perceived adequacy of an individual's performance as a caregiver; score range and interpretation not stated; caregiver report 3) Zeiss Caregiving Self efficacy Scale measure with 3 subscales: problem solving, respite and rewarding interaction; score range and interpretation not stated; caregiver report pre bereavement only |
Forwards from enrolment | 5 weeks |
Preparedness for caregiving group main effect: n.s. group by time interaction: n.s. P value > 0.05 Caregiver competence and caregiving self efficacy n.s. "There were no significant effects or trends found with the variables ‘self efficacy', ‘competence' (...) between the Time 1 [baseline] and Time 2 [five weeks] assessments" (Hudson 2005) |
n = 75 (35 intervention, 40 control) Preparedness for caregiving Intervention: M 2.76 (SD 0.81) Control: M 2.67 (SD 0.81) "There was a trend for the main effect of the within‐subjects factor 'time' [F = 3.36; P value = 0.071]. This indicated that preparedness increased as caregiving duration increased" (Hudson 2005) Caregiver competence Intervention: M 2.37 (SD 0.63) Control: M 2.40 (SD 0.54) Caregiving self efficacy ‐ Problem solving Intervention: M 6.96 (SD 4.02) Control: M 6.76 (SD 3.72) ‐ Respite Intervention: M 6.79 (SD 2.16) Control: M 6.23 (SD 2.67) ‐ Rewarding interaction Intervention: M 8.29 (SD 1.50) Control: M 8.22 (SD 2.50) |
| Forwards from death | 8 weeks after death |
Preparedness for caregiving n.s. "There were no significant effects found with ‘preparedness' between the Time 1 [baseline] and Time 3 [8 weeks after death] assessments" (Hudson 2005) Caregiver competence group main effect: n.s. group by time interaction: n.s. P value > 0.05 |
n = 45 (25 intervention, 20 control) Preparedness for caregiving Intervention: M 2.83 (SD 0.79) Control: M 2.59 (SD 0.88) "The main effect of the within‐subjects factor ‘time' was significant [F = 4.94; P value = 0.032]. Examination of the mean competence scores indicated an overall increase in reported competence between Time 1 and Time 3, irrespective of group" (Hudson 2005) Caregiver competence Intervention: M 2.53 (SD 0.51) Control: M 2.47 (SD 0.48) |
M: mean; n.s.: non‐significant; SD: standard deviation; SE: standard error. aAuthors used a random‐effects model. Non‐significant group main effects or group by time interaction terms indicated no group differences in scores or trajectories of change.
52. Caregiver grief: reinforced versus standard home palliative care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Walsh 2007 UK |
Core Bereavement Items (CBI) score: range and interpretation not stated; caregiver report |
Forwards from death | 4 months after death | n.s. t 0.91 P value = 0.37 |
Intervention (n = 84): M 46.3 (SD 11.4) Control (n = 97): M 45.6 (SD 11.6) |
M: mean; n.s.: non‐significant; SD: standard deviation.
53. Positive aspects of caregiving: reinforced versus standard home palliative care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Hudson 2005 Australia |
Rewards of Caregiving Scale authors used 11 items instead of the original 15, removing 4 items related to caregivers of the aged and 1 item related to caregivers of nursing home residents; score range and interpretation not stated; caregiver report |
Forwards from enrolment | 5 weeks | group main effect: n.s. P value > 0.05 group by time interaction: favours intervention F = 8.44 P value = 0.005 |
n = 75 Intervention (n = 40): M 3.09 (SD 0.82) Control (n = 35): M 2.82 (SD 0.99) "The standard care participants showed an overall decrease in reported rewards of caregiving between the Time 1 [baseline] and Time 2 [5 weeks] assessments, while the reported rewards of caregiving for the intervention group increased slightly" (Hudson 2005) "The main effect of the within‐subjects factor ‘time' indicated a trend for differences in overall mean reward scores over time [F = 2.84; P = 0.096]. Namely, the mean reward score for the entire sample at Time 1 [baseline] was greater than the mean reward scores for the entire sample at Time 2 [5 weeks]" (Hudson 2005) |
| Forwards from death | 8 weeks after death | group main effect: n.s. P value > 0.05 group by time interaction: favours intervention F = 4.68 P value = 0.036 |
n = 45 Intervention (n = 20): M 3.50 (SD 0.70) Control (n = 25): M 3.04 (SD 0.82) "Examination of the means table demonstrated that there was a slight decrease in the average rewards scores of the standard care group between Time 1 [baseline] and Time 3 [8 weeks after death]. In contrast, there was an overall increase in the average reward scores of the intervention group between Time 1 and Time 3" (Hudson 2005) "The main effect of the within‐subjects factor ‘time' indicated a trend for differences in overall mean scores between the two time points [F = 3.22; P = 0.080]. The mean scores for the entire sample at the two assessment times indicated that reported rewards at bereavement were greater than reported rewards at the baseline assessment" (Hudson 2005) |
M: mean; n.s.: non‐significant; SD: standard deviation.
54. Caregiver distress with patient symptoms: reinforced versus standard home palliative care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
McMillan 2007 US |
Symptom Assessment Scale (MSAS) 24 patient symptoms such as pain, lack of energy, diarrhoea, and shortness of breath; adapted by asking caregivers to rate how distressing patient symptoms were to them (caregivers); score range not stated; higher scores equal greater distress with symptom burden; caregiver report |
Forwards from enrolment | 16 days | Group main effect: n.s.a estimate ‐1.27 (SE 0.95); P value = 0.180 Group by time interaction: favours Cope intervention vs. standard home palliative care onlya estimate ‐0.14 (SE 0.04); P value = 0.001 |
Analysis of change over time within each group revealed improvements in the Cope intervention group (estimate ‐0.28; SE 0.07; P value < 0.001) but not in the control group receiving standard home palliative care only (estimate 0.01; SE 0.01; P value = 0.847). The Cope intervention group improved by 30% while the control group showed a slight increase in scores. Comparisons of the control group (i.e. standard specialist home hospice care) with a second control group (receiving standard specialist home hospice care + supportive visits) found no significant group by time interaction (estimate 0.13, SE 0.08; P value = 0.118). Graph of percentage changes provided in McMillan 2006 (McMillan 2007). |
| 30 days |
n.s.: non‐significant; SE: standard error. aUnstandardised estimates from random‐effects model.
55. Caregiver burden: reinforced versus standard home palliative care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
McMillan 2007 US |
Caregiver Demands Scale (CDS) measure of burden and mastery specific to caregiving tasks including assistance with meals, intimate care, treatments, and supervision of the patient; caregivers rated both how stressful the task was (burden) and their confidence in their ability to manage their stress related to this task (mastery); score range and interpretation not stated; caregiver report |
Forwards from enrolment | 16 days |
Caregiving task burden group main effect: marginally significant difference favouring Cope intervention vs. standard home palliative care onlya estimate ‐0.10 (SE 0.05); P value = 0.060 group by time interaction: favours Cope intervention against standard home palliative care onlya estimate ‐0.01 (SE 0.01); P value = 0.021 |
Comparisons of the control group (i.e. standard specialist home hospice care) with a second control group (receiving standard specialist home hospice care and supportive visits) found no significant group by time interaction (estimate 0.01, SE 0.01; P value = 0.542) There was a main effect of time (P value = 0.014) with increases in burden scores over time |
| 30 days | |||||
|
Walsh 2007 UK |
Carer Strain Index score range not stated; higher scores equal greater strain, caregiver report |
Forwards from enrolment | 4 weeks | n.s. "There was no significant interaction between time and trial arm (...) on carer strain" (Walsh 2007) |
Intervention (n = 99): M 27.7 (SD 11.6) Control (n = 86): M 27.8 (SD 11.5) |
| 9 weeks | Intervention (n = 73): M 26.7 (SD 11.4) Control (n = 63): M 25.1 (SD 10.1) |
||||
| 12 weeks | Intervention (n = 69): M 27.2 (SD 11.7) Control (n = 54): M 27.3 (SD 10.2) |
||||
|
Harding 2004 UK |
Zarit Burden Inventory (ZBI, 22 items) score range 0 to 88; higher scores equal greater burden; subscales for personal strain and role strain; caregiver report |
Forwards from enrolment | 8 weeks | n.s.b Zarit total b (effect) 0.06 P value = 0.73 Zarit burden item b (effect) 0.16 P value = 0.31 Zarit personal strain b (effect) 0.04 P value = 0.83 Zarit role strain b (effect) 0.05 P value = 0.74 |
Sample at 8 weeks (n = 41): Zarit total Intervention: M 29.2 (SD 14.9) Control: M 31.0 (SD 16.5) Zarit burden item Intervention: M 1.2 (SD 1.2) Control: M 1.0 (SD 1.3) Zarit personal strain Intervention: M 13.4 (SD 7.8) Control: M 15.0 (SD 8.7) Zarit role strain Intervention: M 8.5 (SD 5.6) Control: M 9.0 (SD 5.2) |
| 5 months | n.s.b Zarit total b (effect) ‐0.02 P value = 0.94 Zarit burden item b (effect) 0.33 P value = 0.11 Zarit personal strain b (effect) 0.12 P value = Zarit role strain b (effect) ‐0.17 P value = 0.38 |
Sample at 5 months (n = 26): Zarit total Intervention: M 27.1 (SD 13.2) Control: M 36.7 (SD 16.1) Zarit burden item Intervention: M 1.1 (SD 1.2) Control: M 1.8 (SD 1.6) Zarit personal strain Intervention: M 14.1 (SD 6.9) Control: M 17.1 (SD 7.5) Zarit role strain Intervention: M 6.7 (SD 4.4) Control: M 10.7 (SD 4.8) |
M: mean; n.s.: non‐significant; SD: standard deviation; SE: standard error. aAuthors used a random‐effects model. Non‐significant group main effects or group by time interaction terms indicated no group differences in scores or trajectories of change. bResults from multivariate regression on change scores from baseline.
56. Caregiver quality of life: reinforced versus standard home palliative care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Walsh 2007 UK |
Caregiver Quality of Life Index (Cancer) score: range not stated; higher scores equal lower quality of life; caregiver report |
Forwards from enrolment | 4 weeks | n.s. "Carer quality of life deteriorated over time, but there was no significant interaction between time and trial arm on this outcome" (Walsh 2007) |
Intervention (n = 93): M 69.6 (SD 22.4) Control (n = 82): M 63.9 (SD 19.3) |
| 9 weeks | Intervention (n = 71): M 69.3 (SD 22.7) Control (n = 59): M 65.2 (SD 17.0) |
||||
| 12 weeks | Intervention (n = 64): M 65.2 (SD 21.3) Control (n = 52): M 62.2 (SD 19.8) |
||||
|
McMillan 2007 US |
Caregiver Quality of Life Index Cancer (CQOL‐C, 35 items) 5‐point items, range of total score not stated; higher scores equal greater quality of life; caregiver report |
Forwards from enrolment | 16 days | Group main effect: n.s.a estimate ‐2.03 (SE 1.45); P value = 0.161 Group by time interaction: marginally significant difference favouring Cope intervention vs. standard home palliative care onlya estimate ‐0.09 (SE 0.05); P value = 0.054 |
Analysis of change over time within each group revealed caregiver quality of life improved in the Cope intervention group over time (estimate 0.16, SE 0.07; P value = 0.033) while it remained unchanged for caregivers in standard home palliative care (estimate 0.02, SE 0.06; P value = 0.718) Comparisons of the control group (i.e. standard specialist home hospice care) with a second control group (receiving standard specialist home hospice care and supportive visits) found no significant group by time interaction (estimate ‐0.06, SE 0.09; P value = 0.512) |
| 30 days |
M: mean; n.s.: non‐significant; SD: standard deviation; SE: standard error. aAuthors used a random‐effects model. Non‐significant group main effects or group by time interaction terms indicated no group differences in scores or trajectories of change.
Satisfaction with care
There was limited evidence provided by Walsh 2007 of no statistically significant effect on whether caregivers' perceived the care received as being poor four months after the patient died (Table 59).
57. Satisfaction with care: reinforced versus standard home palliative care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Walsh 2007 UK |
Care satisfaction tool not stated caregivers asked if they considered that the care received was poor (yes/no); caregiver report |
Backwards from death | 4 months after death | n.s. Chi2 0.96; P value = 0.81 |
Intervention: 16/83 considered care poor (18%) Control: 21/95 considered care poor (22%) |
n.s.: non‐significant.
Overall palliative care outcomes
There was limited evidence provided by Harding 2004 of no statistically significant effect on total scores from the POS at 8 and 20 weeks after enrolment (Table 60).
58. Overall palliative care outcomes: reinforced versus standard home palliative care.
| Study | Measure | Analysis | Follow‐up | Significance and direction | Details |
|
Harding 2004 UK |
Palliative care Outcome Scale (POS, 12 items) total scale score; range not stated; higher scores equal worse outcomes; caregiver report |
Forwards from enrolment | 8 weeks |
n.s.a b (effect) 0.05 P value = 0.78 |
n = 41 Intervention: M 15.0 (SD 7.0) Control: M 17.6 (SD 6.3) |
| 20 weeks |
n.s.a b (effect) 0.08 P value = 0.68 |
n = 26 Intervention: M 13.7 (SD 8.3) Control: M 16.8 (SD 6.3) |
M: mean; n.s.: non‐significant; SD: standard deviation. aResults from multivariate regression on change scores from baseline.
Impact on resource use
Sixteen studies measured the care resources used by the participants in different ways (Table 61). Five relied exclusively on chart review or automated recording systems from care providers. One study (Higginson 2009) relied exclusively on patients' reports of the last 12 weeks, systematically collected using a standard measure (Client Service Receipt Inventory), which the authors adapted to the study. Six studies used a mix of methods but all included reports from patients or caregivers, or both. Three studies validated the information provided by participants. In Hughes 1992, prospective self reported use of VA services via patient diaries was confirmed using VA records, files and computer databases, while self reported use of private sector services was confirmed through letters or telephone calls to hospitals, doctors, clinics, nursing homes and home care agencies. Hughes stated that confirmation by a provider was obtained in 99% of cases and only confirmed data were included in the analyses. In Zimmer 1985, hospitalisations reported by participants in diaries were validated and corrected when necessary against billing records and a sample was cross‐checked with the visiting nurse service and intervention records. In Greer 1986, service use data obtained from caregivers were checked with Medicare and other reimbursement records whenever feasible. Validation results were not reported in the two latter studies. Methods for collecting resource use information were unclear in four trials (Ahlner‐Elmqvist 2008; Jordhøy 2000; McKegney 1981; Tramarin 1992).
59. Methods of collecting resource use information and calculating costs.
| Study | Methods of collecting resource use information and calculating costs |
|
Rabow 2004 US |
At study completion, a trained researcher assistant (blinded to group allocation) reviewed the medical center's computerised medical records (these contained information as entered in written medical records by treating physicians) for all patients during the study period. Charges were identified from the computerised billing record. The authors recognised that analysis of cost data would be preferable but they were able only to acquire data on charges. Costs were USD; currency date and year(s) to which resource use referred were not stated (study first published in 2003) |
|
Grande 1999 UK |
Information on home nursing and inpatient care in the last year of life was collated from electronic health service databases. Year(s) to which resource use referred were not stated (study first published in 1999) |
|
Bakitas 2009 US |
Data on resource use were collected by chart review until death or end of study (2003‐2007) |
|
Brumley 2007 US |
Resource use data for each participant were collected retrospectively from the non‐profit HMO mainframe database, from the time the patient enrolled in the study until the time of death or end of study (2002 to 2004). Costs were calculated using actual costs for contracted medical services (services provided by non‐HMO contracted facilities in Colorado) and proxy cost estimates for all services provided within the HMO. The authors explained that because services provided within the HMO were not billed separately, it was necessary to use proxy costs. Hospitalisation and ED cost estimates were calculated using aggregated data from more than 500,000 HMO patient records and included ancillary services such as laboratory and radiology. Costs of physician office visits included nurse and clerk expenses. Home health and palliative care visits were calculated using "average time spent on each visit" multiplied by the cost for each discipline's reimbursement rate. The authors stated that proxy costs generated for hospital days and ED visits were significantly lower than the actual costs received from contracted providers. Costs were in 2002 USD |
|
McCorkle 1989 US |
A Medical Record Review Instrument was developed to collect systematic information about resource use from the patient's medical record. Participants were asked at each interview if they had been hospitalised, received medical treatment or visited their physician within the last 6 weeks. This information was used as a guide to identify the institutions in which medical records were to be reviewed. Trained research assistants audited the records from the time of diagnosis through the entire 24 weeks (6 months) of home care treatment (1983‐1985) |
|
Higginson 2009 UK |
Research assistants (not blinded to group allocation) collected resource use data in the last 3 months from patients in face‐to‐face interview using an adapted version of the Client Service Receipt Inventory; data were collected at baseline (before randomisation) and at 6 and 12 weeks, at 18 weeks (the latter only for the control group, after receiving the service) and 24 weeks. Costs were assessed using a broad perspective including costs to health, social and voluntary services, and informal caregivers. Service costs were calculated by combining resource use data with nationally applicable unit costs. Informal care costs were estimated by assuming that in the absence of a caregiver, the help would need to be provided by a home care worker; the unit costs of the latter were, therefore, used as a "shadow price". Costs were in 2005 GBP |
|
Aiken 2006 US |
MCOs provided resource use data on each participant for the duration of his/her enrolment in the study (1999‐2001), as well for the 6 months prior to enrolment (or all the time that the patient had been enrolled in the MCO prior to enrolment in the study). The authors had planned to measure hospital admissions as discrete events to compute length of stay for each admission as well as the cumulative number of inpatient days. However, they found that inadequately reported hospital claims data did not permit calculation of length of stay: "In a notable number of instances, admission date/discharge date pairs could not be unambiguously established from streams of MCO claims data; such pairs are required for each hospitalization episode for computation of the LOS of that hospitalization. Beyond this, an extensive line‐by‐line review of medical claims data by the PhoenixCare Medical Director and Project Director revealed that hospitalizations could not be sorted into those directly related to the PhoenixCare target diagnoses (CHF, COPD) versus those related to other ancillary conditions, because all hospitalizations were identified by the primary diagnosis regardless of the treatment provided" (Aiken 2006) |
|
Zimmer 1985 US |
Utilisation data were derived primarily from a health services utilisation diary. The diary was designed for the study and was a complete record of the patient's use of health services for as long as 6 months following study entry (1979‐1982). It was kept on a daily basis by the patient, if able, or otherwise by the caregiver (family member or friend). The diaries were monitored and collected biweekly by study interviewers. The diary recording of hospitalisations was validated, and corrected where necessary, by comparison with billing forms for all hospitalisations during the 6‐month period and also cross‐checked against a sample of Visiting Nurse Service records and records of the intervention team (the latter for the intervention group only). Resource use data were weighted to estimate costs "using current average charges for services in the community at the main provider agencies" where rates were constant (e.g. visiting nurse service, health department, ED, nursing homes). The actual mean of hospital daily charges (USD300) was obtained from their billing forms and was used as the hospital per diem weight. The authors explained that since third‐party reimbursements for physician house calls were well below actual costs, a more realistic physician home visit weighting factor was developed from estimates of total costs of a visit, including overhead and travel time, derived from a previous time‐motion study of the intervention team. Costs were in USD (currency date not stated) |
|
Jordhøy 2000 Norway |
Limited description of data collection methods. The authors stated that sociodemographic and medical data were collected by research assistants from patients at baseline and that these data were recorded partly by interview and partly by consulting patients' medical recorded. Use of healthcare services by patients in both groups was recorded (study took place from 1995 to 1997) |
|
Hughes 1992 US |
Use of healthcare services within and outside the VA was monitored by participants. To improve recall, patients were provided with a healthcare diary and were asked to record services for the 6‐month period of their participation in the study. They were contacted monthly by research staff to retrieve information and diaries were also examined by research staff in patients' homes during the 1 month and 6 month interviews. Self reported use of VA health care services was confirmed using VA records, files and computer databases. Self reported use of private sector health services was confirmed through letters or telephone calls to hospitals, doctors, clinic, nursing homes and home care agencies. Confirmation by a provider was obtained in 99% of cases and only confirmed utilisation data were included in the analysis. All VA hospital cost figures were derived from the hospital except VA ED and outpatient clinics (derived from national VA figures). Hospital costs were based on "average accounting costs per day in the hospital" (the authors believed that average cost data were the best available approximation of marginal costs referring to prior literature). Yearly "average per diem costs" for non‐government not‐for‐profit hospitals in the respective state (Illinois) provided by the American Hospital Association were adjusted based on Medicare national data to include physician costs (an additional 33%), resulting in an adjusted private hospital per diem rate of USD 665.49. ED visit base costs for all private hospitals in Illinois was provided by the Illinois Cost Containment Council and the "average base cost" for hospitals located in the area where the patient sample resided was calculated from this list. Home health agency costs were obtained from the Federal Register's Medicare schedule of maximum limits on home health agency costs for metropolitan Chicago. Medicare nursing home reimbursement rate in Illinois (USD 54.41) were provided by a survey from the Illinois Health Care Association. Actual charges confirmed by providers were used to impute the cost of private ambulatory care and home care services. Costs were in 1985 USD as 40% of patients were enrolled during that year (study took place from 1984 to 1987) |
|
McKegney 1981 US |
Although group differences in hospital inpatient days and costs are stated, the methods of data collection were not described. year(s) which resource use referred to were not stated (study first published in 1977) |
|
Tramarin 1992 Italy |
Limited description of data collection methods. The authors stated this was conducted prospectively using all available clinical documentation; costs were calculated with a specially designed software using a dBIII Plus database with more than 500 items. The authors stated that a top‐down approach was used to calculate costs because it was not possible to identify the separate use of the hospital facilities by each patient in the study (in contrast, the costs of the intervention were calculated for individual patients). The costing model was based on the analytical accounting system in use at the study hospital. Inpatient and outpatient clinical costs were estimated in 4 steps: 1) costs were obtained from the 1989 hospital general ledger (hospital overheads, ancillary services, direct inpatient services and non‐inpatient services) were mapped into initial cost centres (costs of physically discrete patient or support services, e.g. laboratory, laundry ward, radiography unit costs, according to existing hospital accounting schemes); 2) costs from the overhead cost centres were allocated, on the basis of individual cost centre allocation statistics, to the final cost centres; 3) final cost centres were adjusted on the basis of the specific inpatient factions they contained to exclude any costs for outpatient treatment; 4) inpatient and outpatient costs within the final cost centres were allocated to individual patients on the basis of their relative consumption of each final cost centre service. To obtain cost per person‐year, costs calculated during the 6 months following entry in the study (1990) were multiplied by 2. Costs were in 1990 ITL and in order to compare these costs with estimates from studies in other countries, the authors converted them to 1990 USD using health‐care‐specific purchasing power parities |
|
Ahlner‐Elmqvist 2008 Sweden |
Limited description of data collection methods. The authors stated that a full‐time employed research nurse collected medical baseline data; hospital stays were prospectively recorded for the entire study period (1995‐1999) |
|
Buckingham 1978 US |
Data were obtained from existing records, self completed questionnaire items, hospice routine data retrieval system (for the intervention group only) and medical records kept by the primary physician (study took place from 1975 to 1977) |
|
Axelsson 1998 Sweden |
Intervention and control patients received upon discharge from hospital a folder with diary sheets for the registration of their use of different resources at home. At the same time their GP and district nurse were notified by separate letters that the patient was being included in the study and that they should record any contact with the patient in the folder. The time spent on home visits by different categories of staff for the care of these patients was continuously monitored on separate sheets. This included travelling time both ways and was registered in 15‐minute units. In addition, medical records were examined to assess medical care utilisation. This was done prospectively for both groups. When a patient died, the data regarding their nursing requirements at home and in hospital were compiled. Intervention patients died between 1991 and 1993; control patients enrolled from 1992 to 1993 |
|
Greer 1986 (CBA) |
Resource use data were obtained from caregivers (at each interview they presented a record of all services used by the patient); these data were checked with Medicare and other reimbursement records whenever feasible. Information on treatment prior to study enrolment was obtained from medical records (study took place between 1981 and 1983). Hospice inpatient and home care unit cost coefficients were developed using 1982 cost report data compiled either by the Health Care Financing Administration or evaluation staff accountants. Cost reports separately allocated all pertinent agency costs to a hospice cost centre. All inpatient costs were nationally adjusted based on Medicare hospital reporting data; hospice home care costs were not nationally adjusted since national standards did not exist. Total costs combine 'costs' and 'charges' since only charges were available for physician services, drugs, supplies, and equipment purchased at home. Costs include only direct health care costs. Costs were in 1982 USD |
ED: emergency department; CHF: congestive heart failure; COPD: chronic obstructive pulmonary disease; GBP: British pound; GP: general practitioner; HMO: Health Maintenance Organisation; ITL: Italian lira; MCO: Managed Care Organisations; USD: United States dollar; VA: Veteran Affairs.
Institutional care
Sixteen studies compared the effect of home palliative and usual care on institutional care use. There was moderate evidence of no statistically significant effect on ED visits (six RCTs, Table 10) and on intensive care use (two RCTs, Table 62). Four of the six RCTs that examined the effect on ED visits found no statistically significant differences between intervention and control groups. In addition, a sub‐analysis of the last two weeks of life for the 33 patients that died in Zimmer 1985 found there were no ED visits in either group. A significant reduction in ED use as a result of receiving home palliative care was found only in Brumley 2007, where 20% of intervention patients had ED visits during the study period as opposed to 33% of those in usual care (P value = 0.01). Linear regression adjusted for survival, age and severity of illness showed that the 'in‐home palliative care' (IHPC) intervention reduced ED visits by 0.35 (P value = 0.02). Both RCTs examining the effect on intensive care use found no significant differences between intervention and control groups (Bakitas 2009; Hughes 1992).
60. Intensive care unit use.
| Study | Analysis | Time horizon | Significance and direction | Details |
|
Bakitas 2009 US (high quality) |
Forwards from enrolment | During study period | n.s. Wilcoxon rank sum test P value > 0.99 |
Intervention: 0.06 days Control: 0.06 days Note: not clear if the figures are means or medians |
|
Hughes 1992 US |
Forwards from enrolment | 6 months following enrolment | "n.s." t < 1 |
Intervention (n = 86): M 0.13 days (SD 0.80) Control (n = 85): M 0.45 days (SD 3.8) |
M:mean; n.s.: non‐significant; SD: standard deviation.
Findings from Jordhøy 2000 showed that fewer home palliative care patients were admitted to a nursing home in the month before death as compared to those receiving usual care (28/219 (13%) and 42/176 (24%), respectively; P value < 0.01). However, the difference lost statistical significance (P value = 0.08) when adjusted for other predictive factors (age, having home care at trial entry, living with a spouse and having a gastrointestinal or lung cancer diagnosis). This difference in the frequency of nursing home admission between intervention and control groups was also observed in the overall study period (38/235 (16%) and 46/199 (23%), respectively) but statistical significance was not reported (Table 63). The study also provided moderate evidence showing a lower mean proportion of time spent in nursing homes in the intervention group compared to the control both in the overall study period (3.0% and 7.4%, respectively) and in the last month before death (7.2% and 14.6%, respectively); adjusted for baseline imbalances and prognostic factors of nursing home admission, the differences were still significant (P value < 0.05, Table 64).
61. Nursing home admission.
| Study | Analysis | Time horizon | Significance and direction | Details |
|
Jordhøy 2000 Norway (high quality) |
Forwards from enrolment | During study period | Differences and significance not stated | Intervention: 38/235 (16%) were admitted; M 0.2 admissions (SD 0.6) Control: 46/199 (23%) were admitted; M 0.4 admissions (SD 0.9) |
| Backwards from death | Last month before death | Reduced nursing home admission in intervention P value < 0.01 However, multivariate regression showed no statistically significant group effect (P value = 0.08) when adjusted for age (OR 1.07; P value < 0.01), having home care at trial entry (OR 2.41; P value < 0.01), living with a spouse (OR 0.39; P value < 0.01) and having gastrointestinal or lung cancer diagnosis (OR 0.46; P value < 0.01) |
Intervention: 28/219 (13%) were admitted Control: 42/176 (24%) were admitted |
M: mean; OR: odds ratio; SD: standard deviation.
62. Time patient spent in nursing home.
| Study | Analysis | Time horizon | Significance and direction | Details |
|
Jordhøy 2000 Norway (high quality) |
Forwards from enrolment | During study period | Lower proportion of time spent in nursing homes in intervention group P value < 0.05 "The proportion of time spent in nursing homes was higher for the control group for the entire observation period and in the last month before death. Adjusted for baseline imbalances and prognostic factors as described, the differences were significant (p < 0.05). The factors that were predictive of proportion of readmission time in the last month of life were identical to those predictive of nursing‐home admission" (Jordhøy 2000) |
Proportion of days under observation in nursing homes Intervention (n = 235): M 3.0% (SD 10.7), median 0% (range 0% to 87%) Control (n = 199): M 7.4% (SD 18.6), median 0% (range 0% to 94%) |
| Backwards from death | Last month before death |
Proportion of days under observation in nursing homes Intervention (n = 219): M 7.2% (SD 22.0), median 0% (range 0% to 100%) Control (n = 176): M 14.6% (SD 30.5), median 0% (range 0% to 100%) |
M: mean; SD: standard deviation.
The evidence was inconclusive on the effect of home palliative care compared to usual care on the number of days spent in nursing homes (two RCTs, Table 65), hospital admission (10 studies, Table 66), length of hospital admissions (two RCTs, Table 67), length of last hospital admission before death (two trials, Table 68), hospital inpatient days (nine RCTs, Table 69), proportion of time the patient spent in hospital (two trials, Table 70) and overall institutional days (three trials and one CBA, Table 71).
63. Nursing home days.
| Study | Analysis | Time horizon | Significance and direction | Details |
|
Jordhøy 2000 Norway (high quality) |
Forwards from enrolment | During study period | Differences and statistical significance not stated | Intervention (n = 235): M 5.0 days (SD 17.3); total 1176 days Control (n = 199): M 9.3 days (SD 31.4); total 1855 days |
| Backwards from death | Last month before death | Differences and statistical significance not stated | Intervention (n = 219): M 2.2 days (SD 6.8); total 490 days Control (n = 176): M 4.3 days (SD 9.3); total 764 days |
|
|
Hughes 1992 US |
Forwards from enrolment | 6 months following enrolment | "n.s." t < 1 "n.s." t ‐1.00 |
VA nursing home days Intervention (n = 86): M 0.84 (SD 5.6) Control (n = 85): M 0.52 (SD 2.4) Non‐VA nursing home days Intervention (n = 86): M 0.07 (SD 0.07) Control (n = 85): M 0.00 (SD 0.0) |
M: mean; n.s.: non‐significant; SD: standard deviation.
64. Hospital admission.
| Study | Analysis | Time horizon | Significance and direction | Details |
|
Rabow 2004 US (high quality) |
Forwards from enrolment | During study period | n.s. t 1.26; P value = 0.21 |
Intervention (n = 50): M 1.2 admissions (SD 2.0) Control (n = 40): M 0.8 admissions (SD 1.0) |
|
Jordhøy 2000 Norway (high quality) |
Forwards from enrolment | During study period | Differences and statistical significance not stated | Intervention (n = 235): 93% were admitted; M 2.6 admissions (SD 1.9); total 601 admissions Control (n = 199): 94% were admitted; M 2.9 admissions (SD 2.7); total 570 admissions Note: because of structure of hospital files, admissions counted to individual hospital departments |
| Backwards from death | Last month before death | Differences and statistical significance not stated | Intervention (n = 219): 83% were admitted Control (n = 176): 87% were admitted |
|
|
Brumley 2007 US (high quality) |
Forwards from enrolment | During study period | Reduced hospitalisation in intervention group Cramer's V 0.23; P value < 0.001 |
Intervention: 36% were admitted Control: 59% were admitted |
|
McCorkle 1989 US |
Forwards from enrolment | 6 months following enrolment | n.s. "The OHC group had fewer hospitalizations than the other two groups. (...) Differences were not significant" (McCorkle 1989) |
Intervention (n = 24): 14 (59%) were admitted; M 2.08 admissions (SD 2.23, range 0 to 9); total 50 admissions Control1 (cancer home care; n = 27): 18 (67%) were admitted; M 2.82 admissions (SD 2.96, range 0 to 11); total 76 admissions Control2 (conventional care; n = 26): 20 (74%) were admitted; M 2.62 admissions (SD 1.81, range 0 to 8); total 68 admissions Note: excluded admissions for diagnosis and death; data limited to record audits completed at the participating institutions, numbers considered conservative |
|
Zimmer 1985 US |
Backwards from death | Last 2 weeks before death | Differences and statistical significance not stated | Intervention: 6/21 (29%) were admitted Control: 7/12 (58%) were admitted |
|
Hughes 1992 US |
Forwards from enrolment | 6 months following enrolment | Authors stated there was no difference but statistical significance not stated "Percent of subjects readmitted to the hospital by group did not differ" (Hughes 1992) |
Intervention (n = 86): 66% were admitted Control (n = 85): 74% were admitted |
|
Tramarin 1992 Italy |
Forwards from enrolment | 6 months following enrolment | Differences and statistical significance not stated | Intervention: stage2: 1 admission by patient; stage3: 3 admissions by patient Control: stage 2: 2.5 admissions by patient; stage 3: 3.5 admissions by patient Note: not clear if the figures provided are means or medians |
|
Ahlner‐Elmqvist 2008 Sweden |
Forwards from enrolment | During study period | Differences and statistical significance not stated | Intervention: 93/117 (79%) were admitted Control: 161/163 (99%) were admitted |
|
Buckingham 1978 US |
Not stated | Not stated | Authors stated there was no difference but statistical significance not stated | "Nonhospice patients were channelled in and out of hospitals to a greater extent than were hospice patients" (Buckingham 1978); no data provided to support this statement |
|
Axelsson 1998 Sweden |
Backwards from death | Last 6 months before death | n.s. P value ≥ 0.05 |
Intervention (n = 41): median 3 admissions (range 0 to 12) Control (n = 15): median 3 admissions (range 0 to 8) |
M: mean; n.s.: non‐significant; OHC: specialised Oncology Home Care (intervention group); SD: standard deviation.
65. Length of hospital admissions.
| Study | Analysis | Time horizon | Significance and direction | Details |
|
Jordhøy 2000 Norway (high quality) |
Forwards from enrolment | During study period | Statistical significance not stated |
Length of admission Intervention (n = 235): M 10.5 days (SD 7) Control (n = 199): M 11.5 days (SD 8.9) |
|
Tramarin 1992 Italy |
Forwards from enrolment | 6 months following | Statistical significance not stated |
"Average" duration of stay Intervention: stage2: 6 days; stage3: 20 days Control: stage2: 2.19 days; stage3: 37 days Note: not clear if figures are means or medians "The overall reductions in duration of stay for the intervention group were 68.5 and 46% at stages 2 and 3, respectively" (Tramarin 1992) |
M: mean; SD; standard deviation.
66. Length of last hospital admission before death.
| Study | Analysis | Time horizon | Significance and direction | Details |
|
Hughes 1992 US |
Backwards from death | NA |
Length of last hospital admission authors stated reduced length of last hospital admission in intervention group but statistical significance was not stated |
Length of last hospital admission "HBHC patients spent 3.5 fewer days in the hospital prior to death than control group patients (mean 9.9 days versus 13.5 days, respectively)" (Hughes 1992) |
| Axelsson 1998 Sweden | Backwards from death | NA |
Length of terminal hospitalisation P value ≥ 0.05 "We found no significant differences in health care utilization when we compared the study group with the reference group" (Axelsson 1998) |
Length of terminal hospitalisation Intervention (n = 41): median 3 days (range 0 to 85) Control (n = 15): median 12 days (range 0 to 47) |
HBHC: hospital‐based home care (intervention); NA: not applicable.
67. Hospital inpatient days.
| Study | Analysis | Time horizon | Significance and direction | Details |
|
Rabow 2004 US (high quality) |
Forwards from enrolment | During study period | n.s. t 0.88 P value = 0.38 |
Intervention (n = 50): M 6.3 days (SD 12.4) Control (n = 40): M 4.3 (SD 9.0) |
|
Jordhøy 2000 Norway (high quality) |
Forwards from enrolment | During study period | Differences and statistical significance not stated | Intervention (n = 235): M 25.3 days (SD 22.4); total 5937 days Control (n = 199): M 29.1 days (SD 29.3); total 5784 days |
| Backwards from death | Last month before death | Differences and statistical significance not stated | Intervention (n = 219): M 12.1 days (SD 10.0); total 2650 days Control (n = 176): M 12.4 days (SD 9.4); total 2183 days |
|
|
McKegney 1981 US (high quality) |
Not stated | Not stated | Authors stated there were fewer hospital days in intervention group but statistical significance was not stated | "Patients who were home visited by the nurses spent fewer days in the hospital than those not visited by the nurse" (Yates 1979, McKegney 1981); no data provided to support this statement |
|
Bakitas 2009 US (high quality) |
Forwards from enrolment | During study period | n.s. Wilcoxon rank sum test P value = 0.14 |
Intervention: M 6.6 days Control: M 6.5 days |
|
Brumley 2007 US (high quality) |
Forwards from enrolment | During study period | Fewer hospital days in intervention group Linear regression adjusted for survival, age and severity of illness showed intervention reduced hospital days by 4.36 (P value < 0.001) |
No descriptive data provided |
|
McCorkle 1989 US |
Forwards from enrolment | 6 months following enrolment | n.s. "Although not statistically significant, the total length of hospital stays was lower among subjects randomized to the specialized OHC program (OHC 258 days) compared with the SHC group (SHC 317 days) and the OC group (OC 272 days)" (McCorkle 1989) |
Intervention: M 18.43 days (SD 19.71, range 4 to 80); total 258 days Control1 (cancer home care): M 17.61 days (SD 17.72, range 3 to 77); total 317 days Control2 (conventional care): M 13.60 days (SD 10.39, range 1 to 38); total 272 days Note: excluded days in hospital for diagnosis and death; data limited to record audits completed at the participating institutions, numbers considered conservative |
|
Zimmer 1985 US |
Backwards from death | Last 2 weeks before death | Authors stated reduced hospital days in intervention group but statistical significance was not stated "Utilization of health care services during the terminal two weeks differed substantially between team and control patients (...). Team patients on the average had about half the number of hospital days" (Zimmer 1984, Zimmer 1985) |
Intervention (n = 21): "average" 3.1; total 61 days Control (n = 12): "average" 6.1; total 59 days |
|
Hughes 1992 US |
Forwards from enrolment | 6 months following enrolment |
VA total hospital days fewer hospital days in intervention group t 2.27 P value = 0.03 VA hospital rehabilitation days "n.s."; t < 1 VA hospital intermediate bed days "n.s."; t ‐1.22 VA hospital general bed days: fewer hospital general bed days in intervention group; t 3.26; P value = 0.002 Non‐VA private hospital days "n.s."; t < 1 |
VA total hospital days Intervention (n = 86): M 9.94 days (SD 13.3) Control (n = 85): M 15.86 days (SD 20.1) VA hospital rehabilitation days: Intervention (n = 86): M 0.00 (SD 0.0) Control (n = 85): M 0.14 (SD 1.3) VA hospital intermediate bed days: Intervention (n = 86): M 4.00 (SD 8.0) Control (n = 85): M 2.52 (SD 7.9) VA hospital general bed days: Intervention (n = 86): M 5.63 (SD 10.0) Control (n = 85): M 12.06 (SD 15.2) Non‐VA private hospital days Intervention (n = 86): M 0.69 days (SD 3.4) Control (n = 85): M 0.43 days (SD 2.2) |
|
Tramarin 1992 Italy |
Forwards from enrolment | 6 months following enrolment | Differences and statistical significance not stated | Intervention: stage2: 6 days; stage3: 121 days Control: stage2: 288 days; stage3: 467 days Note: not clear if figures are totals, means or medians |
M: mean; n.s.: non‐significant; OC: office care (control2); OHC: specialised oncology home care (intervention); SD: standard deviation; SHC: standard home care (control1); VA: Veteran Affairs.
68. Time patient spent in hospital.
| Study | Analysis | Time horizon | Significance and direction | Details |
|
Jordhøy 2000 Norway (high quality) |
Forwards from enrolment | During study period | n.s. "Overall, the proportion of hospital readmission time did not differ for the entire follow‐up or for the last month. Being female was the only factor predictive of time spent in hospital during the last month before death (p = 0.03)" (Jordhøy 2000) |
Proportion of days under observation in hospital Intervention (n = 235): M 32.2% (SD 31.8), median 20.9 (range 0 to 100) Control (n = 199): M 29.8% (SD 29.3), median 20.8 (range 0 to 100) "Because of bed shortages in Norwegian hospitals, the limited number of nursing‐home beds are used for basic inpatient care whenever possible. By comparison, the inpatient capacity at the Palliative Medicine Unit was large, and we believe that, for the intervention group, hospital care (The Palliative Medicine Unit) was used instead of nursing‐home care for some patients, whereas there was a shift from hospital to home care for other patients, resulting in the overall unchanged use of hospital" (Jordhøy 2000) |
| Backwards from death | Last month before death |
Proportion of days under observation in hospital Intervention (n = 219): M 45.5% (SD 35.2), median 41.9 (range 0 to 100) Control (n = 176): M 45.3% (SD 33.2), median 39.7 (range 0 to 100) |
||
|
Ahlner‐Elmqvist 2008 Sweden |
Forwards from enrolment | During study period | Lower proportion of time in hospital in intervention group P value < 0.005 |
Proportion of time spent in hospital 18% for intervention and 31% for control |
| Backwards from death | Last month before death |
Proportion of time spent in hospital lower proportion of time in hospital in intervention group P value < 0.005 Proportion patients who spent all time in hospital statistical significance not stated |
Proportion of time spent in hospital 31% for intervention and 57% for control Proportion patients who spent all time in hospital Intervention: 13 (11%) Control: 52 (32%) |
M: mean; n.s.: non‐significant; SD: standard deviation.
69. Institutional days.
| Study | Analysis | Time horizon | Significance and direction | Details |
|
Higginson 2009 UK (high quality) |
Forwards from enrolment | 12 weeks following enrolment | Authors stated increased institutional days in control group but statistical significance was not stated "The control care patients were more likely to be (...) admitted to or seen in hospital" (Higginson 2009) |
Intervention: 4/26 (17%) were institutionalised with M 19.0 days (SD 21.6) Control: 6/28 (29%) were institutionalised with M 30.7 days (SD 32.1) |
|
Grande 1999 UK |
Backwards from death | Last year before death | Mann Whitney U test n.s. "None of the differences were statistically significant" (Grande 2004; Grande 1999) |
Subanalysis of sample in bereavement follow‐up (n = 96) Intervention (n = 78): median 24.0 days (IQR 41.0) Control (n = 18): median 14.5 days (IQR 29.6) Note: institutional days included hospice, acute hospital, nursing home and continuing care beds |
|
Axelsson 1998 Sweden |
Backwards from death | Diagnosis to death | n.s. P value ≥ 0.05 |
Intervention (n = 41): median 52.5 days (range 0 to 299) Control (n = 15): median 53.5 days (range 8 to 107) |
| Last 6 months before death | n.s. P value ≥ 0.05 |
Intervention (n = 41): median 31 days (range 0 to 94) Control (n = 15): median 25 days (range 0 to 97) |
||
|
Greer 1986 (CBA) |
Forwards from enrolment | During study period (standardised to 50 days) | Authors stated increased institutional days in control group but statistical significance was not stated "CC patients spent more time in inpatient settings than either HB or HC patients" (Greer 1986) |
Adjusted estimatesa "Average" number of inpatient days per study day multiplied by "average" number of study days for hospice patients (50 days) Community‐based home hospice care: 8.0 days (SE 1.0) Hospice‐based home hospice care: 18.0 days (SE 1.5) Conventional care: 23.0 days (SE 2.0) Note: not clear if the figures are means or medians |
CC: conventional care (control group); HB: hospital‐based (hospital‐based intervention; HC: home‐care based (community‐based intervention); IQR: interquartile range; M: mean; SD: standard deviation; SE: standard error. aStandard errors of estimates were based upon multiple regression analyses adjusted for sample differences. In calculating total per patient utilisation, the authors multiplied the utilisation per study day by the "average" number of study days (50) for hospice patients (intervention group).
Outpatient clinics
Five RCTs and one CBA provided inconclusive evidence on the effect of home palliative care compared to usual care on outpatient clinic visits (Table 72). Rabow 2004 found fewer urgent care visits in the intervention group than in the control group (mean 0.3 and 0.6 visits, respectively, during the study period; P value = 0.04) but no difference in specialist visits (mean 4.9 and 7.0 visits, respectively; P value = 0.25). Hughes 1992 found fewer VA outpatient clinic visits in the intervention group than in the control group (mean 0.73 and 2.59 visits, respectively in the six months following enrolment; P value = 0.01) but no difference in non‐VA ambulatory care visits (mean 0.00 and 0.16 visits, respectively; "n.s." [not significant]). The remaining three RCTs (Higginson 2009; Zimmer 1985; Tramarin 1992) reported fewer outpatient clinic visits (hospital specialist visits, out‐of‐home clinic visits and outpatient daily admissions by patient) in the intervention group but statistical significance was not stated.
70. Outpatient clinic visits.
| Study | Analysis | Time horizon | Significance and direction | Details |
|
Rabow 2004 US (high quality) |
Forwards from enrolment | During study period |
Urgent care visits fewer visits in intervention group t ‐2.13 P value = 0.04 Specialist visits n.s. t ‐1.16 P value = 0.25 |
Urgent care visits Intervention (n = 50): M 0.3 visits (SD 0.5) Control (n = 40): M 0.6 visits (SD 0.9) Specialist visits Intervention (n = 50): M 4.9 visits (SD 8.1) Control (n = 40): M 7.0 visits (SD 9.1) |
|
Higginson 2009 UK (high quality) |
Forwards from enrolment | 12 weeks following enrolment |
Hospital specialist visits differences and statistical significance not stated |
Hospital specialist visits Intervention: 8 (35%) received; M 1.0 contacts (SD 0.0) Control: 16 (76%) received; M 1.3 contacts (SD 0.7) |
|
Zimmer 1985 US |
Backwards from death | Last 2 weeks before death |
Out‐of‐home clinic visits per patient differences and statistical significance not stated |
Out‐of‐home clinic visits per patient Intervention (n = 21): 0 visits Control (n = 12): 0.2 visits Note: not clear if the figures are means or medians |
|
Hughes 1992 US |
Forwards from enrolment | 6 months following enrolment |
VA outpatient clinic visits fewer visits in intervention group t 2.57 P value = 0.01 Non‐VA ambulatory care visits "n.s." t 1.30 |
VA outpatient clinic visits Intervention (n = 86): M 0.73 (SD 1.9) Control (n = 85): M 2.59 (SD 6.1) Non‐VA ambulatory care visits Intervention: M 0.00 (SD 0.0) Control: M 0.16 (SD 1.2) |
|
Tramarin 1992 Italy |
Forwards from enrolment | 6 months following enrolment |
Outpatient visits per patient authors stated reduced use of outpatient clinics in intervention group for stage 3 patients only, but statistical significance was not stated "The range of use of the outpatient clinic differed only for SCSAH stage 3 of the HC group, with a reduction in daily admission per patient of 31.9%" (Tramarin 1992) |
Outpatient daily admissions by patient Intervention: stage2: 25 daily admissions by patient; stage3: 7.5 daily admissions by patient Control: stage2: 24.9 daily admissions by patient; stage3: 11 daily admissions by patient Note: not clear if the figures are means or medians |
| Greer 1986 (CBA) | Forwards from enrolment | During study period (standardised to 50 days) |
Physician and outpatient clinic visits differences and statistical significance not stated |
Adjusted estimatesa Physician and outpatient clinic visits Community‐based intervention: 9.0 visits (SE 1.5) Hospice‐based intervention: 13.0 visits (SE 1.5) Control (conventional care): 20.0 visits (SE 0.5) Note: not clear if the figures are means or medians |
M: mean; n.s.: non‐significant; SE: standard error; VA: Veteran Affairs. aStandard errors of estimates were based upon multiple regression analyses adjusted for sample differences. In calculating total per patient utilisation, the authors multiplied the utilisation per study day by the "average" number of study days (50) for hospice patients (intervention group).
Community care
Nine trials and one CBA compared the effect of home palliative and usual care on community care use (Table 73). Apart from services related to the intervention (not received by controls), the studies measured the use of a range of community services as available locally. There was moderate evidence from the US showing no statistically significant differences in referrals to hospice care (Bakitas 2009; Brumley 2007) and limited evidence of no statistically significant differences in the use of private home care (Hughes 1992) and night sitting (Axelsson 1998). The evidence was inconclusive for all other community services measured including physician visits (five trials), nursing care (five trials and one CBA), social services and home workers (Greer 1986; Zimmer 1985).
71. Community care.
| Study | Analysis | Time horizon | Significance and direction | Details |
|
Rabow 2004 US (high quality) |
Forwards from enrolment | During study period |
Primary care clinic visits fewer visits in intervention group t ‐2.20 P value = 0.03 |
Primary care clinic visits Intervention (n = 50): M 7.5 (SD 4.9) Control (n = 40): M 10.6 (SD 7.5) |
|
Higginson 2009 UK (high quality) |
Forwards from enrolment | 12 weeks after enrolment |
General practice authors stated less GP contact in intervention group but statistical significance was not stated District/practice nurse differences and statistical significance not stated MS nurse authors stated there were no differences but statistical significance was not stated Social services differences and statistical significance not stated Specialist home visit differences and statistical significance not stated |
General practice Intervention: 8 (35%) received; M 3.8 contacts (SD 0.5) Control: 11 (52%) received; M 3.4 contacts (SD 1.2) "Control care patients were more likely to be in contact with general practitioners" (Higginson 2009) District/practice nurse Intervention: 20 (87%) received; M 12.3 contacts (SD 19.7) Control: 13 (62%) received; M 31.9 contacts (SD 50.7) MS nurse Intervention: 11 (48%) received; M 1.8 contacts (SD 1.8) Control: 7 (33%) received; M 1.1 contacts (SD 0.2) "Receipt of MS nurses was similar in the two groups" Social services Intervention: 10 (43%) received; M 6.4 contacts (SD 7.7) Control: 8 (38%) received; M 4.1 contacts (SD 2.4) Specialist home visit Intervention: 5 (22%) received; M 5.2 contacts (SD 4.5) Control: 0 received Note: authors stated that specialist home visits were most likely to be from the intervention home palliative care team |
|
Grande 1999 UK |
Backwards from death |
Penultimate week before death |
GP visits Daytime during week n.s.; P value ≥ 0.05 Daytime during weekend n.s.; P value ≥ 0.05 Fewer evening visits in intervention group; P value < 0.05 Fewer night visits in intervention group; P value < 0.001 |
GP visits Daytime during week: Intervention: M 2.18 (SD 1.73) Control: M 2.32 (SD 2.42) Daytime during weekend: Intervention: M 0.35 (SD 0.81) Control: M 0.39 (SD 0.68) Evening: Intervention: M 0.17 (SD 0.46) Control: M 0.61 (SD 1.42) Night: Intervention: M 0.04 (SD 0.20) Control: M 0.26 (SD 0.55) |
| Last week before death |
GP visits Daytime during week n.s.; P value ≥ 0.05 Daytime during weekend n.s.; P value ≥ 0.05 Evening visits n.s.; P value ≥ 0.05 Night visits n.s.; P value ≥ 0.05 |
GP visits Daytime during week: Intervention: M 2.92 (SD 2.20) Control: M 3.03 (SD 3.18) Daytime during weekend: Intervention: M 0.63 (SD 1.07) Control: M 0.95 (SD 1.56) Evening: Intervention: M 0.59 (SD 0.91) Control: M 1.11 (SD 1.56) Night: Intervention: M 0.47 (SD 0.82) Control: M 0.63 (SD 1.10) |
||
| Last year before death |
Hours of home nursing care n.s. "none of the differences were significant" (Grande 2004, Grande 1999) Hours of HAH home nursing difference due to the intervention (control group received none) |
Subanalysis of sample in bereavement follow‐up (n = 96) Hours of home nursing care Intervention (n = 78): median 46.1 (IQR 83.8) Control (n = 18): median 24.0 (IRQ 46.6) Hours of HAH home nursing Intervention (n = 78): median 18.0 (IRQ 107.0) Control (n = 18): median 0.0 (IRQ 0.0) |
||
|
Bakitas 2009 US (high quality) |
Forwards from enrolment | During study period |
Referral to hospice care n.s. Fisher exact test P value = 0.75 |
Referral to hospice care Intervention: 6/161 (3.7%) Control: 4/161 (2.5%) |
|
Brumley 2007 US (high quality) |
Forwards from enrolment | During study period |
Referral to hospice care (1 of 2 sites only) n.s. Chi2 P value = 0.15 Days in hospice care (1 of 2 sites only) n.s. t 0.52 P value = 0.60 |
Referral to hospice care (1 of 2 sites only) Intervention: 25% Control: 36% Days in hospice care (1 of 2 sites only) descriptive data not provided |
|
Zimmer 1985 US |
Backwards from death | Last 2 weeks before death | Authors stated reduced use of "in‐home" services in intervention group but statistical significance was not stated "Team patients (...) received more in‐home services" (Zimmer 1984, Zimmer 1985) |
MD home visits Intervention (n = 21): 0.8 Control (n = 12): 0.1 MD office visits Intervention (n = 21): 0 Control (n = 12): 0 Nurse home visits Intervention (n = 21): 1.7 Control (n = 12): 1.1 RN/LPN hours Intervention (n = 21): 51.2 Control (n = 12): 42.0 Social worker home visits Intervention (n = 21): 0 Control (n = 12): 0 Aide/homemaker visits Intervention (n = 21): 21.1 Control (n = 12): 11.5 Laboratory technician home visits Intervention (n = 21): 0.1 Control (n = 12): 0 Meals‐on‐wheels visits Intervention (n = 21): 0.5 Control (n = 12): 0 Note: not clear if the figures are means or medians |
|
Hughes 1992 US |
Forwards from enrolment | 6 months following enrolment |
Non‐VA community nursing visits fewer visits in intervention t 4.69 P value = 0.0001 Non‐VA private home care visits "n.s." t ‐1.42 HBHC visits difference due to the intervention (control group received none) |
Non‐VA community nursing visits Intervention (n = 86): M 0.06 (SD 0.5) Control (n = 85): M 7.06 (SD 13.7) Non‐VA private home care visits Intervention (n = 86): M 2.00 (SD 12.8) Control (n = 85): M 0.07 (SD 0.6) HBHC visits Intervention (n = 86): M 17.93 (SD 18.2) Control (n = 85): 0 received |
|
Buckingham 1978 US |
Not stated | Not stated | Authors stated reduced use of home care in control group but statistical significance was not stated | "Few patients in the nonhospice study group received any form of home care service. A strong possibility exists therefore, that home care and not hospice service as such was the critical element in alleviating problems of terminal illness for hospice patients and their families. However, if this is true, the fact remains that Hospice, Inc., has presented itself as an effective vehicle for such home care assistance" (Buckingham 1978); no data provided to support this statement |
|
Axelsson 1998 Sweden |
Forwards from enrolment | During study period |
All listed services: n.s. "When comparing the study group with the reference group, there were no significant differences in the utilization of resources at home outside the PSS, such as district nurses, the domiciliary service and so on" (Axelsson 1998) |
Consultant nurse Intervention: median 14.5 hours (range 2 to 157) Control: 0 received Surgeon Intervention: median 2 hours (range 0 to 11) Control: 0 received District nurse Intervention: median 2.25 hours (range 0 to 81) Control: median 4.5 hours (range 0 to 33.5) Assistant nurse Intervention: median 0 hours (range 0 to 79.5) Control: median 0 hours (range 0 to 1.5) GP Intervention: median 0 hours (range 0 to 3) Control: median 0 hours (range 0 to 3) Home service Intervention: median 0 hours (range 0 to 435) Control: median 0 hours (range 0 to 12) Night sitting Intervention: median 0 hours (range 0 to 96) Control: median 0 hours (range 0 to 0) |
|
Greer 1986 (CBA) |
Forwards from enrolment |
During study period (standardised to 50 days) |
Home nursing visits Differences and statistical significance not stated Home health/homemaker visits Differences and statistical significance not stated Social service and other therapies visits Differences and statistical significance not stated |
Adjusted estimatesa Home nursing visits Community‐based home hospice care: 15.5 (SE 1.5) Hospice‐based home hospice care: 11.0 (SE 1.5) Conventional care: 3.5 (SE 0.5) Home health/homemaker visits Community‐based home hospice care: 18.0 (SE 1.5) Hospice‐based home hospice care: 10.5 (SE 2.0) Conventional care: 4.0 (SE 0.5) Social service and other therapies visits Community‐based home hospice care: 2.5 (SE 0.3) Hospice‐based home hospice care: 1.0 (SE 0.3) Conventional care: 0.2 (SE 0.1) Note: not clear if the figures are means or medians |
| Backwards from death | Last week before death | Authors stated increased use of social services in intervention group but statistical significance was not stated "Hospice patients (...) are more likely to receive social service support than CC patients" (Greer 1986) |
Adjusted estimatesb Receipt of social services (included general counselling, legal/financial counselling, paperwork assistance, help getting services, self care training) Community‐based home hospice care: 61% (SE 0.03) Hospice‐based home hospice care: 65% (SE 0.03) Conventional care: 49% (SE 0.05) |
|
| Last 2 weeks before death |
Receipt of social services increased social care use in intervention groups P value < 0.01 General counselling presented as n.s. by authors; P value ≥ 0.01 Legal/financial counselling presented as n.s. by authors; P value ≥ 0.01 Paperwork assistance increased paper work assistance in intervention groups; P value < 0.001 Help getting services presented as n.s. by authors; P value ≥ 0.01 Self care training presented as n.s. by authors; P value ≥ 0.01 |
Receipt of social services (included general counselling, legal/financial counselling, paperwork assistance, help getting services, self care training) Community‐based home hospice care: 60.1% Hospital‐based home hospice care: 63.5% Conventional care: 51.2% General counselling: Community‐based home hospice care: 34.6% Hospital‐based home hospice care: 34.0% Conventional care: 26.6% Legal/financial counselling: Community‐based home hospice care: 8.0% Hospital‐based home hospice care: 8.0% Conventional care: 7.6% Paperwork assistance: Community‐based home hospice care: 29.3% Hospital‐based home hospice care: 35.1% Conventional care: 20.8% Help getting services: Community‐based home hospice care: 28.1% Hospital‐based home hospice care: 32.0% Conventional care: 23.5% Self care training: Community‐based home hospice care: 7.7% Hospital‐based home hospice care: 9.7% Conventional care: 6.4% |
||
| Total study period |
Receipt of social services increased social care use in intervention group P value < 0.01 General counselling: increased use of general counselling in intervention groups; P value < 0.01 Legal/financial counselling presented as n.s. by authors; P value ≥ 0.01 Paperwork assistance: increased paper work assistance in intervention groups; P value < 0.001 Help getting services: increased help getting services in intervention groups; P value < 0.001 Self care training presented as n.s. by authors; P value ≥ 0.01 |
Receipt of social services (included general counselling, legal/financial counselling, paperwork assistance, help getting services, self care training) Community‐based home hospice care: 77.3% Hospital‐based home hospice care: 77.3% Conventional care: 67.8% "Social service use was more prevalent among hospice patients throughout the course of the study, but this difference also existed prior to hospice admission and, at least partially, might have resulted from the use of social services in the process of transferring from conventional care to hospice" (Greer 1986) General counselling: Community‐based home hospice care: 48.4% Hospital‐based home hospice care: 50.2% Conventional care: 38.6% Legal/financial counselling: Community‐based home hospice care: 13.4% Hospital‐based home hospice care: 13.6% Conventional care: 13.4% Paperwork assistance: Community‐based home hospice care: 43.3% Hospital‐based home hospice care: 44.3% Conventional care: 30.7% Help getting services: Community‐based home hospice care: 45.9% Hospital‐based home hospice care: 50.0% Conventional care: 35.3% Self care training: Community‐based home hospice care: 17.7% Hospital‐based home hospice care: 20.1% Conventional care: 16.1% |
CBA: controlled before and after study; CC: conventional care (control); GP: general practitioner; HAH: hospital at home (intervention); HBHC: hospital‐based team home care (intervention); IQR: interquartile range; LPN: licensed practical nurse; M: mean; MD: medical doctor; MS: multiple sclerosis; n.s.: non‐significant; PSS: palliative support service (intervention); RN: registered nurse; SD: standard deviation; SE: standard error; VA: Veterans Affairs. aStandard errors of estimates were based upon multiple regression analyses adjusted for sample differences. In calculating total per patient utilisation, the authors multiplied the utilisation per study day by the "average" number of study days (50) for hospice patients (intervention group). bStandard errors of the estimates were based upon the logistic regression equation adjusted for sample differences.
Informal care
Three studies compared the effect of home palliative and usual care on the support provided by informal caregivers. Although authors reported group differences in the hours of informal care provided (higher in the control group in Higginson 2009 and in the community‐based intervention group in Greer 1986) and no difference in the number of days families took off work during the study period to support their relative at home (median zero days in both groups in Axelsson 1998), none of the three studies reported statistical significance (Table 74). Hence the evidence about the effect on informal care remained inconclusive.
72. Informal care.
| Study | Analysis | Time horizon | Significance and direction | Details |
|
Higginson 2009 UK (high quality) |
Forwards from enrolment | 12 weeks following enrolment |
Care by informal caregiver authors stated increased care by informal caregivers in control group but statistical significance was not stated "The control care patients were more likely (...) to receive help from family/friends" (Higginson 2009) |
Care by informal caregiver Intervention: 15/23 (65%) received; M 152.5 contacts (SD 53.7) Control: 16/21 (76%) received; M 151.1 contacts (SD 57.7) |
|
Axelsson 1998 Sweden |
Forwards from enrolment | During study period |
Next of kin off work authors stated there were no differences but statistical significance was not stated "We found no differences between the study group and the reference group concerning the number of family members' days off work needed to support the cancer patient at home, the reason probably being that the majority of spouses were retired" (Axelsson 1998) |
Next of kin off work Intervention: median 0 days (range 0 to 12) Control: 0 days (range 0 to 0) |
|
Greer 1986 (CBA) |
Backwards from death | Not stated |
Hours of direct care help from primary care person authors stated increased hours of direct care by primary care person in community‐based intervention but statistical significance was not stated "Hours of direct care provided the patient was significantly higher for HC patients than either HB or CC patients. (Greer 1986) |
Adjusted estimatesa Hours of direct care help from primary care person (categorised from 0 to 6; 0 = least) measured at 3 weeks to death Community‐based home hospice care: M 4.01 (SE 0.19) Hospital‐based home hospice care: M 2.95 (SE 0.27) Conventional care: M 2.27 (SE 0.34) measured at 1 week to death Community‐based home hospice care: M 4.16 (SE 0.20) Hospital‐based home hospice care: M 3.02 (SE 0.25) Conventional care: M 2.82 (SE 0.28) |
CC: conventional care (control); HB: hospital‐based (hospital‐based intervention); HC: home‐based care (community‐based intervention); M: mean; SD: standard deviation; SE: standard error.
aStandard errors of the estimates based on a multiple regression equation adjusted for sample differences.
Caregiver post‐bereavement healthcare use and absenteeism
Despite no evidence from trials, Greer 1986 found that few caregivers (4%) reported increased absenteeism from work in the first 90 to 120 days after the patient died, with no statistically significant differences among settings. Greer stated there were no differences in caregiver post‐bereavement morbidity during the same time period, that is hospitalisation and physician visits, but statistical significance was not reported (Table 75).
73. Caregiver post‐bereavement healthcare use and absenteeism from work.
| Study | Measure | Analysis | Time horizon | Significance and direction | Details |
|
Greer 1986 (CBA) |
1) Physician visits after the patient died (score: from 0 to 4+, 0 = none; caregiver report) 2) Hospitalisation after the patient died (yes/no; caregiver report) 3) Absenteeism from workafter the patient died (yes/no; caregiver report) |
Forwards from death | First 90‐120 days following death |
Physician visits and hospitalisation Authors stated there were no differences but statistical significance was not stated "no difference in morbidity, i.e. hospitalization, physician visits (…) during the bereavement period" (Greer 1986) Absenteeism from work n.s. "Few PCPs (4%) reported increased absenteeism from work (…), with no statistically significant differences among settings" (Greer 1986) |
Adjusted estimatesa Physician visits Community‐based intervention: M 1.35 (SE 0.17) Hospital‐based intervention: M 1.25 (SE 0.22) Control (conventional care): M 0.95 (SE 0.28) Hospitalisation Community‐based intervention: 6% (SE 0.01) Hospital‐based intervention: 6% (SE ‐0.01) Control (conventional care): 5% (SE 0.02) Absenteeism from work Descriptive data not provided |
CBA: controlled before and after study; M: mean; n.s.: non‐significant; SE: standard error. aStandard errors of the estimates based on a multiple regression equation for interval‐scale variables and logistic regression equation for dichotomous variables adjusted for sample differences.
Medication and other resources
Greer 1986 provided the only report comparing home palliative care to usual care in terms of medical treatments. A detailed analysis of analgesic treatment was carried out with a subsample of 181 patients (Table 76). The authors found increased prescription (P value < 0.01) and usage (P value < 0.05) of analgesics in the last week before death in the hospital‐based intervention compared to the community‐based intervention and conventional care groups (differences did not reach statistical significance at three weeks to death); they also found increased oral route administration (P value = 0.05) and reduced pro order consumption (P value = 0.03) in both intervention groups compared to conventional care. No statistically significant differences were found in levels of analgesic use and daily oral morphine equivalent consumption. In addition, analysis of the use of aggressive interventions (radiotherapy, surgery, chemotherapy or hormonal therapy and thoracentesis) over the last two weeks before death found all except thoracentesis were less frequently used in the intervention groups (P value < 0.01). A significantly reduced use of diagnostic tests (blood tests, x‐rays or scans) and respiratory support interventions (oxygen and respiratory therapy) was also reported. Finally, examination of the use of palliative radiotherapy in two clinical profiles for which there was consensus for the rationale regarding its administration found reduced use in intervention groups among 311 participants with primary brain cancer or brain metastases (P value < 0.001) and no statistically significant group differences among 314 participants with bone metastases or bone pain.
74. Medication and other resources.
| Study | Analysis | Time horizon | Significance and direction | Details |
|
Higginson 2009 UK (high quality) |
Forwards from enrolment |
12 weeks after enrolment | Differences and statistical significance not stated |
Palliative care nurse Intervention: 9 (39%) received; M 3.0 (SD 1.5) Control: 0 received Other nurse Intervention: 7 (30%) received; M 40.0 (SD 63.8) Control: 7 (33%) received; M 95.0 (SD 79.6) Specialist (ward) Intervention: 5 (22%) received; M 1.0 (SD 0.0) Control: 7 (33%) received; M 9.6 (SD 12.1) Specialist (other) Intervention: 4 (17%) received; M 1.1 (SD 0.3) Control: 5 (24%) received; M 1.0 (SD 0.0) Occupational therapist/physiotherapist Intervention: 16 (70%) received; M 10.6 (SD 9.9) Control: 14 (67%) received; M 22.5 (SD 47.7) Dietician/chiropodist Intervention: 12 (52%) received; M 3.5 (SD 2.5) Control: 13 (62%) received; M 2.6 (SD 1.3) Day centre Intervention: 5 (22%) received; M 20.2 (SD 21.0) Control: 5 (24%) received; M 20.4 (SD 15.9) Respite care Intervention: 2 (9%) received; M 9.5 (SD 0.7) Control: 5 (24%) received; M 10.0 (SD 5.9) |
|
Grande 1999 UK |
Backwards from death |
Last 2 weeks before death |
Other primary and secondary care authors stated no differences but statistical significance not stated |
Other primary and secondary care "Past analysis has also shown that the CHAH and control groups did not differ in the amount of input from any other primary or secondary care service in the final 2 weeks of life" (Grande 2000, Grande 1999) |
|
Bakitas 2009 US (high quality) |
Forwards from enrolment |
During study period |
Referral to palliative care n.s. P value = 0.34 |
Referral to palliative care Intervention: 34/145 (23.4%) Control: 39/134 (29.1%) |
|
Aiken 2006 US |
Forwards from enrolment | During study period |
Managed Care Organization (MCO) case manager assigned n.s. Chi2 2.36 P value = 0.12 |
MCO case manager assigned Intervention: 51% Control: 62% |
|
Zimmer 1985 US |
Backwards from death |
Last 2 weeks before death |
Ambulance/chairmobile rides differences and statistical significance not stated |
Ambulance/chairmobile rides Intervention (n = 21): 0.1 Control (n = 12): 0.6 Note: not clear if the figures are means or medians |
|
Hughes 1992 US |
Forwards from enrolment |
6 months following enrolment |
Extended care days n.s. t ‐1.0 |
Extended care days Intervention (n = 86): M 0.38 (SD 3.6) Control (n = 85): M 0.0 (SD 0.0) |
|
Greer 1986 (CBA) |
Backwards from death | 24‐hour period at 3 weeks to death |
Analgesics Prescribed and taken n.s. "The direction of the relationship is similar [to measure taken at one week to death] but not statistically significant" (Goldberg 1986, Greer 1986) |
Analgesics Subsample of 181 patients: 59 patients in community‐based intervention; 46 in hospital‐based intervention and 76 in conventional care (control) Prescribed and taken: Community‐based intervention: 76.7% prescribed; 69.4% took the analgesics prescribed Hospital‐based intervention: 85.3% prescribed; 76.5% took the analgesics prescribed Conventional care (control): 75.5% prescribed; 68.3% took the analgesics prescribed |
| 24‐hour period at 1 week to death |
Analgesics Prescribed and taken: increased analgesics prescription and uptake in hospital‐based intervention than in community‐based intervention and conventional care P value < 0.01 (prescribed) P value < 0.05 (taken) Level of analgesic use n.s. (see details) "Average" daily OME consumption 'n.s' Increased oral route of analgesic consumption in intervention groups; P value = 0.05 Reduced analgesic consumption on a pro order (i.e. as needed) in intervention groups; P value = 0.03 |
Analgesics Subsample of 181 patients: 59 patients in community‐based intervention; 46 in hospital‐based intervention and 76 in conventional care (control) Prescribed and taken: Community‐based intervention: 66.1% prescribed; 66.1% took the analgesics prescribed Hospital‐based intervention: 91.3% prescribed; 78.3% took the analgesics prescribed Conventional care (control): 69.7% prescribed; 56.6% took the analgesics prescribed Level of analgesic use: "Of those who reported consuming analgesics at the last contact, 42.5% were classified as low, 51.3% consumed an intermediate amount, and only 6.2% were categorized in the high group. There were no statistically significant differences by setting for the level of analgesic consumed" (Goldberg 1986, Greer 1986) "Average" daily OME consumption: Community‐based intervention: 117 mg/day Hospital‐based intervention: 137 mg/day Conventional care (control): 146 mg/day "These differences are not statistically significant due to high variability in the level of consumption among those studied" (Goldberg 1986, Greer 1986) Oral route of analgesic consumption: Community‐based intervention: 90% Hospital‐based intervention: 85% Conventional care (control): 55% Analgesic consumption on a pro order (i.e. as needed): Community‐based intervention: 23% Hospital‐based intervention: 39% Conventional care (control): 51% |
||
| Last 2 weeks before death |
Aggressive interventions reduced use in intervention groups P value < 0.01 Radiotherapy: reduced use in intervention groups; P value < 0.01 Surgery: reduced use in intervention groups; P value < 0.01 Chemo or hormonal therapy: reduced use in intervention groups; P value < 0.01 Thoracentesis: n.s. "receipt of all services but thoracentesis (a procedure employed for draining air or fluid from the space around the lungs) was significantly more likely among conventional care than hospice patients" (Mor 1990, Greer 1986) |
Aggressive interventions Community‐based intervention: 13.9% Hospital‐based intervention: 13.1% Conventional care (control): 37.7% Radiotherapy: Community‐based intervention: 3.8% Hospital‐based intervention: 5.6% Conventional care (control): 13.5% Surgery: Community‐based intervention: 0.6% Hospital‐based intervention: 1.9% Conventional care (control): 6.8% Chemo or hormonal therapy: Community‐based intervention: 7.2% Hospital‐based intervention: 5.4% Conventional care (control): 24.2% Thoracentesis: Community‐based intervention: 4.3% Hospital‐based intervention: 2.9% Conventional care (control): 6.8% |
||
| Last 3 weeks before death |
Diagnostic tests (blood tests, x‐rays, or scans) reduced use in intervention groups 'hospice patients were also significantly less likely to have diagnostic blood tests or X‐rays' (Mor 1990, Greer 1986) |
Adjusted estimatesa Diagnostic tests (blood tests, x‐rays, or scans) Community‐based intervention: 34% (SE 0.03) Hospital‐based intervention: 37% (SE 0.04) Conventional care (control): 64% (SE 0.06) |
||
| Last week before death | Community‐based intervention: 35% (SE 0.03) Hospital‐based intervention: 36% (SE 0.03) Conventional care (control): 62% (SE 0.06) |
|||
| Last 2 weeks before death |
Respiratory support intervention reduced use in intervention groups P value < 0.001 Oxygen: reduced use in intervention groups; P value < 0.001 Respiratory therapy: reduced use in intervention groups; P value < 0.01 |
Respiratory support intervention Community‐based intervention: 32.2% Hospital‐based intervention: 27.2% Conventional care (control): 44.0% Oxygen: Community‐based intervention: 30.0% Hospital‐based intervention: 26.1% Conventional care (control): 42.8% Respiratory therapy: Community‐based intervention: 7.7% Hospital‐based intervention: 5.4% Conventional care (control): 15.3% |
||
| Not stated |
Palliative radiotherapy (sub‐analysis of 2 clinical profiles) Patients with primary brain cancer or brain metastases: reduced use in intervention groups; P value < 0.001 Patients with bone metastases with bone pain: n.s. |
Palliative radiotherapy (sub‐analysis of 2 clinical profiles) Patients with primary brain cancer or brain metastases (n = 311): 'Significantly higher proportion of nonhospice than hospice patients received radiation therapy (P < 0.001). This finding was obtained for both poorly and well‐functioning patients. Among the 192 patients who were functioning poorly (largely bedbound), 30% of nonhospice patients received radiation therapy, as opposed to only 7% of hospice patients' (Mor 1990, Greer 1986) Patients with bone metastases with bone pain (n = 314): 'Of the 314 patients with bone metastases who reported bone pain, there were no statistically significant differences in the proportions of those who received radiation therapy across the 3 groups. Although poorly functioning nonhospice patients were somewhat more likely to receive radiation than their hospice counterparts, this was not true of the best functioning patients. In neither of these cases, however, was the difference statistically significant' (Mor 1990, Greer 1986) |
CHAH: Cambridge hospital at home service; M: mean; n.s.: non‐significant; OME: oral morphine equivalent; SD: standard deviation; SE: standard error. aStandard errors of the estimates based on a logistic regression equation adjusted for sample differences.
Six RCTs compared the effect of home palliative care to usual care on other resources. There was limited evidence showing no statistically significant differences in referrals to palliative care (Bakitas 2009), assignment of case manager (Aiken 2006) and extended care days (Hughes 1992). Grande 1999 reported that intervention and control groups did not differ in the amount of input from primary and secondary care other than general practitioner (GP) and home nursing in the last two weeks before death (statistical significance not stated). Higginson 2009 and Zimmer 1985 measured the use of a range of other resources (including occupational therapy, day centre, respite care and ambulance/chairmobile rides) but statistical tests for differences were not performed (Table 76).
Costs and cost‐effectiveness
Six studies (five RCTs and one CBA including 2047 patients and 1678 caregivers, all considered high quality economic evaluations) compared the impact on the total care costs of receiving home palliative care as opposed to usual care, alongside an evaluation of clinical effectiveness. Together, the RCTs analysed data related to 590 patients (samples ranged from 33 to 297 patients), adding to 1754 patients in Greer 1986. All studies measured institutional and non‐institutional costs, three included medication costs and one calculated the costs associated with informal care (Higginson 2009). Details of methods for calculating costs are provided in Table 61.
In terms of costs, all six studies reported lower costs in the intervention groups with differences ranging from 18% to 35% except Greer 1986 where the costs under the hospital‐based intervention were 2% lower than conventional care as opposed to 32% lower under the community‐based intervention. Notwithstanding, differences were statistically significant only in Brumley 2007 (a high quality RCT and the study with the largest sample size and only slightly underpowered by three participants as planned by authors to detect differences in costs). Differences in total costs were statistically non‐significant in Higginson 2009 and Hughes 1992, although the existence of economically significant differences cannot be ruled out due to small sample sizes unlikely to have sufficient power to detect statistical significance (mean costs per patient in the intervention group were 29% lower in Higginson 2009 and 18% lower in Hughes 1992, compared to usual care). Statistical significance was not reported in Greer 1986, Tramarin 1992 and Zimmer 1985.
In terms of clinical effectiveness, four studies found significantly better outcomes with the intervention (increased probability of death at home and participant's ability to stay at home as long as wanted, reduced probability of death in hospital, decreased symptom burden, pain and caregiver burden, higher satisfaction with care and better quality of death). However, they all also reported null results on other outcomes. Furthermore, Hughes 1992 reported a statistically significant negative intervention effect on caregiver morale at six months from enrolment and Greer 1986 found significantly higher caregiver burden over the last weeks of the patient's life in the group receiving the community‐based intervention. The higher frequency of deaths at home in the intervention group in Zimmer 1985 failed to reach statistical significance, although a clinically significant difference cannot be ruled out (OR 2.86, 95% CI 0.78 to 10.53 in a sample of 43 patients; Analysis 1.1). It is also unclear if the group differences in quality of life observed in Tramarin 1992 reached statistical significance.
The six studies provide inconclusive evidence regarding the cost‐effectiveness of home palliative care compared to usual care. In two studies, the data showed that the intervention was cost‐effective (Brumley 2007 with 297 patients and Higginson 2009 with 50 patients). In the study by Brumley 2007 in the US, home palliative care was more effective than usual care in some outcomes and equally effective in others. and saved costs; in the study by Higginson 2009 in the UK, the intervention was also more effective in some outcomes and equally in others, with no difference in costs (Table 11). These were both RCTs grading high quality according to EPOC criteria (Figure 2) and are the most recent studies of the six. To account for the right‐skewness in cost data, Brumley 2007 used ordinary least squares regression to analyse total costs and Higginson 2009 used bootstrapping to produce 95% CIs around the cost differences between the groups. Furthermore, Higginson 2009 plotted cost‐effectiveness planes for two of their outcomes: overall patient palliative care outcomes and caregiver burden. These planes plot costs against outcomes forming four‐quadrants to visualise if the intervention has better outcomes and higher costs, better outcomes at lower costs, worse outcomes at higher costs or worse outcomes but at lower costs. Higginson 2009 accounted for uncertainty around the cost‐effectiveness estimates by generating 1000 resamples using bootstrapping and computing cost and outcome differences for each, which were then plotted on the cost‐effectiveness planes. The point estimates in the planes suggest that the intervention was cost saving, with equivalent outcomes on overall palliative care outcomes and improved outcomes for caregiver burden. The authors conducted a sensitivity analysis testing different imputation methods for dealing with missing data (last value carried forward, next value carried backwards, and mean value), reporting similar results in nonimputed and imputed data, for all imputation methods.
It is unclear whether the intervention was cost‐effective in the other four studies. Tramarin 1992 calculated a summary cost‐effectiveness measure for a subsample of 39 more advanced AIDS patients ("average" cost‐effectiveness ratio reported in 1990 USD was USD482 per well‐week in intervention group and USD791 in control group). However, the statistical significance of this difference was not reported, there was no measure of uncertainty (e.g. 95% CIs) around the estimates (overall sample size was of 39 patients), and calculation of more appropriate incremental ratios was not possible from the data presented. The results are therefore difficult to interpret. Zimmer 1985 did not report on the statistical significance of the differences in costs they found among 33 patients. Hughes 1992 found no statistically significant differences in costs and showed both positive and negative results on outcomes for 171 patients and their caregivers. Greer 1986 reported that the total costs per study day were "substantially lower" in the community‐based intervention than in the hospital‐based intervention and conventional care (with the latter two being "comparable") but provided no details of statistical significance, adding to positive, negative and null results on a wide range of outcomes.
Six studies calculated disaggregated costs (five RCTs and one CBA, Table 77). Rabow 2004 found no statistically significant differences in the medical care centre charges incurred during the study period, both aggregated and disaggregated (clinic visits, urgent care visits, ED visits, inpatient services and other charges). In contrast, Hughes 1992 found that the institutional costs incurred during six‐month follow‐up were 38% lower in the intervention group than in usual care (1985; USD2342 and USD3757, respectively; P value = 0.05). However, this reduction in inpatient costs was nearly offset by the increased home care costs, which in the intervention group were more than double that of the control group (USD1001 and USD343, respectively; P value < 0.0001). Inpatient costs per study day in Greer 1986 (study period standardised to 50 days) were also significantly higher in conventional care than in either the community‐based or hospital‐based intervention groups, and so were physician costs. Inpatient costs per study day (1982) were USD135 (SE 11.6), USD46 (SE 8.8) and USD99 (SE 9.6), respectively; physician visit costs per study day were USD18 (SE 1.5), USD9 (SE 1.7) and USD8 (SE 1.9), respectively. The costs with home care were USD6 (SE 1.1), USD54 (SE 4.5) and USD46 (SE 8.8), respectively. Greer stated that the observed differences in home care costs were not large enough to counterbalance the large inpatient cost difference; yet, statistical significance was not reported. Three RCTs provided further descriptive data on disaggregated costs for the intervention and control but with no statistical comparisons of the groups (Higginson 2009; Tramarin 1992; Zimmer 1985).
75. Disaggregated costs.
| Study | Analysis | Time horizon and currency | Significance and direction | Details |
|
Rabow 2004 US |
Forwards from enrolment | Study period currency: USD, date not stated (date when study was conducted also unknown) |
All medical centre services charges n.s. t 0.25; P value = 0.80 Clinic visits n.s.; t ‐0.34; P value = 0.73 Urgent care visits n.s.; t ‐1.06; P value = 0.29 ED visits n.s.; t ‐1.01; P value = 0.32 Inpatient services n.s.; t 0.01; P value = 0.10 Other charges n.s.; t 0.13; P value = 0.89 |
All medical centre services charges Intervention (n = 50): M USD47,211 (SD 73,009) Control (n = 40): M USD43,338 (SD 69,647) Clinic visits: Intervention (n = 50): M USD7311 (SD 10,880) Control (n = 40): M USD8068 (SD 9055) Urgent care visits: Intervention (n = 50): M USD749 (SD 2210) Control (n = 40): M USD1342 (SD 2909) ED visits: Intervention (n = 50): M USD754 (SD 1138) Control (n = 40): M USD1313 (SD 3281) Inpatient services: Intervention (n = 50): M USD31,294 (SD 54,285) Control (n = 40): M USD31,225 (SD 66,611) Other charges: Intervention (n = 50): M USD1619 (SD 7973) Control (n = 40): M USD1427 (SD 4714) "Although analysis of cost data is preferable, we were able only to acquire data on charges using the medical center's computerized billing system" (Rabow 2004) |
|
Higginson 2009 UK |
Forwards from enrolment | 12 weeks following enrolment Currency: 2005 GBP |
Statistical significance not stated (descriptive data only) |
District/practice nurse Intervention: M GBP224 (SD 420) Control: M GBP398 (SD 922) MS nurse Intervention: M GBP33 (SD 62) Control: M GBP13 (SD 22) Palliative care nurse Intervention: M GBP46 (SD 72) Control: M GBP0 (SD 0) Other nurse Intervention: M GBP451 (SD 1573) Control: M GBP922 (SD 2078) General practice Intervention: M GBP48 (SD 87) Control: M GBP68 (SD 96) Specialist (home) Intervention: M GBP93 (SD 258) Control: M GBP0 (SD 0) Specialist (hospital) Intervention: M GBP29 (SD 44) Control: M GBP78 (SD 76) Specialist (ward) Intervention: M GBP18 (SD 37) Control: M GBP260 (SD 707) Specialist (other) Intervention: M GBP16 (SD 39) Control: M GBP19 (SD 39) Occupational therapist/physiotherapist Intervention: M GBP290 (SD 425) Control: M GBP389 (SD 897) Dietician/chiropodist/ dentist Intervention: M GBP41 (SD 65) Control: M GBP33 (SD 29) Speech therapist Intervention: M GBP16 (SD 58) Control: M GBP25 (SD 122) Social services Intervention: M GBP69 (SD 152) Control: M GBP46 (SD 89) Informal caregivers Intervention: M GBP2288 (SD 2254) Control: M GBP2620 (SD 2247) Day centre Intervention: M GBP110 (SD 321) Control: M GBP115 (SD 290) Inpatient centre Intervention: M GBP906 (SD 3173) Control: M GBP2377 (SD 6265) Respite care Intervention: M GBP39 (SD 137) Control: M GBP110 (SD 255) |
|
Zimmer 1985 US |
Backwards from death | Last 2 weeks before death currency: USD, date not stated (study conducted in 1979‐1982) |
Statistical significance not stated (descriptive data only) "although the standard costs 'weight' of $300 was used in this analysis for all hospital days, the actual charges per day, taken from the hospital bills of those who were hospitalized, was higher for control than for team patients" (Zimmer 1984, Zimmer 1985) |
Mean costs per patient of last 2 weeks before death Hospital costs Intervention (n = 21): USD942 Control (n = 12): USD1824 Intervention as % of control: 52% Mean actual hospital charges per day of patients hospitalised during the last 2 weeks before death Intervention (n = 5): M USD282; median USD292 Control (n = 6): M USD347; median USD313 Total out‐of‐home costs Intervention (n = 21): USD946 Control (n = 12): USD1847 Intervention as % of control: 51% Total in‐home costs Intervention (n = 21): USD631 Control (n = 12): USD446 Intervention as % of control: 141% |
|
Hughes 1992 US |
Forwards from enrolment | 6 months following enrolment currency: 1985 USD |
Institutional VA hospital increased in control group; t 2.47; P value = 0.02 Private hospital t < 1; "n.s." Total hospital costs increased in control group; t 2.09; P value = 0.04 Total institution costs increased in control group; t 1.99; P value = 0.05 Non‐institutional Outpatient clinic increased in control group; t 2.76; P value = 0.01 HBHC (intervention) intervention difference (tests not performed) Community nursing increased in control group; t 4.86; P value < 0.01 Total home care costs increased in intervention group; t ‐5.10; P value < 0.01 Total VA costs t < 1; "n.s." Total non‐VA costs t < 1; "n.s." |
Institutional VA hospital Intervention (n = 86): M USD1795.07 Control (n = 85): M USD3434.38 Private hospital Intervention (n = 86): M USD457.56 Control (n = 85): M USD289.68 Total hospital costs (VA and private) Intervention (n = 86): M USD2251.25 Control (n = 85): M USD3724.06 Total institution costs (all hospital and nursing home) Intervention (n = 86): M USD2341.79 Control (n = 85): M USD3757.37 Non‐institutional Outpatient clinic Intervention (n = 86): M USD26.46 Control (n = 85): M USD100.42 HBHC (intervention) Intervention (n = 86): M USD999.28 Control (n = 85): ‐ Community nursing Intervention (n = 86): M USD1.97 Control (n = 85): M USD343.29 Total home care costs (HBHC plus community nurse) Intervention (n = 86): M USD1001.24 Control (n = 85): M USD343.29 Total VA costs Intervention (n = 86): M USD2934.52 Control (n = 85): M USD3602.37 Total non‐VA costs Intervention (n = 86): M USD544.84 Control (n = 85): M USD646.31 "The average general bed costs for HBHC was USD 1,310 as compared to USD 2,807 for controls (t=3.26, df=169, p<0.02)" (Hughes 1992) |
|
Tramarin 1992 Italy |
Forwards from enrolment | 1 year (calculated by multiplying resources used in the 6 months following enrolment by 2) currency: 1990 ITL (million) and 1990 USD (converted from ITL using healthcare‐specific purchasing power parities) |
Statistical significance not stated (descriptive data only |
Inpatient care Intervention:
Control:
Outpatient care Intervention:
Control:
Home care (intervention) Intervention:
Control:
"Analysis of cost distribution revealed that personnel salaries accounted for 71 and 19.9% of the total expenditure of the inpatient and outpatient clinics, respectively, for both groups. In the outpatient clinic, most expenses were associated with direct care of patients. Diagnostic examinations and therapy accounted for 48.5% and zidovudine for a further 29.5%" (Tramarin 1992) |
|
Greer 1986 (CBA) |
Forwards from enrolment | Study period currency: 1982 USD |
Inpatient costs reduced in intervention groups "Inpatient and physician costs per study day were significantly higher in CC than in either HC or HB settings" (Greer 1986) Home care costs statistical significance not stated Physician visit costs reduced in intervention groups (see above) Outpatient costs statistical significance not stated Drugs, supplies and equipment expenditures statistical significance not stated |
Inpatient costs Community‐based intervention: USD46 (SE 8.8) Hospital‐based intervention: USD99 (SE 9.6) Control (conventional care): USD135 (SE 11.6) Home care costs Community‐based intervention: USD54 (SE 4.5) Hospital‐based intervention: USD46 (SE 4.9) Control (conventional care): USD6 (SE 1.1) "Home care costs per study day in CC were approximately 10% of hospice costs"; "HC patients had more home visits than HB patients, but the difference in home care costs per day was not large enough to counterbalance the large inpatient cost difference" (Greer 1986) Physician visit costs Community‐based intervention: USD9 (SE 1.7) Hospital‐based intervention: USD8 (SE 1.9) Control (conventional care): USD18 (SE 1.6) Outpatient costs Community‐based intervention: USD1.8 (SE 0.69) Hospital‐based intervention: USD1.2 (SE 0.75) Control (conventional care): USD3.0 (SE 0.84) Drug, supplies and equipment expenditures Community‐based intervention: USD1.8 (SE 0.51) Hospital‐based intervention: USD0.7 (SE 0.56) Control (conventional care): USD0.1 (SE 0.60) Note: not clear if the figures are means or medians "Inpatient utilization increased as death approached in each of the systems of care [graphs provided]. Home service use increased dramatically in the last week of life only in the HC sample; during the last week of life, HC patients received an average of one home service visit per day in contrast to one per week for CC and 3.5 per week for HB patients" (Greer 1986) |
CBA: controlled before and after study; CC: conventional care (control); CI: confidence interval; ED: emergency department; GBP: British pound; HBHC = hospital‐based home care (intervention); HC: home‐based care (community‐based intervention); HB: hospital‐based (hospital‐based intervention); ITL: Italian lira; M: mean; n.s.: non‐significant; SD: standard deviation; SE = standard error; USD: United States dollar; VA: Veteran Affairs.
Discussion
Summary of main results
Three decades of research on the effectiveness of home palliative care have resulted in clear evidence of the benefit of home palliative care in helping patients to die at home and reducing symptom burden without impacting on caregiver grief. Meta‐analyses (of seven trials with 1222 patients, including three high quality RCTs) showed that home palliative care services more than double the odds for patients with illnesses such as cancer, CHF and COPD to die at home. In addition, narrative synthesis showed evidence of small but statistically significant positive effects on the symptom burden people experience as a result of having an advanced illness (based on three trials, of which two were high quality RCTs, and one CBA with 2107 patients), and of no effect on caregiver grief (based on three RCTs, of which two were high quality, and one CBA with 2113 caregivers). The review also showed there are areas of greater uncertainty where there is conflicting or inconclusive evidence (e.g. pain control, satisfaction with care and cost‐effectiveness). Occasional findings of negative effects on caregiver morale and burden and of positive effects from reinforcing home palliative care services with a specific component of caregiver support are important.
Overall completeness and applicability of evidence
All 23 studies were conducted in high‐income countries. Eleven were from the US and five from the UK. Most interventions served urban and suburban populations. A large majority of people had cancer with median/mean ages ranging from 53 to 77 years. Although sicker patients were likely to be excluded or drop‐out (only two studies were able to follow‐up ≥ 80% on all outcomes analysed) and current practice varies internationally (e.g. on when patients are introduced to palliative care and the format of services), these characteristics match roughly the profile of patients seen routinely in home palliative care/hospice care services in the UK and the US (NHPCO 2012; NCPC 2012); hospice care patients in the US are slightly older and present more frequently with a non‐malignant condition. We therefore believe the external validity to these regions is acceptable. However, the evidence failed to cover middle‐income and low‐income countries, where there is a greater unmet need for care to support people with advanced illness at home. Contextual and cultural factors, as well as health system characteristics are, however, likely to vary. For example, in sub‐Saharan Africa. the resources and clinical supervision needed to sustain quality care are often lacking and referrals and coverage are major problems, but services and research are developing and the integration of palliative care into the well‐established model of home care within HIV/AIDS is promising (Harding 2005; Downing 2010).
Attention should be given to the fact that the majority of the studies were conducted more than 10 years ago, some in the 1970s and 1980s. Although the principles of palliative care and the aims of home palliative care services have remained virtually the same (Saunders 2000), aspects of service provision have changed throughout the years, incorporating adaptations to fit reorganisations in health systems, expanding to earlier stages of illness, and improving practice in symptom management as better ways of treatment are discovered. This may partially explain the more positive findings of recent studies (Brumley 2007; Bakitas 2009; Higginson 2009). Also, the profiles of patients and caregivers have changed and are expected to change further in the future. The studies under‐represented portions of the society that are expected to become more relevant to palliative care in the context of ageing populations. Namely, 10 studies excluded people with no caregiver and a minority of patients (ranging from 12% to 43%) lived alone.
The expression of results in NNTBs applied to populations with low, middle and high home death rates aimed to produce more easily interpretable statistics and enhance the applicability of the evidence to practice and service planning. Readers should be aware that the results were achieved in a study population with a medium home death rate (307 home deaths/1000 deaths) in the control groups receiving usual care. A degree of preference and acceptance to be cared for at home is implicit in consenting to participate in studies evaluating home palliative care and may determine this rate.
Quality of the evidence
The body of evidence has methodological limitations. Most of these derived from the complex ethical and practical challenges of conducting evaluative research with people with advanced illness and their caregivers; the challenges identified are aligned with previous literature (Grande 2000; Rinck 1997; Zimmermann 2008) and have been thoroughly discussed in methodological papers by the authors of four trials (Higginson 2009; Jordhøy 2000; McMillan 2007; McWhinney 1994). Loss to follow‐up and attrition bias are among the most problematic aspects to deal with because although most of the times the cause is 'natural' in palliative care (i.e. death), a high level of attrition jeopardises the study's ability to produce enough data to conduct a powered analysis (which increases the chances of not detecting a significant difference when there is one).
Cluster and fast‐track trials responded well to some of the problems posed by randomisation in trials of home palliative care services but these designs have also their own limitations (e.g. recruitment bias due to difficult concealment of cluster allocation and limited time for comparison before the control group is offered the intervention, respectively). Blinding of participants is deemed unfeasible by the nature of the intervention and the controls; blinding of researchers is difficult to maintain throughout the trial, particularly when they are involved in the prospective collection of data from patients and caregivers on satisfaction with care and resource use information (as they are asked what services they get). Unless there is an assessment of the extent to which blinding is maintained throughout the study, blinding for a complex intervention should be regarded cautiously (Farquhar 2009). In addition, baseline differences in seven trials (particularly evident in CCTs where it is clearer they favoured the intervention group) suggest selection bias and weaken findings. However, the CCTs approximated more to the circumstances of services in the real world than the RCTs, as the criteria used for allocation (preference and proximity to services) are often used in practice.
There were issues around the measurement of outcomes and resource use. A wide variety of measures were used that limited comparisons and meta‐analysis. The use of caregivers as proxies and retrospective assessments were alternatives when patient reports were not feasible, particularly at time points closer to death. These methods have limitations (Addington‐Hall 2001b; McPherson 2003; Tang 2002; Teno 2005, e.g. caregiver over‐estimation of symptoms compared to patient reports and moderate correlations between the two as found in McMillan 2007), although it would be expected that these apply equally to the intervention and control group, hence having minimal impact on group comparisons.
Despite challenges, the amount of evidence (23 studies with 37,561 patients and 4042 caregivers), the methodological quality championed by the six RCTs that met the Cochrane EPOC Review Group strict criteria (followed closely by six other trials), and the high consistency of findings (across ≥ 75% of studies) determined the existence of strong evidence on our primary outcome (death at home), symptom burden and caregiver grief and of moderate evidence on a few other outcomes important to patients and caregivers facing an advanced illness. Having found consistent results observed by different researchers in different places with different samples strengthens the likelihood of the finding to be true (Bradford Hill 1965).
It is noted that although nine studies measured the effect of home palliative care on death at home, others did not plan to examine this outcome or had few deaths to detect a difference ‐ they may or may not have had an effect on death at home beyond the study period. We also note that although the evidence on cost‐effectiveness was inconclusive, all economic evaluations which compared total care costs reached high quality as per the BMJ's 35‐item checklist (Drummond 1996) and that in general a comprehensive range of resources was measured across studies. Nevertheless, we urge some caution when interpreting quality scores. Using a cut point of 60% to consider an economic evaluation of high quality (following the system proposed by Gonzalez‐Perez 2002) obscured variation between studies, which becomes clearer in the detailed assessment of each of the 35 quality criteria of the BMJ checklist (Drummond 1996) in Figure 3. This showed that there are aspects which were less than perfect such as the measurement and valuing of productivity changes (important for home palliative care as family caregivers may be required to be absent from work to help care for their relative at home), although the choice of appropriate measurement methods remains controversial (Brunetti 2003). The reporting of imprecision such as 95% CIs and statistical significance is another pitfall, although this would have been unusual or exceptional at the time some of the studies were reported.
A word of caution is needed regarding inconclusive and conflicting findings and when there was evidence of no effect. This was found in critical areas of the effectiveness and cost‐effectiveness of home palliative care services based on narrative synthesis (more opened to interpretation than meta‐analysis). Often this happened because a large number of studies failed to detect statistically significant differences and some did not report on statistical significance. Such is the case with evidence comparing home palliative care with usual care on pain control and on patients' psychological well‐being. Statistically significant positive effects were rare: they were found in Grande 1999, Higginson 2009 and Greer 1986 among nine studies on pain and in Bakitas 2009 and Rabow 2004 among 11 studies on psychological well‐being. We cannot be sure that the non‐significant findings from a large number of trials mean that the services made no difference to these outcomes (Altman 1995; Tarnow‐Mordi 1999), although in some instances clinically or economically significant differences could be ruled out (e.g. for caregiver grief). Moreover, all studies that conducted sample size calculations failed to reach the planned numbers. Most studies (12 out of 23) examined post‐intervention assessments of fewer than 120 participants. Trials of this size lack the power to detect medium‐sized treatment effects and carry a considerable risk of false negatives (Cohen 1992; Tarnow‐Mordi 1999). Wide CIs indicate considerable uncertainty and lack of study power to detect differences (Altman 1995), but these were rarely provided in studies (although recommended in the CONSORT [Consolidated Standards of Reporting Trials] statement) (Schulz 2010). There is also an added risk that some of the findings may have occurred by chance as several studies conducted multiple statistical tests on a wide range of outcomes and the primary were poorly defined.
Potential biases in the review process
Only one review author conducted the initial screening of abstracts and applied the inclusion/exclusion criteria to produce a list of 608 potentially eligible studies. Two reviewers independently assessed these records for eligibility, extracted data and assessed the methodological quality. Two of the review authors (PMcC and IJH) were investigators in one of the included studies (Higginson 2009); although this represented potential for bias in the quality assessment (the study was considered of high quality), we used transparent criteria and the assessment was independently carried out by different review authors (BG/NC). The use of arbitrary cut points for considering studies and economic evaluations of high quality introduced subjectivity and it is possible that the use of more stringent cut points would lower the strength of the evidence on some outcomes. This would have minimal impact on the results of our primary outcome but could affect the findings on symptom burden and caregiver grief, for example (where the evidence was graded strong based on narrative synthesis without meta‐analysis). It should be noted that we did not pursue data retrieval from authors on secondary outcomes and on cost‐effectiveness where the evidence was too heterogeneous to perform meta‐analysis. We identified two Korean trials (Hwang 2009; Park 2011) which are pending classification as we wait for the authors' reply to decide eligibility. Furthermore, there are six ongoing studies eligible for inclusion (Abernethy 2006 in Australia, Allen 2012 in the US, Battaglia 2012 in Italy, Butler 2012 in the UK, Chvetzoff 2006 in France and Duursma 2011 in the Netherlands). These will be included in future updates.
Agreements and disagreements with other studies or reviews
We added 11 new studies on home palliative care (including six RCTs, three CCTs and two other studies) to the ones found in two systematic reviews of palliative care services (searches conducted in 2000 and 2008) (Higginson 2003; Zimmermann 2008). Tramarin 1992 remains the only full economic evaluation known.
Higginson and colleagues reviewed 44 studies of intermediate and specialist palliative care models, of which 22 were home teams (Higginson 2003). The effect on death at home was described as equivocal, but this may be explained by the fact that the authors analysed palliative care provided in different settings, not just home teams. Meta‐analysis of 19 studies (of six home care models but mainly other types of services) demonstrated small benefits on pain (OR 0.38, 95% CI 0.23 to 0.64) and other symptoms (OR 0.51, 95% CI 0.30 to 0.88). We found too much heterogeneity in the measurement and reporting of these variables (most often reported as ordinal or continuous rather than dichotomised) to undertake meta‐analysis.
Zimmerman and colleagues reviewed 22 RCTs of specialist palliative care models and reported high consistency for a positive effect on satisfaction with care (seven out of 10 RCTs favoured the intervention). Significant positive effects on quality of life and control of specific symptoms were rare (as in our review); the authors discussed the lack of study power to detect statistical differences as well as the use of outcome measures that are non‐specific to palliative care (Zimmermann 2008).
A systematic review of home care for people with incurable cancer (Smeenk 1998b), including home palliative care but also other types of home care models, found unclear results from nine studies on quality of life and time spent in hospital; this is aligned with our findings on evidence for these two outcomes (conflicting for quality of life and inconclusive for time spent in hospital). It would be expected that general home care and home palliative care differ in terms of impact on death at home and other outcomes because of the degree of specialisation in caring for patients at the end of life (advanced training and experience). However, this is difficult to confirm based on indirect comparisons and also because the characteristics of the general home care which is often included in usual care varies.
A Cochrane review of a specific model of home palliative care – hospital at home – found, on the basis of three trials, that patients receiving the intervention were more likely to die at home compared with those receiving usual care (Shepperd 2011). The authors reported a pooled risk ratio (RR) of 1.33 (95% CI 1.14 to 1.55). We added four studies to this meta‐analysis, used a random‐effects model (to account for heterogeneity that was greater in our review as we examined different home palliative care models) but found similar findings; we chose to calculate ORs rather than RRs and included only patients who died within the study period (for whom place of death was known). Due to wide heterogeneity in the reporting and types of models included, we were limited in the indirect comparisons we could make between different models of home palliative care.
Finally, our findings on models of home palliative care reinforced with an extra caregiver support component added no new studies to a systematic review of caregiver interventions in palliative care (Harding 2003; Harding 2011). Harding highlighted positive effects on satisfaction with care in home care models (from two studies) but also evidence of unmet need among caregivers under home palliative care, derived from experimental but also observational and qualitative research.
Authors' conclusions
Implications for practice.
The results provide reliable evidence that home palliative care increases the chance of dying at home and reduces symptom burden in particular for patients with cancer. The effects found are relevant in practice for two reasons. First, the effect on death at home, with a pooled OR of 2.21 and NNTB of 5, is clinically significant; larger, for example, than the beneficial effect of gabapentin for treating neuropathic pain as compared to placebo (NNTB 6 for achieving at least 30% pain relief and NNTB 7 for achieving at least 50% pain relief) (Moore 2011). Increasing the chances of dying at home is not an easy task, with influence by a complex network of factors (Gomes 2006). This is reflected, for example in the rate at which home death rates increase in countries where they are increasing, e.g. 0.4 percentual point per year from 2004 to 2010 in England and Wales despite the existence of a national strategy for end of life care focused on enabling people to die in their place of choice, which for most is home (Gomes 2012a). It is also worth noting that the control groups in our review received a form of 'active comparator' (usual care) not just a placebo (particularly in countries where primary care and home care are well developed), hence comparative effects are expected to be small, as found for symptom burden. Second, although the findings on cost‐effectiveness were inconclusive, even evidence of no effect on other outcomes with slightly higher costs would be enough to justify the existence of home palliative care services as they exist to fulfil the desire of many people to live at home in the last days of their life.
The decision for someone with an advanced illness to start receiving home palliative care should balance the benefits, potential downsides and areas of uncertainty, integrating what matters most to that person and their preferences, as well as the views of caregivers. It is known that there is a minority of people who prefer not to die at home (inpatient hospice is often the second most frequent preference; Higginson 2000); there is also a minority that change their mind as the illness progresses (Gomes 2013). In some circumstances a death at home may not be appropriate. For example, a family may keep a patient at home because of lack of resources, healthcare insurance, access to inpatient beds, or awareness of alternatives. There are also unexpected acute events that make an ED visit or admission inevitable or appropriate (Beynon 2011). This requires the existence of palliative care services in other settings (e.g. in hospitals, inpatient hospices and nursing homes).
Policy makers and service planners can now calculate the extent to which current home palliative care services may need expansion locally on the basis of current and target home death rates, applying NNTB from this meta‐analysis to current and projected local need. Attention should also be given to cultural variations in preferences for dying at home. For example, a recent population survey of 9344 adults across seven EU countries showed that the preference to die at home if faced with advanced cancer varied from 51% in Portugal to 84% in the Netherlands, with country variation unexplained by differences in age and gender distributions (Gomes 2012b). It is possible that differences in preferences relate to local care provision or macro‐social, economic and cultural factors. A recent systematic review of preferences for dying at home reported even more heterogeneity in estimates among studies with patients (Gomes 2013). Improvements to existing home palliative care services should also be informed by an appraisal of the format, components and resources of the different models examined and what people value, particularly those that improved outcomes for patients or caregivers, or both, but also innovative features of home palliative care. Negative effects on caregivers (e.g. caregiver burden) and impact on costs should be carefully monitored.
Implications for research.
This review demonstrates clear benefits of home palliative care in helping patients, particularly those with advanced cancer, to die at home with reduced symptom burden and without impacting on caregiver grief. Further meta‐analyses on symptom burden and caregiver grief would produce more robust data but for this to happen, future studies need to harmonise measurement and reporting practices.
More work is needed to study cost‐effectiveness especially for patients with non‐malignant conditions and their caregivers, assessing place of death and appropriate outcomes that are sensitive to change and valid in these populations, and to compare different models of home palliative care. Shared methodologies across studies would enable examination of outcomes where the evidence is conflicting, inconclusive, limited or suggests no effect. Further primary research should be powered and include a concurrent economic evaluation. New home palliative care interventions must respond to the challenges ahead, posed by rapidly ageing populations with increased complexity and growing need for home palliative care; these are international challenges (Gomes 2008; Gomes 2011). Research in middle‐income and low‐income countries does not yet exist.
A limitation of the evidence found in this review is the heterogeneity in the characteristics of home palliative care interventions and the control interventions called 'usual care'. Some of this heterogeneity relates to differences between countries and contexts but also in the proposed models of home palliative care (e.g. in the US 'hospice care' takes over all care including home nursing whereas UK models of home palliative care are more advisory except in Grande 1999). This must be taken into account and further research must define better the usual care provided locally and what parts of the intervention are likely to produce benefits and what parts are less effective.
What's new
| Date | Event | Description |
|---|---|---|
| 17 July 2022 | Amended | See Published notes. |
History
Protocol first published: Issue 2, 2009 Review first published: Issue 6, 2013
| Date | Event | Description |
|---|---|---|
| 14 March 2016 | Amended | Contact details updated. |
| 10 November 2015 | Review declared as stable | This review will be assessed for further updating in 2017. See Published notes. |
| 19 March 2014 | Amended | Reference added to Other published versions of this review. |
Notes
A search was run in June 2021 for a planned update by the authors, however unfortunately the review authors were unable to revise the review to account for any new studies at this time. Therefore, this review has now been stabilised following discussion with the authors and editors. The review should be re‐assessed for updating in two years if practical. If possible, the review authors, or a new review author team, will update the review before this date if new evidence likely to change the conclusions is published, or if standards change substantially which necessitate major revisions.
In November 2015, the authors and editors agreed to re‐assess this review for updating in 2017. No new studies with the potential to change the conclusions of this review were identified by a recent search (June 2015).
Acknowledgements
We thank Barbara Antunes and Katherine Sleeman for their help with data extraction and quality assessment, Caroline Struthers and Jane Hayes (Trials Search Co‐ordinators) for assistance with the search strategy, Jessica Thomas and Anna Hobson (Managing Editors) for their support throughout the review process. We also thank Phil Wiffen (member of the Editorial Board of the Cochrane PaPaS Review Group) for his help and advice and Anne Lawson (Copy Editor) for proofreading the review. We thank the researchers who provided us with information, references or unpublished data from their studies (Gunn Grande, Marie Bakitas, Susan Enguidanos, Michael Rabow, Xavier Gómez‐Batiste, Penny Feldman and Miriam Ryvicker, Claire Butler, Gisele Chvetzoff, Susan Hazelett, Jeroen Hasselaar and Patrick Hoek, Marilynne Hebert and Tatsuya Morita). We also thank other researchers who provided information in earlier stages of the screening process. We thank Despina Anagnostou, Claudia Bausewein, Hamid Benalia, Justyna Hamada, Eun‐Jeong Lee, Wendy Magee, Hristina Petkova and Gao Wei for their help with the translation of studies in languages other than English. We are grateful to Vera Sarmento for her help when preparing this review for publication. We also thank the three peer‐reviewers for comments which helped improve the review.
Appendices
Appendix 1. MEDLINE search strategy
1. exp Palliative Care/
2. exp Terminal Care/
3. exp Terminally Ill/
4. palliat*.mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier]
5. (terminal* and (care or caring or ill*)).mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier]
6. ((advanced or end stage or terminal*) adj4 (disease* or illness* or cancer* or malignan*)).mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier]
7. (last year of life or LYOL or life's end or end of life).mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier]
8. or/1‐7
9. exp Home Care Services/
10. exp Home Care Agencies/
11. exp Mobile Health Units/
12. exp Community Health Nursing/
13. (home adj4 (hospital or palliat*)).mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier]
14. ((macmillan or marie curie or district) adj nurs*).mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier]
15. ((home or in‐home or domicile or outreach or residential or housing or posthospital or post‐hospital or communit* or mobile or ambulatory or door to door) adj2 (team* or center* or centre* or treat* or care or interven* or therap* or management or model* or program or programs or programme* or service* or base* or nurs*)).mp.
16. (homecare or home‐care or homebased or home‐based).mp. [mp=title, original title, abstract, name of substance word, subject heading word, unique identifier]
17. or/9‐16
18. hospice*.mp.
19. 18 or (8 and 17)
20. (child* or adolescent* or infant* or baby or babies or neonat* or juvenil* or pediatric* or paediatric* or young person* or young people or youth* or young adult* or matern*).ti.
21. 19 not 20
22. clinical trial/ or controlled clinical trial/ or multicenter study/ or randomized controlled trial/
23. (randomized controlled trial or controlled clinical trial or multicenter study).pt.
24. chi‐square distribution/ or chi‐square?.ti,ab.
25. "random*".ab,ti.
26. controlled.ti.
27. trial.ti.
28. Control Groups/
29. (control* adj2 (clinical or group* or trial* or study or studies or design* or method*)).ti,ab.
30. ((multicent* or multi‐cent* or multisite? or multi‐site?) adj (study or studies or trial*)).ti,ab.
31. double‐blind method/ or single‐blind method/
32. ((single or double or triple or treble) adj blind*).ti,ab.
33. or/22‐32
34. (intervention? or multiintervention? or multi‐intervention? or postintervention? or post‐intervention? or preintervention? or pre‐intervention?).ti,ab.
35. intervention.hw.
36. (pre‐post or "pre test*" or pretest* or posttest* or "post test*" or "pre and post").ti,ab,hw.
37. before‐after.ti,ab.
38. (before adj4 after).ti,ab.
39. ("quasi‐experiment*" or quasiexperiment* or "quasi random*" or quasirandom* or "quasi control*" or quasicontrol* or ((quasi* or experimental) adj3 (method* or study or studies or trial or design*))).ti,ab,hw.
40. ("time series" adj2 interrupt*).ti,ab,hw.
41. or/34‐40
42. follow‐up studies/
43. (("follow up" or follow‐up) adj2 (design or study or studies)).ti,ab.
44. pilot projects/
45. pilot.ti. or (pilot* adj3 (program* or project? or study or studies)).ab.
46. comparative study.pt.
47. (comparative and (study or studies)).ti.
48. intervention studies/
49. evaluation studies.pt.
50. evaluat*.ti.
51. or/42‐50
52. 33 or 41 or 51
53. groups.ab.
54. 52 or 53
55. humans.sh.
56. 54 and 55
57. 56 and 21
Appendix 2. PaPaS Trials Register search strategy
hospice* or ((palliat* or terminal* or "end stage") and (home or community or outreach or ambulatory))
Appendix 3. EPOC Group Register search strategy
1. hospice* (all indexed fields)
2. hospice\* (all non‐indexed fields)
3. palliative (abstract)
4. (palliative) AND (home\*) (all non‐indexed fields)
5. (palliative) AND (home\*) (all indexed fields)
6. (Hospice care*) OR (Hospices*) (keywords)
7. (#1 OR #2 OR #3 OR #4 OR #5 OR #6)
Appendix 4. CENTRAL, CDSR, DARE, HTA and NHS EED search strategy
1. MeSH descriptor Palliative Care explode all trees
2. MeSH descriptor Terminal Care explode all trees
3. MeSH descriptor Terminally Ill explode all trees
4. (palliat*):ti,ab,kw
5. (terminal* and (care or caring or ill*))
6. (advanced or end stage or terminal*) near/4 (disease* or illness* or cancer* or malignan*):ti,ab,kw
7. (last year of life or LYOL or life's end or end of life):ti,ab,kw
8. (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7)
9. MeSH descriptor Home Care Services explode all trees
10. MeSH descriptor Home Care Agencies explode all trees
11. MeSH descriptor Mobile Health Units explode all trees
12. MeSH descriptor Community Health Nursing explode all trees
13. (macmillan or marie curie or district) near nurs*
14. (home near/4 (hospital or palliat*)):ti,ab,kw
15. (home or in‐home or domicile or outreach or residential or housing or posthospital or post‐hospital or communit* or mobile or ambulatory or door to door) near/2 (team* or center* or centre* or treat* or care or interven* or therap* or management or model* or program or programs or programme* or service* or base* or nurs*):ti,ab,kw
16. (homecare or home care or home‐care or homebased or home based or home‐based):ti,ab,kw
17. (#9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16)
18. (hospice*):ti,ab,kw
19. (#18 OR ( #8 AND #17 ))
20. (child* or adolescent* or infant* or baby or babies or neonat* or juvenil* or pediatric* or paediatric* or young person* or young people or youth* or young adult* or matern*):ti
21. (#19 AND NOT #20)
Appendix 5. EMBASE search strategy
1. exp palliative therapy/
2. exp palliative nursing/
3. exp cancer palliative therapy/
4. exp terminal care/
5. exp terminal disease/
6. exp terminally ill patient/
7. palliat*.mp
8. terminal* and (care or caring or ill*).mp
9. ((advanced or end stage or terminal*) adj4 (disease* or illness* or cancer* or malignan*)).mp
10. last year of life or LYOL or or end of life.mp
11. or/1‐10
12. exp home care/
13. exp home health agency/
14. exp community care/
15. exp community health nursing/
16. home adj4 (hospital or palliat*).mp
17. (macmillan or marie curie or district) adj nurs*.mp
18. (home or in‐home or domicile or outreach or residential or housing or posthospital or post‐hospital or communit* or mobile or
ambulatory or door to door) adj2 (team* or center* or centre* or treat* or care or interven* or therap* or management or model* or
program or programs or programme* or service* or base* or nurs*).mp
19. homecare or home‐care or homebased or home‐based.mp
20. or/12‐19
21. hospice*.mp
22. 21 or (11 and 20)
23. (child* or adolescent* or infant* or baby or babies or neonat* or juvenil* or pediatric* or paediatric* or young person* or young people or youth* or young adult* or matern*).ti.
24. 22 not 23
25. clinical trial/ or controlled clinical trial/ or multicenter study/ or randomized controlled trial/
26. chi‐square distribution/ or chi‐square?.ti,ab.
27. "random*".ab,ti.
28. controlled.ti.
29. trial.ti.
30. Control Groups/
31. (control* adj2 (clinical or group* or trial* or study or studies or design* or method*)).ti,ab.
32. ((multicent* or multi‐cent* or multisite? or multi‐site?) adj (study or studies or trial*)).ti,ab.
33. double‐blind method/ or single‐blind method/
34. ((single or double or triple or treble) adj blind*).ti,ab.
35. (intervention? or multiintervention? or multi‐intervention? or postintervention? or post‐intervention? or preintervention? or pre‐intervention?).ti,ab.
36. intervention.hw.
37. (pre‐post or "pre test*" or pretest* or posttest* or "post test*" or "pre and post").ti,ab,hw.
38. before‐after.ti,ab.
39. (before adj4 after).ti,ab.
40. ("quasi‐experiment*" or quasiexperiment* or "quasi random*" or quasirandom* or "quasi control*" or quasicontrol* or ((quasi* or experimental) adj3 (method* or study or studies or trial or design*))).ti,ab,hw.
41. ("time series" adj2 interrupt*).ti,ab,hw.
42. follow‐up studies/
43. (("follow up" or follow‐up) adj2 (design or study or studies)).ti,ab.
44. pilot projects/
45. pilot.ti. or (pilot* adj3 (program* or project? or study or studies)).ab.
46. (comparative and (study or studies)).ti.
47. intervention studies/
48. evaluat*.ti.
49. or/25‐48
50. groups.ab
51. 49 or 50
52. human.sh
53. 51 and 52
54. 53 and 24
Appendix 6. CINAHL search strategy
1. MH palliative care
2. MH terminal care
3. MH terminally ill patients
4. TX palliat*
5. TX terminal* and (care or caring or ill*)
6. TX ((advanced or end stage or terminal*) and (disease* or illness* or cancer* or malignan*))
7. TX last year of life or LYOL or life's end or end of life
8. S1 or S2 or S3 or S4 or S5 or S6 or S7
9. MH home health care
10. MH home health agencies
11. MH mobile health units
12. MH community health nursing
13. TX home and (hospital or palliat*)
14. TX (macmillan or marie curie or district) and nurs*
15. TX (home or in‐home or domicile or outreach or residential or housing or posthospital or post‐hospital or communit* or mobile or ambulatory or door to door) and (team* or center* or centre* or treat* or care or interven* or therap* or management or model* or program or programs or programme* or service* or base* or nurs*)
16. TX homecare or home‐care or homebased or home‐based
17. S9 or S10 or S11 or S12 or S13 or S14 or S15 or S16
18. TX hospice*
19. S18 or (S8 and S17)
20. TI (child* or adolescent* or infant* or baby or babies or neonat* or juvenil* or pediatric* or paediatric* or young person* or young people or youth* or young adult* or matern*)
21. S19 not S20
22. MH clinical trials or MH multicenter studies
23. PT clinical trial
24. AB chi‐square? or TI chi‐square?
25. AB "random*" or TI "random*"
26. TI controlled
27. TI trial
28. MH control group
29. AB (control* and (clinical or group* or trial* or study or studies or design* or method*)) or TI (control* and (clinical or group* or trial* or study or studies or design* or method*))
30. AB ((multicent* or multi‐cent* or multisite? or multi‐site?) and (study or studies or trial*)) or TI ((multicent* or multi‐cent* or multisite? or multi‐site?) and (study or studies or trial*))
31. MH triple‐blind studies or MH double‐blind studies or MH single‐blind studies
32. AB ((single or double or triple or treble) and blind*) or TI ((single or double or triple or treble) and blind*)
33. S22 or S23 or S24 or S25 or S26 or S27 or S28 or S29 or S30 or S31 or S32
34. AB (intervention? or multiintervention? or multi‐intervention? or postintervention? or post‐intervention? or preintervention? or pre‐intervention?) or TI (intervention? or multiintervention? or multi‐intervention? or postintervention? or post‐intervention? or preintervention? or pre‐intervention?)
35. MW intervention
36. AB (pre‐post or "pre test*" or pretest* or posttest* or "post test*" or "pre and post") or TI (pre‐post or "pre test*" or pretest* or posttest* or "post test*" or "pre and post") or MW (pre‐post or "pre test*" or pretest* or posttest* or "post test*" or "pre and post")
37. AB before‐after or TI before‐after
38. AB (before and after) or TI (before and after)
39. AB ("quasi‐experiment*" or quasiexperiment* or "quasi random*" or quasirandom* or "quasi control*" or quasicontrol* or ((quasi* or experimental) and (method* or study or studies or trial or design*))) or TI ("quasi‐experiment*" or quasiexperiment* or "quasi random*" or quasirandom* or "quasi control*" or quasicontrol* or ((quasi* or experimental) and (method* or study or studies or trial or design*))) or MW ("quasi‐experiment*" or quasiexperiment* or "quasi random*" or quasirandom* or "quasi control*" or quasicontrol* or ((quasi* or experimental) and (method* or study or studies or trial or design*)))
40. BG ("time series" and interrupt*) or TI ("time series" and interrupt*) or MW ("time series" and interrupt*)
41. S34 or S35 or S36 or S37 or S38 or S39 or S40
42. MH prospective studies
43. AB (("follow up" or follow‐up) and (design or study or studies)) or TI (("follow up" or follow‐up) and (design or study or studies))
44. MH pilot studies
45. TI pilot or AB (pilot* and (program* or project? or study or studies))
46. MH comparative studies
47. TI (comparative and (study or studies))
48. MH evaluation research
49. MH program evaluation
50. TI evaluat*
51. S42 or S43 or S44 or S45 or S46 or S47 or S48 or S49 or S50
52. S33 or S41 or S51
53. AB groups
54. S52 or S53
55. S54 and S21
Appendix 7. PsycINFO search strategy
1. exp palliative care/
2. exp terminal cancer/
3. exp terminally ill patients/
4. palliat*.mp
5. terminal* and (care or caring or ill*).mp
6. ((advanced or end stage or terminal*) adj4 (disease* or illness* or cancer* or malignan*)).mp
7. last year of life or LYOL or life's end or end of life.mp
8. or/1‐7
9. exp home care/
10. exp home visiting programs/
11. home adj4 (hospital or palliat*).mp
12. (macmillan or marie curie or district) adj nurs*.mp
13. (home or in‐home or domicile or outreach or residential or housing or posthospital or post‐hospital or communit* or mobile or ambulatory or door to door) adj2 (team* or center* or centre* or treat* or care or interven* or therap* or management or model* or program or programs or programme* or service* or base* or nurs*).mp
14. homecare or home‐care or homebased or home‐based.mp
15. or/9‐14
16. hospice*.mp
17. 16 or (8 and 15)
18. (child* or adolescent* or infant* or baby or babies or neonat* or juvenil* or pediatric* or paediatric* or young person* or young people or youth* or young adult* or matern*).ti.
19. 17 not 18
20. clinical trial/
21. chi‐square?.ti,ab.
22. "random*".ab,ti.
23. controlled.ti.
24. trial.ti.
25. Control Groups/
26. (control* adj2 (clinical or group* or trial* or study or studies or design* or method*)).ti,ab.
27. ((multicent* or multi‐cent* or multisite? or multi‐site?) adj (study or studies or trial*)).ti,ab.
28. ((single or double or triple or treble) adj blind*).ti,ab.
29. or/20‐28
30. (intervention? or multiintervention? or multi‐intervention? or postintervention? or post‐intervention? or preintervention? or pre‐intervention?).ti,ab.
31. intervention.hw.
32. (pre‐post or "pre test*" or pretest* or posttest* or "post test*" or "pre and post").ti,ab,hw.
33. before‐after.ti,ab.
34. (before adj4 after).ti,ab.
35. ("quasi‐experiment*" or quasiexperiment* or "quasi random*" or quasirandom* or "quasi control*" or quasicontrol* or ((quasi* or experimental) adj3 (method* or study or studies or trial or design*))).ti,ab,hw.
36. ("time series" adj2 interrupt*).ti,ab,hw.
37. or/30‐36
38. followup studies/
39. (("follow up" or follow‐up) adj2 (design or study or studies)).ti,ab.
40. pilot.ti. or (pilot* adj3 (program* or project? or study or studies)).ab.
41. (comparative and (study or studies)).ti.
42. treatment effectiveness evaluation/
43. evaluat*.ti.
44. or/38‐43
45. 29 or 37 or 44
46. groups.ab
47. 45 or 46
48. 47 and 19
Appendix 8. EURONHEED search strategy
1. hospice*
2. (palliat* or terminal* or end stage) and (home* or community or outreach or ambulatory)
3. (#1 or #2)
Appendix 9. References of literature reviews screened
Curiale 2007: Curiale V, Cella A, Luzzani M, Prete C. Home‐based palliative care for adults with cancer. (Protocol) Cochrane Database of Systematic Reviews 2007; Issue 2. Art. No.: CD006510. DOI: 10.1002/14651858.CD006510
Douglas 2003: Douglas HR, Halliday D, Normand C, Corner J, Bath P, Beech N, et al. Economic evaluation of specialist cancer and palliative nursing: a literature review. International Journal of Palliative Nursing 2003; 9(10): 424‐8.
Dy 2008: Dy SM, Shugarman LR, Lorenz KA, Mularski RA, Lynn J. A systematic review of satisfaction with care at the end of life. Journal of the American Geriatrics Society 2008; 56(1): 124‐9.
Elkan 2001: Elkan R, Kendrick D, Dewey M, Hewitt M, Robinson J, Blair M, et al. Effectiveness of home based support for older people: systematic review and meta‐analysis. BMJ 2001; 323(7315): 719‐25.
Evans 2003: Evans R, Stone D, Elwyn G. Organizing palliative care for rural populations: a systematic review of the evidence. Family Practice 2003; 20(3): 304‐10.
Finlay 2002: Finlay IG, Higginson IJ, Goodwin DM, Cook AM, Edwards AG, Hood K, et al. Palliative care in hospital, hospice, at home: results from a systematic review. Annals of Oncology 2002; 13 suppl 4: 257‐64.
Fordham 1999: Fordham S, Dowrick C. Is care of the dying improving? The contribution of specialist and non‐specialist to palliative care. Family Practice 1999; 16(6): 573‐9.
Francke 2000: Francke AL. Evaluative research on palliative support teams: a literature review. Patient Education & Counseling 2000; 41(1): 83‐91.
García‐Pérez 2008: García‐Pérez L, Linertová R, Martín‐Olivera R, Serrano‐Aguilar P, Benítez‐Rosario MA. A systematic review of specialised palliative care for terminal patients: which model is better? Palliative Medicine 2009; 23(1): 17‐22.
Gomes 2006: Gomes B, Higginson IJ. Factors influencing death at home in terminally ill patients with cancer: systematic review. BMJ 2006; 332(7540): 515‐8.
Harding 2003: Harding R, Higginson IJ. What is the best way to help caregivers in cancer and palliative care? A systematic literature review of interventions and their effectiveness. Palliative Medicine 2003; 17(1): 63‐74.
Harding 2005: Harding R, Karus D, Easterbrook P, Raveis VH, Higginson IJ, Marconi K. Does palliative care improve outcomes for patients with HIV/AIDS? A systematic review of the evidence. Sexually Transmitted Infections 2005; 81(1): 5‐14.
Harding 2011: Harding R, List S, Epiphaniou E, Jones H. How can informal caregivers in cancer and palliative care be supported? An updated systematic literature review of interventions and their effectiveness. Palliative Medicine 2012; 26(1): 7‐22.
Hearn 1998: Hearn J, Higginson IJ. Do specialist palliative care teams improve outcomes for cancer patients? A systematic literature review. Palliative Medicine 1998; 12(5): 317‐32.
Higginson 2000a: Higginson IJ, Finlay IG, Goodwin DM, Cook AM, Edwards AGK, Hood K, et al. The role of palliative care teams: a systematic review of their effectiveness and cost‐effectiveness. Report to Wales Office of Research and Development of the National Assembly of Wales London: Department of Palliative Care and Policy, Velindre NHS Trust, and Department of General Practice, University of Wales College of Medicine, 2000.
Higginson 2000b: Higginson IJ, Sen‐Gupta GJ. Place of care in advanced cancer: a qualitative systematic literature review of patient preferences. Journal of Palliative Medicine 2000; 3(3): 287‐300.
Higginson 2003: Higginson IJ, Finlay IG, Goodwin DM, Hood K, Edwards AGK, Cook A, et al. Is there evidence that palliative care teams alter end‐of‐life experiences of patients and their caregivers? Journal of Pain & Symptom Management 2003; 25(2): 150‐68.
Holland 2005: Holland R, Battersby J, Harvey I, Lenaghan E, Smith J, Hay L. Systematic review of multidisciplinary interventions in heart failure. Heart 2005; 91(7): 899‐906.
Hughes 1997: Hughes SL, Ulasevich A, Weaver FM, Henderson W, Manheim L, Kubal JD, et al Impact of home care on hospital days: a meta analysis. Health Services Research 1997; 32(4): 415‐32.
Ingleton 2003: Ingleton C, Payne S, Nolan M, Carey I. Respite in palliative care: a review and discussion of the literature. Palliative Medicine 2003; 17(7): 567‐75.
Lindstrom 2009: Lindstrom KB, Melnyk BM. Interventions for family caregivers of loved ones on hospice: a literature review with recommendations for clinical practice and future research. Journal of Hospice & Palliative Nursing 2009; 11(3): 167‐78.
McAlister 2001: McAlister FA, Lawson FM, Teo KK, Armstrong PW. A systematic review of randomized trials of disease management programs in heart failure. American Journal of Medicine 2001; 110(5): 378‐84.
McPherson 2001: McPherson CJ, Higginson IJ, Hearn J. Effective methods of giving information in cancer: a systematic literature review of randomized controlled trials. Journal of Public Health Medicine 2001; 23(3): 227‐34.
Miller 2009: Miller RG, Jackson CE, Kasarskis EJ, England JD, Forshew D, Johnston W, et al. Practice Parameter update: the care of the patient with amyotrophic lateral sclerosis: multidisciplinary care, symptom management, and cognitive/behavioral impairment (an evidence‐based review): Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2009; 73(15): 1227‐33.
Murray 2009: Murray MA, Fiset V, Young S, Kryworuchko J. Where the dying live: a systematic review of determinants of place of end‐of‐life cancer care. Oncology Nursing Forum 2009; 36(1): 69‐77.
National Institutes of Health 2004: National Institutes of Health (NIH) State‐of‐the‐Science Conference Statement on improving end‐of‐life care. NIH Consensus & State‐of‐the‐Science Statements 2004; 21: 1‐26.
Nowak 1998: Nowak F, Nagle L, Bernardo A. Review: case management programmes improve patient outcomes [commentary on Ferguson JA, Weinberger M. Case management programs in primary care. Journal of General Internal Medicine 1998; 13:123‐126]. Evidence‐Based Nursing 1998; 1(4): 128.
Phillips 2004: Phillips CO, Wright SM, Kern DE, Singa RM, Shepperd S, Rubin HR. Comprehensive discharge planning with postdischarge support for older patients with congestive heart failure: a meta‐analysis. JAMA 2004; 291(11): 1358‐67.
Rinck 1997: Rinck GC, van den Bos GA, Kleijnen J, de Haes HJ, Schade E, Veenhof CH. Methodologic issues in effectiveness research on palliative cancer care: a systematic review. Journal of Clinical Oncology 1997; 15(4): 1697‐707.
Robinson 1996: Robinson BE, Pham H. Cost‐effectiveness of hospice care. Clinics in Geriatric Medicine 1996; 12(2): 417‐28.
Salisbury 1999: Salisbury C, Bosanquet N, Wilkinson EK, Franks PJ, Kite S, Lorentzon M, et al. The impact of different models of specialist palliative care on patients' quality of life: a systematic literature review. Palliative Medicine 1999; 13(1): 3‐17
Shepperd 1998: Shepperd S, Iliffe S. The effectiveness of hospital at home compared with in‐patient hospital care: A systematic review. Journal of Public Health Medicine 1998; 20(3): 344‐50.
Shepperd 2005: Shepperd S, Iliffe S. Hospital at home versus in‐patient hospital care. Cochrane Database of Systematic Reviews 2005, Issue 3. Art. No.: CD000356.
Shepperd 2008: Shepperd S, Doll H, Angus RM, Clarke MJ, Iliffe S, Kalra L, et al. Admission avoidance hospital at home. Cochrane Database of Systematic Reviews 2008, Issue 4. Art. No.: CD007491. DOI: 10.1002/14651858.CD007491.
Shepperd 2009: Shepperd S, Doll H, Broad J, Gladman J, Iliffe S, Langhorne P, et al. Early discharge hospital at home. Cochrane Database of Systematic Reviews 2009, Issue 1. Art. No.: CD000356. DOI: 10.1002/14651858.CD000356.
Shepperd 2011: Shepperd S, Wee B, Straus S. Hospital at home: home‐based end of life care. Cochrane Database of Systematic Reviews 2011, Issue 7. Art. No.: CD009231. DOI: 10.1002/14651858.CD009231.
Smeenk 1998b: Smeenk FWJ, Van Haastregt JCM, de Witte LP, Crebolder HFJ. Effectiveness of home care programmes for patients with incurable cancer on their quality of life and time spent in hospital: systematic review. BMJ 1998; 316(7149): 1939‐44.
Soderstrom 1999: Soderstrom L, Tousignant P, Kaufman T. The health and cost effects of substituting home care for inpatient acute care: a review of the evidence. Canadian Medical Association Journal 1999; 160(8): 1151‐5.
Stuck 2002: Stuck AE, Egger M, Hammer A, Minder CE, Beck JC. Home visits to prevent nursing home admission and functional decline in elderly people: systematic review and meta‐regression analysis. JAMA 2002; 287(8): 1022‐8.
Taylor 2005: Taylor SJC, Bestall JC, Cotter S, Falshaw M, Hood SG, Parsons S, et al. Clinical service organisation for heart failure. Cochrane Database of Systematic Reviews 2005, Issue 2. Art. No.: CD002752. DOI: 10.1002/14651858.CD002752.pub2.
Thomé 2003: Thomé B, Dykes A, Hallberg IR. Home care with regard to definition, care recipients, content and outcome: systematic literature review. Journal of Clinical Nursing 2003; 12(6): 860‐72.
Thomas 2006: Thomas RE, Wilson D, Sheps S. A literature review of randomized controlled trials of the organization of care at the end of life. Canadian Journal on Aging 2006; 25(3): 271‐93.
Tieman 2008: Tieman J, Sladek R, Currow D. Changes in the quantity and level of evidence of palliative and hospice care literature: the last century. Journal of Clinical Oncology 2008; 26(35): 5679‐83.
Turner‐Stokes 2005: Turner‐Stokes L, Nair A, Sedki I, Disler PB, Wade DT. Multi disciplinary rehabilitation for acquired brain injury in adults of working age. Cochrane Database of Systematic Reviews 2005, Issue 3. Art. No: CD004170. DOI: 10.1002/14651858.CD004170.pub2.
van Haastregt 2000: van Haastregt JC, Diederiks JP, van Rossum E, de Witte LP, Crebolder HF. Effects of preventive home visits to elderly people living in the community: systematic review. BMJ 2000; 320(7237): 754‐8.
Wilkinson 1999: Wilkinson EK, Salisbury C, Bosanquet N, Franks PJ, Kite S, Lorentzon M, et al. Patient and carer preference for, and satisfaction with, specialist models of palliative care: a systematic literature review. Palliative Medicine 1999; 13(3): 197‐216.
Wilson 2006: Wilson DM, Justice C, Sheps S, Thomas R, Reid P, Leibovici K. Planning and providing end‐of‐life care in rural areas. Journal of Rural Health 2006; 22(2): 174‐81.
Young 2010: Young T, Busgeeth K. Home based care for reducing morbidity and mortality in people infected with HIV/AIDS Cochrane Database of Systematic Reviews 2010, Issue 1. Art. No.: CD005417. DOI: 10.1002/14651858.CD005417.pub2.
Zimmermann 2008: Zimmermann C, Riechelmann R, Krzyzanowska M, Rodin G, Tannock I. Effectiveness of specialized palliative care: a systematic review. JAMA 2008; 299(14): 1698‐709.
Data and analyses
Comparison 1. Home palliative care versus usual care.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Death at home | 7 | 1222 | Odds Ratio (M‐H, Random, 95% CI) | 2.21 [1.31, 3.71] |
| 1.1.1 RCTs | 5 | 886 | Odds Ratio (M‐H, Random, 95% CI) | 1.73 [1.28, 2.33] |
| 1.1.2 CCTs | 2 | 336 | Odds Ratio (M‐H, Random, 95% CI) | 3.44 [0.60, 19.57] |
| 1.2 death at home with only high quality RCTs | 3 | 614 | Odds Ratio (M‐H, Random, 95% CI) | 1.75 [1.24, 2.47] |
| 1.3 Death in hospital | 6 | 1179 | Odds Ratio (M‐H, Random, 95% CI) | 0.31 [0.12, 0.79] |
| 1.3.1 RCTs | 4 | 843 | Odds Ratio (M‐H, Random, 95% CI) | 0.29 [0.08, 1.13] |
| 1.3.2 CCTs | 2 | 336 | Odds Ratio (M‐H, Random, 95% CI) | 0.32 [0.07, 1.46] |
| 1.4 death in hospital with only high quality RCTs | 3 | 614 | Odds Ratio (M‐H, Random, 95% CI) | 0.19 [0.03, 1.11] |
| 1.5 Death in nursing home | 5 | 899 | Odds Ratio (M‐H, Random, 95% CI) | 0.64 [0.40, 1.03] |
| 1.5.1 RCTs | 4 | 843 | Odds Ratio (M‐H, Random, 95% CI) | 0.63 [0.38, 1.02] |
| 1.5.2 CCTs | 1 | 56 | Odds Ratio (M‐H, Random, 95% CI) | 1.11 [0.11, 11.53] |
| 1.6 death in nursing home with only high quality RCTs | 3 | 614 | Odds Ratio (M‐H, Random, 95% CI) | 0.66 [0.39, 1.10] |
| 1.7 Death in inpatient hospice/palliative care unit | 5 | 1123 | Odds Ratio (M‐H, Random, 95% CI) | 1.46 [0.51, 4.19] |
| 1.7.1 RCTs | 4 | 843 | Odds Ratio (M‐H, Random, 95% CI) | 1.98 [0.36, 10.98] |
| 1.7.2 CCTs | 1 | 280 | Odds Ratio (M‐H, Random, 95% CI) | 1.30 [0.77, 2.19] |
| 1.8 death in inpatient hospice/palliative care unit with only high quality RCTs | 3 | 614 | Odds Ratio (M‐H, Random, 95% CI) | 3.71 [0.25, 54.92] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ahlner‐Elmqvist 2008.
| Study characteristics | ||
| Methods |
Design: CCT (patient and caregiver) Methodological quality: 1.5/6a (EPOC RCT/CCT checklist) |
|
| Participants |
Country and regions: Sweden, Malmö, metropolitan area Recruitment (1995‐1998, 30 months): physician referrals or self referrals from departments of Oncology, Respiratory Medicine, Haematology, Surgery, Otorhinolaryngology, Urology and Gynaecology at Malmö University Hospital; patients living in the city of Malmö, with cancer (histological verified), life expectancy from 2 to 12 months (not stated who estimated), informed about diagnosis, about the palliative care situation and possibility to get care at home and additional hospital treatment if needed. Exclusion criteria: non‐Swedish speaking, mentally or physically unable to fill in questionnaires Number of patients (allocated according to their preference): 297 (119 intervention and 178 control) Diseases: cancer (297) Patient characteristics: median age 67 years intervention, 68 years control; 48% female intervention, 54% female control; 29% lived alone Number of caregivers (consented): 204 (102 in each group) Caregiver characteristics: median age 63 years intervention, 65 years control; 64% female; 77% spouses Deaths at end of study: 117 intervention (98%) and 163 control (92%) Withdrawals/other drop‐outs: "no patients are lost for follow‐up" |
|
| Interventions | Home palliative care vs. usual care "Advanced Home Care (AHC)" Type: intermediate palliative care Service base: hospital oncology department (Malmö University Hospital) Team: 9 experienced nurses, oncologist, social worker, physiotherapist, secretary; priest associated on consultation basis; all with long experience in advanced cancer care with no formal training but attended palliative care training programme prior to service start; nurses worked day and evening shifts and on night emergency services; other staff worked daytime hours; weekly meetings; able to care for 25 patients at a time Responsibility: not stated Description: new 7‐days‐a‐week service to complement existing inpatient and community care; included symptom treatment, counselling and emotional, social and family support; team home visits planned according to patient's needs and with degree of flexibility, could include injections, intravenous fluid therapy, blood transfusions, chemotherapy, nasogastric intubation and catheterisation of the urine bladder and other forms of technical support; access to on‐call service from service base (evenings, nights and weekends with on‐call oncologist home visits if need be); 3 'back‐up' beds available (2 at hospice and 1 at the oncology unit) Duration: not stated but likely to be from enrolment to death or study end (median survival for intervention group was 94 days, only 2 patients were still alive at study end) Control: CC provided jointly by hospital and community services, including inpatient and outpatient hospital care, primary care and access to inpatient hospice care (public health system); basic ideology was for patients to be cared for at 'lowest' possible level, implying that patients who do not need hospital care were cared for at home by primary care physicians and district nurses; generally, patients had to visit primary care centres and the primary care physician only visited at home in exceptional circumstances; HC on a 24‐hour basis was difficult due to organisational limitations in primary care thus if patients need advanced medical and nursing care, they had to be admitted to hospital or possibly offered a bed in a hospice |
|
| Outcomes | Death at home (primary outcome) Death in hospital Death in inpatient hospice Survival Caregiver pre‐ and post‐bereavement outcomes (quality of life; general health; vitality; physical, psychological and social functioning; bodily pain) Assessment points: caregivers were assessed every second month until death and then 1, 3, 6 and 13 months after death Analysis: backwards from death and forwards from death |
|
| Resource use/costs | Hospitalisations (admission, proportion of time in hospital) Time horizon: enrolment to death or study end (admission and proportion of time in hospital); month before death (proportion of time in hospital) |
|
| Notes |
Power considerations: "the planned sample size was 150 patients in each group. (...) This number of patients is adequate to detect a 14% absolute change in place of death (...) power 90%, significant level 0.05" Return of the first completed questionnaire was regarded as written consent. Those with a preference for HC who refused to participate still received HC. No patients changed from intervention to control or vice‐versa |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Concealment of allocation (RCT / CCT) | High risk | Allocation based on patient preference |
| Follow‐up (RCT / CCT) | Unclear risk | 117 intervention (98%) and 163 control (92%) for primary outcome and survival (patients alive at the end of study were excluded from survival analysis); 122/204 (60%) for caregiver pre‐bereavement outcomes (first assessment) and 130/204 (64%) for caregiver post‐bereavement outcomes (1 month after death) |
| Blinding (RCT / CCT) | Unclear risk | Source of primary outcome not stated; blinding not stated |
| Baseline measurement (RCT / CCT) | High risk | Intervention patients preferred to be cared for at home (variable influencing in same direction as results). In addition, there were significant differences in physical function (intervention poorer KPS), primary cancer diagnosis (controls had more often lung and gastrointestinal) and weeks from diagnosis to inclusion (intervention longer time) |
| Reliability of outcome measurement (RCT / CCT) | Unclear risk | Source of primary outcome not stated, although it was objective; others were self completed |
| Protection against contamination (RCT / CCT) | High risk | Patient allocation |
Aiken 2006.
| Study characteristics | ||
| Methods |
Design: RCT (patient) Methodological quality: 3/6a (EPOC RCT/CCT checklist) |
|
| Participants |
Country and regions: US, Phoenix, Arizona, metropolitan area Recruitment (1999‐2001, 20 months): from community agencies, hospitals, 7 HMOs, physicians, family/friends and self referral; patients aged ≥ 18 years with CHF and COPD disease‐specific criteria of life expectancy ≤ 24 months (expert judgement) with ED or urgent care facility or hospital admissions in last 3 months and marked limitation in physical function with activity resulting in fatigue, palpitations, dyspnoea or angina Number of patients (randomised): 192 (101 intervention and 91 control) Diseases: CHF (130), COPD (62) Patient characteristics: "average" age 68.5 years; 64% female Deaths at end of study: 16% intervention and 13% control Withdrawals/other drop‐outs: 41% intervention and 54% control (entered hospice care or skilled nursing facilities, declined continued participation, left the HMO) |
|
| Interventions | Home palliative care vs. usual care "PhoenixCare intervention" Type: intermediate palliative care Service base: Hospice of the Valley – largest community‐based hospice care provider in the US Team: physician (medical director), 2 or 3 nurses (RN case managers with 30‐35 patient caseload), half‐time social worker, half‐time pastoral counsellor; staff training (2 weeks on FairCare communication model and other monthly training) Responsibility: team's nurse (with primary care physician and HMO case manager); nurse went with patient to physician visits to discuss progress and care options Description: intervention grounded on patient empowerment model and behaviour change theory (shift from crisis‐response to self empowerment and prevention); without forgoing curative treatment; included disease and symptom management, patient and caregiver education (included self monitoring, home safety, equipment and medication), psychosocial and spiritual support, co‐ordination of care and case management; needs assessment (including psychological and spiritual); referral to counselling and community resources (custodial care, transportation, help with finances); management protocols by phase of illness (initially unstable, stable, unstable following exacerbation); individualised emergency response plan at home (used in hospice care) and on‐call nurse contact; advanced care planning with patient and family; patient notebook at home (with goals patient was working towards, emergency plans, information material, reviewed in calls and visits); nurses telephone calls and home visits ("average" 6, 5, 4, 4, 3 and 3 in first 6 months and stable from then onwards; half calls, half visits); visits from other staff (45% saw social worker, "average" 6 times); on‐call nursing Duration: from enrolment to death, transfer to hospice care or skilled nursing care facility, or study end (length of stay not stated) Control: usual care focused on technical care (medication and laboratory monitoring, weight/blood pressure and blood glucose monitoring, implementation of prior authorisation mechanisms) and most patients had HMO case management (51% intervention vs. 62% control; P value = 0.12). 7 HMOs had telephone monitoring and 5 had occasional home visits. Other services included disease and symptom education, nutrition and psychological counselling, transportation and care co‐ordination. During the study, HMOs greatly narrowed criteria for case management and reduced services, due to financial pressures. 5 HMOs ended use of telephone calls and all terminated home visits and other support services. 3 HMOs reinstated some services in last study quarter, when enrolment was sparse |
|
| Outcomes | Physical symptoms (pain, most troublesome symptom) Quality of life General health and vitality Physical, psychological and social functioning Self management of illness and knowledge of resources Advance care planning (preparation for end of life) Assessment points: baseline and 3, 6 and 9 months after Analysis: forwards from enrolment |
|
| Resource use/costs | ED visits HMO case manager assigned to patient Time horizon: from enrolment to death or study end |
|
| Notes |
Power considerations: "Statistical power to detect moderate effect size differences between intervention and control participants fell from 0.93 to 0.74 to 0.64 at time 0, 3, and 6, respectively" Data at 9 months were not analysed except for quality of life (reason not stated). Data on hospitalisations (presence and number of days) were assessed but could not be analysed because of "inadequately reported hospital claims data" related to problems in pairing admission and discharge dates and to reporting based on primary diagnosis regardless of treatment provided |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Concealment of allocation (RCT / CCT) | Low risk | "Randomization was carried out within diagnosis, in blocks of 30 patients (15 intervention, 15 control) by a member of the project administration staff. Sealed envelopes, colour‐coded by diagnosis and containing the assignment to condition, were shuffled and assigned to participants in order of shuffling" |
| Follow‐up (RCT / CCT) | High risk | 62% intervention and 54% control follow‐up at 3 months |
| Blinding (RCT / CCT) | Unclear risk | Single‐blind: "interviewers were blind to condition and diagnosis", but participants not stated |
| Baseline measurement (RCT / CCT) | Low risk | Statistical tests of differences in sociodemographics not reported. Trend towards significant differences at baseline SF‐36 subscales (same direction as treatment effect): "PhoenixCare participants tended to have higher scores on the SF‐36 Social Functioning Scale, F(1,189) = 3.45, P = 0.07, g = 0.27, and on the SF‐36 Mental Health Scale, F(1,190) = 3.35, P = 0.07, g = 0.26." Analysis was adjusted for baseline scores and authors reported all effects were maintained when controlling for SF‐36 baseline differences |
| Reliability of outcome measurement (RCT / CCT) | Unclear risk | Collected from patients by interviewers on the telephone. "Proxy respondents could read or translate for patients. Proxy responses were not accepted" |
| Protection against contamination (RCT / CCT) | High risk | Patients randomised |
Axelsson 1998.
| Study characteristics | ||
| Methods |
Design: cluster CCT (patient) Methodological quality: 2.5/6a (EPOC RCT/CCT checklist) |
|
| Participants |
Country and regions: Sweden, Östersund, County of Jämtland, metropolitan area (sparsely populated region) Recruitment (1991‐1993, 30 months): mainly from Department of General Surgery at County Hospital of Östersund but also from other departments and other GPs; patients with symptomatic incurable cancer (disease within the realm of general surgery), who wished to stay at home and had a caregiver; patients living within 40 km of the hospital (9 primary care health centres) were allocated to the intervention; controls met all inclusion criteria but the latter (unknown number of primary care health centres) Number of patients (allocated): 72 (57 intervention and 15 control; authors referred to the control group as "reference group") Diseases: cancer (72) Patient characteristics: median age 72 years intervention, 71 years control; 46% female Deaths at end of study: 72 Withdrawals/other drop‐outs: 17 intervention (1 actively dying, 16 who were not matched to a third historical control group, see notes) |
|
| Interventions | Home palliative care vs. usual care "Palliative Support Service (PSS)" Type: specialist palliative care Service base: Department of General Surgery at County Hospital of Östersund Team: full‐time nurse (15 years' experience of practical cancer care on a surgical ward, trained in pain relief and symptom control, worked weekdays 8 a.m. to 5 p.m.), surgeon (half‐day per week basis); leasing car and mobile telephone; weekly conference to review cases; collaboration with the 9 local primary care centres Responsibility: not stated Description: new programme; nurse role ‐ acted as link between home and hospital, supported patient, caregiver and district nurse, district nurse education on management of infusors, epidural catheters, central venous catheters and other technical devices, administered blood transfusions, low‐dose chemotherapy and parenteral nutrition at home when needed; surgeon role ‐ scrutinised all referrals to select patients for whom support could imply improved palliation and extended time at home, reviewed patients at weekly conference with nurse, occasional home visits if needed (supported by 6 interested colleagues); patient dossier – given to the patient on discharge to improve communication between the hospital and primary healthcare service, included copies of essential information from medical records, with 3 specific fact sheets (1. sheet listed all names and telephone numbers of staff involved, namely surgeon, ward, GP, district nurse, HC assistant, consultant nurse, emergency telephone numbers for nights and weekends; 2. all prescribed drugs, information on effects and administration instructions; 3. exact wording used by doctor informing the patient of their disease and its dissemination, stating clearly whether patient had been informed of a lump, a tumour or a cancer and which metastases the patient knew of, also noted the family member(s) who had received the same information) Duration: median length of stay in intervention 70 days Control: usual care, mainly home care and conventional primary and hospital care |
|
| Outcomes | Death at home Death in hospital Death in nursing home Percentage of time and days spent at home Survival Assessment points: prospectively for intervention and retrospectively for control group, through medical records |
|
| Resource use/costs | Hospitalisations (number of admissions, terminal hospitalisation days) Institutional days (in hospital and nursing homes) HC (hours of contact with intervention consultant nurse and surgeon, district nurse, assistant nurse, GP, home service, night sitting) Informal care (days next of kin off work) Time horizon: from enrolment to death; from diagnosis to death (institutional days); last 6 months before death (hospital admissions, institutional days) |
|
| Notes |
Power considerations: none stated Analysis involved only part of the intervention group, those matched to a third historical control group who died locally prior to service start (1990); patients aged ≥ 58 years were matched for age, diagnosis, place of residence and as far as possible for gender and marital status (younger patients could not be adequately matched). This excluded 16 of 57 eligible patients, resulting in a sample of 41 in the intervention group Longer recruitment for intervention patients (30 months) than for controls (4 months) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Concealment of allocation (RCT / CCT) | High risk | Allocation based on area proximity to service (not random) |
| Follow‐up (RCT / CCT) | High risk | 56/72 (78%) |
| Blinding (RCT / CCT) | Unclear risk | Not stated |
| Baseline measurement (RCT / CCT) | Unclear risk | No significant differences in age, sex distribution, marital status and KPS; however, groups differed in distance to hospital |
| Reliability of outcome measurement (RCT / CCT) | Unclear risk | Patient and staff filled sheets in patient's dossier |
| Protection against contamination (RCT / CCT) | Low risk | Allocation was by area |
Bakitas 2009.
| Study characteristics | ||
| Methods |
Design: RCT (patient and caregiver) Methodological quality: 3.5/6a (high quality, EPOC RCT/CCT checklist) |
|
| Participants |
Country and regions: US, New Hampshire and Vermont, rural areas Recruitment (2003‐2007, 42 months): from weekly management meetings of tumour boards for gastrointestinal, genitourinary, breast and thoracic cancers at the Norris Cotton Cancer Center in New Hampshire (National Cancer Institute‐designated comprehensive cancer centre) and affiliated outreach clinics and the VA medical centre in White River Junction, Vermont; newly diagnosed (from 8 to 12 weeks) gastrointestinal, lung, genitourinary or breast cancers with specific clinical markers of advanced illness and life expectancy of approximately 1 year (assessor not stated). Exclusion criteria: impaired cognition, axis I psychiatric disorder, active substance use Number of patients (randomised): 322 (161 intervention and 161 control) Diseases (outcome sample): cancer (279): gastrointestinal (119), lung (93), genitourinary (37), breast (30) Patient characteristics (outcome sample): mean age 65.4 years intervention, 65.2 years control; 39.8% female Number of caregivers ( ): 220 (116 intervention and 104 control) Caregiver characteristics (outcome sample of 198 caregivers): mean age 58.0 years intervention, 59.9 years control; 77% female; 71% spouse/partner Deaths at end of study: 231 (72%); 112 intervention (70%) and 119 control (74%) Withdrawals/other drop‐outs: 57 patients (18%): 29 intervention (18%) and 28 control (17%) (reasons not stated); 134 caregivers (61%): 66 intervention (57%) and 68 control (65%) (due to withdrawal, refusal or completion of initial form of the questionnaire) |
|
| Interventions | Home palliative care vs. usual care "Project ENABLE II" Type: specialist palliative care Service base: palliative care programme, Dartmouth‐Hitchcock Medical Center Team: certified palliative care physician, advanced practice nurses with high speciality training in palliative care (acting as case managers with caseload balanced by diagnosis and gender); staff training (12‐20 hours on problem solving and group medical appointments provided by study psychologist; methods included didactic presentations, written treatment manuals, role‐playing with feedback – training materials available from authors); biweekly reviews of audio‐taped educational sessions and feedback on difficult patient management issues Responsibility: team's nurse (but final responsibility rested with primary clinical team for medical decisions including medication and inpatient care management, although intervention nurses, in consultation with primary team, could facilitate referrals to ancillary resources) Description: grounded on chronic care model and previous demonstration project; without forgoing curative treatment; included case management, crisis prevention, and patient and caregiver education to encourage activation, self management and empowerment; telephone‐based format (for rural population); 4 initial structured educational and problem‐solving modular sessions (31‐40 minutes each) and at least monthly telephone follow‐ups; initial full needs assessment on practical problems (e.g. work or school), family, emotional, spiritual or religious and physical problems (made use of Distress Thermometer following National Comprehensive Cancer Network guidelines – if distress rated > 3, sources of distress and problem solving explored); education manual with 4 modules (problems solving, communication and social support, symptom management, advance care planning and unfinished business) and list of supportive care resources (available from authors); referral to other resources (e.g. palliative care team, hospice, spiritual counsellor); nurse encouraged or offered to contact oncology and palliative care team when problems were identified (e.g. unrelieved pain); nurse readily available by telephone; monthly group shared medical appointments with physician and nurse for patients and caregivers to ask about medical problems and related issues, more in‐depth than clinic visits; follow‐up call in bereavement Duration: from enrolment into bereavement or study end (median survival 14 months in intervention group) Control: all oncology and supportive services without restrictions including referral to the institutions' interdisciplinary palliative care service; 1 of the sites (VA Medical Center in Vermont) had an advanced illness co‐ordinated care programme that provided consultation to oncology staff for inpatients with life‐limiting illness |
|
| Outcomes | Quality of life (primary outcome) Symptom intensity (primary outcome) Depression Death at home Death in hospital Death in nursing home Death in inpatient hospice Survival Caregiver satisfaction with care Caregiver pre‐bereavement outcomes (burden) Caregiver post‐bereavement outcomes (grief intensity) Assessment points: baseline, 1 month after, and then every 3 months until death of study end; approximately 4‐6 months after death Analysis: forwards from enrolment and backwards from death |
|
| Resource use/costs | Hospital inpatient days ED visits Intensive care unit days Referral to palliative care Referral to hospice care Time horizon: from referral to death or study end (median 14 months intervention and 8.5 months control) |
|
| Notes |
Power considerations: "Original target sample size of 400 was chosen to provide 80% power to detect treatment effects of at least 0.35 SDs for scores on the Functional Assessment of Chronic Illness Therapy for Palliative Care, ESAS, and CES‐D based on a t test comparing the treatment groups with respect to the last observed value with a 2‐sided α of.01. However, at the planned study completion date, the final total study enrolment was 322 due to slightly slower accrual than anticipated" Authors conducted semi‐structured interviews of a subsample of intervention and control participants and caregivers, as well as oncology clinicians, to obtain in‐depth data about their experience with intervention and usual care |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Concealment of allocation (RCT / CCT) | Low risk | "stratified randomization scheme developed for each of the 2 primary sites (...) stratified by disease and blocked within strata (block lengths of 2 and 4 varied randomly)" |
| Follow‐up (RCT / CCT) | Unclear risk | 108 intervention (67%) and 97 control (60%) 1 month follow‐up for quality of life; 109 intervention (68%) and 100 control (62%) for symptoms; 102 intervention (63%) and 98 control (61%) for depression; 112 intervention (70%) and 119 control (74%) for place of death; 161/161 intervention (100%) and 161/161 control (100%) for survival; 50/116 intervention (43%) and 36/104 control (35%) for caregiver burden |
| Blinding (RCT / CCT) | High risk | Blinded at baseline but not subsequently: "research assistants notified the participant of group allocation when the baseline assessment was returned" |
| Baseline measurement (RCT / CCT) | Low risk | No statistically significant differences at baseline between intervention and control for demographic and clinical characteristics, the 3 patient reported outcomes and care use. "Each analysis was adjusted for the respective baseline instrument score" |
| Reliability of outcome measurement (RCT / CCT) | Low risk | Patients and caregivers completed the baseline questionnaires upon enrolment and the follow‐up questionnaires mailed to them |
| Protection against contamination (RCT / CCT) | High risk | Patients/caregivers randomised |
Brumley 2007.
| Study characteristics | ||
| Methods |
Design: RCT (patient) Methodological quality: 3.5/6a (high quality, EPOC RCT/CCT checklist) |
|
| Participants |
Country and regions: US, Hawaii and Colorado, metropolitan areas Recruitment (2002‐2004, 18 months): from discharge planners, primary care and specialist physicians in 2 non‐profit HMOs (Kaiser Permanente Group), life expectancy ≤ 12 months with ED or hospital admissions in last year and physical function ≤ 70 in Palliative Performance Scale (from 0 death to 100 normal) Number of patients (randomised): 310 (155 intervention and 155 control) Diseases: cancer (138), CHF (97), COPD (62) Patient characteristics: mean age 73.8 years; 49% female; 26.3% lived alone Deaths at end of study: 225 (73%) Withdrawals/other drop‐outs: 5 withdrawals (2 in the intervention and 3 in the control); 8 patients died after randomisation but prior intervention (all in the intervention group) |
|
| Interventions | Home palliative care vs. usual care "In‐Home Palliative Care – IHPC" Type: intermediate palliative care Service base: 2 non‐profit Kaiser Permanente Group HMOs – 1) Hawaii: 18 medical offices of 317 medical group physicians providing all outpatient care and most inpatient care (with internal home health agency, contracts with external providers for hospice care only); 2) Colorado: 16 ambulatory medical offices of more than 500 physicians representing all medical specialities and subspecialities (contracts with external providers for ED, hospital, home health and hospice care) Team: physician, nurse, social worker with support from others (spiritual counsellor/chaplain, bereavement co‐ordinator, home health aide, pharmacist, dietician, volunteer, physiotherapist, occupational therapist, speech therapist) Responsibility: team's physician (but allowed primary provider to continue) Description: modelled on hospice programmes but without forgoing curative treatment; patients assigned to palliative care physician to co‐ordinate care from a variety of healthcare providers; included medical care, symptom management, education, biopsychosocial support, co‐ordination, continuous assessment and management of care across all settings; initial inter‐disciplinary assessment (physical, medical, psychological, social and spiritual needs); joint care plan to decide frequency of visits on individual basis; advance directives with patient and family; training patients and caregivers on use of medication, self management and crisis intervention at home; patient wrist band for ED staff to know patient was in home palliative care and had advance directives on file (1 site only); physicians home visits and nursing care 24 hours on‐call Duration: from enrolment to death or transfer to hospice care (mean survival 196 days in the intervention group) Control: usual care with various amounts and levels of primary care services, home health services (when Medicare criteria met), acute care services and hospice care |
|
| Outcomes | Death at home Patient satisfaction with care Survival Assessment points: satisfaction with care measured at baseline, 30, 60, 90 and 120 days after enrolment Analysis: forwards from enrolment |
|
| Resource use/costs | Hospitalisations (admission and inpatient days) ED visits Hospice care (referral and days) Time horizon: from enrolment to death, transfer to hospice care or study end Costs: mean adjusted total costs and mean adjusted total costs per day (included those associated with physician visits, ED visits, hospital days, skilled nursing facility days, and home health or palliative days) Currency: 2002 USD |
|
| Notes |
Power considerations: study powered for cost differences (planned 300; randomised 310; analysed 297) Data on satisfaction with care at 120 days were not analysed due to "significant reduction in sample size" (n = 136) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Concealment of allocation (RCT / CCT) | Low risk | "blocked randomization using a computer generated random number chart, stratified according to study site" |
| Follow‐up (RCT / CCT) | Unclear risk | 70% follow‐up for patient satisfaction with care at 30 days (n = 216); 73% follow up for place of death (n = 225); 145/155 intervention (94%) and 152/155 control for survival (98%) |
| Blinding (RCT / CCT) | Unclear risk | Single‐blind: research assistants blinded but patients not stated |
| Baseline measurement (RCT / CCT) | Low risk | Baseline differences in care satisfaction scores (intervention higher satisfaction; P value = 0.03) but analysis conducted with binary variable (no baseline differences) |
| Reliability of outcome measurement (RCT / CCT) | Unclear risk | Collected from patients or their caregivers by research assistants (care satisfaction), HMO's records, death certificates and family report (death at home, survival) |
| Protection against contamination (RCT / CCT) | High risk | Patients randomised |
Buckingham 1978.
| Study characteristics | ||
| Methods |
Design: cluster CCT (patient and caregiver) Methodological quality: 3/6a (EPOC RCT/CCT checklist) |
|
| Participants |
Country and regions: US, New Haven, metropolitan area Recruitment (1975‐1977, 21 months): referrals from oncologists; patients aged ≥ 18 years with terminal cancer (primary site lung, colon or breast) with life expectancy ≤ 6 months and ≥ 14 days survival after enrolment, living with friend or relative with potential for being primary caregiver; areas within hospice geographical region allocated to intervention and other areas allocated to control (allocation according to area where patient lived); control group matched to age (within 10 years), gender and cancer primary site of intervention group Number of patients (allocated): 70 (35 intervention and 35 control) Number of caregivers (allocated): 70 (35 intervention and 35 control) Diseases: cancer (70); primary site lung, colon or breast Patient and caregiver characteristics: not stated Deaths at end of study: not stated Withdrawals/other drop‐outs: not stated |
|
| Interventions | Home palliative care vs. usual care "Hospice home care program" Type: intermediate palliative care Service base: not stated Team: not stated Responsibility: not stated Description: hospice HC programme of terminal care, 'experienced services', "providing for many needs that often cannot be met in acute care settings" Duration: not stated Control: usual care with "differing therapeutic philosophies of organizations charged with their care" |
|
| Outcomes | Anxiety and depression Social adjustment Caregiver pre‐bereavement outcomes (anxiety, depression, social adjustment) Assessment points: not stated Analysis: forwards from enrolment |
|
| Resource use/costs | Time spent in an acute hospital or institutional setting Hospitalisations HC Time horizon: not stated |
|
| Notes | Power considerations: none stated | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Concealment of allocation (RCT / CCT) | High risk | Allocation based on area proximity to service (not random) |
| Follow‐up (RCT / CCT) | Unclear risk | Not stated |
| Blinding (RCT / CCT) | Unclear risk | Not stated |
| Baseline measurement (RCT / CCT) | Unclear risk | Not stated |
| Reliability of outcome measurement (RCT / CCT) | Unclear risk | Self report questionnaires (unclear who provided) |
| Protection against contamination (RCT / CCT) | Low risk | Allocation by area |
Gómez‐Batiste 2010.
| Study characteristics | ||
| Methods |
Design: CBA (patient) Methodological quality: 3/6a (EPOC CBA checklist) |
|
| Participants |
Country and regions: Spain, all 19 country regions, urban and rural areas Recruitment (2007, 3 months): consecutive new referrals in 5 days to 105 palliative care services, patients > 18 years with advanced or terminal cancer, not receiving chemotherapy or radiotherapy in previous 30 days. Exclusion criteria: unavailable on the telephone Number of patients (included): 265 (158 intervention and 107 control) Diseases: cancer (265) Patient characteristics: mean age 72.2 years; 39% female Deaths at end of study: 43 (drop‐outs) Withdrawals/other drop‐outs: 19 (14 due to severe impairment, 5 reasons not stated) |
|
| Interventions | Home vs. hospital palliative care Type: specialist palliative care Service base: 62 services, base not stated Team: typically included doctor, 2 or 3 nurses and psychosocial worker (social worker or psychologist) with advanced training in palliative care; listed in national directory of palliative care services; according to a previous study, each team cared for a mean of 112 advanced or terminal patients/year Responsibility: not stated although services aimed to advise other conventional teams in the community (primary physician/team likely to remain in charge) Description: no specific information about intervention aims, components and availability of on‐call; according to previous study the teams performed a mean of 9 interventions per patient and telephone calls were the second most frequent activity Duration: not stated (median length from day of first clinical visit to death or last monitoring visit within study period was 42 days) Control: specialist palliative care provided in hospitals (43 services) including palliative care units in acute bed hospitals, palliative care units in medium‐term stay facilities, hospital support teams and outpatient clinics |
|
| Outcomes | Symptoms (pain, anorexia, nausea/vomiting, constipation, insomnia, breathlessness, anxiety, depression) Assessment points: baseline, 7 and 14 days after |
|
| Resource use/costs | Not assessed | |
| Notes |
Power considerations: none stated Of 318 services invited to take part, 223 accepted (70%) and 105 (33%) were able to recruit patients; excessive clinical workload was main reason for refusal |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Baseline measurement (CBA) | Unclear risk | Baseline characteristics for intervention patients and controls not reported separately |
| Characteristics of intervention and control providers (CBA) | Unclear risk | Limited information on providers' characteristics |
| Blinded assessment of outcomes (CBA) | Unclear risk | Source not stated |
| Protection against contamination (CBA) | Low risk | Second sites used as controls (hospital palliative care services) |
| Reliable outcome measurement (CBA) | Unclear risk | Source not stated |
| Follow‐up of patients/caregivers (CBA) | High risk | 203 (77%) patients followed‐up (drop‐out reasons: 69% death, 23% severe impairment, 8% reasons not stated) |
Grande 1999.
| Study characteristics | ||
| Methods |
Design: RCT (patient and caregiver) Methodological quality: 3/6a (EPOC RCT/CCT checklist) |
|
| Participants |
Country and regions: UK, Cambridge health district Recruitment (date not stated, 15 months): mainly from primary care (admission avoidance) and less than one‐third from secondary care (enabling discharge); any diagnosis with life expectancy ≤ 2 weeks (estimated by clinicians) and need for terminal care or cancer/MND/AIDS patients with need for respite care. Exclusion criteria: emergency cases without usual care and those enrolled in periods where service was 'empty' (these were given the intervention without entering trial) Number of patients (randomised): 241 Diseases (outcome sample of 229 patients): cancer (198), non‐cancer (31) Patient characteristics: mean age 72.1 years intervention, 72.6 years control; 50.2% female; 20.6% lived alone Number of caregivers (randomised): 198 Caregiver characteristics (subsample of 96 bereaved caregivers): mean age 63.6 years intervention, 62.3 years control; 49.0% female; 71.9% spouses Deaths at end of study: 229 (95%); 186 intervention and 43 control Withdrawals/other drop‐outs: 13 patients who were still alive at end of study and 31 with no caregiver were excluded from caregiver after death follow‐ups; non‐response from 55 caregivers to 6 weeks after death questionnaire; 102 caregiver drop‐outs at 6 months after death (83 did not agree to take part and 19 non‐responses) |
|
| Interventions | Home palliative care versus usual care "Cambridge Hospital At Home ‐ HAH ‐ for palliative care" Type: intermediate palliative care Service base: Marie Curie nursing service and inpatient hospice, under the same palliative care manager (ran separately with separate funding). Location appeared to ease informal service cooperation and access to specialist medical advice Team: 6 qualified nurses (2 ENs and 4 RGNs), 2 nursing auxiliaries and 1 co‐ordinator (RGN); most with Marie Curie Nursing experience (i.e. non‐profit nursing service supporting people in their last months of life spending several hours at a time in their home with nursing care and emotional support, often overnight); extra help from agency nurses; service resourced to accommodate 100 people per year Responsibility: not stated Description: aimed to provide practical home palliative nursing care, improve care for terminally ill patients and increase their choice of place of care; limited description of components; care available up to 24 hours a day Duration: maximum of 2 weeks Control: usual care included care in hospital/hospice/home with input from general practice, Marie Curie nursing, Macmillan nursing (i.e. non‐profit nursing service supporting cancer patients often since diagnosis, spending up to 1 hour in their home with advice on pain management and symptom control together with emotional support), day and evening district nursing (i.e. senior HC nurses), social services, private care and a Flexible Care nursing service (i.e. home nursing service, similar to Marie Curie nursing, but funded by primary care authority from national health system and available for all diagnosis) |
|
| Outcomes | Death at home (primary outcome) Death in hospital Death in inpatient hospice Death in nursing home Patient spent time at home in last 2 weeks of life Appropriateness of place of death (to caregiver) Physical symptoms (pain, nausea/vomiting, constipation, diarrhoea, breathlessness) Psychological well‐being (anxiety, depression) Patient unmet support needs Survival Caregiver pre‐bereavement outcomes (caregiver unmet support needs) Caregiver post‐bereavement outcomes (quality of life and grief intensity) Assessment points: questionnaires posted to caregiver 6 weeks after death (symptoms and needs) and 6 months after death (bereavement outcomes); questionnaire posted to primary care team (GP and district nurse) 6 weeks after death (patient spent time at home) Analysis: backwards from death and forwards from death |
|
| Resource use/costs | Institutional days (included hospice, acute hospital and continuing care beds) Hours of home nursing care (generic and palliative care nursing) GP visits (daytime during week, daytime during weekend, evening, night) Other primary and secondary care Time horizon: last year before death (inpatient days and home nursing care); last 2 weeks before death (GP visits and other primary and secondary care) |
|
| Notes |
Power considerations: "The study attained less statistical power than initially planned." Authors planned a 1:1 random allocation of 180 patients to each trial arm to achieve 80% power to detect a 15% difference (from 50% to 65%) in numbers of patients dying at home α = 0.05. Factors contributing to study underpower: unequal randomisation ratio of 4:1 requiring 450 intervention and 110 controls to achieve same power (change from 1:1 to 4:1 was needed to allow for attrition and ensure intervention places were filled for service to operate at full capacity and gain cooperation from health professionals); limited time available for the study (15 months); and the high base rate of death at home in the control group (58%) Of patients randomised to intervention, 73 (39%) were not admitted to service (intention‐to‐treat analysis performed) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Concealment of allocation (RCT / CCT) | Low risk | "The randomization sequence was generated from a statistical table of random numbers and concealed in sequentially numbered, opaque, sealed envelopes" |
| Follow‐up (RCT / CCT) | Unclear risk | 95% for primary outcome (n = 229); 60% at 6 weeks after death (n = 144); 49% at 6 months after death (96/198 caregivers) |
| Blinding (RCT / CCT) | Unclear risk | Objective and standardised primary outcome assessment (death certificate); remaining outcomes: "It was not possible to blind recipients to the fact that the hospital at home service was provided". Researcher blinding not stated |
| Baseline measurement (RCT / CCT) | Unclear risk | Comparison of groups limited to percentage with cancer and living alone, age, gender (no significant differences) |
| Reliability of outcome measurement (RCT / CCT) | Unclear risk | Collected from death certificates for primary outcome and from caregivers (self completed questionnaire; retrospective proxy report for symptoms and patient unmet needs; cross‐sectional self report for post‐bereavement outcomes) |
| Protection against contamination (RCT / CCT) | High risk | Patients/caregivers randomised |
Greer 1986.
| Study characteristics | ||
| Methods |
Design: CBA (patient and caregiver) Methodological quality: 3.5/6a (EPOC CBA checklist) |
|
| Participants |
Country and regions: US, Southern New England, Northern Midwest and Southern California, metropolitan and rural areas Recruitment (1981‐1983, 19 months): trained staff interviewers screened records from 39 hospices (20 community‐based and 19 hospital‐based, both groups provided hospice home care and are hereby called community‐based intervention and hospital‐based intervention, respectively) and 14 conventional oncology care settings (outpatient clinics and oncology units) representing "good" oncology care according to knowledgeable area physicians (control, hereby called conventional care ‐ CC); Medicare and non‐Medicare patients aged ≥ 21 years with cancer confirmed by tissue diagnosis (except for brain and pancreatic cancer), remote metastasis (except for lung, brain and pancreatic cancer), presence of caregiver (this requirement excluded nursing home patients); additional criteria for controls KPS ≤ 50 (i.e. requiring assistance in daily activities) and poor life expectancy in the relatively short‐term (judged by referring physician) Number of patients (outcome sample): 1754 (833 community‐based intervention, 624 hospital‐based intervention, 297 control) Diseases: cancer (1754) Patient characteristics: median age band 65‐74 years; 52% female; 6.7% community‐based intervention, 16.1% hospital‐based intervention, 16.6% controls lived alone ("average" 11.7%) Number of caregivers (outcome sample): 1754 (833 community‐based intervention, 624 hospital‐based intervention, 297 control) Caregiver characteristics: not stated Deaths at end of study: 1754 (100%) Withdrawals/other drop‐outs: 4.4% with no differences among settings |
|
| Interventions | Home palliative care vs. usual care "Hospice care" Type: intermediate palliative care Service base: 20 community‐based hospices without inpatient beds (intervention1 ‐ HC), 19 hospital‐based hospices with inpatient beds (intervention2 ‐ HB) Team: medically supervised interdisciplinary teams composed of several individuals with appropriate skills including professionals and volunteers Responsibility: not stated (although team is medically supervised) Description: intervention grounded on hospice and humanistic philosophy of caring for terminally ill patients and their families (as per National Hospice Organization's 1979 standards of hospice programme of care); palliative, preventive, supportive, less resource‐intensive and with more informal care (family and volunteers) than CC; repertoire of services including palliative care and control of symptoms, physical, emotional and spiritual distress, with emphasis placed upon care in the home, individualised care plan and provision, choices about treatment and place of death; supportive care for the family during the dying process and bereavement (this may include follow‐up visits), maximum accessibility to care regardless time of day or ability to pay, and treating the patient and caregivers as a unit; inpatient and HC services closely integrated to ensure continuity and co‐ordination of care; care available 24/7; education programme (for patient, family and team) Duration: "average" length of stay ‐ intervention 1: 72 days and intervention 2: 63 days, half of all patients dead within 35 days of admission, nearly 20% stayed 10 days or less Control: CC "promotes aggressive care rather than palliative care; is directed by a physician with limited input from other professionals, focuses treatment on only the identified patient; generally ceases to provide services after death occurs; and varies greatly in quality depending upon the financial resources of the patient and the time at which services are most needed" |
|
| Outcomes | Quality of life (primary outcome) Death at home Patient at home as long as wanted Caregiver satisfaction with place of death Pain Symptom severity Psychological well‐being (emotional quality of life) Social functioning (social quality of life, hours of social visiting, chatting with household members) Spiritual well‐being Quality of death Awareness Physical function Survival Patient and caregiver satisfaction with care Caregiver pre‐bereavement outcomes (anxiety/depression, caregiver burden, increased drinking, medication use for anxiety and depression) Caregiver post‐bereavement outcomes (grief intensity, medication use for anxiety and depression) Assessment points: baseline, 7 days after and 14 days thereafter until death (last measure "on average" 7 days before death and penultimate measure approximately 21 days before death with no differences among settings); 90‐120 days after death for post‐bereavement outcomes Analysis: forward from enrolment, backwards from death and forwards from death |
|
| Resource use/costs | Institutional days Home nursing visits, home health/homemaker visits, social services/other therapies visits, physician and outpatient clinic visits Social services (general counselling, legal/financial counselling, paperwork assistance, help getting services, self care training) Aggressive interventions (radiotherapy, surgery, chemotherapy or hormonal therapy, thoracentesis) Diagnostic tests (blood tests, x‐rays, or scans) Respiratory support intervention (oxygen, respiratory therapy) Analgesics (for a subsample of 181 patients) Palliative radiation (for a sub‐sample of 2 clinical profiles) Informal care (hours of direct care help from primary care person) Caregiver post‐bereavement healthcare use (hospitalisation, number of physician's visits) and bereavement absenteeism from work Time horizon: from enrolment to death; last 3, 2 and 1 week before death Costs: inpatient, HC, physician visits, outpatient clinic visits, drugs, supplies and equipment expenditures, total costs per study day (included all the former) Currency: 1982 USD |
|
| Notes |
Power considerations: "Sample sizes are predicated upon a 95% confidence limit, or at α = 0.05. The differences between samples are expressed as percentages of the mean on the QLI scale which ranges from 0 to 10. A difference of at least 15% on this scale will be accepted as a true difference. A sample size of 304 conventional care patients will be required to assure that 80% of the time we will be correct in assuming a true difference actually exists"; "a minimum of a 20% difference in the terminal care health costs associated with the two samples will be accepted as a true difference. At a desired power level of 0.8, a sample size of 404 patients in the conventional care group will be required" Considerations about hospice care sites (i.e. intervention): initial number of hospices involved was 40 but 1 hospital‐based hospice was excluded from all analyses since it provided virtually no HC service; 26 were demonstration sites (receiving Medicare demonstration waiver allowing payment for normally non‐covered services) but analyses of patterns of care and of quality of life showed no differences between demonstration and non‐demonstration hospices thus these were aggregated Only patients who died during the study period were included in analyses since outcomes were assessed in relation to proximity to death Self report data are from first and second patient interview rather than those interviews closest to death; most patients were unable to communicate as they approached death (e.g. patient self reports on pain could not be completed by 50% patients at 2 weeks before death and 80% at 1 week before death) thus caregiver reports were used |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Baseline measurement (CBA) | High risk | Significant differences in age, family income, living alone, caregiver employment, KPS (hospital‐based intervention group was more functionally impaired than community‐based intervention), hospitalisation in 2 months prior to study (control and hospital‐based intervention more often than community‐based intervention); analysis adjusted for differences in patient case mix |
| Characteristics of intervention and control providers (CBA) | Unclear risk | Limited information on providers' characteristics |
| Blinded assessment of outcomes (CBA) | Unclear risk | Blinding not stated; source of some information not stated; mix of self and proxy reports |
| Protection against contamination (CBA) | Low risk | Second sites used as controls |
| Reliable outcome measurement (CBA) | Unclear risk | Source of some information not stated (e.g. place of death); mix of self and proxy reports |
| Follow‐up of patients/caregivers (CBA) | Low risk | 4.4% drop‐outs with no differences among settings |
Harding 2004.
| Study characteristics | ||
| Methods |
Design: CCT (patient and caregiver) Methodological quality: 2/6a (EPOC RCT/CCT checklist) |
|
| Participants |
Country and regions: UK, London, metropolitan area Recruitment (date and length not stated): from clinical nurse specialists of 2 home palliative care services; patients with life expectancy ≥ 3 weeks and with adult caregivers (staff estimated); allocated to intervention or control according to caregiver preference. Exclusion criteria: lack of fluency in spoken English Number of patients (initial inclusion): 77 (40 intervention and 37 control) Diseases (baseline sample): cancer (63), HIV (4), MND (2), Bechet's disease (1), CHF (1), Leigh's syndrome (1), Parkinson's disease (1) Patient characteristics: mean age 65 years Number of caregivers (initial inclusion): 77 (40 intervention and 37 control) Caregiver characteristics: mean age 59.2 years; 69% female Deaths at end of study: not stated Withdrawals/other drop‐outs: 4 intervention caregivers (unable to do baseline measures) |
|
| Interventions | Reinforced vs. standard home palliative care Additional component: "90 Minute Group" Type: specialist palliative care Service base: 2 home palliative care teams (base not stated) Team: additional component delivered by a facilitator‐led multi‐professional group (1 facilitator per site); standard home palliative care team composition not stated Responsibility: for additional component – group facilitator (1 per site); for standard home palliative care team – not stated Description: research‐based short‐term caregiver group intervention (following literature review and qualitative study); aimed to promote self care by combining informal teaching with group support (addressing information and support needs of caregivers); 4 principles: 1) lack of identification with the label of 'carer', 2) provision of safe and legitimate time and space away from caring, 3) time limited, 4) respectful of existing coping strategies; 6 weekly 90‐minute sessions with consistent facilitator to introduce multi‐professional input from a changing weekly speaker (welfare benefits advice, occupational therapy and physiotherapy, clinical nurse specialist, and aromatherapy) and to subsequently facilitate group discussion of the weekly themes for a maximum of 12 carers; group initially focused on patient issues in order to provide legitimacy for attending, and to address the patient‐oriented sources of distress; transport and patient‐sitting provided when needed; detailed programmed objectives for each session, weekly facilitators' peer supervision (for intervention consistency); 2 groups delivered at each site; usual home palliative care included 24‐hour home access to specialist nursing, advice and support Duration: additional component lasted 6 weeks; standard home palliative care likely to be provided from enrolment to death (length not stated) Control: specialist home palliative care with 24‐hour home access to specialist nursing, advice, and support (any other service provided by the palliative care teams but no other carer‐specific services were available at the time of the study) |
|
| Outcomes | Physical function Caregiver pre‐bereavement outcomes (burden, coping, general health, anxiety) Assessment points: baseline, 8 weeks (post‐intervention) and 5 months after Analysis: forwards from enrolment |
|
| Resource use/costs | Not assessed | |
| Notes |
Power considerations: "lack of significant quantitative outcome differences in the present study may primarily be a result of the small sample size" Qualitative data on processes and experience of the intervention |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Concealment of allocation (RCT / CCT) | High risk | Allocation based on caregiver preference |
| Follow‐up (RCT / CCT) | High risk | 24 intervention (60%) and 17 control (46%) post‐intervention, 15 intervention (38%) and 11 control (30%) at 5 months |
| Blinding (RCT / CCT) | Unclear risk | Blinding not stated |
| Baseline measurement (RCT / CCT) | Low risk | "the two groups did not differ significantly on age, sex, months of caring, patient physical scores, POS family score, depression, anxiety, or any of the eight composite coping scales" |
| Reliability of outcome measurement (RCT / CCT) | Unclear risk | Collected from caregivers by researchers |
| Protection against contamination (RCT / CCT) | High risk | Patient/caregiver allocation |
Higginson 2009.
| Study characteristics | ||
| Methods |
Design: phase II RCT (patient and caregiver) Methodological quality: 3.5/6a (high quality, EPOC RCT/CCT checklist) |
|
| Participants |
Country and regions: UK, South East London, metropolitan area Recruitment (2004‐2005, 11 months): from local health and social professionals and in a few instances via voluntary groups and self referrals; patients with MS living in South East London, deemed (by clinicians) to have specialist palliative care needs (i.e. 1 or more unresolved symptoms, psychosocial concerns, end of life issues, progressive illness or complex needs); referrals screened by consultant in palliative medicine independent to study. Exclusion criteria: very urgent needs or rapid deterioration (immediate referral to service offered) Number of patients (randomised): 52 (26 intervention and 26 control) Diseases: MS (52) Patient characteristics: mean age 53 years; 69% female; 17.3% lived alone Number of caregivers (randomised): 52 (26 intervention and 26 control) Caregiver characteristics: not stated Deaths at end of study: 4 (1 in the intervention and 3 in the control) Withdrawals/other drop‐outs: 2 controls (1 protocol violation, 1 severely ill) |
|
| Interventions | Home palliative care vs. usual care (fast‐track design with a 12‐week wait) Type: specialist palliative care Service base: King's College Hospital (general public teaching hospital) Team: part‐time consultant in palliative medicine with training in neurology and special interest in MS, part‐time clinical nurse specialist (working in neurology and with some palliative care training), full‐time administrator; easy access to consultant neurologist through weekly multi‐professional MS clinic (in addition to telephone and email contact) to joint review by neurology and palliative care and other relevant professionals; team worked closely with the existing hospital palliative care team, using time from their psychosocial worker (on maternity leave for 7 months during project); weekly meetings to discuss caseload and for consultant to input into management of all patients Responsibility: not stated, "the service aimed to complement and not to replace existing services" Description: new short‐term intervention grounded in previous work (pre‐clinical and phase I comprising systematic reviews and qualitative studies, as per the Medical Research Council framework for the evaluation of complex interventions); referral form – referrers were asked to identify the main issues requiring team's involvement and record in a standard form with criteria based on palliative care need criteria and specific triggers identified by team (hydration and nutrition, advance directives, competency and consent); initial comprehensive assessment – conducted by team member including demographics, ability to communicate, main symptom issues, current medication, psychological concerns, social issues (including care package and agencies involved), caregiver concerns and advance care planning (this took an "average" 110 minutes of direct contact and 90 minutes of liaison/administration); action plan and follow‐up – following assessment, communicated to primary team and other professionals as appropriate, and followed through calls or visits depending on need; specialist welfare benefits advice; bereavement support; crisis prevention; education and support for primary and secondary care; patients were seen in their place of choice (often at home and sometimes at outpatient clinics, nursing home, hospital); 1‐3 contacts per patient (visits or telephone calls or both); referral to longer‐term specialist community palliative care – identification of specialist need by consultant based on WHO definition of palliative care (specifically physical symptoms, integration of psychological and spiritual aspects of care, need for ongoing support for patients and families, terminal care and bereavement support) and referral to local teams for those in need (12%) Duration: 1‐3 contacts Control: usual care, including community and hospital services (e.g. neurologists, MS nurses, district nurses, GPs, rehabilitation, neurological, social services) in first 12 weeks after enrolment, topped up with access to intervention from then onwards; a few patients received home physiotherapy, occupational therapy, specialist rehabilitation services, continence advice, psychological and psychiatric care; emergency access to intervention in case of very urgent needs or rapid deterioration |
|
| Outcomes | Palliative outcomes (primary outcome) Pain Symptom burden Physical and psychological disease impact Caregiver pre bereavement outcomes (burden, mastery, positivity) Assessment points: baseline, 6 and 12 weeks after (primary analysis), 18 weeks (only controls – after receiving intervention) and 24 weeks after Analysis: forwards from enrolment |
|
| Resource use/costs | Formal care (included a range of health, social and voluntary services – inpatient care, respite care, day centre, contacts with district/practice, MS nurse, palliative care nurse, other nurse, general practice, specialist at home, in hospital, in a ward and in other places, occupational therapist, physiotherapist, dietician, chiropodist, dentist, speech therapist, social services, day centre, inpatient care, respite care); informal care (hours of care) Time horizon: 12 weeks following enrolment Costs: mean costs for each of the categories above; difference in total costs per patient: a) including formal and informal care, and b) excluding inpatient and informal care as above Currency: 2005 GBP Cost‐effectiveness: cost‐effectiveness planes for palliative outcomes (primary outcome) and caregiver burden |
|
| Notes | Power considerations: "We estimated that a sample of more than 25 patients in each arm would enable us to detect differences of >2 on the POS‐8 at P < 0.05, power 80% (with a standard deviation [SD] of 2.25) at 12 weeks" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Concealment of allocation (RCT / CCT) | Low risk | "The researcher e‐mailed relevant data to independent statisticians who conducted the randomization using the minimization method to give an equal balance of gender, age, date of diagnosis, and according to whether patients could or could not communicate. (...) The statistician informed researchers who then informed patients of their allocation" |
| Follow‐up (RCT / CCT) | Low risk | 46/52 (89%) at study end |
| Blinding (RCT / CCT) | High risk | "We were unable to blind the interviewers or participants from group allocation" |
| Baseline measurement (RCT / CCT) | Low risk | No significant baseline differences: gender, age, ethnicity, type of MS, education, caregiver characteristics, functional status and outcomes (analysis adjusted for baseline scores) |
| Reliability of outcome measurement (RCT / CCT) | Unclear risk | Face‐to‐face interview with patients using standard measures; self complete questionnaires with caregivers |
| Protection against contamination (RCT / CCT) | High risk | Patients/caregivers randomised |
Hudson 2005.
| Study characteristics | ||
| Methods |
Design: RCT (caregiver) Methodological quality: 2.5/6a (EPOC RCT/CCT checklist) |
|
| Participants |
Country and regions: Australia, Melbourne, Victoria, metropolitan area Recruitment (date not stated, 12 months): from 2 home palliative care services (similar annual admissions and similar to national "average" length of stay of 75 days); new patient referrals (within 1 week) with ECOG Performance Status from 0 to 3, i.e. at least capable of minimal self care; up and about more than 50% of waking hours (criteria to minimise attrition). Exclusion criteria: no caregiver living with patient, patient with intellectual or psychiatric illness or lack of English language skills Diseases: cancer (106) Number of caregivers (randomised): 106 (54 intervention and 52 control) Caregiver characteristics: mean age 60.78 years; 65.1% female Deaths at end of study: not stated Withdrawals/other drop‐outs: 34 intervention and 27 control (non‐response to questionnaire) |
|
| Interventions | Reinforced vs. standard home palliative care Additional component: "psychoeducational intervention" Type: specialist palliative care Service base: 2 home palliative care teams (base not stated) Team: additional component delivered by nurse; standard home palliative care team comprised specialist nurses, doctors, and allied health professionals (similar range of disciplines in each service, including nurses, social workers, medical consultants, pastoral care workers, volunteers and bereavement counsellors) Responsibility: for additional component ‐ nurse; for standard home palliative ‐ team's nurse (not clear if responsibility rested with primary physician/team) Description: additional component grounded on literature and focus groups with nurses and caregivers (current and bereaved); aimed to top up home palliative care with a psychoeducational component to enhance support and guidance for caregivers – this consisted of 2 fortnightly home visits with follow‐up call between visits, structured around and complemented by audiotape with reflections from caregivers and self care strategies and structured relaxation exercise, and guidebook with information on typical aspects of caring for dying person (link provided in paper); caregivers read guidebook sections and noted questions prior to visits ‐ first visit prepared for caregiver role and aspects of caregiving (section 1 and 2 of guidebook); telephone call focused on evaluating plans, self care (section 3), new issues and caregiver desire to go on to next section; second visit focused on evaluating previous strategies, new issues and preparing for dying phase (final section of guidebook) Duration: additional component lasted 2 weeks; standard home palliative care likely to be provided from enrolment to death (length not stated) Control: specialist home palliative care including information and access to services outside the team and spiritual guidance; emergency visits from nurses in addition to pre‐scheduled home visits from team members; 24/7 phone advice |
|
| Outcomes | Caregiver pre‐ and post ‐bereavement outcomes (preparedness, competence, self efficacy, caregiving rewards, anxiety) Assessment points: baseline, 5 weeks after (questionnaire posted 28 days after baseline), and 8 weeks after death Analysis: forwards from enrolment and forwards from death |
|
| Resource use/costs | Not assessed | |
| Notes | Power considerations: "There was insufficient power to detect differences based on a simultaneous comparison of data obtained at all three assessment times (...) only moderate to large effects were likely to be found."; "Owing to time and financial constraints, sample size was not calculated on the basis of a predetermined power and effect size"; "Cohen's power tables were used to determine the power associated with each statistical test based on the pre‐specified effect and sample size (alpha levels were set at 0.05; all tests were two tailed). Power values ranged from 0.70 (t‐test for two independent samples) to 0.99 (t‐test for related samples)" | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Concealment of allocation (RCT / CCT) | Low risk | "Randomization to group occurred via a computer‐generated software system" |
| Follow‐up (RCT / CCT) | High risk | 40 intervention (74%) and 35 control (67%) follow‐up 5 weeks after baseline; 20 intervention (37%) and 25 control (48%) 8 weeks after death |
| Blinding (RCT / CCT) | Unclear risk | Blinding not stated |
| Baseline measurement (RCT / CCT) | Unclear risk | "Chi‐squared tests and t‐tests for independent samples were used to assess the possibility of pre‐existing differences between the standard care and intervention groups based on baseline data"; no results stated, descriptive data not shown |
| Reliability of outcome measurement (RCT / CCT) | Unclear risk | Collected from caregivers by research assistants at baseline and 8 weeks after death (home); self completed by caregivers 5 weeks after baseline (mail) |
| Protection against contamination (RCT / CCT) | High risk | Patients randomised |
Hughes 1992.
| Study characteristics | ||
| Methods |
Design: RCT (patient and caregiver) Methodological quality: 3/6a (EPOC RCT/CCT checklist) |
|
| Participants |
Country and regions: US, Hines, Illinois, metropolitan area Recruitment (1984‐1987, 37 months): from medicine, surgery and neurology acute wards at Edward Hines Jr. VA Hospital; new inpatient admissions with life expectancy < 6 months (estimated by primary physician), presence of caregiver, residence within 30‐mile (48‐km) catchment area Number of patients (randomised): 175 (87 intervention and 88 control) Diseases (baseline sample): cancer (80% of intervention, 73% of control), genitourinary system (5% of intervention, 4% of control), other respiratory (3% of intervention, 4% of control), other (12% of intervention, 19% of control) Patient characteristics: mean age 65.73 years intervention, 63.26 years control; gender distribution not given but stated "predominantly male veterans" Number of caregivers (randomised): 175 (87 intervention and 88 control) Caregiver characteristics: mean age 55.5 years intervention, 56.4 years control; 92% female; 88% intervention caregivers and 97% controls lived with patient; 58% intervention caregivers and 72% controls were spouses Deaths at end of study: 79% intervention and 78% control Withdrawals/other drop‐outs: 2 in the intervention and 2 in the control (entered nursing home before receiving intervention or control) |
|
| Interventions | Home palliative care vs. usual care "Hospital based home care (HBHC)" Type: intermediate palliative care Service base: Edward Hines Jr. VA Hospital (department not stated) Team: physician‐led interdisciplinary team including nurses, social worker, physiotherapist, dietician, health technicians (physician also managed hospital's inpatient intermediate care unit thus maximised potential for continuity of care between home and hospital); team meetings Responsibility: not stated Description: existing service (for 13 years) emphasising on provision of care to high‐risk patients, comprehensive services based on need, importance of timely communication about patients across team members, and instruction and involvement of informal caregivers in patient care to the maximum extent possible; both patient and family constituted unit of care, with education being a strong service component; goal‐oriented, interdisciplinary patient care plans developed at team meetings; scheduled visits according to individual patient needs; physician home visits, pharmaceuticals, and supplies are also included Duration: up to 6 months (mean survival in intervention group 76 days) Control: traditional community HC services, customary care within or outside the VA hospital with exception of access to intervention; control patients could be seen by VA discharge planners and receive community HC or hospice care |
|
| Outcomes | Physical function Cognitive functioning Morale Survival Patient and caregiver satisfaction with care Caregiver pre‐bereavement outcome (morale) Assessment points: baseline and 1 and 6 months after (or if patient died before 6 months after), the caregiver was interviewed within 1 month after death) Analysis: forwards from enrolment |
|
| Resource use/costs | Hospital admission VA services (total hospital inpatient days, intensive care days, rehabilitation days, intermediate bed days, general bed days; ED visits; extended care days; nursing home days; intervention team's visits; outpatient clinic visits) Non‐VA services (private hospital inpatient days, ED visits, ambulatory care visits, community nursing visits, private HC visits, nursing home days) Time horizon: 6 months following enrolment Costs: institutional (VA hospital, private hospital, total hospital costs, total institutional costs including all hospital and nursing home); non‐institutional (outpatient clinic, intervention team, community nursing, total HC costs); total VA costs, total non‐VA costs, total costs including VA and non‐VA costs Currency: 1985 USD |
|
| Notes |
Power considerations: none stated As the study took place at a VA Hospital, 65% patients were male veterans cared for by spouses (92% of caregivers were female) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Concealment of allocation (RCT / CCT) | Unclear risk | Patients with caregivers "randomly assigned"; details of process not stated |
| Follow‐up (RCT / CCT) | Unclear risk | 96 patients at 1‐month follow‐up (55%) and 34 at 6 months; 149 caregivers at 1 month (85%) and 72 at 6 months (41%); 59 at 1 or 6 months after death (34%) |
| Blinding (RCT / CCT) | Unclear risk | Blinding not stated |
| Baseline measurement (RCT / CCT) | Low risk | No significant differences at baseline (demographic, clinical and outcomes) |
| Reliability of outcome measurement (RCT / CCT) | Unclear risk | Collected from patients or caregivers or both by interviewers face‐to‐face |
| Protection against contamination (RCT / CCT) | High risk | Patients/caregivers randomised |
Jordhøy 2000.
| Study characteristics | ||
| Methods |
Design: cluster RCT (patient and caregiver) Methodological quality: 3.5/6a (high quality, EPOC RCT/CCT checklist) |
|
| Participants |
Country and regions: Norway, Trondheim, 6 metropolitan and 2 rural areas Recruitment (1995‐1997, 32 months): from hospital departments, particularly gastrointestinal surgery, urological surgery, oncology and gynaecology, lung and gastrointestinal departments of internal medicine (through professionals, lead nurse and researchers screening visits once or twice per week) and primary care professionals in 8 healthcare districts; patients aged > 18 years with incurable cancer, life expectancy 2‐9 months (not stated who estimated) living in 8 community healthcare districts (clusters) stratified into 3 pairs according to number of inhabitants > 60 years and urban/rural status (2 smaller urban districts merged with larger ones) and randomised to intervention or control. Exclusion criteria: haematological malignant disorders other than lymphomas, patient not informed about their diagnosis and that the disease was incurable, participation in other trials with quality of life as outcome, unable to fill in questionnaire Number of patients (randomised): 434 (235 intervention and 199 control) Diseases: cancer (434): gastrointestinal (181), lung (52), breast and female genitals (67), prostate and male genitals (41), kidney or vesica (29), lymphomas (13), skin (12), others (39) Patient characteristics: median age 70 years intervention, 69 years control; 47% female; 32.5% lived alone Number of caregivers (consented): 313 (183 intervention and 130 control) Caregiver characteristics: median age 57.6 years intervention, 53.9 years control; 68.3% female Deaths at end of study: 395 (219 intervention (93%) and 176 control (88%)) Withdrawals/other drop‐outs: 6 intervention and 10 control (reasons not stated) |
|
| Interventions | Home palliative care vs. usual care Type: specialist palliative care Service base: palliative medicine unit at University Hospital of Trondheim (12 beds, outpatient clinic and consultant team in and out of hospital) Team: 1 full‐time physician; 2 palliative care nurses, social worker, priest, nutritionist, part‐time physiotherapist; staff worked daytime hours only; weekly meetings Responsibility: consultant nurse was the care co‐ordinator; primary family physician and community nurse maintained as main professional carers Description: new intervention grounded on holistic philosophy, included multidisciplinary approach to the patient's needs and co‐ordination of care; consultant team who co‐ordinated care; initial care plan set up in meeting of patient, caregivers, family physician, community nurse, and consultant nurse or physician from team; follow‐up routine consultations by community staff supervised by team (available for joint home visits); no additional out of hours or on‐call service; service linked the palliative medicine unit to community services under pre‐defined guidelines to keep interaction at optimum level; education programme (including bedside training and 6‐12 hours of lecturers every 6 months on symptoms and difficulties in palliative care); inpatient and outpatient services provided at unit except when required for medical reasons (e.g. surgery or acute intensive care for intercurrent disease) Duration: from enrolment to death or study end (median survival 99 days in the intervention group) Control: usual care shared among University hospital departments and community services according to diagnosis and medical needs (no well‐defined routines existed and poor communication between levels of services had been addressed as general problem); despite minor variations, community services were similar in all districts, including family physicians, HC nursing (nurses and nurse‐assistants) and nursing homes (when extensive need for attention or basic nursing care but not specialised hospital care is required); all except smallest urban district had 24 hours HC; limited night coverage (generally only short visits or telephone consultations); HC and nursing home services co‐ordinated at district level (common community nursing office ‐ decisions based on patient's medical and social needs and current availability of community resources); no specialist palliative care service available other than the intervention |
|
| Outcomes | Quality of life (primary outcome) Physical symptoms (pain – primary outcome; breathlessness, nausea/vomiting, constipation, diarrhoea, sleep disturbance, fatigue, appetite loss) Physical function (primary outcome) Psychological well‐being (primary outcome; emotional functioning and psychological stress) Death at home (primary outcome) Death in hospital Death in hospital palliative care unit Death in nursing home Percentage of time spent at home General health and vitality Social functioning Survival Caregiver satisfaction with care Caregiver pre‐bereavement outcomes (quality of life, general health, vitality, physical, psychological and social functioning, bodily pain) Caregiver post‐bereavement outcomes (quality of life, general health, vitality, physical, psychological and social functioning, bodily pain, grief intensity) Assessment points: baseline and monthly until death (or up to 2 years to avoid research burden); satisfaction with care measured 1 month after death; caregivers assessed 1, 3, 6 and 13 months after death Analysis: forwards from enrolment, backwards and forwards from death (caregivers' outcomes) |
|
| Resource use/costs | Hospitalisations (admission, number of admissions, mean length of admission, inpatient days, proportion of time in hospital) Care in nursing homes (admission, number of admissions, nursing home days, proportion of time in nursing homes) Time horizon: from enrolment to death or study end; last month before death |
|
| Notes |
Power considerations: "Pre‐planned sample size was 200 patients in each group, based on quality of life."; "Because there was uncertainty about the likely difference, the impact of a variety of effect sizes was explored. Between 50 to 75 patients per group would be realistic to detect differences as small as 0.5 SDs in an ordinary randomized clinical trial (RCT), an effect size that is commonly regarded as a moderate change, and for which the EORTC QLQ‐C30 scores are roughly comparable to a change of 10 units. This represented a plausible and realistic effect of the intervention policy. However, for a cluster randomized design, the statistical power will be reduced because of within‐cluster correlation. This can be taken into account by increasing the total number of clusters, or to a lesser extent, by increasing the number of subjects per cluster. In this trial, for practical and economical reasons, participation had to be restricted to the clusters (health care districts) located within close reach from the palliative medicine unit, and it was decided to include 200 patients in each treatment group" Authors discuss issues related to recruitment attrition, and compliance in a methodological paper. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Concealment of allocation (RCT / CCT) | Unclear risk | "Cluster randomised design"; unit of allocation was health district but random process not explicit |
| Follow‐up (RCT / CCT) | Unclear risk | Patients: 153 intervention (65%) and 116 control (58%) follow‐up at 1 month on questionnaire‐based measures (including primary outcomes); 219 intervention (93%) and 176 control (88%) on place of death Caregivers: 113 (49%) intervention and 70 control (36%) 1 month after death |
| Blinding (RCT / CCT) | Unclear risk | Not stated |
| Baseline measurement (RCT / CCT) | Unclear risk | Significant differences in diagnosis (intervention more gastrointestinal/lung, less breast/prostate/kidney/vesica/lymphoma/skin), housing (intervention higher proportion living in villa/apartment), access to informal help (intervention higher) and receipt of HC nursing (intervention lower); unclear if all are in same direction as results. No significant baseline differences in quality of life (1 of primary outcomes) |
| Reliability of outcome measurement (RCT / CCT) | Unclear risk | Questionnaire‐based measures were self completed; source of data on place of death not stated |
| Protection against contamination (RCT / CCT) | Low risk | Health districts randomised |
McCorkle 1989.
| Study characteristics | ||
| Methods |
Design: RCT (patient and caregiver) Methodological quality: 2.5/6a (EPOC RCT/CCT checklist) |
|
| Participants |
Country and regions: US, Washington, King County, rural and urban areas Recruitment: (1983‐1985, 18 months): from cancer registries and pathology reports in 19 hospitals and 1 radiation outpatient facility; newly diagnosed stage II lung cancer patients (included squamous cell, adenocarcinoma, small cell, giant cell cancer), King County residence, meeting Medicare criteria for homebound (i.e. unable to use public transportation on a routine basis without assistance). Exclusion criteria: judged by physician as too ill to participate, receiving standard home nursing care in prior 6 months, enrolled in home health agency Number of patients (randomised): 166; (outcome sample): 78; 24 intervention, 27 control1, 26 control2 (group for 1 patient not stated) Diseases: cancer (166); all primary site lung Patient characteristics: aged 18‐89 years; 37% female Number of caregivers (eligible): 127; (outcome sample): 46 Caregiver characteristics: not stated Deaths at end of study: 87 (52%) Withdrawals/other drop‐outs: 24 patients (11 too sick to handle interviews, 5 caregivers refused interview, 3 caregiver or patients or both unable to cope with questions, 3 patients moved out of King County, 2 unknown); 81 caregivers at bereavement follow‐up (30 refused, 9 did not complete first interview, 21 patients still alive, 10 lost to follow‐up, 11 incomplete data) |
|
| Interventions | Home palliative care vs. usual care (2 control groups) "Specialized Oncology Home Care Program – OHC" Type: intermediate palliative care Service base: not stated Team: nurses with masters' degrees and trained to give personalised clinical care to persons with advanced cancer and their families; advanced training on knowledge of symptom management, cancer treatments, pain management, physical assessment, psychosocial assessment, grief and mourning theory, communications systems, community resources and agencies, systems analysis, self support, professional role development, pathophysiology of death, and research theory and methodology; specialised services by other disciplines called upon as needed Responsibility: nurse was care co‐ordinator (not clear if patient's primary physician remained in charge) Description: intervention grounded on Oncology Transition Services model (personalised care in home setting with key features including advanced education in cancer symptom management, nurse being central care co‐ordinator, 24‐hour access to nursing staff) Duration: not stated but likely to be from enrolment to death Control: control1 (HC) consisted of care provided by an interdisciplinary team (RNs, physiotherapists, home health aides, medical social work, occupational therapist and a speech pathologist); upon referral, the patient was assigned to team members appropriate to meet the patient's needs as identified on referral and approved by the patient's physician; entire team discussed treatment and case management plans, co‐ordination of visits, length and intensity of services, need for consultation, co‐ordination with physician, family and community resources, and discharge from care; this represented standard Medicare‐reimbursed services available in the community. Control2 (outpatient care) consisted of care provided by the patient's physician and outpatient staff (traditional treatment for cancer patients) with no general or specialised home nursing care |
|
| Outcomes | Pain Symptom distress General health Physical function (enforced social dependency) Psychological distress (mood, psychosocial concerns) Caregiver post‐bereavement outcomes (psychological distress) Assessment points: baseline (from 8 to 10 weeks of diagnosis), and 6, 12, 18, 24 weeks after; baseline, 6 weeks after death and then 6, 13 and 25 months after Analysis: forwards from enrolment and forwards from death |
|
| Resource use/costs | Hospitalisations (admission, number of admissions, inpatient days) Time horizon: 6 months following enrolment |
|
| Notes |
Power considerations: none stated Data collected on fifth and last time point (24 weeks after baseline) not analysed because of small sample size (n = 55, 33% of initial sample) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Concealment of allocation (RCT / CCT) | Unclear risk | "subjects were assigned randomly after the initial interview was completed"; no details of process |
| Follow‐up (RCT / CCT) | High risk | 78 patients (47%) follow‐up at fourth interview (18 weeks after baseline); 46/127 (36%) caregivers |
| Blinding (RCT / CCT) | Unclear risk | Double‐blind at baseline; not stated for follow‐up |
| Baseline measurement (RCT / CCT) | Unclear risk | "Chi‐square tests indicated no statistically significant group differences on demographic variables"; intervention group did "notably better" at baseline on most outcomes; analyses adjusted for baseline scores (covariates); no differences in caregivers baseline psychological distress |
| Reliability of outcome measurement (RCT / CCT) | Low risk | Patients and caregivers completed the baseline questionnaires upon enrolment and the follow‐up questionnaires mailed to them |
| Protection against contamination (RCT / CCT) | High risk | Patients randomised |
McKegney 1981.
| Study characteristics | ||
| Methods |
Design: cluster RCT (patient) Methodological quality: 4/6a (high quality, EPOC RCT/CCT checklist) |
|
| Participants |
Country and regions: US, Vermont, rural area Recruitment (date not stated, "four‐year study"): from radiotherapy and medical oncology clinics at Vermont Regional Cancer Center; new patients with cancer (histologically confirmed) aged ≥ 16 years with life expectancy from 3 months to 1 year (judged by experienced oncologist) living in Vermont counties; counties randomly allocated to intervention and control (number of counties not stated, paired based on population density, distance from centre, socioeconomic status, local medical facilities, referral patterns and local social services). Exclusion criteria: patients mentally incompetent Number of patients (allocated): 199 (98 intervention and 101 control) Diseases: cancer (199) Patient characteristics (primary outcome sample of 83 patients): mean age 58.7 years intervention, 56.1 years control; 42% female Deaths at end of study: 139 (70%) Withdrawals/other drop‐outs: not stated |
|
| Interventions | Home palliative care vs. usual care "Intensive home care" Type: intermediate palliative care Service base: Vermont Regional Cancer Center (department not stated) Team: trained oncology nurse practitioners with "extensive experience in care of the patients with advanced cancer" backed up by usual multidisciplinary team of nurses, medical and radiation oncologists, dieticians, enterostomal therapist, physiotherapists, occupational therapists, psychiatrists, social workers and clergymen at the cancer centre; formal interdisciplinary training on extended assessment skills (sophisticated approach to physical, psychological, nutritional and financial assessments of both patients and families); weekly team conferences Responsibility: team's nurse (acting as link between the multidisciplinary team and care co‐ordinator responsible for following patients through home visits, clinic visits and hospitalisations to ensure continuity of care; primary physician informed and collaborating in complex medical problems) Description: intervention designed to improve patient's quality of life and communication between the conventional cancer rehabilitation team and the patient by assigning oncology nurses to closely monitor and co‐ordinate patient care; assumed nurses would anticipate and solve medical and psychosocial problems and that their expertise would improve quality and extend survival; initial interdisciplinary assessment (by each team member) followed by care plan build by nurse; frequency of home visits defined based on prognosis (life expectancy < 3 months – biweekly; ≥ 3 months – monthly); home visits (35‐40 minutes) focused on patient needs ("incidental interactions with family"); physical care, talking with patient about illness and implications, mobilising family and social resources and co‐ordinating with patient's physician; protocol for pain management (in varying degrees of pain), nausea, vomiting and administration of intravenous chemotherapy drugs at home (available from authors); pain killers given regularly to ensure continuous control Duration: not stated but likely to be from enrolment to death or study end (mean survival in intervention group was 345 days) Control: usual care provided by multidisciplinary team at cancer centre and patient's local/private physician |
|
| Outcomes | Pain (primary outcome) Physical activity/function Nutrition Psychological well‐being (optimism) Survival Assessment points: baseline and then timed with nurse visits (biweekly for patients with life expectancy < 3 months; monthly for those with ≥ 3 months) Analysis: backwards from death |
|
| Resource use/costs | Hospital inpatient days Time horizon: not stated |
|
| Notes |
Powerconsiderations: none stated Potential for measurement bias: less frequent assessments for patients with longer life expectancy (assessment timed with nurse visits, frequency of visits decided based on patient estimated life expectancy) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Concealment of allocation (RCT / CCT) | Unclear risk | "paired counties were randomly separated into two groups"; process not stated |
| Follow‐up (RCT / CCT) | Unclear risk | 38 intervention (39%) and 45 control (45%) follow‐up (minimum of 3 time points on pain backwards from death, primary outcome); not stated for other outcomes |
| Blinding (RCT / CCT) | Unclear risk | Not stated |
| Baseline measurement (RCT / CCT) | Low risk | "A comparison of patient characteristics for these two groups demonstrated similarities in cancer diagnosis, sex, age, social class, and religious preference. The initial, on‐study scores on the CMI, I‐E, and KPS did not differ significantly"; "When pain levels (…) were compared over time, in 30‐day periods before death, the two groups had essentially the same mean pain scores until the last 90 days before death" |
| Reliability of outcome measurement (RCT / CCT) | Unclear risk | "by trained independent raters, using structured interviews in the patients' homes, done at the same frequency as the nurses' visits, which were based upon the patients' prognosis. Follow‐up interviews were carried out in the patients' homes because earlier data had indicated greater validity of home vs. clinical evaluations for some measures. Initial and follow‐up rater training took place during the pilot phase of the project using videotapes. At the end of the first year the raters had achieved acceptable interrater agreement on major scale items (Pearson correlation coefficient 0.70)" |
| Protection against contamination (RCT / CCT) | Low risk | Counties randomised |
McMillan 2007.
| Study characteristics | ||
| Methods |
Design: RCT (patient and caregiver) Methodological quality: 2.5/6a (EPOC RCT/CCT checklist) |
|
| Participants |
Country and regions: US, Tampa, Florida, metropolitan area Recruitment (1999‐2003, 50 months): sample drawn from large non‐profit community‐based hospice face sheets; consecutive new cancer patients aged ≥ 18 years living in study county, with a caregiver and problems with at least 2 symptoms (pain, breathlessness, constipation). Exclusion criteria: patient low level of consciousness (assessed by admission team), excessively debilitated (≥ 40 score on Palliative Performance Scale) or actively dying, admitted to inpatient hospice or assisted‐living facility or nursing home; patient and caregiver < sixth grade education, unable to read or understand English, ≥ 7 in Short Portable Mental Status Questionnaire, caregiver in active treatment for cancer themselves Number of patients (randomised): 329 (111 intervention, 109 control1, 109 control2) Diseases: cancer (329) Patient characteristics: mean age 70.84 years intervention, 71.02 years control1 and 70.12 years control2; 39.9% female Number of caregivers (randomised): 329 (111 intervention, 109 control1, 109 control2) Caregiver characteristics: mean age 63.06 years intervention, 61.53 years control1, 59.98 years control2; 85.4% female Deaths at end of study: not stated Withdrawals/other drop‐outs: "Most commonly, attrition was due to patient decline (29%) or death (21%), and the caregiver feeling overwhelmed (23%), which was largely associated with patients' worsening condition" |
|
| Interventions | Reinforced vs. standard home palliative care (2 control groups) Additional component: "COPE Intervention" Type: specialist palliative care Service base: large non‐profit community‐based hospice Team: additional component delivered by newly hired nurses (1 full‐time and 1 back‐up) and home health aides with hospice experience; 4 day training on intervention with role‐play; composition of standard home hospice care team not stated (cared for 850 patients/day) Responsibility: for additional component – nurse; for standard home hospice care team – not stated Description: home hospice care with new additional brief psychoeducational support (COPE intervention); caregiver problem‐solving education component grounded on conceptual and research literature on stress process models and problem solving training and therapy; 9‐day intervention with 3 visits (first 45 minutes, second and third 30 minutes) and continued support in between with calls to assess problems, offered support and answer questions and nurse pager contact; intervention adapted to teach a problem‐solving method to assess and manage patient symptoms (focus on pain, dyspnoea and constipation); 4 components:
Duration: 9 days for additional component; duration of standard home hospice care not stated but likely to be from admission to death Control: control1 ‐ standard specialist home hospice care with additional supportive visits from intervention nurse and home health aide (same visit frequency and length as intervention); nurse provided individual caregiver support, discussed feelings, fears, and relationship with patient; trained not to give advice about managing problems and not to teach structured problem‐solving skills (e.g. dealt with questions asking about advice given by hospice nurse); manual and audiotapes of sessions reviewed monthly to ensure protocols were followed; home health aide provided respite staying with patient during supportive visits; control2 ‐ standard specialist home hospice care, which included some caregiver education and support about symptom management and what to expect with disease progression |
|
| Outcomes | Caregiver pre‐bereavement outcomes (3 primary outcomes ‐ quality of life, burden, mastery; distress with patient symptoms, coping) Physical symptoms (pain, breathlessness and constipation) Symptom distress Quality of life Assessment points: at baseline, 16 days after baseline (1 week post intervention) and 30 days after (2 weeks post intervention) Analysis: forwards from enrolment |
|
| Resource use/costs | Not assessed | |
| Notes |
Power considerations: based on power calculations, 160 patient‐caregiver dyads were sought for each group (n = 480) Authors discussed challenges of recruitment in methodological paper: large amount of time spent screening face sheets (to bypass nurse gatekeeping) for very low proportion of eligible patients (5%), need to delay recruiting from 24 up to 48 hours after hospice care admission (to avoid time of transition and opt out of curative treatment), attrition due to decline and death (69% 30 days after baseline); this led to extension of recruitment period, problems with generalisability and adjustments to study budget |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Concealment of allocation (RCT / CCT) | Low risk | "randomly assigned to the three treatment conditions at baseline by using a computerized randomization procedure by telephone" |
| Follow‐up (RCT / CCT) | High risk | 42 intervention (38%), 47 control1 (43%), 60 control2 (55%) at 16 day follow‐up; 31 intervention, 32 control1, 40 control2 at 30‐day follow‐up |
| Blinding (RCT / CCT) | Unclear risk | Single‐blind: self completed questionnaires administered without offer of information or assistance; "research assistants were blind to treatment conditions and had contact with intervention staff only at regularly scheduled staff meetings where individual cases were not discussed" |
| Baseline measurement (RCT / CCT) | Unclear risk | No significant sociodemographic differences in patient and caregiver characteristics (P value > 0.10); outcome baseline data not reported |
| Reliability of outcome measurement (RCT / CCT) | Unclear risk | Self completed questionnaires administered by blinded research assistants (see above); caregivers overestimated symptom intensity for pain (the difference in mean scores was 1.33 in a 0 to 10 scale), breathlessness (0.78 difference in mean scores in a 0 to 10 scale) and constipation (1.08 difference in mean scores in 0 to 16 scale); all 3 differences were very significant (paired t‐tests; P value < 0.001). Pearson correlation coefficients were 0.40, 0.46 and 0.51, respectively |
| Protection against contamination (RCT / CCT) | High risk | Patients/caregivers randomised |
McWhinney 1994.
| Study characteristics | ||
| Methods |
Design: RCT (patient and caregiver) Methodological quality: 3/6a (EPOC RCT/CCT checklist) |
|
| Participants |
Country and regions: Canada, London, Ontario, metropolitan area Recruitment (date and length not stated): from family physicians and HC nurses (with "strenuous efforts to attract referrals, including an information sheet for family doctors and presentations to medical meetings" resulting in short lived increases); patients aged ≥ 18 years with symptomatic cancer metastasised or spread to surrounding tissues, life expectancy ≥ 2 months and being cared for at home by an eligible caregiver Number of patients (randomised): 146 Number of caregivers (randomised): 146 Diseases: cancer (146) Patient and caregiver characteristics: not stated Deaths at end of study: 36 within the first month (25%) Withdrawals/other drop‐outs: 14 patients (10%) and 72 caregivers (49%) failed to complete 1‐month questionnaire; 3 patients with reasons unknown |
|
| Interventions | Home palliative care vs. usual care (fast‐track design with 4 weeks' wait) "Palliative care home support team" Type: specialist palliative care Service base: 14 bed palliative care unit (host organisation not stated) Team: physician, 2 experienced palliative care nurses (working 1 week on, 1 off) and a part‐time social worker Responsibility: family physician and HC nurses (team was consulting and support service only) Description: existing service (available for 18 months) with weekly team meetings but limited description of its aim and components; included initial full nurse assessment at home within 3 days of referral; care plan was then discussed with team's physician and copies sent to family physician, home nurse and case manager; involvement of team after assessment varied from no further contact to monitoring telephone calls to periodic visits and close relationship (dependent on wishes of patient and family and negotiation with family physician and home nurse); 24‐hour on‐call nursing with physician back up and contact given (if family physician and home nurse not available); team's physician consultation available on request (not clear if at home) Duration: not stated Control: range of HC services from family physician, HC nurses and case manager (without 24‐hour coverage) and admission to palliative care unit if needed in first 4 weeks after enrolment, topped up with access to home palliative care team from then onwards; emergency consultation with team's physician available to waiting list group in first 4 weeks if requested by family physician |
|
| Outcomes | Physical symptoms (primary outcomes – pain and nausea) Quality of life Caregiver pre‐bereavement outcome (depression) Assessment points: baseline and 1 and 2 months after Analysis: forwards from enrolment |
|
| Resource use/costs | Not assessed | |
| Notes |
Power considerations: "The number of patients necessary for the trial was calculated on the basis of a reduction of 33% in the main outcomes of pain and nausea. With a α level of 0.05 and a β of 0.20, it was calculated that 110 patients would be required for each group, allowing for 20% attrition."; "because of early deaths, problems with recruitment, and a low compliance rate for completion of questionnaires, the required sample size was not attained" Authors discussed challenges of recruitment in a methodological paper: problems emerged within 3 months of start of study: some patients who did not enter the study because of a predicted early death were found to be eligible when assessed by the team; eligible referrals varied widely from month to month, with the "average" (3.7 per week) being less than predicted; inpatient admission to palliative care unit soon after baseline assessment either due to inaccurate prognosis or unexpected deterioration (exposure to standard of palliative care equivalent to offered by home team); failure of some patients and caregivers to complete questionnaires at 1 month (due to weakness, exhaustion, cognitive impairment) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Concealment of allocation (RCT / CCT) | Low risk | "Conducted randomisation using a computer generated table of random numbers" |
| Follow‐up (RCT / CCT) | High risk | 93 patients (64%) and 74 caregivers (51%) follow‐up at 1 month |
| Blinding (RCT / CCT) | Unclear risk | Single‐blind: a research assistant blinded to assignment provided and collected questionnaires from patients and caregivers at home; patient and caregiver blinding not stated |
| Baseline measurement (RCT / CCT) | Unclear risk | Sample characteristics at baseline not reported nor discussed |
| Reliability of outcome measurement (RCT / CCT) | Low risk | Questionnaires with outcome measures self completed by patients and caregivers and collected from their home by research assistant (blinded) |
| Protection against contamination (RCT / CCT) | High risk | Patients/caregivers randomised |
Rabow 2004.
| Study characteristics | ||
| Methods |
Design: Cluster RCT (patient) Methodological quality: 3.5/6a (high quality, EPOC RCT/CCT checklist) |
|
| Participants |
Country and regions: US, San Francisco, California, metropolitan area Recruitment (date not stated, 14 months): from 70 physicians in a general medicine practice at University of California Medical Center (tertiary care), adult patients with diagnoses of cancer (metastatic, albumin less than 2.5 mg/dL or a 6‐month weight loss > 10%), advanced COPD (FEV1 < 30% predicted, oxygen saturation < 88% or dyspnoea at rest) or advanced CHF (ejection fraction < 20% or NYHA class IV symptoms) with life expectancy 1‐5 years and not yet ready for hospice care; 1 clinic module randomly assigned to intervention and second module assigned to control (each comprised separate patients and physicians originally assigned based on space and appointment availability, housed in the same building, but with separate waiting areas and nursing and clerical staff). Exclusion criteria: non‐melanoma skin cancers, dementia, psychosis, enrolled in hospice care, unable to complete a written survey in English or Spanish Number of patients (allocated): 90 (50 intervention and 40 control) Diseases: cancer (30), CHF (31), COPD (29) Patient characteristics: mean age 67.9 years intervention, 69.4 years control; 64% female; 43.3% lived alone Deaths at end of study: 15 (17%); 10 intervention (20%) and 5 control (13%) Withdrawals/other drop‐outs: 5 in the intervention (6%) and 4 in the control (10%) (reasons not stated) |
|
| Interventions | Home palliative care vs. usual care 'Comprehensive Care Team (CCT)' Type: intermediate palliative care Service base: general medicine practice at University of California Medical Center Team: 3 physicians, nurse, social worker, chaplain, pharmacist, psychologist, art therapist, volunteer co‐ordinator (all except latter had expertise in palliative care), volunteer medical and pharmacy student patient advocates; regularly scheduled physician led meetings; the team collaborated with spiritual care service, art for recovery programme, centre for collaborative primary care, nationally recognised family support programme, local non‐profit community hospice Responsibility: social worker responsible for case management; team's physician advised primary physician who retained responsibility for medical care Description: new intervention (demonstration project) grounded on social work centred case management approach with interdisciplinary team consultation integrated with family caregivers and primary physicians; "mixed management" model allowing simultaneous palliative and curative management care for multiple types of illness; aimed to improve advance care planning, reduce healthcare utilisation, and support caregivers; included primary care physician consultation, case management, group, volunteer and chaplaincy support, artistic expression; focused on 7 components:
Duration: 1 year Control: described as usual primary care |
|
| Outcomes | Place of death Physical symptoms (primary outcome: pain; breathlessness and sleep) Psychological well‐being (anxiety, depression) Quality of life Patient satisfaction with care Spiritual well‐being Advance care planning Assessment points: baseline and 6 and 12 months after Analysis: forwards from enrolment |
|
| Resource use/costs | Primary care clinic visits Speciality clinic visits Urgent care clinic visits ED visits Hospitalisations (number of admissions and inpatient days) Time horizon: from enrolment to death or study end Costs: primary care visits, urgent care clinic visits, ED visits, inpatient services, other charges, total medical centre charges Currency: USD (date not stated) |
|
| Notes |
Power considerations: "Power calculations were made based on the ability to detect a 10% change in pain score on a 0–10 scale. Study sample size was recalculated once preliminary data from the initial surveys was available to customise the power assessment. Based on the close similarity between intervention and control patients as well as the unexpectedly high severity of baseline symptoms, recruitment goals were amended from 150 to 50 in each group" Patients meeting inclusion criteria were identified through computerised searches of electronic medical records and recruited to intervention or control based on module affiliation. Primary physicians were given lists of patients they had seen in last 3 months and asked to identify the "sickest patients" with cancer, CHF or COPD who were expected to die within 1‐5 years 4 USD10 grocery store incentive gifts provided to controls |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Concealment of allocation (RCT / CCT) | Low risk | "On the basis of a coin flip, patients in one clinic module (GMA) were assigned to be the intervention group and patients in the second module (GMB) were assigned to the control group" |
| Follow‐up (RCT / CCT) | High risk | 35 intervention (70%) and 31 control (78%) completed study |
| Blinding (RCT / CCT) | Unclear risk | Not stated |
| Baseline measurement (RCT / CCT) | Low risk | No significant baseline differences on outcomes, demographic and clinical characteristics apart from gender (more female patients in intervention; P value = 0.05). Analysis controlled for baseline scores (entered as covariates) |
| Reliability of outcome measurement (RCT / CCT) | Unclear risk | "A member of the CCT clinical team (for intervention patients) or research staff (for controls) brought the survey to the study subject at home or during a clinic visit and supervised its completion" |
| Protection against contamination (RCT / CCT) | Unclear risk | Clinics within same practice randomised |
Tramarin 1992.
| Study characteristics | ||
| Methods |
Design: RCT (patient) Methodological quality: 2.5/6a (EPOC RCT/CCT checklist) |
|
| Participants |
Country and regions: Italy, Vicenza health district and surroundings, metropolitan and rural areas Recruitment (1990, 1 month): from infectious diseases department at San Bortolo General Hospital;
Number of patients (allocated): 42 (10 intervention and 32 control; 7 randomised controls and 25 non‐randomised who did not meet ≥ 1criteria above) Diseases: AIDS (42) Patient characteristics: median age 28.0 and 31.3 years intervention (stage 2 and 3, respectively), 30.6 and 32.5 years control (stage 2 and 3, respectively); 21% female Deaths at end of study: 22 (5 intervention and 17 control) Withdrawals/other drop‐outs: 1 intervention (care refusal) and 2 controls (attending other AIDS clinics) |
|
| Interventions | Home palliative care vs. usual care "Home‐care Assistance" Type: intermediate palliative care Service base: infectious diseases department at San Bortolo Hospital, with 15 beds, outpatient clinic and hospice offering HC Team: multidisciplinary team of 4 trained nurses, 1 psychologist, 10 volunteers, social workers (where available), 2 infectious disease specialists; family doctor seen as part of team Responsibility: consultant doctor; "personnel (medical and paramedical) employed in the referral infectious disease department are responsible for home care"; "other caregivers (family doctors, volunteers, social care agencies) should participate under supervision of consultant doctors of the referral department" Description: integrated package of HC "based on the principles of palliative care"; aimed to improve quality of life whenever possible through symptom control; aligned with National Health AIDS Plan guidelines, aiming to limit use of inappropriate inpatient services by substituting with more suitable palliative care; chemotherapy, parenteral nutrition, blood transfusion and fluids administered if needed at home using a tunnelled catheter Duration: "average" 74.1 days Control: usual care, mainly HB treatment and care |
|
| Outcomes | Quality of life (QWB) Assessment points: weekly from enrolment to death or up to 6 months Analysis: forwards from enrolment |
|
| Resource use/costs | Inpatient (number of hospital admissions, hospital inpatient days, hospital length of stay) Outpatient clinics (number of day admissions) Home palliative care (length of stay, staff hours, nurse and specialist visits) Time horizon: from study entry to death or up to 6 months (multiplied by 2 to produce estimates per person‐year) Costs: inpatient, outpatient, HC and total costs per person‐year Currency: 1990 ITL (converted to 1990 USD using healthcare‐specific purchasing power parities) Cost‐effectiveness: cost‐utility ratio (expressed as cost per well‐week) |
|
| Notes |
Power considerations: none stated Risk of selection bias as 25/32 controls were not randomised Death at home and time spent at home reported for intervention group only (4/9 home deaths; 74.1 days/patient spent at home) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Concealment of allocation (RCT / CCT) | High risk | 17 patients were randomised to intervention (10) and control (7); process not stated; remaining 25 controls not randomly allocated |
| Follow‐up (RCT / CCT) | Low risk | 39/42 (93%) |
| Blinding (RCT / CCT) | Unclear risk | Not stated |
| Baseline measurement (RCT / CCT) | Unclear risk | 25/32 controls failed to meet ≥ 1 of the following criteria – adequate economic and family support, living within 10 km from hospital, willingness to accept HC and stage 2/3 (as opposed to 1); however, comparisons were made only with stage 2/3 patients with no significant differences in age, baseline quality of life scores and risk behaviour categories |
| Reliability of outcome measurement (RCT / CCT) | Unclear risk | Unclear if self report or proxy‐report; "individual QWB scores were calculated each week by a trained caregiver using a standard checklist" |
| Protection against contamination (RCT / CCT) | High risk | Patients randomised |
Walsh 2007.
| Study characteristics | ||
| Methods |
Design: RCT (patient and caregiver) Methodological quality: 2/6a (EPOC RCT/CCT checklist) |
|
| Participants |
Country and regions: UK, London, metropolitan area Recruitment (2001‐2003, 28 months): from 7 home palliative care services covering 3 regional cancer networks; new patients likely to survive the time taken to introduce the intervention (not stated who estimated) with caregiver scoring > 5/6 in GHQ‐28. Exclusion criteria: caregiver lack of English skills Number of patients (randomised): 271 (137 intervention and 134 control) Diseases: cancer (271): lung (79), gastrointestinal (55), genitourinary (40), head and neck (24), breast (18), others (55) Patient characteristics: not stated Number of caregivers (randomised): 271 (137 intervention and 134 control) Caregiver characteristics: mean age 56.3 years; 79% female Deaths at end of study: 109 (40%); 47 intervention (34%) and 62 control (46%) Withdrawals/other drop‐outs: 21 intervention and 18 control (refusals) |
|
| Interventions | Reinforced vs. standard home palliative care Additional component: "Carer Advisor Intervention" Type: specialist palliative care Service base: 2 hospital‐based, 2 community‐based, 3 hospice‐based Team: clinical nurse specialists with specialist medical support and sometimes social work support; caregiver advice component delivered by 2 part‐time carer advisors with experience in community nursing and social work (1 month's training involving fieldwork in palliative care in community, hospice and hospital settings); advisors met weekly with research team for debriefing, advice on any emerging issues and to ensure all domains of need were covered; half‐day in‐service training session on carer advice component after 1 year of service Responsibility: for additional component – carer advisor; for standard home palliative care – not stated Description: new caregiver advice component grounded on literature and pilot work with caregivers on preferred mode of extra support (> 80% preferred weekly visit from trained advisor over respite care, practical help, written information and telephone advice); brief caregiver‐focused intervention (6 visits over 6 weeks); aimed to meet caregiver alone (meetings outside home or at workplace, evenings or weekends if needed); mainly face‐to‐face but sometimes on phone (enabled flexibility and helped some caregivers to approach issues difficult to discuss face‐to‐face; calls discussed with team to decide whether equivalent to full visit); included comprehensive needs assessment, discussion and advice on past, present and future issues, information and emotional support; covered needs in terms of physical psychological health, for time away from patient in short and long term, to plan the future, relationships and social networks, relationship with health and social care services, finances; kept to giving advice and support rather than taking action on behalf of caregivers (but advice went as far as helping caregivers to calculate benefit entitlements); bereavement support and advice; mean 5 contacts and mean 3.6 contacts up to death; intervention manual (available from authors) Duration: additional component lasted up to 6 weeks (screening introduced at second or third contact with palliative care team) and if patient died before sixth contact, visits took place after death; duration of standard home palliative care not stated but likely to be from start to death and into bereavement (median survival 13 weeks in intervention group, range 2‐41 weeks) Control: existing specialist home palliative care provided by team of clinical nurse specialists, with specialist medical support and sometimes specialist social work support, giving advice to patients at home, to families and primary clinical teams; patients assisted with control of pain and other physical symptoms, social, psychological, emotional and spiritual issues |
|
| Outcomes | Caregiver pre‐bereavement outcomes (primary outcome ‐ general health; strain; quality of life) Caregiver post‐bereavement outcomes (grief intensity) Caregiver satisfaction with care Survival Assessment points: baseline, 4, 9 and 12 weeks after; 4 months after death Analysis: forwards from enrolment and forwards from death |
|
| Resource use/costs | Not assessed | |
| Notes |
Power considerations: "power calculation indicated that in order to detect a drop to 50% caseness in the experimental group at 90% power and the 5% level of significance, 124 carers would be required in each arm. To cover an expected 10% attrition from the trial we needed to recruit 280 carers, a sample that would also provide sufficient power for examination of GHQ–28 score as a continuous measure" Brief, semi‐structured interviews at the final follow‐up provided a qualitative assessment of acceptability and helpfulness of the support given by the caregiver advice component |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Concealment of allocation (RCT / CCT) | Unclear risk | "Participants were randomised using a block randomisation design, stratified according to the seven participating teams" |
| Follow‐up (RCT / CCT) | High risk | 100 intervention (73%) and 91 control (68%) at 4‐week follow‐up; 58 intervention (42%) and 46 control (34%) at 12 weeks; 84 intervention (61%) and 97 control (72%) at 4 months after death |
| Blinding (RCT / CCT) | Unclear risk | Questionnaires self completed and mailed back; "interviewers were masked to the block size of 12" |
| Baseline measurement (RCT / CCT) | Unclear risk | "No major difference occurred between the randomised groups at baseline on demographic variables, GHQ–28 score or the patient's physical performance status assessed using the criteria of the ECOG. However, there was some imbalance in carer strain and quality of life." Lower carer strain scores and higher quality of life scores in intervention group (statistical significance not stated) |
| Reliability of outcome measurement (RCT / CCT) | Unclear risk | Questionnaires self completed and mailed back; "interviewers were masked to the block size of 12" |
| Protection against contamination (RCT / CCT) | High risk | Patients/caregivers randomised |
Ward 1987.
| Study characteristics | ||
| Methods |
Design: ITS with nested CBA Methodological quality: 5/8a (EPOC ITS checklist); 3.5/6a (EPOC CBA checklist) |
|
| Participants |
Country and regions: UK, Trent and Yorkshire health regions, metropolitan and rural areas Recruitment (date not stated): all deaths from neoplasms (ICD 140 to 209) in 3 years before and 3 years after 8 Macmillan HC nursing services started (identified from Office of Population, Censuses and Surveys Classification of Surgical Operations and Procedures); CBA included patients newly referred to the 8 services during 1 year or until 100 patients were enrolled Number of patients: 40,072 for ITS (17,864 in 3 years before and 22,208 in 3 years after the introduction of the 8 services); 957 for CBA Diseases: cancer (40,072) for ITS; not stated for CBA but likely to be all cancer as Macmillan nurses provide care to people with cancer Patient characteristics: not stated Deaths at end of study: 100% (ITS); not stated for CBA Withdrawals/other drop‐outs: none stated |
|
| Interventions | Home palliative care vs. usual care "Macmillan home care nursing care" Type: intermediate palliative care Service base: 4 inpatient hospice; 4 non‐hospice base (1 hospital, 1 non‐inpatient hospice, 1 in grounds of future in‐patient hospice, 1 in primary care community team offices) Team: members ranged from 2 to 8; 7 teams were multidisciplinary and 1 was of nurses only; all had nurses (from 81 to 182 patients per nurse/year for hospice based services vs. from 33 to 70 for non‐hospice based), 7 had medical input, 5 had social workers; 2 had case conferences (1 daily, 1 weekly) Responsibility: not clear although services' aim was to augment but not replace care from district nursing, GPs and families (primary physician/team likely to be in charge) Description: services varied in provision but also had common components; all were in operation for ≥ 18 months; mean from 2.3 to 7.7 home visits per patient/month for hospice‐based services and mean from 7.9 to 12.5 for non‐hospice based) – visits aimed to monitor current situation, reassure/support, monitor pain and other symptoms, assess need for community care, inpatient or day unit, give advice, deliver equipment/ medication, practical nursing care; arrangements for out‐of‐hours crisis ‐ all had 24/7 coverage (e.g. hospice out of hours, bleeps, radio paging, nursing message systems and nurses home number, coverage by inpatient hospice staff for advice); out of hours visits ranged from 0 to 9 except in 1 hospice‐based service (40 visits) and in 1 non‐hospice based service (81 visits); patients from hospice‐based services could access hospice beds, day centres, family relief and other hospice services Duration: from enrolment to death (median 32 days, range 21.5‐44.5 days across services) Control: usual care including district nursing and care from GPs |
|
| Outcomes | Death at home Preference for place of death met |
|
| Resource use/costs | Terminal institutional days (before death in hospital or hospice) Time horizon: variable (identified backwards from death) |
|
| Notes |
Power considerations: none stated For 2 of the 8 services, the authors could only provide 2 or 1 year data prior to their introduction; as this did not meet our ITS inclusion criteria we analysed outcome data only for the remaining 6 services (this is referred to in the review as the Trent and Yorkshire analysis, with 31,890 deaths) The authors collected other outcome data on a small sample (40 patients): on pain, activities of daily living, quality of life, patient preference for place of death and satisfaction with care ‐ but did not use these to compare services |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Baseline measurement (CBA) | Unclear risk | Characteristics not reported |
| Characteristics of intervention and control providers (CBA) | Unclear risk | Providers' characteristics in text but no data presented |
| Blinded assessment of outcomes (CBA) | Unclear risk | Source of information on place of death not stated |
| Protection against contamination (CBA) | Low risk | Second sites used as controls (non‐hospice‐based services) |
| Reliable outcome measurement (CBA) | Unclear risk | Source of information on place of death not stated |
| Follow‐up of patients/caregivers (CBA) | Unclear risk | Not stated if some were still alive |
| Intervention dependent of other changes (protection against secular trends) (ITS) | Unclear risk | Not specified |
| Data analysed appropriately (ITS) | High risk | Data described only (no ARIMA models or time series regression models used) |
| Reason for number of points pre‐ and post‐intervention (ITS) | High risk | Rationale for choice of 3 years pre‐ and post‐intervention not given; sample size calculation not reported |
| Shape of intervention effect specified (ITS) | Unclear risk | Rationale for shape of intervention effect not reported |
| Intervention likely to affect data collection (protection against detection bias) (ITS) | Low risk | Sources and methods of data collection were the same before and after intervention |
| Blinded assessment of outcomes (ITS) | Low risk | Objective outcome variable (using standard and official statistics) |
| Completeness of data set (ITS) | Low risk | 100% of total number of deaths in study |
| Reliable outcome measurement (ITS) | Low risk | Outcome obtained from standard and official statistics |
Zimmer 1985.
| Study characteristics | ||
| Methods |
Design: RCT (patient) Methodological quality: 3/6a (EPOC RCT/CCT checklist) |
|
| Participants |
Country and regions: US, Rochester, New York, metropolitan area Recruitment (1979‐1982; 27 months): from "variety of sources" following publicity campaign informing health professionals and the community; homebound patients living in study county with chronic illness or terminal illness (the latter were largely cancer patients receiving palliative care only and with life expectancy ≤ 3 months) who had a caregiver not necessarily living in same household and who wished to remain at home, with no physician to make home visits. Exclusion criteria: primary psychiatric illness, unable to fill in questionnaires Number of patients (randomised): 167 (85 intervention and 82 control); (baseline): 158 (82 intervention and 76 control) ; 22% intervention and 18% control classified as terminal (subanalysis performed) Diseases (overall baseline sample): cancer (21% intervention, 17% control), stroke (12% intervention, 17% control), arthritis/rheumatism (9% intervention, 12% control), others, all below 10% (59% intervention, 54% control); those classified as terminal were "largely cancer" patients Patient characteristics: mean age 76 years, median age 77 years; 68% female; 23.2% intervention patients and 18.4% controls lived alone Deaths at end of study: 48 (29 intervention and 19 control, including 3 patients who died before the initial interview) Withdrawals/other drop‐outs: 21: 5 drop‐outs/changed their minds and 1 patient moved away before initial interview; 15 drop‐outs after initial interview (17 deliberate dropped out: 4 intervention and 13 control) |
|
| Interventions | Home palliative care vs. usual care "Home Health Care Team" Type: intermediate palliative care Service base: ambulatory care unit at University of Rochester Medical Center Team: physician‐led multiprofessional team with geriatric nurse practitioner (Masters' medical nurse practitioner) and social worker; weekly team conferences to assure co‐ordination of patient care Responsibility: 1 team member designated as primary provider in care plan following initial interdisciplinary assessment Description: existing service (since 1977) aimed to provide care for home‐bound, chronically or terminally ill, or disabled patients (largely elderly) for whom transportation to clinic had become too costly or cumbersome; initial home visit by each team member for initial assessment; interdisciplinary care plan then established which designated 1 team member as primary provider with consultative visits by others as needed; nurse conducted physical assessments in community (routine and emergency), was responsible for the nursing plan and supported medical care in close cooperation with physician; physician conducted home visits and evaluation at intake and follow‐ups as needed, and acted as patient's attending physician during any hospitalisations; social worker helped to deal with social, financial and emotional problems, freeing physician and nurse to devote mostly to medical and nursing care; encouraged informal care by family and friends by providing them with needed physical and psychological support and education to take on or continue HC; 24‐hour telephone service backed up by physician (all patients advised to restrict calls and service requests to office hours if possible, but were given nurse and physician's home numbers for emergencies and the physician's pager as ultimate resource); low number of out‐of‐hours calls (> 70% handled on telephone) Duration: not stated Control: usual care, including HC services available in community (area described as with well‐developed long‐term care services in general) |
|
| Outcomes | Death at home Survival Assessment points: not stated |
|
| Resource use/costs | Out‐of‐home care (hospital admission, hospital inpatient days, ED visits, clinic visits, MD office visits, ambulance or chairmobile rides, nursing home days) In‐home care (MD home visits, nurse home visits, social worker home visits, RN/LPN hours, aide/homemaker visits, laboratory technician home visits, meals‐on‐wheels visits) Time horizon: terminal 2 weeks before death (subanalysis relevant to this review) Costs: out‐of‐home, in‐home, total costs (mean costs per patient of terminal 2 weeks) Currency: USD (date not stated) |
|
| Notes |
Power considerations: none stated: "A sample size of 200 to 250 was desired over the period of study based on ability of the team to care for half that number (estimated from previous team experience of turnover, visit frequency, and case load)" The analyses relevant for our review were those conducted with the subsample of terminal patients/deaths, and the outcomes were:
|
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Concealment of allocation (RCT / CCT) | Unclear risk | Sample stratified into terminal and non‐terminal; "randomized into experimental (team) and control groups"; process not stated |
| Follow‐up (RCT / CCT) | Unclear risk | 45 (27%) for place of death; 80/85 intervention (94%) and 66/82 control for survival (81%) |
| Blinding (RCT / CCT) | Unclear risk | Double‐blind at baseline only: "The patients were informed of the result of randomization immediately following the initial interview, in order to keep the base‐line information as free as possible of bias from knowledge of the result either by the patient or interviewer" |
| Baseline measurement (RCT / CCT) | Low risk | "The only demographic variable which showed a statistically significant difference was sex, with 61 per cent females in the team group compared with 76 per cent in the controls; this is taken into account in the analysis by adjustment for sex. Previous health care utilization and diagnoses in the two groups were quite similar" |
| Reliability of outcome measurement (RCT / CCT) | Unclear risk | Interviewers (10/14 had previous survey experience) trained by study co‐ordinator with practice of interviews, role play, biweekly feedback meetings |
| Protection against contamination (RCT / CCT) | High risk | Patients/caregivers randomised |
aIn all Risk of bias tables, "high risk" is equivalent to the EPOC criteria “not done” (scored 0), unclear risk is equivalent to “not clear or varied across outcomes” (scored 0.5) and "low risk" is equivalent to “done” (scored 1)
AIDS: acquired immune deficiency syndrome; ARIMA: autoregressive integrated moving average; CBA: controlled before and after study; CC: conventional care; CCT: controlled clinical trial; CES‐D: Center for Epidemiological Studies Depression; CHF: congestive heart failure; COPD: chronic obstructive pulmonary disease; ECOG: Eastern Cooperative Oncology Group; ED: emergency department; EORTC QLQ‐C30: European Organisation for Research and Treatment of Cancer Quality of Life questionnaire; EN: enrolled nurse; EPOC: Effective Practice and Organisation of Care; ESAS: Edmonton Symptom Assessment Scale; FEV1: forced expiratory volume in 1 second; GHQ‐28: 28‐item General Health Questionnaire; GP: general practitioner; HB: hospital based; HC: home care; HIV: human immunodeficiency virus; HMO: health management organisations; ICD: International Classification of Diseases; ITS: interrupted time series; KPS: Karnofsky Performance Status; LPN: licensed practical nurse; MD: medical doctor; MND: motor neurone disease; MS: multiple sclerosis; NYHA: New York Health Association; POS: Palliative Care Outcome Scale; QLI: quality of life index; QWB: quality of well‐being; RCT: randomised controlled trial; RGN: registered general nurse; RN: registered nurse; SD: standard deviation; SF‐36: Short Form 36; VA: Veterans Administration; WHO: World Health Organization
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Addington‐Hall 1992 | Intervention does not meet criteria for palliative care; co‐ordinators did not provide "practical nursing care" or "specialist palliative care advice"; co‐ordination only |
| Brumley 2003 | CBA not meeting criteria, conducted in only 1 intervention site and 1 control site |
| Feldman 2011 | Intervention focused on staff education and mentoring with the main goal of increasing hospice admissions; not specifically aimed to support patients or caregivers at home |
| Hebert 2006 | Televisits provided in addition to standard home palliative care; additional component procedural only and non‐comprehensive addition to care |
| Kane 1984 | Intervention focused on inpatient care with a component of home care; however, inpatients and patients at home are shown together (both part of the hospice group); no subanalysis and frequent transits between inpatient and home care mentioned |
| McCorkle 2000 | Study conducted with post‐surgical patients and only a few died, thus population was not considered terminal/advanced |
| Morita 2012 | Study designed to be a cluster RCT but authors decided to adopt a mixed‐method approach because "1) the intervention itself should be applied to all populations over the country and clear distinction between intervention and control groups is difficult, 2) a concealment problem is likely to occur, and 3) the most important mission at a national level is not to clarify if one specific intervention actually changes outcomes, but to obtain comprehensive insights into how to disseminate palliative care throughout the country". The resulting study is an ITS that does not meeting the criteria for our review, where data collected in the two years prior the program was implemented (2007‐2008) was compared to data collected in the two years after program implementation (2010‐2011) |
| Smeenk 1998a | Intervention does not meet criteria for palliative care; "care specially tailored to meet his [patients] individual needs, and provided by professional caregivers from primary and hospital teams" |
| Temel 2010 | Intervention focused on outpatient meetings with patients at a large academic medical centre; not specifically aimed to support patients or caregivers at home |
CBA: controlled before and after study.
Characteristics of studies awaiting classification [ordered by study ID]
Hwang 2009.
| Methods | Design: CCT (awaiting confirmation from authors) |
| Participants |
Country and regions: South Korea (included regions to be confirmed by authors) Recruitment: to be confirmed by authors Number of patients: 46 (24 intervention and 22 control) Diseases: cancer (46): digestive system (22), lung (11), liver, biliary or pancreatic (10), others (3) Patient characteristics: mean/median age not stated, 59% male, 76% married Deaths at end of study: to be confirmed by authors Withdrawals/other drop‐outs: to be confirmed by authors |
| Interventions |
Type: to be confirmed by authors Service base: to be confirmed by authors Team: to be confirmed by authors Responsibility: to be confirmed by authors Description: several components for patients, caregivers or both: pain and symptom control (drug and non‐drug therapy, care co‐ordination); empowering (providing information, promoting control of emotions and supporting patient and family); finding the meaning (thinking about life and facing death); and networking (making and maintaining relationships, connecting and referring). Duration: to be confirmed by authors Control: to be confirmed by authors |
| Outcomes | Pain
Symptom burden (decreasing symptom experience)
Psychological well‐being (improving psychological QoL)
Caregiver pre bereavement social well‐being (improving family‐related and social QoL)
Spiritual well‐being (relieving spiritual pain and improving spiritual QoL)
Caregiver burden Assessment points: to be confirmed by authors Analysis: to be confirmed by authors |
| Notes |
Park 2011.
| Methods | Design: CCT (awaiting confirmation from authors) |
| Participants |
Country and regions: South Korea (included regions to be confirmed by authors) Recruitment: to be confirmed by authors Number of patients: 40 (20 intervention and 20 control) Diseases: breast cancer (40) Patient characteristics: mean age 50.2 intervention and 47.2 control, 80% married Deaths at end of study: to be confirmed by authors Withdrawals/other drop‐outs: to be confirmed by authors |
| Interventions |
Type: to be confirmed by authors Service base: to be confirmed by authors Team: to be confirmed by authors Responsibility: to be confirmed by authors Description: Either face‐to‐face or phone “Hospice Smart Service” at least once a week for 5 months for patients and families. Provision of cancer and hospice related services. Cancer related services involved needs assessment; provision of information on cancer and its management (such as signs and symptoms, diagnosis, prognosis, treatment and rehabilitation); provision of emotional and practical support (such as control of negative emotion and management of body image); education about communication skill strategy of patient and family; provision of spiritual care and family support. Hospice related services involved provision of information on DNR/advance directives and decision making; provision of information on hospice; information on complementary and alternative therapy; referral to specialist; provision of information on funeral process and insurance; following up bereaved family; assisting to participate in self‐help group. Duration: to be confirmed by authors Control: to be confirmed by authors |
| Outcomes | Satisfaction
Quality of life
Communication skills Decision making skills Mastery sense Understanding of hospice and palliative care Assessment points: to be confirmed by authors Analysis: to be confirmed by authors |
| Notes |
CCT: controlled clinical trial; DNR: Do Not Resuscitate; QoL: quality of life.
Characteristics of ongoing studies [ordered by study ID]
Abernethy 2006.
| Study name | Palliative Care Trial (PCT) |
| Methods | Design: cluster RCT (patient and general practitioner) |
| Participants |
Country and regions: South Australia Recruitment (2002‐2004, 26 months): every patient referred to SAPS was screened by a triage nurse who assessed eligibility. Inclusion criteria: patients mentally competent at enrolment as documented by an MMSE score ≥ 24, or who had a GP‐identified caregiver or legal healthcare proxy who could provide informed consent. Patient and subsequent GP consent were further required for enrolment and randomisation. Exclusion criteria: patients not living within the region served by the palliative care services or expected to die within 48 hours of referral. Number of patients: pending for full sample Diseases: pending for full sample Patient characteristics: pending for full sample Deaths at end of study: pending for full sample Withdrawals/other drop‐outs: pending for full sample |
| Interventions | "GP Educational Outreach visiting in addition to standard palliative care" (intervention 1); "Structured patient and caregiver educational outreach visiting in addition to standard palliative care" (intervention 2) "Case conferencing in addition to standard palliative care" (intervention 3) vs. "standard palliative care"' "Palliative Care Trial (PCT)" Type: specialist palliative care Service base: organised as regional whole‐population networks with consultative specialist medical, nursing and allied health support for GPs and community nurses Team: at least the GP, a palliative care nurse and a trained educator (GP) employed for the study, plus 1 educator for the GP intervention (intervention 1); weekly palliative care team meetings. Medical specialists from other disciplines, district nurses, domiciliary care representatives, social worker, volunteers, pharmacists and pastoral care workers were also available according to patients' needs. Responsibility: not clear Description: intervention 1: GP Educational Outreach Visiting in addition to standard palliative care. Educational sessions took place in GP's office, 2 x 20‐ to 30‐minute sessions with GPs 2‐4 weeks apart. Evidence‐based messages on palliative care pain management derived from structure literature review. Key message focused on knowledge and attitude deficits. Intervention based on the "educational outreach visiting" or "academic detailing" model that "demonstrated to change physician practice". Intervention 2: standard palliative care plus structured patient and caregiver educational outreach visiting. Trained educator conducted 2 x 30‐ to 40‐minute sessions with patient with or without their caregivers in place chosen by patients. Evidence‐based messages on palliative care pain management derived from structure literature review. Key message focused on knowledge and attitude deficits. Intervention derived from a blend of "patient coaching" and "educational outreach visiting". Intervention 3: case conferencing in addition to palliative care. Used a case conferencing model, minimally including the patient, the caregiver, or both, the GP and the palliative care nurse. Other professionals took part based on patients' needs. Conferences organised by the palliative care nurse and conducted within 28 days of randomisation. Agenda set by patients and caregivers by identifying functional, physical, or emotional goals and concerns. GPs paid for participation. Duration: not clear Control: described as standard palliative care |
| Outcomes | Place of death Pain Symptom burden Physical function Quality of life Assessment points: from baseline until death Analysis: forwards from enrolment |
| Starting date | April 2002 |
| Contact information | |
| Notes | Both intervention and control groups received standard palliative care |
Allen 2012.
| Study name | Promoting Effective Advance Care for Elders (PEACE) study |
| Methods | Design: RCT (patient) |
| Participants |
Country and regions: Ohio, United States Recruitment (pending): New PASSPORT (Ohio's community‐based, long‐term care Medicaid waiver program) enrollees randomised either to the intervention or the usual care. Inclusion criteria: > 60 years old who passed a mental status screening (the Mental Status Questionnaire) and had one of the following: congestive heart failure and being actively treated (American Heart Association stage C); chronic obstructive pulmonary disease and on home oxygen; diabetes with renal disease, neuropathy, visual problems, or coronary artery disease; end‐stage liver disease or cirrhosis; cancer (active, not history of) except skin cancer; renal disease and actively receiving dialysis; Amyotrophic Lateral Sclerosis with history of aspiration; Parkinson’s disease stages 3 and 4; or pulmonary hypertension. Exclusion criteria: active alcoholics (i.e., those who drink >2 drinks per day "on average") and illegal substance users as well as clients who have schizophrenia or are psychotic; consumers who could not pass the Mental Status Questionnaire and those were already enrolled in hospice Number of patients: pending for full sample (80 in pilot study; 40 intervention and 40 usual care) Diseases: pending for full sample Patient characteristics: pending for full sample Deaths at end of study: pending for full sample Withdrawals/other drop‐outs: pending for full sample |
| Interventions | Intervention ['Promoting Effective Advance Care for Elders (PEACE)'] versus usual care Type: pending Service base: pending Team: PASSPORT care manager, interdisciplinary team (details pending) and primary care physician Responsibility: not clear Description: Intervention based on Wagner's Chronic Care Model and includes comprehensive interdisciplinary care management for frail elders with chronic illnesses. It emphasises patient activation, and integrates with community‐based long‐term care and other community agencies. Intervention involves an in‐home geriatrics/palliative care needs assessment by a trained PASSPORT case manager. The case manager presents the findings to an interdisciplinary team who develops and individualised care plan based on the consumer’s goals and best practice guidelines. The case manager then implements the plan with the consumer. Family and primary care physician. Duration: not clear Control: described as usual care |
| Outcomes | Symptom management Quality of life Mood Decision making/care planning Spirituality Assessment points: pending Analysis: pending |
| Starting date | pending |
| Contact information | |
| Notes |
Battaglia 2012.
| Study name | Palliative Network for Severely Affected Adults with MS in Italy (PeNSAMI) study |
| Methods | Design: RCT |
| Participants |
Country and regions: Northern, Central and Southern Italy Recruitment (pending): patients with MS, details pending Number of patients: pending Diseases: MS Patient characteristics: pending Deaths at end of study: pending Withdrawals/other drop‐outs: pending |
| Interventions | Palliative care integrated with standard MS care versus standard MS care alone Type: pending Service base: pending Team: pending Responsibility: pending Description: Contents of the intervention will be obtained from a Phase I study composed of individual semi‐structured interviews of adults with severe MS, three focus group meetings with caregivers of people with severe MS and two focus group meetings with health professionals caring for MS patients. A phase II RCT will follow to examine the acceptability, feasibility and effectiveness of the intervention. In order to cover a range of experiences, participants will be selected from Northern, Central and Southern Italy. Duration: pending |
| Outcomes | Pending Assessment points: pending Analysis: pending |
| Starting date | Phase II RCT planned for 2013 |
| Contact information | |
| Notes |
Butler 2012.
| Study name | Hospice rapid response community service |
| Methods | Design: cluster RCT |
| Participants |
Country and regions: East Kent, England Recruitment (pending): All new referrals to the hospice who are assessed by a member of the hospice team during the study period are potentially eligible for inclusion in the study, but only those referred who die within the intervention or control period will be included in the analysis. Number of patients: pending (441 patients needed according to sample size calculations) Diseases: pending Patient characteristics: pending Deaths at end of study: pending Withdrawals/other drop‐outs: pending |
| Interventions | Rapid response service ('Hospice rapid response community service') plus usual care vs usual care only fast‐track design applied to three centres (intervention rolled out sequentially in the three centres with six months between the start of provision in each site) Type: specialist palliative care Service base: hospice‐based (three hospice centres with inpatient beds, community outreach service and day centre) Team: Rapid response teams (details below) Responsibility: pending Description: Intervention provided by rapid response teams was developed in line with best practice and following a literature review, Its main features are: 1) available to patients in their homes (or care homes); 2) has a robust ‘hospice standard’ assessment which takes account of: patient preferences, caregiver/family preferences, patient needs, and patient prognosis; 3) provides hands on care; 4) responds rapidly to crises using human and material resources available 24/7 with access to health care assistants, service coordinator, palliative care nursing, medical advice, and small pieces of equipment which can be carried by car; 5) works in coordination with other community services Duration: pending |
| Outcomes | Dying in the preferred place (primary patient outcomes) Preferences and change of preferences for place of death Actual place of death Caregiver quality of life (primary caregiver outcome) Caregiver anxiety and depression (HADS) Caregiver health status (EQ‐5D) Caregiver demand Satisfaction with care (caregiver) Service utilisation costs (including intervention costs such as staff time, mileage travelled to patient homes and consumables; general practice and community resources, outpatient, inpatient stays, out‐of‐hours service, Marie Curie nurse visits, and social care packages) Assessment points: baseline until death, timepoints not stated (patients); baseline and eight months after enrolment, and six to eight months after the patient died (caregiver) Analysis: pending |
| Starting date | pending |
| Contact information | |
| Notes |
Chvetzoff 2006.
| Study name | TRAPADO study |
| Methods | Design: CCT |
| Participants |
Country and regions: Lyon, France Recruitment (2000‐2002, 24 months): Inclusion criteria: ≥ 18 years, cancer diagnosis, prognosis (estimated by clinician) of < 3 months, plus 2 of the following 3 criteria: performance status > 2, LDH levels higher than normal, albumin < 30 g/L. Participants also needed to be living in the Lyon area for home care intervention and have someone available to answer the questionnaires. After being informed of their prognosis, patients were invited to take part in the study by their oncologist, hospital doctor or the home care physician co‐ordinator. Informed consent was done in writing and patients expressed their choice of cohort (TRA, PA or DO), knowing that a change was possible at any time Number of patients: 52 (at the time of interim analysis ‐ aimed to have 100 patients, this was achieved in 2005 but complete data not yet published) Diseases: cancer (52) Patient characteristics (interim analysis): median age 61 years, 56% male Deaths at end of study: 46 (at the time of interim analysis) Withdrawals/other drop‐outs: 1 (at the time of interim analysis) |
| Interventions | Standard hospitalisation (TRA), Palliative Care Unit (PA) (presented together) vs. home care or hospitalisation at home (DO) 'TRAPADO study' Type: pending Service base: hospital‐based Team: the project is co‐ordinated by a nurse or a psychologist, further information pending Responsibility: pending Description: main objective to measure the quality of care and quality of life in palliative patients in the 3 cohorts. The goal was to examine the settings instead of comparing them. The secondary objective of the study was to describe the patient's choices, the characteristics of the 3 populations and the impact on families Duration: pending |
| Outcomes | Quality of care Quality of life Anxiety Depression Pain General health Assessment points: baseline, 15 days after baseline, 30 days after baseline and every month until death, for a maximum of 4 months Analysis: pending |
| Starting date | 2002 |
| Contact information | |
| Notes |
Duursma 2011.
| Study name | Optimization of complex palliative care at home via telemedicine |
| Methods | Design: cluster RCT |
| Participants |
Country and regions: Nijmegen region, the Netherlands Recruitment (starting date and duration not stated but ongoing and planned to continue at least until December 2013): clustering took place on the level of the GP, who is invited with a letter describing the aim of the study and its procedures. Inclusion criteria for patients are: to live in the area where the study is taking place; be a Dutch‐speaking patient, aged 18 years or older; have a progressive oncological disease; have a score of ≤ 60 on the Karnofsky Performance Scale (assessed by the GP); have a life expectancy of ≤ 3 months Number of patients: pending Diseases: cancer Patient characteristics: pending Deaths at end of study: pending Withdrawals/other drop‐outs: pending |
| Interventions | Intervention vs. “care as usual” Type: specialist palliative care Service base: hospital‐based Team: nurse practitioner, palliative care specialist, GP Responsibility: remains with the GP Description: The intervention consists of a weekly consultation by means of telemedicine between the patient and a specialist nurse practitioner, when the nurse checks for problems in palliative care following a predefined consultation protocol. After the first teleconsultation, the specialist nurse and a palliative care specialist advise the GP on the treatment policy for the patient. In addition to the weekly teleconsultations, the patient can also videophone the 24/7 support service of the homecare organization. The patient also has access to an information database, an internet‐browser and some entertainment options via the telemedicine application. Duration: pending |
| Outcomes | Symptom burden (primary outcome) Depression Anxiety Place of death Experienced problems and needs for palliative care Patient and caregiver satisfaction with the teleconsultation Experienced continuity of medical care in the last phase of life Experienced burden of the family caregiver Resource use (including number of contacts by telephone with the GP practice, number of home visits by the GP, number of contacts with the GPs out of hours service, number of and indications for hospital admissions) Assessment points: patient: baseline and every four weeks (symptom burden every week as it is the primary outcome). Family caregiver: baseline and every two weeks Analysis: pending |
| Starting date | April 2011 |
| Contact information | |
| Notes |
CBA: controlled before and after study; CCT: controlled clinical trial; GP: general practitioner; HADS: Hospital Anxiety and Depression Scale; LDH: lactate dehydrogenase; MS: multiple sclerosis; MMSE: mini‐mental state examination; RCT: randomised controlled trial; SAPS: Southern Adelaide Palliative Services.
Differences between protocol and review
The review updated the background literature from the protocol and made several changes in the style and organisation of the text, to improve readability and to accommodate the overlapping protocol from Vito Curiale.
We rephrased the first review objective to quantify the effect of the intervention on patients' odds of dying at home (primary outcome) and the second objective to examine other outcomes for patients and caregivers (secondary outcomes). The fourth objective (on cost‐effectiveness) was rephrased as suggested by one of the peer‐reviewers.
We did not compare different disease groups since the data were not sufficient for meaningful comparisons. Comparisons between models of care were limited by the level of description of the different interventions.
The inclusion/exclusion criteria were slightly revised. Interventions not directly delivering care (e.g. staff training) were excluded. When it was clear that the majority of intervention contacts were delivered while the patients/caregivers were at home we considered that the intervention aimed to support people at home. We were also more flexible with the definition of intermediate palliative care services, taking into account the team's training and years of experience caring for people with advanced illness and in terminal care (or similar terms such as 'care of the dying'). Furthermore, when authors used terms such as 'palliative care' and 'hospice care' to describe their intervention we considered those as palliative care interventions.
Finally, the search strategies were broadened to generate a more comprehensive search.
Contributions of authors
For the protocol
BG PMc and IJH: developed the idea, developed the search strategies and the data extraction form, wrote and approved the final protocol.
VC: published the protocol "Home‐based palliative care for adults with cancer" in 2008 that was later withdrawn due to a substantial overlap with the protocol for this review, published in 2009.
For the review
BG: searched for studies and conducted updates, obtained copies of the studies, extracted data from the studies, contacted authors, entered data into RevMan (RevMan 2011), carried out quality assessment and analysis, drafted the review and finalised it after discussion with the other review authors.
NC: searched for studies and conducted updates, obtained copies of the studies, extracted data from the studies, contacted authors, entered data into RevMan (RevMan 2011), carried out quality assessment and analysis, discussed the outcomes with the other review authors and revised the manuscript.
VC: searched for studies, discussed the outcomes with the other review authors and revised the manuscript.
PMcC: carried out quality assessment, discussed the outcomes with the other review authors and revised the manuscript.
IJH: carried out quality assessment, discussed the outcomes with the other review authors and revised the manuscript.
All review authors selected which studies to include, interpreted the data, helped to draft and revise the manuscript, and approved the final manuscript.
Sources of support
Internal sources
King's College London, Cicely Saunders Institute, Department of Palliative Care, Policy and Rehabilitation, UK
External sources
Cicely Saunders International, UK
Calouste Gulbenkian Foundation, Portugal
Declarations of interest
IJH and PMcC were authors of one of the studies included in the review but played no part in the decision to include/exclude, quality assessment, data extraction or conclusions in relation to this study.
Edited (no change to conclusions)
References
References to studies included in this review
Ahlner‐Elmqvist 2008 {published data only}
- Ahlner-Elmqvist M, Jordhøy MS, Bjordal K, Jannert M, Kaasa S. Characteristics and quality of life of patients who choose home care at the end of life. Journal of Pain & Symptom Management 2008;36(3):217-27. [DOI] [PubMed] [Google Scholar]
- Ahlner-Elmqvist M, Jordhøy MS, Jannert M, Fayers P, Kaasa S. Place of death: hospital-based advanced home care versus conventional care. Palliative Medicine 2004;18(7):583-93. [DOI] [PubMed] [Google Scholar]
- Ringdal GI, Ringdal K, Jordhøy MS, Ahlner-Elmqvist M, Jannert M, Kaasa S. Health-related quality of life (HRQOL) in family members of cancer victims: results from a longitudinal intervention study in Norway and Sweden. Palliative Medicine 2004;18(2):108-20. [DOI] [PubMed] [Google Scholar]
Aiken 2006 {published data only}
- Aiken LS, Butner J, Lockhart CA, Volk-Craft BE, Hamilton G, Williams FG. Outcome evaluation of a randomized trial of the PhoenixCare intervention: program of case management and coordinated care for the seriously chronically ill. Journal of Palliative Medicine 2006;9(1):111-26. [DOI] [PubMed] [Google Scholar]
- Lockhart CA, Volk-Craft BE, Hamilton G, Aiken LS, Williams FG. The PhoenixCare program. Journal of Palliative Medicine 2003;6(6):1001-12. [DOI] [PubMed] [Google Scholar]
Axelsson 1998 {published data only}
- Axelsson B, Christensen SB. Evaluation of a hospital-based palliative support service with particular regard to financial outcome measures. Palliative Medicine 1998;12(1):41-9. [DOI] [PubMed] [Google Scholar]
Bakitas 2009 {published and unpublished data}
- Bakitas M, Lyons KD, Hegel MT, Balan S, Barnett KN, Brokaw FC, et al. The project ENABLE II randomized controlled trial to improve palliative care for rural patients with advanced cancer: baseline findings, methodological challenges, and solutions. Palliative and Supportive Care 2009b;7(1):75-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bakitas M, Lyons KD, Hegel MT, Balan S, Brokaw FC, Seville J, et al. Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: the Project ENABLE II randomized controlled trial. JAMA 2009a;302(7):741-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Hara RE, Hull JG, Lyons KD, Bakitas M, Hegel MT, Li Z, Ahles TA. Impact on caregiver burden of a patient-focused palliative care intervention for patients with advanced cancer. Palliative and Supportive Care 2010;8(4):395-404. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brumley 2007 {published and unpublished data}
- Brumley R, Enguidanos S, Jamison P, Seitz R, Morgenstern N, Saito S, et al. Increased satisfaction with care and lower costs: results of a randomized trial of in-home palliative care. Journal of the American Geriatrics Society 2007;55(7):993-1000. [DOI] [PubMed] [Google Scholar]
- Brumley R, Enguidanos S. Findings from a multisite in-home palliative care study. Journal of Palliative Care 2006;22(3):199. [Google Scholar]
- Enguidanos S, Chambers J. In-home palliative care increased patient satisfaction and reduced use and costs of medical services: commentary. Evidence-Based Medicine 2008;13(1):19. [DOI] [PubMed] [Google Scholar]
Buckingham 1978 {published data only}
- Buckingham RW, Foley SH. A guide to evaluation research in terminal care programs. Death Education 1978;2(1-2):127-41. [DOI] [PubMed] [Google Scholar]
Gómez‐Batiste 2010 {published data only}
- Espinosa J, Gómez-Batiste X, Picaza JM, Limon E. Specialist palliative care home care support teams in Spain [Equipos de soporte domiciliario de cuidados paliativos en España]. Medicina Clinica 2010;135(10):470-5. [DOI] [PubMed] [Google Scholar]
- Gómez-Batiste X, Porta-Sales J, Espinosa-Rojas J, Pascual-Lopez A, Tuca A, Rodriguez J. Effectiveness of palliative care services in symptom control of patients with advanced terminal cancer: a Spanish, multicenter, prospective, quasi-experimental, prepost study. Journal of Pain & Symptom Management 2010;40(5):652-60. [DOI] [PubMed] [Google Scholar]
- Porta-Sales J, Espinosa-Rojas J, Mañas-Izquierdo V, Tuca-Rodriguez A, Gómez-Batiste X, Martín FJP, et al. Symptom control effectiveness in advanced cancer patients by Spanish palliative care team: national-wide study. In: Palliative Medicine. Vol. 22. 2008:501.
Grande 1999 {published and unpublished data}
- Grande GE, Farquhar MC, Barclay SIG, Todd CJ. Caregiver bereavement outcome: relationship with hospice at home, satisfaction with care, and home death. Journal of Palliative Care 2004;20(2):69-77. [PubMed] [Google Scholar]
- Grande GE, Todd CJ, Barclay SIG, Farquhar MC. A randomized controlled trial of a hospital at home service for the terminally ill. Palliative Medicine 2000;14(5):375-85. [DOI] [PubMed] [Google Scholar]
- Grande GE, Todd CJ, Barclay SIG, Farquhar MC. Does hospital at home for palliative care facilitate home death? A randomised controlled trial. BMJ 1999;319(7223):1472-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Greer 1986 {published data only}
- Bernard LL, Guarnaccia CA. Two models of caregiver strain and bereavement adjustment: a comparison of husband and daughter caregivers of breast cancer hospice patients. Gerontologist 2003;43(6):808-16. [DOI] [PubMed] [Google Scholar]
- Birnbaum H, Kidder D. What does hospice cost? American Journal of Public Health 1984;74(7):689-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg RJ, Mor V, Wiemann M, Greer DS, Hiris J. Analgesic use in terminal cancer patients: report from the National Hospice Study. Journal of Chronic Diseases 1986;39(1):37-45. [DOI] [PubMed] [Google Scholar]
- Greer DS, Mor V, Morris JN. An alternative in terminal care: results of the National Hospice Study. Journal of Chronic Diseases 1986a;39(1):9-26. [DOI] [PubMed] [Google Scholar]
- Greer DS, Mor V. An overview of National Hospice Study findings. Journal of Chronic Diseases 1986b;39(1):5-7. [DOI] [PubMed] [Google Scholar]
- Morris JN, Mor V, Goldberg RJ, Sherwood S, Greer DS, Hiris J. The effect of treatment setting and patient characteristics on pain in terminal cancer patients: a report from the National Hospice Study. Journal of Chronic Disability 1986;39(1):27-35. [DOI] [PubMed] [Google Scholar]
- Mor V, Hiris J. Determinants of site of death among hospice cancer patients. Journal of Health and Social Behavior 1983;24(4):375-85. [PubMed] [Google Scholar]
- Mor V, Laliberte L, Morris JN, Wiemann M. The Karnofsky Performance Status Scale. An examination of its reliability and validity in a research setting. Cancer 1984;53(9):2002-7. [DOI] [PubMed] [Google Scholar]
- Mor V, Masterson-Allen S. A comparison of hospice vs conventional care of the terminally ill cancer patient. Oncology 1990;4(7):85-96. [PubMed] [Google Scholar]
- Mor V. Assessing patient outcomes in hospice: what to measure? Hospice Journal 1986;2(3):17-35. [PubMed] [Google Scholar]
- Mor V. Hospice: the older person as patient and caregiver. Generations: Journal of the American Society on Aging 1987;11(3):19-21. [Google Scholar]
- Powers JS, Burger C. Terminal care preferences: hospice placement and severity of disease. Public Health Reports 1987;102(4):444-9. [PMC free article] [PubMed] [Google Scholar]
- Reuben DB, Mor V, Hiris J. Clinical symptoms and length of survival in patients with terminal cancer. Archives of Internal Medicine 1988;148(7):1586-91. [PubMed] [Google Scholar]
- Reuben DB, Mor V. Dyspnea in terminally ill cancer patients. Chest 1986;89(2):34-6. [DOI] [PubMed] [Google Scholar]
- Wallston KA, Burger C, Smith RA, Baugher RJ. Comparing the quality of death for hospice and non-hospice cancer patients. Medical Care 1988;26(2):177-82. [DOI] [PubMed] [Google Scholar]
Harding 2004 {published data only}
- Harding R, Higginson IJ, Leam C, Donaldson N, Pearce A, George R, et al. Evaluation of a short-term group intervention for informal carers of patients attending a home palliative care service. Journal of Pain & Symptom Management 2004;27(5):396-408. [DOI] [PubMed] [Google Scholar]
- Harding R, Leam C, Pearce A, Taylor E, Higginson IJ. A multi-professional short-term group intervention for informal caregivers of patients using a home palliative care service. Journal of Palliative Care 2002;18(4):275-81. [PubMed] [Google Scholar]
Higginson 2009 {published and unpublished data}
- Edmonds P, Hart S, Gao W, Vivat B, Burman R, Silber E, et al. Palliative care for people severely affected by multiple sclerosis: evaluation of a novel palliative care service. Multiple Sclerosis 2010;16(5):627-36. [DOI] [PubMed] [Google Scholar]
- Gruenewald DA, Higginson IJ, Vivat B, Edmonds P, Burman RE. Quality of life measures for the palliative care of people severely affected by multiple sclerosis: a systematic review. Multiple Sclerosis 2004;10(6):690-725. [DOI] [PubMed] [Google Scholar]
- Higginson IJ, Hart S, Burman R, Silber E, Saleem T, Edmonds P. Randomised controlled trial of a new palliative care service: compliance, recruitment and completeness of follow-up. BMC Palliative Care 2008;7:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higginson IJ, McCrone P, Hart SR, Burman R, Silber E, Edmonds PM. Is short-term palliative care cost-effective in multiple sclerosis? A randomized phase II trial. Journal of Pain & Symptom Management 2009;38(6):816-26. [DOI] [PubMed] [Google Scholar]
- Higginson IJ, Vivat B, Silber E, Saleem T, Burman R, Hart S, et al. Study protocol: delayed intervention randomised controlled trial within the Medical Research Council (MRC) Framework to assess the effectiveness of a new palliative care service. BMC Palliative Care 2006;5:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hudson 2005 {published data only}
- Hudson PL, Aranda S, Hayman-White K. A psycho-educational intervention for family caregivers of patients receiving palliative care: a randomized controlled trial. Journal of Pain & Symptom Management 2005;30(4):329-41. [DOI] [PubMed] [Google Scholar]
Hughes 1992 {published data only}
- Cummings JE, Hughes SL, Weaver FM, Manheim LM, Conrad KJ, Nash K, et al. Cost-effectiveness of Veterans Administration hospital-based home care. A randomized clinical trial. Archives of Internal Medicine 1990;150(6):1274-80. [PubMed] [Google Scholar]
- Hughes SL, Cummings J, Weaver F, Manheim L, Braun B, Conrad K. A randomized trial of the cost effectiveness of VA hospital-based home care for the terminally ill. Health Services Research 1992;26(6):801-17. [PMC free article] [PubMed] [Google Scholar]
Jordhøy 2000 {published data only}
- Fredheim OMS, Kaasa S, Fayers P, Saltnes T, Jordhøy M, Borchgrevink PC. Chronic non-malignant pain patients report as poor health-related quality of life as palliative cancer patients. Acta Anaesthesiologica Scandinavica 2008;52(1):143-8. [DOI] [PubMed] [Google Scholar]
- Jordhøy MS, Fayers P, Loge JH, Ahlner-Elmqvist M, Kaasa S. Quality of life in palliative cancer care: results from a cluster randomized trial. Journal of Clinical Oncology 2001a;19(18):3884-94. [DOI] [PubMed] [Google Scholar]
- Jordhøy MS, Fayers P, Loge JH, Saltnes T, Ahlner-Elmqvist M, Kaasa S. Quality of life in advanced cancer patients: the impact of sociodemographic and medical characteristics. British Journal of Cancer 2001b;85(10):1478-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordhøy MS, Fayers P, Saltnes T, Ahlner-Elmqvist M, Jannert M, Kaasa S. A palliative-care intervention and death at home: a cluster randomised trial. Lancet 2000;356(9233):888-93. [DOI] [PubMed] [Google Scholar]
- Jordhøy MS, Fayers PM, Ahlner-Elmqvist M, Kaasa S. Lack of concealment may lead to selection bias in cluster randomized trials of palliative care. Palliative Medicine 2002;16(1):43-9. [DOI] [PubMed] [Google Scholar]
- Jordhøy MS, Kaasa S, Fayers P, Underland G, Ahlner-Elmqvist M. Challenges in palliative care research; recruitment, attrition and compliance: experience from a randomized controlled trial. Palliative Medicine 1999;13(4):299-310. [DOI] [PubMed] [Google Scholar]
- Jordhøy MS, Saltvedt I, Fayers P, Loge JH, Ahlner-Elmqvist M, Kaasa S. Quality of life, medical and sociodemographic characteristics. Palliative Medicine 2003;17(5):433-44. [DOI] [PubMed] [Google Scholar]
- Ringdal GI, Jordhøy MS, Kaasa S. Family satisfaction with end-of-life care for cancer patients in a cluster randomized trial. Journal of Pain & Symptom Management 2002;24(1):53-63. [DOI] [PubMed] [Google Scholar]
- Ringdal GI, Jordhøy MS, Kaasa S. Measuring quality of palliative care: psychometric properties of the FAMCARE scale. Quality of Life Research 2003;12(2):167-76. [DOI] [PubMed] [Google Scholar]
- Ringdal GI, Jordhøy MS, Ringdal K, Kaasa S. Factors affecting grief reactions in close family members to individuals who have died of cancer. Journal of Pain & Symptom Management 2001;22(6):1016-26. [DOI] [PubMed] [Google Scholar]
- Ringdal GI, Jordhøy MS, Ringdal K, Kaasa S. The first year of grief and bereavement in close family members to individuals who have died of cancer. Palliative Medicine 2001;15(2):91-105. [DOI] [PubMed] [Google Scholar]
- Ringdal GI, Ringdal K, Jordhøy MS, Ahlner-Elmqvist M, Jannert M, Kaasa S. Health-related quality of life (HRQOL) in family members of cancer victims: results from a longitudinal intervention study in Norway and Sweden. Palliative Medicine 2004;18(2):108-20. [DOI] [PubMed] [Google Scholar]
- Ringdal GI, Ringdal K, Jordhøy MS, Kaasa S. Does social support from family and friends work as a buffer against reactions to stressful life events such as terminal cancer? Palliative and Supportive Care 2007;5(1):61-9. [DOI] [PubMed] [Google Scholar]
- Ringdal GI, Ringdal K, Jordhøy MS, Kaasa S. Does social support work as a buffer against reactions to external stressful life events such as terminal cancer? In: Abstracts of the 9th Congress of the European Association for Palliative Care, Aachen. Vol. 76. 2005.
McCorkle 1989 {published data only}
- McCorkle R, Benoliel JQ, Donaldson G, Georgiadou F, Moinpour C, Goodell B. A randomized clinical trial of home nursing care for lung cancer patients. Cancer 1989;64(6):1375-82. [DOI] [PubMed] [Google Scholar]
- McCorkle R, Robinson L, Nuamah I, Lev E, Benoliel JQ. The effects of home nursing care for patients during terminal illness on the bereaved's psychological distress. Nursing Research 1998;47(1):2-10. [DOI] [PubMed] [Google Scholar]
McKegney 1981 {published data only}
- Kassakian MG, Bailey LR, Rinker M, Stewart CA, Yates JW. The cost and quality of dying: a comparison of home and hospital. Nurse Practitioner 1979;4(1):18-9. [PubMed] [Google Scholar]
- McKegney FP, Bailey LR, Yates JW. Prediction and management of pain in patients with advanced cancer. General Hospital Psychiatry 1981;3(2):95-101. [DOI] [PubMed] [Google Scholar]
- Yates J, Stewart C, Hasler G, Hochstein S. Controlled study of home care by nurse-practitioners in patients with advanced cancer. In: Proceedings of the 69th Annual Meeting of the American Association for Cancer Research. 1978.
- Yates JW, Chalmer B, McKegney FP. Evaluation of patients with advanced cancer using the Karnofsky performance status. Cancer 1980;45(8):2220-4. [DOI] [PubMed] [Google Scholar]
- Yates JW, McKegney FP, Visco G, Brown GS. Intensive rehabilitative support of the patient with advanced cancer through home health care. In: Proceedings of the American Association for Cancer Research (AACR). Vol. 18. 1977:199.
McMillan 2007 {published data only}
- McMillan SC, Moody LE. Hospice patient and caregiver congruence in reporting patients' symptom intensity. Cancer Nursing 2003;26(2):113-8. [DOI] [PubMed] [Google Scholar]
- McMillan SC, Small BJ, Weitzner M, Schonwetter R, Tittle M, Moody L, et al. Impact of coping skills intervention with family caregivers of hospice patients with cancer: a randomized clinical trial. Cancer 2006;106(1):214-22. [DOI] [PubMed] [Google Scholar]
- McMillan SC, Small BJ. Symptom distress and quality of life in patients with cancer newly admitted to hospice home care. Oncology Nursing Forum 2002;29(10):1422-8. [DOI] [PubMed] [Google Scholar]
- McMillan SC, Small BJ. Using the COPE intervention for family caregivers to improve symptoms of hospice homecare patients: a clinical trial. Oncology Nursing Forum 2007;34(2):313-21. [DOI] [PubMed] [Google Scholar]
- McMillan SC, Weitzner MA. Methodologic issues in collecting data from debilitated patients with cancer near the end of life. Oncology Nursing Forum 2003;30(1):123-9. [DOI] [PubMed] [Google Scholar]
McWhinney 1994 {published data only}
- McWhinney IR, Bass MJ, Donner A. Evaluation of a palliative care service: problems and pitfalls. BMJ 1994;309(6965):1340-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rabow 2004 {published data only}
- Rabow MW, Dibble SL, Pantilat SZ, McPhee SJ. The Comprehensive Care Team: a controlled trial of outpatient palliative medicine consultation. Archives of Internal Medicine 2004;164(1):83-91. [DOI] [PubMed] [Google Scholar]
- Rabow MW, Petersen J, Schanche K, Dibble SL, McPhee SJ. The Comprehensive Care Team: a description of a controlled trial of care at the beginning of the end of life. Journal of Palliative Medicine 2003a;6(3):489-99. [DOI] [PubMed] [Google Scholar]
- Rabow MW, Schanche K, Petersen J, Dibble SL, McPhee SJ. Patient perceptions of an outpatient palliative care intervention: "it had been on my mind before, but I did not know how to start talking about death…". Journal of Pain & Symptom Management 2003b;26(5):1010-5. [DOI] [PubMed] [Google Scholar]
Tramarin 1992 {published data only}
- Tramarin A, Milocchi F, Tolley K, Vaglia A, Marcolini F, Manfrin V, et al. An economic evaluation of home-care assistance for AIDS patients: a pilot study in a town in northern Italy. AIDS 1992;6(11):1377-83. [DOI] [PubMed] [Google Scholar]
Walsh 2007 {published data only}
- Walsh K, Jones L, Tookman A, Mason C, McLoughlin J, Blizard R, et al. Reducing emotional distress in people caring for patients receiving specialist palliative care. Randomised trial. British Journal of Psychiatry 2007;190:142-7. [DOI] [PubMed] [Google Scholar]
Ward 1987 {published data only}
- Ward AW. Home care services - an alternative to hospices? Community Medicine 1987;9(1):47-54. [DOI] [PubMed] [Google Scholar]
Zimmer 1985 {published data only}
- McCusker J. Development of scales to measure satisfaction and preferences regarding long-term and terminal care. Medical Care 1984;22(5):476-93. [DOI] [PubMed] [Google Scholar]
- Zimmer JG, Groth-Juncker A, McCusker J. A randomized controlled study of a home health care team. American Journal of Public Health 1985;75(2):134-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmer JG, Groth-Juncker A, McCusker J. Effects of a physician-led home care team on terminal care. Journal of the American Geriatrics Society 1984;32(4):288-92. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Addington‐Hall 1992 {published data only}
- Addington-Hall JM, MacDonald LD, Anderson HR, Chamberlain J, Freeling P, Bland JM, et al. Randomised controlled trial of effects of coordinating care for terminally ill cancer patients. BMJ 1992;305(6865):1317-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addington-Hall JM, MacDonald LD, Anderson HR, Freeling P. Dying from cancer: the views of bereaved family and friends about the experiences of terminally ill patients. Palliative Medicine 1991;5:207-14. [Google Scholar]
- Addington-Hall JM, MacDonald LD, Anderson HR. Can the Spitzer Quality of Life Index help to reduce prognostic uncertainty in terminal care? British Journal of Cancer 1990;62:695-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacDonald LD, Addington-Hall JM. Acceptability and perceived effectiveness of a district co-ordinating service for terminal care: implications for quality assurance. Journal of Advanced Nursing 1994;20:337-43. [DOI] [PubMed] [Google Scholar]
- Raftery JP, Addington-Hall JM, MacDonald LD, Anderson HR, Bland JM, Chamberlain J, et al. A randomized controlled trial of the cost-effectiveness of a district co-ordinating service for terminally ill cancer patients. Palliative Medicine 1996;10:151-61. [DOI] [PubMed] [Google Scholar]
Brumley 2003 {published data only}
- Brumley RD, Enguidanos S, Cherin DA. Effectiveness of a Home-Based Palliative Care Program for End-of-Life. Journal of Palliative Medicine 2003;6(5):715-24. [DOI] [PubMed] [Google Scholar]
- Brumley RD. Future of end-of-life care: the managed care organization perspective. Journal of Palliative Medicine 2002;5(2):263-70. [DOI] [PubMed] [Google Scholar]
Feldman 2011 {published and unpublished data}
- Feldman PH, Ryvicker M et al. Establishing an Advanced Illness Management (AIM) model in a community-based setting: innovation at the Visiting Nurse Service of New York (as supplied 14 April 2011). Data on file.
- Newton V. Visiting Nurse Service of New York. Nursing Spectrum - New York & New Jersey Edition 2008;20(17):18-9. [Google Scholar]
Hebert 2006 {published data only}
- Hebert MA, Brant R, Hailey D, Pol M. Potential and readiness for video-visits in rural palliative homecare: results of a multi-method study in Canada. Journal of Telemedicine and Telecare 2006a;12 Suppl 3:43-5. [Google Scholar]
- Hebert MA, Jansen JJ, Brant R, Hailey D, Pol M. Effectiveness of video-visits in palliative home care: preliminary findings of a RCT in the community. In: Telehealth. Vol. Proceedings of the IASTED International Conference. 2005.
- Hebert MA, Jansen JJ, Brant R, Hailey D, Pol M. Successes and challenges in a field-based, multi-method study of home telehealth. Journal of Telemedicine and Telecare 2004;10 Suppl 1:41-4. [DOI] [PubMed] [Google Scholar]
- Hebert MA, Jansen JJ, Whitten L. Palliative care. In: Wootton R, Dimmick SL, Kvedar JC, editors(s). Home Telehealth: connecting care within the community. London: Royal Society of Medicine Press, 2006b:232-45. [Google Scholar]
Kane 1984 {published data only}
- Kane RL, Bernstein L, Wales J, Rothenberg R. Hospice effectiveness in controlling pain. JAMA 1985;253(18):2683-6. [PubMed] [Google Scholar]
- Kane RL, Klein SJ, Bernstein L, Rothenberg R, Wales J. Hospice role in alleviating the emotional stress of terminal patients and their families. Medical Care 1985;23(3):189-97. [DOI] [PubMed] [Google Scholar]
- Kane RL, Klein SJ, Bernstein L, Rothenberg R. The role of hospice in reducing the impact of bereavement. Journal of Chronic Diseases 1986;39(9):735-42. [DOI] [PubMed] [Google Scholar]
- Kane RL, Wales J, Bernstein L. A randomised controlled trial of hospice care. Lancet 1984;1(8382):890-4. [DOI] [PubMed] [Google Scholar]
- Wales J, Kane R, Robbins S. UCLA hospice evaluation study. Methodology and instrumentation. Medical Care 1983;21(7):734-44. [DOI] [PubMed] [Google Scholar]
McCorkle 2000 {published data only}
- Hughes LC, Hodgson NA, Muller P, Robinson LA, McCorkle R. Information needs of elderly postsurgical cancer patients during the transition from hospital to home. Journal of Nursing Scholarship 2000;32(1):25-30. [DOI] [PubMed] [Google Scholar]
- Hughes LC, Robinson LA, Cooley ME, Nuamah I, Grobe SJ, McCorkle R. Describing an episode of home nursing care for elderly postsurgical cancer patients. Nursing Research 2002;51(2):110-8. [DOI] [PubMed] [Google Scholar]
- McCauley K, Bixby B, Naylor MD. Advanced practice nurse strategies to improve outcomes and reduce cost in elders with heart failure. Disease Management 2006;9(5):302-10. [DOI] [PubMed] [Google Scholar]
- McCorkle R, Hughes L, Robinson L, Levine B, Nuamah I. Nursing interventions for newly diagnosed older cancer patients facing terminal illness. BMJ 2000;14(3):39-45. [PubMed] [Google Scholar]
- McCorkle R, Strumpf NE, Nuamah IF, Adler DC, Cooley ME, Jepson C, et al. A specialized home care intervention improves survival among older post-surgical cancer patients. Journal of the American Geriatrics Society 2000;48(12):1707-13. [DOI] [PubMed] [Google Scholar]
- McCorkle R, Strumpf NE, Nuamah IF, Adler DC, Cooley ME, Jepson C, et al. In older patients with late stage cancer, specialised home care by nurses improved survival after surgery. Evidence Based Nursing 2001;4:1707-13. [Google Scholar]
Morita 2012 {published data only}
- Morita T, Miyashita M, Yamagishi A, Akizuki N, Kizawa Y, Shirahige Y, et al. A region-based palliative care intervention trial using the mixed-method approach: Japan OPTIM study. BMC Palliative Care 2012;11:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamagishi A, Morita T, Komura K, Sueda C, Shirahige Y, Kinoshita H, et al. Problems and potential solutions of regional palliative care: A Trial of the Multiregional and Multidisciplinary Conference in the OPTIM Study. Japanese Journal of Cancer and Chemotherapy 2011;38(11):1889-95. [PubMed] [Google Scholar]
- Yamagishi A, Morita T, Miyashita M, Akizuki N, Kizawa Y, Shirahige Y, et al. Palliative care in Japan: current status and a nationwide challenge to improve palliative care by the Cancer Control Act and the Outreach Palliative Care Trial of Integrated Regional Model (OPTIM) Study. American Journal of Hospice and Palliative Medicine 2008;25(5):412-8. [DOI] [PubMed] [Google Scholar]
Smeenk 1998a {published data only}
- Smeenk FWJM, Ament AJHA, Van Haastregt JCM, De Witte LP, Crebolder HFJM. Cost analysis of transmural home care for terminal cancer patients. Patient Education and Counseling 1998b;35(3):201-11. [DOI] [PubMed] [Google Scholar]
- Smeenk FWJM, Witte LP, Nooyen IWCJ, Crebolder HFJM. Effects of transmural care on coordination and continuity of care. Patient Education and Counseling 2000;41(1):73-81. [DOI] [PubMed] [Google Scholar]
- Smeenk FWJM, Witte LP, Van Haastregt JCM, Schipper RM, Crebolder HFJM. Transmural care of terminal cancer patients: lower re-hospitalization, and increased quality of life for patients and informal caregivers without extra health care costs [Transmurale zorg voor terminale kankerpatiënten: kortere heropnameduur, en toegenomen kwaliteit van leven voor patiënten en verzorgers zonder extra kosten]. Nederlands Tijdschrift voor Geneeskunde 1998;142(52):2846-50. [Google Scholar]
- Smeenk FWJM, De Witte Md LP, Van Haastregt JCM, Schipper RM, Biezemans HPH, Crebolder HFJM. Transmural care. A new approach in the care for terminal cancer patients: its effects on re-hospitalization and quality of life. Patient Education and Counseling 1998a;35(3):189-99. [DOI] [PubMed] [Google Scholar]
Temel 2010 {published data only}
- Temel JS, Greer JA, Muzikansky A, Gallagher ER, Admane S, Jackson VA, et al. Early palliative care for patients with metastatic non–small-cell lung cancer. The New England Journal of Medicine 2010;363(8):733-42. [DOI] [PubMed] [Google Scholar]
- Temel JS, Jackson VA, Billings JA, Dahlin C, Block SD, Buss MK, et al. Phase II study: integrated palliative care in newly diagnosed advanced non-small-cell lung cancer patients. Journal of Clinical Oncology 2007;25(17):2377-82. [DOI] [PubMed] [Google Scholar]
- Temel JS, McCannon J, Greer JA, Jackson VA, Ostler P, Pirl WF, et al. Aggressiveness of care in a prospective cohort of patients with advanced NSCLC. Cancer 2008;113(4):826-33. [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
Hwang 2009 {published data only}
- Hwang MS, Ryu HS. Effects of a palliative care program based on home care nursing [in Korean]. Journal of Korean Academy of Nursing 2009;39(4):528-38. [DOI] [PubMed] [Google Scholar]
Park 2011 {published data only}
- Park CS, Yoo YS, Choi DW, Park HJ, Kim JI. Development and evaluation of hospice smart patient service program [in Korean]. Journal of Korean Academy of Nursing 2011;41(1):9-17. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
Abernethy 2006 {published data only}
- Abernethy AP, Currow DC, Hunt R, Williams H, Roder-Allen G, Rowett D, et al. A pragmatic 2 x 2 x 2 factorial cluster randomized controlled trial of educational outreach visiting and case conferencing in palliative care-methodology of the Palliative Care Trial. Contemporary Clinical Trials 2006;27(1):83-100. [DOI] [PubMed] [Google Scholar]
- Abernethy AP, Shelby-James T, Fazekas BS, Woods D, Currow DC. The Australia-modified Karnofsky Performance Status (AKPS) scale: a revised scale for contemporary palliative care clinical practice. BMC Palliative Care 2005;4:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agar M, Currow D, Shelby-James TM, Plummer J, Sanderson C, Abernethy AP. Preference for place of care and place of death in palliative care: are these different questions? Palliative Medicine 2008;22(7):787-95. [DOI] [PubMed] [Google Scholar]
- Currow D, Abernethy AP, Shelby-James TM, Philips PA. The impact of conducting a regional palliative care clinical study. Palliative Medicine 2006;20(8):735-43. [DOI] [PubMed] [Google Scholar]
- Currow D, Stevenson JP, Abernethy AP, Plummer J, Shelby-James TM. Prescribing in palliative care as death approaches. Journal of the American Geriatrics Society 2007;55(4):590-5. [DOI] [PubMed] [Google Scholar]
- Mitchell GK, Abernethy AP. A comparison of methodologies from two longitudinal community-based randomized controlled trials of similar interventions in palliative care: what worked and what did not? Journal of Palliative Medicine 2005;8(6):1226-37. [DOI] [PubMed] [Google Scholar]
- Shelby-James TM, Currow D, Philips PA, Williams H, Abernethy AP. Promoting patient centred palliative care through case conferencing. Australian Family Physician 2007;36(11):961-4. [PubMed] [Google Scholar]
Allen 2012 {published and unpublished data}
- Allen KR, Hazelett SE, Radwany S, Ertle D, Fosnight SM, Moore PS. The promoting effective advance care for elders (PEACE) randomized pilot study: Theoretical framework and study design. Population Health Management 2012;15(2):71-7. [DOI] [PubMed] [Google Scholar]
- Allen KR, Radwany SM, Kropp DJ, Ertle D Fosnight S, Moore P, Hazelett SE. The peace pilot study: Convergence of geriatrics and palliative care. Journal of the American Geriatrics Society 2012;60:S222-S223. [Google Scholar]
Battaglia 2012 {published data only}
- Battaglia MA, Giordano A, Grasso MG, Lopes L, Martino G, Morino P, et al. Home-based palliative care for people with severe MS: Development of a new intervention (#69). Multiple Sclerosis 2012;18(5):S43-S44. [Google Scholar]
Butler 2012 {published data only}
- Butler C, Holdsworth LM, Coulton S, Gage H. Evaluation of a hospice rapid response community service: A controlled evaluation. BMC Palliative Care 2012;11:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chvetzoff 2006 {published data only}
- Chvetzoff G, Perol D, Devaux Y, Lancry L, Rebattu P, Magnet M, et al. Prospective study on the quality of care and quality of life in advanced cancer patients treated at home or in hospital:intermediate analysis of the Trapado study [Étude prospective de qualité des soins et de qualité de viechez des patients cancéreux en phase palliative, en hospitalisation ou à domicile: analyse intermédiairede l’étude Trapado]. Bulletin du Cancer 2006;93(2):213-21. [PubMed] [Google Scholar]
Duursma 2011 {published data only}
- Duursma F, Schers HJ, Vissers KC, Hasselaar J. Study protocol: Optimization of complex palliative care at home via telemedicine. A cluster randomized controlled trial. BMC Palliative Care 2011;10:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Addington‐Hall 2001a
- Addington-Hall JM, Higginson IJ. Palliative Care for Non-Cancer Patients. Oxford: Oxford University Press, 2001. [Google Scholar]
Addington‐Hall 2001b
- Addington-Hall J, McPherson C. After-death interviews with surrogates/bereaved family members: some issues of validity. Journal of Pain and Symptom Management 2001;22(3):784-90. [DOI] [PubMed] [Google Scholar]
Altman 1995
- Altman DG, Bland JM. Absence of evidence is not evidence of absence. BMJ 1995;311(7003):485. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bell 2009
- Bell CL, Somogyi-Zalud E, Masaki KH. Methodological review: measured and reported congruence between preferred and actual place of death. Palliative Medicine 2009;23(6):482-90. [DOI] [PubMed] [Google Scholar]
Beynon 2011
- Beynon T, Gomes B, Murtagh FE, Glucksman E, Parfitt A, Burman R, et al. How common are palliative care needs among older people who die in the emergency department? Emergency Medicine Journal 2011;28(6):491-5. [DOI] [PubMed] [Google Scholar]
Bradford Hill 1965
- Bradford Hill A. The environment or disease: association or causation? Proceedings of the Royal Society of Medicine 1965;58(5):295-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bruera 2006
- Bruera E, Higginson IJ, Ripamonti C, Gunten C. Textbook of Palliative Medicine. London: Hodder Arnold, 2006. [Google Scholar]
Brunetti 2003
- Brunetti M, Shemilt I, Pregno S, Vale L, Oxman AD, Lord J, et al. GRADE guidelines: 10. Considering resource use and rating the quality of economic evidence. Journal of Clinical Epidemiology 2013;66(2):140-50. [DOI] [PubMed] [Google Scholar]
Choi 2005
- Choi KS, Chae YM, Lee CG, Kim SY, Heo DS, Kim JS, et al. Factors influencing preferences for place of terminal care and of death among cancer patients and their families in Korea. Supportive Care in Cancer 2005;13(8):565-72. [DOI] [PubMed] [Google Scholar]
Cohen 1992
- Cohen J. A power primer. Psychological Bulletin 1992;112(1):155-9. [DOI] [PubMed] [Google Scholar]
Cohen 2010
- Cohen J, Houttekier D, Onwuteaka-Philipsen B, Miccinesi G, Addington-Hall J, Kaasa S, et al. Which patients with cancer die at home? A study of six European countries using death certificate data. Journal of Clinical Oncology 2010;28(13):2267-73. [DOI] [PubMed] [Google Scholar]
DerSimonian 1986
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clinical Trials 1986;7(3):177-88. [DOI] [PubMed] [Google Scholar]
Downing 2010
- Downing J, Powell RA, Mwangi-Powell F. Home-based palliative care in sub-Saharan Africa. Home Healthcare Nurse 2010;28(5):298-307. [DOI] [PubMed] [Google Scholar]
Drummond 1996
- Drummond MF, Jefferson TO. Guidelines for authors and peer reviewers of economic submissions to the BMJ. The BMJ Economic Evaluation Working Party. BMJ 1996;313(7052):275-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
EAPC 2008
EAPC 2010
- EAPC 2010. Abstracts: Oral, Plenaries and Invited Lectures. In: Palliative Medicine. Vol. 24 suppl 4. 2010:S4-S239.
Farquhar 2009
- Farquhar MC, Higginson IJ, Fagan P, Booth S. The feasibility of a single-blinded fast-track pragmatic randomised controlled trial of a complex intervention for breathlessness in advanced disease. BMC Palliative Care 2009;8:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ferrell 2010
- Ferrell BR, Coyle N. Oxford Textbook of Palliative Nursing. Third edition. New York: Oxford University Press, 2010. [Google Scholar]
Flory 2004
- Flory J, Young-Xu Y, Gurol I, Levinsky N, Ash A, Emanuel E. Place of death: U.S. Trends since 1980. Health Affairs 2004;23(3):194-200. [DOI] [PubMed] [Google Scholar]
Gao 2013
- Gao W, Ho YK, Verne J, Glickman M, Higginson IJ, on behalf of the GUIDE_Care project. Changing patterns in place of cancer death in England: a population-based study. PLoS Medicine 2013;10(3):e1001410. doi:10.1371/journal.pmed.1001410. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gomes 2006
- Gomes B, Higginson IJ. Factors influencing death at home for terminally ill patients with cancer. BMJ 2006;332(7540):515-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gomes 2008
- Gomes B, Higginson IJ. Where people die (1974-2030): past trends, future projections and implications for care. Palliative Medicine 2008;22(1):33-41. [DOI] [PubMed] [Google Scholar]
Gomes 2009
- Gomes B, Higginson IJ, McCrone P. Effectiveness and cost-effectiveness of home palliative care services for adults with advanced illness and their caregivers. Cochrane Database of Systematic Reviews 2009, Issue 2. Art. No: CD007760. [DOI: 10.1002/14651858.CD007760] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gomes 2011
- Gomes B, Cohen J, Deliens L, Higginson IJ. International trends in circumstances of death and dying among older people. In: Gott M, Ingleton C, editors(s). Living with ageing and dying: palliative and end of life care for older people. 1st edition. London: Oxford University Press, 2011. [Google Scholar]
Gomes 2012a
Gomes 2012b
- Gomes B, Higginson IJ, Calanzani N, Cohen J, Deliens L, Daveson BA, et al on behalf of PRISMA. Preferences for place of death if faced with advanced cancer: a population survey in England, Flanders, Germany, Italy, the Netherlands, Portugal and Spain. Annals of Oncology 2012;23(8):2006-15. [DOI] [PubMed] [Google Scholar]
Gomes 2013
- Gomes B, Calanzani N, Gysels M, Hall S, Higginson IJ. Heterogeneity and changes in preferences for dying at home: a systematic review. BMC Palliative Care 2013;12:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gonzalez‐Perez 2002
- Gonzalez-Perez JG. Developing a scoring system to quality assess economic evaluations. European Journal of Health Economics 2002;3(2):131-6. [DOI] [PubMed] [Google Scholar]
Grande 2000
- Grande GE, Todd CJ. Why are trials in palliative care so difficult? Palliative Medicine 2000;14(1):69-74. [DOI] [PubMed] [Google Scholar]
Hanks 2009
- Hanks G, Cherny NI, Christakis NA, Fallon M, Kaasa S, Portenoy RK. Oxford Textbook of Palliative Medicine. Fourth edition. New York: Oxford University Press, 2009. [Google Scholar]
Harding 2003
- Harding R, Higginson IJ. What is the best way to help caregivers in cancer and palliative care? A systematic literature review of interventions and their effectiveness. Palliative Medicine 2003;17(1):63-74. [DOI] [PubMed] [Google Scholar]
Harding 2005
- Harding R, Higginson IJ. Palliative care in sub-Saharan Africa. Lancet 2005;365(9475):1971-5. [DOI] [PubMed] [Google Scholar]
Harding 2011
Heyland 2006
- Heyland DK, Dodek P, Rocker G, Groll D, Gafni A, Pichora D, et al. What matters most in end-of-life care: perceptions of seriously ill patients and their family members. Canadian Medical Association Journal 2006;174(5):627–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane-handbook.org.
Higginson 2000
- Higginson IJ, Sen-Gupta GJA. Place of care in advanced cancer: a qualitative systematic literature review of patient preferences. Journal of Palliative Medicine 2000;3(3):287-300. [DOI] [PubMed] [Google Scholar]
Higginson 2003
- Higginson IJ, Finlay IG, Goodwin DM, Hood K, Edwards AGK, Cook A, et al. Is there evidence that palliative care teams alter end-of-life experiences of patients and their caregivers? Journal of Pain and Symptom Management 2003;25(2):150-68. [DOI] [PubMed] [Google Scholar]
Houttekier 2011
- Houttekier D, Cohen J, Surkyn J, Deliens L. Study of recent and future trends in place of death in Belgium using death certificate data: a shift from hospitals to care homes. BMC Public Health 2011;11:228. [DOI] [PMC free article] [PubMed] [Google Scholar]
Khaw 1999
- Khaw KT. How many, how old, how soon? BMJ 1999;319(7221):1350-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
McPherson 2003
- McPherson CJ, Addington-Hall JM. Judging the quality of care at the end of life: can proxies provide reliable information? Social Science & Medicine 2003;56(1):95-109. [DOI] [PubMed] [Google Scholar]
Moore 2011
- Moore RA, Wiffen PJ, Derry S, McQuay HJ. Gabapentin for chronic neuropathic pain and fibromyalgia in adults. Cochrane Database of Systematic Reviews 2011, Issue 3. Art. No: CD007938. [DOI: 10.1002/14651858.CD007938.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
NCPC 2012
- National Council for Palliative Care. National survey of patient activity data for specialist palliative care services. MDS full report for the year 2010-2011. www.endoflifecare-intelligence.org.uk/view?rid=672 (accessed 25 April 2013).
NHPCO 2012
- National Hospice and Palliative Care Organization. NHPCO facts and figures: hospice care in America. http://www.nhpco.org/sites/default/files/public/Statistics_Research/2012_Facts_Figures.pdf (accessed 25 April 2013).
RevMan 2011 [Computer program]
- Review Manager (RevMan). Version 5.1. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011.
Rinck 1997
- Rinck GC, den Bos GA, Kleijnen J, Haes HJ, Schadé E, Veenhof CH. Methodologic issues in effectiveness research on palliative cancer care: a systematic review. Journal of Clinical Oncology 1997;15(4):1697-707. [DOI] [PubMed] [Google Scholar]
Robinson 1996
- Robinson BE Pham H. Cost-effectiveness of hospice care. Clinics in Geriatric Medicine 1996;12(2):417-28. [PubMed] [Google Scholar]
Saunders 2000
- Saunders C. The evolution of palliative care. Patient Education and Counselling 2000;41(1):7-13. [DOI] [PubMed] [Google Scholar]
Schulz 2010
- Schulz KF, Altman DG, Moher D, for the CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c332. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shepperd 2011
- Shepperd S, Wee B, Straus S. Hospital at home: home-based end of life care. Cochrane Database of Systematic Reviews 2011, Issue 7. Art. No: CD009231. [DOI: 10.1002/14651858.CD009231] [DOI] [PMC free article] [PubMed] [Google Scholar]
Smeenk 1998b
- Smeenk FWJM, Haastregt JCM, Witte LP, Crebolder HFJM. Effectiveness of home care programmes for patients with incurable cancer on their quality of life and time spent in hospital. BMJ 1998;316(7149):1939-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Steinhauser 2000
- Steinhauser KE, Christakis NA, Clipp EC, McNeilly M, McIntyre L, Tulsky JA. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA 2000;284(19):2476-82. [DOI] [PubMed] [Google Scholar]
Tang 2002
- Tang ST, McCorkle R. Use of family proxies in quality of life research for cancer patients at the end of life: a literature review. Cancer Investigation 2002;20(7-8):1086-104. [DOI] [PubMed] [Google Scholar]
Tarnow‐Mordi 1999
- Tarnow-Mordi WO, Healy MJ. Distinguishing between "no evidence of effect" and "evidence of no effect" in randomised controlled trials and other comparisons. Archives of Disease in Childhood 1999;80(3):210-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Teno 2005
- Teno JM. Measuring end-of-life care outcomes retrospectively. Journal of Palliative Medicine 2005;8 Suppl 1:S42-9. [DOI] [PubMed] [Google Scholar]
Teno 2013
- Teno J, Gozalo PL, Leland NE, Miller SC, Morden NE, Scupp T, et al. Change in end-of-life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA 2013;309(5):470-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Thomas 2004
- Thomas C, Morris SM, Clark D. Place of death: preferences among cancer patients and their carers. Social Science and Medicine 2004;58(12):2431-44. [DOI] [PubMed] [Google Scholar]
Van Tulder 2003
- Van Tulder M, Furlan A, Bombardier C, Bouter L. Updated method guidelines for systematic reviews in the Cochrane collaboration back review group. Spine 2003;28(12):1290-9. [DOI] [PubMed] [Google Scholar]
Walsh 2009
- Walsh D, Caraceni AT, Fainsinger R, Foley K, Glare P, Goh C, et al. Palliative Medicine. Philadelphia, PA: Saunders Elsevier, 2009. [Google Scholar]
WHO 2011
- World Health Organization. Palliative Care for older people: better practices. www.euro.who.int/__data/assets/pdf_file/0017/143153/e95052.pdf (accessed 25 April 2013).
Wilson 2009
- Wilson DM, Truman CD, Thomas R, Fainsinger R, Kovacs-Burns K, Froggatt K, et al. The rapidly changing location of death in Canada, 1994-2004. Social Science & Medicine 2009;68(10):1752-8. [DOI] [PubMed] [Google Scholar]
Zimmermann 2008
- Zimmermann C, Riechelmann R, Krzyzanowska M, Rodin G, Tannock I. Effectiveness of specialized palliative care: a systematic review. JAMA 2008;299(14):1698-709. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Gomes 2014
- Gomes B, Calanzani N, Higginson IJ. Benefits and Costs of Home Palliative Care Compared With Usual Care for Patients With Advanced Illness and Their Family Caregivers. JAMA 2014;311(10):1060-1. [DOI] [PubMed] [Google Scholar]


