Abstract
Iatrogenic injury accounts for the second most common cause of acquired diaphragmatic hernias after penetrating trauma. An increased incidence of these hernias has been observed with the widespread use of laparoscopic surgery. We present the case of a 65-year-old woman who initially underwent sigmoid resection for an adenocarcinoma and a subsequent liver resection for metastasis. She was noted to have a left lower lobe pulmonary nodule on surveillance computed tomography, for which she underwent a mini-thoracotomy for a planned resection. At the time of surgery, the pulmonary nodule was discovered to be a diaphragmatic hernia, most probably of iatrogenic origin. We discuss the difficulty in diagnosis given her history and the location of such a lesion.
Keywords: Diaphragm, Lung cancer, Surgical therapy, Clinical epidemiology
Iatrogenic diaphragmatic hernias are becoming increasingly common given the increased use of laparoscopy. The majority of them are left-sided owing to the liver protecting the right hemidiaphragm. We present the case of a 65-year-old woman who was referred to our service for consideration for resection of a solitary pulmonary nodule in the left lower lobe. She had previously undergone anterior resection for a sigmoid adenocarcinoma and laparoscopic liver resection for metastasis. At the time of surgery, no lesion was identified in the lung and the suspected pulmonary nodule was noted to be a diaphragmatic hernia. We discuss the challenges of diagnosing a small diaphragmatic hernia.
Case History
A 65-year-old woman was referred with a completely asymptomatic pulmonary nodule, discovered on surveillance computed tomography (CT). This was performed as part of her routine follow-up review for a previous sigmoid adenocarcinoma, for which she had undergone anterior resection in October 2012. Subsequently, in January 2013, she had undergone a laparoscopic partial left hepatic lobectomy for metastasis.
CT of the chest in September 2013 revealed a suspected pulmonary nodule (17mm × 21mm) in the left lower lobe just above the diaphragm (Fig 1A). CT ten months later showed no significant change in this lesion. The positron emission tomography (PET) showed a lesion in the left lower lobe abutting the diaphragm with a maximum standardised uptake value of 1.9 (Fig 1B). Despite the low uptake, this could still represent a pulmonary metastasis and she therefore underwent a left mini-thoracotomy for removal of this suspected nodule.
Figure 1.
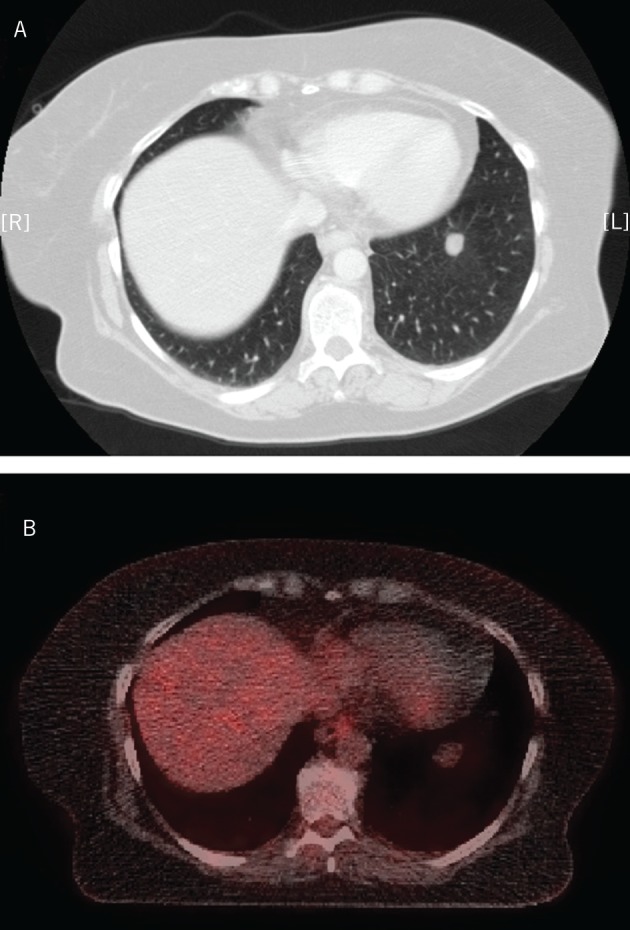
Axial computed tomography suggestive of a left lower lobe lung nodule (A) and positron emission tomography demonstrating a maximum standard uptake value of 1.9 (B)
At the time of surgery, the lung was thoroughly palpated but no pulmonary mass was identified. However, a small lesion on the diaphragmatic surface was noted. It measured approximately 2cm × 2cm and appeared cystic in nature (Fig 2). Following further inspection, a defect of 0.5cm × 0.5cm could be demonstrated in the diaphragm, directly underlying the lesion, and the mass was deemed to be a diaphragmatic hernia, most likely related to the previous abdominal surgery. The hernia sac was opened to reveal omental fat. A small phrenotomy was performed and the sac content was repositioned in the peritoneal cavity. The hernia sac was excised and the diaphragmatic defect was closed in a primary fashion with two layers of non-absorbable suture. The patient made a good recovery and was discharged home on the fourth postoperative day.
Figure 2.
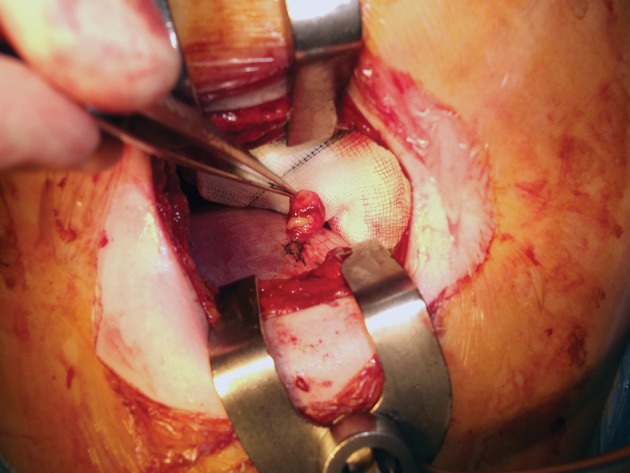
Intraoperative photograph with the sac of the diaphragmatic hernia held in the forceps
Discussion
Diaphragmatic hernias can be subcategorised into congenital or acquired hernias. Of those acquired, trauma is the most common cause, followed by iatrogenic and spontaneous defects. Owing to the increased use of laparoscopic surgery, these hernias are being seen in greater frequency. They most commonly occur on the left side; the right hemidiaphragm is felt to be protected by the liver. The use of long grasping instruments, diathermy and ultrasonically activated scissors is associated with greater risk of diaphragmatic injuries.1
This case demonstrates that diaphragmatic hernias can be difficult to diagnose and could even go as far as to mimic a pulmonary nodule. In the reported case, the diagnosis was made challenging by several issues: the patient was completely asymptomatic, there was strong past medical history of cancer with previous metastasis, the imaging was deceptive and obtaining a tissue diagnosis preoperatively was deemed unfeasible.
Large diaphragmatic defects are often discovered early owing to significant cardiorespiratory compromise. In the case of smaller defects, presenting symptoms can be more discrete and non-specific, such as pain, reflux, nausea or intestinal obstruction. In our case, the diaphragmatic defect was less than 1cm and therefore unlikely to produce symptoms. Given the patient’s history of colorectal carcinoma with previous metastasis, the suspicion of further metastasis was high.
For larger diaphragmatic hernias, chest radiography is a useful screening tool. However, the sensitivity is only 50%.2 A study by Peer et al showed the sensitivity of CT to be 71% (78% for left hemidiaphragm lesions and 50% for right hemidiaphragmatic lesions) and the specificity to be approximately 80%.3 Both the CT and PET reports suggested that this lesion was in the lung and should be treated as a metastasis unless proven otherwise. The PET revealed a standardised uptake value of 1.9. The sensitivity and specificity of PET has been showed to be 96% and 88% respectively in diagnosing a nodule as malignant.4 Owing to the low spatial resolution of PET, the negative predictive value and sensitivity are lower.
As a result of the location, it was not possible to obtain biopsies via an endobronchial approach. A study by Guimarães et al showed that a quarter of CT guided biopsies were not helpful in obtaining a definitive diagnosis.5 These included samples that were inadequate for analysis and where cells were insufficient to confirm a diagnosis. In light of the past medical history, proceeding with elective resection was considered the most prudent approach for definitive resolution.
Conclusions
This case demonstrates the diagnostic challenges a small iatrogenic diaphragmatic hernia can present, which in this case led to misdiagnosis. It provides a unique learning point that an iatrogenic diaphragmatic hernia may present as a pulmonary nodule and patients with previous history of abdominal surgery should be approached with a degree of suspicion when investigated for discrete pulmonary lesions, which appear close to the diaphragmatic surface.
References
- 1. Suh Y, Lee JH, Jeon H et al. Late onset iatrogenic diaphragmatic hernia after laparoscopy-assisted total gastrectomy for gastric cancer. J Gastric Cancer 2012; 12: 49–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Johnson CD, Ellis H. Acquired hernias of the diaphragm. Postgr Med J 1988; 64: 317–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Peer SM, Devaraddeppa PM, Buggi S. Traumatic diaphragmatic hernia – our experience. Int J Surg 2009; 7: 547–549. [DOI] [PubMed] [Google Scholar]
- 4. Patz EF, Lowe VJ, Hoffman JM et al. Focal pulmonary abnormalities: evaluation with F-18 fluorodeoxyglucose PET scanning. Radiology 1993; 188: 487–490. [DOI] [PubMed] [Google Scholar]
- 5. Guimarães MD, Chojniak R, Gross JL, Bitencourt AG. Predictive success factors for CT-guided fine needle aspiration biopsy of pulmonary lesions. Clinics 2009; 64: 1,139–1,144. [DOI] [PMC free article] [PubMed] [Google Scholar]


