Abstract
Introduction
Methylene blue (MB) has been used in the identification of abnormal parathyroid glands in surgery for hyperparathyroidism. Its efficacy and safety profile have been questioned recently and this study sought to demonstrate such aspects in a unit where its use is routine.
Methods
Prospective data collected over six years in a single surgeon’s practice were interrogated to identify factors affecting MB staining, side effects suffered and unusual cases where the dye was invaluable in locating the diseased gland.
Results
A total of 98 patients underwent MB infusion. Of these, 77 cases (78.6%) stained positively with MB and 21 (21.4%) did not. Six patients suffered side effects but there were no cases of neurotoxicity. No positive predictive factors of dye uptake were found. MB was particularly useful in cases of intrathyroidal and ectopic glands as well as improving efficiency in both targeted and open parathyroidectomy.
Conclusions
This series shows that when used correctly, MB is efficacious in locating diseased parathyroid glands, with similar sensitivity rates to preoperative ultrasonography and radionucleotide imaging. Adverse effects were much lower than published previously, which may be attributed to the low dose of MB used (3.5mg/kg).
Keywords: Parathyroidectomy, Methylene blue, Neurotoxicity syndromes, Hyperparathyroidism
The prevalence of primary hyperparathyroidism is increasing.1 The increase is multifactorial but indicates that clinicians treating the condition should expect to operate on larger numbers of patients in the future, and efficient investigation and operative technique are therefore vital.
Identifying diseased glands can be a challenge. A number of tools are available to the surgeon to provide both pre and intraoperative assistance. Preoperative ultrasonography and radioisotope (technetium sestamibi [MIBI] and single photon emission computed tomography [SPECT]) imaging can help to identify hyperfuntioning/enlarged parathyroid glands and their anatomical location. If concordant, they make successful parathyroidectomy via a targeted minimally invasive approach very suitable and preferable in a predominantly older patient population. Although intraoperative parathyroid hormone (PTH) monitoring and the gamma probe have been used more recently to help demonstrate abnormal glands, preoperative intravenous methylene blue (MB) infusion has been used as a safe and effective method of facilitating the identification of abnormal eutopic and ectopic glands for over 40 years.
MB was first advocated in parathyroid surgery in 1971 by Dudley2 and is used regularly in the identification of parathyroid adenomas today. Reports suggest it can be administered by intravenous infusion at varying times both prior and during to surgery at doses ranging from 3mg/kg to 7.5mg/kg.3 However, the staining of parathyroid glands with MB has been found to be variable and ranged from 83% to 100% in a 2012 systematic review by Patel et al, who also questioned the value and safety of MB, particularly with regard to the neurotoxic effects in patients taking selective serotonin reuptake inhibitors (SSRIs).4
The variable staining of pathological parathyroid glands has also been noted in our own department where the use of MB as an adjunct to the intraoperative identification of parathyroid adenomas is routine. This study sought to identify factors that might influence the uptake of MB in patients undergoing a parathyroidectomy for primary and tertiary hyperparathyroidism as well as its safety profile and use in ectopic adenoma identification.
Methods
A detailed audit of a prospective series of patients undergoing parathyroid surgery between February 2007 and January 2013 was carried out from an Excel® spreadsheet database (Microsoft, Redmond, WA, US) and, where required, retrospective medical note review. Results were analysed using SPSS® version 21 (IBM, New York, US).
All patients presented with biochemical evidence of primary hyperparathyroidism (calcium >2.60mmol/l and PTH >6.2pmol/l) and were seen in a joint endocrine clinic. All patients underwent initial ultrasonography and radionucleotide imaging of the neck (MIBI imaging up until 2011, when SPECT was introduced). MB was given as an intravenous infusion at a dose of 3.5mg/kg diluted in 500ml of dextrose saline over the hour immediately prior to surgery.
In cases with concordant imaging locating single gland disease, minimally invasive parathyroidectomy was the standard approach together with surface marking of the adenoma using ultrasonography on the day of surgery. The lateral thyroid space was accessed through a 3cm horizontal incision extending posteriorly from the surface marker. Careful dissection to locate the adenoma was performed with full consideration of the recurrent laryngeal nerve. In multiple endocrine neoplasia syndromes or where imaging was inconclusive, non-concordant or demonstrated multiple adenomas, open exploration of the neck was chosen in order to explore the typical as well as the ectopic sites for parathyroid adenoma if necessary.
Results
A total of 104 parathyroid operations were performed. Six cases were excluded from the study, three owing to unavailability of case notes and three where MB was not given. Consequently, 98 cases receiving preoperative intravenous MB infusion were available for the analysis of parathyroid gland dye uptake, surgical benefit and the incidence of adverse effects.
In 77 cases (78.6%), the diseased parathyroid glands were stained with MB to varying degrees from dark blue to a blue green turquoise (MB positive). In 15 cases (15.3%), a histologically proven parathyroid adenoma was identified that remained a normal colour and did not stain (MB negative) and in 6 cases (6.1%), no abnormal or stained parathyroid gland was found following extensive exploration of the neck. Of these six, subsequent investigation identified two mediastinal adenomas, two intrathyroid adenomas and one MB negative ectopic adenoma in the neck; in one case, an adenoma has never been found despite extensive extensive surgical exploration and investigation including PTH selective venous sampling.
Using Fisher’s exact test for binary data variables including sex, gland side and SPECT result (positive/negative), and the independent t-test for continuous variables of age, preoperative calcium, renal function, PTH and 24-hour urinary calcium levels, no variable was found to have statistical significance in predicting a positive parathyroid uptake of MB.
There was a low number of adverse effects during MB infusion in this series. In particular, no cases of neurotoxicity were encountered. Two patients experienced pain at the infusion site although they completed the full infusion at a slower rate, which resolved the symptom. Hypotension in two other patients resulted in stopping the infusion in one case and completing it at a slower rate in another. A further patient’s infusion was ceased prematurely owing to wheezing and another patient experienced transient bradycardia following the infusion. None of the adverse effects delayed the surgery or caused long-term harm.
A number of patients presented a challenge for which the MB proved invaluable in identifying the pathological gland.
Intrathyroidal tumours
Six patients had intrathyroidal adenomas requiring a thyroid lobectomy. Three of these were performed at the first operation owing to heavy staining of the relevant thyroid pole with MB in the absence of any extrathyroidal adenoma. In another patient, persistent hypercalcaemia followed removal of a proven MB stained inferior parathyroid adenoma, in which a MB negative intrathyroidal adenoma on the same side was removed subsequently by lobectomy at a second operation. Two further lobectomies were performed at a second operation after repeat imaging still identified an adenoma in close proximity to the thyroid that, at operation, could not be identified outside the thyroid gland (and only stained lightly with MB). In all six cases, histology results confirmed the diagnosis and all became normocalcaemic.
Ectopic position
Excluding intrathyroidal tumours, five adenomas in this series were found in ectopic positions. Two were located behind the suprasternal notch, one was adherent to the anterior surface of the T1 vertebral body, one was in the left carotid sheath and one was adjacent to the right carotid bifurcation but not in the sheath itself. All stained a deep blue, aiding tumour identification markedly.
Discussion
The current case series shows that MB is a safe and useful marker of parathyroid disease. While the the cohort of patients in this series was small compared with a systematic review from 2012,4 the outcomes of this specific protocol using low dose MB shows adverse effects of just 6%. This may be due to the lower dose used (3.5mg/kg) compared with other units, where the dose ranges from 5mg/kg to 7.5mg/kg even though the UK National Poisons Information Service recommends a maximum dose of 4mg/kg.
Eighteen other studies have identified serious side effects, including seventeen patients suffering neurotoxicity, all of whom were taking SSRIs. We have addressed this issue by advising the patients to stop their SSRI medication when they are listed for surgery. (Patients are encouraged to seek advice from their general practitioner regarding a suitable alternative.) This has allowed us to continue to use MB without any risk of neurotoxicity.
Initially, any adverse events were managed by nursing staff by stopping the infusion although latterly it was found that recommencing the infusion at a slower rate once the adverse effect had resolved was tolerated by the patient and allowed the infusion to be completed without any further problem. This suggests that adverse effects are not only dependent on the dose of MB but also on the rate of infusion. We therefore advocate a close working partnership with the nursing staff involved in administering MB with a written protocol made available and appropriate training given.
MB has been used regularly in our unit as an adjunct alongside preoperative imaging in the location of parathyroid adenomas. Positive predictive factors identifying which patients would take up the dye would have been valuable in order to avoid its use and the possibility of side effects in those where it would not be of benefit. Unfortunately, no such factors could be identified. While this is disappointing, the current evidence continues to support the use of MB in all patients without specific contraindications.
MB has been used in medicine since the 19th century and its first role was in the treatment of malaria. Since then, it has been used in a variety of conditions from the identification of tuberculosis (after which it was used unsuccessfully to treat the disease) to the monitoring of compliance with psychiatric medication (as the agent turns urine blue).5 In modern times, it has been used to treat priapism, pruritis ani and vasoplegic shock, and it remains a successful treatment of methemoglobinaemia.
Its dry form exists as dark green crystals and in solution, it is classically a dark blue. In its reduced form, it turns into the colourless leucomethylene blue and is readily reoxidised back to the blue state. It can be given both orally and intravenously. Its excretion via the kidney and liver results in blue urine and stools for several days after administration. Doses in excess of 7mg/kg will result in gastrointestinal symptoms5 and because of its structural similarity to monoamine oxidase inhibitors, it can precipitate signs of serotonin induced neurotoxicity with drugs that increase the availability of central serotonin levels.6 For this reason, it is absolutely contraindicated in patients taking concurrent SSRIs.
With a true positive rate of 78.6%, this puts MB use in line with previous case series and other investigative tools used in parathyroid disease. Ultrasonography is an efficient, non-invasive imaging modality with a sensitivity of 79% in locating adenomatous glands.7 Parathyroid scintigraphy has been shown in the same meta-analysis to have a sensitivity of 88% and it is widely acknowledged that the two modalities, in experienced hands, offer optimum location in single gland disease. MB can be considered an adjunct to these measures by complementing and confirming the findings but also offering an important intraoperative marker in multiglandular or ectopic disease, where sensitivity rates are far lower.8 In some cases, thyroid nodules, lymph nodes and other tissue may be mistaken for abnormal parathyroid glands when the patient has not had MB, which can be very helpful in distinguishing the blue stained parathyroids from other types of tissue that do not take up the dye.
In 21 cases, MB was unhelpful in identifying the abnormal parathyroid glands owing to a lack of visible staining, giving a false negative rate of 21.4%. It is therefore important to be able to recognise an abnormal unstained parathyroid gland, which was fortunately identified correctly at primary surgery in 15 patients. Five patients with intrathyroidal and ectopic parathyroid pathology required a second successful procedure following further investigation. Consequently, in an MB negative neck, we would advise that such locations are borne in mind. This might be anticipated in patients with multiple endocrine neoplasia where multiple and ectopic glands are to be expected but in fact only one individual in this subgroup had this syndrome.
Despite our efforts, the exact reason for the lack of MB staining of some parathyroid glands remains unclear. It is possible that at lower doses of MB, the concentration of dye is not sufficient to stain the glands in all cases. In addition, MB may convert to its colourless form (leucomethylene blue) in certain patients although we were also unable to find any specific factor that might account for this and no patients had a diagnosis of methemoglobinaemia. Differing histological subtypes may influence the intensity of staining as MB is taken up by parathyroid cells that can reduce it to the colourless form9 and so some subtypes may stain less readily than others. Future research assessing histological subtype with MB uptake might allow further understanding of this observation.
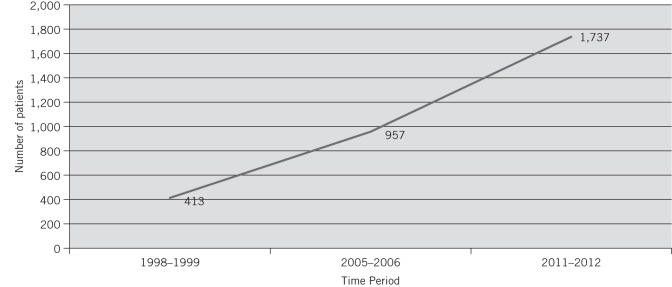
Parathyroid surgeons must have the tools to treat patients efficiently and safely. This is becoming more important as rates of primary hyperparathyroidism are increasing. In England, Hospital Episode Statistics data (http://www.hscic.gov.uk/hes) show that diagnostic coding of primary hyperparathyroidism has quadrupled in the last decade (Fig 1). This can be attributed to two main factors: increased screening for raised calcium and an ageing population in whom the disease is more prevelant, particularly affecting postmenopausal women.10
Figure 1.
Trends in the diagnosis of primary hyperparathyroidism in England
The current series highlights the benefits and advantages of MB infusion in patients undergoing minimally invasive as well as open surgery. MB aids efficient and rapid identification of abnormal glands in eutopic and, especially, in ectopic locations in the neck. As a result, both the amount of tissue dissection and the operating time have been shown to be significantly reduced with the use of MB,11–13 which must be better and safer for what is a generally older population of patients (as demonstrated in this series, where there was an average age of 60 years with a range of 15 to 89 years).
Conclusions
The current case series indicates that MB continues to have a valuable role in the surgical management of hyperparathyroidism. In particular, it is a useful adjunct to standard preoperative imaging by facilitating more rapid identification of an abnormal parathyroid in both targeted and open surgery, thereby leading to a reduction in operating time. It has also been demonstrated that at a low dose and in the absence of concurrent SSRIs, its use is very safe and efficacious.
The value of MB in the management of intrathyroid and ectopic adenomas in the neck is emphasised; familiarity with the technique as well as its effects on the patient through regular use are key to its success. However, the reason why some adenomas do not take up MB has not been determined by this study and further research is required to see whether the variation in MB uptake is related to differences in the cell subtype in the parathyroid adenoma itself.
Acknowledgements
The authors are grateful to the Centre for Applied Medical Statistics, Department of Public Health and Primary Care, University of Cambridge for providing statistical analysis.
References
- 1.Yu N, Donnan PT, Flynn RW et al. Increased mortality and morbidity in mild primary hyperparathyroid patients. The Parathyroid Epidemiology and Audit Research Study (PEARS). Clin Endocrinol 2010; 73: 30–34. [DOI] [PubMed] [Google Scholar]
- 2.Dudley NE. Methylene blue for rapid identification of the parathyroids. BMJ 1971; 3: 680–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pollack G, Pollack A, Delfiner J, Fernandez J. Parathyroid surgery and methylene blue: a review with guidelines for safe intraoperative use. Laryngoscope 2009; 119: 1,941–1,946. [DOI] [PubMed] [Google Scholar]
- 4.Patel HP, Chadwick DR, Harrison BJ, Balasubramanian SP. Systematic review of intravenous methylene blue in parathyroid surgery. Br J Surg 2012; 99: 1,345–1,351. [DOI] [PubMed] [Google Scholar]
- 5.Schirmer RH, Adler H, Pickhardt M, Mandelkow E. ‘Lest we forget you – methylene blue...’. Neurobiol Aging 2011; 32: 2325.e7–2325.e16. [DOI] [PubMed] [Google Scholar]
- 6.Gillman PK. Methylene blue implicated in potentially fatal serotonin toxicity. Anaesthesia 2006; 61: 1,013–1,014. [DOI] [PubMed] [Google Scholar]
- 7.Ruda JM, Hollenbeak CS, Stack BC. A systematic review of the diagnosis and treatment of primary hyperparathyroidism from 1995 to 2003. Otolaryngol Head Neck Surg 2005; 132: 359–372. [DOI] [PubMed] [Google Scholar]
- 8.Johnson NA, Carty SE, Tublin ME. Parathyroid imaging. Radiol Clin North Am 2011; 49: 489–509. [DOI] [PubMed] [Google Scholar]
- 9.May JM, Qu ZC, Cobb CE. Reduction and uptake of methylene blue by human erythrocytes. Am J Physiol Cell Physiol 2004; 286: C1390–C1398. [DOI] [PubMed] [Google Scholar]
- 10.Mackenzie-Feder J, Sirrs S, Anderson D et al. Primary hyperparathyroidism: an overview. Int J Endocrinol 2011; 251410. [DOI] [PMC free article] [PubMed]
- 11.Traynor S, Adams JR, Andersen P et al. Appropriate timing and velocity of infusion for the selective staining of parathyroid glands by intravenous methylene blue. Am J Surg 1998; 176: 15–17. [DOI] [PubMed] [Google Scholar]
- 12.Kuriloff DB, Sanborn KV. Rapid intraoperative localization of parathyroid glands utilizing methylene blue infusion. Otolaryngol Head Neck Surg 2004; 131: 616–622. [DOI] [PubMed] [Google Scholar]
- 13.Thabet MH, Askar SM, Ramadan EM. Minimally invasive, endoscopic assisted, parathyroidectomy (MIEAP) with intraoperative methylene blue (MB) identification. Egypt J Ear Nose Throat Allied Sci 2012; 13: 25–30. [Google Scholar]