Abstract
Introduction
High short-term failure rates have been reported for a variety of metal-on-metal (MoM) total hip replacements (THRs) owing to adverse reactions to metal debris (ARMD). This has led to the withdrawal of certain poorly performing THRs. This study analysed the outcomes of a MoM THR system.
Methods
Between 2004 and 2010, 578 uncemented MoM THRs (511 patients, mean age: 60.0 years) were implanted at one specialist centre. The THR system used consisted of the Corail® stem, Pinnacle® cup, Ultamet® liner and Articul/eze® femoral head (all DePuy, Leeds, UK). All patients were recalled for clinical review with imaging performed as necessary.
Results
The mean follow-up duration was 5.0 years (range: 1.0–9.1 years). Overall, 39 hips (6.7%) in 38 patients (all 36mm femoral head size) underwent revision at a mean time of 3.5 years (range: 0.01–8.3 years) from the index THR with 30 revisions (77%) performed in women. The cumulative eight-year survival rate for all THRs was 88.9% (95% confidence interval [CI]: 78.5–93.4%), with no difference (p=0.053) between male (95.2%, 95% CI: 84.2–98.7%) and female patients (85.3%, 95% CI: 70.2–92.1%) at eight years. Seventeen revisions (44%) were performed for ARMD. There was no significant difference in absolute postoperative Oxford hip scores between men and women (p=0.608). The mean acetabular inclination in unrevised THRs was 44.0°. Forty-seven non-revised THRs (8.7%) had blood metal ion concentrations above recommended thresholds (seven had periprosthetic effusions).
Conclusions
Although this MoM THR system has not failed as dramatically as other similar designs, we recommend against continued use and advise regular clinical surveillance to identify ARMD early.
Keywords: Adverse reaction, Metal-on-metal, Outcomes, Revision surgery, Total hip replacement
Total hip replacement (THR) is a successful procedure for the long-term alleviation of pain and disability in patients with hip arthritis.1 Aseptic loosening secondary to polyethylene wear remains the most frequent cause of failure of metal-on-polyethylene THR.2 Metal-on-metal (MoM) bearings became popular for use in THR as they produce fewer wear particles than traditional metal-on-polyethylene articulations.3 In addition, the use of large diameter MoM bearings has been associated with lower wear and dislocation rates than smaller diameter bearings.4,5 This led to a worldwide increase in large diameter MoM THR usage over the last decade.6,7
More recently, reports have shown that MoM hip bearings can be associated with adverse reactions to metal debris (ARMD) requiring revision surgery.8–10 Both joint registries and independent reports have demonstrated high short-term failure rates for a variety of MoM THR designs.7,11–13 Metal wear debris can be generated from the bearing surface as well as the trunnion–head interface,11,12 with increasing evidence that larger diameter femoral head sizes are associated with significantly higher failure rates than smaller MoM bearings.7,13 Poorly performing devices have subsequently been withdrawn from clinical use, with recommendations published on the surveillance and management of patients with MoM hip bearings that remain in situ.14,15
This single centre study assessed the outcomes of a MoM THR system implanted between 2004 and 2010. The study aims were to report the medium-term outcomes with this device in terms of implant survival, function, blood metal ion and radiological analysis.
Methods
Between 2004 and 2010, data were collected prospectively on all consecutive MoM THRs (n=578) implanted at one specialist arthroplasty centre with the Corail® femoral stem and the Pinnacle® acetabular component (both DePuy, Leeds, UK). Since 2010, this MoM THR system has not been implanted owing to reports of high failure rates with similar implants and various device recalls.11,12,14,15 All operations were performed in a laminar flow operating theatre by ten surgeons with three surgeons performing the majority (n=459, 79.4%). Data on patient demographics, primary indication for THR and components implanted were collected from the institution’s prospectively maintained database (Table 1).
Table 1.
Summary of the study cohort (578 hips)
| Sex | Female
Male |
340 (58.8%)
238 (41.2%) |
| Age | Mean (range) | 60.0 yrs
(19.8–88.0 yrs) |
| Bilateral procedures | Total patients
Single-stage bilateral procedures Two-stage bilateral procedures |
67 (134 hips)
1 (2 hips) 66 (132 hips) |
| Diagnosis | Primary osteoarthritis
Developmental dysplasia Avascular necrosis Inflammatory arthritis Neck of femur fracture Slipped upper femoral epiphysis Other causes |
533 (92.2%)
12 (2.1%) 10 (1.7%) 5 (0.9%) 5 (0.9%) 3 (0.5%) 10 (1.7%) |
| Follow-up duration | Mean (range) | 5.0 yrs (1.0–9.1 yrs) |
| Surgical approach | Posterior
Anterolateral |
537 (92.9%)
41 (7.1%) |
| Grade of surgeon | Consultant
Specialist registrar |
559 (96.7%)
19 (3.3%) |
| Femoral head size | 28mm
36mm |
14 (2.4%)
564 (97.6%) |
| Acetabular component size | Median (range) | 52mm (48–66mm) |
Implants
The Corail® femoral stem is a fully hydroxyapatite coated titanium alloy stem designed for insertion without cement. It is available in a range of sizes (6–20) with all but the smallest sizes being available with either a collar or collarless option. Three different options of neck geometry are available (standard, high offset and coxa vara) but the neck itself is not modular. All stem options have a 12/14 taper on to which, in this series, a 36mm or 28mm diameter cobalt chromium alloy metal femoral head (Articul/eze®; DePuy) was impacted. The Pinnacle® acetabular component is a hemispheric, porous coated titanium shell that is inserted without cement and can accommodate a polyethylene, ceramic or metal liner. In this series, metal liners were used (Ultamet®; DePuy). The acetabular component is available in a range of diameters (38–66mm) and includes solid back, spiked solid back, three-hole and multi-hole cup varieties.
Follow-up regimen
Patients underwent clinical review at six weeks, six months and one year following surgery with invitations for annual clinical review thereafter. All consultations included clinical examination, anteroposterior pelvic radiography and completion of the Oxford hip score (OHS) questionnaire.16 After the 2010 Medicines and Healthcare products Regulatory Agency (MHRA) alert, which highlighted concerns regarding ARMD associated with MoM hip replacements,14 all patients with MoM THRs were recalled for clinical review and blood metal ion sampling. Only patients with high blood metal ion concentrations underwent further hip imaging according to MHRA recommendations.15 Patients with high blood metal ion concentrations and periprosthetic effusions on further imaging were considered to have ARMD. ARMD was confirmed intraoperatively at revision and after histopathological analysis.
Data were collected on all revision THRs performed up until 31 October 2013 with details obtained from other hospitals if revisions were performed elsewhere. Data from the National Joint Registry were also used to confirm no revisions performed elsewhere were missed. All deaths were recorded with an assessment made in each case using the clinical notes and details held by the general practitioner as to whether the death was related to the surgery and whether the hip had been revised or remained in situ at the time of death.
Blood metal ion sampling
Blood metal ion sampling was performed at a minimum of one year following arthroplasty to avoid taking measurements during the running-in phase.17 Whole blood was obtained from each patient with cobalt and chromium concentrations measured using inductively coupled plasma mass spectrometry, as described previously.18 Blood metal ions were considered raised if cobalt and/or chromium concentrations were greater than 7μg/l, as per MHRA recommendations.15
Functional outcome and radiological analysis
The OHS was used to assess postoperative pain and disability following THR.16 It was expressed as a percentage (0% = healthy joint, 100% = worst possible joint), with questionnaires considered valid if they met the minimum inclusion criteria described previously.19,20 As the OHS is frequently scored on a scale of 0 to 48 points (0 = worst possible joint, 48 = healthy joint),21 these scores have also been provided to assist comparison with other reports. Preoperative scores were also available for analysis.
All postoperative anteroposterior pelvic radiography was consulted for signs of implant failure. Each radiograph was analysed using previously described recommendations for evidence of femoral22 or acetabular component loosening,23 acetabular component inclination,24 osteolysis and femoral stem subsidence.25
Statistical analysis
All statistical analysis was performed using R statistical software (R Foundation for Statistical Computing, Vienna, Austria). Cumulative THR survival was determined using the Kaplan–Meier method. The endpoint for survival analysis was revision surgery, defined as removal or exchange of any component implanted at the index arthroplasty. Patients not undergoing revision surgery were censored after their last contact with the hospital or after death. A Cox proportional hazards model was used to compare differences in THR survival for sex.26 Mood’s test was used to compare OHSs between the sexes. The level of significance was set at 95% (p<0.05) with confidence intervals (CIs) also at the 95% level.
Results
Survival analysis
All patients were reviewed following the institution’s recall. No patients were therefore lost to follow-up. The mean follow-up time since the index THR was 5.0 years (range: 1.0–9.1 years) with 92% (529/578 THRs) having a minimum follow-up duration of three years. There were 22 patient deaths (22 hips) during the follow-up period at a mean of 2.7 years (range: 1.4–6.5 years) from the index procedure. All deaths were unrelated to surgery.
During the follow-up period, 39 hips (6.7%) in 38 patients underwent revision surgery (Appendix 1 – available online) with all revisions performed at our institution. All 39 hips revised had an initial femoral head size of 36mm. The mean time from index THR to revision arthroplasty was 3.5 years (range: 0.01–8.3 years) with 30 revisions (77%) performed in women (Appendix 1).
The cumulative survival for all THRs (n=578) was 94.1% (95% CI: 91.3–96.3%) at 5 years (257 hips at risk) and 88.9% (95% CI: 78.5–93.4%) at 8 years (31 hips at risk) (Fig 1). The cumulative survival for the 238 THRs implanted in men was 96.3% (95% CI: 92.4–99.1%) at 5 years (84 hips at risk) and 95.2% (95% CI: 84.2–98.7%) at 8 years (14 hips at risk) with nine hips requiring revision. The cumulative survival for the 340 THRs implanted in women was 92.7% (95% CI: 89.0–95.7%) at 5 years (173 hips at risk) and 85.3% (95% CI: 70.2–92.1%) at 8 years (17 hips at risk) with 30 hips requiring revision. Sex did not significantly affect implant survival (p=0.053).
Figure 1.
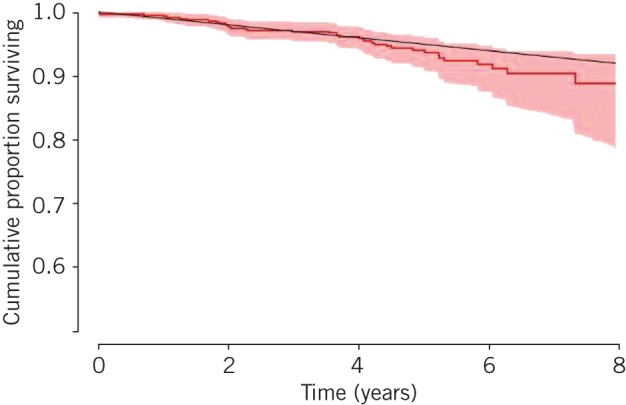
Kaplan–Meier survival curve for all 578 metal-on-metal total hip replacements. Revision for any indication was used as the endpoint for survival, with 39 hips revised in total. The shaded area represents the upper and lower limits of the 95% confidence intervals. The black line represents National Institute for Health and Care Excellence recommendations for implant survival (acceptable implant failure rate of up to 1% per year).
ARMD was the most common indication for revision surgery, accounting for 44% of the revisions performed (17/39) (Appendix 2 – available online). The mean acetabular inclination prior to ARMD revision for the 17 cases was 45.0° (range: 37.5–55.5°). Trunnion wear was observed macroscopically in six cases (35%) with four undergoing femoral component revisions and the other two less severe cases retaining their well fixed femoral stems (Appendix 2). All cases of ARMD were revised to a non-MoM articulation with no complications recorded at a mean of 0.8 years (range: 0.1–2.1 years) following revision surgery (Appendix 1). Blood metal ions normalised following revision in all but the five most recently performed ARMD revisions. The mean acetabular inclination following ARMD revision was 45.7° (range: 40.4–51.6°). At the time of writing, none of the surviving 539 MoM THRs were awaiting revision surgery.
Blood metal ion analysis
The median maximum blood metal ion concentrations recorded were 2.06μg/l (interquartile range [IQR]: 0.83–3.71μg/l) for cobalt and 1.25μg/l (IQR: 0.83–2.03μg/l) for chromium. Excluding revisions (n=39), 36 patients with 47 MoM THRs (8.7% of the non-revised cohort) had blood metal ion concentrations above 7μg/l (Figs 2 and 3). Fifteen hips had raised blood cobalt and chromium concentrations and thirty-two hips had raised blood cobalt concentrations with normal chromium levels.
Figure 2.
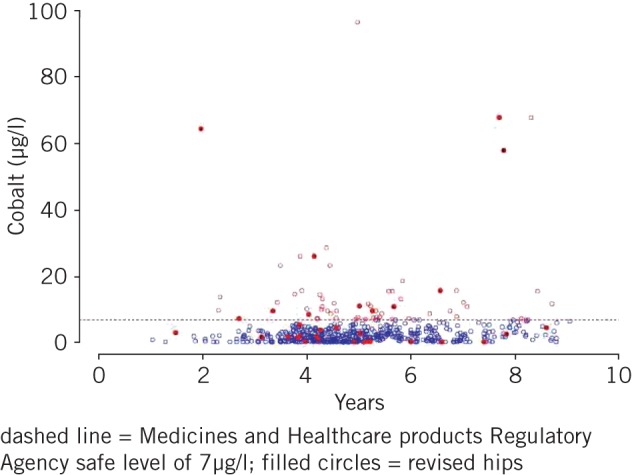
Maximum blood cobalt concentration following metal-on-metal total hip replacement
Figure 3.
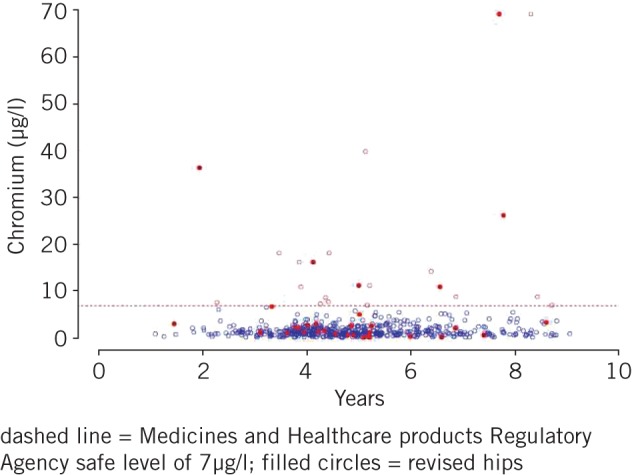
Maximum blood chromium concentration following metal-on-metal total hip replacement
Of the 25 unilateral MoM THRs with raised blood metal ion concentrations, 23 hips had normal hip ultrasonography and/or magnetic resonance imaging (under annual clinical follow-up) and 2 hips had periprosthetic fluid collections of variable sizes (under more regular review). Of the 11 cases (22 hips) with bilateral MoM THRs with raised blood metal ion concentrations, 17 hips had normal hip ultrasonography and/or magnetic resonance imaging (under annual clinical follow-up) and 5 hips had periprosthetic fluid collections of variable sizes (under more regular review).
Functional outcome and radiological analysis
Preoperative and postoperative OHS data are summarised in Table 2. There was no statistically significant difference in absolute postoperative scores between the sexes (p=0.608).
Table 2.
Functional and radiological outcomes following 539 non-revised metal-on-metal total hip replacements
| Functional outcome | Median preoperative OHS (IQR) | |
| Overall | 66.7% (54.2–79.2%)
16/48 (10–22) |
|
| Female | 70.8% (58.3–81.3%)
14/48 (9–20) |
|
| Male | 62.5% (50.0–72.9%)
18/48 (13–24) |
|
| Median postoperative OHS (IQR) | ||
| Overall | 6.3% (0–27.1%)
45/48 (35–48) |
|
| Female | 6.8% (0–27.1%)
44.7/48 (35–48) |
|
| Male | 6.3% (0–25.5%)
45/48 (36–48) |
|
| Radiological outcome | Mean acetabular component inclination (range) | 44.0° (21.1–58.3°) |
| Mean femoral stem subsidence (range) | 1mm (0–7mm) | |
| Femoral radiolucent lines (zones 1 and 7) | 19 hips (3.5% of non-revised hips) | |
| Acetabular radiolucent lines (zone 1) | 3 hips (0.6% of non-revised hips) |
OHS = Oxford hip score (provided as a percentage and on a scale of 0–48); IQR = interquartile range
Excluding cases with initial femoral stem subsidence, there were no changes in femoral or acetabular component position in hips not undergoing revision (n=539). All femoral (n=19) and acetabular (n=3) radiolucent lines observed during the follow-up period were non-progressive (Table 2). There were no cases of femoral or acetabular osteolysis.
Discussion
This represents one of the largest single centre studies reporting medium-term outcomes on any modern MoM THR system.11,12,27 Furthermore, we are unaware of any independent reports on outcomes for this particular THR system.
Our findings demonstrated lower than expected implant survival at eight years (88.9%). Although survival was not significantly different between the sexes, it was below that expected in published guidelines.28 The survival curve appears to diverge from these guidelines at the 4-year point (Fig 1), which is most likely due to 13 of 17 ARMD revisions occurring after this time. However, good functional outcomes were reported in non-revised patients, which are comparable with those reported in young patients following hip resurfacing.29–31 ARMD was the most common cause of failure requiring revision surgery with this THR system. In light of recent findings from registry data that confirm stemmed MoM hip replacements have significantly higher revision rates than non-MoM articulations,7,32 we would advise against implantation of all MoM THRs in the future with regular surveillance recommended for patients with these bearings in situ.
Although ARMD was the most common indication for revision, it only accounted for 44% of all revisions performed. More traditional modes of THR failure (eg aseptic loosening, dislocation and deep infection) were responsible for the remaining revisions performed. In contrast, previous studies reporting on MoM THRs observed that ARMD accounted for nearly all the revisions performed (at least 82%).11,12 One potential explanation for this discrepancy relates to implant metallurgy, with studies demonstrating that subtle differences in hip resurfacing design can have a significant impact on failure rates.9,33
Another reason may relate to femoral head size. Recent observations suggest that larger femoral head sizes are associated with increasing failure rates in MoM THRs.7,34 Interestingly, despite also having a MoM articulation, the opposite has been observed in hip resurfacing.20,35 It is likely that a number of factors may contribute to these contrasting failure rates between hip resurfacing and THR such as metallurgy, clearance, lubrication, head–neck ratio and component orientation.5
However, the increasing failure rates with larger femoral head sizes observed in MoM THRs might be due to higher wear at the trunnion–head interface because of increased mechanical stress on the trunnion with larger heads,11,12 failure to achieve optimum lubrication and/or early loosening as a result of increased transmitted torque when using larger femoral heads.7 The femoral head sizes implanted in this cohort (median: 36mm) were smaller than those used in previous studies reporting higher failure rates (range: 38–58mm).11,12 No 28mm femoral head used in the present series has required revision.
The lower failure rates for ARMD observed in this study compared with previous reports11,12 may also be related to cases being performed by surgeons experienced in hip resurfacing.20,31 The mean acetabular component inclination in this series (n=539) was acceptable at 44.0° with 10 of 17 ARMD revisions also having acceptable acetabular component inclination.
It is important that MoM THR patients undergo regular clinical surveillance as they may eventually develop ARMD. In this cohort, 8.7% of non-revised hips had blood metal ion concentrations above MHRA thresholds. The subgroups in which subsequent management remains unclear are patients with: (1) high blood metal ion levels and normal imaging (n=40), and (2) raised metal ion levels (most with bilateral MoM bearings) and periprosthetic fluid collections of variable sizes (n=7). Repeat blood sampling and hip imaging may assist in identifying ARMD.5,15 However, the natural history of ARMD is not well understood.36,37 Decisions relating to revision surgery must therefore be considered on a case-by-case basis. This should include thorough discussion with the patient about the potential risks of further surveillance as well as risks associated with revision surgery.38,39 More detailed investigative and treatment algorithms should be developed for patients with suspected ARMD as new evidence becomes available regarding its natural history.
In addition to the common findings of metallosis and acetabular component malposition, a variety of other intraoperative findings were observed in the 17 ARMD revisions performed. These included effusions of variable sizes and consistencies, granulomas, tissue necrosis and osteolysis. This heterogeneity of findings in hips revised for ARMD was also observed in an earlier report from this centre on hip resurfacings40 as well as by other authors,8,41 and is likely to be related to the complex and incompletely understood pathogenesis of this condition. All revisions for ARMD in the present series underwent bearing exchange to non-MoM articulations with subsequent normal blood metal ion concentrations and no complications reported at short-term follow-up appointments. Nevertheless, given the poor outcomes reported following revision arthroplasty for ARMD,38,39 these patients will continue to undergo regular follow-up reviews.
Study limitations
Our study has some recognised limitations. The follow-up period may be considered relatively short. However, this THR system was only implanted from 2004. It is consequently not possible to determine long-term outcomes at this stage. Other studies reporting on these devices have similar follow-up periods.11,12 In addition, although all patients were reviewed after the institution’s recall, 8% had a follow-up duration of less than three years. This reflects the logistical challenge of reviewing large numbers of patients in clinic with over 4,000 MoM hips implanted at this centre. Understandably, it has taken time to achieve complete follow-up after the recall. As a result, at the time of writing, some patients have not yet had their second clinical review.
It was not possible to accurately measure anteversion of the acetabular component from pelvic radiography. This study also spans a time when subtle nuances of anteversion and combined anteversion were not fully appreciated42 although they may have been responsible for some ARMD failures. During the study, it was not routine practice to perform forensic explant analysis but it is recognised that this would have enabled an assessment of component wear.
Conclusions
Medium-term results of this MoM THR system demonstrated good functional outcomes in non-revised patients with less dramatic failure rates than for similar devices11,12 although survival was still below that recommended in published guidelines.28 Given the growing concerns with stemmed MoM hip replacements (in particular, their higher failure rates compared with non-MoM articulations and with larger femoral head sizes),7,32,34 we recommend against implantation of all MoM THRs in the future. It is advised that patients with surviving MoM THRs are under regular clinical surveillance so that ARMD can be identified and treated early.
Appendix
References
- 1.Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet 2007; 370: 1,508–1,519. [DOI] [PubMed] [Google Scholar]
- 2.Howard JL, Kremers HM, Loechler YA et al. Comparative survival of uncemented acetabular components following primary total hip arthroplasty. J Bone Joint Surg Am 2011; 93: 1,597–1,604. [DOI] [PubMed] [Google Scholar]
- 3.Fisher J, Jin Z, Tipper J et al. Tribology of alternative bearings. Clin Orthop Relat Res 2006; 453: 25–34. [DOI] [PubMed] [Google Scholar]
- 4.Dowson D, Hardaker C, Flett M, Isaac GH. A hip joint simulator study of the performance of metal-on-metal joints: Part II : design. J Arthroplasty 2004; 19: 124–130. [DOI] [PubMed] [Google Scholar]
- 5.Haddad FS, Thakrar RR, Hart AJ et al. Metal-on-metal bearings: the evidence so far. J Bone Joint Surg Br 2011; 93: 572–579. [DOI] [PubMed] [Google Scholar]
- 6.Bozic KJ, Kurtz S, Lau E et al. The epidemiology of bearing surface usage in total hip arthroplasty in the United States. J Bone Joint Surg Am 2009; 91: 1,614–1,620. [DOI] [PubMed] [Google Scholar]
- 7.Smith AJ, Dieppe P, Vernon K et al. Failure rates of stemmed metal-on-metal hip replacements: analysis of data from the National Joint Registry of England and Wales. Lancet 2012; 379: 1,199–1,204. [DOI] [PubMed] [Google Scholar]
- 8.Pandit H, Glyn-Jones S, McLardy-Smith P et al. Pseudotumours associated with metal-on-metal hip resurfacings. J Bone Joint Surg Br 2008; 90: 847–851. [DOI] [PubMed] [Google Scholar]
- 9.Langton DJ, Jameson SS, Joyce TJ et al. Early failure of metal-on-metal bearings in hip resurfacing and large-diameter total hip replacement: a consequence of excess wear. J Bone Joint Surg Br 2010; 92: 38–46. [DOI] [PubMed] [Google Scholar]
- 10.Hart AJ, Satchithananda K, Liddle AD et al. Pseudotumors in association with well-functioning metal-on-metal hip prostheses: a case-control study using three-dimensional computed tomography and magnetic resonance imaging. J Bone Joint Surg Am 2012; 94: 317–325. [DOI] [PubMed] [Google Scholar]
- 11.Bolland BJ, Culliford DJ, Langton DJ et al. High failure rates with a large-diameter hybrid metal-on-metal total hip replacement: clinical, radiological and retrieval analysis. J Bone Joint Surg Br 2011; 93: 608–615. [DOI] [PubMed] [Google Scholar]
- 12.Langton DJ, Jameson SS, Joyce TJ et al. Accelerating failure rate of the ASR total hip replacement. J Bone Joint Surg Br 2011; 93: 1,011–1,016. [DOI] [PubMed] [Google Scholar]
- 13.Australian Orthopaedic Association National Joint Replacement Registry. Annual Report 2012. Adelaide: AOANJRR; 2012. [Google Scholar]
- 14.Medicines and Healthcare products Regulatory Agency. Medical Device Alert. Ref: MDA/2010/069. London: MHRA; 2010. [Google Scholar]
- 15.Medicines and Healthcare products Regulatory Agency. Medical Device Alert. Ref: MDA/2012/036. London: MHRA; 2012. [Google Scholar]
- 16.Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br 1996; 78: 185–190. [PubMed] [Google Scholar]
- 17.Van Der Straeten C, Grammatopoulos G, Gill HS et al. The 2012 Otto Aufranc Award: The interpretation of metal ion levels in unilateral and bilateral hip resurfacing. Clin Orthop Relat Res 2013; 471: 377–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Langton DJ, Jameson SS, Joyce TJ et al. The effect of component size and orientation on the concentrations of metal ions after resurfacing arthroplasty of the hip. J Bone Joint Surg Br 2008; 90: 1,143–1,151. [DOI] [PubMed] [Google Scholar]
- 19.Pynsent PB, Adams DJ, Disney SP. The Oxford hip and knee outcome questionnaires for arthroplasty. J Bone Joint Surg Br 2005; 87: 241–248. [DOI] [PubMed] [Google Scholar]
- 20.McBryde CW, Theivendran K, Thomas AM et al. The influence of head size and sex on the outcome of Birmingham hip resurfacing. J Bone Joint Surg Am 2010; 92: 105–112. [DOI] [PubMed] [Google Scholar]
- 21.Murray DW, Fitzpatrick R, Rogers K et al. The use of the Oxford hip and knee scores. J Bone Joint Surg Br 2007; 89: 1,010–1,014. [DOI] [PubMed] [Google Scholar]
- 22.Gruen TA, McNeice GM, Amstutz HC. ‘Modes of failure’ of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res 1979; 141: 17–27. [PubMed] [Google Scholar]
- 23.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res 1976; 121: 20–32. [PubMed] [Google Scholar]
- 24.Hing CB, Young DA, Dalziel RE et al. Narrowing of the neck in resurfacing arthroplasty of the hip. J Bone Joint Surg Br 2007; 89: 1,019–1,024. [DOI] [PubMed] [Google Scholar]
- 25.Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res 1990; 257: 107–128. [PubMed] [Google Scholar]
- 26.Cox DR. Regression models and life-tables. J R Stat Soc Series B 1972; 34: 187–220. [Google Scholar]
- 27.Kindsfater KA, Sychterz Terefenko CJ, Gruen TA , Sherman CM. Minimum 5-year results of modular metal-on-metal total hip arthroplasty. J Arthroplasty 2012; 27: 545–550. [DOI] [PubMed] [Google Scholar]
- 28.National Institute for Clinical Excellence. Guidance on the Selection of Prostheses for Primary Total Hip Replacement. London: NICE; 2000. [Google Scholar]
- 29.Coulter G, Young DA, Dalziel RE, Shimmin AJ. Birmingham hip resurfacing at a mean of ten years: results from an independent centre. J Bone Joint Surg Br 2012; 94: 315–321. [DOI] [PubMed] [Google Scholar]
- 30.Murray DW, Grammatopoulos G, Pandit H et al. The ten-year survival of the Birmingham hip resurfacing: an independent series. J Bone Joint Surg Br 2012; 94: 1,180–1,186. [DOI] [PubMed] [Google Scholar]
- 31.Matharu GS, McBryde CW, Pynsent WB et al. The outcome of the Birmingham Hip Resurfacing in patients aged < 50 years up to 14 years post-operatively. Bone Joint J 2013; 95: 1,172–1,177. [DOI] [PubMed] [Google Scholar]
- 32.Jameson SS, Baker PN, Mason J et al. Independent predictors of failure up to 7.5 years after 35 386 single-brand cementless total hip replacements: a retrospective cohort study using National Joint Registry data. Bone Joint J 2013; 95: 747–757. [DOI] [PubMed] [Google Scholar]
- 33.Langton DJ, Joyce TJ, Jameson SS et al. Adverse reaction to metal debris following hip resurfacing: the influence of component type, orientation and volumetric wear. J Bone Joint Surg Br 2011; 93: 164–171. [DOI] [PubMed] [Google Scholar]
- 34.Langton DJ, Sidaginamale R, Lord JK et al. Taper junction failure in large-diameter metal-on-metal bearings. Bone Joint Res 2012; 1: 56–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Glyn-Jones S, Pandit H, Kwon YM et al. Risk factors for inflammatory pseudotumour formation following hip resurfacing. J Bone Joint Surg Br 2009; 91: 1,566–1,574. [DOI] [PubMed] [Google Scholar]
- 36.Ebreo D, Bell PJ, Arshad H et al. Serial magnetic resonance imaging of metal-on-metal total hip replacements. Follow-up of a cohort of 28 mm Ultima TPS THRs. Bone Joint J 2013; 95: 1,035–1,039. [DOI] [PubMed] [Google Scholar]
- 37.Almousa SA, Greidanus NV, Masri BA et al. The natural history of inflammatory pseudotumors in asymptomatic patients after metal-on-metal hip arthroplasty. Clin Orthop Relat Res 2013; 471: 3,814–3,821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grammatopoulos G, Pandit H, Kwon YM et al. Hip resurfacings revised for inflammatory pseudotumour have a poor outcome. J Bone Joint Surg Br 2009; 91: 1,019–1,024. [DOI] [PubMed] [Google Scholar]
- 39.Munro JT, Masri BA, Duncan CP, Garbuz DS. High complication rate after revision of large-head metal-on-metal total hip arthroplasty. Clin Orthop Relat Res 2014; 472: 523–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Matharu GS, Revell MP, Pynsent PB, Treacy RB. A review of hip resurfacings revised for unexplained pain. Hip Int 2012; 22: 633–640. [DOI] [PubMed] [Google Scholar]
- 41.Campbell P, Ebramzadeh E, Nelson S et al. Histological features of pseudotumor-like tissues from metal-on-metal hips. Clin Orthop Relat Res 2010; 468: 2,321–2,327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McMinn DJ, Snell KI, Daniel J et al. Mortality and implant revision rates of hip arthroplasty in patients with osteoarthritis: registry based cohort study. BMJ 2012; 344: e3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


