Abstract
Introduction
There remains a lack of high quality randomised trial evidence for the use of adjuvant chemotherapy in stage II rectal cancer, particularly in the presence of high risk features such as extramural venous invasion (EMVI). The aim of this study was to explore this issue through a survey of colorectal surgeons and gastrointestinal oncologists.
Methods
An electronic survey was sent to a group of colorectal surgeons who were members of the Association of Coloproctology of Great Britain and Ireland. The survey was also sent to a group of gastrointestinal oncologists through the Pelican Cancer Foundation. Reminder emails were sent at 4 and 12 weeks.
Results
A total of 142 surgeons (54% response rate) and 99 oncologists (68% response rate) responded to the survey. The majority in both groups of clinicians thought EMVI was an important consideration in adjuvant treatment decision making and commented routinely on this in their multidisciplinary team meeting. Although both would consider treating patients on the basis of EMVI detected by magnetic resonance imaging, oncologists were more selective. Both surgeons and oncologists were prepared to offer patients with EMVI adjuvant chemotherapy but there was lack of consensus on the benefit.
Conclusions
This survey reinforces the evolution in thinking with regard to adjuvant therapy in stage II disease. Factors such as EMVI should be given due consideration and the prognostic information we offer patients must be more accurate. Historical data may not accurately reflect today’s practice and it may be time to consider an appropriately designed trial to address this contentious issue.
Keywords: Rectal cancer, Extramural venous invasion, Adjuvant chemotherapy
Adjuvant chemotherapy improves survival outcomes in patients with stage III rectal cancer.1–5 Nodal disease, which distinguishes stage II from stage III disease, is known to be associated with worse survival outcomes, disease recurrence and is an independent marker of poor prognosis.6–10 Nevertheless, the survival benefit following adjuvant chemotherapy for patients with stage II disease is not so clear, and much of the current advice given to patients is based on a combination of historical trial evidence and personal opinion of the treating clinician.
Extramural venous invasion (EMVI) is a known independent tumour factor associated with disease recurrence and metastases.11–13 Despite this, it has not been considered as a risk factor for routine adjuvant chemotherapy. This may be explained partly by the inconsistent definitions of the past, and the variability in pathological detection and techniques.14 However, more recently, magnetic resonance imaging (MRI) has been shown to accurately identify EMVI (mrEMVI), which correlates highly with EMVI detected by pathology.15 It is now recognised as part of the minimum data reporting set for (colo)rectal cancer.16
The current use of adjuvant chemotherapy in stage II rectal cancer varies widely.5 There is no robust randomised trial evidence with regard to novel prognostic factors such as EMVI and outcomes in stage II rectal cancer. It is therefore not surprising that there is such variability in practice. The aim of this study was to explore the variability between clinicians in treating patients with EMVI positive, stage II rectal cancer.
Methods
An electronic questionnaire was sent to a group of colorectal surgeons and oncologists. The cohort of surgeons comprised a limited membership of the Association of Coloproctology of Great Britain and Ireland who had given their consent previously to participate in such surveys. Their primary practice consisted of university and district general hospitals. Overall, 263 consultant surgeons were sent the questionnaire along with a covering letter explaining the aims of the survey and how these results may help in designing future studies. The same survey and letter were also sent electronically to 146 oncologists through the Pelican Cancer Foundation database, a national database of oncologists with a diverse practice of university and district general hospitals. Two reminder emails were sent at four and twelve weeks.
The survey featured nine questions including four specifically on clinical scenarios and treatment efficacy (Fig 1). Participants were asked to comment on the importance and detection of EMVI in their respective multidisciplinary team (MDT) meetings, their personal approach to patients with EMVI and the clinical scenarios. Responses were recorded for surgeons and oncologists as absolute numbers and percentages. These were compared using Fischer’s exact test and the chi-squared test where appropriate.
Figure 1.
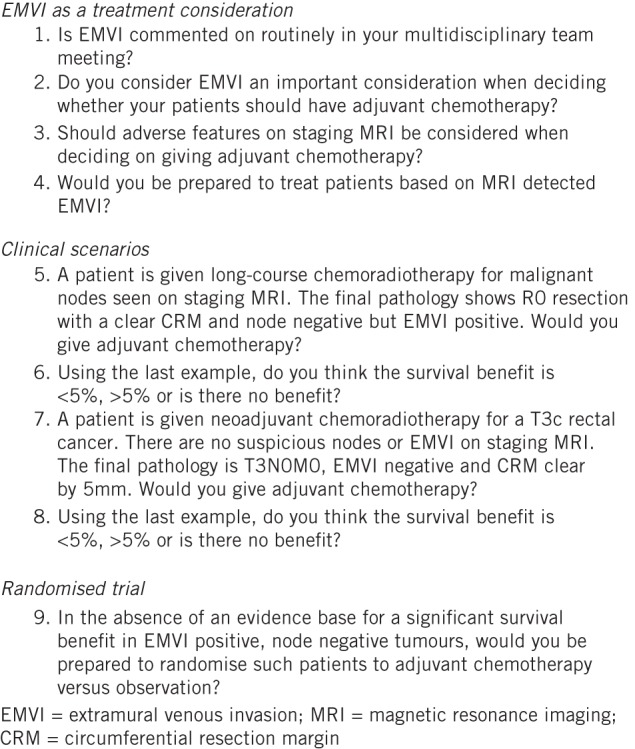
Summary of survey questions
Results
Of the 263 surgeons who were sent the electronic questionnaire, 142 (54%) responded. This compared with 99 (68%) out of the 146 oncologists who were also sent the survey. Less than 2% in each group did not answer all the questions on the survey.
EMVI as a treatment consideration
A summary of the responses by surgeons and oncologists to the questions on extramural venous invasion as a treatment consideration is given in Table 1. EMVI was commented on in the MDT meetings of almost all respondents either by pathology or radiology. Over two-thirds (69%) of surgeons would always consider EMVI when deciding on treatment options whereas 30% would only do so in selected patients. (Not all respondents answered this question.) There was a significant difference in the responses between surgeons and oncologists with surgeons being more likely to react to the presence of EMVI than oncologists: 68% of surgeons were in favour of treating EMVI vs 53% of oncologists (p<0.015).
Table 1.
Comparison of responses by surgeons and oncologists to questions on extramural venous invasion as a treatment consideration
| Response | Surgeons | Oncologists | p-value | |
| Q1 | Yes – pathology only
Yes – radiology only Yes – both No |
28 (19.7%)
0 (0%) 114 (80.3%) 0 (0%) |
19 (19.2%)
2 (2.0%) 76 (76.8%) 2 (2.0%) |
0.633 |
| Q2 | Yes
No In selected patients |
97 (68.3%)
2 (1.4%) 43 (30.3%) |
52 (52.5%)
0 (0%) 47 (47.5)% |
0.015 |
| Q3 | Yes
No |
120 (84.5%)
22 (15.5%) |
76 (76.8%)
23 (23.2%) |
0.135 |
| Q4 | Yes
No Maybe |
51 (35.9%)
13 (9.2%) 78 (54.9%) |
14 (14.1%)
29 (29.3%) 56 (56.6%) |
<0.001 |
| Q9 | Yes
No Only in patients aged >70 |
110 (77.5%)
24 (16.9%) 8 (5.6%) |
67 (67.7%)
14 (14.1%) 18 (18.2%) |
0.010 |
The majority of surgeons and oncologists (85% and 77% respectively) believed MRI features to be an important consideration when deciding on treatment. When asked whether they would use mrEMVI alone in treatment decision making, 36% of surgeons said they would and 55% would consider it in selected cases while 10% would not rely on mrEMVI alone. Only 14% of the oncologists were prepared to treat patients on the basis of mrEMVI, with a further 57% prepared to do this in selected circumstances. Almost a third (29%) would not treat patients on the basis of mrEMVI alone. This was a significant difference (p<0.001).
Clinical scenarios
A summary of the responses by surgeons and oncologists to the clinical scenario questions is given in Table 2. The majority of surgeons and oncologists (71% and 69% respectively) were prepared to treat the patient in the first scenario (question 5 in Fig 1) with adjuvant chemotherapy. Only 13% of surgeons and 12% of oncologists thought there was no survival benefit.
In the second scenario (question 7 in Fig 1), 89% of surgeons would not offer adjuvant chemotherapy to the patient described. Fifty per cent thought there was some benefit (albeit <5%) while forty-seven per cent thought there was no benefit whatsoever. There was a difference in the surgeons’ responses to the use of adjuvant chemotherapy compared with the oncologists, who were more likely to offer adjuvant treatment in this case than the surgeons (p<0.045). For a patient with stage II disease and no adverse features, 21% of oncologists would still offer adjuvant therapy but the majority thought there was either less than 5% benefit (54%) or no benefit at all (42%).
Randomised trial: chemotherapy versus observation
Over three-quarters (78%) of surgeons would support their patients being involved in such a trial and a further 6% would support this in patients over 70 years old (Table 1). However, 17% would not be prepared to take part in such a trial. Interestingly, 68% of the oncologists would consider a randomised trial for stage II patients with EMVI and only 14% would not. Eighteen per cent would be prepared to involve patients who were over seventy years of age in the trial.
Discussion
The results of the survey show that EMVI is recognised by both surgeons and oncologists as a prognostic factor, and discussed in almost all MDT meetings. Furthermore, whether it was detected on pathology and/or radiology, it is a consideration in treatment decisions. Nevertheless, oncologists seemed to be more selective in their approach to EMVI. Although this survey did not explore the relative importance of EMVI compared with other prognostic factors, it is notable that it is considered in overall management strategy. A further point highlighted is that most clinicians are now prepared to treat patients on the basis of MRI findings preoperatively. This signals a significant shift in attitude towards risk stratification in the last decade as MRI can now be used confidently to be more selective in terms of which patients should be offered preoperative treatment.
MRI plays a central role in the local staging and risk stratification of patients with rectal cancer in the UK and Europe. Important prognostic factors such as circumferential resection margin involvement and extent of tumour spread into the mesorectum (T3 substaging), which influence treatment decisions, are readily identifiable on MRI.17,18 The standard of care for locally advanced high risk rectal cancer without metastatic disease is preoperative chemoradiation.19 Along with refinement of surgical technique, this has led to significant improvements in local recurrence rates and overall survival.20 Although there has been some debate surrounding the benefit of adjuvant chemotherapy in patients who have already undergone neoadjuvant chemoradiation,21,22 it still forms the mainstay of treatment for systemic disease and the risk of metastases.
The QUASAR trial is the most frequently quoted with regard to adjuvant chemotherapy decisions for stage II tumours and the perceived survival benefit for patients is approximately 3.6%.23 However, the National Surgical Adjuvant Breast and Bowel Project R-01 trial showed a survival benefit in terms of overall survival and disease free survival for patients randomised to chemotherapy over observation or radiation.1 Histopathological staging remains the basis for decision making and it is important that stage II tumours, which may benefit from adjuvant therapy, are identified through high quality pathology reporting.22 The emphasis is very much on the pathologist examining the specimen diligently with appropriate sections to reveal as much information as possible. Quirke et al have reported extensively on the importance of this.24–26
EMVI is arguably the most debated of these additional risk factors in deciding on oncological treatment. There is little doubt that venous invasion has a prognostic influence but lack of consistent reporting in both pathology and radiology has made it difficult for clinicians to understand its exact clinical relevance. This lack of confidence in accurate detection of EMVI may be one of the reasons why it is not considered as a mandatory treatment factor. Nevertheless, a study by Chand et al from 2013 has demonstrated the importance of mrEMVI as a potential prognostic (and predictive) imaging biomarker in rectal cancer,27 giving further support to MRI detected tumour characteristics being used for treatment decisions. Furthermore, the importance of EMVI in stage II disease has now been shown on multivariate analysis as a prognostic marker of disease recurrence.28
In the present study, surgeons were more likely to rely on MRI than oncologists for decision making (85% vs 77%) and, specific to EMVI, oncologists were less likely to base treatment on mrEMVI. Despite this, the responses to the clinical scenarios of offering adjuvant chemotherapy to a patient with stage II rectal cancer with evidence of EMVI but no other adverse features and to a patient with no adverse features whatsoever were similar (71% surgeons vs 69% oncologists).
However, while the surgeons were divided equally as to whether the perceived survival benefit was >5% or <5%, 55% of the oncologists thought the benefit was <5% and 33% thought it was >5%. The interesting point is that the QUASAR trial shows that the benefit for patients in receiving adjuvant chemotherapy is 3.6%23 but more than a third of surgeons and oncologists believe the benefit to be >5%. In the second scenario, where there were no adverse features in stage II disease, the surgeons were less likely to offer adjuvant chemotherapy (11%) (a proportion that is consistent with the current literature) than the oncologists (22%), who would offer adjuvant treatment with no obvious evidence base.
One of the limitations of this survey is that there were no detailed explanations from the respondents regarding reasons for decision making. As the results include a degree of subjectivity and are not based entirely on trial evidence, it would have been interesting to understand the rationale behind some of the decisions. It should also be noted that this questionnaire was sent predominantly to UK-based clinicians. The importance and understanding of EMVI as a prognostic factor is more apparent in the UK than in other countries such as the US. Furthermore, the central role of MRI and using it to guide treatment through risk stratification is also more common in the UK, where a more selective approach is taken in the use of preoperative therapy.
Conclusions
This survey reinforces the evolution in thinking with regard to adjuvant therapy in stage II disease. Factors such as EMVI should be given due consideration and the information we offer patients must be more accurate. We cannot continue to rely on historical studies, which may, by no fault of design, have missed the importance of surgical technique and the emergence of novel prognostic factors, which do not rely solely on pathology for identification. There appears to be an acknowledged need for a randomised controlled trial investigating EMVI although it will be important to select the inclusion criteria and trial design carefully. Moreover, the effect of adjuvant chemotherapy in patients who have undergone preoperative chemoradiation and have also been downstaged must be accounted for in any future trial design.
Acknowledgements
We are grateful to Anne O’Mara (Association of Coloproctology of Great Britain and Ireland) and Sarah Crane (Pelican Cancer Foundation) for help with this study.
Funding for this study was provided by the National Institute for Health Research Biomedical Research Centre at The Royal Marsden, Sutton.
References
- 1.Wolmark N. Adjuvant therapy for colorectal cancer: the NSABP clinical trials. Adv Exp Med Biol 1988; 244: 261–266. [DOI] [PubMed] [Google Scholar]
- 2.Fisher B, Wolmark N, Rockette H et al. Postoperative adjuvant chemotherapy or radiation therapy for rectal cancer: results from NSABP protocol R-01. J Natl Cancer Inst 1988; 80: 21–29. [DOI] [PubMed] [Google Scholar]
- 3.Radiation therapy and fluorouracil with or without semustine for the treatment of patients with surgical adjuvant adenocarcinoma of the rectum. J Clin Oncol 1992; 10: 549–557. [DOI] [PubMed] [Google Scholar]
- 4.Wu X, Zhang J, He X et al. Postoperative adjuvant chemotherapy for stage II colorectal cancer: a systematic review of 12 randomized controlled trials. J Gastrointest Surg 2012; 16: 646–655. [DOI] [PubMed] [Google Scholar]
- 5.Petersen SH, Harling H, Kirkeby LT et al. Postoperative adjuvant chemotherapy in rectal cancer operated for cure. Cochrane Database Syst Rev 2012; 3: CD004078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grinnell RS. The lymphatic and venous spread of carcinoma of the rectum. Ann Surg 1942; 116: 200–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grinnell RS. The spread of carcinoma of the colon and rectum. Cancer 1950; 3: 641–652. [DOI] [PubMed] [Google Scholar]
- 8.Dukes CE, Bussey HJ. The spread of rectal cancer and its effect on prognosis. Br J Cancer 1958; 12: 309–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gilbertsen VA. Adenocarcinoma of the rectum. Ann Surg 1960; 151: 340–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moossa AR, Ree PC, Marks JE et al. Factors influencing local recurrence after abdominoperineal resection for cancer of the rectum and rectosigmoid. Br J Surg 1975; 62: 727–730. [DOI] [PubMed] [Google Scholar]
- 11.Talbot IC, Ritchie S, Leighton MH et al. The clinical significance of invasion of veins by rectal cancer. Br J Surg 1980; 67: 439–442. [DOI] [PubMed] [Google Scholar]
- 12.Knudsen JB, Nilsson T, Sprechler M et al. Venous and nerve invasion as prognostic factors in postoperative survival of patients with resectable cancer of the rectum. Dis Colon Rectum 1983; 26: 613–617. [DOI] [PubMed] [Google Scholar]
- 13.Freedman LS, Macaskill P, Smith AN. Multivariate analysis of prognostic factors for operable rectal cancer. Lancet 1984; 2: 733–736. [DOI] [PubMed] [Google Scholar]
- 14.Messenger DE, Driman DK, Kirsch R. Developments in the assessment of venous invasion in colorectal cancer: implications for future practice and patient outcome. Hum Pathol 2012; 43: 965–973. [DOI] [PubMed] [Google Scholar]
- 15.Smith NJ, Barbachano Y, Norman AR et al. Prognostic significance of magnetic resonance imaging-detected extramural vascular invasion in rectal cancer. Br J Surg 2008; 95: 229–236. [DOI] [PubMed] [Google Scholar]
- 16.Royal College of Pathologists. Dataset for Colorectal Cancer (2nd Edition). London: RCPath; 2007. p26. [Google Scholar]
- 17.Taylor FG, Quirke P, Heald RJ et al. Preoperative high-resolution magnetic resonance imaging can identify good prognosis stage I, II, and III rectal cancer best managed by surgery alone: a prospective, multicenter, European study. Ann Surg 2011; 253: 711–719. [DOI] [PubMed] [Google Scholar]
- 18.Shihab OC, Taylor F, Salerno G et al. MRI predictive factors for long-term outcomes of low rectal tumours. Ann Surg Oncol 2011; 18: 3,278–3,284. [DOI] [PubMed] [Google Scholar]
- 19.Sauer R, Becker H, Hohenberger W et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med 2004; 351: 1,731–1,740. [DOI] [PubMed] [Google Scholar]
- 20.van Gijn W, Marijnen CA, Nagtegaal ID et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12-year follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol 2011; 12: 575–582. [DOI] [PubMed] [Google Scholar]
- 21.O’Connell MJ, Martenson JA, Wieand HS et al. Improving adjuvant therapy for rectal cancer by combining protracted-infusion fluorouracil with radiation therapy after curative surgery. N Engl J Med 1994; 331: 502–507. [DOI] [PubMed] [Google Scholar]
- 22.Bujko K, Glynne-Jones R, Bujko M. Does adjuvant fluoropyrimidine-based chemotherapy provide a benefit for patients with resected rectal cancer who have already received neoadjuvant radiochemotherapy? A systematic review of randomised trials. Ann Oncol 2010; 21: 1,743–1,750. [DOI] [PubMed] [Google Scholar]
- 23.Gray R, Barnwell J, McConkey C et al. Adjuvant chemotherapy versus observation in patients with colorectal cancer: a randomised study. Lancet 2007; 370: 2,020–2,029. [DOI] [PubMed] [Google Scholar]
- 24.Quirke P, Morris E. Reporting colorectal cancer. Histopathology 2007; 50: 103–112. [DOI] [PubMed] [Google Scholar]
- 25.Maughan NJ, Morris E, Forman D, Quirke P. The validity of the Royal College of Pathologists’ colorectal cancer minimum dataset within a population. Br J Cancer 2007; 97: 1,393–1,398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Morris EJ, Maughan NJ, Forman D, Quirke P. Identifying stage III colorectal cancer patients: the influence of the patient, surgeon, and pathologist. J Clin Oncol 2007; 25: 2,573–2,579. [DOI] [PubMed] [Google Scholar]
- 27.Chand M, Swift RI, Tekkis PP et al. Extramural venous invasion is a potential imaging predictive biomarker of neoadjuvant treatment in rectal cancer. Br J Cancer 2014; 110 (1): 19–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chand M, Bhangu A, Wotherspoon A et al. EMVI-positive stage II rectal cancer has similar clinical outcomes as stage III disease following pre-operative chemoradiotherapy. Ann Oncol 2014; 25 (4): 858–863. [DOI] [PubMed] [Google Scholar]


