Abstract
Although basal cell carcinoma is a very common malignancy, metastasis from this tumour is extremely rare. For this reason, many plastic surgeons, dermatologists and physicians dealing with skin malignancies consider this as a locally invasive malignancy. We present a rare case of metastatic basal cell carcinoma manifested as a bronchial tumour. This case highlights the fact that despite basal cell carcinoma’s local invasive potential, the possibility of distant metastasis still exists and clinicians should therefore be cautious about interpreting extracutaneous symptoms. Chest physicians should always consider the possibility of this rare tumour in the lungs in patients with a history of large basal cell carcinomas in the head and neck region.
Keywords: Basal cell carcinoma, Metastasis, Bronchial
Basal cell carcinoma (BCC) is the most common skin malignancy in the UK.1 It accounts for 10–15% of carcinomas in women and 20% in men. The majority (80–85%) of BCCs occur in the head and neck area.2 Despite its high incidence, metastasis is uncommon with a reported frequency of 0.0028–0.5% of cases.3 We report a case scalp BCC with metastasis to the right main bronchus.
Case history
A 67-year-old man presented with a non-healing BCC on his scalp. He had had radiotherapy for treatment of tinea capitis on his skull as a child. As a result, he had had several excisions for multiple recurring scalp BCCs over a period of 15 years.
As the patient had an unstable scalp, he underwent extensive excision of scalp skin and resurfacing of part of the scalp with an anterolateral thigh (ALT) flap. His postoperative recovery was complicated by a pulmonary embolus, which was diagnosed with ventilation-perfusion lung imaging.
Two years later, the patient had a tissue expander inserted under the ALT flap to provide tissue for further excision and resurfacing of the rest of his scalp. A few months later, he developed breathing problems in the form of dry coughs and right lower chest pain. He also had 17kg of weight loss.
A chest x-ray showed a deviated trachea to the right and widened mediastinum as well as minor right middle zone opacity. Computed tomography showed a mass on the right main bronchus less than 10mm from the carina with significant narrowing (Fig 1).
Figure 1.
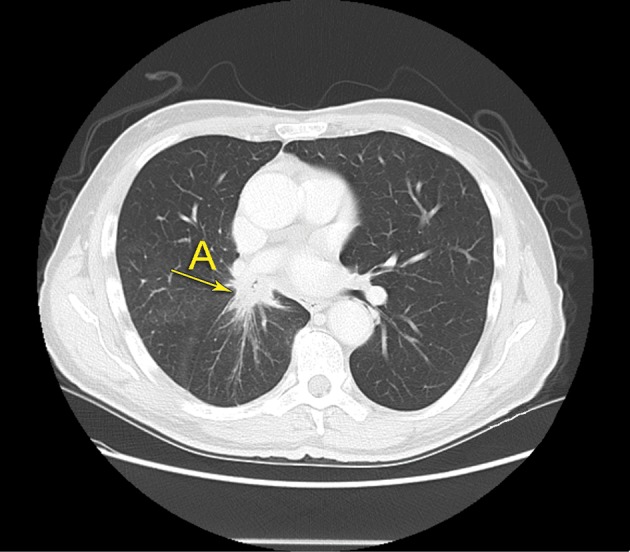
Spiculated soft tissue mass with strands of tissue (A) extending into the adjacent lung parenchyma, which is a feature of metastatic carcinoma
A bronchoscopy confirmed obstruction of the right main bronchus by infiltrated irregular mucosa with necrosis. Bronchial biopsy showed a non-small cell carcinoma with basaloid features. Immunohistochemical staining for keratins 5/6 and anion exchange proteins 1/3 showed a positive staining pattern of the tumour cells and a negative staining pattern for thyroid transcription factor-1, consistent with a diagnosis of a metastatic BCC (Fig 2).
Figure 2.
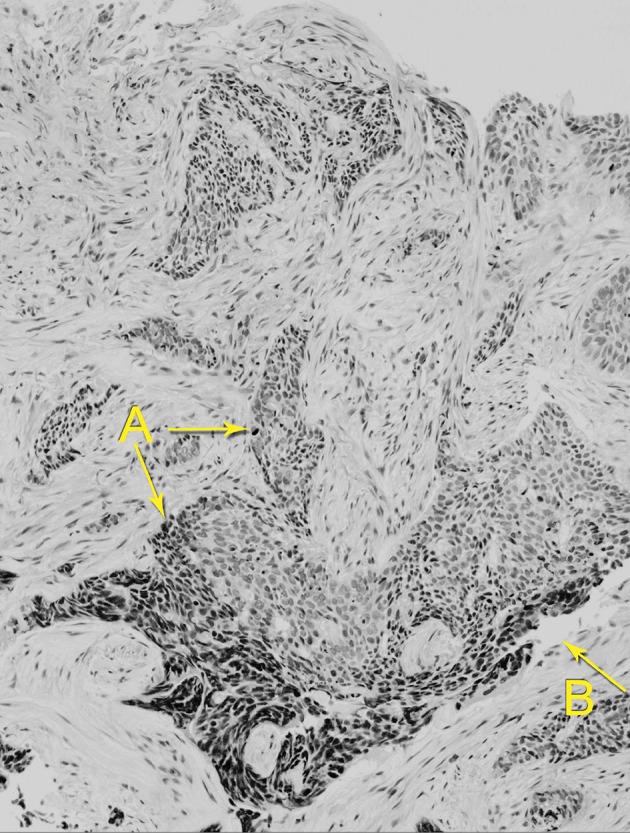
Nests of malignant cells surrounded by loose stroma (A) and cleft-like retraction spaces between nests of cells and surrounding stroma (B)
The patient had another bronchoscopy and a stent was inserted in the right main bronchus. He underwent radical radiotherapy. He was not considered suitable for any further treatment for scalp BCCs and the tissue expander was removed. He subsequently had stenting of his right main bronchus and is stable at the moment.
Discussion
BCC is the most common of all skin malignancies, accounting for 65–75% of all skin cancers.4 BCCs are usually slow growing and rarely metastasise.3 Risk factors for metastasis in BCCs include a history of irradiation,5 large and deeply invasive tumours, perineural invasion and multiple local recurrences.3 A localised metastasis is treated with surgery but the widespread disease is treated by radiotherapy and/or chemotherapy. The results of these treatments are not very promising, with an estimated median survival after metastasis ranging from 8 to 14 months. The longest known survival is 25 years.6
Conclusions
As plastic surgeons dealing with BCCs and skin malignancies, we should be cautious about patients with BCCs and risk factors for metastasis, and we should investigate any extracutaneous complaint promptly.
References
- 1.Brewster DH, Bhatti LA, Inglis JH et al. Recent trends in incidence of nonmelanoma skin cancers in the East of Scotland, 1992–2003. Br J Dermatol 2007; 156: 1,295–1,300. [DOI] [PubMed] [Google Scholar]
- 2.Lorenzini M, Gatti S, Giannitrapani A. Giant basal cell carcinoma of the thoracic wall: a case report and review of the literature. Br J Plast Surg 2005; 58: 1,007–1,010. [DOI] [PubMed] [Google Scholar]
- 3.von Domarus H, Stevens PJ. Metastatic basal cell carcinoma. Report of five cases and review of 170 cases in the literature. J Am Acad Dermatol 1984; 10: 1,043–1,060. [DOI] [PubMed] [Google Scholar]
- 4.Barksdale SK, O’Connor N, Barnhill R. Prognostic factors for cutaneous squamous cell and basal cell carcinoma. Determinants of risk of recurrence, metastasis, and development of subsequent skin cancers. Surg Oncol Clin N Am 1997; 6: 625–638. [PubMed] [Google Scholar]
- 5.Spoor HJ, Lindo SD, Erlandson RA. Skin cancer: comparison of aggressive potentials of sunlight-induced and x-ray-induced tumors. Cutis 1977; 20: 74–80. [PubMed] [Google Scholar]
- 6.Lo JS, Snow SN, Reizner GT et al. Metastatic basal cell carcinoma: report of twelve cases with a review of the literature. J Am Acad Dermatol 1991; 24: 715–719. [DOI] [PubMed] [Google Scholar]


