Abstract
Benign cardiac tumours are rare and cardiac lipomas account only for a small fraction among those. Most of these tumours differ in terms of clinical manifestation, diagnosis, morphology and size, and are therefore not diagnosed easily unless they become symptomatic. We report the case of a 71-year-old Caucasian woman with recurrent episodes of shortness of breath presenting with an acute exacerbation of dyspnoea and hypertensive crisis. Diagnosis of a right atrial lipoma with a coexisting patent foramen ovale was established on echocardiography and computed tomography, and the patient was evaluated for elective surgery. Comprising the entire free wall of the right atrium, the tumour was removed during open heart surgery on cardiopulmonary bypass. The right atrium and the orifices of both the superior and inferior vena cava were reconstructed with bovine pericardium. No evidence of tumour relapse was observed during successive follow-up visits.
Keywords: Rare cardiac tumour, Right atrial lipoma, Obstructive atrial lipoma
Benign cardiac tumours are rare and lipomas represent only a minor percentage among those.1 The incidence of primary tumours of the heart and pericardium ranges from 0.002% to 0.28%, according to a series of postmortem examinations reported by McAllister et al.1,2 Approximately 75% of cardiac tumours are benign, myxomas being the most common in adults, followed by lipomas, fibromas and teratomas, with the left atrium being the most common location.3 Rhabdomyomas represent the most frequent primary cardiac tumours in infancy and are associated with phakomatoses such as tuberous sclerosis.4 However, metastases spreading from malignant melanomas and lymphomas are the most common aetiology of heart tumours.
Cardiac lipomas account for 8.4% of primary tumours of the heart and pericardium.1,2 According to the literature, 25% of cardiac lipomas are intramyocardial, 25% are extracavitary of epicardial origin and 50% are intracavitary of subendocardial origin; those of the right atrium are extremely rare.5,6
Case history
A 71-year-old Caucasian woman presented to the emergency department with acute exacerbation of a 2-year history of recurrent dyspnoea and a new onset manifestation of hypertensive crisis. She did not complain of angina. Her past medical history included essential hypertension, dyslipidaemia, diabetes mellitus type 2 and obesity. Her past surgical history was significant for strumectomy in 1991 and tonsillectomy in early childhood. On physical examination, Kussmaul’s sign was detectable on inspiration, suggestive of an increased jugular venous pressure. Laboratory analysis and tumour biomarkers were within normal ranges except for an elevated D-dimer. Chest x-rays revealed no signs of cardiomegaly or pulmonary oedema. The electrocardiography showed a sinus rhythm with premature atrial complexes and T wave abnormalities from lead V4 to lead V6.
Transoesophageal echocardiography revealed a large 5.5cm mass located in the right atrium extending along the free right atrial wall, severely impairing blood flow from the superior vena cava into and through the right atrium. Both the left and right atria were moderately enlarged. The left ventricle showed moderate concentric hypertrophy with a preserved ejection fraction. There was a grade I/IV tricuspid insufficiency with a maximal pulmonary arterial pressure of 43mmHg.
With the elevated D-dimer in mind, spiral computed tomography (CT) was initiated to exclude pulmonary embolism. The diagnosis of a 5.5cm right atrial mass was confirmed, suspicious of cardiac myxoma (Fig 1). The percutaneous coronary angiography showed a right dominant system and a non-significant stenosis in the proximal right coronary artery (<30%). The left main stem, left coronary artery and circumflex artery appeared unremarkable. Additionally performed duplex ultrasonography of the large neck vessels revealed bilateral stenotic disease of the carotid arteries (50%).
Figure 1.

Preoperative computed tomography of the chest showing a large right atrial mass severely obstructing the right atrium down to 0.7cm. The mass showed a homogenous fat density. No direct signs of ventricular or mediastinal infiltration were detectable. There was no evidence of pulmonary embolism.
Upon evaluation for elective cardiac intervention, the patient underwent open heart surgery. After a median sternotomy, the ascending aorta and both the superior and inferior vena cava were used as cannulation sites. The aorta was cross-clamped and cardiopulmonary bypass was initiated. Antegrade cardioplegia and mild hypothermia (32°C) were used during bypass. The tumour was palpated (Fig 2A) and the right atrium incised. A large, well circumscribed mass was visible, stretching down from the superior vena cava comprising the entire free right atrial wall all the way to the orifice of the inferior vena cava. Macroscopically, the mass appeared to be of lipomatous composition (Fig 2B). Frozen section diagnosis confirmed a true atrial lipoma.
Figure 2.
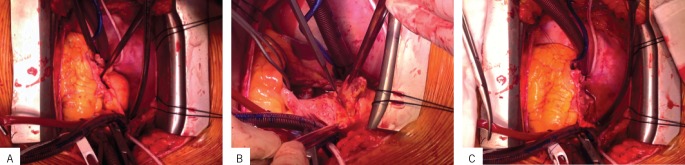
Median sternotomy and initiation of cardiopulmonary bypass: Tumour visible as a bulging protrusion of the free right atrial wall (A). Aortic cross-clamp and antegrade cardioplegia visible at the bottom. The lipomatous mass was excised completely (B). The orifices of both caval veins were detached fully for excision with surrounding healthy tissue. When the tumour was resected, almost the whole of the right atrium was removed (C).
In order to allow for comprehensive excision of the mass, the caval veins were partially detached from their atrial origins (Fig 2B), and both free atrial wall and tumour were removed en bloc (Fig 2C). A patent foramen ovale became apparent and was closed subsequently. The caval veins were reconstructed using 5/0 polypropylene sutures and bovine pericardium. The atrium was newly formed with a bovine pericardial patch and the patient weaned from cardiopulmonary bypass.
The postoperative period was significant for pacemaker dependency, requiring the implantation of a permanent dual chamber pacemaker. The patient was discharged from hospital in good condition.
Discussion
In the scientific literature, cardiac lipomas are referred to as infrequently occurring neoplasias, accounting for 8.4% of primary cardiac tumours1,2 with those located in the right atrium being extremely rare. According to their histological composition, lipomas are divided into two groups: lipomatous hypertrophy and true lipomas. When infiltrating the myocardium, the tumour is called a myolipoma. If fibroblasts are present, the tumour is called a fibrolipoma and if the tumour consists solely of lipocytes, it is a lipoma. The tumour does have congenital origins belonging to the group of homeoplastic dysembryomas.7 The tumour described in the current case was classified as a true lipoma.
The diagnosis of this tumoral entity is difficult to establish owing to its variable manifestation, depending on size and localisation. Consequently, as with other cardiac tumours, its diagnosis is often accidental and almost exclusively on postmortem findings.2 Lipomas may be detected on chest x-rays, echocardiography or thoracic CT and magnetic resonance imaging studies. Especially the latter two are of utmost importance in providing information regarding size, location and nature of the mass. Cardiac tumours become equally symptomatic and potentially dangerous if compressing the heart from the outside when in a pericardial location, interfering with the electrical conduction system when infiltrating certain myocardial structures or impairing blood flow and valvular function as intracavitary masses. Whenever the tumour has an intracavitary location or a potentially dangerous size, it should therefore be resected as early surgical intervention may guarantee complete cure, preventing sudden death and irreversible heart failure.
Conclusions
Our patient, who had a cardiac intracavitary tumour mass characterised as a true right atrial lipoma, underwent tumour resection. This was justified by the risks of sudden death and late complications in cardiac function.
References
- 1.Xie LX, Chen YS, Liu SY. A giant cardiac lipoma associated with ventricular inversion and ventricular aneurysm. Chest 2012; 141: 241–244. [DOI] [PubMed] [Google Scholar]
- 2.McAllister HA, Hall RJ, Cooley DA. Tumors of the heart and pericardium. Curr Probl Cardiol 1999; 24: 57–116. [PubMed] [Google Scholar]
- 3.Tazelaar HD, Locke TJ, McGregor CG. Pathology of surgically excised primary cardiac tumors. Mayo Clin Proc 1992; 67: 957–965. [DOI] [PubMed] [Google Scholar]
- 4.Jabir S, Al-Hyassat S. Histological diagnosis of cardiac lipoma in an adult with tuberous sclerosis. BMJ Case Rep 2013; bcr2012007484. [DOI] [PMC free article] [PubMed]
- 5.Grande AM, Minzioni G , Pederzolli C et al. Cardiac lipomas. Description of 3 cases. J Cardiovasc Surg 1998; 39: 813–815. [PubMed] [Google Scholar]
- 6.Rajiah P, To AC , Tan CD , Schoenhagen P. Multimodality imaging of an unusual case of right ventricular lipoma. Circulation 2011; 124: 1,897–1,898. [DOI] [PubMed] [Google Scholar]
- 7.McNamara RF, Taylor AE, Panner BJ. Superior vena caval obstruction by lipomatous hypertrophy of the right atrium. Clin Cardiol 1987; 10: 609–610. [DOI] [PubMed] [Google Scholar]


