Abstract
Hemolymphangioma is a malformation of the lymphatic and blood vessels. To the best of our knowledge, only a limited number of hemolymphangioma cases have been reported in the literature thus far, with no cases developed in the waist region. The present study reported the case of a 17-year-old male patient with hemolymphangioma growing on the waist, presented with back pain for four months. Upon physical examination, the lesion was identified to be oval in shape, soft and compressible, with mild tenderness. No abnormalities were detected in the results of laboratory examinations. However, a magnetic resonance imaging (MRI) scan revealed a tumor with low signal intensity on T1-weighted imaging (WI) and high signal intensity on T2-WI. The mass was successfully removed during surgery. During the seven-month follow-up period, the patient was asymptomatic with no evidence of recurrence. The present study discussed the imaging findings and pathological features of this uncommon case and reviewed the relevant literature.
Keywords: waist, hemolymphangioma, back pain
Introduction
Lymphangioma, also known as angioma lymphaticum, is a congenital malformation of the vascular system, comprising newly-formed lymph spaces and channels (1). Landing and Farber (2) classified this benign malformation in four categories, including capillary, cavernous and cystic (hygroma) lymphangioma, and hemolymphangioma, which is a combination of hemangioma and lymphangioma.
Hemolymphangioma is a congenital malformation that may be asymptomatic for a long period of time (3). This lesion is typically considered to be a benign and noninvasive disorder, characterized by the presence of dilated lymphatic spaces, extravasation of red blood cells, hemosiderin deposition and fibrosis (4). Hemolymphangioma formation may be due to venolymphatic communication obstruction between the dysembrioplastic vascular tissue and systemic circulation (5).
The incidence of hemolymphangioma is 1.2–2.8 per 1,000 newborn infants (6). Hemolymphangioma has been previously detected at the pancreas (5,7–12), spleen (13–16), stomach (1,17), rectum (18), mediastinum (19–21), chest wall (22–25), small intestine (26), extremities (3,27,28), cervix (29,30), pericardium (31), oral region (32), esophagus (33), axilla (34), retroperitoneal space (35,36), adrenal gland (37), abdomen (38), duodenum (4) and hepatica (39), as well as on the tongue (40,41) and orbit (42,43). However, to the best of our knowledge, no studies have reported this type of tumor in the waist region, as determined by a review of the medical literature until June 2014 using the PubMed database (http://www.ncbi.nlm.nih.gov/pubmed; accessed on 9th June 2014). Complete excision is considered the optimal treatment for hemolymphangioma, which exhibits a low recurrence rate. Non-surgical treatments are also used, including aspiration and drainage, cryotherapy, injection of sclerotic agents, laser therapy and radiotherapy, however, to date, the outcomes of such treatments have been unsatisfactory (3,22). In cases of tumor recurrence, conservative treatment methods such as laser therapy, may be applied (3,44). Generally, the prognosis of hemolymphangioma is good (3,4,13,17,18), however, careful follow-up is required.
The present study reported the case of a 17-year-old male patient with hemolymphangioma on the waist and reviewed the characteristics of this disease based on the existing literature.
Case report
A 17-year-old male was admitted at the General Hospital of Armed Police Force (Beijing, China) in September 2013, complaining of a mass on the right side of the waist and back pain for approximately four months. The back pain was significantly increased when the patient was sedentary and was slightly alleviated by rest. On admission, the patient was well, with no symptoms of lower extremity numbness and pain, or abdominal pain. Upon physical examination, the lesion was identified to be oval in shape, soft and compressible, with mild tenderness. No abnormalities were detected in the results of laboratory examinations. An ultrasound (Doppler sonography) detected a cystic lesion (15.0×10.0 cm) with blood flow, and revealed multiple echo and irregular cavities in the subcutaneous fat layer of the right waist. The most likely diagnosis was hemolymphangioma.
Magnetic resonance imaging (MRI) examination was performed preoperatively, in order to establish the extent of the tumor and define its association with the surrounding tissues. A waist MRI scan (Fig. 1) revealed a 12.6×9.7-cm mass, with low signal intensity on T1-weighted imaging (WI) and high signal intensity on T2-WI in the right side of the waist subcutaneous tissue with the fifth lumbar level parallel. Upon performing a tumor biopsy with a 5-ml syringe, 10-ml yellow, clear liquid was extracted and laboratory examinations were performed. Preoperatively, no abnormalities were revealed in the laboratory data, including the levels of tumor markers [α-fetoprotein, carcinoembryonic antigen, carbohydrate antigen (CA) 19-9, and CA-125] and concentrated mycobacterium tuberculosis.
Figure 1.
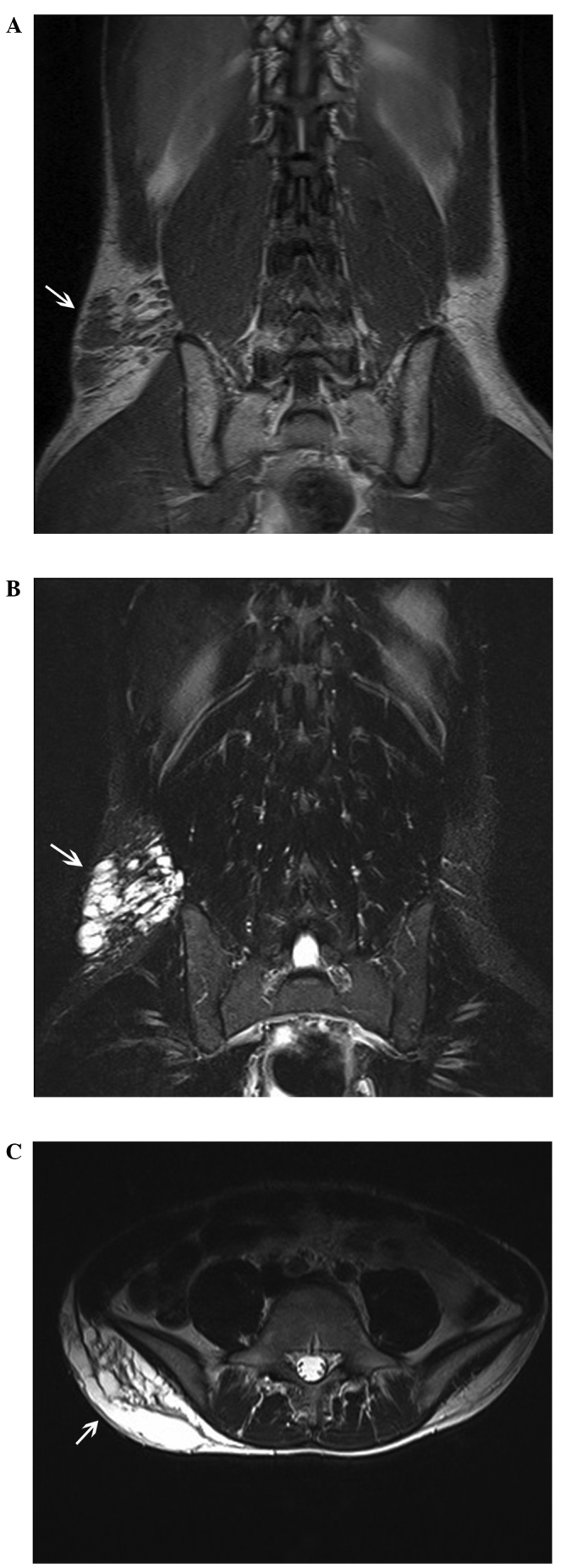
Magnetic resonance imaging (MRI) findings. The scans demonstrate the (A) coronal T1-weighted imaging (WI), (B) coronal T2-WI and (C) axial T2-WI. A mass (arrows) was identified, with low signal intensity on T1-WI and high signal intensity on T2-WI in the right side of the waist subcutaneous tissue with the fifth lumbar level parallel.
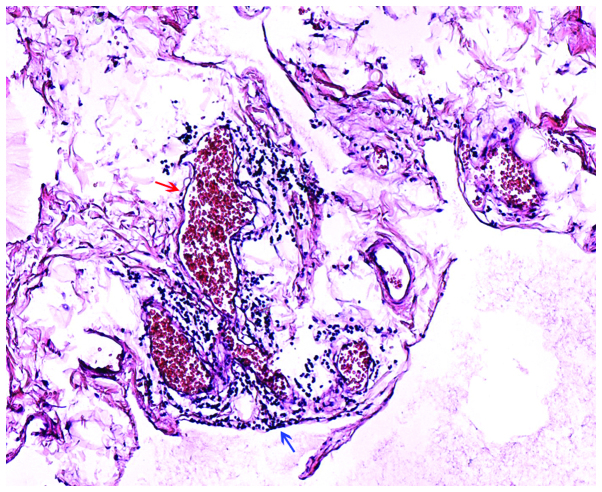
Due to the patient experiencing back pain that was increased upon sitting, surgical excision was decided as the treatment strategy. During surgery, the boundary of the mass was unclear and a bloody yellow exudate was observed. Macroscopically, the mass measured approximately 12.0×6.0×6.0 cm, and was oval and soft. Multiloculated cystic masses filled with blood and yellow fluid were extracted. Histologically, the tumor was composed of lymphatic and blood vessels with polycystic spaces (Fig. 2). Considering these observations, the definitive histological diagnosis was hemolymphangioma of the waist. The postoperative course of the patient was uneventful. In the course of a seven-month follow-up period, no recurrence of hemolymphangioma was observed. This study was approved by the ethics committee of General Hospital of Armed Police Force (Beijing, China) and written informed consent was obtained from the patient's family.
Figure 2.
Histological analysis of biopsy specimen (hematoxylin and eosin stain; magnification, ×100). Blood vessels (red arrow) and lymphatic vessels (blue arrow) can be observed in the tumor.
Discussion
Hemolymphangiomas, a congenital malformation of the vascular system, can be classified into primary and secondary lymphatic vascular tumors. Primary tumors are congenital malformations of the lymphatic vascular system, possibly formed due to obstruction of the venolymphatic communication between the dysembryoplastic vascular tissue and the systemic circulation. By contrast, secondary tumors are likely to be caused by poor lymph drainage and lymphatic damage resulting from surgery or trauma (43). Hemolymphangioma mainly presents as cystic or cavernous lesions. Histologically, hemolymphangioma is composed of dense fibrous tissue that develops in bands between the numerous vascular spaces, invading the subcutaneous fat and involving the blood or lymphatic vessels (3).
The incidence of hemolymphangioma is 1.2–2.8 per 1,000 newborns (45), and the two genders are equally affected. In the present study, a review of the literature up to June 2014 was performed using the PubMed database. The search strategy to identify all possible studies involved use of the word ‘hemolymphangioma’. In total, 47 previous studies concerning this type of tumor were identified (1,3–42,44,46–50). However, to the best of our knowledge, no studies have reported hemolymphangioma of the waist. In the current case, the patient was a 17-year-old male, and the tumor occurred on the waist and appeared as a cystic lesion.
Clinically, the onset of hemolymphangioma can vary between a slow-growing cyst over a period of years and an aggressive enlarging tumor without invasive ability (3). The size of these tumors varies due to the different anatomical location and association with the neighboring tissues. In clinical examinations, they are usually described as soft and compressible masses, loculated in pattern. The most common complications are random or traumatic hemorrhage, rupture and infection (3). However, no abnormal laboratory findings were observed in the current patient, and the only symptom was back pain for four months.
In the present study, a waist MRI scan revealed a tumor with low signal intensity on T1-WI and high signal intensity on T2-WI on the right side of the waist subcutaneous tissue in the fifth lumbar level. These observations may indicate the presence of a lower number of tortuous blood vessels and water-based substance in the lesion, which was then confirmed during surgery. Imaging examinations, including ultrasound, computed tomography and MRI scans, are useful in order to confirm the diagnosis, identify the tumor nature, and observe its extension and association with the surrounding tissues, assisting the selection of the surgical strategy and follow-up treatment (51). However, a definitive diagnosis of the tumor in the present study was based on histological evidence.
Surgical resection appears to be the most effective treatment for hemolymphangioma. In order to prevent recurrence, thorough radical resection may be required during surgery. In the English literature, the reported recurrence rates were in the range of 10–27% upon complete removal of the lesions, while the recurrence rates were 50–100% in cases where the lesions were partially removed (4,52). The extend of surgical resection depends mainly on the anatomical location and complexity of the tumor (3,4,12,52).
In conclusion, hemolymphangioma of the waist is an uncommon vascular and lymphatic lesion, presenting mainly with back pain. Preoperative imaging examinations, including ultrasound and MRI, are important for a full evaluation of the tumor in order to confirm the diagnosis and plan the surgical strategy. Complete surgical resection is the most effective treatment with good prognosis.
References
- 1.Li QY, Xu Q, Fan SF, Zhang Y. Gastric haemolymphangioma: a literature review and report of one case. Br J Radiol. 2012;85:e31–e34. doi: 10.1259/bjr/31987746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Landing BH, Farber S. Atlas of Tumor Pathology. Armed Forces Institute of Pathology; Washington DC: 1956. Tumors of the Cardiovascular System; pp. 124–138. [Google Scholar]
- 3.Kosmidis I, Vlachou M, Koutroufinis A, Filiopoulos K. Hemolymphangioma of the lower extremities in children: two case reports. J Orthop Surg Res. 2010;5:56. doi: 10.1186/1749-799X-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Antonino A, Gragnano E, Sangiuliano N, et al. A very rare case of duodenal hemolymphangioma presenting with iron deficiency anemia. Int J Surg Case Rep. 2014;5:118–121. doi: 10.1016/j.ijscr.2013.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Balderramo DC, Di Tada C, de Ditter AB, Mondino JC. Hemolymphangioma of the pancreas: case report and review of the literature. Pancreas. 2003;27:197–199. doi: 10.1097/00006676-200308000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Filston HC. Hemangiomas: cystic hygromas and teratomas of the head and neck. Semin Pediatr Surg. 1994;3:147–159. [PubMed] [Google Scholar]
- 7.Sun LF, Ye HL, Zhou QY, et al. A giant hemolymphangioma of the pancreas in a 20-year-old girl: a report of one case and review of the literature. World J Surg Oncol. 2009;7:31. doi: 10.1186/1477-7819-7-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Toyoki Y, Hakamada K, Narumi S, et al. A case of invasive hemolymphangioma of the pancreas. World J Gastroenterol. 2008;14:2932–2934. doi: 10.3748/wjg.14.2932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Banchini E, Bonati L, Villani LG. A case of hemolymphangioma of the pancreas. [(In Italian)]. Minerva Chir. 1987;42:807–813. [PubMed] [Google Scholar]
- 10.Montete P, Marmuse JP, Claude R, Charleux H. Hemolymphangioma of the pancreas. [(In French)]. J Chir (Paris) 1985;122:659–663. [PubMed] [Google Scholar]
- 11.Couinaud C, Jouan, Prot, Chalut, Favre, Schneiter A rare tumor of the head of the pancreas. Hemolymphangioma weighing 1,500 kg. [(In French)]. Presse Med. 1967;75:1955–1956. [PubMed] [Google Scholar]
- 12.Couinaud, Jouan, Prot, Chalut, Schneiter Hemolymphangioma of the head of the pancreas. [(In French)]. Mem Acad Chir (Paris) 1966;92:152–155. [PubMed] [Google Scholar]
- 13.Zhang Y, Chen XM, Sun DL, Yang C. Treatment of hemolymphangioma of the spleen by laparoscopic partial splenectomy: a case report. World J Surg Oncol. 2014;12:60. doi: 10.1007/s00268-013-2271-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dong F, Zheng Y, Wu JJ, et al. Hemolymphangioma: a rare differential diagnosis of cystic-solid or cystic tumors of the pancreas. World J Gastroenterol. 2013;19:3520–3523. doi: 10.3748/wjg.v19.i22.3520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bethouart M, Houcke M, Proye C, Linquette M. Hepatosplenic hemolymphangioma. [(In French)]. Lille Med. 1980;25:288–290. [PubMed] [Google Scholar]
- 16.Scaltriti F, Manenti A. Hemolymphangioma of the lower pole of the spleen (migrated into the pelvis minor) [(In Italian)]. Chir Ital. 1967;19:543–554. [PubMed] [Google Scholar]
- 17.Kim WT, Lee SW, Lee JU. Bleeding gastric hemolymphangioma: endoscopic therapy is feasible. Dig Endosc. 2013;25:553–554. doi: 10.1111/den.12147. [DOI] [PubMed] [Google Scholar]
- 18.Chen G, Cui W, Ji XQ, Du JF. Diffuse hemolymphangioma of the rectum: a report of a rare case. World J Gastroenterol. 2013;19:1494–1497. doi: 10.3748/wjg.v19.i9.1494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zehani A, Ayadi-Kaddour A, Cherif J, Marghli A, et al. Cystic mediastinal hemolymphangioma. [(In French)]. Tunis Med. 2012;90:754–755. [PubMed] [Google Scholar]
- 20.Contamin C, Denis B, Mallion JM, et al. Heart hemolymphangioma. Apropos of a case. [(In French)]. Coeur Med Interne. 1973;12:671–678. [PubMed] [Google Scholar]
- 21.Bagolan P, Alati E, Fisicaro M. Some defects of development of the mediastinum; three cases: one cavernous hemolymphangioma and two cystic hygromas. [(In Italian)]. Archivio Chir Torace. 1953;10:559–573. [PubMed] [Google Scholar]
- 22.Zhang X, Sheng X, Liu F, et al. Hemolymphangioma of the chest wall: A rare case report. Oncol Lett. 2012;3:816–818. doi: 10.3892/ol.2012.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bosdure E, Mates M, Mely L, et al. Cystic intrathoracic hemolymphangioma: a rare differential diagnosis of acute bronchiolitis in an infant. [(In French)]. Arch Pediatr. 2005;12:168–172. doi: 10.1016/j.arcped.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 24.Zernov NG, Poliakov VE, Vorob'eva ML. Diseases of the lymphatic vessels in children lymphangioma, hemolymphangioma, lymphangitis. [(In Russian)]. Feldsher Akush. 1986;51:27–29. [PubMed] [Google Scholar]
- 25.Sztaba R, Vondrat W. Thoracic hemolymphangioma with chylothorax in a newborn infant. [(In French)]. Ann Chir Infant. 1965;6:21–26. [PubMed] [Google Scholar]
- 26.Fang YF, Qiu LF, Du Y, Jiang ZN, Gao M. Small intestinal hemolymphangioma with bleeding: a case report. World J Gastroenterol. 2012;18:2145–2146. doi: 10.3748/wjg.v18.i17.2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beninson J, Hurley JP. Hemolymphangioma in a neonate-a therapeutic problem-case history. Angiology. 1988;39:1043–1047. doi: 10.1177/000331978803901207. [DOI] [PubMed] [Google Scholar]
- 28.Cole DJ, Sood SC, Broomhead IW. Pulmonary embolism associated with hemolymphangioma of lower extremity. Plast Reconstr Surg. 1979;63:265–268. doi: 10.1097/00006534-197902000-00026. [DOI] [PubMed] [Google Scholar]
- 29.Gaillard de Collogny L, Delage J. Cervical hemolymphangioma in a young patient. [(In French)]. J Fr Otorhinolaryngol Audiophonol Chir Maxillofac. 1981;30:469–473. [PubMed] [Google Scholar]
- 30.Bortolozzi G, Santoni G. Hemolymphangioma of the uterine cervix associated with early carcinoma. [(In Italian)]. Minerva Ginecol. 1974;26:722–729. [PubMed] [Google Scholar]
- 31.Nataf P, Martin de Lasalle E, Benomar M, Gandjbakhch I, Cabrol C. Pericardial hemolymphangioma. Apropos of a case. [(In French)]. Arch Mal Coeur Vaiss. 1988;81:1137–1140. [PubMed] [Google Scholar]
- 32.Ullik R. On a hemolymphangioma of the floor of the mouth. [(In German)]. Wien Klin Wochenschr. 1959;71:958–960. [PubMed] [Google Scholar]
- 33.Canavese F, Cortese MG, Proietti L, et al. Bulky-pedunculated hemolymphangioma of the esophagus: rare case in a two-years old girl. Eur J Pediatr Surg. 1996;6:170–172. doi: 10.1055/s-2008-1066499. [DOI] [PubMed] [Google Scholar]
- 34.Tsonchev P. Hemolymphangioma cavernosum axillae dextrae. [(In Bulgarian)]. Khirurgiia (Sofiia) 1958;11:869–870. [PubMed] [Google Scholar]
- 35.Kanaitsuka T, Itani K, Shigeta H, et al. A case report of giant retroperitoneal hemolymphangioma. [(In Japanese)]. Nihon Naika Gakkai Zasshi. 1987;76:1595–1603. doi: 10.2169/naika.76.1595. [DOI] [PubMed] [Google Scholar]
- 36.Houdart R, Palau R, Auclair E, Costa JC, Potet F. Infected retroperitoneal hemolymphangioma in an adult with the Klippel-Trenaunay syndrome. Ultrasonic diagnosis. [(In French)]. Presse Med. 1986;15:216. [PubMed] [Google Scholar]
- 37.Gossot D, Decazes JM, Sarfati E, Dubost C. Cystic hemolymphangioma of the adrenal gland. [(In French)]. J Chir (Paris) 1987;124:404–405. [PubMed] [Google Scholar]
- 38.Giacalone PL, Boulot P, Marty M, et al. Fetal hemangiolymphangioma: a case report. Fetal Diagn Ther. 1993;8:338–340. doi: 10.1159/000263849. [DOI] [PubMed] [Google Scholar]
- 39.Daudet M. Reflections apropos of a case of hepatic hemolymphangioma of the infant. Operation recovery. [(In French)]. Pediatrie. 1965;20:445–451. [PubMed] [Google Scholar]
- 40.Laufer J, Girsault M. Hemolymphangioma of the tongue treated with combination embolization-surgery. Apropos of a case. [(In French)]. Rev Stomatol Chir Maxillofac. 1986;87:184–187. [PubMed] [Google Scholar]
- 41.Bureau Y, Delaire J, Barriere H, Litoux P, Bureau B. Hemolymphangioma of the tongue. Results of surgical treatment. [(In French)]. Bull Soc Fr Dermatol Syphiligr. 1966;73:422–423. [PubMed] [Google Scholar]
- 42.Chanfi M. Hemolymphangioma of the orbit in a young girl: a clinical observation. [(In French)]. J Fr Ophtalmol. 2004;27:1047–1049. doi: 10.1016/S0181-5512(04)96263-8. [DOI] [PubMed] [Google Scholar]
- 43.Guillot M, Dufier JL, Pierre-Kahn A, Nihoul-Fekete C, Lenoir G, Haye C. Hemolymphangioma of the orbit in children. [(In French)]. Arch Fr Pediatr. 1983;40:401–403. [PubMed] [Google Scholar]
- 44.Wang LC, Krunic AL, Medenica MM, Soltani K, Busbey S. Treatment of hemorrhagic lymphatic malformation of the tongue with a pulsed-dye laser. J Am Acad Dermatol. 2005;52:1088–1090. doi: 10.1016/j.jaad.2005.03.014. [DOI] [PubMed] [Google Scholar]
- 45.Lu YY, Zhan AL. Imaging diagnosis of CT and MRI on hemolymphangioma. [(In Chinese)]. Zhongguo CT He MRI Za Zhi. 2010;8:51–53. [Google Scholar]
- 46.Fan Z, Li Y, Yan K, et al. Application of contrast-enhanced ultrasound in the diagnosis of solid pancreatic lesions—a comparison of conventional ultrasound and contrast-enhanced CT. Eur J Radiol. 2013;82:1385–1390. doi: 10.1016/j.ejrad.2013.04.016. [DOI] [PubMed] [Google Scholar]
- 47.Cophignon J, d'Hermies F, Civit T. Vascular tumors of the orbit. [(In French)]. Neurochirurgie. 2010;56:197–212. doi: 10.1016/j.neuchi.2010.02.028. [DOI] [PubMed] [Google Scholar]
- 48.Riquet M, Briere J, Le Pimpec-Barthes F, et al. Cystic lymphangioma of the neck and mediastinum: are there acquired forms? Report of 37 cases. [(In French)]. Rev Mal Respir. 1999;16:71–79. [PubMed] [Google Scholar]
- 49.Giron J, Conte J, Chicoisne MP, Mazères F, Berjaud J, Dahan M. Cervico-mediastinal cystic lymphangioma. [(In French)]. Ann Radiol (Paris) 1992;35:217–221. [PubMed] [Google Scholar]
- 50.Fontaliran F, Guillois B, Colin A. Congenital atrioventricular block and maternal lupus erythematosus. Histologic discovery of tumor of the atrioventricular node. [(In French)]. Arch Mal Coeur Vaiss. 1989;82:609–613. [PubMed] [Google Scholar]
- 51.Kennedy TL, Whitaker M, Pellitteri P, Wood WE. Cystic hygroma/lymphangioma: a rational approach to management. Laryngoscope. 2001;111:1929–1937. doi: 10.1097/00005537-200111000-00011. [DOI] [PubMed] [Google Scholar]
- 52.Hebra A, Brown MF, McGeehin KM, Ross AJ., III Mesenteric, omental and retroperitoneal cysts in children: a clinical study of 22 cases. South Med J. 1993;86:173–176. doi: 10.1097/00007611-199302000-00005. [DOI] [PubMed] [Google Scholar]