ABSTRACT
Human coronavirus (hCoV) HKU1 is one of six hCoVs identified to date and the only one with an unidentified cellular receptor. hCoV-HKU1 encodes a hemagglutinin-esterase (HE) protein that is unique to the group a betacoronaviruses (group 2a). The function of HKU1-HE remains largely undetermined. In this study, we examined binding of the S1 domain of hCoV-HKU1 spike to a panel of cells and found that the S1 could specifically bind on the cell surface of a human rhabdomyosarcoma cell line, RD. Pretreatment of RD cells with neuraminidase (NA) and trypsin greatly reduced the binding, suggesting that the binding was mediated by sialic acids on glycoproteins. However, unlike other group 2a CoVs, e.g., hCoV-OC43, for which 9-O-acetylated sialic acid (9-O-Ac-Sia) serves as a receptor determinant, HKU1-S1 bound with neither 9-O-Ac-Sia-containing glycoprotein(s) nor rat and mouse erythrocytes. Nonetheless, the HKU1-HE was similar to OC43-HE, also possessed sialate-O-acetylesterase activity, and acted as a receptor-destroying enzyme (RDE) capable of eliminating the binding of HKU1-S1 to RD cells, whereas the O-acetylesterase-inactive HKU1-HE mutant lost this capacity. Using primary human ciliated airway epithelial (HAE) cell cultures, the only in vitro replication model for hCoV-HKU1 infection, we confirmed that pretreatment of HAE cells with HE but not the enzymatically inactive mutant blocked hCoV-HKU1 infection. These results demonstrate that hCoV-HKU1 exploits O-Ac-Sia as a cellular attachment receptor determinant to initiate the infection of host cells and that its HE protein possesses the corresponding sialate-O-acetylesterase RDE activity.
IMPORTANCE Human coronaviruses (hCoV) are important human respiratory pathogens. Among the six hCoVs identified to date, only hCoV-HKU1 has no defined cellular receptor. It is also unclear whether hemagglutinin-esterase (HE) protein plays a role in viral entry. In this study, we found that, similarly to other members of the group 2a CoVs, sialic acid moieties on glycoproteins are critical receptor determinants for the hCoV-HKU1 infection. Interestingly, the virus seems to employ a type of sialic acid different from those employed by other group 2a CoVs. In addition, we determined that the HKU1-HE protein is an O-acetylesterase and acts as a receptor-destroying enzyme (RDE) for hCoV-HKU1. This is the first study to demonstrate that hCoV-HKU1 uses certain types of O-acetylated sialic acid residues on glycoproteins to initiate the infection of host cells and that the HKU1-HE protein possesses sialate-O-acetylesterase RDE activity.
INTRODUCTION
Human coronaviruses (hCoVs) are enveloped RNA viruses. They are usually associated with mild to moderate respiratory tract illnesses but can also cause severe and highly lethal disease, depending on the virus strain (1). Six hCoV strains have been identified to date and belong to four different groups, including hCoV-229E and hCoV-NL63 in the alphacoronaviruses (group 1); hCoV-OC43 and hCoV-HKU1 in the group a betacoronaviruses (group 2a); severe acute respiratory syndrome CoV (SARS-CoV) in the group b betacoronaviruses (group 2b); and Middle East respiratory syndrome CoV (MERS-CoV) in the group c betacoronaviruses (group 2c). Infections by viruses in groups 1 and 2a are common worldwide and can also cause severe disease in young children or immunocompromised adults. SARS-CoV (2–4) and MERS-CoV (5, 6) are two highly virulent hCoVs causing severe respiratory diseases with high morbidity and mortality (7); the latter strain is still circulating in human populations.
Cellular receptor specificity plays an important role in viral cell and tissue tropism, pathogenesis, interspecies transmission, and adaptation. The CoV Spike (S) glycoprotein is generally responsible for binding to cellular receptors and mediating viral entry. The S protein is a large type I transmembrane glycoprotein that exists as a trimer protruding from the surface of virions (8). S proteins have an amino-terminal (NT) S1 domain that mediates binding with cellular receptors and a carboxy-terminal (CT) S2 domain that mediates subsequent virus-cell membrane fusions. A wide range of diverse cellular receptors specifically recognized by the S1 domains have been identified for all the aforementioned hCoVs except hCoV-HKU1. Human aminopeptidase N (CD13) is the cellular receptor for hCoV-229E (9). 9-O-Acetylated sialic acid (9-O-Ac-Sia) is the cellular receptor determinant for hCoV-OC43 (10). hCoV-NL63 and SARS-CoV both employ human angiotensin-converting enzyme 2 (ACE2) to mediate cellular entry (11, 12), while hCoV-NL63 utilizes heparan sulfate proteoglycans for attachment to target cells (13). MERS-CoV utilizes dipeptidyl peptidase 4 (DPP4 or CD26) receptor to enter host cells (14).
hCoV-HKU1 was initially identified in 2005 from a pneumonia patient in Hong Kong (15). It was subsequently found to be as common and widespread as previously known hCoVs, namely, hCoV-229E, hCoV-OC43, and hCoV-NL63 (16–19). Characterization of hCoV-HKU1 has been challenging due to the lack of a convenient cell line-based culture system. It was recently demonstrated that hCoV-HKU1 replicates to a high titer in an in vitro culture system that uses primary human ciliated airway epithelial (HAE) cells or type II alveolar epithelial cells (20–22); however, the functional receptor(s) of hCoV-HKU1 and other important aspects of virus-host interaction remains unknown. As a member of group 2a CoVs, HKU1-CoVs also carry another viral surface protein hemagglutinin-esterase (HE)-encoding gene that is present exclusively in this group of CoV genomes (23). The HE protein is also a type I transmembrane glycoprotein comprised of two functional domains: an O-acetylated sialic acid binding domain and a corresponding sialate O-acetylesterase domain (24). HE protein functions primarily as a receptor-destroying enzyme (RDE) for CoVs, e.g., hCoV-OC43 and its proposed zoonotic ancestor, bovine coronavirus (BCoV) (25). Both viruses bind to receptor 9-O-Ac-Sia via their S proteins, and their HE proteins mediate RDE activity late in the infection cycle via the sialate-9-O-acetylesterase domain to facilitate the release of viral progeny and escape from attachment on nonpermissive host cells (23, 26). In contrast, mouse hepatitis virus (MHV), another member of group 2a CoVs, infects cells via the interaction of S protein with its principal receptor, the carcinoembryonic antigen-related cell adhesion molecule (CEACAM1a), while the MHV HE protein functions at very early viral attachment steps through the concerted action of its O-acetylated sialic acid binding and RDE activities (27, 28). To date, the function and role of the hCoV-HKU1 HE protein have remained undefined.
In this study, we found that the hCoV-HKU1 S protein mediated viral attachment by utilizing O-acetylated sialic acids on glycoprotein(s) as a receptor determinant or as initial attachment factors. The HE protein of hCoV-HKU1 did not exhibit sialic acid binding activity but instead mediated sialate-O-acetylesterase RDE activity specific to the O-acetylated sialic acids recognized by the S protein. Interestingly, HKU1-HE protein displayed sialate-9-O-acetylesterase RDE activity similar to that seen with OC43-HE and BCoV-HE. In the hCoV-HKU1 in vitro replication model, we further demonstrated that the HE protein but not an enzymatically inactive HE mutant acted as a RDE and completely blocked or greatly reduced infection, depending on the dose of inoculating hCoV-HKU1. These findings revealed that early viral entry steps for hCoV-HKU1 are similar to but also distinct from those for other members of group 2a CoVs. Like hCoV-OC43 and BCoV, hCoV-HKU1 employs O-acetylated sialic acids as a primary receptor determinant or attachment factor and its HE protein as a corresponding RDE; however, hCoV-HKU1 also uniquely requires additional receptor determinants beyond those required by hCoV-OC43 and BCoV.
MATERIALS AND METHODS
Construction of expression plasmids.
A synthetic codon-optimized sequence for the HKU1-S1 gene (GenBank accession number NC_006577.2) encoding amino acids (aa) 15 to 600 was cloned into a mammalian expression vector containing a CD5 signal peptide and a C-terminal Fc tag from mouse IgG2a (mFc). The expression cassette was under the control of a cytomegalovirus (CMV) early enhancer/chicken β actin (CAG) promoter. The resulting construct, pCAGGS-HKU1-S1(600)-mFc, encodes a chimeric S1 protein with an N-terminal CD5 signal peptide and mFc at its C terminus. Similarly, plasmids encoding other proteins, including the NT domain of HKU1-S1 (aa 15 to 268), the NT domain of hCoV-OC43-S1 (aa 15 to 268) (ATCC VR-759 strain; GenBank accession no. AAT84354), and the NT domain of S1 of CoV-HKU3 (aa 16 to 323) (DQ022305), were constructed. The extracellular domains of HE proteins from different CoVs, including HKU1-HE (aa 14 to 358; GenBank accession no. NC_006577.2), hCoV-OC43-HE protein (aa 19 to 376; AAX85668.1), BCoV-HE (aa 19 to 377; AAA92991.1), and MHV-S-HE (aa 25 to 393; AAX08110.1), were similarly constructed. Plasmids encoding mutants of HKU1-HE were generated by the site-directed QuikChange mutagenesis method (Stratagene). All mutations were confirmed by DNA sequencing, in which the codon for esterase-catalytic residue Ser40 was replaced by Ala (S40A mutant) or the catalytic triad S40, H329, and D326 were all replaced by Ala (S40A/H329A/D326A).
Expression and purification of recombinant proteins.
HEK293T cells were transiently transfected with the expression plasmids using polyethyleneimine (Polysciences). At 12 h after transfection, the medium was replaced by 293 SFM II expression medium (Life Technology). Tissue culture supernatants were harvested 3 days after transfection, and the recombinant proteins were purified by protein A-based affinity chromatography.
Flow cytometry FACS analysis.
HKU1-S1(600)-mFc or other proteins at different concentrations were diluted in fluorescence-activated cell sorter (FACS) buffer (phosphate-buffered saline [PBS] containing 0.5% bovine serum albumin [BSA] and 0.1% NaN3) and then incubated with 0.5 × 106 to 1 × 106 RD cells or red blood cells (RBCs) from mouse or rat blood samples at 4°C for 0.5 to 1 h. Cells were then washed three times with FACS buffer followed by incubation with fluorescein isothiocyanate (FITC)-labeled anti-mouse Fc antibody at a dilution following the instructions of the manufacturer (Sigma or Pierce) at 4°C for 30 min. Cells were washed as described above, and the binding of proteins to cells was analyzed by the use of a BD FACS LSRII (Becton Dickinson) flow cytometer and FCS Express software (De Novo Software). For FACS analysis to examine the inhibition of HKU1-S1 binding to RD cells, the cells were pretreated with the indicated HE proteins or enzymes at different concentrations and then incubated with HKU1-S1, after which binding was analyzed as described above. The neuraminidase (NA) was from Clostridium perfringens (Sigma), and the bovine pancreas-derived trypsin treated with N-tosyl-l-phenylalanyl chloromethyl ketone (TPCK) was purchased from Sigma. For both NA and trypsin, the pretreatment was carried out at 37°C for 1 h; for the HE proteins, the pretreatment was carried out at 4°C for 1 h.
Indirect immunofluorescence.
RD cells were seeded on glass coverslips 1 day before staining. Cells were washed three times with PBS, blocked with 0.5%BSA–PBS at 37°C for 30 min, incubated with HKU1-600-mFc or HKU3-323-mFc at 20 μg/ml in PBS at 4°C for 1 h followed by washing three times with PBS, and then incubated with FITC-goat anti-mouse Fc antibody (Sigma) at 4°C for 1 h. Cells were washed three times and then incubated with 5 μg/ml Hoechst 33258 at 37°C for 10 min, followed by three additional washes, and finally incubated with 5 μg/ml FM-4-64 on ice for 1 min. Cells were analyzed and imaged with a 63× oil objective using an Zeiss LSM510 Meta confocal microscope. Representative images are shown.
HA assay.
RBCs in an approximately 0.25% to 0.5% suspension prepared from mouse (BALB/c) or rat (Sprague Dawley) blood were added to a round-bottom 96-well plate at 50 μl/well. S1 proteins were 2-fold serial diluted with 0.5%BSA–PBS and added at 50 μl/well to the wells containing RBCs. For the HE protein inhibition assay, RBCs were first pretreated with HE (2-fold serially diluted) and washed by the use of PBS followed by addition of 50 μl/well of 10 μg/ml of hCoV-OC43-S1 to the wells containing the HE-pretreated and washed RBCs. The plates were left at room temperature for 60 min or longer until hemagglutination (HA) developed or the RBCs gradually settled. Positive hemagglutination resulted in the formation of a uniform reddish color across the well, whereas negative results appeared as dots in the center of round-bottomed plates due to the sedimentation of RBCs.
ELISA.
The binding of S1 proteins to bovine submaxillary mucin (BSM) was determined by an enzyme-linked immunosorbent assay (ELISA) as previously described (28) with modification. Maxisorp 96-well plates (Nunc) were coated overnight at 4°C with BSM (Sigma) at 10 μg/ml and at 100 μl/well. The wells were washed with washing buffer (PBST [0.05% Tween 20–PBS]) and treated with blocking buffer (PBS, 0.05% Tween 20, 2% nonfat milk) for 1 h at room temperature. Serially diluted S1 proteins were prepared in blocking buffer (starting concentration, 20 μg/ml) and then added to the BSM-coated wells at 100 μl/well. Incubation was continued for 1 h followed by washing with PBST six times. Binding was detected using an horseradish peroxidase (HRP)-conjugated goat anti-mouse IgG (Pierce) (1:10,000 in blocking buffer) followed by washing again. The optical density at 450 nm (OD450) was measured after incubation of the peroxidase tetramethylbenzidine (TMB) substrate and stop solution.
Acetylesterase activity assay.
Chromogenic p-nitrophenyl acetate (pNPA; Sigma) substrate was 2-fold serially diluted and then incubated with 1 or 2 μg/ml HE-mFc protein or its mutants in a 100-μl volume in PBS (pH 7.4) at 37°C for different time periods as indicated. The acetylesterase activity was determined by measuring the release of para-nitrophenol (OD450) at the end of each reaction in microtiter plates with a microplate spectrophotometer (Bio-Rad). An unrelated protein was used as a control in the enzymatic assay, and the OD405 for HE protein or mutants was subtracted from that of this control. The Km value of HE protein was calculated from the Michaelis-Menten enzyme kinetics curve using Graphpad Prism 5 software.
Neuraminidase activity assay.
An Amplex red neuraminidase assay kit (Molecular Probes/Invitrogen) was used to measure NA activity. Briefly, 25 μg/ml of HKU1-HE protein was serially diluted in 50 μl of 1× reaction buffer followed by addition of 50 μl of a 2× working solution containing 100 μM Ample Red reagent, 0.2 U/ml of HRP, and 4 U/ml of galactose oxidase, and the fetuin substrate was serially diluted 100-fold from 2.5 mg/ml to 2.5 pg/ml. The mixture was incubated at 37°C for 10 min under dark conditions, the fluorescence signal was then measured at a wavelength of 595 nm, and the measured values were used to indicate relative NA activity levels.
HKU1 infection of HAE cells.
The HAE cell culture system has been described previously (20). Briefly, the apical surface of HAE cells was washed three times in situ with phosphate-buffered saline (PBS) and then treated with testing reagents or controls by incubation at 32°C for 1 h followed by washing with PBS to remove the testing reagents. The treatment and washing were repeated two more times. HAE cells were then inoculated with 100 μl of viral stock. Following incubation for 2 h at 32°C, the unbound virus was removed by washing with 500 μl for 10 min at 32°C for three washes, and the HAE cells were maintained at an air-liquid interface for the remainder of the experiment at 32°C. HKU1 replication kinetics were determined at specific time points postinoculation as indicated, 120 μl of PBS was applied to the apical surface of HAE cells, and the apical sample was harvested for RNA isolation after 10 min of incubation at 32°C. The RNA was then analyzed by real-time reverse transcriptase (RT)-PCR to determine viral genomic mRNA copy numbers (20).
RESULTS
S1 domain of hCoV-HKU1 binds to RD cells.
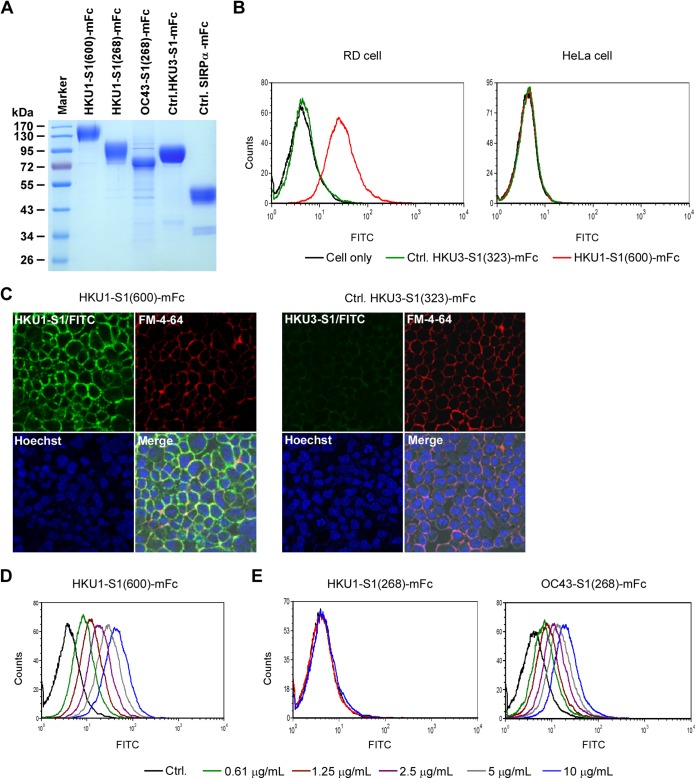
As CoV S1 domains generally mediate the interactions with a cellular receptor(s) to trigger subsequent virus-host cell membrane fusion to initiate viral entry, we first expressed the codon-optimized soluble HKU1 S1 domain (aa 15 to 600) and fused it to the Fc domain from murine IgG2a [HKU1-S1(600)-mFc] (Fig. 1A) to identify the cellular receptor/attachment factor for hCoV-HKU1. As a control, we also expressed the NT of the bat coronavirus HKU3 (29) S1 domain (aa 16 to 323) fused to mFc, HKU3-S1(323)-mFc. To determine, which if any, immortalized cell lines expressed the cellular receptor for hCoV-HKU1, we probed cell lines that were isolated from several different species and tissues with our HKU1-S1 protein using flow cytometry. These cell lines included 293T (human embryonic kidney cells), HeLa (human cervical adenocarcinoma), CHO (Chinese hamster ovary cells), A549 (human lung epithelial adenocarcinoma cells), Caco2 (human epithelial colorectal adenocarcinoma cells), HepG2 (human liver hepatocellular carcinoma cell line), Huh-7 (human hepatoma cells), RD (human rhabdomyosarcoma/muscle tumor cells), HRT-18 (human colon adenocarcinoma cells), Lovo (human colon adenocarcinoma cells), MDCK (Madin-Darby canine kidney cells), and Vero (African green monkey kidney cells). Interestingly, only RD cells showed specific strong binding with 5 μg/ml of HKU1-S1(600)-mFc compared with the control protein (Fig. 1B, left panel); no specific binding was found for any of the other cell lines tested (a representative negative-staining result on HeLa cells is shown in the right panel of Fig. 1B). To independently confirm that HKU1-S1 binds to the surface of RD cells, we incubated cells with either HKU1-S1(600) or HKU3-S1(323) followed by fluorescently labeled secondary antibody and then used FM-4-64, a lipophilic probe that fluoresces intensely upon binding to the outer leaf of the plasma membrane. As shown in the left panel of Fig. 1C, HKU1-S1(600) and FM-4-64 had similar staining patterns on the cell membrane of RD cells, suggesting that both were labeling the surface of the cells. In contrast, no HKU3-S1(323) could be detected on the surface of the RD cells (Fig. 1C, right panel). FACS analysis also showed that the binding of HKU1-S1 with RD cells occurred in a dose-dependent manner (Fig. 1D); the binding was detected at a low concentration of HKU1-S1(600)-mFc protein at 0.61 μg/ml. These results indicate that a cellular attachment factor or receptor(s) for hCoV-HKU1 is present on the surface of the RD cells. We further tested whether the NT of HKU1-S1 can bind with RD cells. The NT (aa 15 to 268) of HKU1-S1 was expressed as a mFc-fusion protein [HKU1-S1(268)-mFc] (Fig. 1A) and was examined for binding with RD cells by FACS analysis. As shown in Fig. 1E, left panel, the NT domain did not bind to RD cells even at a high concentration of 10 μg/ml, suggesting that the binding of HKU1-S1 to RD cells requires regions beyond the NT of S1; the NT domain alone is not sufficient to support the binding. In contrast, the NT of hCoV-OC43-S1(268) protein could bind to RD cells in a dose-dependent manner (Fig. 1E, right panel), but the binding activity was weaker than that of HKU1-S1(600) to RD cells.
FIG 1.
Specific binding of HKU1-S1 to RD cells. (A) SDS-PAGE of expressed recombinant S1 or control (Ctrl.) proteins. All proteins were expressed in 293T cells and purified by the use of protein A Sepharose beads. Purified proteins were run on SDS-PAGE and stained by the use of Coomassie blue. (B) FACS analysis of HKU1-S1(600)-mFc (5 μg/ml) binding to RD and HeLa cells. HKU3-323-mFc was used as a negative-control protein. (C) HKU1-S1(600)-mFc binding to a molecule(s) located on the RD cell surface. Results of immunofluorescence microscopy imaging of RD cells stained by HKU1-S1(600)-mFc or the control protein, HKU3-323-mFc, are shown. Cell membranes were stained with FM-4-64 (red), the nuclei were stained with Hoechst dye 33258 (blue), and the HKU1-S1 staining was detected by an FITC-labeled anti-mouse Fc antibody. (D) HKU1-S1(600)-mFc binding to RD cells in a dose-dependent manner in a FACS analysis. (E) FACS analysis of the N termini of HKU1-S1 and OC43-S1 binding to RD cells. HKU3-323-mFc at 10 μg/ml was used as a control (Ctrl.) in panels D and E. The graphs shown in panels B to E are representative of the results of at least two independent experiments for each panel.
Binding of HKU1-S1 to RD cells is sialic acid dependent.
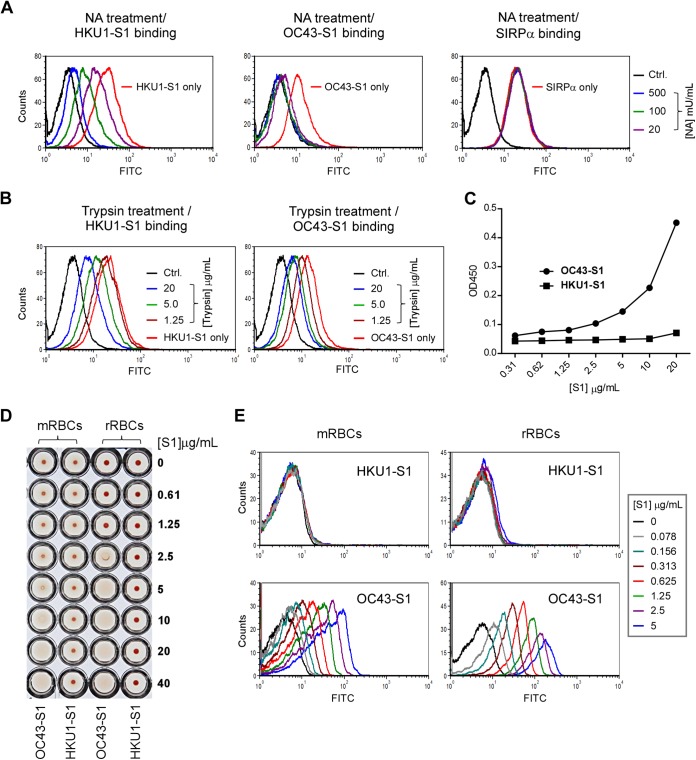
Sialic acids serve as attachment factors or receptors for a number of viruses (28, 30, 31). 9-O-Ac-Sia was found to be essential for viral entry of BCoV and hCoV-OC43 (10, 30). To investigate whether sialic acids are also involved in the binding of HKU1-S1 to RD cells, we first pretreated cells with neuraminidase (NA), a sialidase that removes terminal free or modified sialic acids which are α2,3-, α2,6-, or α2,8-linked to the subterminal residue of a sugar chain. Treated cells were then incubated with 5 μg/ml of HKU1-S1(600)-mFc. As shown in Fig. 2A, left panel, pretreatment with NA at concentrations ranging from 20 to 500 mU/ml markedly reduced the binding of HKU1-S1(600) to RD cells in a dose-dependent manner; 500 mU/ml of NA reduced the binding to about 3% to 5% of the levels observed in the mock-treated cells. Similarly, NA treatment of RD cells resulted in the reduction of OC43-S1(268)-mFc binding (Fig. 2A, middle panel), whereas a control protein, signal regulatory protein alpha (SIRPα), binding to RD cells via its protein receptor, CD47 (32), expressed on the RD cell surface was not affected by NA treatment (Fig. 2A, right panel). This result indicated that cell surface sialic acids participated in the binding of HKU1-S1(600) protein to RD cells. To further test whether sialic acids involved in the binding are attached to glycoprotein(s), RD cells were pretreated with TPCK-trypsin protease and then inoculated with 5 μg/ml of HKU1-S1(600)-mFc. As shown in Fig. 2B, pretreatment with trypsin dose-dependently reduced the binding of HKU1-S1 to RD cells; the maximum dose tested at 20 μg/ml trypsin reduced the binding to about 20% of the levels in the mock-treated cells. Trypsin treatment also similarly reduced binding of OC43-S1 to RD cells. Taken together, these findings suggest that HKU1-S1 protein, similarly to OC43-S1, can bind to sialic acids that are attached to glycoprotein(s).
FIG 2.
Characterization of the binding receptor of HKU1-S1 protein on RD cells by FACS. (A) Pretreatment of RD cells with neuraminidase (NA) greatly reduced HKU1-S1 binding in a dose-dependent manner. RD cells were pretreated with NA at different concentrations as indicated and then stained with 5 μg/ml of HKU1-S1(600)-mFc, OC43 (268)-mFc, or SIRPα-mFc control protein followed by detection with an FITC-labeled anti-mouse Fc antibody. (B) Pretreatment of RD cells with TPCK-treated trypsin reduced HKU1-S1(600) and OC43-S1(268) binding to RD cells. The FACS assay method was similar to that described for panel A. “Ctrl.” indicates RD cells that were stained with HKU1-S1(268)-mFc only in panels A and B. (C) HKU1-S1(600)-mFc did not bind to BSM (containing 9-O-Ac-sia) directly coated on an ELISA plate. OC43-S1 served as a positive control. (D) HKU-S1 did not hemagglutinate mouse RBCs (mRBCs) or rat RBCs (rRBCs). OC43-S1(268)-mFc served as a positive control and showed HA activity in a dose-dependent manner. (E) Binding of HKU1-S1 and OC43-S1 to rat RBCs and mouse RBCs determined by FACS analysis. Data shown are representative of the results of at least two independent experiments for each panel.
Unlike S1 of hCoV-OC43, HKU1-S1 cannot bind to 9-O-acetylated sialic acid-containing glycoprotein or RBCs.
To understand the sialic acid specificity and preference of HKU1-S1, bovine submaxillary mucin (BSM), which mainly contains 9-O-Ac-Sia and 8,9-di-O-Ac-Sia (33), was first tested for binding with HKU-S1 by ELISA. As shown in Fig. 2C, no binding was observed for BSM coated on ELISA plate, whereas the positive-control OC43-S1(268)-mFc bound to BSM under the same tested condition.
Engagement of sialic acid by viruses usually correlates with the capacity to agglutinate red blood cells (RBCs) from different animal species. hCoV-OC43 and influenza C viruses use 9-O-Ac-Sia for attachment, and both viruses consequently have hemagglutination (HA) activity specific for rat and mouse RBCs, which have a high concentration of 9-O-Ac-Sia on their surface (33, 34), but not for human, sheep, or horse RBCs, as they have little to no 9-O-Ac-Sia expressed (10, 35, 36). By the use of OC43-S1(268)-mFc protein as a positive control, both rat and mouse RBCs could be agglutinated dose-dependently by the OC43-S1 protein as expected, but HKU1-S1(600) protein showed no HA activity on RBCs from either species (Fig. 2D). Consistently, HKU1-S1 showed no binding whereas OC43-S1 strongly bound dose-dependently to both RBCs in a FACS analysis (Fig. 2E). These results suggest that hCoV-HKU1 is different from influenza C virus, hCoV-OC43, and BCoV in using 9-O-Ac-Sia as a binding determinant; the presence of 9-O-Ac-Sia alone at least is not sufficient to mediate entry for hCoV-HKU1.
HKU1-HE is an O-acetylesterase and possesses RDE activity.
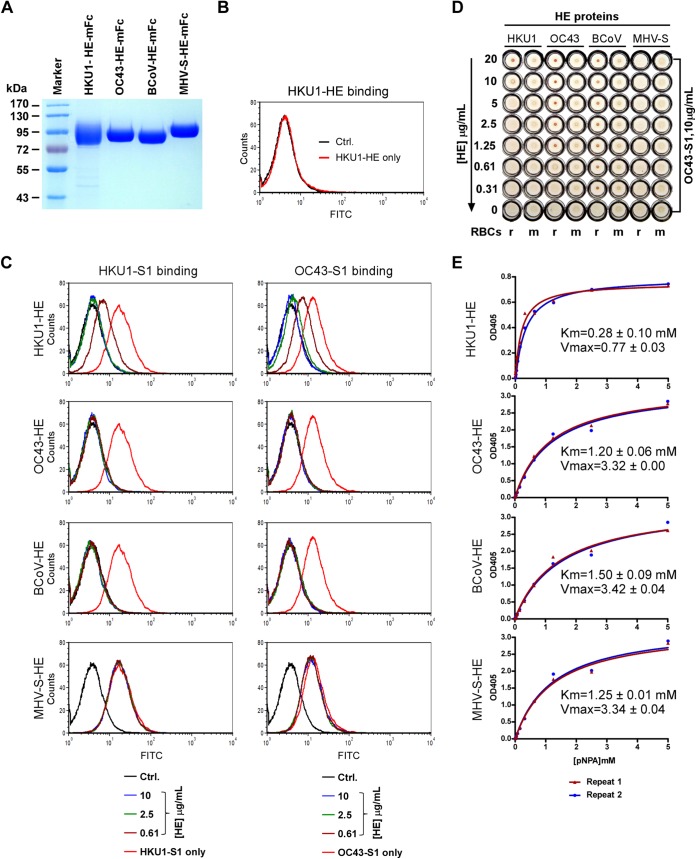
By sequence similarity analysis, the HE protein of HKU1 was predicted to have a hemagglutinin domain and a putative Sia-O-acetyl-esterase active site (15). However, there is only 50% to 57% amino acid conservation between the HKU1-HE and those of other group 2a CoVs. Thus far, no function for HKU1-HE during infection has been demonstrated. Sia-O-Acetylesterases and NAs are two types of viral RDEs identified so far. Sia-O-Acetylesterases, e.g., 9-O-acetylesterase, which was originally found in influenza C viruses, are also represented by the HE proteins of CoVs, including hCoV-OC43, BCoV, and porcine toroviruses (23); NAs are present in influenza A and B viruses. NA removes both free and modified terminal sialic acids from a sugar chain, whereas Sia-O-acetylesterases remove the O-acetyl modifications from sialic acids. To investigate whether HKU1-HE has functions similar to those of other CoVs, acting as a lectin and/or a RDE, we first expressed the extracellular domain of HKU1 HE protein (aa 14 to 358) and fused it to the Fc domain of murine IgG2a (HKU1-HE-mFc) (Fig. 3A). When HKU1-HE-mFc protein was incubated with RD cells, no direct binding was detected (Fig. 3B). This result suggests that HKU1-HE is unlikely to mediate viral attachment. To determine if the HKU1-HE protein has RDE activity, RD cells were pretreated with HKU1-HE-mFc protein and then incubated with HKU1-S1(600)-mFc followed by FACS analysis to determine how much HKU1-S1(600) could still bind to the RD cells. Remarkably, pretreatment of RD cells with HKU1-HE dramatically reduced the binding of S1 to RD cells in a dose-dependent manner (Fig. 3C), similarly to the reduction seen followed NA pretreatment. This indicates that the HKU1-HE serves as a RDE for hCoV-HKU1, possessing enzymatic activities capable of cleaving off the binding determinants for the S protein of HKU1 from the surface of the host cell. We next expressed OC43-HE, BCoV-HE, and MHV-S-HE proteins (Fig. 3A) and compared their RDE activities on RD cells to HKU1-HE's activity in eliminating HKU1-S1 or OC43-S1 binding to the cells. Similarly to HKU1-HE, these HE proteins showed no direct binding to RD cells by FACS analysis (data not shown). Interestingly, HKU1-HE pretreatment also reduced OC43-S1 binding to RD cells and vice versa; pretreatment of cells with OC43-HE blocked not only OC43-S1 binding but also the binding of HKU1-S1 (Fig. 3C). BCoV-HE had the same activities as OC43 in acting as a RDE for both HKU1-S1 and OC43-S1 on RD cells, whereas pretreatment of RD cells with MHV-S-HE, which is a 4-O-acetylesterase, had no effects on the binding of either HKU1-S1 or OC43-S1 (Fig. 3C). Furthermore, the HA activity of OC43-S1 with respect to rat and mouse RBCs was inhibited not only by OC43-HE and BCoV-HE but also by HKU1-HE, whereas MHV-S-HE had no effect (Fig. 3D). These results suggest that HKU1-HE has 9-O-acetylesterase activity similar to that of OC43-HE and BCoV-HE but different from that of MHV-S-HE.
FIG 3.
HKU1-HE is an O-acetylesterase and RDE for HKU1-S1 binding to RD cells. (A) SDS-PAGE of expressed recombinant HE proteins. All proteins were expressed in 293T cells and purified by the use of protein A Sepharose beads. Purified proteins were run on SDS-PAGE and stained by the use of Coomassie blue. (B) HE-mFc protein itself did not bind to RD cells. (C) HKU1-HE acted as a RDE on RD cells for HKU1- and OC43-S1 protein. Pretreatment of RD cells with HKU1-HE as well as with OC43- and BCoV-HE greatly reduced binding of HKU1-S1 or OC43-S1 (at 5 μg/ml) to RD cells in a dose-dependent manner. MHV-S-HE showed no effect. The graphs shown in panels B and C are representative of the results of at least two independent experiments. (D) HKU1-HE acted as a RDE on RBCs for OC43-S1 protein. Pretreatment of rat (r) or mouse (m) RBCs with HKU1-, OC43-, or BCoV-HE inhibited OC43-S1-mediated hemagglutination activity, whereas MHV-S-HE had no effect. Data or images representative of the results of at least two independent experiments are shown for panels A to D. (E) HKU1-HE is an acetylesterase. HEs of HKU1, OC43, BCoV, and MHV-S at 2 μg/ml were used to hydrolyze pNPA (2-fold serially diluted) at room temperature for 15 min. Enzyme activity was assessed by measuring optical density at 405 nm (OD405). The Km and Vmax values were calculated from the Michaelis-Menten enzyme kinetics curve fitting of two independent repeats.
To further confirm that HKU1-HE indeed acts as a RDE solely by its Sia-O-acetylesterase activity, we first determined if HKU1-HE had any neuraminidase activity using an Amplex red neuraminidase assay kit. As expected, HKU1-HE had no detectable NA activity (data not shown). On the other hand, HKU1-HE protein showed strong acetylesterase activity as measured by using chromogenic p-nitrophenyl acetate (pNPA) as the substrate (Fig. 3E). HKU1-HE hydrolyzed pNPA, releasing a para-nitrophenol (pNP) product with a Km value of 0.28 ± 0.1 mM and a Vmax value of 0.77 ± 0.03 in the presence of 2 μg/ml of HKU1-HE protein. Similarly, OC43-HE, BCoV-HE, and MHV-S-HE were measured for acetylesterase activity, and they all showed stronger acetylesterase activity than HKU1-HE (Fig. 3E) with the following parameters: a Km value of 1.20 ± 0.06 mM and a Vmax value of 3.32 ± 0.00 for OC43-HE, a Km of 1.50 ± 0.09 mM and a Vmax of 3.42 ± 0.04 for BCoV-HE, and a Km of 1.25 ± 0.01 mM and a Vmax of 3.34 ± 0.04 for MHV-S-HE, respectively. Considering that HKU1-HE treatment has the same effect as NA treatment of RD cells on the HKU1-S1 binding and that it has no NA activity, it is conceivable that the HKU1-HE mediates RDE through its sialate-9-O-acetylesterase activity similarly to BCoV-HE and OC43-HE.
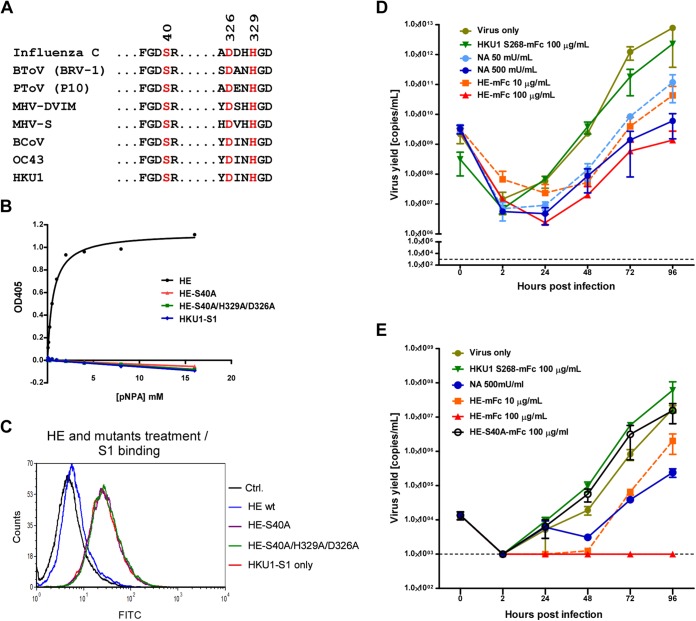
Sequence alignment of HKU1-HE protein against the hemagglutinin-esterase fusion protein (HEF) of influenza C virus and the HEs of hCoV-OC43, BCoV, MHV, and toroviruses revealed that the conserved sialate-O-acetylesterase catalytically active sites (the S40, H329, and D326 catalytic triad [24]) are also present in the HE protein of HKU1 (Fig. 4A). BCoV-HE mutant protein containing a S40A substitution has been demonstrated to be enzymatically inactive (24). To determine if the three amino acids were critical for the acetylesterase activity of HKU1-HE, HE mutants containing a single S40A mutation or triple S40A/H329A/D326A mutations were expressed and tested for their capacity to hydrolyze pNPA substrate. As shown in Fig. 4B, both HE mutants completely lost esterase activity. Furthermore, unlike the wild-type HE protein, pretreatment of RD cells with these acetylesterase-inactive mutant HEs had no effect on HKU1-S1 protein binding to RD cells (Fig. 4C). This result suggests that HKU1-S1 binding required a specific type(s) of O-acetylated sialic acid(s) to be present on the cell surface, which corresponds to the sialic acid acetylesterase specificity of the HKU1-HE. Considering that HKU1-S1 did not bind to 9-O-Ac-containing BSM and RBCs, combined with the result showing that HKU1-HE and OC43-HE mutually served as RDEs for the binding of their S1 proteins to RD cells, it is very likely that the acetyl modification at the 9-O position of sialic acid is a necessary but not sufficient binding determinant for HKU1-S protein. Accordingly, HKU1-HE protein possesses sialate-9-O-acetylesterase activity or even broader sialate-O-acetylesterase activity.
FIG 4.
Treatment of HAE cells with HE or NA but not the enzymatically inactive HE mutant inhibited HKU1 infection. (A) Esterase-catalytic active-site residues in HE. Sequence alignment of amino acids around the catalytically active site (in red) is shown. The BCoV-HE amino acid numbering scheme was used (22). The GenBank accession numbers of HE proteins of BCoV, OC43, HKU1, MHV-DVIM, and influenza C virus are AAA92991.1, AAX85668.1, NC_006577.2, AAC63044.1, and AJ872181, respectively. For HE proteins of MHV-S, bovine torovirus (BToV), and porcine torovirus (PToV) strain p10, the Uniprot accession numbers are P31614, P0C0V9, and Q70KP1, respectively. (B) HKU1-HE proteins with substitutions at catalytically active sites are enzymatically inactive. HKU1-HE or the mutants at 1 μg/ml were incubated with 2-fold serially diluted pNPA at room temperature for 15 min prior to measuring OD405. Each data point represents the OD405 value for HE or its mutants subtracted from that of a negative control. (C) Esterase inactive mutants of HE did not block HKU1-S1 protein binding to RD cells. RD cells were treated with 10 μg/ml of HE or HE mutant proteins prior to HKU1-S1 staining (5 μg/ml). (D) HE and NA pretreatment of HAE cells inhibited HKU1 infection. Prior to HKU1 virus inoculation, HAE cells were pretreated with HE proteins or NA at different concentrations as indicated for 1 h, followed by HKU1 virus inoculation at a high dose as indicated. The replication kinetics of HKU1 virus was assessed in apical washes from infected HAE cultures by real-time RT-PCR. Virus yield is presented as the number of virus RNA copies/ml. (E) HE pretreatment blocked HKU1 infection of HAE cells. HAE cells were pretreated with HE protein or enzymatically inactive HE mutant (S40A) for 1 h prior to viral challenge at a lower dose than that used for the experiment whose results are shown in panel D. The replication kinetics of HKU1 virus was assessed as described for panel D. The dotted line indicates the detection limit of the assay for panels D and E.
HKU1-HE inhibited hCoV-HKU1 infection in tracheobronchial HAE cultures via its RDE activity.
Though HKU1-S protein can bind to RD cells, the lentivirus-based HKU1 spike protein pseudovirus was not able to enter RD cells (data not shown), and previous attempts to culture clinical isolates of HKU1 in RD cells also failed (20). To date, no cell line has been found to be permissive for hCoV-HKU1 infection. Only the human epithelial (HAE) primary cell culture system utilizing well-differentiated human bronchial epithelial cells has been demonstrated to be a robust in vitro model for hCoV-HKU1 infection and propagation (20). HAE cultures have also been successfully used as a model system for studying SARS-CoV, hCoV-NL63, hCoV-229E, MERS-CoV, and hCoV-OC43 (22, 37–39). The infection and propagation of hCoV-HKU1 in the HAE cultures model natural infection of the human upper respiratory tract. To determine whether sialic acids are important during hCoV-HKU1 infection and whether HKU1-HE protein possesses RDE activity in a natural infection model, HAE cells were incubated with NA, HKU1-HE, or control proteins for 1 h and were removed by washing prior to hCoV-HKU1 virus inoculation. Apical washes of infected cultures were collected over time until 96 h postinoculation for RNA isolation, and the number of viral genomic RNA copies was analyzed by real-time RT-PCR to determine the level of viral infection. As shown in Fig. 4D, both NA pretreatment and HKU1-HE pretreatment of HAE cells markedly inhibited hCoV-HKU1 infection. HKU1-HE at 100 μg/ml reduced viral titers by 2 to 3 logs at 48, 72, and 96 h post-viral inoculation. NA also showed dose-dependent inhibition of viral infection, though it was not as efficient as that seen with HE protein. Preincubation of HAE cells with HKU1-HE protein inhibited viral replication, suggesting that HKU1-HE can destroy the sialic acid moieties required for hCoV-HKU1 entry. When a lower titer of HKU1 virus inocula was used, HKU1-HE protein at 100 μg/ml completely blocked hCoV-HKU1 replication in HAE cells, whereas an enzymatically inactive HE variant, HKU1-HE-S40A, showed no inhibition activity (Fig. 4E). These results demonstrate that hCoV-HKU1 uses O-acetylated sialic acids as an attachment factor, that this interaction is required for efficient infection of the target cell, and that HKU1-HE protein possesses sialate-O-acetylesterase RDE activity.
DISCUSSION
Sialic acid, a 9-carbon monosaccharide, includes a large number of derivatives arising from differential modifications of the parental molecule as well as various glycosidic linkages (e.g., α2,3 and α2,6) to the subterminal residue of a sugar chain. O-Acetylation is one of the most common types of sialic acid modification. It can occur at all the four hydroxyl groups of sialic acids at positions of C4, C7, C8, and C9 and generates mostly mono-O-acetylated but also oligo-O-acetylated sialic acids at more than one position. O-Ac-Sia plays fundamental roles in many biological and pathophysiological events (40). The 9-O-Ac-Sia serves as a receptor determinant for several members of group 2a CoVs, including the closely related BCoV, hCoV-OC43, and porcine hemagglutinating encephalomyelitis virus (PHEV) (10, 30, 41). The binding with 9-O-Ac-Sia is essential for these viruses to initiate infection, and their S protein is the major viral protein responsible for the binding. In this study, we found that the S protein of hCoV-HKU1 can also recognize O-Ac-Sia but only those presented on RD cells among the many cell lines tested. Differently from the aforementioned CoVs in the same group, no binding of hCoV-HKU1 S1 with 9-O-Ac-Sia-containing BSM as well as RBCs from mouse and rat could be detected. In addition, a previous study (42) and our data (Fig. 1E) both demonstrated that the NT of HKU1-S1 was unable to bind with carbohydrate moieties. In contrast, the carbohydrate receptor binding domains for hCoV-OC43 and BCoV were located in the NT of S1 (Fig. 2) (42). On the other hand, for hCoV-HKU1, as well as for other 9-O-Ac-Sia recognition-dependent CoVs, the issue remains of whether, in addition to O-Ac-Sia, they also interact with a protein receptor during the entry process. O-Ac-Sia on RD cells can be recognized by hCoV-HKU1 S1 protein; however, the cells are not permissive for viral infection. One explanation for this is the lack of a protein receptor for hCoV-HKU1 on RD cells. In line with this, our attempts to use HKU1-S1(600) as a viral ligand protein for immunoprecipitation combined with mass spectrometric identification did not find a protein(s) specifically binding to HKU1-S1 (data not shown). It is also possible that there is another molecule(s) present only in HAE cell cultures but not on RD cells, which are important for viral infection at a later stage, e.g., for membrane fusion or viral replication, or that a restriction factor(s) may exist in RD cells to limit viral infection.
Among CoVs, HE protein is present only in members of group 2a CoVs. Sequence and structural similarities suggest that CoV HE evolved from the HEF protein of influenza C virus (24). Although the dual function of HEF (O-Ac-Sia receptor binding and sialate-O-acetylesterase activity) was maintained in some CoVs, the HE appears to mainly function as a RDE in these CoVs. Comparing to the essential role of S protein in Sia-receptor binding and mediating viral entry, the Sia binding activity of HE seems to be an accessory function and its affinity and Sia preference characteristics differ among CoV strains (23, 43). HEs of two closely related MHV field strains, MHV-DVIM and MHV-S, recognize two different types of O-Ac-Sia, 9-O-Ac-Sia and 4-O-Ac-Sia, respectively, whereas many MHV laboratory strains carry defective HE genes (27, 28). hCoV-OC43 HE lost its Sia binding activity although it has high (97%) sequence identity with the HE of BCoV (Mebus stain), which exhibits high Sia binding affinity (43). Similarly, we did not find that HKU1-HE has O-Ac-Sia binding activity. This is consistent with the observation described previously by Langereis et al. that the HE of hCoV-HKU1 failed to hemagglutinate erythrocytes and bind to O-Ac-Sia (43). Sequence comparison of HKU1-HE with HEF of influenza C virus and HEs of CoVs with known protein structures demonstrated that HKU1-HE was the most divergent one at the Sia binding loops (23, 43), whereas the Sia-O-acetylesterase domain is highly conserved among them. The key residues contributing to the catalytic activity of HEF and other CoV HEs, including the Ser-His-Asp catalytic triad, the oxyanion hole-contributing residues Gly85 and Asn117 in HEF, and an Arg322 residue in HEF important for Sia substrate binding, are completely conserved in hCoV-HKU1 (23). In our study, HKU1-HE indeed showed strong O-AC-esterase activity with pNPA substrate, and the Ser-His-Asp catalytic triad mutant HEs completely lost this activity. We demonstrated that the sialic acids expressed by RD cells not only are specifically recognized by the HKU1-S1 protein but also are substrates for HE protein. Wild-type but not mutant HE treatment of RD cells showed effects similar to those seen with neuraminidase and abolished the subsequent binding of S1 to RD cells. These results indicate that the S1 protein binds with O-Ac-Sia and that the HE has matching or even broader esterase activity.
Langereis et al. (43) reported that the HKU1-HE, like the BCoV-HE, displayed Sia-9-O-Ac-esterase activity using a synthetic 4,9-di-O-Ac-Sia substrate analogue. Consistently, we demonstrated that HKU1-HE had RDE activity similar to that seen with OC43-HE and BCoV-HE with respect to removal of the binding moiety from RD cells for S1 proteins of both HKU1 and OC43. These results strongly support the idea that HKU1-HE has Sia-9-O-Ac-esterase activity similar to that of OC43-HE and BCoV-HE. However, unlike the results seen with S1 of OC43, Sia-9-O-AC binding activity was not detected for the S1 of hCoV-HKU1 by BSM binding and erythrocyte hemagglutination assays, which are standard methods for examining the usage of Sia-9-O-AC as a receptor by other CoVs (Fig. 2C to E). Thus, it is likely that HKU1 is different from OC43 and BCoV in terms of the use of Sia-9-O-AC as a receptor via its Spike protein. Sia-9-O-AC may be required for but not sufficient to support the HKU1-S1 binding. In addition of Sia-9-O-AC, RD cells may express other types of O-acetylated sialic acid that are lacking or at a lower level in BSM and at the erythrocyte cell surface but required for HKU1-S1 recognition. One may also speculate that certain examples of di-O-Ac-Sia, tri-O-Ac-Sia, or oligo-O-acetylated Sia in which all have an acetyl group at C9 (9-O-AC) in common or a certain particular sugar chain core structure(s) to which Sia-9-O-Ac is attached or the linkage of sialic acid to the penultimate residue of a sugar chain may also be required.
Finally, in HAE cultures, we demonstrated that NA and HKU1-HE but not an enzymatically inactive HE mutant dramatically reduced virus infection or completely blocked infection when a lower viral challenge dose was applied. The results of treatment of HAE cells with NA and HKU1-HE prior to infection strongly suggested that the Sia-9-O-AC-esterase activity of HE acted as a RDE and removed the critical receptor binding moieties so that the early viral entry was impaired. Considering that the HAE cells continuously secrete a large amount of mucus, the effect of inhibition of viral infection by pretreatment of the cells with NA and HE is remarkable and suggests an essential role for sialic acids in the initiation of infection. Our study results also suggest that acetyl modification at 9-O of sialic acid may be a necessary but not sufficient receptor or attachment factor determinant and warrant further investigation to determine the fine specificity and preference of sialic acids recognized by HKU1-S protein. Nevertheless, for the first time, this study provided experimental evidence to support the idea that O-Ac-Sia, by interacting with S1 of hCoV-HKU1, serves as an essential determinant for viral attachment during the early entry step and that HE possesses 9-O-AC-esterase or even broader activity and primarily acts as a RDE for hCoV-HKU1 infection. hCoV-HKU1 is similar to BCoV and hCoV-OC43, employing its two surface proteins, S and HE, to complete the viral infection cycle in a concerted manner, with S protein mediating receptor binding and entry and HE protein mediating RDE activity late in the infection cycle to facilitate viral progeny release and achieve efficient virus dissemination (23, 26).
ACKNOWLEDGMENTS
This work was supported by grants from the Ministry of Science and Technology, China, to J.S. (2012CB837602) and to W.L. (2010CB530101), from the Science and Technology Bureau of Beijing Municipal Government to W.L. and J.S., from the Thousand Young Talents Program, China, to J.S., from the National Centre for Research and Development, Poland (Lider/27/55/L-2/10/2011), and from the National Science Center, Poland (UMO-2012/07/E/NZ6/01712), to K.P., and from NIH (U19 AI109761) to R.S.B. and NIH (AI085524) to W.A.M. and R.S.B.
REFERENCES
- 1.Graham RL, Donaldson EF, Baric RS. 2013. A decade after SARS: strategies for controlling emerging coronaviruses. Nat Rev Microbiol 11:836–848. doi: 10.1038/nrmicro3143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rota PA, Oberste MS, Monroe SS, Nix WA, Campagnoli R, Icenogle JP, Penaranda S, Bankamp B, Maher K, Chen M-h, Tong S, Tamin A, Lowe L, Frace M, DeRisi JL, Chen Q, Wang D, Erdman DD, Peret TCT, Burns C, Ksiazek TG, Rollin PE, Sanchez A, Liffick S, Holloway B, Limor J, McCaustland K, Olsen-Rasmussen M, Fouchier R, Gunther S, Osterhaus ADME, Drosten C, Pallansch MA, Anderson LJ, Bellini WJ. 2003. Characterization of a novel coronavirus associated with severe acute respiratory syndrome. Science 300:1394–1399. doi: 10.1126/science.1085952. [DOI] [PubMed] [Google Scholar]
- 3.Ksiazek TG, Erdman D, Goldsmith CS, Zaki SR, Peret T, Emery S, Tong S, Urbani C, Comer JA, Lim W, Rollin PE, Dowell SF, Ling AE, Humphrey CD, Shieh WJ, Guarner J, Paddock CD, Rota P, Fields B, DeRisi J, Yang JY, Cox N, Hughes JM, LeDuc JW, Bellini WJ, Anderson LJ; SARS Working Group . 2003. A novel coronavirus associated with severe acute respiratory syndrome. N Engl J Med 348:1953–1966. doi: 10.1056/NEJMoa030781. [DOI] [PubMed] [Google Scholar]
- 4.Anderson LJ, Tong S. 2010. Update on SARS research and other possibly zoonotic coronaviruses. Int J Antimicrob Agents 36(Suppl 1):S21–S25. doi: 10.1016/j.ijantimicag.2010.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Assiri A, McGeer A, Perl TM, Price CS, Al Rabeeah AA, Cummings DA, Alabdullatif ZN, Assad M, Almulhim A, Makhdoom H, Madani H, Alhakeem R, Al-Tawfiq JA, Cotten M, Watson SJ, Kellam P, Zumla AI, Memish ZA. 2013. Hospital outbreak of Middle East respiratory syndrome coronavirus. N Engl J Med 369:407–416. doi: 10.1056/NEJMoa1306742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zaki AM, van Boheemen S, Bestebroer TM, Osterhaus AD, Fouchier RA. 2012. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med 367:1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- 7.Coleman CM, Frieman MB. 2014. Coronaviruses: important emerging human pathogens. J Virol 88:5209–5212. doi: 10.1128/JVI.03488-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heald-Sargent T, Gallagher T. 2012. Ready, set, fuse! The coronavirus spike protein and acquisition of fusion competence. Viruses 4:557–580. doi: 10.3390/v4040557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yeager CL, Ashmun RA, Williams RK, Cardellichio CB, Shapiro LH, Look AT, Holmes KV. 1992. Human aminopeptidase N is a receptor for human coronavirus 229E. Nature 357:420–422. doi: 10.1038/357420a0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vlasak R, Luytjes W, Spaan W, Palese P. 1988. Human and bovine coronaviruses recognize sialic acid-containing receptors similar to those of influenza C viruses. Proc Natl Acad Sci U S A 85:4526–4529. doi: 10.1073/pnas.85.12.4526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hofmann H, Pyrc K, van der Hoek L, Geier M, Berkhout B, Pohlmann S. 2005. Human coronavirus NL63 employs the severe acute respiratory syndrome coronavirus receptor for cellular entry. Proc Natl Acad Sci U S A 102:7988–7993. doi: 10.1073/pnas.0409465102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li W, Moore MJ, Vasilieva N, Sui J, Wong SK, Berne MA, Somasundaran M, Sullivan JL, Luzuriaga K, Greenough TC, Choe H, Farzan M. 2003. Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature 426:450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Milewska A, Zarebski M, Nowak P, Stozek K, Potempa J, Pyrc K. 3 September 2014. Human coronavirus NL63 utilize heparan sulfate proteoglycans for attachment to target cells. J Virol doi: 10.1128/JVI.02078-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lu G, Hu Y, Wang Q, Qi J, Gao F, Li Y, Zhang Y, Zhang W, Yuan Y, Bao J, Zhang B, Shi Y, Yan J, Gao GF. 2013. Molecular basis of binding between novel human coronavirus MERS-CoV and its receptor CD26. Nature 500:227–231. doi: 10.1038/nature12328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Woo PC, Lau SK, Chu CM, Chan KH, Tsoi HW, Huang Y, Wong BH, Poon RW, Cai JJ, Luk WK, Poon LL, Wong SS, Guan Y, Peiris JS, Yuen KY. 2005. Characterization and complete genome sequence of a novel coronavirus, coronavirus HKU1, from patients with pneumonia. J Virol 79:884–895. doi: 10.1128/JVI.79.2.884-895.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jevšnik M, Uršič T, Zigon N, Lusa L, Krivec U, Petrovec M. 2012. Coronavirus infections in hospitalized pediatric patients with acute respiratory tract disease. BMC Infect Dis 12:365. doi: 10.1186/1471-2334-12-365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dominguez SR, Shrivastava S, Berglund A, Qian Z, Goes LG, Halpin RA, Fedorova N, Ransier A, Weston PA, Durigon EL, Jerez JA, Robinson CC, Town CD, Holmes KV. 2014. Isolation, propagation, genome analysis and epidemiology of HKU1 betacoronaviruses. J Gen Virol 95:836–848. doi: 10.1099/vir.0.059832-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lau SK, Woo PC, Yip CC, Tse H, Tsoi HW, Cheng VC, Lee P, Tang BS, Cheung CH, Lee RA, So LY, Lau YL, Chan KH, Yuen KY. 2006. Coronavirus HKU1 and other coronavirus infections in Hong Kong. J Clin Microbiol 44:2063–2071. doi: 10.1128/JCM.02614-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Woo PC, Lau SK, Yip CC, Huang Y, Yuen KY. 2009. More and more coronaviruses: human coronavirus HKU1. Viruses 1:57–71. doi: 10.3390/v1010057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pyrc K, Sims AC, Dijkman R, Jebbink M, Long C, Deming D, Donaldson E, Vabret A, Baric R, van der Hoek L, Pickles R. 2010. Culturing the unculturable: human coronavirus HKU1 infects, replicates, and produces progeny virions in human ciliated airway epithelial cell cultures. J Virol 84:11255–11263. doi: 10.1128/JVI.00947-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dominguez SR, Travanty EA, Qian Z, Mason RJ. 2013. Human coronavirus HKU1 infection of primary human type II alveolar epithelial cells: cytopathic effects and innate immune response. PLoS One 8:e70129. doi: 10.1371/journal.pone.0070129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dijkman R, Jebbink MF, Koekkoek SM, Deijs M, Jonsdottir HR, Molenkamp R, Ieven M, Goossens H, Thiel V, van der Hoek L. 2013. Isolation and characterization of current human coronavirus strains in primary human epithelial cell cultures reveal differences in target cell tropism. J Virol 87:6081–6090. doi: 10.1128/JVI.03368-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.de Groot RJ. 2006. Structure, function and evolution of the hemagglutinin-esterase proteins of corona- and toroviruses. Glycoconj J 23:59–72. doi: 10.1007/s10719-006-5438-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zeng Q, Langereis MA, van Vliet AL, Huizinga EG, de Groot RJ. 2008. Structure of coronavirus hemagglutinin-esterase offers insight into corona and influenza virus evolution. Proc Natl Acad Sci U S A 105:9065–9069. doi: 10.1073/pnas.0800502105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vijgen L, Keyaerts E, Moes E, Thoelen I, Wollants E, Lemey P, Vandamme AM, Van Ranst M. 2005. Complete genomic sequence of human coronavirus OC43: molecular clock analysis suggests a relatively recent zoonotic coronavirus transmission event. J Virol 79:1595–1604. doi: 10.1128/JVI.79.3.1595-1604.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Desforges M, Desjardins J, Zhang C, Talbot PJ. 2013. The acetyl-esterase activity of the hemagglutinin-esterase protein of human coronavirus OC43 strongly enhances the production of infectious virus. J Virol 87:3097–3107. doi: 10.1128/JVI.02699-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Langereis MA, van Vliet AL, Boot W, de Groot RJ. 2010. Attachment of mouse hepatitis virus to O-acetylated sialic acid is mediated by hemagglutinin-esterase and not by the spike protein. J Virol 84:8970–8974. doi: 10.1128/JVI.00566-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Langereis MA, Zeng Q, Heesters BA, Huizinga EG, de Groot RJ. 2012. The murine coronavirus hemagglutinin-esterase receptor-binding site: a major shift in ligand specificity through modest changes in architecture. PLoS Pathog 8:e1002492. doi: 10.1371/journal.ppat.1002492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lau SK, Woo PC, Li KS, Huang Y, Tsoi HW, Wong BH, Wong SS, Leung SY, Chan KH, Yuen KY. 2005. Severe acute respiratory syndrome coronavirus-like virus in Chinese horseshoe bats. Proc Natl Acad Sci U S A 102:14040–14045. doi: 10.1073/pnas.0506735102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schwegmann-Wessels C, Herrler G. 2006. Sialic acids as receptor determinants for coronaviruses. Glycoconj J 23:51–58. doi: 10.1007/s10719-006-5437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ströh LJ, Stehle T. 2014. Glycan engagement by viruses: receptor switches and specificity. Annu Rev Virol 1:285–306. doi: 10.1146/annurev-virology-031413-085417. [DOI] [PubMed] [Google Scholar]
- 32.Barclay AN, Van den Berg TK. 2014. The interaction between signal regulatory protein alpha (SIRPalpha) and CD47: structure, function, and therapeutic target. Annu Rev Immunol 32:25–50. doi: 10.1146/annurev-immunol-032713-120142. [DOI] [PubMed] [Google Scholar]
- 33.Ravindranath MH, Higa HH, Cooper EL, Paulson JC. 1985. Purification and characterization of an O-acetylsialic acid-specific lectin from a marine crab Cancer antennarius. J Biol Chem 260:8850–8856. [PubMed] [Google Scholar]
- 34.Traving C, Schauer R. 1998. Structure, function and metabolism of sialic acids. Cell Mol Life Sci 54:1330–1349. doi: 10.1007/s000180050258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rogers GN, Herrler G, Paulson JC, Klenk HD. 1986. Influenza C virus uses 9-O-acetyl-N-acetylneuraminic acid as a high affinity receptor determinant for attachment to cells. J Biol Chem 261:5947–5951. [PubMed] [Google Scholar]
- 36.Bulai T, Bratosin D, Pons A, Montreuil J, Zanetta JP. 2003. Diversity of the human erythrocyte membrane sialic acids in relation with blood groups. FEBS Lett 534:185–189. doi: 10.1016/S0014-5793(02)03838-3. [DOI] [PubMed] [Google Scholar]
- 37.Banach B, Orenstein JM, Fox LM, Randell SH, Rowley AH, Baker SC. 2009. Human airway epithelial cell culture to identify new respiratory viruses: coronavirus NL63 as a model. J Virol Methods 156:19–26. doi: 10.1016/j.jviromet.2008.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mossel EC, Wang J, Jeffers S, Edeen KE, Wang S, Cosgrove GP, Funk CJ, Manzer R, Miura TA, Pearson LD, Holmes KV, Mason RJ. 2008. SARS-CoV replicates in primary human alveolar type II cell cultures but not in type I-like cells. Virology 372:127–135. doi: 10.1016/j.virol.2007.09.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Scobey T, Yount BL, Sims AC, Donaldson EF, Agnihothram SS, Menachery VD, Graham RL, Swanstrom J, Bove PF, Kim JD, Grego S, Randell SH, Baric RS. 2013. Reverse genetics with a full-length infectious cDNA of the Middle East respiratory syndrome coronavirus. Proc Natl Acad Sci U S A 110:16157–16162. doi: 10.1073/pnas.1311542110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schauer R, Schmid H, Pommerencke J, Iwersen M, Kohla G. 2001. Metabolism and role of O-acetylated sialic acids. Adv Exp Med Biol 491:325–342. doi: 10.1007/978-1-4615-1267-7_21. [DOI] [PubMed] [Google Scholar]
- 41.Vijgen L, Keyaerts E, Lemey P, Maes P, Van Reeth K, Nauwynck H, Pensaert M, Van Ranst M. 2006. Evolutionary history of the closely related group 2 coronaviruses: porcine hemagglutinating encephalomyelitis virus, bovine coronavirus, and human coronavirus OC43. J Virol 80:7270–7274. doi: 10.1128/JVI.02675-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Peng G, Sun D, Rajashankar KR, Qian Z, Holmes KV, Li F. 2011. Crystal structure of mouse coronavirus receptor-binding domain complexed with its murine receptor. Proc Natl Acad Sci U S A 108:10696–10701. doi: 10.1073/pnas.1104306108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Langereis MA. 2011. Viral hemagglutinin-esterases; mediators of dynamic virion-glycan interactions. Ph.D. thesis University of Utrecht, Utrecht, Netherlands: http://dspace.library.uu.nl/handle/1874/211181. [Google Scholar]