Abstract
Background
Difficult airway cases can quickly become emergencies, increasing the risk of life-threatening complications or death. Emergency airway management outside the operating room is particularly challenging.
Methods
We developed a quality improvement program—the Difficult Airway Response Team (DART)—to improve emergency airway management outside the operating room. DART was implemented by a team of anesthesiologists, otolaryngologists, trauma surgeons, emergency medicine physicians, and risk managers in 2005 at The Johns Hopkins Hospital in Baltimore, Maryland. The DART program had three core components: operations, safety, and education. The operations component focused on developing a multidisciplinary difficult airway response team, standardizing the emergency response process, and deploying difficult airway equipment carts throughout the hospital. The safety component focused on real-time monitoring of DART activations and learning from past DART events to continuously improve system-level performance. This objective entailed monitoring the paging system, reporting difficult airway events and DART activations to a web-based registry, and using in situ simulations to identify and mitigate defects in the emergency airway management process. The educational component included development of a multispecialty difficult airway curriculum encompassing case-based lectures, simulation, and team building/communication to ensure consistency of care. Educational materials were also developed for non-DART staff and patients to inform them about the needs of patients with difficult airways and ensure continuity of care with other providers after discharge.
Results
Between July 2008 and June 2013, DART managed 360 adult difficult airway events comprising 8% of all code activations. Predisposing patient factors included body mass index > 40, history of head and neck tumor, prior difficult intubation, cervical spine injury, airway edema, airway bleeding, and previous or current tracheostomy. Twenty-three patients (6%) required emergent surgical airways. Sixty-two patients (17%) were stabilized and transported to the operating room for definitive airway management. There were no airway management-related deaths, sentinel events, or malpractice claims in adult patients managed by DART. Five in situ simulations conducted in the first program year improved DART's teamwork, communication, and response times and increased the functionality of the difficult airway carts. Over the 5-year period, we conducted 18 airway courses, through which more than 200 providers were trained.
Conclusions
DART is a comprehensive program for improving difficult airway management. Future studies will examine the comparative effectiveness of the DART program and evaluate how DART has impacted patient outcomes, operational efficiency, and costs of care.
Introduction
Difficult airway cases can quickly become emergencies, increasing the risk of life-threatening complications or death.1,2 In a 2005 closed claims analysis, brain injury or death was cited in over half of claims for perioperative care and in all claims for events occurring outside the operating room. Morever, payments for these claims ranged from $2,200 to $8,500,000.3
The American Society of Anesthesiologists (ASA) published its initial practice guidelines for difficult airway management in 1993,4 with follow-up revisions in 20035 and 2013.6 The 2013 ASA practice guidelines describe a difficult airway as a clinical situation in which a conventionally trained anesthesiologist experiences difficulty with mask ventilation, tracheal intubation, or both.6 A difficult airway thus represents a complex interaction between patient factors, the clinical setting, and the provider's skills.6
Emergency airway management outside the OR is particularly challenging, with the incidence of difficult intubation ranging from 9 to 12%7-10 and a complication rate ranging from 4.2 to 28%.7,8,10 Unfortunately, it is not easy to predict whether a patient has a difficult airway. A meta-analysis by Shiga et al.11 revealed poor to moderate diagnostic accuracy of five bedside screening tests for predicting difficult intubation in patients with apparently normal anatomy. The authors also found a 6.2% incidence of difficult intubation in nonobese, nonobstetric patients with no airway pathology.
In Maryland hospitals, adverse airway events consistently rank among the top five adverse event types.12 Between 2005 and 2008, 44 adverse airway events were reported in Maryland, all of which resulted in death or anoxic brain injury (Anne Jones, RN, BSN, MA, Department of Health and Mental Hygience, Personal Communication, January 10, 2014). An analysis of adverse airway events at our institution over the same time period revealed that all events occurred outside of the OR, and involved the disciplines of anesthesiology, otolaryngology, trauma surgery, and emergency medicine. Important contributing factors across these events were ineffective provider-to-provider communication, an outdated paging system, unreliable access to difficult airway equipment and to clinicians trained or skilled in performing airway procedures, and unclear roles within the multidisciplinary team during events.
In response to these findings, we established a program to improve hospital-wide emergency airway management in 2005. This program—the Difficult Airway Response Team (DART)—required a year and a half for development and has operated successfully since then. The objectives of this paper are to describe the development and implementation of the DART program, to explain its structure and function, and to summarize the characteristics of patients managed by DART during the first 5 years of operation. We describe contextual factors related to the implementation of DART to allow anesthesiologists, airway experts in other specialities, and quality improvement researchers to ask: “Can this program be implemented in or adapted to my/our organization?”
Methods
The institutional review board of the Johns Hopkins University School of Medicine (NA_00089582) reviewed the quality improvement project, deemed it exempt, and waived the need for informed consent.
Design and Setting
This article describes the implementation of the DART program and the characteristics and outcomes of patients who required a DART activation between July 2008 and June 2013 at The Johns Hopkins Hospital in Baltimore, Maryland, an urban tertiary care teaching hospital. The institution has 1,059 licensed patient beds, 46,864 inpatient admissions, and 421,933 outpatient encounters annually.
Difficult Airway Management Before DART
Management in the Operating Room
Between 1991 and 1993, the Departments of Anesthesiology and Critical Care Medicine (ACCM) and Otolaryngology—Head and Neck Surgery (OHNS) jointly created an airway management initiative in the OR and formed a hospital-wide airway program.13 The program included: (1) a multidisciplinary service with joint clinical faculty appointments, (2) preoperative evaluation and identification of “airway alert” patient status, (3) formulation of intra and postoperative patient airway management plans, (4) standardization of difficult airway carts maintained by the anesthesia department, and creation of an adult airway emergercy cart containing specialized surgical equipment, (5) OHNS nursing staff, surgical technologists, and airway equipment specialists, (6) nursing critical care pathways for patients with difficult airways, (7) in-hospital difficult airway alert wristbands and chart labels, and (8) electronic medical record (EMR) Anesthesiology Consultant Report, Difficult Airway note, and Difficult Airway “alert.” A standardized anesthesia difficult airway cart was specifically designed for emergency and elective use in the OR. This cart included 3.5-mm and 6.0-mm fiberoptic bronchoscopes, lighted stylets, subglottic airways, an Eschmann intubation stylet, an Aintree intubation catheter, a disposable cricothyrotomy kit, and a jet ventilator. In conjunction with OHNS surgeons and nurses, we developed a second surgical emergency airway cart for use by the OHNS surgeons during emergency airway events. This cart included rigid laryngoscopes and bronchoscopes, fiberoptic bronchoscopes, and emergency surgical airway equipment and was organized as a single flat-surface cart without drawers but with equipment assembled for immediate use. When a “stat” airway was called in the OR, our practice was to have the anesthesia attending coordinator respond with the anesthesia difficult airway cart. The OHNS surgeon would be contacted separately. If the surgeon was in a noncritical portion of surgery in the same OR suite, he/she would would respond to the stat call. The OHNS nurse delivered the surgical emergency airway cart to the specific OR in the suite.
Management outside the Operating Room
While the multidisciplinary response program worked efficiently in the OR, issues remained in non-OR areas—intensive care units, inpatient floors, remote procedural areas, and the Emergency Department. Historically, in these non-OR areas a traditional code team managed patients with difficult airway 24 hours per day, 7 days per week, and were activated using a paging system. The code team consisted of senior residents (from anesthesiology, internal medicine, and general surgery), a respiratory therapist, nurse manager, pharmacist, and chaplain. The code equipment included a hospital-wide fleet of standardized code carts that contained basic airway equipment (MAC/Miller laryngoscopes, tracheostomy kit), defibrillator, disposable airway and vascular accesss supplies, and a full compliment of resuscitative medications for bolus or infusions. When a code was activated, the charge nurse on the unit delegated one of the support associates to transport the cart to the patient's bedside. The anesthesia resident carried a backpack with additional airway equipment such as supraglottic airway devices, elastic gum bougies, and a medication box that included sedatives, paralytics, local anesthetics that were non-controlled substances and a full array of resuscitative medications for bolus injections.
While an attending anesthesiologist was always immediately available for any code call, the attending would only be requested for back up if an unexpected difficulty with airway management was encountered. This request usually involved a second page. Upon arrival, if the attending anesthesiologist determined that the surgical emergency airway cart and/or additional expertise was needed then additional pages were sent to mobilize resources and personnel, potentially resulting in a delay in managing the difficult airway. Consequently, we expanded our airway service to include additional surgical emergency airway carts for use in non-OR areas. Following this change, when a code was called from a non-OR area and the code team had difficulty managing the airway, the OR suite was called for delivery of the surgical emergency airway cart to the bedside. However, we still had to make additional calls to bring the OHNS senior resident or attending surgeon to the site in the event that the code team needed assistance.
Comprehensive review of the adverse airway events that occurred in the non-OR areas revealed:
Inconsistent communication processes, including paging issues and delays
Lack of knowledge among providers in non-OR areas on when and how to activate airway support
Limited accessibility and availability of surgical emergency airway cart from the OR
Inconsistent availability of additional experienced attending physicians
Lack of clear roles during difficult airway events
Lack of familiarity with specialized airway techniques
Concerns regarding residents' training and experience
These findings suggested the need for, and resulted in, development of a comprehensive quality improvement program to expand our existing difficult airway management system.
Development of a DART Program
In order to address the identified issues, a formal DART program was proposed in 2005 and expanded to include trauma surgery and emergency medicine. This program was designed to: (1) identify difficult airway patients proactively, (2) mobilize physicians and support staff consistently and efficiently, (3) deliver functional OHNS equipment within defined time metrics, (4) implement appropriate airway algorithms, (5) document airway techniques used, and (6) disseminate airway information to healthcare providers. The DART program was specifically designed not to supplant or duplicate the roles of other hospital-based response teams, such as code or rapid response teams, but rather to leverage the resources of these teams and build off existing systems whenever possible.
The business proposal for this DART program was jointly funded in 2008 by the Patient Safety Committee of our institution and by the four departments involved in the initiative: ACCM, OHNS, Surgery, and Emergency Medicine (EM). The business plan was crucial to defining the expansion of clinical operations necessary to address aforementioned systems issues, streamlining operations, and ensuring that each stakeholder department shared accountability for success. Other team members included: (1) a risk manager to prospectively identify and mitigate risk, (2) a human factors engineer to identify safety hazards, (3) a patient safety officer, 4) a clinical coordinator to manage on-call schedules for DART members, (5) respiratory therapists, (6) equipment specialists, and (7) nurses.
The DART program had three core components: operations, safety, and education. All three components were implemented from inception and are described in the following sections.
Operations
The operations component focused on: (1) identifying clinical personnel to staff DART, (2) developing an emergency response process, including indications for activation of DART, (3) deploying difficult airway carts with critical airway equipment and supplies (“DART carts”), and (4) establishing documentation standards for patients with difficult airways.
The clinical personnel present at each event include an attending anesthesiologist, otolaryngologist (available in-house between 7 AM and 5 PM and home call from 5 PM to 7 AM), and trauma surgeon (in-house). An attending EM physician is present when a difficult airway occurs in the emergency department. A senior resident from each department is also present. Thus, at any given time, at least two but up to four attendings are present 24/7. Overall, approximately thirty anesthesiologists, six otolaryngologists, five trauma surgeons, and four EM physicians staff the DART program along with their senior residents.
The DART is activated via a standardized emergency paging system and triage protocol. When a patient requires emergent airway management, a code team or a rapid response team is activated with an expected response time of less than 5 minutes. The code team intubates non-difficult airways. If the airway is found to be more complex than expected or the code team is unable to establish an airway successfully, DART is activated (Figure 1). An operational metric for the DART personnel and cart to arrive on site is within 10 minutes of the DART page. If the patient is known to have a difficult airway, the DART team is activated simultaneously as part of the initial code or rapid response team.
Figure 1.
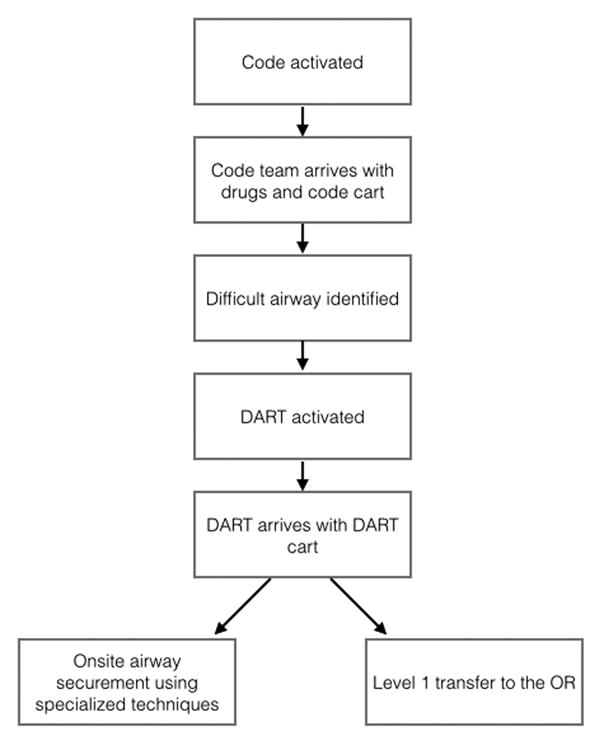
Flow chart depicting the response process used to activate the Difficult Airway Response Team (DART). OR, operating room.
The criteria for activating DART for adult patients include: (1) known difficult airways (identified by a difficult airway wristband or documentation in the patient's medical record) that requires urgent intubation and (2) inability to intubate with standard intubation techniques available to the code team. DART is not indicated or activated for non-emergent difficult airway bedside consultations or for extubation of difficult airway patients. Each patient identified as having a difficult airway is given a blue wristband to immediately activate DART should their airway become compromised. Additionally, the patient's EMR is flagged with an alert, a difficult airway note is documented in the EMR, and the patient is provided with difficult airway education materials.
With the formal establishment of the DART program, which coincided with expansion of the hospital, additional carts were added to the fleet and strategically placed based on frequency of DART activations in non-OR areas (Figure 2). These 14 DART carts complement a fleet of approximately 400 code carts institution-wide. Each DART cart has the advanced airway equipment to support the following techniques: (1) fiberoptic and rigid bronchoscopy, (2) rigid laryngoscopy, (3) cricothyrotomy and (4) tracheostomy (Table 1). Nurses on units that house a DART cart review the inventory checklist and cart integrity daily to ensure that it is appropriately stocked. In addition, equipment specialists perform weekly safety rounds on each DART cart unit to ensure that the carts are completely stocked and the equipment fully functional. Processing of a used DART cart takes approximately 90 minutes once received by equipment specialists, who provide in-house coverage 24/7 during weekdays to accommodate the volume of surgical services. If a second DART call is placed to a unit whose cart is actively being processed, cross-coverage is provided by the next closest unit with a DART cart. Carts used during the weekend are processed the next morning in the OR.
Figure 2.
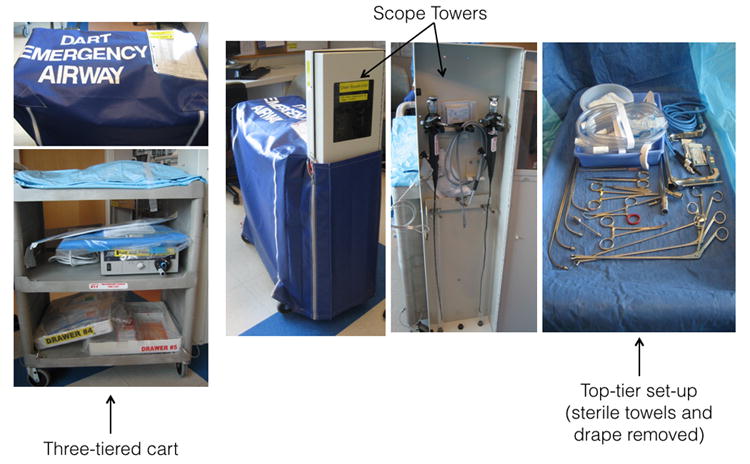
Difficult Airway Response Team (DART) cart. This series of images depicts the three-tiered cart containing instruments and bronchoscopes, the scope towers, and the top-tier set up.
Table 1. DART Cart Inventory.
| Tier 1 | D/ND | No. | Tier 3 | D/ND | No. |
|---|---|---|---|---|---|
| Jackson Cup Forceps 11″ Straight, 6mm | ND | 1 | Drawer #4 | ||
| Jackson Cup Forceps 11″ Angled, 6mm | ND | 1 | LMA Size 1, Size 1.5, Size 2, Size 2.5, Size 3, Size 4, Size 5 | D | 1 |
| Jackson Grasping Alligator Forceps 28cm | ND | 1 | Specimen bag | D | 5 |
| #3 Knife Handle | ND | 1 | 10cc Control Syringe | D | 1 |
| #15 Blade | D | 2 | Drawer # 5 | ||
| Bronch Pack | D | 1 | Medicine Cup 2 oz | D | 1 |
| Kelly Clamp 6-1/4 Cvd (Pean) | ND | 1 | 1% Lidocaine and Epi | D | 1 |
| Towel Clip 5-1/8 Non- Perf | ND | 1 | Surgical Glove Size 7 & 8 | D | 1 |
| Mayo Hegar Needle Holder Tc7″ | ND | 1 | Trach tube 4-lpc | D | 1 |
| Mayo Scissors Tc 6-3/4 Straight | ND | 1 | Trach tube 6-lpc | D | 1 |
| Gerald Forceps 7in Straight 1×2 | ND | 1 | Chloraprep 26ml | D | 1 |
| Holinger Bronchoscope 6mmX35cm | ND | 1 | 14ga Angiocath | D | 1 |
| Holinger Hour Glass Laryngoscope Adult X-long | ND | 1 | Hypo Needle 25ga | D | 1 |
| Light Carrier Oval 35cm Medium for Holinger Bronchoscope | ND | 1 | Teeth guard | D | 1 |
| Drape 3/4 with reinforcement | D | 1 | Bite block | D | 1 |
| Endolube PPM | D | 1 | Soap Castile | D | 1 |
| Fiberoptic Light Carrier 18hg for Holinger Hour Glass | ND | 1 | Suture monosof 3-0 c-14 | D | 1 |
| Fiberoptic Cable Pilling (Blue) | ND | 1 | Suture sofsilk 2-0 v-20 | D | 1 |
| Window Plug | ND | 1 | Endo Lube | D | 1 |
| Tooth Guard | D | 1 | Surgilube | D | 1 |
| Jolly Tube | D | 1 | |||
| Dedo Micro Laryngoscope Adult | ND | 1 | |||
| Light Carrier for Dedo item # 52225 | ND | 1 | |||
| JAKO Fine Suction Tube 23cm, 6 Fr | ND | 1 | |||
| Tube Aspirating Velvet Eye 45mm | ND | 1 | |||
| Jackson Open-End Asp. Tube 50cm. 12Fr. | ND | 1 | |||
| Jackson Aspirating Tube Open End 12 Fr. | ND | 1 | |||
| Jackson Asp Tube Velvet Eye 20cm, 12Fr. | ND | 1 | |||
|
| |||||
| Tier 2 | ND | 1 | Side/Other | D/ND | No. |
|
| |||||
| Eschmann Stylet | D | 1 | Suction Valve 11301CE | D | 1 |
| Aintree | D | 1 | Biopsy Valve 11301CA | D | 1 |
| CSP Emergency Tracheostomy Tray | ND | 1 | Storz Flexible Scope 5.0 Model | ND | 1 |
| Storz light source with Pilling turret adapter | ND | 1 | Storz Flexible Scope 3.7 Model | ND | 1 |
| Scope Cabinet | ND | 1 | |||
| Cart (Storage Cart) | ND | 1 | |||
| Custom Vinyl Covers for Difficult Airway Carts | ND | 1 | |||
| Fiber optic Cable, Karl Storz (gray) | ND | 1 | |||
| Extension Cable (Medical Grade) | ND | 1 | |||
D/ND = Disposable/Non-disposable
DART = Difficult Airway Response Team; LMA = laryngeal mask airway
Since DART activation occurs after a code activation, sedatives/paralytics and a full complement of resuscitative medications are already available at the bedside in both the anesthesiologist's code bag and the emergency drug boxes found on each unit. They are also available in the unit-based Pyxis machines. A code pharmacist facilitates preparation and use of medications during an event. Local anesthetics are also available in the anesthesiologist's code bag and the DART cart for use.
Safety
To faculitate continuous improvement of system-level performance and patient safety, and to identify elements of the DART program that need modification, all DART events are reviewed in real time. This process includes: (1) reporting DART activations and airway techniques utilized to an electronic web-based airway registry, (2) using in situ simulations to identify and mitigate defects in the emergency airway management process, and (3) holding quarterly multidisciplinary DART case review conferences.
To systematically collect data about DART and code activations, monitor trends, and identify and rectify process of care issues, the anesthesia department developed a web-based, Health Insurance Portability and Accountability Act-compliant registry. Data collected include general patient information (demographic data, clinical characteristics, and outcomes) and a detailed description of the event, including the clinical team members present, response times, and equipment and techniques used. After a DART event is reported to the registry, an electronic report is automatically generated and sent to the DART oversight committee and DART members via secure in-hospital email. The DART oversight committee debriefs the providers to identify potential patient safety or system-based issues. This debriefing occurs within 24 hours to optimize information capture from the event before the providers and staff change shifts. Ongoing reviews of the registry information led to the use of in situ simulation scenarios, quarterly multidisciplinary DART case review conferences, and content for the educational component of the DART curriculum.
We conducted in situ simulations to prospectively identify and mitigate defects in the difficult airway management process and to test the effectiveness of modifications to the process. These simulations were carried out in the clinical space where care was delivered, rather than in a simulation center.14,15 We conducted five in situ simulations in different clinical areas of the hospital in the first year. In a surgical intensive care unit, the labor and delivery unit, and an inpatient floor, we simulated codes to test DART processes, such as activation of the universal paging system and ideal locations for airway carts. In the postoperative acute care unit and the adult critical care unit, individuals originally involved in a DART event reenacted the scenario using high-fidelity, human-patient simulators to study the DART process and to identify and resolve unique issues that may prevent successful mobilization of DART.
Quarterly multidisciplinary DART case conferences were held to achieve safety-based learning and standardization of care across different specialties. Representatives from all four departments met to review DART events. Senior residents involved in the events presented each case.
Education
The educational component of DART focuses on enhancing individual-level knowledge and performance. It consists of in-person, skills-based courses tailored for physicians, nurses, or respiratory therapists, and educational materials for all staff.
We developed a multidisciplinary difficult airway management course that is held quarterly for residents and fellows in ACCM, OHNS, general surgery, and EM. The one-day course is conducted by faculty from each specialty and comprises didactic lectures on complex airway management, simulation, skills training on mannequins and pig trachea models, and training in teamwork and communication. All senior residents and fellows are expected to participate in this course and are divided into small multidisciplinary groups to interact in high-fidelity simulations of difficult airway scenarios and practice technical and communication skills in our institution's simulation center.
Additional educational materials were developed to support in-hospital DART operations. We developed policy standards and designed supporting documents to improve hospital-wide understanding of how and when to activate DART. These materials include fast fact sheets; a DART orientation presentation for new housestaff, respiratory therapists, nurses, and support staff; a cricothyrotomy information badge; emergency information cards placed at each unit phone with location of the nearest DART cart; and a patient education information sheet.
Data Collection and Statistical Analysis
Data regarding demographic information, patient characteristics, potential risk factors for difficult airway, morbidity and mortality information, DART response time, communication processes, airway techniques used, equipment issues, sentinel events, and malpractice claims were prospectively collected for all patients who required DART management between fiscal years 2008 and 2013. Descriptive data are reported as percentages, means, and standard deviations, as appropriate.
Results
Operations
The characteristics of DART activations are provided in Table 2. DART managed 360 difficult airway events out of 4,738 code requests (8%) between July 2008 and June 2013. On average, there were 643 intubations per year (out of approximately 948 codes per year). To note, not all codes required intubations because: (1) no airway management was required (observation only), (2) presence of preexisting tracheostomy tube (i.e., code called for bleeding from tube, tube malfunction, or tube decannulation), (3) preexisting laryngeal stoma, (4) patient's endotracheal tube required repositioning or exchange, and (5) patient required a surgical airway.
Table 2. Characteristics of Difficult Airway Response Team Patients and Events.
| Overall (n = 360) |
Year 1 (n = 43) |
Year 2 (n = 73) |
Year 3 (n = 80) |
Year 4 (n = 62) |
Year 5 (n = 100) |
|
|---|---|---|---|---|---|---|
| July 2008 – June 2013 | July 2008 – June 2009 | July 2009 – June 2010 | July 2010 – June 2011 | July 2011 – June 2012 | July 2012 – June 2013 | |
| Age, mean ± SD | 56 ± 17 | 58 ± 14 | 59 ± 16 | 60 ± 18 | 52 ± 17 | 53 ± 17 |
| Sex, frequency (%) | ||||||
| Women | 146 (41) | 17 (40) | 30 (40) | 23 (29) | 24 (39) | 52 (52) |
| Men | 214 (59) | 26 (60) | 45 (60) | 57 (71) | 38 (61) | 48 (48) |
| BMI, frequency (%) | ||||||
| < 18.5 (underweight) | 23 (6) | 1 (2) | 2 (3) | 3 (4) | 5 (8) | 12 (12) |
| 18.5 – 24.9 (normal) | 93 (26) | 12 (28) | 16 (21) | 16 (20) | 23 (37) | 26 (26) |
| 25 – 29.9 (overweight) | 79 (22) | 11 (25) | 15 (20) | 26 (32) | 13 (21) | 14 (14) |
| 30 – 34.9 (Class I)a | 51 (14) | 1 (2) | 12 (16) | 16 (20) | 7 (11) | 15 (15) |
| 35 – 39.9 (Class II)a | 27 (7) | 3 (7) | 6 (8) | 7 (9) | 2 (3) | 9 (9) |
| > 40 (Class III)a | 52 (14) | 8 (19) | 11 (15) | 8 (10) | 6 (10) | 19 (19) |
| Unknown | 35 (10) | 7 (16) | 13 (17) | 4 (5) | 6 (10) | 5 (5) |
| Location, frequency (%) | ||||||
| Floor | 81 (22) | 14 (33) | 25 (33) | 26 (32) | 14 (23) | 2 (2) |
| Intensive care unit | 192 (53) | 22 (51) | 29 (39) | 41 (51) | 29 (47) | 71 (71) |
| Emergency department | 71 (20) | 3 (7) | 18 (24) | 9 (11) | 17 (27) | 24 (24) |
| Operating suite where OHNS or trauma surgeons were not available | 8 (2) | 1 (2) | 3 (4) | 1 (1) | 0 | 3 (3) |
| Diagnostic/remote | 8 (2) | 3 (7) | 0 | 3 (4) | 2 (3) | 0 |
| Potential risk factors for difficult airway | ||||||
| History of difficult airway | 99 (27) | 12 (28) | 15 (20) | 31 (39) | 20 (32) | 21 (21) |
| History of head and neck tumor | 79 (22) | 8 (19) | 24 (32) | 22 (27) | 16 (26) | 9 (9) |
| History of COPD | 33 (9) | 4 (9) | 7 (9) | 7 (9) | 5 (8) | 10 (10) |
| History of tracheostomy | 31 (9) | 5 (12) | 5 (7) | 7 (9) | 4 (6) | 10 (10) |
| Current tracheostomy | 37 (10) | 3 (7) | 10 (13) | 5 (6) | 4 (6) | 15 (15) |
| Limited cervical spine range of motion | 38 (11) | 4 (9) | 10 (13) | 11 (14) | 7 (11) | 6 (6) |
| Active airway edema not related to allergies | 22 (6) | 1 (2) | 4 (5) | 4 (5) | 3 (5) | 10 (10) |
| Angioedema | 30 (8) | 3 (7) | 7 (9) | 3 (4) | 5 (8) | 12 (12) |
| Active airway bleeding | 37 (10) | 5 (12) | 8 (11) | 7 (9) | 2 (3) | 15 (15) |
| Timing of events | ||||||
| 7:00 AM – 7:00 PM | 196 (54) | 20 (46) | 37 (49) | 41 (51) | 38 (61) | 60 (60) |
| 7:00 PM – 7:00 AM | 137 (38) | 15 (35) | 26 (35) | 35 (44) | 23 (37) | 38 (38) |
| No documentation | 27 (7) | 8 (19) | 12 (16) | 4 (5) | 1 (2) | 2 (2) |
| Response time (minutes) | 4 ± 4 | 3 ± 2 | 4 ± 5 | 4 ± 7 | 3 ± 2 | 4 ± 3 |
| Mean ± SD | (n = 317) | (n = 25) | (n = 58) | (n = 76) | (n = 61) | (n = 97) |
SD = standard deviation; BMI = body mass index; OHNS = Otolaryngology—Head and Neck Surgery; COPD = chronic obstructive pulmonary disease.
Obesity
Mean age of patients was 56 years, and 214 (59%) were men. Seventy-nine (22%) were overweight and 130 (36%) were obese. Patient history was notable for difficult airway in 99 (28%) cases, head and neck tumor in 79 (22%), chronic obstructive pulmonary disease in 33 (9%), and past tracheostomy in 31 (9%). Twenty-two patients (6%) had active airway edema, and 37 (10%) had current tracheostomy. Patients were transported to the OR for definitive airway management in 62 (17%) of the 360 events. Twenty-three events resulted in surgical airways, and patients were transported to the OR for definitive airway management in 12 (52%) of these cases. Airway techniques used during the project period are listed in Table 3. Three case examples of DART activations are described in the supplementary Appendix 1.
Table 3. DART Cart Airway Techniques Useda.
| Year 1 | Year 2 | Year 3 | Year 4 | Year 5 | |
|---|---|---|---|---|---|
| Direct laryngoscope | 21 | 19 | 29 | 27 | 46 |
| Advanced techniques FOB | 16 | 28 | 15 | 31 | 26 |
| Advanced techniques LMA/Aintree/FOB | 1 | 5 | 2 | 9 | 5 |
| Advanced techniques rigid laryngoscope | 7 | 9 | 5 | 7 | 12 |
| Advanced techniques Eschmann | 7 | 2 | 9 | 9 | 9 |
| Advanced techniques rigid bronchoscope | 0 | 0 | 1 | 0 | 0 |
| Tracheostomy tube exchange | 1 | 2 | 3 | 4 | 9 |
| Awake / open tracheostomy | 5 | 1 | 1 | 3 | 4 |
| Cricothyroidotomy | 1 | 1 | 5 | 4 | 4 |
| Advanced techniques videolaryngoscopeb | 6 | 10 | 20 | 16 | 25 |
| Total number of techniques performed | 65 | 77 | 90 | 110 | 140 |
DART = Difficult Airway Response Team; FOB = fiberoptic bronchoscopy; LMA = laryngeal mask airway
This table does not account for techniques used before arrival of DART because, with the exception of the videolaryngoscope, these techniques are exclusively available on the DART cart.
Not part of DART carts, obtained from units.
More than half of DART events (54%) occurred between 7:00 AM and 7:00 PM (Table 2), and an equal number of DART activations (53%) were in the intensive care unit. For the 317 events in which both the page time and arrival time were recorded, the DART's mean response time was 4 minutes. During the 5-year study period there were no deaths related to airway management, no sentinel events, and no malpractice claims for adult patients managed by DART.
Cost of Operations
The DART operation is an extension of the institutional cardiopulmonary resuscitation program, which includes the code team. Our institution initially invested approximately $440,000 to obtain a fleet of 14 DART carts with specialized airway equipment. This is not a recurring cost. The annual operational cost was approximately $540,000, which includes salary support, maintenance of DART carts, and educational expenditures (Table 4). To offset the annual operations cost, the program also generates revenue through billing for airway consultations and procedures. A more detailed cost-benefit analysis is beyond the scope of the present paper.
Table 4. Cost of DART Operations.
| Expenses | Cost in dollars | ||
|---|---|---|---|
| Initial Investment | 14 DART Carts | 438,524 | |
|
| |||
| Education and Operations | Anesthesiology and Critical Care Medicine | 40,500 | |
| Otolaryngology—Head and Neck Surgery | 40,500 | ||
| Trauma Surgery | 17,500 | ||
| Emergency Medicine | 40,500 | ||
| Operating Expenses | Patient Safety Nurse | 61,000 | |
| On-call coverage | Otolaryngology—Head and Neck Surgery | 167,500 | |
| DART Cart Maintenance | Equipment Specialist | 64,400 | |
| Disposable equipment | 111,733 | ||
|
| |||
| Total operating expenses | 543,633 | ||
DART = Difficult Airway Response Team
Safety
The five in situ simulations conducted in Year 1 produced improvements in teamwork, communication, DART response times, and functionality of DART carts. Details of each simulation are presented in the online supplementary Appendix 2; key results are described below.
The simulations clarified DART provider roles and choice of airway algorithms. They also established the importance of onsite, post-event debriefings with providers and registry reporting for documentation and long-term improvement. These practices became standard in the DART program.
We also observed a delayed response time to mobilize DART carts from remote locations to the intended bedside during simulation. Subsequently, we conducted a time-and-motion study for each DART cart to ensure that it could be delivered within 10 minutes. As a result we relocated carts, added elevator service keys to reduce elevator emergency response time, and educated staff on their use.
Our simulation experience also led us to make the following improvements to the DART cart design and equipment: (1) replaced non-safety disposable sharps (such as scalpels and needles) with retractable/safe equivalents, (2) relocated fiberoptic scopes to hang in a locked side cabinet attached to each DART cart to optimize infection-control standards, (3) standardized the light boxes for equipment to a single manufacturer, (4) protected the carts with a secure/locked cover, (5) labeled light-source connectors and cables to decrease confusion during scope setup, and (6) conducted daily and weekly maintenance rounds to ensure the integrity of the equipment.
Oversight of DART documentation resulted in 100% compliance with reporting each event within 24 hours, facilitating real-time communications to hospital risk managers, and documenting airway management in the patient's medical record.
Education
The multidisciplinary airway course is held in the Simulation Center at our institution. The course is composed of core lectures, high-fidelity simulation, porcine tissue preps, and work stations for advanced skill development. The course aims to improve multidisciplinary teamwork and communications and has been taught twelve times since its inception in 2008. In the first two years, as the course was being developed, we held two courses that were offered solely to the senior residents in the four departments. Starting in 2010, we expanded the number of courses to three to four per year and began offering it to additional airway providers, including clinical fellows, nurse practitioners, physician assistants, certified registered nurse anesthetists, respiratory therapists, and critical care transport team members. By 2013, 200 learners had attended the multidisciplinary airway course. The overwhelming response to the course has been positive based on completed evaluations.
Discussion
Given the risk of life-threatening complications or death related to emergency airway management, and the preponderance of airway-related litigation, the development of interventions to improve complex airway management is urgently needed. Therefore, we created the DART program to improve emergency airway management hospital-wide. In the first 5 years of the program, we experienced no deaths, sentinel events, or malpractice claims related to airway management of our adult patients.
Within the state of Maryland, the third most frequently reported sentinel event causing death or permanent disability is associated with airway management. Although the number of events may be small, the risk is significant. The state of Maryland currently has a cap for noneconomic damages in malpractice cases that result in patient death, but other states do not. In addition, patients with anoxic brain injury secondary to complications of airway management may require a long-term life care plan to manage their medical needs. Such cases could result in multi-million dollar settlements.
The design of the DART program borrows from both the airway and the quality-improvement literature. Shiga and colleagues reported that 5.8% of elective intubations became difficult cases in ORs where senior physicians were present.11 In contrast, the incidence of emergent intubations becoming difficult cases was reported to be higher in non-OR settings.7-10 Additional studies have shown that performance of non-OR emergency intubations by clinicians with expertise in airway management, such as anesthesiologists16 or senior residents,8 decreases complications. In one recent report, 98% of difficult airway cases were managed successfully when a specific airway algorithm was used during pre-hospital emergency airway situations.17 In an accompanying editorial, Schmidt and Eikermann16 attribute this near-perfect intubation performance to the highly trained and skilled team. Long and colleagues describe a program that uses an “alpha team” and educational sessions to improve hospital-wide airway management.18 Similarly, in the quality-improvement literature, team-based interventions have been shown to improve the quality and safety of patient care.19 Morever, in our own experience, establishing a difficult airway team in the OR reduced the number of emergent surgical airways.14 Our DART program is unique and comprehensive, and aimed at reducing adverse events related to airway management.
In designing the DART program, we used a conceptual model described by Gurses et al.20 that focuses on identifying characteristics of the work environment, clinician, desired intervention, implementation of the intervention, and patient to improve quality and patient outcomes. The DART program's components target these characteristics to improve airway management. The DART program is multidisciplinary, and draws on the collective expertise of different specialties in airway management. In addition, it uses an integrative approach that emphasizes operations, safety, and education to reinforce DART's central purpose of improving hospital-wide emergency airway management.
Operations were standardized throughout the hospital by reorganizing the emergency paging system, strategically locating DART carts in high-risk locations, stocking the carts with appropriate supplies, developing an airway management protocol, initiating 24-hour attending physician coverage, and reviewing DART events daily. Review of our DART events enabled us to standardize airway management and make system-wide improvements proactively. For example, otolaryngologists and trauma surgeons agreed on using the same technique for emergency surgical airways to reduce team member bedside conflicts and promote patient safety; we formed a consensus regarding when to transport a patient to the OR during a DART event for definitive airway management; included on each DART cart in addition to their availability in ICUs and ORs; and the DART cart fleet was increased and reallocated based on actual yearly use. Our DART reviews also helped us to fine-tune the equipment stocked on DART carts. Despite the growing popularity of videolaryngoscopy, we found a less-than-optimal success rate for intubation with these devices during DART events in the first several years. Therefore, videolaryngoscopes are not currently part of DART carts because they were selectively available throughout the hospital. With experience and use of the hospital-based airway registry, we developed five in situ simulations14,15 that were modeled after actual DART events and proactively addressed complex airway management in various hospital settings. These simulations were videotaped and used in our multidisciplinary airway courses and in our teamwork and communcation workshops.
The DART program can be adopted and customized by other institutions based on their patient population, resources, and size. We developed a DART program implementation package (Table 5) that includes a detailed manual and specific tools for operations, safety, and quality improvement. The manual also describes the educational components required for the success of our program. This package can be easily customized for use in similar academic institutions.
Table 5. Inventory of DART Implementation Package.
| Item | Description |
|---|---|
| DART implementation manual | Documents how to implement the DART program and includes the necessary tools, templates, and resources to replicate the program in place at The Johns Hopkins Hospital. Suggestions for adapting the program to other hospital contexts are also provided. Discussion is provided on how to:
|
| DART operations tools | |
| DART provider roster template | Provides a template to enumerate all of the DART providers across multiple departments and capture their contact information (phone number, pager number, email address) |
| DART activation paging script | This script provides the language needed to activate DART, including the verbal verification used by the emergency response operators to verify the specific response team needed, location, caller's identity, and call-back phone number |
| DART cart tools: | |
| Inventory and price list | Contains all of the equipment and supplies stocked on a DART cart and their costs |
| Cart assembly instructions | Describes how to organize and assemble a DART cart with picture illustrations |
| Cart safety rounds handbook | This handbook offers a checklist to use when conducting safety rounds on DART carts |
| Cart location list template | Suggested template for tracking the locations of DART carts deployed throughout an institution or hospital |
| Job description of airway services equipment specialist | Describes the roles and responsibilities of an airway services equipment specialist who maintains the integrity of the carts and educates other providers about use and maintenance of the cart; this description can be adapted locally by hospitals to suit their needs |
| Cricothyrotomy kit inventory | List of supplies to assemble a pocket-sized, sterile, disposable emergency cricothyrotomy kit containing safety scalpel, tracheal hook, and Kelly clamp |
| Information systems-related | |
| Difficult airway consultation, alert, and order set for EHR | Contains two components:
|
| DART safety dashboard template | Reporting tool to aggregate data on the number of DART calls, types of calls and location, lessons learned from events, and areas for improvement |
| DART education tools | |
| Multidisciplinary airway course curriculum | An overview of the multidisciplinary airway course curriculum used to develop individual-level competencies and skills in managing difficult airways |
| DART house-staff orientation presentation | A presentation template for all incoming house-staff that describes what DART is and how to activate it |
| DART educational modules | DART educational content customized into distinct modules depending on the type of provider; content covers who comprises DART, how to call DART, what equipment is included on a cart, and how to use the equipment |
| Cricothyrotomy information badge | A small laminated card that can be clipped to the identification badges of DART providers and that illustrates the proper steps for performing a cricothyrotomy; backside of the card describes how to activate DART, where DART carts are located, and who responds to DART events |
| DART fast facts | One-page summary and description of the DART program in a question-and-answer format that can be distributed to all hospital providers; includes contact information for DART physician lead and references location of DART program in hospital policies and procedures manual |
| Patient-education document with difficult airway armband | Information sheet covering basic difficult airway medical facts in laymen's terms with generic description of difficult airway, who is at risk, signs and symptoms, how it is diagnosed, how it is treated, potential complications, what to report to clinical providers, and recommendations for entry into MedicAlert National Difficult Airway/Intubation Registry |
| DART safety tools | |
| In situ simulation handbook for DART | Describes how to conduct an in situ simulation as part of the DART program, including selection of the actual case to simulate, selection of the site to conduct the simulation, planning for the in situ simulation (including equipment needed), conducting the actual simulation, debriefing the participants, and implementing changes to practice |
| Data collection tool for the web-based registry | Contains the fields and demographic, clinical, and outcome variables used for collecting data on DART events |
| Case-based learning conference presentation template | A presentation template for use as part of case-based review conferences; it uses the Situation, Background, Assessment, Recommendations (SBAR) format for presenting DART cases |
DART = Difficult Airway Response Team; EHR = electronic health record.
Generalization of our program to other institutions does have several limitations. Implementation of a DART program such as ours would require substantial commitment of institutional resources and financial support. For example, we had to purchase a new emergency activation system for the whole institution and obtain necessary informational technology support for its operations. Buy-in from all four departments was also crucial to promote inter-departmental and interdisciplinary communication and teamwork. Prior to the establishment of our DART program, each department had its own airway management algorithm. Four departments combined these algorithms to optimize the skillsets of the airway providers. It might be challenging for other institutions that do not have the same specialties or departments that comprise our DART program. However, this challenge can be resolved by having an existing department serve as a backup by identifying providers that have expertise in advanced airway management techniques (e.g., intensivists and pulmonologists). Nevertheless, some institutions might not have enough multidisciplinary airway experts to cover patient care 24/7. Two-thirds of adverse airway events reported in Maryland are from mid-size hospitals (200-300 beds) (Anne Jones, RN, BSN, MA, personal communication, January 10, 2014) that likely lack the resources to implement such a comprehensive program. In light of these concerns and our experience, we believe that such institutions should consider developing a multidisciplinary emergency airway protocol. This protocol should specifically define (1) who the multidisciplinary airway experts are and how these experts can be summoned to the patient's bedside in a timely manner, (2) when and how to transport difficult airway patients to the OR, (3) skillsets of each speciality and who performs a surgical airway, (4) baseline metrics to evaluate success of difficult airway management, and (5) collaboration with code teams, risk management, and quality improvement staff to perform ongoing patient-based learning and process improvement.
Conclusion
The DART program was designed and implemented in response to adverse airway events. It is a comprehensive program with three components—operations, safety, and education—that improves multidisciplinary difficult airway management. Future studies are needed to examine comparative effectiveness research questions from our registry of difficult airway cases and evaluate how DART has affected patient outcomes, operational efficiency, and costs of care.
Acknowledgments
We wish to acknowledge members of the Difficult Airway Response Team (DART), the nurses and respiratory therapists at The Johns Hopkins Hospital who have helped make the DART program a success. We thank Blair Anton for her assistance in reviewing literature and Claire Levine for editorial support.
Funding: Research reported in this publication was supported by the Harry S. Truman Foundation and by the National Institutes of Health under award number T32 GM007309. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Appendix 1 - Examples of DART calls
Example 1
A 58-year-old woman presented to the Emergency Department with history of nausea, vomiting, lethargy, and a blown pupil. She had a documented difficult airway note in our hospital's electronic records. Per difficult airway note, “patient was induced for general anesthesia with propofol and was easily ventilated. After paralysis with succinylcholine, direct laryngoscopy with Macintosh and Miller blades did not reveal the glottic opening. A supraglottic device was easily placed, and intubation was accomplished with an Aintree catheter with fiberoptic assistance.” The Emergency Department physicians induced the patient with propofol and succinylcholine but were unable to visualize the glottic opening with direct laryngoscopy (Macintosh and Miller). They placed a supraglottic device and activated DART. The responding DART providers administered additional propofol and secured her airway with an Aintree catheter with fiberoptic assistance. A #7.0 endotracheal tube was placed over the Aintree with end tidal CO2 (ETCO2) and bilateral breath sounds. She tolerated the procedure and was further medically stabilized.
Example 2
On postoperative day 1 after retinal detachment surgery with general anesthesia, a 47-year-old man experienced acute onset facial and tongue swelling. The patient had been easily mask ventilated and intubated with conventional laryngoscopy during the surgery. The medical team identified probable onset angioedema secondary to an ACE-inhibitor medication. A code was activated. The code team arrived to find the patient unresponsive and bag-mask ventilation unsuccessful. The anesthesiology attending immediately placed a supraglottic device, established ventilation, and activated a DART call. Upon arrival, the DART providers attempted to intubate via the supraglottic device with an Aintree catheter and fiberoptic assistance but were unable to visualize the glottic opening secondary to significant laryngeal edema. The Otolaryngology—Head and Neck Surgery (OHNS) attending successfully visualized the glottic opening with rigid laryngoscopy, and an Eschmann stylet was placed through the vocal cords. A #7.0 endotracheal tube was advanced over the Eschmann, and intubation was verified with ETCO2 and bilateral breath sounds. The patient tolerated the intubation and was transported to the intensive care unit for further medical management.
Example 3
A 55-year-old man with cardiomyopathy was transferred from an outside hospital to our cardiac intensive care unit with septic shock. The patient had increased airway secretions and was unable to protect his airway. The intensive care team activated the code team. The anesthesiology attending was unable to intubate after multiple attempts with conventional laryngoscopy. In addition, the videolaryngoscope failed to expose the glottic opening. DART was activated while the patient was effectively bag-mask ventilated, and oxygen saturation was maintained at >95%. The OHNS attending performed rigid laryngoscopy with a rigid laryngoscope but was not able to view the glottic opening. The patient's oxygen saturation decreased to 78%, and a supraglottic device was placed. The anesthesiologist and OHNS attendings attempted to use an Aintree catheter with fiberoptic assistance but could not visualize the glottic opening and aborted their attempt. The patient became bradycardic, his oxygen saturation decreased to <60%, and he had difficulty maintaining ventilation. The OHNS and trauma surgeon present performed an emergent cricothyroidotomy without difficulty, and oxygenation saturation increased to 97% with ETCO2 and bilateral breath sounds. The patient was further stabilized in the intensive care unit and did not develop any neurologic deficits.
Appendix 2
Overview of Five In Situ Simulations Used During Implementation of DART.
| Unit | Type of Simulation | Goals | Defects Identified | Results and Lessons Learned |
|---|---|---|---|---|
| PACU | Code to DART using high fidelity human patient simulator |
|
|
|
| WICU | Code to DART testing phone activation process |
|
|
|
| CCU | Code to DART using high fidelity human patient simulator |
|
|
|
| L&D | Code to DART testing phone activation process |
|
|
|
| WBG 5 | Code to DART testing phone activation process |
|
|
|
PACU = postanesthesia care unit; DART = Difficult Airway Response Team; WICU = Weinberg intensive care unit; CCU = coronary care unit; L&D = labor and delivery; AMBER = America's Missing: Broadcast Emergency Response; OB = obstetrics; WBG 5 = Weinberg 5th floor
Disclosures
Name: Lynette J. Mark, MD
Contribution: This author helped design the study, conduct the study, collect data, analyze data, and prepare the manuscript.
Attestation: Lynette Mark approved the final manuscript. Lynette Mark attests to the integrity of the original data and the analysis reported in this manuscript. Lynette Mark is the archival author.
Conflicts of Interest: Lynette J. Mark is a physician advisor to the MedicAlert Foundation.
Name: Kurt R. Herzer, MSc
Contribution: This author helped design the study, conduct the study, collect data, analyze data, and prepare the manuscript.
Attestation: Kurt Herzer approved the final manuscript. Kurt Herzer attests to the integrity of the original data and the analysis reported in this manuscript.
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: Renee Cover, BSN, RN, CPHRM
Contribution: This author helped design the study, conduct the study, collect data, analyze data, and edit the manuscript.
Attestation: Renee Cover approved the final manuscript. Renee Cover attests to the integrity of the original data and the analysis reported in this manuscript.
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: Vinciya Pandian, PhD, RN
Contribution: This author helped design the quality improvement project, analyze data, and critically review the manuscript.
Attestation: Vinciya Pandian approved the final manuscript. Vinciya Pandian attests to the integrity of the original data and the analysis reported in this manuscript.
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: Nasir I. Bhatti, MD, MHS
Contribution: This author helped design the study, conduct the study, collect data, analyze data, and prepare the manuscript.
Attestation: Nasir Bhatti approved the final manuscript. Nasir Bhatti attests to the integrity of the original data and the analysis reported in this manuscript.
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: Lauren C. Berkow, MD
Contribution: This author helped design the quality improvement project, analyze data, and critically review the manuscript
Attestation: Lauren Berkow approved the final manuscript. Lauren Berkow attests to the integrity of the original data and the analysis reported in this manuscript.
Conflicts of Interest: Lauren Berkow is a consultant and member of the Scientific Advisory Board for Teleflex Medical
Name: Elliott R. Haut, MD, PhD
Contribution: This author helped design the quality improvement project, analyze data, and critically review the manuscript
Attestation: Elliott Haut approved the final manuscript. Elliott Haut attests to the integrity of the original data and the analysis reported in this manuscript.
Conflicts of Interest: Dr. Haut is the primary investigator of a contract (CE-12-11-4489) with The Patient-Centered Outcomes Research Institute (PCORI) entitled “Preventing Venous Thromboembolism: Empowering Patients and Enabling Patient-Centered Care via Health Information Technology.” Dr. Haut receives royalties from Lippincott, Williams & Wilkins for a book - “Avoiding Common ICU Errors.”
Name: Alexander T. Hillel, MD
Contribution: This author helped design the quality improvement project, analyze data, and critically review the manuscript
Attestation: Alexander Hillel approved the final manuscript. Alexander Hillel attests to the integrity of the original data and the analysis reported in this manuscript.
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: Christina R. Miller, MD
Contribution: This author helped design the quality improvement project, analyze data, and critically review the manuscript
Attestation: Christina Miller approved the final manuscript. Christina Miller attests to the integrity of the original data and the analysis reported in this manuscript.
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: David J. Feller-Kopman, MD
Contribution: data analysis, manuscript preparation
Attestation: David Feller-Kopman approved the final manuscript. David Feller-Kopman attests to the integrity of the original data and the analysis reported in this manuscript.
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: Adam J. Schiavi, PhD, MD
Contribution: This author helped design the quality improvement project, analyze data, and critically review the manuscript
Attestation: Adam Schiavi approved the final manuscript. Adam Schiavi attests to the integrity of the original data and the analysis reported in this manuscript.
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: Yanjun J. Xie, BA
Contribution: This author helped conduct the study, collect data, analyze data, and review the manuscript.
Attestation: Yanjun Xie approved the final manuscript. Yanjun Xie attests to the integrity of the original data and the analysis reported in this manuscript.
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: Christine Lim, BS
Contribution: This author helped to collect and analyze data.
Attestation: Christine Lim approved the final manuscript. Christine Lim attests to the integrity of the original data and the analysis reported in this manuscript.
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: Christine Holzmueller, BLA
Contribution: This author helped draft the manuscript and revise the manuscript for critical content.
Attestation: Christine Holzmueller approved the final manuscript. Christine Holzmueller attests to the integrity of the original data and the analysis reported in this manuscript.
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: Mueen Ahmad, MD
Contribution: This author helped to collect and analyze data.
Attestation: Mueen Ahmad approved the final manuscript. Mueen Ahmad attests to the integrity of the original data and the analysis reported in this manuscript.
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: Pradeep Thomas, MBA, MS
Contribution: This author helped to collect and analyze data.
Attestation: Pradeep Thomas approved the final manuscript. Pradeep Thomas attests to the integrity of the original data and the analysis reported in this manuscript.
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: Paul W. Flint, MD
Contribution: The author helped establish and participated in the DART program and reviewed and edited the manuscript.
Attestation: Paul Flint approved the final manuscript. Paul Flint attests to the integrity of the original data and the analysis reported in this manuscript.
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: Marek A. Mirski, MD, PhD
Contribution: This author helped design the quality improvement project, analyze data, and critically review the manuscript.
Attestation: Marek Mirski approved the final manuscript. Marek Mirski attests to the integrity of the original data and the analysis reported in this manuscript.
Conflicts of Interest: The author has no conflicts of interest to declare.
Footnotes
This manuscript was handled by: Avery Tung, MD
Contributor Information
Lynette J. Mark, Departments of Anesthesiology and Critical Care Medicine and Otolaryngology—Head and Neck Surgery, Johns Hopkins School of Medicine, Baltimore, Maryland.
Kurt R. Herzer, Medical Scientist Training Program, Johns Hopkins School of Medicine, Baltimore, Maryland.
Renee Cover, Legal Department, The Johns Hopkins Hospital, Baltimore, Maryland.
Vinciya Pandian, Department of Anesthesiology and Critical Care Medicine, Johns Hopkins Medical Institutions, Baltimore, Maryland.
Nasir I. Bhatti, Otolaryngology—Head and Neck Surgery, Johns Hopkins Medical Institutions, Baltimore, Maryland.
Lauren C. Berkow, Departments of Anesthesiology and Critical Care Medicine and Otolaryngology—Head and Neck Surgery, Johns Hopkins School of Medicine, Baltimore, Maryland.
Elliott R. Haut, Department of Surgery, Johns Hopkins School of Medicine, Baltimore, Maryland.
Alexander T. Hillel, Department of Otolaryngology—Head and Neck Surgery, Johns Hopkins School of Medicine, Baltimore, Maryland.
Christina R. Miller, Department of Anesthesia & Critical Care Medicine, Johns Hopkins School of Medicine, Baltimore, Maryland.
David J. Feller-Kopman, Department of Pulmonary and Critical Care Medicine, Johns Hopkins University, Baltimore, Maryland.
Adam J. Schiavi, Department of Anesthesia & Critical Care Medicine, Johns Hopkins School of Medicine, Baltimore, Maryland.
Yanjun J. Xie, MD Program, Johns Hopkins School of Medicine, Baltimore, Maryland.
Christine Lim, University of Maryland, School of Medicine, Baltimore, Maryland.
Christine Holzmueller, Johns Hopkins University School of Medicine, Baltimore, Maryland.
Mueen Ahmad, Otolaryngology—Head and Neck Surgery, Johns Hopkins Medical Institutions, Baltimore, Maryland.
Pradeep Thomas, Anesthesiology & Critical Care Medicine, Johns Hopkins Medical Institutions, Baltimore, Maryland.
Paul W. Flint, Otolaryngology – Head & Neck Surgery, Oregon Health & Science University, Portland, Oregon.
Marek A. Mirski, Department of Anesthesia & Critical Care Medicine, Johns Hopkins School of Medicine, Baltimore, Maryland.
References
- 1.Mort TC. Complications of emergency tracheal intubation: immediate airway-related consequences: part II. J Intensive Care Med. 2007;22:208–15. doi: 10.1177/0885066607301359. [DOI] [PubMed] [Google Scholar]
- 2.Mort TC. Complications of emergency tracheal intubation: hemodynamic alterations--part I. J Intensive Care Med. 2007;22:157–65. doi: 10.1177/0885066607299525. [DOI] [PubMed] [Google Scholar]
- 3.Peterson GN, Domino KB, Caplan RA, Posner KL, Lee LA, Cheney FW. Management of the difficult airway: a closed claims analysis. Anesthesiology. 2005;103:33–9. doi: 10.1097/00000542-200507000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Practice guidelines for management of the difficult airway. A report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 1993;78:597–602. [PubMed] [Google Scholar]
- 5.American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2003;98:1269–77. doi: 10.1097/00000542-200305000-00032. [DOI] [PubMed] [Google Scholar]
- 6.Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, Hagberg CA, Caplan RA, Benumof JL, Berry FA, Blitt CD, Bode RH, Cheney FW, Connis RT, Guidry OF, Nickinovich DG, Ovassapian A American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013;118:251–70. doi: 10.1097/ALN.0b013e31827773b2. [DOI] [PubMed] [Google Scholar]
- 7.Benedetto WJ, Hess DR, Gettings E, Bigatello LM, Toon H, Hurford WE, Schmidt U. Urgent tracheal intubation in general hospital units: an observational study. J Clin Anesth. 2007;19:20–4. doi: 10.1016/j.jclinane.2006.05.018. [DOI] [PubMed] [Google Scholar]
- 8.Martin LD, Mhyre JM, Shanks AM, Tremper KK, Kheterpal S. 3,423 emergency tracheal intubations at a university hospital: airway outcomes and complications. Anesthesiology. 2011;114:42–8. doi: 10.1097/ALN.0b013e318201c415. [DOI] [PubMed] [Google Scholar]
- 9.Mort TC. Emergency tracheal intubation: complications associated with repeated laryngoscopic attempts. Anesth Analg. 2004;99:607–13. doi: 10.1213/01.ANE.0000122825.04923.15. table of contents. [DOI] [PubMed] [Google Scholar]
- 10.Jaber S, Amraoui J, Lefrant JY, Arich C, Cohendy R, Landreau L, Calvet Y, Capdevila X, Mahamat A, Eledjam JJ. Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Crit Care Med. 2006;34:2355–61. doi: 10.1097/01.CCM.0000233879.58720.87. [DOI] [PubMed] [Google Scholar]
- 11.Shiga T, Wajima Z, Inoue T, Sakamoto A. Predicting difficult intubation in apparently normal patients: a meta-analysis of bedside screening test performance. Anesthesiology. 2005;103:429–37. doi: 10.1097/00000542-200508000-00027. [DOI] [PubMed] [Google Scholar]
- 12.Office of Health Care Quality. Maryland Hospital Patient Safety Program Fiscal Year 2013 Annual Report. Catonsville: Maryland Department of Health & Mental Hygiene; 2013. [Google Scholar]
- 13.Mark LJ, Herzer KR, Akst S, Michelson JD. General Considerations of Anesthesia and Management of the Difficult Airway. In: Flint PW, Haughey BH, Lund VJ, Niparko JK, Richardson MA, Robbins T, Thomas JR, editors. Cummings Otolaryngology: Head & Neck Surgery. 5th. Philadelphia: Mosby Elsevier; 2010. pp. 108–20. [Google Scholar]
- 14.Herzer KR, Rodriguez-Paz JM, Doyle PA, Flint PW, Feller-Kopman DJ, Herman J, Bristow RE, Cover R, Pronovost PJ, Mark LJ. A practical framework for patient care teams to prospectively identify and mitigate clinical hazards. Jt Comm J Qual Patient Saf. 2009;35:72–81. doi: 10.1016/s1553-7250(09)35010-2. [DOI] [PubMed] [Google Scholar]
- 15.Rodriguez-Paz JM, Mark LJ, Herzer KR, Michelson JD, Grogan KL, Herman J, Hunt D, Wardlow L, Armour EP, Pronovost PJ. A novel process for introducing a new intraoperative program: a multidisciplinary paradigm for mitigating hazards and improving patient safety. Anesth Analg. 2009;108:202–10. doi: 10.1213/ane.0b013e31818ca423. [DOI] [PubMed] [Google Scholar]
- 16.Schmidt U, Eikermann M. Organizational aspects of difficult airway management: think globally, act locally. Anesthesiology. 2011;114:3–6. doi: 10.1097/ALN.0b013e318201c6ff. [DOI] [PubMed] [Google Scholar]
- 17.Combes X, Jabre P, Margenet A, Merle JC, Leroux B, Dru M, Lecarpentier E, Dhonneur G. Unanticipated difficult airway management in the prehospital emergency setting: prospective validation of an algorithm. Anesthesiology. 2011;114:105–10. doi: 10.1097/ALN.0b013e318201c42e. [DOI] [PubMed] [Google Scholar]
- 18.Long L, Vanderhoff B, Smyke N, Shaffer LE, Solomon J, Steuer JD. Management of difficult airways using a hospital-wide “Alpha Team” approach. Am J Med Qual. 2010;25:297–304. doi: 10.1177/1062860610366587. [DOI] [PubMed] [Google Scholar]
- 19.Lemieux-Charles L, McGuire WL. What do we know about health care team effectiveness? A review of the literature Med Care Res Rev. 2006;63:263–300. doi: 10.1177/1077558706287003. [DOI] [PubMed] [Google Scholar]
- 20.Gurses AP, Marsteller JA, Ozok AA, Xiao Y, Owens S, Pronovost PJ. Using an interdisciplinary approach to identify factors that affect clinicians' compliance with evidence-based guidelines. Crit Care Med. 2010;38:S282–91. doi: 10.1097/CCM.0b013e3181e69e02. [DOI] [PubMed] [Google Scholar]


