Abstract
Introduction
Total hip arthroplasty is one of the most commonly performed orthopaedic procedures. Despite this, medical evidence to inform the choice of surgical approach is lacking. Currently in the UK, the two most frequently performed approaches to the hip are the posterior and the direct lateral.
Methods
This systematic review was performed according to Cochrane guidelines following an extensive search for prospective controlled trials published in any language before January 2014. Of the 728 records identified from searches, 6 prospective studies (including 3 randomised controlled trials) involving 517 participants provided data towards this review.
Findings
Compared with the lateral approach, the posterior approach conferred a significant reduction in the risk of Trendelenburg gait (odds ratio [OR]: 0.31, p=0.0002) and stem malposition (OR: 0.24, p=0.02), and a non-significant reduction in dislocation (OR: 0.37, p=0.16) and heterotopic ossification (OR: 0.41, p=0.13). Neither approach conferred a functional advantage. We draw attention to the paucity of evidence and the need for a further randomised trial.
Keywords: Hip, Arthroplasty, Meta-analysis
The ideal surgical approach to the hip should be relatively easy, allow for early functional recovery, and, most importantly, generate the fewest complications such as dislocation, blood loss, nerve injury and pain. UK practice is largely split between the posterior (61%) and the lateral approach (33%),1 demonstrating the uncertainty concerning the most appropriate approach for routine hip arthroplasty surgery.
The lateral approach popularised by Hardinge has undergone numerous modifications2–5 but makes use of the superficial interval between tensor fasciae latae and gluteus maximus.6 Deep to this, gluteus medius and vastus lateralis are split in continuity, gaining access to the hip joint. The posterior approach has also been described and refined by numerous authors7–9 but it employs a superficial plane splitting through gluteus maximus, and requires a tenotomy of the short external rotators and a posterior capsulotomy. This review asks which of these two approaches is more appropriate for routine primary hip arthroplasty, with specific regard to dislocation rate, Trendelenburg gait, formation of heterotopic ossification and functional outcome.
Methods
The systematic review and meta-analysis were conducted using methods described in the Cochrane Handbook for Systematic Reviews of Interventions 10 and in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines.11 Acknowledging the paucity of randomised trials, we also included quasi-randomised and clinical controlled trials but in order to reduce potential selection bias, we excluded retrospective cohort and registry studies. The protocol for this study was registered at inception on the PROSPERO database (CRD42013003817).
Search strategy
Electronic searches of MEDLINE® (1950 to January 2014), Embase™ (1980 to 2013 Week 52), AMED (1985 to January 2014), CAB Abstracts (1973 to 2013 Week 51) and the Cochrane Central Register of Controlled Trials (up to 2 January 2014) were conducted. Searches of the reference lists of relevant studies and the Web of Science™ citation tracking facility were used to identify other relevant studies. Hand searching of abstracts and proceedings from the annual meetings of the British Hip Society, European Federation of National Associations of Orthopaedics and Traumatology, and the American Academy of Orthopaedic Surgeons was also undertaken. Relevant non-English articles were translated for consideration of inclusion.
Study selection, data extraction and assessment of risk of bias
Relevant studies included adult participants (>19 years old) undergoing primary total hip arthroplasty, largely for the treatment of osteoarthritis, who were either operated on via the direct lateral or the posterior approach. For the purpose of this study, the direct lateral approach was defined as an approach requiring a release of approximately one-third of the gluteus medius from the trochanter but not the use of an osteotomy. Studies examining minimally invasive surgery, the anterolateral (Watson-Jones) approach or an approach utilising a trochanteric osteotomy were excluded. Studies of surgical approach in the setting of hip fracture, infection, revision surgery or resurfacing arthroplasty were also excluded.
The primary outcome measure was dislocation. Secondary outcome measures were Trendelenburg gait, heterotopic ossification, component malposition, leg length discrepancy, mean operative time, functional assessment scores and nerve injury.
Two authors (JB and ADB) independently reviewed all the titles and abstracts of studies identified from the literature searches. Full texts of any potentially useful studies were reviewed in detail. Disagreements regarding which studies to include were resolved by consensus among the authors (JB, ADB and AWB).
We attempted to contact the authors of studies to provide full datasets when these were lacking. Information was also requested on outcomes not reported in the publications. One author responded and the additional data were included.12 Data extraction was performed in duplicate, using a standardised form. The risk of bias for each study was assessed using the Cochrane risk of bias tool.10
Meta-analysis
Meta-analysis was performed using RevMan version 5 (Nordic Cochrane Centre, Copenhagen, Denmark) if two or more studies reported a particular outcome. A classical, frequentist statistical approach with a fixed effects model was used for the analysis to create odds ratios (ORs) and a standard error for the pooled intervention effect, which itself was used to derive 95% confidence intervals (CIs) and p-values to quantify the strength of evidence against the null hypothesis. The intervention effect estimate was calculated using weighted averages of study effect size according to the number of people in each study. Peto's method13 was used for ORs because of the rarity of observed outcomes such as dislocation.14 Statistical heterogeneity was analysed by chi-squared tests, with the I2 statistic to quantify inconsistency.
Results
Literature searches identified 728 articles and after screening in duplicate, six studies were found to be relevant to the review.12,15–19 Progress of the review is summarised as a flow diagram in Figure 1. Three randomised controlled trials (RCTs)17–19 and three non-randomised prospective cohort studies12,15,16 were included, involving a total of 517 participants.
Figure 1.
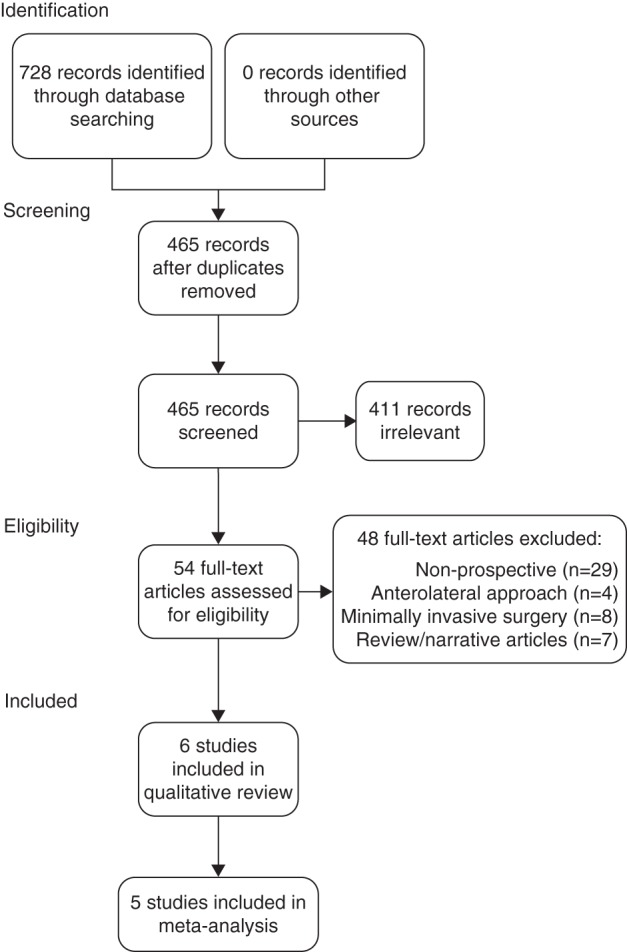
Study flow diagram
Quality assessment
Assessment of the standardisation of implants, bearing sizes and rehabilitation protocols in studies is provided in Table 1. Overall, the three RCTs have a low risk of bias and the three non-randomised prospective studies have a relatively high risk of bias. Table 2 provides a summary of our assessment of risk of bias for each of these studies.
Table 1.
Assessment of methodological quality
| Baker, 198915 | Weale, 199612 | Downing, 200116 | Witzleb, 200917 | Teratani, 201018 | Ji, 201219 | |
|---|---|---|---|---|---|---|
| Explicit standardised surgical technique described | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Same implant for both groups | NR | NR | ✗ | ✓ | ✗ | ✓ |
| Same bearing size for both groups | NR | NR | NR | ✓ | NR | ✓ |
| Same rehabilitation protocol for both groups | NR | NR | ✓ | ✓ | NR | ✓ |
| Minimal loss to follow-up | ✓ | ✓ | ✗ | ✓ | ✓ | ✓ |
✓ = robust methodology; ✗ = differences in methodology between the groups exist; NR = not recorded
Table 2.
Risk of bias
| Baker, 198915 | Weale, 199612 | Downing, 200116 | Witzleb, 200917 | Teratani, 201018 | Ji, 201219 | |
|---|---|---|---|---|---|---|
| Random sequence generation | ⊕ | ⊕ | ⊕ | ⊖ | ⊖ | ⊖ |
| Blinding of participants | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ | ⊕ |
| Blinding of outcome assessment | ⊕ | ⊕ | ⊖ | ⊖ | ⊕ | ⊖ |
| Incomplete outcome data (attrition bias) | ⊕ | ⊖ | ⊕ | ⊛ | ⊖ | ⊛ |
| Selective reporting | ⊕ | ⊖ | ⊖ | ⊖ | ⊖ | ⊖ |
⊕ = high risk of bias; ⊖ = low risk of bias; ⊛ = unclear risk of bias
Sensitivity analysis
A post-hoc sensitivity analysis, with the removal of non-RCTs, did not alter the findings of this review. This is because the older prospective studies included a small number of participants and, generally, their findings do not contradict those of the larger RCTs.
Publication bias
The funnel plot for the primary outcome measure (dislocation) was symmetrical, suggesting an absence of publication bias. An additional funnel plot was created for one of the secondary outcome measures (Trendelenburg gait), showing similar results.
Dislocation
Three prospective studies used dislocation as an outcome.16,17,19 Dislocation data from a fourth study12 were obtained by contacting the author. Two of these studies were well conducted RCTs, using the same implants and bearing sizes in both groups.17,19 Bearing size was not recorded in the two other smaller studies.15,18 A total of 398 participants were included in this meta-analysis, with 2 dislocations (1.00%) occurring in the posterior approach group and six (3.03%) in the lateral approach patients. This difference did not reach statistical significance (Peto OR: 0.37, 95% CI: 0.09–1.48, p=0.16) (Fig 2).
Figure 2.
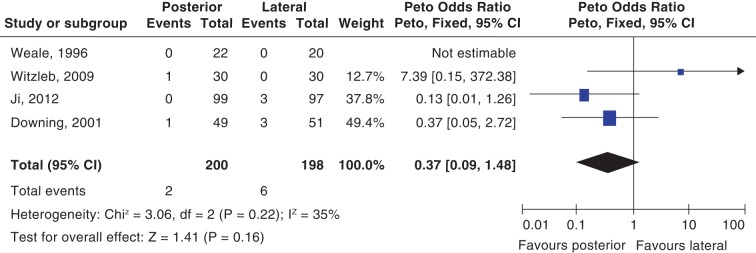
Forest plot of dislocation in posterior and lateral approaches
Trendelenburg gait
Studies reported on the Trendelenburg test,16 the modified Trendelenburg test,15 the Trendelenburg sign17 and the incidence of postoperative limp.19 These outcomes were grouped for the purpose of meta-analysis. We believe this is justified by the low chi-squared test for heterogeneity and I2 for inconsistency, suggesting that these are surrogate markers of a similar underlying adverse outcome. The clinical assessment took place between 3 and 24 months postoperatively at a mean of 15.5 months. Where multiple assessments of Trendelenburg gait were recorded in an individual study, data from the longer follow-up period were used for the meta-analysis. Overall, the posterior approach conferred a significant reduction in the risk of Trendelenburg gait (Peto OR: 0.43, 95% CI: 0.23–0.80, p=0.008) (Fig 3). When we repeated the meta-analysis with data reflecting the shortest follow-up period (average 6.4 months), the benefit of the posterior approach was greater.
Figure 3.
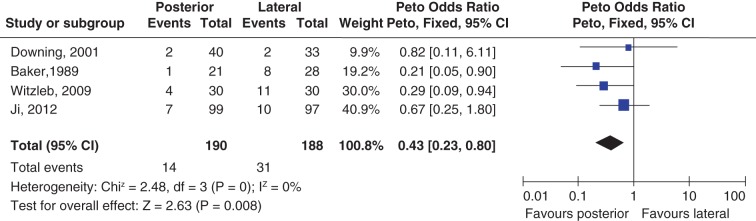
Forest plot of Trendelenburg gait in posterior and lateral approaches
Heterotopic ossification
Two studies recorded heterotopic ossification at 3 and 24 months.17,19 Subgroup stratification according to Brooker grade was not performed because of the small numbers of participants. Any heterotopic ossification was dichotomously considered a positive outcome for the purpose of meta-analysis. Compared with the lateral approach, the posterior approach showed a trend towards reduction in the risk of heterotopic ossification (Fig 4). However, this was not statistically significant (Peto OR: 0.41, 95% CI: 0.13–1.31, p=0.13).
Figure 4.
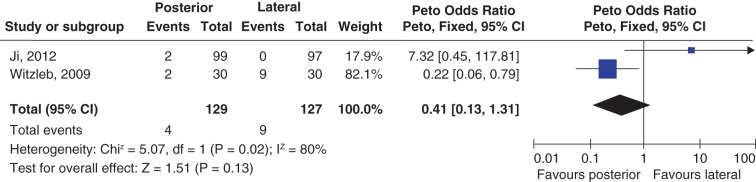
Forest plot of heterotopic ossification in posterior and lateral approaches
Stem malposition
Two studies summarised investigated stem malposition.17,19 Both studies observed fewer stem malpositions with the posterior approach (Peto OR: 0.24, 95% CI: 0.08–0.78, p=0.02).
Leg length inequality
Witzleb et al reported a leg length inequality of >0.5cm in 53% of participants following the posterior approach compared with 43% receiving a lateral approach.17 Weale et al found 18% with a leg length discrepancy of >1cm in the posterior approach group compared with 30% in the lateral approach group.12 Caution must be taken when grouping these together as different amounts of discrepancy have been used to indicate an inequality. However, there did not appear to be a difference between approaches with regard to leg length discrepancy (Peto OR: 1.05, 95% CI: 0.46–2.37, p=0.91).
Other outcomes
There were not enough data to enable a meta-analysis for functional outcomes, operative times or the incidence of nerve injury.
Discussion
In 2006 a Cochrane review comparing the lateral with the posterior approach could not draw any conclusions regarding the superiority of one approach over another.20 This meta-analysis includes three additional RCTs. One study included in the previous review compared the posterior approach with a lateral approach performed via a trochanteric osteotomy and was excluded from our review because of potential complications associated with the trochanteric osteotomy.21–32
Dislocation is a leading cause of morbidity following hip arthroplasty because revision surgery is eventually required in 20–66% of cases.2,33–39 In this review, the incidence of dislocation was 1.00% for the posterior approach and 3.03% for the lateral approach although this did not reach statistical significance. Given the relatively short follow-up periods, it is likely that the true prevalence during the life of the participant is higher. However, Blom et al have shown that dislocation is much more likely in the first three months following surgery.40 Three of the four studies contributing data regarding dislocation have followed up participants for more than three months.
The findings of this review, which was based on prospective studies, do not consistently mirror findings from large retrospective case-controlled series.41 The posterior approach used in this series did not include formal capsular repair.
A meta-analysis of retrospective studies comparing dislocation rates with and without a posterior soft tissue repair following the posterior approach has suggested a reduction in the dislocation rate from 4.46% to 0.49%.42 The use of such capsulotendinous repairs may explain the overall lower rate of dislocation following the posterior approach in this meta-analysis in contrast with older studies and some studies based on registry data.
In order to minimise bias in this systematic review, the current best practice was used. A protocol for the methodology underpinning the review was published before commencement of this work and adhered to, to ensure the methodology was explicit and reproducible. Despite the use of the highest available grades of evidence, our review is limited by the small number of prospective studies on which it is based. Although the results are weighted towards the larger, well constructed RCTs, the inclusion of less methodologically rigorous prospective studies introduces the risk of bias. However, the findings of this meta-analysis were not significantly altered by the post-hoc exclusion of these studies.
A further, adequately powered RCT is necessary to improve the robustness of the findings of this meta-analysis. Determination of which approach minimises dislocation is an important outcome following total hip arthroplasty. A one-sided sample size calculation (α 0.05, β 0.8) based on the overall incidence of dislocation in this meta-analysis indicates that 769 participants would be needed in each arm of such a randomised study to identify a 2% difference in dislocation rates.
Conclusions
Data from prospective trials suggest that the posterior approach is not associated with an increased dislocation rate. This review enables weak recommendations in favour of the posterior approach with regard to reducing dislocation, stem malposition and heterotopic ossification as well as strong recommendations in favour of the posterior approach for reducing early postoperative limp.
Conflict of interest
A small grant was received for this work from the North Bristol NHS Trust Springboard Fund.
References
- 1. National Joint Registry for England and Wales. 10th Annual Report. Hemel Hempstead: NJR; 2013. [Google Scholar]
- 2. Frndak PA, Mallory TH, Lombardi AV. Translateral surgical approach to the hip. The abductor muscle ‘split’. Clin Orthop Relat Res 1993; 295: 135–141. [PubMed] [Google Scholar]
- 3. Learmonth ID, Allen PE. The omega lateral approach to the hip. J Bone Joint Surg Br 1996; 78: 559–561. [PubMed] [Google Scholar]
- 4. Mulliken BD, Rorabeck CH, Bourne RB, Nayak N. A modified direct lateral approach in total hip arthroplasty: a comprehensive review. J Arthroplasty 1998; 13: 737–747. [DOI] [PubMed] [Google Scholar]
- 5. Schneider M, Kawahara I, Breusch SJ. Modified Hardinge approach with limited incision. Orthopade 2006; 35: 751–760. [DOI] [PubMed] [Google Scholar]
- 6. Hardinge K. The direct lateral approach to the hip. J Bone Joint Surg Br 1982; 64: 17–19. [DOI] [PubMed] [Google Scholar]
- 7. Gibson A. Posterior exposure of the hip joint. J Bone Joint Surg Br 1950; 32: 183–186. [DOI] [PubMed] [Google Scholar]
- 8. Marcy GH, Fletcher RS. Modification of the posterolateral approach to the hip for insertion of femoral-head prosthesis. J Bone Joint Surg Am 1954; 36: 142–143. [PubMed] [Google Scholar]
- 9. Moore AT. The Moore self-locking Vitallium prosthesis in fresh femoral neck fractures: a new low posterior approach (the Southern Exposure). Instr Course Lect 1959; 16: 309. [Google Scholar]
- 10. Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions. London: Cochrane Collaboration; 2008. [Google Scholar]
- 11. Liberati A, Altman DG, Tetzlaff J et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 2009; 339: b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Weale AE, Newman P, Ferguson IT, Bannister GC. Nerve injury after posterior and direct lateral approaches for hip replacement. J Bone Joint Surg Br 1996; 78: 899–902. [DOI] [PubMed] [Google Scholar]
- 13. Yusuf S, Peto R, Lewis J et al. Beta blockade during and after myocardial infarction: an overview of the randomized trials. Prog Cardiovasc Dis 1985; 27: 335–371. [DOI] [PubMed] [Google Scholar]
- 14. Bradburn MJ, Deeks JJ, Berlin JA, Russell Localio A. Much ado about nothing: a comparison of the performance of meta-analytical methods with rare events. Stat Med 2007; 26: 53–77. [DOI] [PubMed] [Google Scholar]
- 15. Baker AS, Bitounis VC. Abductor function after total hip replacement. J Bone Joint Surg Br 1989; 71: 47–50. [DOI] [PubMed] [Google Scholar]
- 16. Downing ND, Clark DI, Hutchinson JW et al. Hip abductor strength following total hip arthroplasty: a prospective comparison of the posterior and lateral approach in 100 patients. Acta Orthop Scand 2001; 72: 215–220. [DOI] [PubMed] [Google Scholar]
- 17. Witzleb WC, Stephan L, Krummenauer F et al. Short-term outcome after posterior versus lateral surgical approach for total hip arthroplasty – a randomized clinical trial. Eur J Med Res 2009; 14: 256–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Teratani T, Naito M, Shiramizu K. Intraoperative muscle damage in total hip arthroplasty. J Arthroplasty 2010; 25: 977–981. [DOI] [PubMed] [Google Scholar]
- 19. Ji HM, Kim KC, Lee YK et al. Dislocation after total hip arthroplasty: a randomized clinical trial of a posterior approach and a modified lateral approach. J Arthroplasty 2012; 27: 378–385. [DOI] [PubMed] [Google Scholar]
- 20. Jolles BM, Bogoch ER. Posterior versus lateral surgical approach for total hip arthroplasty in adults with osteoarthritis. Cochrane Database Syst Rev 2006; 3: CD003828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Clarke RP, Shea WD, Bierbaum BE. Trochanteric osteotomy: analysis of pattern of wire fixation failure and complications. Clin Orthop Relat Res 1979; 141: 102–110. [PubMed] [Google Scholar]
- 22. Dall DM, Miles AW. Re-attachment of the greater trochanter. J Bone Joint Surg Br 1983; 65: 55–59. [DOI] [PubMed] [Google Scholar]
- 23. Rozing PM. Trochanter fixation with the Dutchman’s hook. Acta Orthop Scand 1983; 54: 174–177. [DOI] [PubMed] [Google Scholar]
- 24. Browne AO, Sheehan JM. Trochanteric osteotomy in Charnley low-friction arthroplasty of the hip. Clin Orthop Relat Res 1986; 211: 128–133. [PubMed] [Google Scholar]
- 25. Jensen NF, Harris WH. A system for trochanteric osteotomy and reattachment for total hip arthroplasty with a ninety-nine percent union rate. Clin Orthop Relat Res 1986; 208: 174–181. [PubMed] [Google Scholar]
- 26. Hodgkinson JP, Shelley P, Wroblewski BM. Re-attachment of the un-united trochanter in Charnley low friction arthroplasty. J Bone J Surg Br 1989; 71: 523–525. [DOI] [PubMed] [Google Scholar]
- 27. Ritter MA, Eizember LE, Keating EM, Faris PM. Trochanteric fixation by cable grip in hip replacement. J Bone J Surg Br 1991; 73: 580–581. [DOI] [PubMed] [Google Scholar]
- 28. Frankel A, Booth RE, Balderston RA et al. Complications of trochanteric osteotomy. Long-term implications. Clin Orthop Relat Res 1993; 288: 209–213. [PubMed] [Google Scholar]
- 29. Nercessian OA, Newton PM, Joshi RP et al. Trochanteric osteotomy and wire fixation: a comparison of 2 techniques. Clin Orthop Relat Res 1996; 333: 208–216. [PubMed] [Google Scholar]
- 30. McCarthy JC, Bono JV, Turner RH et al. The outcome of trochanteric reattachment in revision total hip arthroplasty with a Cable Grip System: mean 6-year follow-up. J Arthroplasty 1999; 14: 810–814. [DOI] [PubMed] [Google Scholar]
- 31. Shahin Y, Choudhary R, Al-Naser S, Mullins M. Early loosening and secondary dislocation due to a broken trochanteric osteotomy wire following a Charnley total hip arthroplasty: a case report. Cases J 2009; 2: 7117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wieser K, Zingg P, Dora C. Trochanteric osteotomy in primary and revision total hip arthroplasty: risk factors for non-union. Arch Orthop Trauma Surg 2012; 132: 711–717. [DOI] [PubMed] [Google Scholar]
- 33. Lindberg HO, Carlsson AS, Gentz CF, Pettersson H. Recurrent and non-recurrent dislocation following total hip arthroplasty. Acta Orthop Scand 1982; 53: 947–952. [DOI] [PubMed] [Google Scholar]
- 34. Dorr LD, Wolf AW, Chandler R, Conaty JP. Classification and treatment of dislocations of total hip arthroplasty. Clin Orthop Rel Res 1983; 173: 151–158. [PubMed] [Google Scholar]
- 35. Coventry MB. Late dislocations in patients with Charnley total hip arthroplasty. J Bone Joint Surg Am 1985; 67: 832–841. [PubMed] [Google Scholar]
- 36. Ekelund A. Trochanteric osteotomy for recurrent dislocation of total hip arthroplasty. J Arthroplasty 1993; 8: 629–632. [DOI] [PubMed] [Google Scholar]
- 37. Hedlundh U, Karlsson M, Ringsberg K et al. Muscular and neurologic function in patients with recurrent dislocation after total hip arthroplasty. J Arthroplasty 1999; 14: 319–325. [DOI] [PubMed] [Google Scholar]
- 38. Woolson ST, Rahimtoola ZO. Risk factors for dislocation during the first 3 months after primary total hip replacement. J Arthroplasty 1999; 14: 662–668. [DOI] [PubMed] [Google Scholar]
- 39. Demos HA, Rorabeck CH, Bourne RB et al. Instability in primary total hip arthroplasty with the direct lateral approach. Clin Orthop Relat Res 2001; 393: 168–180. [DOI] [PubMed] [Google Scholar]
- 40. Blom AW, Rogers M, Taylor AH et al. Dislocation following total hip replacement: the Avon Orthopaedic Centre experience. Ann R Coll Surg Engl 2008; 90: 658–662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Berry DJ, von Knoch M, Schleck CD, Harmsen WS. Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am 2005; 87: 2,456–2,463. [DOI] [PubMed] [Google Scholar]
- 42. Kwon MS, Kuskowski M, Mulhall KJ et al. Does surgical approach affect total hip arthroplasty dislocation rates? Clin Orthop Rel Res 2006; 447: 34–38. [DOI] [PubMed] [Google Scholar]


