Abstract
Introduction
Acute leg ischaemia (ALI) is a common vascular emergency for which new minimally invasive treatment options were introduced in the 1990s. The aim of this study was to determine recent hospital trends for ALI in England and to assess whether the introduction of the new treatment modalities had affected management.
Methods
Routine hospital data covering ALI were provided by Hospital Episode Statistics for the years 2000 to 2011 and mortality data were obtained from the Office for National Statistics. All data were age standardised, reported per 100,000 of the population, and stratified by age band (60–74 years and ≥75 years) and sex.
Results
Hospital admissions have risen significantly from 60.3 to 94.3 per 100,000 of the population, with an average annual increase of 6.2% since 2003 (p<0.001). The rise was greater in the older age group (from 79.9 to 134.4 vs 49.3 to 73.0) and yet procedures for ALI have shown a significant decrease since 2000 from 14.3 to 12.4 per 100,000 (p=0.013), independent of age and sex. Open embolectomy of the femoral artery remains the most common procedure and the proportion of endovascular interventions showed only a small increase. Only a few deaths were attributed to ALI (range: 95–150 deaths per year).
Conclusions
Hospital workload for ALI has increased, particularly since 2003, but this trend does not appear to have translated into increased endovascular or surgical activity.
Keywords: Acute leg ischaemia, Endovascular treatment, Hospital trends
Acute leg ischaemia (ALI) is a common and potentially devastating vascular emergency. It is associated with a high risk of amputation and even death. For many years, the only potential treatment was urgent surgery, either by embolectomy or vascular reconstruction. In the 1990s, options were expanded by the introduction of intra-arterial thrombolysis and percutaneous thrombectomy. Up until this time, the incidence of ALI was increasing, in association with an increasing elderly population with cardiovascular risk factors.
In the past decade, there has been a notable reduction in the incidence of common vascular events in the cerebrovascular and coronary arterial territories.1,2 ALI is much less frequent than these, accounting for only 7% of vascular events in the Oxford Vascular Study, which assessed all individuals presenting with an acute vascular event in Oxfordshire between 2002 and 2005.3 The rate of ruptured abdominal aortic aneurysm is also declining, possibly owing to reduced smoking rates in the population and better management of cardiovascular risk factors.4
In the last few years, there has been considerable focus on time trends of incidence rates for a variety of cardiovascular diseases such as coronary artery disease, abdominal aortic aneurysm and thoracic aortic disease.1,4–6 It remains unknown whether ALI is another vascular complication in decline. A previous study assessed time trends from 1965 to 1983 in the Swedish population, showing a steady increase in admissions and procedures.7 Acute vascular event rates rise with age3 and this, together with the aging of the population, suggests that there may be an increase in hospital workload due to ALI. The aims of this study were to investigate recent hospital trends for ALI in England and to determine whether the introduction of new treatments in the 1990s had affected management.
Methods
Routine hospital data covering admissions and procedures for ALI in England from 2000 to 2011 were obtained from freely available data published online by Hospital Episode Statistics (HES) (http://www.hscic.gov.uk/hes/). HES data years run from 1 April to 31 March of the following year.
The database was examined using the diagnostic codes for hospital admissions, obtained from the tenth revision of the International Statistical Classification of Diseases (ICD-10). The codes relating to ALI are listed in Appendix 1 (available online only). Eligible codes focused on embolism and thrombosis of lower leg arteries while codes for chronic leg ischaemia were excluded.
Data for hospital procedures in this cohort were also obtained from HES. Procedures were coded according to the Office of Population Censuses and Surveys Classification of Interventions and Procedures version 4 (OPCS-4) and were used to identify interventions associated with ALI (Appendix 2 – available online only). Codes relating to dedicated endovascular procedures for ALI were L26.3, L54.2, L63.2 and L66.1.
Mortality statistics for England for the same years were obtained by accessing annual publications from the Office for National Statistics (ONS), using the codes from the ninth and tenth revision of the ICD for the underlying cause of death, which correspond to the codes used for hospital admissions (Appendix 1). ONS gathers data concerning residents in England and Wales, and mortality data do not distinguish between in-hospital or out-of-hospital death events.
Annual age standardised admission, procedure and mortality rates were calculated using age and sex specific population-based hospital admissions, procedures and mortality. The number of admissions, procedures and deaths were used as the numerators, and the total corresponding age thresholds were used as the denominators to calculate admissions, procedures and deaths per 100,000 of the population. All data were stratified by broad age bands (60–74 years and ≥75 years) and by sex.
Trends within age bands and sex were assessed by linear regression analysis using the Comprehensive R Archive Network (http://cran.r-project.org/). A p-value of <0.05 was chosen to imply statistical significance.
Results
Admissions for acute leg ischaemia
Overall, hospital admissions for ALI rose from 60.3 in 1999 to 94.3 in 2011 per 100,000 of the population in those aged ≥60 years; only a few patients were aged <60 (Fig 1). There was a suggestion of a hinge point in 2003 with an average annual rise of 6.2% thereafter. The increase was slightly more marked in those aged ≥75 years: there was a 1.7-fold increase (from 79.9 to 134.4 per 100,000, p<0.001) compared with a 1.5-fold increase in the group aged 60–74 years (from 49.3 to 73.0 per 100,000, p<0.001). There was a similar increase in men (100.7 to 159.2 per 100,000, p<0.001) and women (56.0 to 86.9 per 100,000, p<0.001), and the relative proportion of women affected remained almost constant at 55% (Fig 2).
Figure 1.
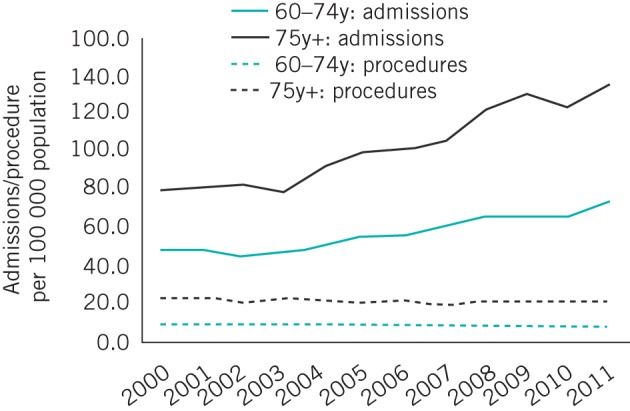
Hospital admissions versus procedures for acute leg ischaemia in England. All data are age standardised.
Figure 2.
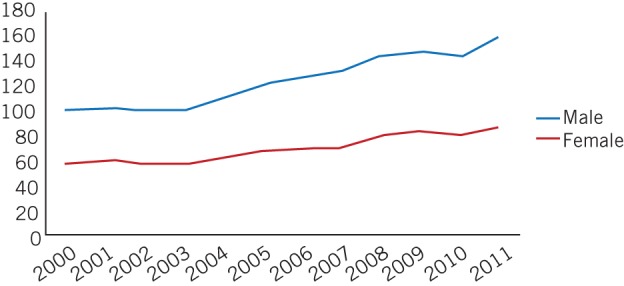
Hospital admissions for acute leg ischaemia in England. Data are age standardised (60+ years). ICD-10 codes used: I74.0, I74.1, I74.3, I74.4, I74.5, I74.8, I74.9.
Procedures for acute leg ischaemia
Overall, recorded procedures have shown a significant decrease since 2000 from 14.3 to 12.4 per 100,000 of the population (p=0.013). After stratification by age bands, the decrease in patients aged ≥75 years was similar to those aged 60–74 years: from 23.0 to 20.9 per 100,000 (10%) (p=0.142) and from 9.3 to 7.9 per 100,000 (15%) (p=0.052) respectively. This did not, however, reach statistical significance in either age band (Fig 1). The most common recorded procedure was L62.2 (open embolectomy of femoral artery), followed by L63.2 (percutaneous transluminal embolectomy of femoral artery) and L58.3 (emergency bypass of femoral artery by anastomosis of femoral artery to popliteal artery using vein graft).
Restricting the analysis to percutaneous interventions
When restricting analysis to ICD codes L26.3, L54.2, L63.2 and L66.1, the total number of procedures increased in those aged 60–74 years (from 79 to 117 per 100,000 of the population) while remaining steady in those aged ≥75 (129 to 131 per 100,000) (Fig 3). However, standardised data show that numbers remained almost constant in both age groups (1.2 to 1.5 per 100,000 and 3.5 to 3.2 per 100,000 respectively). Over the decade, the relative proportion of endovascular procedures compared with surgery for ALI was 14.3% in 2000 and 16.8% in 2011. The proportion of age standardised total procedures compared with total admissions has decreased over the years (24% in 2000, 13% in 2011) (Fig 1).
Figure 3.
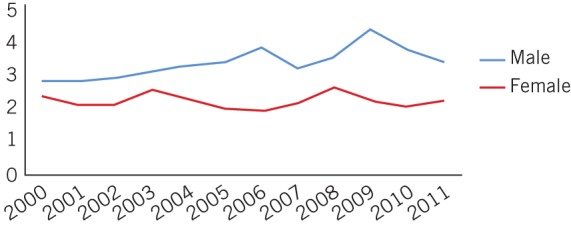
Percutaneous procedures for acute leg ischaemia in England. Data are age standardised (60+ years). OPCS-4 codes used: L63.2, L66.1, L54.2, L26.3.
Mortality trends since 2000
Trends in age standardised mortality from ALI (ICD-10 codes shown in Appendix 1) fluctuated. Nevertheless, overall, relatively few deaths were attributed to ALI (range: 95–150 deaths per year).
Discussion
ALI remains a common vascular emergency among the older population, occurring more frequently in men than in women. It is about six times more common than ruptured abdominal aortic aneurysm.8 The present study suggests that in England during the last decade, hospital admission rates with a diagnosis of ALI have increased although this has not been matched by an increased rate of either endovascular or surgical procedures.
Unlike other common cardiovascular complications that are decreasing in incidence, ALI appears to be on the increase. Reasons for the decrease in incidence in emergency admissions for many cardiovascular diseases are multifactorial but include improved risk factor management and the decrease in smoking.4 A consistent finding across all cardiovascular conditions is the shift of the disease burden to the oldest population.1,4,6 It remains unclear why these factors do not apply to the same extent to ALI, which has aetiological factors in common with some additional factors including atrial fibrillation or diabetes.9 One particular problem in the elderly is the increasing prevalence of atrial fibrillation,10 which is associated with cardiac embolism. A number of authors have bemoaned the failure to ensure that the elderly with fibrillation are protected from cardiac embolism by therapeutic anticoagulation.11
Corroborative evidence for the lack of decline in ALI is scant. A Swedish study published in 1991 showed a yearly average rise in procedures for ALI of 3.0% in women and 7.5% in men.7 The only recent information comes from North America using administrative data from the National Hospital Discharge Survey.12 The study used similar diagnostic codes to our study (albeit from an earlier version [ICD-9]) but reported different results. In America, between 1998 and 2007, the incidence of admission for ALI fell from 42.4 to 23.3 per 100,000 of the population and the mortality rate from 8.28% to 6.34% (p<0.0001). The authors reported a reducing rate of surgery for this condition from 37% to 30% in the two decades and increasing use of intra-arterial thrombolysis from 5% to 7%.
The present contemporary data from England also indicate stagnating procedure rates. Consequently, there is a steadily increasing gap between admissions and procedures, suggesting that either more patients are being treated conservatively or that coding inaccuracy is increasing, with procedures not being coded or being underreported because codes for newer endovascular procedures may be missing. In addition, some procedures possibly related to ALI (eg prostanoid infusions, fasciotomies or primary amputations) may not have been captured in the data presented.
An alternative explanation is that coding errors have confounded these results. Coding errors are always inherent in population-based studies using routine hospital statistics but a systematic review from 2012 on routinely collected data in the UK confirmed an average accuracy of 83%,13 sufficient for use in most circumstances. The North American study conducted an internal review of coding and found satisfactory validation for lower limb thromboembolism.12 The present study is based on freely available data. Admissions and procedures cannot therefore be linked to specific patients and those who have repeat or multiple admissions are not identifiable. As a result, the ratio of admissions to procedures is difficult to interpret. Finally, some non-arterial procedures triggered by the event of ALI may be missed if these are not captured by HES. The total number of procedures could consequently be underestimated.
Owing to treatment heterogeneity, a broad variety of emergency arterial procedure codes were included whereas codes for non-arterial procedures were excluded (eg emergency leg amputation). However, only about 6% of all major amputations are performed for ALI14 and so a significant bias would have been introduced if amputation codes had been included.
It was expected that the research carried out in the 1990s on intra-arterial thrombolysis and percutaneous thrombectomy would have expanded the number of endovascular procedures, in a similar way to other areas of vascular surgery. With surgeons’ increasing experience in interventional procedures and the availability of hybrid operating theatres, it was thought surgical embolectomy might be consigned to history. The present study suggests endovascular procedures still represent a small proportion of interventions for ALI; even in North America, only 7% of patients underwent intra-arterial thrombolysis.12 Perhaps the evidence for endovascular procedures for ALI remains unconvincing. Endovascular procedures, especially thrombolysis, have some drawbacks such as the delay to achieve reperfusion, which is critical for limb salvage,15 and the 6–12% risk of systemic bleeding including major intracranial haemorrhage.15–17 Another possibility is the lack of radiological facilities in some hospitals out of hours.
ALI is limb threatening but also life threatening; historical mortality rates are reported as 15–38%.18,19 However, the number of deaths attributed to ALI in the English database examined was surprisingly low, with only a few deaths annually. Similarly, the American study had mortality rates below 10%,12 which does not fit with clinical impression.
It seems likely that the procedures for reporting the underlying cause of death are inadequate. Many of the patients affected have major co-morbidities, of which an acute embolic or thrombotic process may be only one manifestation. It is therefore likely that the main cause of death in such patients is attributed to other medical conditions (eg myocardial infarction, malignancy or acute renal failure). In the ILAILL (Iloprost in Acute Ischemia of Lower Limbs) trial, all main causes of death were attributed to a variety of medical conditions and none to ALI.20 The mortality figures for ALI in England and America are likely to represent the tip of the iceberg.
Conclusions
Despite the study limitations, the present administrative data from England suggest that trends in ALI are different from other cardiovascular disorders. There has been no reduction in incidence; ALI remains a common vascular condition. It is still unclear whether the fact that fewer procedures are undertaken is a coding issue or represents a genuine increase in the number of patients treated without interventions. Comparative temporal data from large single institutions or other well defined populations are needed to address these issues. Finally, it appears that the endovascular revolution may have passed ALI by, and that thrombolysis and percutaneous thrombectomy have not secured a significant role in this condition. Further targeted research into the costs and benefits of these endovascular procedures might define their role more clearly.
Appendix
References
- 1. Schmidt M, Jacobsen JB, Lash TL et al. 25 year trends in first time hospitalisation for acute myocardial infarction, subsequent short and long term mortality, and the prognostic impact of sex and comorbidity: a Danish nationwide cohort study. BMJ 2012; 344: e356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Carandang R, Seshadri S, Beiser A et al. Trends in incidence, lifetime risk, severity, and 30-day mortality of stroke over the past 50 years. JAMA 2006; 296: 2,939–2,946. [DOI] [PubMed] [Google Scholar]
- 3. Rothwell PM, Coull AJ, Silver LE et al. Population-based study of event-rate, incidence, case fatality, and mortality for all acute vascular events in all arterial territories (Oxford Vascular Study). Lancet 2005; 366: 1,773–1,783. [DOI] [PubMed] [Google Scholar]
- 4. von Allmen RS, Anjum A, Powell JT. Incidence of descending aortic pathology and evaluation of the impact of thoracic endovascular aortic repair: a population-based study in England and Wales from 1999 to 2010. Eur J Vasc Endovasc Surg 2013; 45: 154–159. [DOI] [PubMed] [Google Scholar]
- 5. Anjum A, von Allmen R, Greenhalgh R, Powell JT. Explaining the decrease in mortality from abdominal aortic aneurysm rupture. Br J Surg 2012; 99: 637–645. [DOI] [PubMed] [Google Scholar]
- 6. Smolina K, Wright FL, Rayner M, Goldacre MJ. Determinants of the decline in mortality from acute myocardial infarction in England between 2002 and 2010: linked national database study. BMJ 2012; 344: d8059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ljungman C, Adami HO, Bergqvist D et al. Time trends in incidence rates of acute, non-traumatic extremity ischaemia: a population-based study during a 19-year period. Br J Surg 1991; 78: 857–860. [DOI] [PubMed] [Google Scholar]
- 8. Anjum A, Powell JT. Is the incidence of abdominal aortic aneurysm declining in the 21st century? Mortality and hospital admissions for England & Wales and Scotland. Eur J Vasc Endovasc Surg 2012; 43: 161–166. [DOI] [PubMed] [Google Scholar]
- 9. Lip GY, Nieuwlaat R, Pisters R et al. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach. Chest 2010; 137: 263–272. [DOI] [PubMed] [Google Scholar]
- 10. Duncan ME, Pitcher A, Goldacre MJ. Atrial fibrillation as a cause of death increased steeply in England between 1995 and 2010. Europace 2014; 16: 797–802. [DOI] [PubMed] [Google Scholar]
- 11. Scowcroft AC, Cowie MR. Atrial fibrillation: improvement in identification and stroke preventive therapy – data from the UK Clinical Practice Research Datalink, 2000–2012. Int J Cardiol 2014; 171: 169–173. [DOI] [PubMed] [Google Scholar]
- 12. Korabathina R, Weintraub AR, Price LL et al. Twenty-year analysis of trends in the incidence and in-hospital mortality for lower-extremity arterial thromboembolism. Circulation 2013; 128: 115–121. [DOI] [PubMed] [Google Scholar]
- 13. Burns EM, Rigby E, Mamidanna R et al. Systematic review of discharge coding accuracy. J Public Health 2012; 34: 138–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Eskelinen E, Lepäntalo M, Hietala EM et al. Lower limb amputations in Southern Finland in 2000 and trends up to 2001. Eur J Vasc Endovasc Surg 2004; 27: 193–200. [DOI] [PubMed] [Google Scholar]
- 15. Ouriel K, Veith FJ, Sasahara AA. A comparison of recombinant urokinase with vascular surgery as initial treatment for acute arterial occlusion of the legs. N Engl J Med 1998; 338: 1,105–1,111. [DOI] [PubMed] [Google Scholar]
- 16. Results of a prospective randomized trial evaluating surgery versus thrombolysis for ischemia of the lower extremity. Ann Surg 1994; 220: 251–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Earnshaw JJ, Whitman B, Foy C. National Audit of Thrombolysis for Acute Leg Ischemia (NATALI): clinical factors associated with early outcome. J Vasc Surg 2004; 39: 1,018–1,025. [DOI] [PubMed] [Google Scholar]
- 18. Eliason JL, Wainess RM, Proctor MC et al. A national and single institutional experience in the contemporary treatment of acute lower extremity ischemia. Ann Surg 2003; 238: 382–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Braithwaite BD, Davies B, Birch PA et al. Management of acute leg ischaemia in the elderly. Br J Surg 1998; 85: 217–220. [DOI] [PubMed] [Google Scholar]
- 20. de Donato G, Gussoni G, de Donato G et al. The ILAILL study: iloprost as adjuvant to surgery for acute ischemia of lower limbs. Ann Surg 2006; 244: 185–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


