Abstract
Introduction
The aim of this study was to examine the durability of photoselective vaporisation of the prostate (PVP) with the 120W GreenLight HPS® laser (American Medical Systems, Minnetonka, MN, US), and to examine the incidence, nature and factors associated with complications from the procedure.
Methods
Clinical records of PVP patients were reviewed to compare details between patients who developed complications and those who did not. Kaplan–Meier survival curves were used to assess durability. Cox regression was used to examine associations between complications and perioperative factors.
Results
Successful outcomes were maintained in 84% of 117 patients at the 2-year follow-up appointment. Complication rates were low and comparable with transurethral resection of the prostate (TURP). Complications were developed by 18 patients (15.4%) over a mean follow-up duration of 20.8 months. The most common complications were residual prostate requiring another surgery (5/117, 4.3%) and urethral stricture (4/117, 3.4%). Patients with complications had significantly longer catheterisation duration. Length of hospital stay, lasing energy, pre and postoperative levels of prostate specific antigen (PSA), pre and postoperative maximum flow rate (Qmax), and age at surgery were not found to influence development of complications.
Conclusions
Results from PVP with an HPS® laser are durable. Complications are low and compare favourably with TURP. Lasing energy, PSA, Qmax, patient age and length of stay are not associated with development of complications. However, a longer postoperative catheterisation after PVP is associated with development of complications.
Keywords: GreenLight™ lithium triborate laser, Photoselective vaporisation of prostate, Benign prostatic hyperplasia, Lasing energy, Length of stay, Duration of catheterisation
GreenLight™ laser (American Medical Systems, Minnetonka, MN, US) photoselective vaporisation of the prostate (PVP) is being increasingly accepted as a minimally invasive treatment for the treatment of bladder outflow obstruction due to prostatic enlargement.1,2 Its perceived benefits over transurethral resection of the prostate (TURP) include less blood loss, the absence of haemodynamic changes, less risk of erectile dysfunction and safety in men on anticoagulants.3,4 Furthermore, GreenLight™ laser PVP is reputed to carry health cost benefits as a result of a shorter length of hospital stay (LOS) and duration of postoperative catheter use.5 Some studies have also suggested a lower incidence of complications when compared with TURP.1
While many papers have reviewed the efficacy, outcomes and complications from the 80W potassium titanyl phosphate (KTP) laser, the newer 120W GreenLight HPS® lithium triborate (LBO) laser has not been investigated so widely.6 This study evaluated the nature and frequency of complications arising from the 120W HPS® laser, and investigated some factors that may be associated with complications.
Methods
In this retrospective observational self-controlled case series, patients who underwent PVP with the 120W LBO laser between April 2008 and August 2010 were studied. A 23Fr laser cytoscope (Karl Storz, Tuttlingen, Germany) was used in all patients. Antimicrobial prophylaxis with amikacin and co-amoxiclav was used routinely. Only cases carried out by two urologists who had prior experience of more than 25 cases each with PVP were included in the study.
Information from the prospective database was reviewed to study the incidence and nature of complications. These included stricture, bladder neck obstruction, residual tissue requiring further resection or vaporisation, haematuria, failed or delayed removal of catheter and persistent storage symptoms.7 The data for patients with infective complications were also reviewed. For this purpose, infection was defined as being present in patients with a systemic inflammatory response syndrome (SIRS) or sepsis. SIRS was diagnosed by the American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference definition.8
Age at surgery, LOS, catheterisation duration, preoperative and postoperative levels of prostate specific antigen (PSA), preoperative and postoperative maximum flow rate (Qmax), and lasing energy used during PVP were compared in patients who developed complications and those who had no complications. Durability of PVP was defined as the absence of complications over the follow-up period of two years.
Statistical analysis
Categorical variables were summarised by the number and percentage of patients. All continuous variables were found to have positively skewed distributions, and so were summarised by the median and interquartile range. LOS, time with catheter and PSA (both pre and postoperative) had some values that were much higher than the majority of the values. So that the outlying values did not have too much influence on the results, these variables were categorised for the purposes of analysis.
As not all patients had a complication and also as patients had been followed up for different lengths of time, ‘survival analysis’ methods were used to analyse the data. Patients who did not have a complication were censored at the time of last known follow-up appointment. Kaplan–Meier curves were constructed to show the occurrence of complications over time and to determine the rate of complications at key time points.
Cox regression was performed in two stages to examine factors associated with the time to complications. First, a set of univariate analyses was performed to separately examine the association between each factor and complications. Subsequently, multivariate analysis was performed to examine the joint effect of the factors on the outcome, using only those variables that showed some evidence of an association in the univariate analysis.
Results
A total of 117 patients underwent PVP with the 120W LBO laser during the study period. The mean patient age was 72.6 years (standard deviation [SD]: 10 years; range: 43–91 years). Data variables are summarised in Table 1.
Table 1.
Summary of data variables
| Variable | Summary |
|---|---|
| Complications | 18/117 (15%) |
| Median LOS in days | 1 (IQR: 1–2) |
| LOS >1 day | 36/117 (32%) |
| Median duration with catheter in days | 1 (IQR: 1–2) |
| Catheter >5 days | 10/76 (13%) |
| Median energy in J | 67,637 (IQR: 28,785–109,813) |
| Energy >100,000J | 32/116 (28%) |
| Median preoperative PSA in ng/ml | 3.2 (IQR: 1.6–6.8) |
| Postoperative PSA >5ng/ml | 29/78 (37%) |
| Median postoperative PSA in ng/ml | 4.3 (IQR: 2.0–8.2) |
| Postoperative PSA >5ng/ml | 15/41 (37%) |
| Median preoperative Qmax in ml/s (n=11) | 9.3 (IQR: 6.0–10.6) |
| Median postoperative Qmax in ml/s (n=18) | 13.5 (IQR: 9.1–16.2) |
LOS = length of stay; IQR = interquartile range; PSA = prostate specific antigen; Qmax = maximum flow rate
Eighteen patients (15.4%) developed complications over a mean follow-up period of 20.8 months (SD: 6.6 months; range: 5–32 months). For patients where a complication occurred, the mean time of occurrence of complications after surgery was 4.3 months (SD: 4.7 months, range: 1 day – 16 months). The nature and frequency of complications along with their Clavien grade9 as well as reoperations performed are shown in Table 2. Of these, the most common conditions requiring further surgery were residual prostate tissue (5/117 patients, 4.3%) and urethral stricture (4/117 patients, 3.4%). Two patients who failed a trial without catheter at discharge were also considered to have complications although the catheter was removed successfully 2–3 weeks later. Eleven of these patients needed to be reoperated (9.4%) at a mean interval of 6.4 months (SD: 4.5 months; range: 1–16 months) following PVP (Table 2).
Table 2.
Complications with Clavien grade, frequency and reoperations among 117 patients undergoing photoselective vaporisation of the prostate with the 120W GreenLight HPS® laser
| Case | Complication | Clavien grade | Reoperation |
|---|---|---|---|
| 1 | Urethral stricture | IIIb | Optical urethrotomy |
| 2 | Urethral stricture | IIIb | Optical urethrotomy twice |
| 3 | Urethral stricture | IIIb | Optical urethrotomy |
| 4 | Residual prostate | IIIb | ‘Redo’ GreenLight™ laser |
| 5 | Residual prostate | IIIb | TURP |
| 6 | Residual prostate | IIIb | TURP |
| 7 | Residual prostate | IIIb | ‘Redo’ GreenLight™ laser |
| 8 | Residual prostate | IIIb | ‘Redo’ GreenLight™ laser |
| 9 | Stricture and bladder stone | IIIb | Urethral dilation, cystolitholapaxy |
| 10 | Bladder neck obstruction | IIIb | Optical urethrotomy |
| 11 | Delayed haematuria and clot retention* | IIIb | Clot evacuation, TURP |
| 12 | Failed TWOC | Id | Nil |
| 13 | Failed TWOC | Id | Nil |
| 14 | Persistent storage symptoms | Id | Nil |
| 15 | Persistent storage symptoms | Id | Nil |
| 16 | High residual urine | Id | Nil |
| 17 | High residual urine | Id | Nil |
| 18 | Cardiac complications | IVa | Nil |
TURP = transurethral resection of the prostate; TWOC = trial without catheter
Not on an anticoagulants
Figure 1 shows the proportion of patients who were free from complications at varying points in the follow-up period. The Kaplan–Meier estimates of the proportion of patients who were free from complications at selected time points are quantified in Table 3: 92% of patients were free from complications after 3 months and 84% after 24 months.
Figure 1.
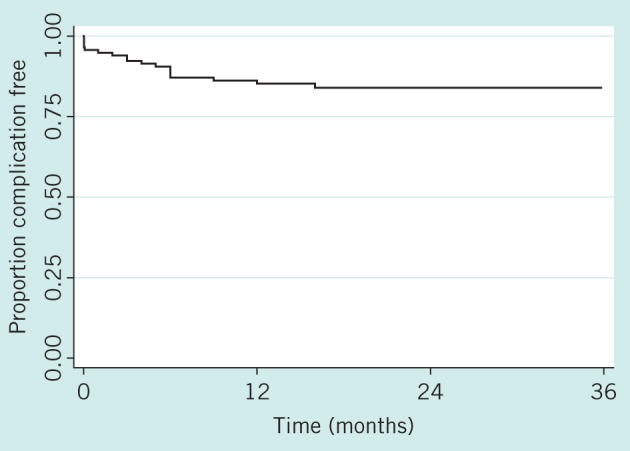
Kaplan–Meier estimates of the percentage of patients who were complication free
Table 3.
Proportion of patients free of complications
| Time | Proportion free of complications (95% CI) |
|---|---|
| 3 months | 0.92 (0.86–0.96) |
| 6 months | 0.87 (0.80–0.92) |
| 12 months | 0.85 (0.77–0.90) |
| 24 months | 0.84 (0.76–0.90) |
CI = confidence interval
The mean age of patients developing complications was 71.4 years (SD: 8.8 years; range: 59–86 years) and in those with no complications it was 72.8 years (SD: 10 years; range: 43–91 years). This difference is not significant (p=0.69).
Cox regression was used to examine associations between patient factors and the occurrence of complications. The size of effect of each factor as p-values and hazard ratios is presented in Table 4. For categorical variables, these represent the hazard of complications in one group relative to another. For continuous variables, the hazard ratios give the change in the risk of complications for a given increase in each variable.
Table 4.
The association between variables and the development of complications in univariate analysis
| Variable | n | Category | Hazard ratio (95% CI) | p-value |
|---|---|---|---|---|
| Length of stay | 111 | ≤1 day | 1 | 0.23 |
| ≥2 days | 1.77 (0.70–4.47) | |||
| Time with catheter | 76 | ≤5 days | 1 | |
| >5 days | 4.67 (1.75–12.5[0]) | 0.002 | ||
| Lasing energy | 116 | – | 1.47* (1.00–2.16) | 0.05 |
| Preoperative PSA | 78 | ≤5 | 1 | 0.89 |
| >5 | 1.07 (0.42–2.77) | |||
| Postoperative PSA | 41 | ≤5 | 1 | 0.77 |
| >5 | 1.17 (0.42–3.28) | |||
| Preoperative Qmax | 11 | – | 0.56** (0.19–1.64) | 0.29 |
| Postoperative Qmax | 18 | – | 0.89** (0.51–1.55) | 0.68 |
CI = confidence interval; PSA = prostate specific antigen; Qmax = maximum flow rate
Hazard ratio for a 50,000J increase in energy
Hazard ratio for a 5-unit increase in Qmax
The analysis suggested that there was a significant association between catheterisation duration and the occurrence of complications. The risk of complications at any time was over four times higher for patients with a catheter duration of >5 days than for those with a catheter duration of ≤5 days (Fig 2).
Figure 2.
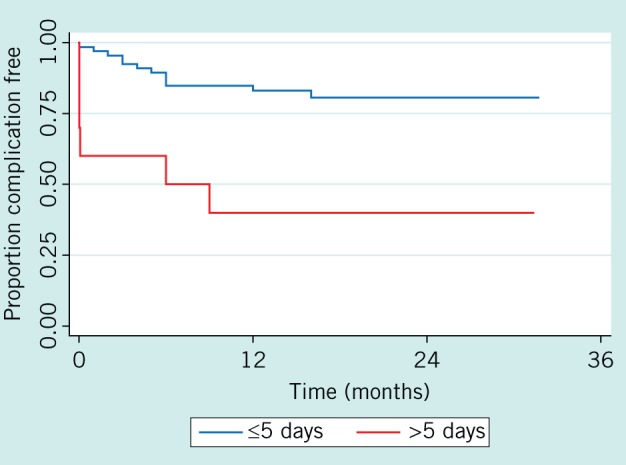
Kaplan–Meier estimates showing the effect of catheter duration on the percentage of patients who were complication free
Lasing energy was also associated with the time to complications although this association was only of borderline significance (p=0.05). The results suggested that an increase of 50,000J was associated with around a 50% increase in the chance of complications at any time. This result is depicted in Figure 3, where for the purposes of illustration, patients were split into ≤100,000 and >100,000J. None of the other variables (LOS, pre or postoperative PSA, pre or postoperative Qmax) were associated significantly with the occurrence of complications.
Figure 3.
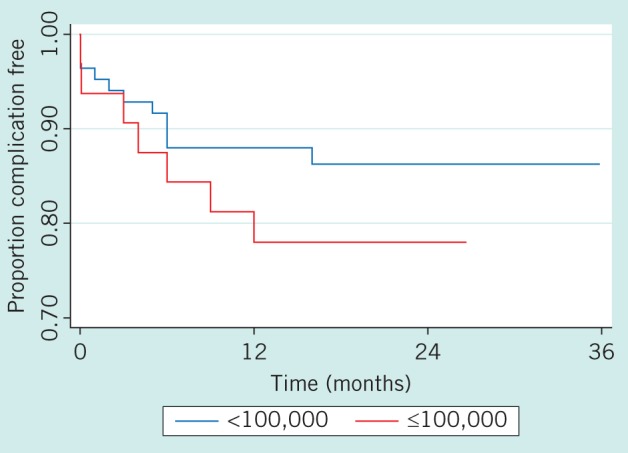
Kaplan–Meier survival estimates showing the effect of lasing energy used during photoselective vaporisation of the prostate on the percentage of patients who were complication free
The results of the multivariate analysis examining the joint effect of catheter duration and lasing energy on the time to complications are given in Table 5. Of the two variables, only catheter duration was associated significantly with complications. As with the univariate analyses, patients with a catheter time of >5 days had a risk of complications at any time that was over four times higher than for those with a shorter catheter time. After adjusting for catheter duration, there was no additional effect of energy on the likelihood of complications.
Table 5.
Results of multivariate analysis showing the association of catheter duration and lasing energy on the occurrence of complications
| Variable | Category | Hazard ratio (95% CI) | p-value |
|---|---|---|---|
| Time with catheter | ≤5 days | 1 | 0.007 |
| >5 days | 4.12 (1.47–11.6) | ||
| Lasing energy | – | 1.18* (0.80–1.74) | 0.40 |
CI = confidence interval
Hazard ratio for a 50,000J increase in energy
Discussion
The quest for a minimally invasive surgical technique that is at least as effective as TURP and yet has a lower incidence of complications has yielded many alternatives such as laser vaporisation, laser enucleation, electrovaporisation, radiofrequency treatment or thermotherapy. GreenLight™ laser PVP has emerged as one of the leading options because of its consistent and predictable efficacy, and because the technique of PVP is relatively easy to learn.10,11 GreenLight™ laser PVP is also attractive because it can be used in diverse clinical situations where TURP is not advisable owing to safety concerns and for large glands in excess of 100g.12 Most studies with the 80W KTP lasers have demonstrated a lower incidence of complications than for TURP and a similar reoperation rate.13,14 However, owing to a limited number of RCTs comparing GreenLight™ laser with TURP, its use is still not widespread.
The 120W HPS® system with an operating wavelength of 532nm and employing a LBO crystal is marketed as an improvement on the 80W KTP laser because of higher energy delivery achieving faster and more complete vaporisation of prostate tissue.15 While there are some studies on the new 120W HPS® system that support its efficacy in outcome, there are not many peer reviewed studies that have examined complications or investigated perioperative factors that may be associated with the development of complications. Indeed, the National Institute for Health and Care Excellence in the UK has cited the limited evidence available on laser vaporisation to recommend that its use be considered only in the context of a randomised trial.16
While not a RCT, in this observational self-controlled case study, we have considered mainly those complications listed in the Methods section. Complications such as erectile or ejaculatory dysfunction were not investigated.
Urethral strictures and obstruction due to residual prostate tissue were the most frequent complications (3.4% and 4.3% respectively). However, Spaliviero et al reported no strictures despite higher energy usage over a 52-month follow-up period.17 Nevertheless, the incidence of complications and retreatment rate compare favourably with those occurring after TURP. Urethral and bladder neck strictures after treatment with the 80W GreenLight™ laser have been reported in 4.4% and 3.6% respectively, with an overall retreatment rate of 6.8%.3 For TURP, the major late complications reported have been urethral stricture (2.2–9.8%) and bladder neck contracture (0.3–9.2%), with a combined retreatment rate ranging from 3% to 14.5% after five years.7 We did not have infective complications amounting to SIRS or sepsis. Conceivably, our regime of perioperative antimicrobial cover contributed to this outcome.
In our study, PVP with the 120W HPS® laser produced outcomes that are durable at 84% over a two-year follow-up duration. At our centre, after TURP, the median LOS and duration of catheterisation are 2.5 days each (unpublished data). These are considerably longer than those observed in PVP patients (1 day each).
Patients who had increased durations of catheterisation were more likely to develop further complications such as urethral stricture, bladder outflow obstruction due to residual prostate tissue and bladder neck obstruction. LOS, lasing energy used, pre and postoperative PSA, pre and postoperative Qmax, and age at surgery were not found to influence development of complications.
There are some limitations to this study. First, it was a retrospective study. Prostate volume, Qmax measurements and PSA were not available for all patients, and the relatively low number of patients with available PSA readings following PVP might help explain the paradoxical rise seen in this parameter. Information on anticoagulant use was also not collected. Furthermore, the link between postoperative catheter duration and the development of complications is unexplained. It was not possible to establish whether the prolonged catheterisation was a cause or a consequence of the complications.
Conclusions
Our study shows that PVP with the HPS® laser produces an 84% successful and durable outcome at two years of follow-up. It also suggests that the incidence and nature of complications from PVP with the 120W LBO laser is low and compares favourably with those that occur after TURP. Both LOS and catheterisation duration were shorter with PVP than with TURP. Higher lasing energy, PSA, Qmax, patient age and LOS are not associated with the development of complications. However, postoperative catheter duration is associated with development of complications. To our knowledge, this is the first study on this laser that examines perioperative factors in the context of complications. Further prospective studies that also include correlation with prostate volume are needed to confirm these findings.
Acknowledgements
We gratefully acknowledge Paul Bassett and Neha Batura for their help with the statistics.
References
- 1.Bouchier-Hayes DM, Anderson P, Van Appledorn S et al KTP laser versus transurethral resection: early results of a randomized trial. J Endourol 2006; 20: 580–580. [DOI] [PubMed] [Google Scholar]
- 2.Ahmed HU, Thwaini A, Shergill IS et al Greenlight prostatectomy: a challenge to the gold standard? A review of KTP photoselective vaporization of the prostate. Surg Laparosc Endosc Percutan Tech 2007; 17: 156–156. [DOI] [PubMed] [Google Scholar]
- 3.Ruszat R, Seitz M, Wyler SF et al GreenLight laser vaporization of the prostate: single-center experience and long-term results after 500 procedures. Eur Urol 2008; 54: 893–893. [DOI] [PubMed] [Google Scholar]
- 4.Ruszat R, Wyler S, Forster T et al Safety and effectiveness of photoselective vaporization of the prostate (PVP) in patients on ongoing oral anticoagulation. Eur Urol 2007; 51: 1,031–1,031. [DOI] [PubMed] [Google Scholar]
- 5.Tugcu V, Tasci AI, Sahin S, Zorluoglu F. Comparison of photoselective vaporization of the prostate and transurethral resection of the prostate: a prospective nonrandomized bicenter trial with 2-year follow-up. J Endourol 2008; 22: 1,519–1,519. [DOI] [PubMed] [Google Scholar]
- 6.Van Cleynenbreugel B, Srirangam SJ, Van Poppel H. High-performance system GreenLight laser: indications and outcomes. Curr Opin Urol 2009; 19: 33–33. [DOI] [PubMed] [Google Scholar]
- 7.Rassweiler J, Teber D, Kuntz R, Hofmann R. Complications of transurethral resection of the prostate (TURP) – incidence, management, and prevention. Eur Urol 2006; 50: 969–969. [DOI] [PubMed] [Google Scholar]
- 8.Bone RC, Balk RA, Cerra FB et al Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest 2009; 136: e28. [DOI] [PubMed] [Google Scholar]
- 9.Clavien PA, Barkun J, de Oliveira ML et al The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg 2009; 250: 187–187. [DOI] [PubMed] [Google Scholar]
- 10.Sulser T, Reich O, Wyler S et al Photoselective KTP laser vaporization of the prostate: first experiences with 65 procedures. J Endourol 2004; 18: 976–976. [DOI] [PubMed] [Google Scholar]
- 11.Wosnitzer MS, Rutman MP. KTP/LBO laser vaporization of the prostate. Urol Clin North Am 2009; 36: 471–471. [DOI] [PubMed] [Google Scholar]
- 12.Rajbabu K, Chandrasekara SK, Barber NJ et al Photoselective vaporization of the prostate with the potassium-titanyl-phosphate laser in men with prostates of >100 mL. BJU Int 2007; 100: 593–593. [DOI] [PubMed] [Google Scholar]
- 13.Bouchier-Hayes DM, Van Appledorn S, Bugeja P et al A randomized trial of photoselective vaporization of the prostate using the 80-W potassium-titanyl-phosphate laser vs transurethral prostatectomy, with a 1-year follow-up. BJU Int 2010; 105: 964–964. [DOI] [PubMed] [Google Scholar]
- 14.Rieken M, Ebinger Mundorff N, Bonkat G et al Complications of laser prostatectomy: a review of recent data. World J Urol 2010; 28: 53–53. [DOI] [PubMed] [Google Scholar]
- 15.Reich O. Greenlight: from potassium-titanyl-phosphate to lithium triborate or from good to better? Curr Opin Urol 2011; 21: 27–27. [DOI] [PubMed] [Google Scholar]
- 16.National Institute for Health and Clinical Excellence. Lower Urinary Tract Symptoms. London: NICE; 2010. [Google Scholar]
- 17.Spaliviero M, Araki M, Wong C. Short-term outcomes of Greenlight HPS laser photoselective vaporization prostatectomy (PVP) for benign prostatic hyperplasia (BPH). J Endourol 2008; 22: 2,341–2,341. [DOI] [PubMed] [Google Scholar]


