Abstract
Introduction
Incidental gallbladder cancer is found in 0.6–2.1% of patients undergoing laparoscopic cholecystectomy for symptomatic gallstones. Patients with Tis or T1a tumours generally undergo no further intervention. However, spilled stones during surgery may have catastrophic consequences. We present a case and suggest aggressive management in patients with incidental gallbladder cancer who had spilled gallstones at surgery.
Case History
A 37-year-old woman underwent a laparoscopic cholecystectomy for symptomatic gallstones, during which some stones were spilled into the peritoneal cavity. Subsequent histological examination confirmed incidental pT1a gallbladder cancer. Hepatopancreatobiliary multidisciplinary team discussion agreed on regular six-monthly follow-up. The patient developed recurrent pain two years after surgery. Computed tomography revealed a lesion in segment 6 of the liver. At laparotomy, multiple tumour embedded gallstones were found on the diaphragm. Histological examination showed features (akin to the original pathology) consistent with a metastatic gallbladder tumour.
Conclusions
This case highlights the potential for recurrence of early stage disease resulting from implantation of dysplastic or malignant cells carried through spilled gallstones. It is therefore important to know if stones were spilled during original surgery in patients with incidental gallbladder cancer following a laparoscopic cholecystectomy. Aggressive and early surgical management should be considered for these patients.
Keywords: Gallstones, Gallbladder cancer, Laparoscopic cholecystectomy
The numbers of laparoscopic cholecystectomies (LCs) have increased dramatically over the last two decades and it is now the gold standard for symptomatic gallstone disease. Up to 3.5% of laparoscopic cholecystectomy specimens turn out to harbour incidental gallbladder cancer (IGC) on histology.1 Such patients are usually referred to a hepatopancreaticobiliary (HPB) centre for further treatment. Traditionally, stage pTis and pT1 IGC are managed conservatively, and radical re-resection is offered to patients with pT2 or pT3 disease. Gallbladder perforation and spillage of stones is not uncommon during LC, raising the question of whether spilled bile and gallstones can lead to tumour cell implantation in early stage IGC. We describe a case of a young woman who presented with such a problem.
Case History
A 37-year-old fit woman underwent a LC to treat biliary colic due to gallstone disease. Perioperatively, the gallbladder was perforated, leading to bile and stone spillage. Thorough washout and retrieval of some of the stones was performed. Histological examination of the gallbladder showed evidence of diffuse surface mucosal dysplasia, which in areas was severe (biliary intraepithelial neoplasia grade 3) with additional small foci of poorly differentiated adenocarcinoma infiltrating into the lamina propria and muscular wall (Fig 1), indicating stage pT1b.
Figure 1.
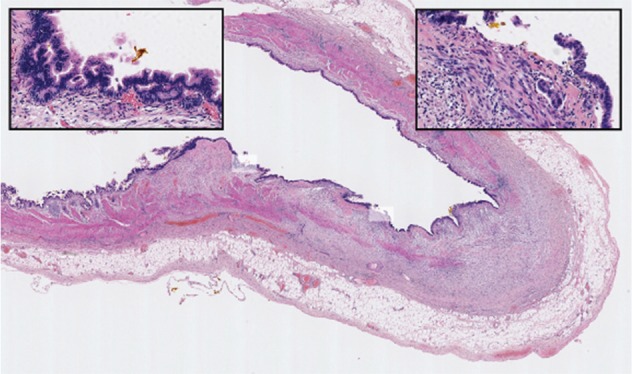
Cholecystectomy specimen showing features of chronic cholecystitis with shaded areas in high power insets demonstrating diffuse surface mucosal dysplasia (left) and foci of early infiltrating adenocarcinoma (right)
The case was referred to the regional HPB multidisciplinary team (MDT) meeting. Unfortunately, the MDT was unaware of the bile and stone spillage during the LC. The MDT recommended a regular six-monthly clinical and radiological follow-up. Following a two-year asymptomatic period, the patient presented with right upper quadrant pain. Computed tomography revealed a small subcapsular lesion in segment 6 of the liver. The patient underwent open excision and was found to have two gallstone nodules on the surface of segment 6. Histological examination of a subcapsular wedge biopsy revealed a gallstone nodule embedded in a plaque of undifferentiated carcinoma (Fig 2). It was postulated that the subcapsular liver deposit may have resulted from misplaced or implanted neoplastic cells, which disseminated from the gallbladder along with the spilled gallstones during the original LC.
Figure 2.
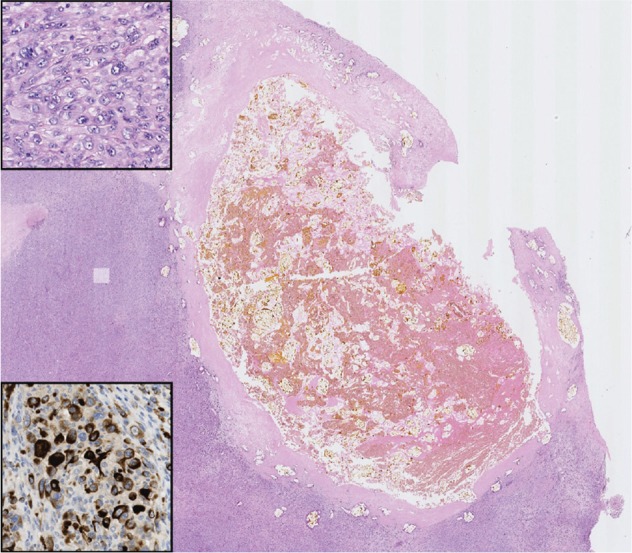
Subcapsular liver tumour associated with gallstone nodule. High power of the shaded area (upper inset) shows a pleomorphic spindle cell population with immunoreactivity for the epithelial marker CAM 5.2 (lower inset), indicating undifferentiated carcinoma, most likely representing recurrence of the primary gallbladder cancer.
Given the histological diagnosis of recurrent carcinoma, the patient underwent a relaparotomy to ensure clear tumour resection margins. At laparotomy, two further suspicious liver lesions were identified (Fig 3). On liver mobilisation, multiple gallstones were found embedded in clinically malignant peritoneal nodules on the diaphragm although these were not confirmed as malignant on biopsy. The disease was deemed inoperable and the patient was referred to the oncology team for palliative chemotherapy. She died of metastatic disease four months after the second laparotomy.
Figure 3.
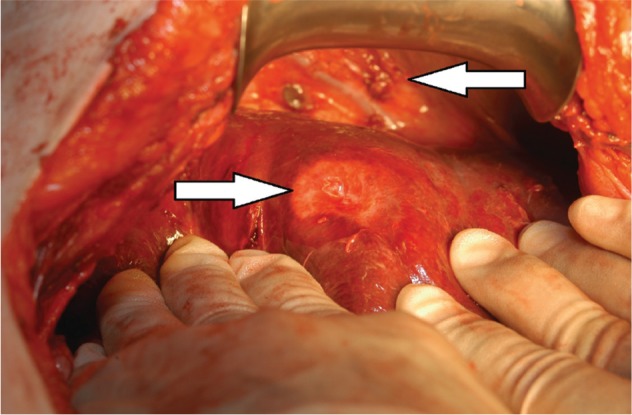
Operative findings after liver mobilisation. Left arrow: malignant looking lesion in segment 6 of the liver. Right arrow: spilled gallstones embedded in tumour nodules on diaphragm.
Discussion
There is a paucity of literature on the management of patients with spilled gallstones who are found subsequently to have IGC. Patients with stage pTis or pT1 IGC and in whom the gallbladder has been removed intact have a favourable prognosis with conservative treatment, with over 85% surviving for more than five years.2 On the other hand, survival is significantly worse in cases of bile and stone spillage owing to the risk of peritoneal seeding caused by contamination with neoplastic cells. One has to ask whether a different approach is required for those patients with early IGC on histology of the cholecystectomy specimen who had bile or stones spilled during surgery.
Recurrence of gallbladder cancer following a LC due to seeding along laparoscopic trocar sites is reported to occur in 0.5–17% of cases, both at the site through which the gallbladder was removed and at trocar sites through which the laparoscopic instruments were inserted.3,4 Management of port sites in cases of IGC has been discussed extensively in the literature with port site excision being recommended by some authors to remove the area of skin and abdominal wall where tumour cells might have implanted.3 If port site excision can reduce the incidence of port site recurrence in operable gallbladder cancer, an aggressive approach should be considered in patients with early IGC who had bile or stone spilled during surgery.
In this case, after the IGC diagnosis and MDT discussion, a conservative approach was favoured. The MDT was unaware of the bile and stone spillage during the original operation as sometimes operation notes do not accurately reflect spill or perforation during mobilisation of the gallbladder in LC.5 If the HPB MDT had known about the spilled stones, we would have carefully explained the dilemma to the patient and given her the option either of close observation with six-monthly clinical and radiological follow-up appointments or of undergoing a further procedure to retrieve the spilled gallstones. Unfortunately, she subsequently developed recurrent and metastatic disease in the liver. It was felt that this was most probably due to spillage of neoplastic cells at the primary operation.
Similar to this case, tumour recurrence around a gallstone embedded in a port site has been described previously.4 Interestingly, there was a two-year lag between the primary cholecystectomy and symptom recurrence. This could potentially be explained either by spillage of a low tumour cell burden or by dysplastic cells being spilled, rather than invasive malignancy, with recurrence developing after malignant transformation of these dysplastic cells.
Conclusions
Gallbladder cancer is often a particularly aggressive cancer, with a significant propensity to seed and metastasise in the abdominal cavity. This case highlights the potential for recurrence of early stage disease resulting from implantation of dysplastic or malignant cells carried through spilled gallstones. It is therefore recommended that such an event during a LC should be documented carefully in operation notes. HPB MDTs should look actively for information regarding spilled gallstones in cases of IGC and consider a more aggressive management approach in this clinical situation.
References
- 1.Tantia O, Jain M, Khanna S, Sen B. Incidental carcinoma gall bladder during laparoscopic cholecystectomy for symptomatic gall stone disease. Surg Endosc 2009; 23: 2,041–2,046. [DOI] [PubMed] [Google Scholar]
- 2.Lee HY, Kim YH, Jung GJ et al. Prognostic factors for gallbladder cancer in the laparoscopy era. J Korean Surg Soc 2012; 83: 227–236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Steinert R, Nestler G, Sagynaliev E et al. Laparoscopic cholecystectomy and gallbladder cancer. J Surg Oncol 2006; 93: 682–689. [DOI] [PubMed] [Google Scholar]
- 4.Tan YM, Lim DT. Gallstone embedded within a port site metastasis – report of a case. Singapore Med J 2002; 43: 637–639. [PubMed] [Google Scholar]
- 5.Wauben LS, van Grevenstein WM, Goossens RH et al. Operative notes do not reflect reality in laparoscopic cholecystectomy. Br J Surg 2011; 98: 1,431–1,436. [DOI] [PubMed] [Google Scholar]


