Abstract
Pyelonephritis is defined as an inflammation of the kidney and renal pelvis. The diagnosis is usually clinical. Acute multifocal bacterial nephritis is a rare form of pyelonephritis that is more severe and sepsis is more common. We report a patient who presented with fever and right-sided abdominal pain associated with right flank tenderness, suggesting right acute pyelonephritis. Bilateral multifocal pyelonephritis was diagnosed on ultrasonography, radionuclide renal scintigraphy and computed tomography. However, owing to non-resolution of symptoms, a biopsy was performed, which showed bilateral papillary renal cell carcinoma (PRCC). PRCC is known to exhibit multicentricity. To our knowledge, a case of bilateral multicentric PRCC masquerading as bilateral multifocal pyelonephritis has not been reported in the English literature. This case highlights the need to be vigilant while treating patients with focal lesions of the kidney as an inflammatory condition lest a malignancy should be missed.
Keywords: Renal adenocarcinoma, Multifocal pyelonephritis, Radionuclide renal scintigraphy, Computed tomography, Haematuria, Renal biopsy
Pyelonephritis, an inflammation of the kidney and renal pelvis, is usually diagnosed clinically.1 Acute multifocal bacterial nephritis is a rare form of pyelonephritis. It is more severe and sepsis is more common.1 Papillary renal cell carcinoma (PRCC) is known to be multicentric in up to 40% of cases.2 Both acute multifocal bacterial nephritis and PRCC have a similar appearance on ultrasonography, contrast enhanced computed tomography (CT) and renal nuclear scintigraphy (technetium-99m dimercaptosuccinic acid [DMSA] imaging).1 PRCC can have a bilateral multifocal presentation. More than half of symptomatic PRCC patients have macrohaematuria at presentation.3 We report, for the first time in the English language literature, a patient who presented with clinical features as well as features suggestive of multifocal pyelonephritis on ultrasonography, CT and DMSA renal imaging and who was subsequently diagnosed as having PRCC on renal biopsy.
Case History
A 60-year-old man presented with intermittent, low grade fever, predominantly at night, with no chills and rigors, and right-sided abdominal pain of one week’s duration. The patient had no history of medical illness and was not a known diabetic or hypertensive. He had no urinary symptoms and his general physical examination was unremarkable. His pulse was 86bpm and blood pressure was 140/86mmHg. He had right loin tenderness on palpation. Examination of the other systems was normal.
Laboratory investigations revealed mild anaemia (haemoglobin 10.5g/dl) as well as elevated blood urea (56mg/dl) and serum creatinine (2.3mg/dl). Microscopic examination of the urine showed 4–6 pus cells and 10–12 red blood cells per high power field. His urine culture showed Escherichia coli sensitive to amikacin, furazolidone and meropenem. His blood culture was sterile.
Ultrasonography of the kidneys showed normal sized kidneys bilaterally with altered echoes, and multiple focal hypoechoic and isoechoic areas consistent with multifocal pyelonephritis. The fever subsided with a renal modified dose of amikacin. After 14 days of antibiotics, technetium-99m DMSA static imaging (Fig 1) was performed, which revealed bilateral impaired functioning pyelonephritic kidneys. Plain computed tomography (CT) of the kidneys showed multiple round, ill defined hypodense lesions in both the kidneys (Fig 2).
Figure 1.
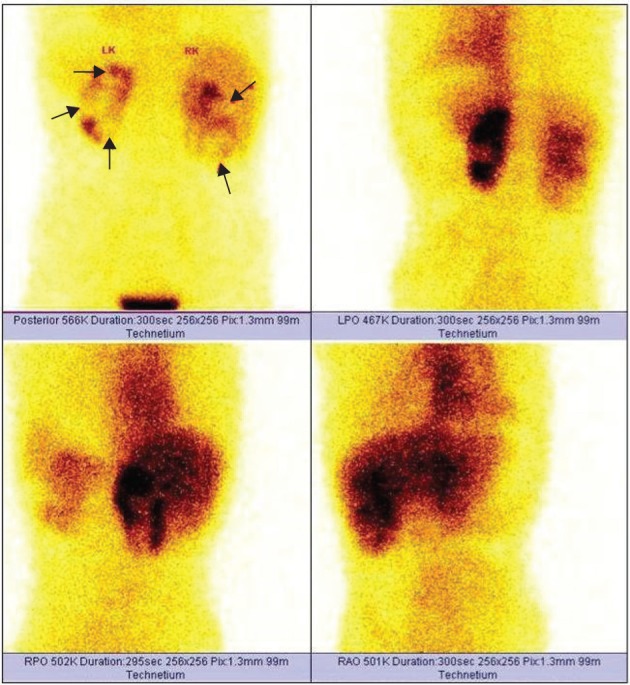
Dimercaptosuccinic acid imaging (posterior view) showing multiple cortical-based cold areas in both kidneys (arrows) suggestive of pyelonephritis. Increased background and liver uptake seen as a result of renal failure.
Figure 2.
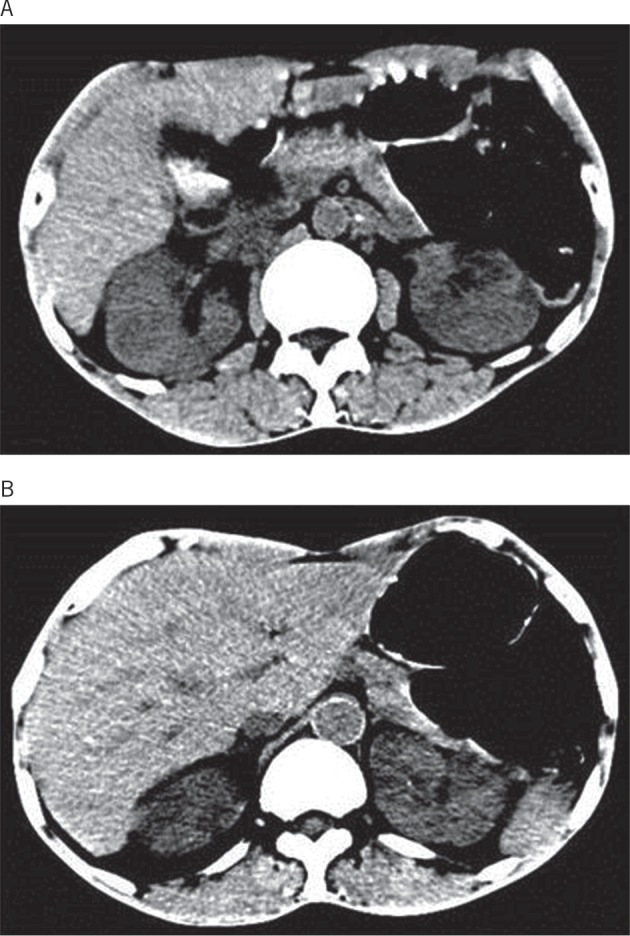
Axial non-contrast axial computed tomography showing multiple round, ill defined hypodense lesions in both kidneys.
The patient was discharged in a stable condition with a diagnosis of pyelonephritis but he presented again four weeks later with fever, abdominal pain and haematuria with clots. Physical examination was normal. Contrast enhanced CT of the abdomen was performed as renal failure had improved. The CT showed multiple hypodense lesions in both kidneys (Fig 3), suggestive of renal tuberculosis or multifocal pyelonephritis. As the patient continued to have haematuria and fever, bilateral renal biopsies were performed. This revealed globally sclerosed glomeruli and atrophic tubules with thyroidisation. The interstitium showed PRCC (Fig 4). The patient was not willing to undergo further treatment. There was no history of renal malignancies in the family.
Figure 3.
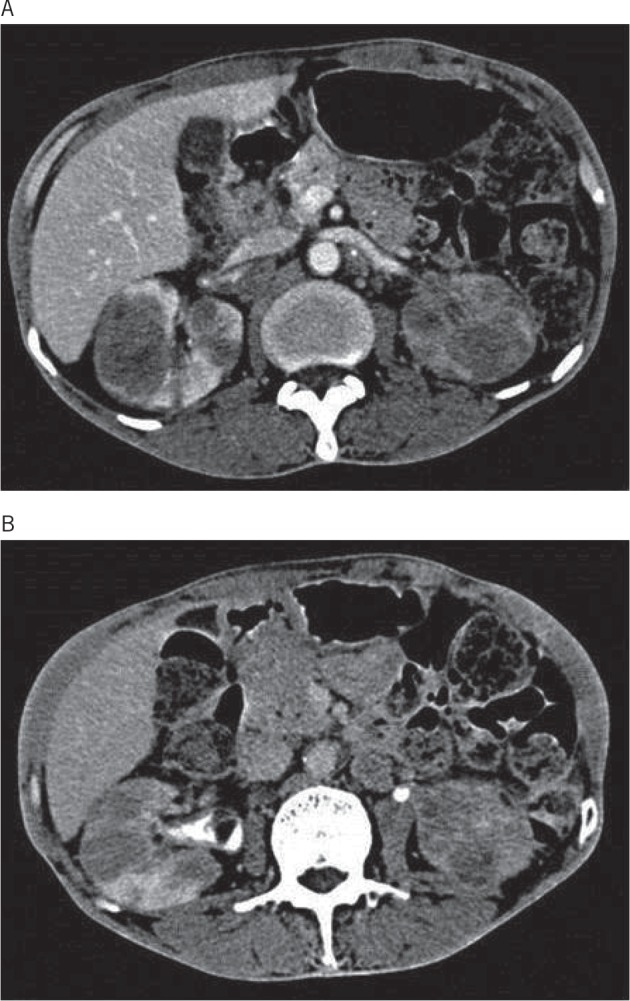
Axial contrast enhanced computed tomography one month later showing: nephrographic phase with multiple homogeneous hypovascular mass lesions in both kidneys (A) and urographic phase with multiple homogeneous hypovascular mass lesions in both kidneys (B). Irregular filling defect noted in right renal pelvis.
Figure 4.
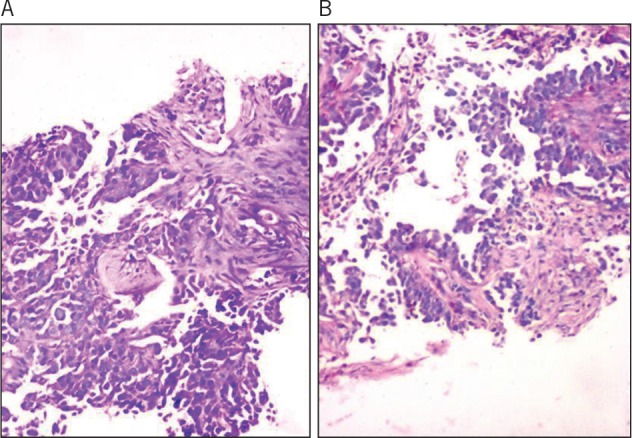
Histological study (haematoxylin and eosin stain, 20x magnification): tumour cells in glandular and papillary configuration infiltrating the renal parenchyma (A) and tumour cells arranged in papillary configuration with central fibrovascular cores (B).
Discussion
Although it is defined as inflammation of the kidney and renal pelvis, pyelonephritis is usually a clinical diagnosis.1 The clinical spectrum of pyelonephritis ranges from cystitis with mild flank pain to frank Gram-negative sepsis.
Classically, it presents with abrupt onset chills, fever (≥100°F), unilateral/bilateral flank or costovertebral angle pain with or without tenderness.1 The patient may also have leucocytosis with neutrophilic preponderance. Numerous leucocytes, often in clumps, and bacterial rods or chains of cocci are seen on urine microscopy. Urine cultures are positive but about 20% of patients have urine cultures with fewer than 105 colony forming units/ml, leading to negative results on Gram staining of the urine. E coli accounts for 80% of cases. Acute multifocal bacterial nephritis is an uncommon, more severe form of acute renal infection where a heavy leucocyte infiltrate is seen in multiple lobes. About half of these patients are diabetic and sepsis is common. Generally, leucocytosis and urinary tract infections resulting from Gram-negative organisms are found. More than 50% of these patients have bacteraemia.
Non-invasive tests do not determine pyelonephritis reliably. Renal ultrasonography and CT are used to evaluate such patients. Ultrasonography and CT show renal enlargement with hypoechoic or attenuated parenchyma with a compressed collecting system or focal bacterial nephritis with obstruction. In cases of more pronounced parenchymal destruction, abscess formation may be seen, and complicated renal and perirenal infections may be identified. Such patients should be treated using parenteral therapy, followed by an appropriate oral antimicrobial drug in full dosage for an additional 10–14 days. In multifocal pyelonephritis, contrast enhanced CT is necessary as the lesions are difficult to visualise on unenhanced CT. Wedge-shaped areas of decreased enhancement are seen, with no definite wall or liquefaction.1,4
Acute bacterial nephritis represents a relatively early phase of renal abscess formation. Treatment of this condition includes hydration and intravenous antimicrobial agents for at least seven days, followed by seven days of oral antimicrobial therapy. Patients with bacterial nephritis respond typically to medical therapy and follow-up studies show resolution of the wedge-shaped zones of diminished attenuation. When there is failure to respond to antimicrobial therapy, as in our patient, it is an indication for appropriate studies to rule out obstructive uropathy, renal or perirenal abscess, RCC or acute renal vein thrombosis.1,5
PRCC (chromophilic) is the second most common histological subtype of RCC, representing 10–15% of all RCCs, and it is more frequent in patients with end-stage renal failure and acquired renal cystic disease.2 At present, most authors believe that PRCC (and type 1 PRCC in particular) carry a better prognosis than clear cell RCC when compared grade for grade and stage for stage.2,3,6 PRCC has been found to coexist with or complicate emphysematous pyelonephritis.7,8 However, an extensive PubMed search with the keywords ‘papillary renal cell carcinoma’ and ‘multifocal pyelonephritis’ did not reveal any report where bilateral multicentric papillary RCC has masqueraded as bilateral multifocal pyelonephritis.
Synchronous bilateral RCCs are treated with nephron sparing surgery (NSS) to avoid maintenance haemodialysis. Multifocality could, however, impair complete surgical resection with NSS. The surgical treatment of synchronous bilateral RCC might pose a significant challenge for long-term tumour control and renal function. According to recent data, NSS in bilateral RCC provides lower long-term haemodialysis rates and a favourable prognosis comparable with that for patients with unilateral RCC.9 In patients with bilateral multicentric PRCC, the optimal management would be bilateral nephrectomy with haemodialysis, followed by transplantation.
Our case illustrates that the treating physician should be vigilant and patients who have focal lesions of the kidney on imaging must undergo follow-up studies to document their resolution. Patients whose lesions do not show evidence of resolution and those who do not show rapid clinical improvement despite appropriate medical management of pyelonephritis should undergo biopsy of the lesion for possible malignancy.
Conclusions
PRCC can present as multifocal pyelonephritis or tuberculosis of the kidney, and this should be kept in mind during evaluation of bilateral hypodense lesions on CT and pyelonephritis on DMSA imaging. Early diagnosis could be beneficial to the patient.
References
- 1.Schaeffer AJ, Schaeffer EM. Infections of the Urinary Tract In: Wein AJ, Kavoussi LR, Novick AC et al Campbell-Walsh Urology. 10th edn. Philadelphia: Saunders; 2012. pp257–326. [Google Scholar]
- 2.Campbell SC, Lane BR. Malignant Renal Tumors In: Wein AJ, Kavoussi LR, Novick AC et al Campbell-Walsh Urology. 10th edn. Philadelphia: Saunders; 2012. pp1,413–1,474. [Google Scholar]
- 3.Yamanaka K, Miyake H, Hara I et al Papillary renal cell carcinoma: a clinicopathological study of 35 cases. Int J Urol 2006; 13: 1,049–1,052. [DOI] [PubMed] [Google Scholar]
- 4.Shen Y, Brown MA. Renal imaging in pyelonephritis. Nephrology 2004; 9: 22–25. [DOI] [PubMed] [Google Scholar]
- 5.Pertel PE, Haverstock D. Risk factors for a poor outcome after therapy for acute pyelonephritis. BJU Int 2006; 98: 141–147. [DOI] [PubMed] [Google Scholar]
- 6.Gontero P, Ceratti G, Guglielmetti S et al Prognostic factors in a prospective series of papillary renal cell carcinoma. BJU Int 2008; 102: 697–702. [DOI] [PubMed] [Google Scholar]
- 7.Lin CH, Huang JJ, Liu HL et al Renal cell carcinoma complicated by emphysematous pyelonephritis in a non-diabetic patient with renal failure. Nephron 2002; 92: 227–229. [DOI] [PubMed] [Google Scholar]
- 8.Takizawa A, Yanada S, Iwamuro S et al Papillary renal cell carcinoma complicated with emphysematous pyelonephritis: a case report. Hinyokika Kiyo 2000; 46: 899–901. [PubMed] [Google Scholar]
- 9.Klatte T, Wunderlich H, Patard JJ et al Clinicopathological features and prognosis of synchronous bilateral renal cell carcinoma: an international multicentre experience. BJU Int 2007; 100: 21–25. [DOI] [PubMed] [Google Scholar]


