Abstract
Introduction
Fast track methodology or enhanced recovery schemes have gained increasing popularity in perioperative care. While evidence is strong for colorectal surgery, its importance in gastric and oesophageal surgery has yet to be established. This article reviews the evidence of enhanced recovery schemes on outcome for this type of surgery.
Methods
A systematic literature search was conducted up to March 2014. Studies were retrieved and analysed using predetermined criteria.
Results
From 34 articles reviewed, 18 eligible studies were identified: 7 on gastric and 11 on oesophageal resection. Three randomised controlled trials, five case-controlled studies and ten case series were identified. The reported protocols included changes to each stage of the patient journey from pre to postoperative care. The specific focus following oesophageal resections was on early mobilisation, a reduction in intensive care unit stay, early drain removal and early (or no) contrast swallow studies. Following gastric resections, the emphasis was on reducing epidural anaesthesia along with re-establishing oral intake in the first three postoperative days and early removal of nasogastric tubes.
In the papers reviewed, mortality rates following fast track surgery were 0.8% (9/1,075) for oesophageal resection and 0% (0/329) for gastric resection. The reported morbidity rate was 16.5% (54/329) following gastric resection and 38.6% (396/1,075) following oesophageal resection. Length of stay was reduced in both groups compared with conventional recovery groups in comparative studies.
Conclusions
The evidence for enhanced recovery schemes following gastric and oesophageal resection is weak, with only three (low volume) published randomised controlled trials. However, the enhanced recovery approach appears safe and may be associated with a reduction in length of stay.
Keywords: Oesophagectomy, Gastrectomy, Enhanced recovery
Surgical resection is central to curative treatment for both gastric and oesophageal cancer that has progressed beyond the earliest stages. It is, however, associated with high mortality and morbidity, with the National Oesophago-Gastric Cancer Audit reporting rates of 3.2% and 29.7% respectively for oesophageal resection, and 2.8% and 14.7% for gastric resection.1 The audit reports a median postoperative stay of 13 days for oesophageal and 11 days for gastric resection, increasing to 37 and 43 days respectively after an anastomotic leak. Following upper gastrointestinal (GI) resection, patients gain no quality of life benefit until at least two years postoperatively.2 Methods of reducing postoperative stay, improving quality of life and decreasing morbidity are of great importance.
Fast track or enhanced recovery surgery was introduced by Kehlet and Wilmore,3,4 resulting in a move towards standardised clinical care pathways and a multidisciplinary approach across surgery. There are 17 multimodal recognised elements of enhanced recovery. These bundles of care provide a structured pathway from preoperative through to postoperative care and discharge. This combination of factors is thought to reduce stress response and organ dysfunction.4 The enhancement of organ function in postoperative recovery aims to reduce morbidity, hospital stay and convalescence time.3,5 Modified for procedure specific characteristics, the benefits of fast track surgery have been demonstrated in colorectal surgery,6 pancreatic surgery7 and pulmonary resections.8
There is no current consensus on the essential components of enhanced recovery in gastric surgery and limited evidence in oesophageal surgery.9,10 This paper aims to review the current literature and provide a consensus on current published protocols for enhanced recovery following gastric and oesophageal resection.
Methods
Using PubMed, Ovid®, Embase and MEDLINE® as primary sources, two reviewers conducted an electronic literature search independently. No time limits were specified up to the date of the search (March 2014). A comprehensive search was performed using the search terms ‘oesophageal cancer’, ‘gastric cancer’, ‘enhanced recovery’ and ‘fast track surgery’. Logical combinations of these and related terms (oesophagus, stomach, gastric, neoplasm and carcinoma) were used to maximise the sensitivity of the search. The search was restricted to articles involving humans, with retrievable full text in the English language (or English abstract).
Selection process
Following identification of relevant titles, abstracts of these articles were read to decide study eligibility. The full text article was retrieved when the title and/or abstract appeared to meet the predefined eligibility criteria for this review. A manual cross-reference search of bibliographies was carried out to identify articles missed on the computerised search.
Data extraction and analysis
Each retrieved full text article was studied using a predesigned proforma to identify relevant components of enhanced recovery protocols and outcome criteria (Table 1). Owing to the limited number of studies addressing the study question, articles were not restricted to randomised controlled trials (RCTs) but also included comparative studies and case series. The primary outcome parameters assessed included 30-day in-hospital mortality, major morbidity (respiratory tract infection, anastomotic leak), length of hospital stay, reoperation rate and readmission rate. The components comprising the pathway were also assessed: preoperative information; day of admission; preoperative carbohydrate loading; bowel preparation; analgesia; planned length of stay in the intensive care unit (ICU); use of drains, catheters and nasogastric tubes; mobilisation; quality of life; contrast swallow; and nutrition.
Table 1.
Study variables
| Variable | Extracted data |
|---|---|
| Authors | All authors |
| Journal citation | Jounal name |
| Study design | Case series, case-controlled studies OR randomised controlled stdies |
| Number of patients studied | In enhanced recovery group and standard recovery group |
| Mortality | Number of deaths within 30 days OR not recorded |
| Morbidity | Overall stated complication rate OR not recorded |
| Anastomotic leak rate | Number of recorded leaks OR not reported |
| Respiratory tract infections | Total respiratory complications quoted OR not recorded |
| Reoperation rate | Number of patients requiring a second or subsequent operation OR not recorded |
| Length of intensive care stay | Mean time in days OR not recorded |
| Length of hospital stay | Mean time in days OR not recorded |
| Readmission rate | Number of patients readmitted to hospital following initial discharge OR not recorded |
| Failed fast track surgery | Number of patients taken off fast track regime OR not recorded |
Statistical analysis
Owing to reporting bias and considerable confounding factors such as patient selection, statistical significance tests for outcome comparison were not considered appropriate.
Results
The initial search identified 34 reports published between 1998 and 2014, of which 18 were suitable for quantitative synthesis (Fig 1). There were 11 articles (1,128 patients) on fast track oesophageal surgery11–21 and 7 (329 patients) on fast track gastric surgery.12,22–27 Ten articles were case series, five were case-controlled studies and three were RCTs (all gastrectomy related with a Jadad score of 1 or 2). All articles involved single centre data, most being small volume. (All had fewer than 100 patients except 2 oesophagectomy papers.)13,19 The indication for surgery was gastric or oesophageal cancer or high grade dysplasia in Barrett’s oesophagus. Oesophageal resections were performed as Ivor–Lewis, left thoracoabdominal or transhiatal resections. The gastric resections included distal, total and subtotal gastric resections.
Figure 1.
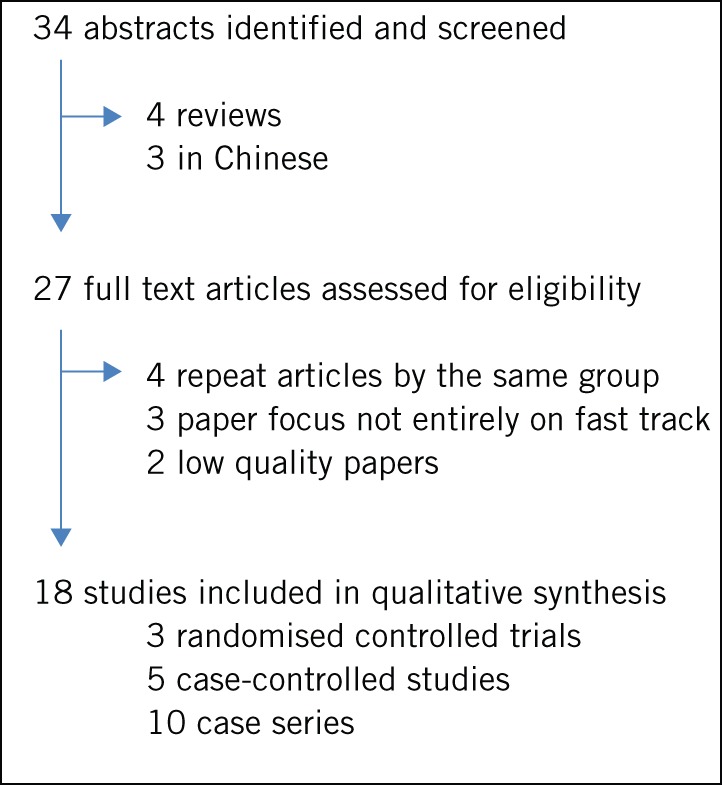
Study flow diagram
Components of oesophageal pathways
Three studies out of eleven provided no details about giving patients information regarding their fast track protocol prior to surgery (Table 2). There were no details regarding bowel preparation and one study used carbohydrate loading.13 Most studies used postoperative epidural analgesia. ICU use following surgery varied, with patients kept ventilated for 24–36 hours in the oldest study.21 However, more recent studies limited ICU stay to one day or less, with immediate postoperative extubation. (Cerfolio et al no longer admitted patients routinely to the ICU after the first 35 patients were fast tracked.)20
Table 2.
Oesophagectomy enhanced recovery pathway elements (numbers in days, earliest possible date given)
| Elements | Ford, 201411 | Tang, 201312 | Blom, 201313 | Lee, 201314 | Cao, 201315 | Preston, 201316 | Jianjun, 201217 | Munitiz, 201018 | Low, 200719 | Cerfolio, 200420 | Zehr, 199821 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Preoperative | |||||||||||
| Information about ERAS | ✓ | ✓ | ✓ | ✓ | ? | ✓ | ? | ✓ | ✓ | ✓ | ? |
| Admitted on day of surgery | ✓ | ✓ | ? | ? | ? | ? | ? | ? | ? | ✓ | ? |
| Oral carbohydrate loading | × | × | ✓ | × | × | ? | ? | ? | ? | ? | ? |
| Bowel preparation | × | × | ? | ? | × | ? | ? | ? | ? | ? | ? |
| Perioperative | |||||||||||
| Epidural | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Postoperative | |||||||||||
| Length of ICU stay | × | 1 | 1 | × | × | 2 | × | 4 | <18 | <24 | 1 |
| Early mobilisation | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ? | ✓ | ✓ | ✓ | ✓ |
| Supplemental nutrition | ✓ | × | ✓ | × | ✓ | ✓ | × | ✓ | ✓ | ✓ | ✓ |
| Urinary catheter removal | 3 | 6 | ? | 2 | 1 | 5 | 1 | 4 | ? | 3 | 2 |
| Chest drain removal | 5+6 | 5 | 2 | 5 | 3 | 3+6 | 1+3 | 4 | 1+3 | 1+2 | 4 |
| Contrast swallow | × | × | ? | × | ✓ | × | × | ✓ | ✓ | ✓ | ✓ |
| Nasogastric tube removal | 5 | 5 | 2 | 3 | × | 2 | 1 | 5 | 5 | 3 | ? |
| Predicted discharge | ? | 7 | ? | 7 | 7 | 7 | 7 | 7 | 7 | 7 | 10 |
✓ = yes; × = no; ? = no information given
ERAS = enhancced recovery after surgery; ICU = intensive care unit
All except one study aimed to mobilise the patient on the first postoperative day. Seven studies used jejunostomy feeding on days 1–3, with one study using total parenteral nutrition. Chest drain removal occurred early, all studies aiming for drain removal by day 5. Contrast swallows were used in five studies (days 4–6 following surgery); five studies did not routinely perform swallows. The nasogastric tube was removed between days 1 and 6 (most on day 5).
The predicted stay was 7–10 days across the studies. In the largest study, completion rates of these milestones were: immediate extubation (99%,) patient controlled epidural analgesia (98.5%) and day 1 mobilisation (85.9%).19 Two studies reported failure rates of their enhanced recovery programmes at 31% and 23% respectively (principally due to a postoperative complication). One study reported a significant association between neoadjuvant chemoradiotherapy and failure of enhanced recovery (33% compared with 11%, p=0.025), with this group having a higher rate of major complications (25% vs 8%, p=0.048).20
Components of gastric pathways
Preoperative information was reported in all but one of the gastric resection studies. Four groups gave preoperative carbohydrate drinks (one gave protein drinks) and bowel preparation was performed in one study (Table 3). No information was given regarding postoperative ICU stay in five studies and ICU was not used routinely in one study.26 Recommencing oral intake ranged from the day of surgery to three days postoperatively and only one study used a postoperative contrast swallow routinely.26 The predicted discharge day ranged from day 3 to day 7. One study gave details of fast track surgery failure: 5.5% of patients.19
Table 3.
Gastric resection enhanced recovery pathway elements (numbers in days, earliest possible date given)
| Elements | Tang, 201312 | Feng, 201322 | Kim, 201223 | Yamada, 201224 | Wang, 201025 | Grantcharov, 201026 | So, 200827 |
|---|---|---|---|---|---|---|---|
| Preoperative | |||||||
| Information about ERAS | ✓ | ✓ | ✓ | ? | ✓ | ✓ | ✓ |
| Admitted on day of surgery | ✓ | × | × | × | ✓ | ✓ | ? |
| Oral carbohydrate loading | × | ✓ | ✓ | ✓ | ✓ | × | × |
| Bowel preparation | × | ? | × | ✓ | × | × | ? |
| Perioperative | |||||||
| Epidural | ✓×** | × | × | ✓ | ✓ | × | ✓×* |
| Postoperative | |||||||
| Length of ICU stay | 1 | ? | ? | ? | ? | × | ? |
| Early mobilisation | ✓ | ✓ | ✓ | ✓ | ✓ | ? | ✓ |
| Supplemental nutrition | × | ✓ | × | × | × | × | ✓ |
| Nutrition (liquids commenced) | 5 | 0 | 2 | 2 | 1 | 1 | 3 |
| Urinary catheter removal | 6 | <1 | 2 | ? | 1 | 1 | ? |
| Contrast swallow | × | × | × | ? | × | ✓ | ? |
| Nasogastric tube removal | 5 | <1 | × | Immediate | × | × | 1 |
| Predicted discharge | 7 | ? | 4 | 7 | 4 | 3 | ? |
ERAS = enhancced recovery after surgery; ICU = intensive care unit
choice of anaesthetic;
or wound infusion catheter
Oesophageal resection
The 30-day mortality rate was 0–5.6% (pooled mortality 0.8%, 9/1,075) in those undergoing fast track surgery compared with 0–5% (pooled estimate 2.8%, 12/431) in those undergoing conventional surgery (Table 4). The reported morbidity rate was 16.7–75% in the fast track group (pooled estimate 38.6%, 396/1,026), with those undergoing conventional recovery programmes having a morbidity rate of 51.2% (198/387). Of the major complications, 5.2% (51/979) were due to anastomotic leaks compared with 13.1% (43/328) in the conventional group. The median length of stay was 7–14 days (14.4 days in the conventional group). Of the two studies reporting costs for fast track protocol, there was a significant reduction ($21,977 vs $17,919, p<0.05)21 and €1,055 cost saving per patient.14
Table 4.
Summary of outcomes following oesophageal surgery and fast track surgery
| Study | Study group (n) | 30-day mortality (%) | Morbidity (%) | Reoperation (%) | Length of hospital stay (days) | Readmission (%) | Anastomotic leak (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases | Controls | Cases | Controls | Cases | Controls | Cases | Controls | Cases | Controls | Cases | Controls | Cases | Controls | |
| Ford, 201411 | 75 | 80 | 0 | 1.3 | 64 | 52 | – | – | 10** | 13** | 13.0 | 11.0 | 4.0 | 14.0 |
| Tang, 201312 | 36 | 27 | 5.6 | 3.7 | 16.7 | 25.9 | – | – | 11** | 15** | 19.4 | 14.8 | 2.8 | 11.1 |
| Blom, 201313 | 103 | 78 | 4 | – | 71 | 68 | – | – | 14** | 15** | 10.0 | 8.0 | 15.0 | 23.0 |
| Lee, 201314 | 47 | 59 | – | – | 59 | 62 | – | – | 8** | 10** | 3.0 | 4.0 | – | – |
| Cao, 201315 | 55 | 57 | 2 | 5 | 29 | 47 | – | – | 8** | 15** | 4.0 | 5.0 | 7.0 | 11.0 |
| Preston, 201316 | 12 | 12 | 0 | 0 | 75 | 33.3 | 8.3 | 8.3 | 7** | 17** | – | – | 8.3 | 8.3 |
| Jianjun, 201217 | 80 | – | 0 | – | 20 | – | – | – | 7.8* | – | 0.0 | – | 0.0 | – |
| Munitiz, 201018 | 74 | 74 | 1 | 5 | 31 | 38 | – | – | 9** | 13** | 4.5 | 6.5 | 7.0 | 8.0 |
| Low, 200719 | 340 | – | 0.3 | – | 45 | – | 2.9 | – | 11.5* | – | – | – | 3.8 | – |
| Cerfolio, 200420 | 90 | – | 4.4 | – | 26.6 | – | – | – | 7** | – | 4.4 | – | 0.0 | – |
| Zehr, 199821 | 96 | 56 | 0 | 3.6 | – | – | – | – | 9.5* | 13.6* | – | – | – | – |
| Total† | 1,122 | 443 | 0.8 | 2.8 | 38.6 | 51.2 | 5.3 | 7.7 | 5.2 | 13.1 | ||||
mean;
median;
weighted outcomes
Gastric resection
There were no deaths within 30 days of surgery in the fast track groups and there was a 1% (3/309) mortality rate in the control groups across 6 studies (Table 5). The reported morbidity rate was 5.3–39.0% (16.5%, 54/329) compared with 12.0–39.0% (19.4%, 60/309) in the conventional group. The main morbidity reported was anastomotic leak (1.2% [11/329] vs 0.6% [2/309] in the conventional group). Length of stay was reported as mean and median, with a pooled mean of 5 days and a median of 6–11 days. The 30-day readmission rate was 8.0% (19/238) vs 3.7% (89.5/253). One study reported quality of life, with a significantly higher score following fast track surgery (14.7 vs 15.7, p<0.05).26 Three studies reported cost reduction following the implementation of a fast track protocol (RMB 43,783 [$7,000] vs RMB 39,598 [$6,300], p=0.005; RMB 31,125 [$5,000] vs RMB 26,993 [$4,300], p<0.001; and SGD 17,371 [$13,900] vs SGD 13,338 [$10,700], p=0.047).22,25,27
Table 5.
Summary of outcomes following gastric resection and fast track surgery
| Study | Study group (n) | 30-day mortality (%) | Morbidity (%) | Reoperation (%) | Length of hospital stay (days) | Readmission (%) | Anastomotic leak (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases | Controls | Cases | Controls | Cases | Controls | Cases | Controls | Cases | Controls | Cases | Controls | Cases | Controls | |
| Tang, 201312 | 19 | 26 | 0.0 | 0.0 | 5.3 | 23.1 | – | – | 11** | 15** | 21.1 | 7.7 | 5.3 | 0.0 |
| Feng, 201322 | 59 | 60 | 0.0 | 0.0 | 6.0 | 17.0 | 0.0 | 1.0 | 5.7* | 7.1* | 0.0 | 0.0 | 0.0 | 0.0 |
| Kim, 201223 | 22 | 22 | 0.0 | 0.0 | 13.6 | 18.2 | – | – | 5.4* | 8.0* | 4.5 | 0.0 | 0.0 | 0.0 |
| Yamada, 201224 | 91 | 100 | 0.0 | 0.0 | 7.6 | 12.0 | – | – | 9.0** | 9.0** | – | – | 1.0 | 2.0 |
| Wang, 201025 | 45 | 47 | 0.0 | 0.0 | 20.0 | 14.9 | – | – | 6.0** | 8.0** | 2.2 | 2.1 | 0.0 | 0.0 |
| Grantcharov, 201026 | 32 | – | 0.0 | – | 25.0 | – | 3.1 | – | 5.2* | – | 6.3 | – | 3.1 | – |
| So, 200827 | 61 | 54 | 0.0 | 5.6 | 39.0 | 38.9 | – | – | 8.9* | 11.0* | 18.0 | 13.0 | 1.6 | 0.0 |
| Total† | 329 | 309 | 0 | 1 | 16.5 | 19.4 | 8 | 3.7 | 1.2 | 0.6 | ||||
mean;
median;
weighted outcomes
Discussion
The evidence supporting enhanced recovery pathways following upper GI resection is currently limited. No standard protocol has been adopted and no protocol encompasses all of the key facets of enhanced recovery. Other review articles such as those by Findlay et al9 and Dorcaratto et al10 in oesophageal surgery suggest acceptable outcomes following enhanced recovery programmes in upper GI resection. Readmission and reoperation rates appear low throughout.
Limitations
This review outlines the limited literature on enhanced recovery schemes following upper GI surgery. The quality of included studies is generally poor, many are retrospective and there were only three RCTs, all single centre22,23,25 with only one blinded.22 The maximum number per arm in any of the studies was 61 patients and all excluded those undergoing neoadjuvant chemo or radiotherapy. Restricting our review to the English language literature may have led to the omission of some studies but this is unlikely to have influenced our summary outcome estimates.28–30 Among the published literature, those papers with significant results are more likely to be published in English, to be cited and published repeatedly, leading to English language bias, citation and multiple publication bias.31 Previous work suggests that studies omitted by this restriction are likely to be smaller and of lower quality than those included.32
All articles stated consecutive patient inclusion in their studies. Despite this, selection bias may have influenced reported results. Some studies failed to give full results following pathway implementation, causing further potential bias. Geographical differences in patients, selection for surgery and healthcare systems in place may also play a role given the diverse populations from which the studies were drawn.
The reported 30-day mortality rates in these series of 0.8% and 0% fall below the 1.7% and 1.1% reported in the 2013 UK national audit for upper GI resections.1 This may represent reporting bias or it could be due to the dominance of Low et al’s oesophagectomy series of 340 patients (mortality 0.3%).19 The morbidity rate following fast track oesophageal resection was significant at 38.6% but less than that reported in the control groups (51.2%). It is, however, greater than the 29.7% reported in the national audit and may be due to morbidity misclassification, given the limited reporting in some of the studies. Morbidity following gastric resections (16.5%) was comparable with that reported in the UK national audit (14.7%)1 but length of stay was shorter. The average stay exceeded the target length of stay in all studies, likely owing to postoperative complications.
This review notes a potential relationship between failure of a fast track protocol and increased complications following chemoradiotherapy.20 Although this may have implications, the finding should be treated with caution as the study was low volume. Other studies, using neoadjuvant chemotherapy alone, such as the trial by Cunningham et al,33 found no increased complications.
The ‘typical’ enhanced recovery pathway for oesophagectomy encompassed provision of enhanced recovery information, use of epidural anaesthesia, early mobilisation and supplemental nutrition in the postoperative period. The greatest variance surrounds postoperative nutrition supplementation (none, jejunostomy, total parenteral nutrition), length of ICU stay and recommencement of oral intake (use of contrast studies and removal of nasogastric tubes). Length of ICU stay ranged across oesophageal resection groups, with a trend towards reducing ICU use, clearly resulting in reduced costs. Contrast swallow use following oesophageal resection was reported in five studies. Nevertheless, previous studies demonstrate swallows have low sensitivity and a low positive predictive value for detecting anastomotic leaks.34
Consistent elements of gastrectomy enhanced recovery pathways include information provision, early mobilisation, drain and nasogastric tube removal, not using contrast swallow studies and early resumption of oral intake. The biggest differences in enhanced recovery protocols for gastrectomies were preoperative carbohydrate loading and epidural use.
Five studies reported on cost effectiveness following the introduction of fast track protocols (3 gastric, 2 oesophageal).14,21,22,25,27 All reported cost reduction. On the other hand, no detailed economic analysis was performed and they were limited to in-hospital costs. Only one paper addressed quality of life following gastric resection, the fast track group having significantly higher scores on discharge.25
Conclusions
There are limited data available on the use of fast track protocols in oesophagogastric surgery. Its high risk nature has undoubtedly limited its uptake and caused varied use of certain elements. However, evidence is growing of its safety, common acceptable principles and modest, achievable benefits. Future work is required to fine-tune elements to allow its widespread adoption.
References
- 1.National Oesophago-Gastric Cancer Audit 2013. London: RCS; 2013. [Google Scholar]
- 2.Blazeby JM, Farndon JR, Donovan J, Alderson D. A prospective longitudinal study examining the quality of life of patients with esophageal carcinoma. Cancer 2000; 88: 1,781–1,787. [PubMed] [Google Scholar]
- 3.Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg 2002; 183: 630–641. [DOI] [PubMed] [Google Scholar]
- 4.Wilmore DW, Kehlet H. Management of patients in fast track surgery. BMJ 2001; 322: 473–476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kehlet H, Dahl JB. Anaesthesia, surgery, and challenges in postoperative recovery. Lancet 2003; 362: 1,921–1,928. [DOI] [PubMed] [Google Scholar]
- 6.Eskicioglu C, Forbes SS, Aarts MA et al. Enhanced recovery after surgery (ERAS) programs for patients having colorectal surgery: a meta-analysis of randomized trials. J Gastrointest Surg 2009; 13: 2,321–2,329. [DOI] [PubMed] [Google Scholar]
- 7.Ypsilantis E, Praseedom RK. Current status of fast-track recovery pathways in pancreatic surgery. JOP 2009; 10: 646–650. [PubMed] [Google Scholar]
- 8.Tovar EA, Roethe RA, Weissig MD et al. One-day admission for lung lobectomy: an incidental result of a clinical pathway. Ann Thorac Surg 1998; 65: 803–806. [PubMed] [Google Scholar]
- 9.Findlay JM, Gillies RS, Millo J et al. Enhanced recovery for esophagectomy: a systematic review and evidence-based guidelines. Ann Surg 2014; 259: 413–431. [DOI] [PubMed] [Google Scholar]
- 10.Dorcaratto D, Grande L, Pera M. Enhanced recovery in gastrointestinal surgery: upper gastrointestinal surgery. Dig Surg 2013: 30: 70–78. [DOI] [PubMed] [Google Scholar]
- 11.Ford SJ, Adams D, Dudnikov S et al. The implementation and effectiveness of an enhanced recovery programme after oesophago-gastrectomy: a prospective cohort study. Int J Surg 2014: 12: 320–324. [DOI] [PubMed] [Google Scholar]
- 12.Tang J, Humes DJ, Gemmill E et al. Reduction in length of stay for patients undergoing oesophageal and gastric resections with implementation of enhanced recovery packages. Ann R Coll Surg Engl 2013; 95: 323–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blom RL, van Heijl M, Bemelman WA et al. Initial experiences of an enhanced recovery protocol in esophageal surgery. World J Surg 2013; 37: 2,372–2,378. [DOI] [PubMed] [Google Scholar]
- 14.Lee L, Li C, Robert N et al. Economic impact of an enhanced recovery pathway for oesophagectomy. Br J Surg 2013; 100: 1,326–1,334. [DOI] [PubMed] [Google Scholar]
- 15.Cao S, Zhao G, Cui J et al. Fast-track rehabilitation program and conventional care after esophagectomy: a retrospective controlled cohort study. Support Care Cancer 2013; 21: 707–714. [DOI] [PubMed] [Google Scholar]
- 16.Preston SR, Markar SR, Baker CR et al. Impact of a multidisciplinary standardized clinical pathway on perioperative outcomes in patients with oesophageal cancer. Br J Surg 2013; 100: 105–112. [DOI] [PubMed] [Google Scholar]
- 17.Jianjun Q, Yin L, Wenqun X et al. Fast track program for esophagectomy patients. Thorac Cancer 2012; 3: 55–59. [DOI] [PubMed] [Google Scholar]
- 18.Munitz V, Martinez-de-haro LF, Ortiz A et al. Effectiveness of a written clinical pathway for enhanced recovery after transthoracic (Ivor Lewis) oesophagectomy. Br J Surg 2010; 97: 714–718. [DOI] [PubMed] [Google Scholar]
- 19.Low DE, Kunz S, Schembre D et al. Esophagectomy – it’s not just about mortality anymore: standardized perioperative clinical pathways improve outcomes in patients with esophageal cancer. J Gastrointest Surg 2007; 11: 1,395–1,402. [DOI] [PubMed] [Google Scholar]
- 20.Cerfolio RJ, Bryant AS, Bass CS et al. Fast tracking after Ivor Lewis esophagogastrectomy. Chest 2004; 126: 1,187–1,194. [DOI] [PubMed] [Google Scholar]
- 21.Zehr KJ, Dawson PB, Yang SC, Heitmiller RF. Standardized clinical care pathways for major thoracic cases reduce hospital costs. Ann Thorac Surg 1998; 66: 914–919. [DOI] [PubMed] [Google Scholar]
- 22.Feng F, Ji G, Li JP et al. Fast-track surgery could improve postoperative recovery in radical total gastrectomy patients. World J Gastroenterol 2013; 19: 3,642–3,648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim JW, Kim WS, Cheong JH et al. Safety and efficacy of fast-track surgery in laparoscopic distal gastrectomy for gastric cancer: a randomized clinical trial. World J Surg 2012; 36: 2,879–2,887. [DOI] [PubMed] [Google Scholar]
- 24.Yamada T, Hayashi T, Cho H et al. Usefulness of enhanced recovery after surgery protocol as compared with conventional perioperative care in gastric surgery. Gastric Cancer 2012; 15: 34–41. [DOI] [PubMed] [Google Scholar]
- 25.Wang D, Kong Y, Zhong B et al. Fast-track surgery improves postoperative recovery in patients with gastric cancer: a randomized comparison with conventional postoperative care. J Gastrointest Surg 2010; 14: 620–627. [DOI] [PubMed] [Google Scholar]
- 26.Grantcharov TP, Kehlet H. Laparoscopic gastric surgery in an enhanced recovery programme. Br J Surg 2010; 97: 1,547–1,551. [DOI] [PubMed] [Google Scholar]
- 27.So JB, Lim ZL, Lin HA, Ti TK. Reduction of hospital stay and cost after the implementation of a clinical pathway for radical gastrectomy for gastric cancer. Gastric Cancer 2008; 11: 81–85. [DOI] [PubMed] [Google Scholar]
- 28.Jüni P, Holenstein F, Sterne J et al. Direction and impact of language bias in meta-analyses of controlled trials: empirical study. Int J Epidemiol 2002; 31: 115–123. [DOI] [PubMed] [Google Scholar]
- 29.Egger M, Zellweger-Zähner T, Schneider M et al. Language bias in randomised controlled trials published in English and German. Lancet 1997; 350: 326–329. [DOI] [PubMed] [Google Scholar]
- 30.Moher D, Fortin P, Jadad AR et al. Completeness of reporting of trials published in languages other than English: implications for conduct and reporting of systematic reviews. Lancet 1996; 347: 363–366. [DOI] [PubMed] [Google Scholar]
- 31.Egger M, Smith GD. Bias in location and selection of studies. BMJ 1998; 316: 61–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Miller JN, Colditz GA, Mosteller F. How study design affects outcomes in comparisons of therapy. II: Surgical. Stat Med 1989; 8: 455–466. [DOI] [PubMed] [Google Scholar]
- 33.Cunningham D, Allum WH, Stenning SP et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med 2006; 355: 11–20. [DOI] [PubMed] [Google Scholar]
- 34.Boone J, Rinkes IB, van Leeuwen M, van Hillegersberg R. Diagnostic value of routine aqueous contrast swallow examination after oesophagectomy for detecting leakage of the cervical oesophagogastric anastomosis. ANZ J Surg 2008; 78: 784–790. [DOI] [PubMed] [Google Scholar]


