Abstract
Introduction
The aim of this study was to analyse the treatment and management of renal injury patients presenting to our major trauma unit to determine the likelihood of patients needing immediate nephrectomy.
Methods
The Trauma Audit and Research Network (TARN) database was used to review trauma cases presenting to our department between February 2009 and September 2013. Demographic data, mechanism and severity of injury, grade of renal trauma, management and 30-day outcome were determined from TARN data, electronic patient records and imaging.
Results
There were a total of 1,856 trauma cases, of which 36 patients (1.9%) had a renal injury. In this group, the median age was 28 years (range: 16–92 years), with 28 patients (78%) having blunt renal trauma and 8 (22%) penetrating renal trauma. The most common cause for blunt renal trauma was road traffic accidents. Renal trauma cases were stratified into American Association for the Surgery of Trauma (AAST) grades (grade I: 19%, grade II: 22%, grade III: 28%, grade IV: 28%, grade V: 0%). All patients with grade I and II injuries were treated conservatively. There were three patients (1 with grade III and 2 with grade IV renal injuries) who underwent radiological embolisation. One of these patients went on to have a delayed nephrectomy owing to unsuccessful embolisation.
Conclusions
Trauma patients rarely require emergency nephrectomy. Radiological selective embolisation provides a good interventional option in cases of active bleeding from renal injury in haemodynamically stable patients. This has implications for trauma care and how surgical cover is provided for the rare event of nephrectomy.
Keywords: Renal, Trauma, Management
The National Health Service has seen major changes with attempts at greater centralisation of services to high volume centres, most notably in cancer care. Such centralisation has also occurred in the area of trauma, with the development of major trauma centres, the rationale being that units with high volume trauma will have better expertise in dealing with such cases, with resultant better outcomes.1 The greatest experience of such centralisation has been in North America, which is reflected in the published literature. London experiences approximately 1,600 major trauma cases each year, most of which are treated in one of the four major trauma centres. Our institution is one such trauma centre, based at St Mary’s Hospital and serving the north west of the city.
Renal trauma typically constitutes 1–5% of all trauma cases,2–4 the majority being blunt trauma (80–95%).5 Penetrating renal trauma is less common but comprises up to 20% of renal trauma cases in urban areas.6,7 Life threatening haemodynamic instability due to renal haemorrhage remains an absolute indication for surgical exploration. However, conservative management where possible, consisting of careful observation and bed rest, has been shown to result in a lower nephrectomy rate with no increased morbidity or mortality.2 Consequently, there is consensus that non-operative management of renal trauma is often safe for all but the most severe cases of renal injury in haemodynamically stable patients.8–11 Our aim was to analyse the management of renal trauma patients in our trauma unit, with a view to determining the likelihood of such patients requiring immediate nephrectomy.
Methods
All significant trauma cases admitted to our institution over a 56-month period, from the time of inception of the London trauma system (February 2009 to September 2013 inclusive) were analysed using the national Trauma Audit and Research Network (TARN) database. TARN collates data on significant trauma cases presenting to all TARN participating hospitals, which include all major trauma centres in the UK.
TARN defines significant trauma cases as those requiring either: 1) >72 hours of hospital admission, 2) high dependency unit (HDU) or critical care admission, 3) transfer to another centre for specialist care, HDU care or critical care, or 4) trauma related deaths. In addition, each case must have evidence of at least one form of traumatic injury.
Data of cases to be included in the TARN database are collated by dedicated TARN staff in trauma units, with potential TARN patients identified through analysis of all patients admitted as a trauma call, as part of the London Trauma System. Furthermore, any patients who have trauma coded as the presenting complaint (including shootings, stabbings, falls, non-accidental injuries, vehicle or sporting incidents, fires or assaults) on their electronic discharge summary are regarded as potential TARN patients. Once a TARN patient is discharged or dies, the complete patient notes are analysed and if the patient meets TARN inclusion criteria, the data are added to a national electronic data collection and reporting system.
For any case with renal injury, our electronic patient record and imaging systems were reviewed to collect demographic data, mechanism and severity of injury, presence and grade of renal trauma, and 30-day outcome. Computed tomography for patients with renal trauma was reviewed retrospectively by a consultant uroradiologist (blinded to the original reports) and the severity of renal injury was graded according to the American Association for the Surgery of Trauma (AAST) classification (Table 1). The management and any interventions were recorded for all renal trauma cases.
Table 1.
American Association for the Surgery of Trauma kidney injury scale
| Grade | Nature of injury | Description of injury |
|---|---|---|
| I | Contusion | Microscopic or gross haematuria, urological studies normal |
| Haematoma | Subcapsular, non-expanding without parenchymal laceration | |
| II | Haematoma | Non-expanding perirenal haematoma confirmed to renal retroperitoneum |
| Laceration | <1.0cm parenchymal depth of renal cortex without urinary extravasation | |
| III | Laceration | >1.0cm parenchymal depth of renal cortex without collecting system rupture or urinary extravasation |
| IV | Laceration | Parenchymal laceration extending through renal cortex, medulla and collecting system |
| Vascular | Main renal artery or vein injury with contained haemorrhage | |
| V | Laceration | Completely shattered kidney |
| Vascular | Avulsion of renal hilum, which devascularises kidney |
Results
A total of 1,856 significant trauma cases presented to our institution during the study period. Of these cases, 36 patients (27 male, 9 female; 1.9%) had a renal injury. The mechanisms and grading of the injuries are outlined in Table 2. The median patient age was 28 years (range: 16–92 years).
Table 2.
Renal trauma cases by American Association for the Surgery of Trauma grade and mechanism
| Grade I | Grade II | Grade III | Grade IV | Grade V | Total | |
|---|---|---|---|---|---|---|
| Blunt injury | 7 | 7 | 7 | 7 | 0 | 28 |
| Road traffic accident | 3 | 3 | 6 | 3 | 0 | 14 |
| Fall | 4 | 3 | 1 | 4 | 0 | 13 |
| Blow | 0 | 1 | 0 | 0 | 0 | 1 |
| Penetrating injury | 0 | 2 | 3 | 3 | 0 | 8 |
| Stabbing | 0 | 1 | 3 | 2 | 0 | 6 |
| Shooting | 0 | 1 | 0 | 1 | 0 | 2 |
| Total | 7 (19%) | 9 (25%) | 10 (28%) | 10 (28%) | 0 (0%) | 36 (100%) |
Blunt trauma accounted for 28 cases (78%) with 8 cases (22%) being caused by a penetrating mechanism of injury. The most common cause of blunt trauma was road traffic accidents (n=14, 50%) while other causes included falls from heights and blows to the abdomen. Penetrating injuries comprised shootings and stabbings, all of which occurred to men aged between 18 and 30 years.
The majority of renal trauma observed was classified as AAST grade III (28%) or grade IV (28%). A smaller proportion had lower severity renal injury (22% grade II and 19% grade I). No AAST grade V renal injury cases occurred throughout the study period (Fig 1).
Figure 1.
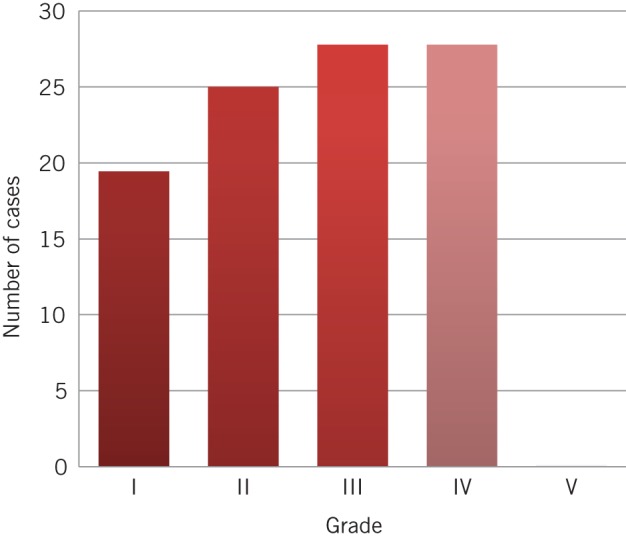
Proportion of renal trauma by American Association for the Surgery of Trauma grade
Management of cases
The management of the majority (89%) of renal trauma cases in this period was conservative, with all grade I and II injuries being managed conservatively. Three patients required intervention; all underwent radiological embolisation. This occurred within 24 hours (Table 3). For one patient (Patient B), the embolisation was unsuccessful, requiring further emergency surgical exploration resulting in a nephrectomy, which occurred more than 24 hours following admission and attempted embolisation.
Table 3.
Time from admission to intervention
| Patient | Time of admission | Time of embolisation | Time of nephrectomy |
|---|---|---|---|
| A | 2.40am | 3.00pm – 4.40pm (+ 12h 20m) | – |
| B | 4.37am | 6.42am – 7.47am (+ 2h 5m) | 10.00am (+24h) (+ 29h 23m) |
| C | 4.24am | 5.42pm – 6.42pm (+ 13h 18m) | – |
All three patients requiring intervention sustained their injury as a result of stabbing (ie penetrating trauma). All suffered a grade III or IV renal injury and as there were ten patients in each of these groups in total, this equated to a 10% intervention rate for grade III injuries and a 20% intervention rate for grade IV injuries. All patients survived to 30 days after admission.
The mortality rate for significant trauma patients with renal injuries was 8.3% over the study period. Of these mortalities, all patients had suffered polytrauma with significant head and/or intrathoracic injuries. Renal injury in the patients who died was low grade (I and II) and was not considered to be the cause of death.
Discussion
Data was collected prospectively by dedicated TARN staff based at our institution, and should therefore be accurate and consistent. This is the first UK-based study of renal trauma and its management using the TARN database. It is a large study encompassing a significant period of time.
TARN is a non-governmental organisation in the UK established to drive improvements in trauma care through supporting audit and research. It collates data on significant trauma cases presenting to all TARN participating hospitals, which include all major trauma centres in the UK. As such, TARN provides an invaluable resource for research into trauma care, providing a mechanism for the collation of nationwide data on trauma cases.
However, there is likely to be a selection bias towards high grade renal trauma in this study as the TARN database only captures significant trauma cases as defined by meeting one of its four criteria (outlined above). Such criteria specify that cases must have extended and/or specialised hospital treatment or resulted in death following injury. TARN data are therefore not likely to capture all renal trauma (ie those with minor injuries resulting in low grade renal trauma not requiring a hospital stay of >72 hours or needing an advanced level care) and the population in this dataset is likely to represent a skewed bias towards higher grade renal injury. As a result, the actual rate of grade I injury may actually be higher than reported in this study.
Is urological surgical intervention a common occurrence for renal trauma?
The incidence of renal trauma presenting to our institution, a major trauma centre for London, is broadly in keeping with other international comparisons.6,7,10 We observed a greater proportion of renal trauma resulting from blunt mechanism of injury (particularly as a result of road traffic accidents), rather than penetrating mechanisms. The rates of penetrating injury leading to renal trauma seen in this study are comparable with those from international studies in urban settings, reflecting our experience in a major city.5,6
The majority of renal trauma cases at our institution are managed conservatively, including all blunt trauma cases and all cases graded I and II. The intervention rate equated to just under 1 case per year, with only 1 nephrectomy needed during the entire 56 months of the study period. Of the 85% of grade III and IV renal trauma cases managed conservatively, all patients survived to 30 days following injury, supporting previously reported evidence that intervention is not required in such cases, even when injury is deemed to be of high grade severity.
Comparison of radiological intervention in similar renal trauma series
In our institution, renal artery embolisation was the first intervention of choice in all three cases, with two of them being successful. Renal artery embolisation has had a similar success rate in other studies. In one study of 26 patients, 17 (65%) had successful angiography and endovascular treatment for renal haemorrhage,12 and a study of blunt renal injury found 18 (73%) of 22 cases of renal artery embolisation were successful while 6 required further laparotomy.13 An Australian study from 2013 reported a success rate of 88% for cases undergoing embolisation.10
A further study examining the US National Trauma Data Bank® showed that of over 9,000 renal injuries, 77 angioembolisations were performed, and although a high need for successive embolisations was identified (88%), the renal salvage rate was also high (92%).14 Consequently, the use of interventional radiology in the treatment of renal trauma is becoming widely accepted and offers a significant advance in the treatment of renovascular injury. Renal artery embolisation is a less invasive treatment option than surgical intervention, providing a high renal salvage rate with lower complication rates and reduced length of hospital stay compared with surgical intervention.15 In accordance with this, guidelines on urological trauma produced by the European Association of Urology (EAU) recommend that haemodynamically stable patients with renal injury of grade III or higher and active bleeding should be considered for formal angiography followed by embolisation.2
Implications for urology
As seen from our experience in a major trauma centre, the need for nephrectomy due to renal trauma is exceedingly rare and this is reflected in other similar studies. The modern day urologist should be able to manage such patients in an acute setting along with other members of the trauma team but is unlikely to need to perform an emergency nephrectomy. Modern trainees are less experienced in undertaking emergency nephrectomy and this is unlikely to change owing to the low emergency nephrectomy rates even in a major trauma centre. There has also been an emergence of dedicated trauma surgeons in certain UK trauma centres, which may affect training opportunities.
In order to gain adequate exposure to emergency trauma nephrectomy, current trainees may need to seek experience in regions of the world where penetrating trauma is more prevalent and interventional radiology is not available. The need for interventional radiological expertise is highlighted by the EAU guidelines2 and is reflected by the success of renal artery embolisation in two out of three cases in our unit. In the context of urological trauma, our findings support the need for trauma services to be delivered in dedicated high volume trauma centres, where interventional radiological expertise is available 24 hours a day and seven days a week.
In the era of modern trauma management, the issue of a newly appointed on-call urologist having the required skillset to perform an emergency nephrectomy is problematic because of the low exposure to such cases during training. This further supports the centralisation of trauma to specialised units where possible, to a place where a broad range of surgical expertise is available in one unit. It may be suggested that separate ‘nephrectomy rotas’ could provide a solution to the varied skill mix among urologists covering major trauma centres. Such rotas would involve cross-specialty participation from urologists performing high volume elective nephrectomy, transplant surgeons and vascular surgeons, and could potentially be regional in urban areas, thereby drawing on expertise from surrounding centres to cover the rare eventuality of nephrectomy being required in the trauma setting. As on-call duties and rotas remain highly topical for qualified urologists and trainees alike, this dialogue is vital.
Conclusions
Renal trauma is likely to be low grade (I/II) in nature and can be managed conservatively in the majority of cases even if it is more severe. In the rare need for intervention, selective renal artery embolisation provides a safe and effective solution, with the likelihood of requiring a nephrectomy being extremely rare. Given the low numbers of emergency nephrectomies, trauma centre cover for the rare eventuality of an ‘emergency nephrectomy’ in urban areas may need to be provided by surgeons on a ‘regional’ nephrectomy rota, where the elective nephrectomy workload may have a bearing on who delivers this care.
References
- 1.Metcalfe D, Bouamra O, Parsons NR et al. Effect of regional trauma centralization on volume, injury severity and outcomes of injured patients admitted to trauma centres. Br J Surg 2014; 101: 959–964. [DOI] [PubMed] [Google Scholar]
- 2.European Association of Urology. Guidelines on Urological Trauma. Arnhem, Netherlands: EAU; 2013. [Google Scholar]
- 3.McAninch JW. Genitourinary trauma. World J Urol 1999; 17: 65. [DOI] [PubMed] [Google Scholar]
- 4.Meng MV, Brandes SB, McAninch JW. Renal trauma: indications and techniques for surgical exploration. World J Urol 1999; 17: 71–77. [DOI] [PubMed] [Google Scholar]
- 5.Krieger JN, Algood CB, Mason JT et al. Urological trauma in the Pacific Northwest: etiology, distribution, management and outcome. J Urol 1984; 132: 70–73. [DOI] [PubMed] [Google Scholar]
- 6.Kansas BT, Eddy MJ, Mydlo JH, Uzzo RG. Incidence and management of penetrating renal trauma in patients with multiorgan injury: extended experience at an inner city trauma center. J Urol 2004; 172(4 Pt 1): 1,355–1,360. [DOI] [PubMed] [Google Scholar]
- 7.Sagalowsky AI, McConnell JD, Peters PC. Renal trauma requiring surgery: an analysis of 185 cases. J Trauma 1983; 23: 128–131. [PubMed] [Google Scholar]
- 8.Altman AL, Haas C, Dinchman KH, Spirnak JP. Selective nonoperative management of blunt grade 5 renal injury. J Urol 2000; 164: 27–30. [PubMed] [Google Scholar]
- 9.Robert M, Drianno N, Muir G et al. Management of major blunt renal lacerations: surgical or nonoperative approach? Eur Urol 1996; 30: 335–339. [DOI] [PubMed] [Google Scholar]
- 10.Shoobridge JJ, Bultitude MF, Koukounaras J et al. A 9-year experience of renal injury at an Australian level 1 trauma centre. BJU Int 2013; 112(Suppl 2): 53–60. [DOI] [PubMed] [Google Scholar]
- 11.Wessells H, McAninch JW, Meyer A, Bruce J. Criteria for nonoperative treatment of significant penetrating renal lacerations. J Urol 1997; 157: 24–27. [PubMed] [Google Scholar]
- 12.Breyer BN, McAninch JW, Elliott SP, Master VA. Minimally invasive endovascular techniques to treat acute renal hemorrhage. J Urol 2008; 179: 2,248–2,252. [DOI] [PubMed] [Google Scholar]
- 13.Menaker J, Joseph B, Stein DM, Scalea TM. Angiointervention: high rates of failure following blunt renal injuries. World J Surg 2011; 35: 520–527. [DOI] [PubMed] [Google Scholar]
- 14.Hotaling JM, Sorensen MD, Smith TG et al. Analysis of diagnostic angiography and angioembolization in the acute management of renal trauma using a national data set. J Urol 2011; 185: 1,316–1,320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sarani B, Powell E, Taddeo J et al. Contemporary comparison of surgical and interventional arteriography management of blunt renal injury. J Vasc Interv Radiol 2011; 22: 723–728. [DOI] [PubMed] [Google Scholar]


