Abstract
Introduction
There has been a significant rise in the volume of subacromial decompression surgery performed in the UK. This study aimed to determine whether arthroscopic subacromial decompression improves health related quality of life in a cost effective manner.
Methods
Patients undergoing arthroscopic subacromial decompression surgery for impingement were enrolled between 2012 and 2014. The Oxford shoulder score and the EQ-5D™ instruments were completed prior to and following surgery. A cost–utility analysis was performed.
Results
Eighty-three patients were eligible for the study with a mean follow-up duration of 15 months (range: 4–27 months). The mean Oxford shoulder score improved by 13 points (95% confidence interval [CI]: 11–15 points). The mean health utility gain extrapolated from the EQ-5D™ questionnaire improved by 0.23 (95% CI: 0.16–0.30), translating to a minimum cost per QALY of £5,683.
Conclusions
Subacromial decompression leads to significant improvement in function and quality of life in a cost effective manner. This provides justification for its ongoing practice by appropriately trained shoulder surgeons in correctly selected patients.
Keywords: Subacromial decompression, Impingement, Patient reported outcome measures, Cost effectiveness, Cost–utility
Subacromial decompression is being performed increasingly in the UK with epidemiological data showing intervention rates rising from 5.2 per 100,000 in 2001–2002 to 40.2 per 100,000 in 2009–2010.1 This has occurred against a background of controversy as to the efficacy of this intervention, with some suggesting there is no benefit of subacromial decompression over and above a structured exercise programme.2 Nevertheless, there is a cohort of patients who fail conservative treatment with injection therapy and a physiotherapy programme, and for these patients, surgery is frequently the only recourse. With such a substantial rise in surgical intervention rates combined with an element of controversy, it is of vital importance to understand whether subacromial decompression procedures are leading to health gains and improvements in quality of life, and, furthermore, whether they are cost effective in doing so.
The quality adjusted life year (QALY) is an internationally accepted measurement of health gain taking into account the quantity and quality of health. It can be calculated using a variety of instruments including the SF-36® and EQ-5D™ questionnaires.3 The latter is the preferred method for the National Institute for Health and Care Excellence (NICE) in the UK.4 Indeed, the QALY is currently used by NICE in the cost–utility analysis of health interventions.
The aim of this study was to determine whether arthroscopic subacromial decompression (ASAD) improves health related quality of life in a cost effective manner.
Methods
Over a two-year period (2012 to 2014), consecutive patients who were listed for an isolated subacromial decompression having failed non-operative treatment for impingement were considered for enrolment in the study. Non-operative treatment consisted of one or more steroid injections and physiotherapy with a symptomatic period of more than six months. The diagnosis of impingement was made on the basis of a typical history with a positive Hawkins–Kennedy test and a positive Neer sign with either partial or complete resolution of symptoms after a subacromial steroid injection. Exclusions were made if the patient did not wish to have his or her details entered on our database, had no scoring available, or if he or she subsequently underwent concurrent surgery in the form of a rotator cuff repair or other major intervention.
Patients were followed up for a clinical check initially at two weeks. At subsequent follow-up intervals of 3 months, 12 months and 2 years, patients completed the Oxford shoulder score (OSS) and EQ-5D™ instruments. For those discharged from clinic follow-up before this time, the scoring was administered remotely by telephone or electronically. The EQ-5D™ results were translated into health utilities, which were then used to calculate the QALYs and inform a cost–utility analysis. Where multiple scores were available, the score from the latest follow-up point was used for any calculations.
Statistical analysis
Statistical analysis was performed using Excel® (Microsoft, Redmond, WA, US) and SPSS® version 21 (IBM, New York, US). Improvements were calculated for those with both pre and postoperative scores. Improvements for the whole cohort of patients were also calculated and differences assessed for significance using a two-tailed Student’s t-test for independent samples.
Results
One hundred and twenty-nine subacromial decompressions were carried out over the two-year period between 2012 and 2014. Data were available for 83 patients (45 male, 38 female) who had completed a pre and/or postoperative EQ-5D™ questionnaire. The mean age was 57 years and the mean follow-up duration was 15 months (range: 4–27 months). Figures 1 and 2 demonstrate the mean improvement in OSS and EQ-5D™ for the entire cohort of patients. The mean improvement in functional outcome of matched pairs as measured by the OSS was 13 points (95% confidence interval [CI]: 11–15 points) (n=68). The mean health utility gain extrapolated from the EQ-5D™ measurements for matched pairs was 0.23 (95% CI: 0.16–0.30) (n=50).
Figure 1.
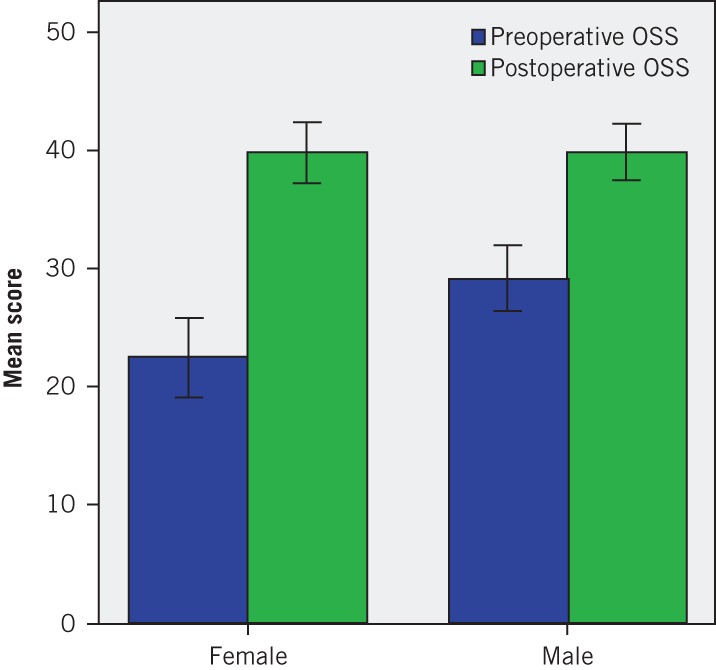
The mean preoperative (n=71) and postoperative (n=79) Oxford shoulder scores (with 95% confidence intervals) at mean follow-up for the pooled dataset. The mean improvement was 14 points (p<0.00001).
Figure 2.
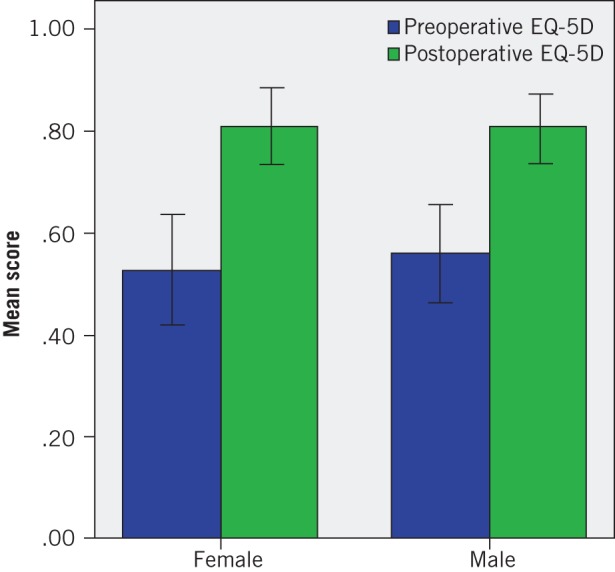
The mean health utility gain as extrapolated from the pooled preoperative (n=53) and postoperative (n=80) EQ-5D™ scores (with 95% confidence intervals). The mean improvement was 0.25 (p<0.00001).
The health utility gain of 0.23 over a mean follow-up period of 15 months translates to a gain of 0.29 QALYs. The national tariff payment system in the UK for 2014–2015 lists the price of ‘therapeutic arthroscopy of shoulder’ at £2,368.5 This system does not distinguish the more major procedures such as rotator cuff repair from ASAD but it does give an indication of the cost to the commissioning service. A previous detailed estimate of the costs associated with ASAD gave a figure of £1,307.6 Using the former figure, the cost per QALY is £10,296 and using the latter, it is £5,683.
Discussion
Our results demonstrate that subacromial decompression leads to significant improvements in function and quality of life. This is important to recognise in the context of increasing frequency of use, alongside evidence questioning the efficacy of the procedure.1,2
Cost effectiveness calculations have been performed in other areas of shoulder and orthopaedic surgery. Dattani et al worked out the cost per QALY of arthroscopic capsular release to be £2,563 and the cost of arthroscopic capsular release plus subacromial decompression to be £3,189.7 These figures are notably lower than those we present as a result of a difference in methodology. Dattani et al used the baseline assessment of the EQ-5D™ and made the assumption this would remain so for 2.5 years.7 The QALY improvements they found based on their 6-month follow-up period were then multiplied over the arbitrary 2.5-year timeframe, potentially giving an inflated estimate of the value of the procedure. Our figure is based solely on our follow-up period to give a true reflection of what we have observed rather than a modelled cost of care.
Jenkins et al present a cost–utility analysis calculation for hip and knee replacement procedures, known to be among the most cost effective medical interventions performed.8 The health utility gain calculated at the one-year follow-up time point in their study was 0.36 compared with our calculated value of 0.29. Using life table data to predict the life expectancy of their cohort, they calculated the lifetime cost per QALY for total hip and knee replacements of £1,372 and £2,101 respectively.
Renfree et al performed a cost–utility analysis of reverse shoulder arthroplasty with a methodology similar to our own.9 They calculated a cost per QALY of $16,747, translating to £9,831 per QALY at the exchange rate at the time of writing.
The NICE threshold for a cost effective intervention is set at £30,000.10 This study has demonstrated that subacromial decompression is an economically viable health intervention. This is an important finding at a time of increasing scrutiny of the value of surgical procedures.
Study limitations
There are limitations to our study. It was a single surgeon series from a single institution and it was an observational study with no control group. It is possible that with a longer follow-up period, the EQ-5D™ score may reduce back to lower levels as our patients develop new morbidity or even recurrence in their shoulder symptomatology although the health gains identified remain important.
Conclusions
ASAD leads to significant improvement in function and quality of life in a cost effective manner. This provides justification for its ongoing practice by appropriately trained shoulder surgeons in correctly selected patients who have previously failed a course of non-operative treatment.
References
- 1.Judge A, Murphy RJ, Maxwell R et al. Temporal trends and geographical variation in the use of subacromial decompression and rotator cuff repair of the shoulder in England. Bone Joint J 2014; 96: 70–74. [DOI] [PubMed] [Google Scholar]
- 2.Ketola S, Lehtinen J, Rousi T et al. No evidence of long-term benefits of arthroscopic acromioplasty in the treatment of shoulder impingement syndrome. Bone Joint Res 2013; 2: 132–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Whitehead SJ, Ali S. Health outcomes in economic evaluation: the QALY and utilities. Br Med Bull 2010; 96: 5–21. [DOI] [PubMed] [Google Scholar]
- 4.National Institute for Health and Care Excellence. Guide to the Methods of Technology Appraisal 2013. London: NICE; 2013. [PubMed] [Google Scholar]
- 5.2014/15 National Tariff Payment System: A Consultation Notice – Annex 5A Draft National Prices. GOV.UK. http://www.gov.uk/government/uploads/system/uploads/attachment_data/file/300657/Annex5A__1__consultation.xlsx (cited February 2015).
- 6.Hearnden A, Tennent D. The cost of shoulder arthroscopy: a comparison with national tariff. Ann R Coll Surg Engl 2008; 90: 587–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dattani R, Ramasamy V, Parker R, Patel VR. Improvement in quality of life after arthroscopic capsular release for contracture of the shoulder. Bone Joint J 2013; 95: 942–946. [DOI] [PubMed] [Google Scholar]
- 8.Jenkins PJ, Clement ND, Hamilton DF et al. Predicting the cost-effectiveness of total hip and knee replacement. Bone Joint J 2013; 95: 115–121. [DOI] [PubMed] [Google Scholar]
- 9.Renfree KJ, Hattrup SJ, Chang YH. Cost utility analysis of reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2013; 22: 1,656–1,661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Institute for Health and Clinical Excellence. Methods for the Development of NICE Public Health Guidance (third edition). London: NICE; 2012. [PubMed] [Google Scholar]


