Abstract
Introduction
In 2013 the Department of Health specified eligibility for bariatric surgery funded by the National Health Service. This included a mandatory specification that patients first complete a Tier 3 medical weight management programme. The clinical effectiveness of this recommendation has not been evaluated previously. Our bariatric centre has provided a Tier 3 programme six months prior to bariatric surgery since 2009. The aim of our retrospective study was to compare weight loss in two cohorts: Roux-en-Y gastric bypass only (RYGB only cohort) versus Tier 3 weight management followed by RYGB (Tier 3 cohort).
Methods
A total of 110 patients were selected for the study: 66 in the RYGB only cohort and 44 in the Tier 3 cohort. Patients in both cohorts were matched for age, sex, preoperative body mass index and pre-existing co-morbidities. The principal variable was therefore whether they undertook the weight management programme prior to RYGB. Patients from both cohorts were followed up at 6 and 12 months to assess weight loss.
Results
The mean weight loss at 6 months for the Tier 3 cohort was 31% (range: 18–69%, standard deviation [SD]: 0.10 percentage points) compared with 23% (range: 4–93%, SD: 0.12 percentage points) for the RYGB only cohort (p=0.0002). The mean weight loss at 12 months for the Tier 3 cohort was 34% (range: 17–51%, SD: 0.09 percentage points) compared with 27% (range: 14–48%, SD: 0.87 percentage points) in the RYGB only cohort (p=0.0037).
Conclusions
Our study revealed that in our matched cohorts, patients receiving Tier 3 specialist medical weight management input prior to RYGB lost significantly more weight at 6 and 12 months than RYGB only patients. This confirms the clinical efficacy of such a weight management programme prior to gastric bypass surgery and supports its inclusion in eligibility criteria for bariatric surgery.
Keywords: Gastric bypass, Bariatric surgery, Weight loss, Tier 3 service, Weight management
Obesity is defined as a body mass index (BMI) of >30kg/m2 while severe or morbid obesity is defined as a BMI of >40kg/m2.1 Data from the World Health Organization suggest that at least 600 million people worldwide are obese.2 In 2013 the Department of Health published specifications for National Health Service funded bariatric surgery.3 This included a mandatory programme of multidisciplinary specialist weight management (Tier 3) (Fig 1) prior to proceeding for bariatric surgery,4 with the patient required to meet pre-set targets usually related to weight loss. However, evidence for the clinical effectiveness of this recommendation is limited.5,6 Although a few studies have reported that surgical intervention produces more weight loss when preceded by medical interventions, many were not statistically significant.1,7,8
Figure 1.
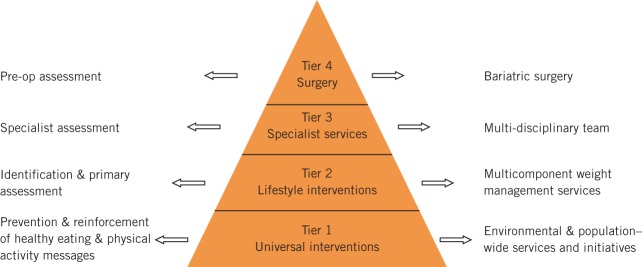
Clinical care components4
Our hospital is a regional centre for Tier 3 medical weight management and Tier 4 bariatric surgery. Since 2009, we have used a structured multidisciplinary weight management programme, which consists of nine appointments over a period of six months prior to undergoing bariatric surgery. Our aim was to compare weight loss following surgery of patients undergoing a Roux-en-Y gastric bypass (RYGB) only and of those whose RYGB was preceded by a Tier 3 medical weight loss management programme.
Methods
A retrospective study was conducted to compare weight loss in a group of patients undergoing Tier 3 specialist medical weight management followed by a RYGB versus those undergoing a RYGB only. A total of 110 patients were identified, of which 66 received a RYGB only (prior to the initiation of the Tier 3 service in 2009) and 44 received Tier 3 specialist medical weight management input prior to undergoing a RYGB.
The cohort receiving a RYGB only was selected randomly from patients who underwent a RYGB between 2008 and 2009. The mandatory weight management clinic was established in 2009, with a cohort of patients selected subsequently who were matched for age (±3 years), sex, preoperative BMI and pre-existing co-morbidities between the two groups so that the principal variable was whether they received medical weight management prior to a RYGB. Co-morbidities included type 2 diabetes, hypertension and ischaemic heart disease. The Tier 3 weight management programme was delivered in a hospital setting by a multidisciplinary team, which included a consultant bariatric physician, a bariatric specialist nurse, a bariatric psychologist, a specialist dietician and an exercise advisor.
Preoperative weight was recorded prior to the RYGB in both groups. All patients were followed up at 6 and 12 months (± 1 month) to assess weight loss. Postoperative weight loss was determined using preoperative weight as the baseline weight in both groups to allow comparability. Weight lost by the Tier 3 cohort during the six months of their weight management programme was not included.
There were no differences in operative technique between the two cohorts. In all patients, a circular 25mm CEEA stapler (Covidien, Dublin, Ireland) was used to fashion the gastrojejunostomy and the Roux limb was positioned in an antecolic, antegastric location. The standard limb lengths used were 70cm for the biliopancreatic and 100cm for the alimentary limb.
Results
Of the 66 patients in the RYGB only cohort, 50 (76%) were female and 16 (24%) male while of the 44 patients in the weight management cohort, 30 (68%) were female and 14 (32%) male. The mean age in the RYGB only cohort was similar to that of the Tier 3 cohort: 46.5 years (standard deviation [SD]: 9.21 years) versus 44.0 years (SD: 8.51 years). The mean preoperative weight in the RYGB only cohort was similar to that of the Tier 3 cohort: 145.8kg (range: 90.4–228.0kg, SD: 32.8kg) versus 153.3kg (range: 100.0–228.0kg, SD: 29.7kg). The mean preoperative BMI in the RYGB only cohort was similar to that of the Tier 3 cohort: 53.2kg/m2 (range: 36.0–85.0kg/m2, SD: 11.2kg/m2) versus 54.1kg/m2 (range: 39.5–77.7kg/m2, SD: 9.4kg/m2) (Table 1).
Table 1.
Summary of patient age, preoperative weight and BMI
| RYGB only cohort | Weight management cohort | |
|---|---|---|
| Mean age | 46.5 years | 44.0 years |
| Mean weight | 145.8kg | 153.3kg |
| Mean BMI | 53.2kg/m2 | 54.1kg/m2 |
BMI = body mass index; RYGB = Roux-en-Y gastric bypass
Unpaired two-tailed t-tests were conducted at 6 and 12 months following surgery. The mean weight loss at six months for the Tier 3 cohort was 31% (range: 18–69%, SD: 0.10 percentage points) compared with 23% (range: 4–93%, SD: 0.12 percentage points) for the RYGB only cohort (p=0.0002). The mean weight loss at 12 months for the Tier 3 cohort was 34% (range: 17–51%, SD: 0.09 percentage points) compared with 27% (range: 14–48%, SD: 0.87 percentage points) in the RYGB only cohort (p=0.0037) (Fig 2).
Figure 2.
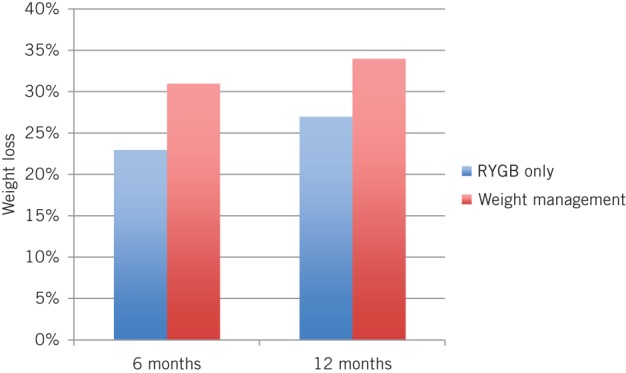
Mean weight loss at 6 and 12 months for Roux-en-Y gastric bypass (RYGB) only versus Tier 3 weight management followed by RYGB
Discussion
The aim of our retrospective study was to look objectively at the percentage weight loss at 6 and 12 months following RYGB surgery in the two cohorts. Given that completion of a Tier 3 specialist medical weight management programme is mandatory prior to the state funded bariatric surgery in England,4 it was not possible to examine contemporaneous cohorts. A cohort of patients undergoing bariatric surgery according to current specifications was therefore compared against one prior to 2009 and the initiation of our Tier 3 service. Nevertheless, given the limitations of this methodology, we consider its results valid and an important contribution towards optimising the care of bariatric patients using evidence-based practice.
The two cohorts were matched closely by age, co-morbidities and preoperative BMI, where no statistical difference was shown. In addition, the surgical technique of RYGB, with a gastrojejunal anastomosis performed using a circular stapler, remained consistent. As a result, the principal factor being assessed was weight loss at 6 and 12 months. In an ideal situation with no restriction of waiting times for a postoperative clinic appointment, all patients would have been followed up at 6 and 12 months exactly without a ±1 month adjustment.
Patients receiving Tier 3 intervention followed by RYGB lost on average more weight than the RYGB only patients, by 8 percentage points at 6 months (p=0.0002) and by 7 percentage points at 12 months (p=0.0037). Although the primary aim of the Tier 3 service is to treat morbid obesity successfully (thereby also reducing the number of patients requiring bariatric surgery),4 where this is not achieved and the programme precedes RYGB surgery, our study provides evidence that the Tier 3 service improves the outcomes of this procedure.
There is limited evidence to support any proposed mechanism to explain the advantage of a preoperative Tier 3 service. However, demonstration of lifestyle changes including patients having an overall improved understanding of their own co-morbidities and adherence to strict dietary and exercise regimes preoperatively are possible explanations for better weight loss results postoperatively. Resolution of co-morbidities following a RYGB was beyond the scope of this study as there is extensive literature suggesting an improvement or resolution of the metabolic syndrome following a RYGB.9
Conclusions
Our retrospective study revealed that in our matched cohorts, patients receiving Tier 3 specialist medical weight management input prior to RYGB lost significantly more weight at 6 and 12 months than patients undergoing RYGB only. This confirms the clinical efficacy of such weight management prior to gastric bypass surgery and supports its inclusion in eligibility criteria for bariatric surgery.
Acknowledgement
The material in this paper was presented at the Congress of the International Federation for the Surgery of Obersity and Metabolic Disorders held in Montreal, August 2014.
References
- 1.Colquitt J, Clegg A, Loveman E et al. Surgery for morbid obesity. Cochrane Database Syst Rev 2005; 4: CD003641. [DOI] [PubMed] [Google Scholar]
- 2.Obesity and Overweight. World Health Organization. http://www.who.int/mediacentre/factsheets/fs311/en/ (cited February 2015).
- 3.NHS Commissioning Board. Clinical Commissioning Policy: Complex and Specialised Obesity Surgery. London: DH; 2013. [Google Scholar]
- 4.Royal College of Surgeons of England. Commissioning Guide: Weight Assessment and Management Clinics (Tier 3). London: RCS; 2014. [Google Scholar]
- 5.Randomised trial of jejunoileal bypass versus medical treatment in morbid obesity. Lancet 1979; 2: 1,255–1,258. [PubMed] [Google Scholar]
- 6.Andersen T, Backer OG, Stokholm KH, Quaade F. Randomized trial of diet and gastroplasty compared with diet alone in morbid obesity. N Engl J Med 1984; 310: 352–356. [DOI] [PubMed] [Google Scholar]
- 7.Cooper Z, Fairburn CG. A new cognitive behavioural approach to the treatment of obesity. Behav Res Ther 2001; 39: 499–511. [DOI] [PubMed] [Google Scholar]
- 8.Anderson JW, Grant L, Gotthelf L, Stifler LT. Weight loss and long-term follow-up of severely obese individuals treated with an intense behavioral program. Int J Obes 2007; 31: 488–493. [DOI] [PubMed] [Google Scholar]
- 9.Buchwald H, Avidor Y, Braunwald E et al. Bariatric surgery. JAMA 2004; 292: 1,724–1,737. [DOI] [PubMed] [Google Scholar]


