Introduction
Active tuberculosis (TB) is a reportable communicable disease in all 50 states, but nationwide, county-level data are not released publicly. The CDC’s Online Tuberculosis Information System (OTIS) provides public surveillance data only by state. Owing to an agreement with the states, the CDC cannot publicly release TB data at the county level, precluding the development of publicly available, county-level maps of TB cases and incidence rates.
The lack of a more granular nationwide data set has limited the study of TB trends and socioeconomic risk factors to states,1 Metropolitan Statistical Areas,2 or census tracts within a single state.3 A nationwide county-level data set of TB rates provides opportunities to examine TB-related trends across multiple states, metropolitan areas, and across counties with similar demographic characteristics, such as the number of people deemed to be at high risk.4
Methods
TB statistics were generated after extracting publicly available data from state health department websites and requesting public but unpublished county-level data from state TB programs. States providing TB data assented to their use and presentation. The data set, metadata, and sources are published on an interactive map with downloadable data at healthmap.org/tb.
TB incidence rates were calculated using 5-year county-level case counts with corresponding (2006–2010) population estimates from the American Community Survey (ACS). Specifically, the total county-level case counts for 2006–2010 were divided by five to obtain the average number of cases per year. This average was divided by the average population in the county in those 5 years, and finally multiplied by 100,000 to calculate the incidence rate (cases/ 100,000). Therefore, “rates” reported in Table 1 and Figure 1 represent average annual incidence during the 5-year period.
Table 1.
Comparison of average annual TB rates of U.S. counties and regions by urban (rural/micropolitan/metropolitan) classification, 2006–2010a
| A. Number of counties, county equivalents, and health districts
|
B. Median annual TB rates per 100,000 by county and urban classification
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Region | Rural | Micropolitan | Metropolitan | Total | Region | Rural | Micropolitan | Metropolitan | All classes |
| Midwest | 486 | 218 | 259 | 963 | Midwest | 0 | 0.805 | 0.95 | 0.33 |
|
| |||||||||
| Northeast | 41 | 53 | 123 | 217 | Northeast | 0.52 | 0.90 | 1.78 | 1.10 |
|
| |||||||||
| South | 594 | 297 | 570 | 1,461 | South | 1.67 | 2.49 | 2.305 | 2.16 |
|
| |||||||||
| West | 165 | 82 | 118 | 365 | West | 0 | 1.28 | 2.21 | 1.22 |
|
| |||||||||
| Total | 1,286 | 650 | 1,070 | 3,006 | All regions | 0 | 1.38 | 1.78 | 1.28 |
|
| |||||||||
|
C. Mean annual TB rates per 100,000 by county and urban classification, 2006–2010, M (SD)
|
D. Annual TB rates per 100,000 by region and urban classification, 2006–2010
|
||||||||
| Region | Rural | Micropolitan | Metropolitan | All classes | Region | Rural | Micropolitan | Metropolitan | All classes |
|
| |||||||||
| Midwest | 1.01 (3.06) | 1.30 (2.28) | 1.26 (1.64) | 1.14 (2.57) | Midwest | 0.95 | 1.17 | 2.70 | 2.32 |
|
| |||||||||
| Northeast | 0.68 (0.82) | 0.94 (0.67) | 2.49 (2.57) | 1.77 (2.16) | Northeast | 0.63 | 0.99 | 4.50 | 4.14 |
|
| |||||||||
| South | 3.07 (6.21) | 3.72 (5.86) | 2.90 (2.70) | 3.14 (5.06) | South | 3.09 | 3.43 | 4.60 | 4.33 |
|
| |||||||||
| West | 1.70 (3.95) | 1.81 (1.88) | 3.33 (3.34) | 2.25 (3.46) | West | 2.33 | 1.95 | 5.64 | 5.31 |
|
| |||||||||
| All regions | 2.04 (4.93) | 2.44 (4.40) | 2.50 (2.66) | 2.29 (4.14) | All regions | 2.20 | 2.27 | 4.48 | 4.11 |
|
| |||||||||
| SIGNIFICANT DIFFERENCE OF M PAIRS FROM TABLE 1Cb | Between regions | ||||||||
|
| |||||||||
| National: South versus all other regions (p< 0.0001); Midwest versus all other regions (p<0.001) | |||||||||
|
| |||||||||
| Within regions | Rural: South versus all other regions (p<0.001) | ||||||||
|
| |||||||||
| Northeast: Metro versus rural or micro (p<0.0001) | Micro: South versus all other regions (p<0.0001); Northeast versus West (p<0.001) | ||||||||
|
| |||||||||
| West: Metro versus rural or micro (p<0.001) | Metro: Midwest versus all other regions (p< 0.0001) | ||||||||
Region and metropolitan/micropolitan classifications follow Office of Management and Budget definitions. Rural counties are those not defined as either metropolitan or micropolitan.
Significant according to Welch two-sample t-test and Bonferroni adjustment, where α=0.0012. Number of comparisons=42.
TB, tuberculosis
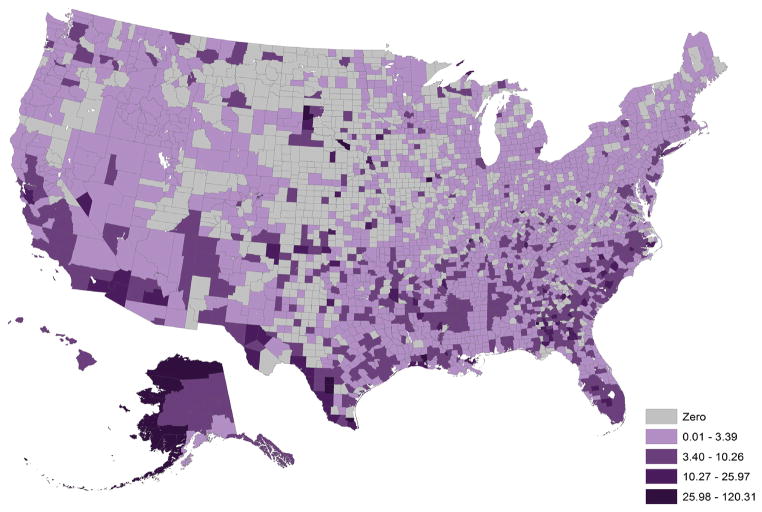
Figure 1.
Average annual tuberculosis rate per 100,000 population, 2006–2010, by county
Tuberculosis data from publicly available sources.
Population estimates from US. Census American Community Survey, 2006–2010.
Counties were cross-classified by four U.S. regions (Midwest, Northeast, South, and West) and by urban/rural classification (metropolitan [urban area of ≥50,000]; micropolitan [urban area of 10,000–49,999]; and rural), according to the Office of Management and Budget classifications. ANOVA was performed to assess differences in means across these 12 cross-classifications. ANOVAs were examined using Welch two-sample t-tests with Bonferroni adjustment for 42 comparisons (α=0.0012); significant comparisons were defined as p<0.0012. Maps were created using ESRI ArcMap, version 10.3, and statistical analyses were performed using R, version 2.14.2.
Data were available on a year-by-year basis for 2,892 (92.0%) counties; supra-county health district level for 161 (5.1%) counties; and only multi-year aggregated data for 90 counties (2.9%). Collectively, these data enabled the creation of a U.S. map depicting 5-year average TB incidence rates (Figure 1) and a corresponding data set of 3,006 counties for analysis. Henceforth, we use the term “county” to refer collectively to counties; county-equivalents (e.g., boroughs); and health districts.
Results
More than 600 counties have TB rates above the 2011 national rate of 3.4 cases per 100,000 people.5 The top 15 counties exceeded a rate of 20 cases per 100,000 (range=20.9–120.3 cases); nine of these were rural, and eight were in the Southern region. TB case rates were generally highest in U.S. metropolitan areas; the South had the highest mean and median rates among U.S. regions (Table 1). Only the Northeast and West had statistically different mean rates when metropolitan counties were compared with micropolitan and rural means.
Discussion
A publicly available, county-level TB data set enables analysis of TB rates (per 100,000) at the substate level. Although TB rates in the U.S. are expected to be high in urban areas6 that have large at-risk foreign-born populations,7 certain rural areas also have high TB rates, particularly in Southern states.
Publicly available county-level TB data can assist TB surveillance and control efforts. TB “hotspots” that cross state borders can be identified. Socioeconomic variables can now be tested to identify nationwide trends in at-risk populations for targeted prevention efforts. Thus, we encourage all states to publish county-level TB data online.
Additional demographic information distinguishing cases by birth country will help researchers and public health officials understand emerging TB trends. Although TB data should be interpreted within a local context, these data will facilitate more efficient identification of locales where high rates of TB cross state lines, facilitate collaboration between states to jointly target those areas, and allow health departments to discern regional and nationwide trends.
Acknowledgments
We gratefully acknowledge the state and county public health departments that contributed to this project by posting data online (Alaska, Alabama, Arizona, California, Colorado, Connecticut, District of Columbia, Delaware, Florida, Georgia, Idaho, Illinois, Indiana, Kentucky, Louisiana, Maryland, Michigan, Minnesota, Missouri, Mississippi, Montana, North Carolina, Nebraska, New Hampshire, New Jersey, New Mexico, Nevada, New York, Ohio, Oklahoma, Oregon, Pennsylvania, Rhode Island, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, Washington, Wisconsin, West Virginia, and Wyoming) or providing data via e-mail (Arkansas, Hawaii, Iowa, Kansas, Massachusetts, Maine, North Dakota, and Vermont). We thank Rachel Chorney for her work on the healthmap.org/tb website, for which no direct compensation was received. DS had full access to all study data and takes responsibility for its integrity and the accuracy of the data analysis.
Dr Brownstein is supported by grant R01 LM010812-04 from the National Library of Medicine.
This study was funded by the CDC.
Dr. Cetron from the Division of Global Migration and Quarantine at the CDC participated as a full scientific collaborator in the investigation; however, the findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC.
Footnotes
No financial disclosures were reported by the authors of this paper.
Contributor Information
David Scales, Email: david.scales@aya.yale.edu, Children’s Hospital Informatics Program, Boston. Children’s Hospital, Harvard Medical School, Boston, Massachusetts.
John S. Brownstein, Children’s Hospital Informatics Program, Boston. Children’s Hospital, Harvard Medical School, Boston, Massachusetts.
Kamran Khan, Department of Medicine, Division of Infectious Diseases, University of Toronto, Toronto, Ontario, Canada.
Martin S. Cetron, Division of Global Migration and Quarantine, the CDC, Atlanta, Georgia.
References
- 1.Holtgrave DR, Crosby RA. Social determinants of tuberculosis case rates in the U. S Am J Prev Med. 2004;26(2):159–62. doi: 10.1016/j.amepre.2003.10.014. [DOI] [PubMed] [Google Scholar]
- 2.Greenwood MJ, Warriner WR. Immigrants and the spread of tuberculosis in the U.S: a hidden cost of immigration. Popul Res Policy Rev. 2011;30:839–59. [Google Scholar]
- 3.Myers WP, Westenhouse JL, Flood J, Riley LW. An ecological study of tuberculosis transmission in California. Am J Public Health. 2006;96(4):685–90. doi: 10.2105/AJPH.2004.048132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cain KP, Benoit SR, Winston CA, Mac Kenzie WR. Tuberculosis among foreign-born persons in the U. S J Am Med Assoc. 2008;300(4):405–12. doi: 10.1001/jama.300.4.405. [DOI] [PubMed] [Google Scholar]
- 5.Miramontes R, Pratt R, Price SF, Jeffries C, Navin TR, Oramasionwu GE. Trends in tuberculosis—U.S. 2011. MMWR Morb Mortal Wkly Rep. 2012;61(11):181–5. [Google Scholar]
- 6.Oren E, Winston CA, Pratt R, Robison VA, Narita M. Epidemiology of urban tuberculosis in the U.S. 2000–2007. Am J Public Health. 2011;101(7):1256–63. doi: 10.2105/AJPH.2010.300030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu Y, Weinberg MS, Ortega LS, Painter JA, Maloney SA. Overseas screening for tuberculosis in U.S-bound immigrants and refugees. N Engl J Med. 2009;360(23):2406–15. doi: 10.1056/NEJMoa0809497. [DOI] [PubMed] [Google Scholar]