Abstract
Introduction
Total hip replacement (THR) is successful and performed commonly. Component placement is a determinant of outcome. Influence of surgeon handedness on component placement has not been considered previously. This study was a radiographic assessment of component positioning with respect to handedness. Early data from 160 patients are reported.
Methods
Overall, 160 primary THRs for osteoarthritis were included. Equal numbers of left and right THRs were performed by four surgeons, two right-handed and two left-handed. Postoperative radiography was assessed for THR component position by measurement of leg length inequality, acetabular inclination and centre of rotation. Surgeons’ handedness was assessed using the Edinburgh inventory.
Results
For leg length inequality, no significant interaction was seen between hip side and surgeon handedness. Acetabular inclination angles showed a statistically significant difference, however, depending on hand dominance, with higher inclination angles recorded when operating on the dominant side. There was a trend towards greater medialisation of the centre of rotation on the non-dominant side although this did not reach statistical significance.
Conclusions
Surgeon handedness appears to influence acetabular component position during THR but it is one factor of many that interact to achieve a successful outcome.
Keywords: Hip, Arthroplasty, Surgeon handedness, Leg length inequality, Acetabulum
Component placement and minimisation of leg length inequality (LLI) are key determinants of functional outcome in total hip replacement (THR). Orthopaedic surgeons operate on both sides of patients’ bodies but the effect of surgeon handedness on outcome has not been studied. The spatial position of the patient and surgeon will differ depending on which side of the body the THR is being performed. A surgeon’s handedness may therefore influence the technical level to which he or she is able to operate, depending on whether the left or right limb is being operated on.
During THR for a right-handed (RHD) surgeon performing surgery on a right-sided joint, acetabular preparation is led by the dominant right hand while femoral preparation is performed by the non-dominant left hand. During a left THR, this relationship will be reversed. In this paper, ‘dominant side’ refers to a right THR for a RHD surgeon and a left THR for a left-handed (LHD) surgeon. This proposed relationship should be unaffected by patient position or surgical approach.
The purpose of this study was to investigate whether surgeon handedness had any influence on THR component positioning based on postoperative radiography. We present the early data from analysis of 160 cases in the first study to consider this potentially important factor.
Methods
Four orthopaedic surgeons (>100 cases per year) and 160 patients were recruited retrospectively for the study at Leeds Teaching Hospitals NHS Trust. The stated handedness and preferred surgical approach for each surgeon were:
Surgeon 1: RHD, posterior approach
Surgeon 2: LHD, posterior approach
Surgeon 3: RHD, lateral approach
Surgeon 4: LHD, lateral approach
For each surgeon, 20 right THRs and 20 left THRs were identified from theatre records and surgeons’ logbooks. Inclusion criteria for patients in the study were a diagnosis of osteoarthritis, non-complex primary THR, postoperative anteroposterior pelvis radiography available for review on the picture archiving and communication system (IMPAX® 6; Agfa HealthCare, Mortsel, Belgium) and Surgeon 1, 2, 3 or 4 listed as primary operating surgeon.
For each patient, the anteroposterior radiography was assessed using linear and angular measurement tools in the IMPAX® software. Measurements evaluated were LLI (compared with contralateral hip, be it native or prosthetic), acetabular component angle of inclination and THR centre of rotation (COR).
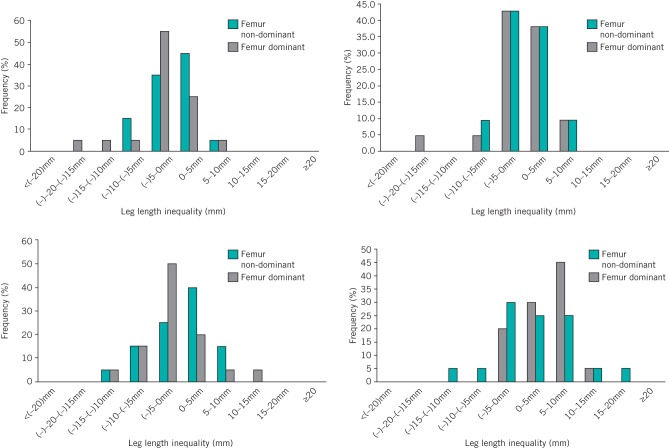
LLI was assessed using the Leeds method (Fig 1),1 with a line connecting the femoral heads’ COR as a reference line, and two further lines parallel to this at the inferior aspects of the acetabular teardrops and midpoint of the lesser trochanters. Two perpendicular measurements were made on each hip. The first was from the reference line to the acetabular teardrop in order to assess the contribution of the acetabular component to the overall LLI. The second measurement from the acetabular teardrop line to the lesser trochanter line provided an assessment of the femoral stem component’s contribution to the LLI. The overall leg length is the sum of these two measurements, and this was compared between the ipsilateral and contralateral hips to provide an overall assessment of any LLI.
Figure 1.
Leeds method of leg length inequality assessment1
The acetabular component inclination angle was assessed using the technique of Pluot et al2 with an ischial tuberosity reference line and measuring the angle subtended between this and a line joining the superior and inferior aspects of the acetabular cup (Fig 2). The COR was assessed using a vertical reference line from the pubic symphysis to the sacral spinous processes. The perpendicular distance from this reference line to the COR of the femoral head was measured bilaterally.
Figure 2.
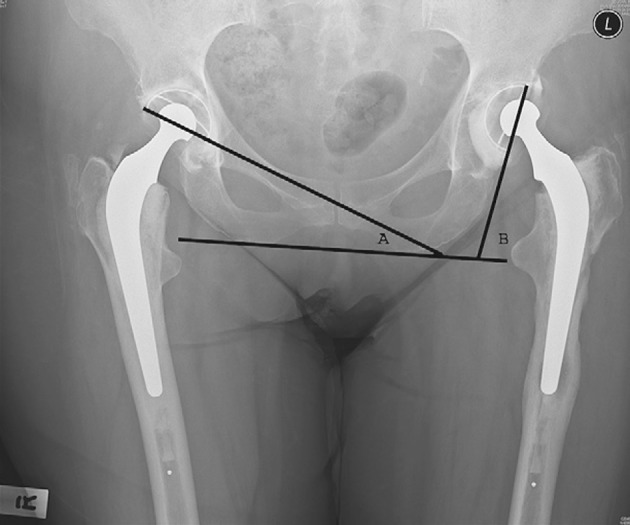
Acetabular inclination angle assessment method2
Where operative records allowed, the actual femoral head component size was compared with the radiographic measurement and a magnification artefact coefficient was calculated. A mean magnification artefact of 4.9mm was seen (standard deviation [SD]: 0.68mm, 95% confidence interval [CI]: 0.30mm). For example, where a 28mm head had been used, the mean measured diameter was 32.9mm and the magnification factor (MF) was therefore calculated as:
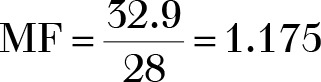
The reduction factor (RF) to be applied to each measured value (MV) to obtain the ‘actual value’ (AV) was determined by:
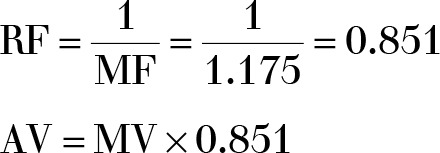
Correction for magnification was applied to all subsequent measured linear values obtained from the radiography. All results described in this paper relate to the ‘corrected’ actual values.
Surgeon handedness was assessed using the Edinburgh inventory.3 A laterality quotient (LQ) was calculated to provide an assessment of the degree of handedness:
All data were transferred to Excel® for Mac 2011 (Microsoft, Redmond, WA, US). Statistical analyses were performed using SPSS® version 19 (IBM, New York, US).
Results
Analysis of total LLI revealed a mean of +0.5mm (95% CI: -0.6–1.6mm) on the dominant operated side and 0.0mm (95% CI: -1.3–1.2mm) on the non-dominant side. Statistical analysis using Student’s t-test showed this to be not significant (p=0.543). The mean absolute LLI was 3.6mm (95% CI: 2.9–4.4mm) on the dominant side and 4.4mm (95% CI: 3.6–5.2mm) on the non-dominant side. Student’s t-test also found this to be not significant (p=0.18).
The mean cup related LLI was -0.4mm (95% CI: -1.4–0.6mm) on the dominant operated side and -1.5mm (95% CI: -2.3–-0.6mm) on the non-dominant side. This difference approached but did not reach statistical significance (p=0.096). The mean absolute cup related LLI was 3.6mm (95% CI: 3.0–4.2mm) on the dominant side and 3.3mm (95% CI: 2.8–3.8mm) on the non-dominant side. A t-test revealed this to be not significant (p=0.422).
The mean femoral stem related LLI was +0.9mm (95% CI: -0.7–2.4mm) on the dominant operated side and +1.4mm (95% CI: -0.1–2.9mm) on the non-dominant side. This result was not statistically significant (p=0.593). The mean absolute stem related LLI was 5.5mm (95% CI: 4.6–6.5mm) on the dominant side and 5.5mm (95% CI: 4.5–6.4mm) on the non-dominant side. A t-test showed this to be not significant (p=0.948).
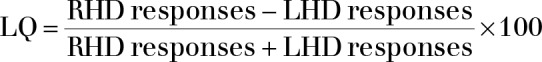
Analysis of absolute total LLI with regard to surgical approach was considered. A mean of 5.1mm (95% CI: 4.2–6.0mm) for the posterior approach and 5.9mm (95% CI: 4.9–6.9mm) for the anterolateral approach was calculated. A t-test showed this to be not statistically significant (p=0.233) (Fig 3).
Figure 3.
Mean absolute total leg length inequality (LLI) for the dominant and non-dominant hands of the four surgeons
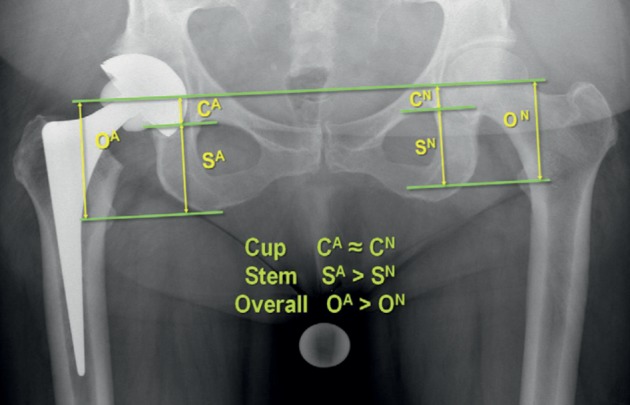
Stratified LLI data for each of the four surgeons indicated that variability in the distribution of LLI values appeared to exist (Fig 4). Surgeons 1 and 3 (RHD) showed a trend towards lower LLIs when femur preparation was led by their dominant hand. In Surgeon 4 (LHD), increased variability in stratified LLI data was observed when femoral preparation was led by the non-dominant hand. Surgeon 2 (LHD) showed comparable stratified LLI results irrespective of side.
Figure 4.
Stratified leg length inequality data showing relationship to handedness of femur preparation
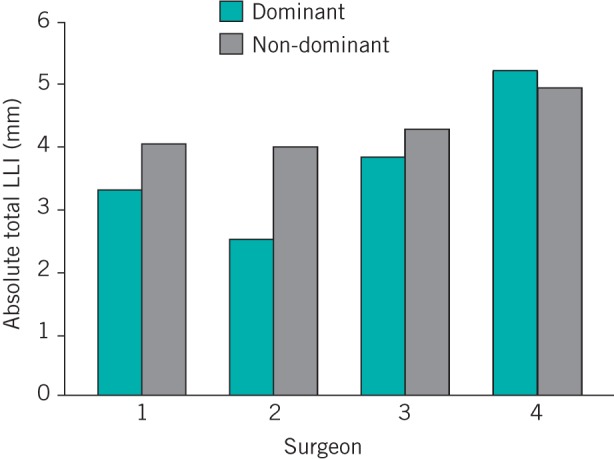
Analysis of the inclination angle of the acetabular component revealed a mean of 46.4° (95% CI: 45.4–47.4°) on the dominant operated side and 43.5° (95% CI: 42.3–44.6°) on the non-dominant side. This difference was statistically significant (p<0.05) (Fig 5). Consideration of the COR revealed a mean medialisation of 0.4mm (95% CI: 1.6–-0.7mm) on the dominant side and 1.7mm (95% CI: 2.7–0.7mm) on the non-dominant side. This result approached but did not reach statistical significance (p=0.098).
Figure 5.
Mean acetabular inclination angle for the dominant and non-dominant hands of each of the four surgeons
The results of the Edinburgh inventory questionnaire are shown in the Table 1. Surgeons 1 and 3 declared themselves to be RHD, and their Edinburgh inventory LQs support this with values of +100 and +78.6 respectively. The LQ results of Surgeons 2 and 4 support their declared left-handedness with LQs of -50 and -100 respectively.
Table 1.
Edinburgh inventory results. A laterality quotient (LQ) of 100 refers to an individual with strong handedness.
| Surgeon | Declared handedness | Edinburgh inventory LQ |
|---|---|---|
| 1 | Right | +100 |
| 2 | Left | -50 |
| 3 | Right | +78.6 |
| 4 | Left | -100 |
Discussion
LLI is an established complication of THR and the overall mean LLI in this study was lower than that found by Konyves and Bannister, where a mean lengthening of 3.5mm was observed.4 Surgeon handedness did not show any statistically significant difference in total LLI between THRs performed on the dominant and non-dominant sides. A trend towards LLI ‘shortening’ in the acetabular component was seen, reflecting relative superior positioning, and appeared more marked when the THR was performed on the non-dominant side. Our results also suggest that acetabular component positioning may be more susceptible to variation when performed on a surgeon’s non-dominant side with statistically significant lower angles of inclination seen, along with a tendency for increased medialisation that approached statistical significance.
Variability in acetabular component insertion position dependent on surgeon handedness appears to exist. A larger study is warranted to explore trends in this study that did not reach statistical significance. Observation of a systematic difference in acetabular inclination is of interest although the small angle (3°) seen is unlikely to be clinically significant. Both groups were within Lewinnek et al’s safe zone of 30–50°.5
During THR on the opposite side of the body to the surgeon’s dominant hand, acetabular preparation is led by the non-dominant hand while femoral preparation and component insertion is led by the dominant hand. One explanation for the observed differences in cup medialisation may be that surgeons exert more pressure and increasingly deepen the acetabulum when operating power reamers with their non-dominant hand, at the same time allowing relatively superior positioning of the cup. It would also be interesting to consider these observed changes in a future study in comparison with the results obtained in investigations of computer guided arthroplasty outcomes.
The Edinburgh inventory used is a validated method of assessing hand dominance and degree of handedness.3 The LQs for the four surgeons supported their subjective ‘handedness’. The LHD surgeons (Surgeons 2 and 4) both had negative LQ values but for Surgeon 2 the LQ showed a less strong handedness preference. This may reflect that LHD individuals will display a less polarised LQ value as many aspects of everyday life are right-hand dominant biased.3 LHD individuals therefore experience a societal pressure to use their non-dominant right hand, more than RHD individuals would to use their left hand. A larger study would be necessary to make the use of handedness LQ data in statistical analysis relevant.
No literature exists specifically looking at whether surgeon handedness affects performance depending on which side of the body a THR is performed. Mehta and Lotke considered a single surgeon series of 728 total knee replacements, half left and half right, performed by a RHD surgeon.6 Postoperative function and pain scores showed that handedness did appear to play a role in outcome. Makay et al’s questionnaire-based study of general surgeons with respect to left-handedness found that 9.3% of surgeons were LHD and 50% felt that standard endoscopic surgical techniques had to be modified for LHD surgeons.7 Gallagher et al considered the roll of spatial awareness in a study of urologists, concluding it is only one component of the successful development of surgical skills alongside intelligence, dexterity, experience, decision making and personality.8
There are several limitations to the current study. The observed values and differences are small and a larger study would be required to determine whether a true systematic effect exists where we found trends. A single person collected all data, and so no cross-checking occurred although the Leeds method of LLI assessment has been shown to be accurate and to have good repeatability.1 The potential effect of pelvic tilt on pelvic radiography appearance has not been controlled for.
This study presents early data. Surgeon factors are likely to account for a significant amount of variation seen in outcomes when compared with implant design and patient factors, and awareness of the potential contribution that handedness may play is important.
Conclusions
THR postoperative parameters have been considered in an attempt to objectify technical surgical outcome in terms of component position. These results have been assessed in the context of surgeon handedness and the side of the patient on which the procedure was performed. Overall technical performance of a THR by any surgeon is the product of a multitude of factors, some related to the surgeon’s inherent attributes and others to the individual character of each case. The results of this study suggest that handedness is one of these factors, especially with regard to the acetabular component. While the observed effect was modest, it has not been demonstrated previously and warrants consideration when performing a THR on the non-dominant side of the body.
Acknowledgement
This work was supported by the NIHR (National Institute for Health Research) through funding of the LMBRU (Leeds Musculoskeletal Biomedical Research Unit). In addition this work was partially funded through WELMEC, a Centre of Excellence in Medical Engineering funded by the Welcome Trust and EPSRC, under grant number WT 088908/Z/09/Z. Support was also received from the John Charnley Trust.
References
- 1.McWilliams A, Stewart TD, Grainger AJ et al. Leg length inequality following total hip replacement. Orthop Trauma 2011; 25: 37–42. [Google Scholar]
- 2.Pluot E, Davis ET, Revell M et al. Hip arthroplasty. Part 2: normal and abnormal radiographic findings. Clin Radiol 2009; 64: 961–971. [DOI] [PubMed] [Google Scholar]
- 3.Oldfield RC. The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia 1971; 9: 97–113. [DOI] [PubMed] [Google Scholar]
- 4.Konyves A, Bannister GC. The importance of leg length discrepancy after total hip arthroplasty. J Bone Joint Surg Br 2005; 87: 155–157. [DOI] [PubMed] [Google Scholar]
- 5.Lewinnek GE, Lewis JL, Tarr R et al. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am 1978; 60: 217–220. [PubMed] [Google Scholar]
- 6.Mehta S, Lotke PA. Impact of surgeon handedness and laterality on outcomes of total knee arthroplasties: should right-handed surgeons only do right TKRs? Am J Orthop 2007; 36: 530–533. [PubMed] [Google Scholar]
- 7.Makay O, Icoz G, Ersin S. Surgeon’s view on the limitations of left-handedness during endoscopic surgery. J Laproendosc Adv Surg Tech A 2008; 18: 217–221. [DOI] [PubMed] [Google Scholar]
- 8.Gallagher HJ, Allan JD, Tolley DA. Spatial awareness in urologists: are they different? BJU Int 2001; 88: 666–670. [DOI] [PubMed] [Google Scholar]