Abstract
Introduction
Dislocation following hip hemiarthroplasty (HHA), its incidence, predictors, treatment outcomes and mortality were investigated in a single centre series.
Methods
The prospectively collected data on neck of femur fracture admissions compiled over 11 years were reviewed. Place of residence, place of fall, past medical history, intraoperative factors (grade of surgeon, delay in surgery, type of implant and operative time), postoperative complications and mortality were compared between patients who suffered a dislocation and those who did not. In the dislocation group, the mean number of dislocations, reduction method, type and fate of implant, and mortality were investigated.
Results
Prospective data on 8,631 admissions were collected; 41% of these were managed with a HHA. The dislocation rate was 0.76%. A delay in surgery of >24 hours was associated with a fourfold increase in the dislocation risk. The majority (81%) of dislocations occurred in the first six weeks and closed manipulation was the definitive treatment in only 23% of the cases. The mortality rate was not increased following HHA dislocation.
Conclusions
The delay in surgery was the most important predictor of HHA dislocation. Closed reduction was associated with a high failure rate. While an initial attempt at closed reduction for a first dislocation is recommended, for redislocators, we recommend early exploration/revision as an alternative to repeat manipulations.
Keywords: Neck of femur, Dislocation, Predictors, Outcome
The number of patients attending with a neck of femur (NOF) fracture is an increasing challenge that reflects an aging population. Hip hemiarthroplasty (HHA) is used to treat the majority of displaced intracapsular NOF fractures,1 and provides a better alternative to reduction and internal fixation when factors such as complications, revision rate and health related quality of life measures are compared.2,3 HHA dislocation is a serious complication encountered in 1–7% of cases,4–6 and it carries substantial morbidity and high mortality.7 The aim of this study was to investigate factors that might predict patients at high risk of dislocation, and to determine the incidence, treatment outcomes and mortality following HHA dislocation.
Methods
Data on all patients with a NOF fracture managed in a university hospital were collected prospectively by independent audit clerks and recorded in a database. The data on patients managed with a HHA for an intracapsular NOF fracture between 1999 and 2010 were reviewed. Information on age, sex, admission source, place of fall, mobility prior to fall, past medical history (cardiovascular disease, chronic obstructive airway disease, renal disease, diabetes, rheumatoid arthritis, parkinsonism, history of malignancy and Paget’s disease), drug history (smoking, steroids, substance abuse, warfarin, clopidogrel and the use of four or more medications), operation (delay in surgery, grade of surgeon, duration of surgery, type of implant), postoperative complications and mortality was compared between patients who suffered a dislocation and those who did not.
Following discharge from the hospital, future follow-up of patients is carried out routinely by the patient’s general practitioner but the university hospital serves a well defined catchment area and has the only emergency department within it, implying that a dislocation will be managed in the same institution, which has both elective orthopaedics and trauma cover. It was not possible to confirm confidently whether additional dislocations had been missed (patient moved out of region and treated in another institution) but this scenario was assumed to be relatively unlikely.
Further analysis on the dislocation group was carried out to determine the success of closed reduction and fate of the implant. The reduction method, number of dislocations, type of implant and fate of implant were investigated. Mortality data on all the patients included in this study were obtained from the Office for National Statistics and analysed. Statistical analysis was carried out using SPSS® version 18 (SPSS, Chicago, IL, US). A two-sample t-test was used for continuous variables and a chi-squared test for categorical data. Odds ratio (OR) analysis was calculated together with the 95% confidence interval (CI) for significant categorical findings. A p-value of 0.05 was considered to be statistically significant.
Results
Between 1999 and 2010, prospective data were collected on 8,631 NOF admissions. HHA was performed on 3,525 (41%) diagnosed with an intracapsular NOF fracture (AO [Arbeitsgemeinschaft für Osteosynthesefragen] type 31-B). Twenty-seven patients (0.77%) suffered a dislocation diagnosed both clinically and radiologically, thirteen (48%) of which occurred while still an inpatient. A summary of the preoperative, operative and postoperative data is presented in Tables 1–4. An anterolateral approach was used in all cases.
Table 1.
Preoperative data
| Dislocated hip hemiarthroplasty (n=27) | Uncomplicated hip hemiarthroplasty (n=3,498) | p-value | |
|---|---|---|---|
| Mean patient age in years | 79 (SD: 8) | 82 (SD: 8) | 0.038* |
| Female sex | 85% | 78% | 0.39** |
| Lives alone | 11 (41%) | 1,466 (42%) | 0.87** |
| Admission source | 0.58** | ||
| Own home | 59.3% | 62.9% | |
| Residential home | 14.8% | 12.7% | |
| Nursing home | 14.8% | 12.5% | |
| Warden aided flat | 7.4% | 9.7% | |
| Acute hospital | 0.0% | 1.2% | |
| Unknown | 3.7% | 1.0% | |
| Mobility prior to fall | 0.93** | ||
| Independent | 48.1% | 42.7% | |
| One stick | 25.9% | 31.4% | |
| Two sticks | 0.0% | 2.6% | |
| Frame | 22.2% | 20.5% | |
| Wheelchair/bedbound | 3.7% | 2.8% | |
| Past medical history | |||
| Cardiovascular disease | 33.3% | 48.1% | 0.13** |
| Chronic obstructive pulmonary disease | 14.8% | 16.0% | 1.0** |
| Renal disease | 7.4% | 5.7% | 0.66** |
| Diabetes mellitus | 18.5% | 12.2% | 0.37** |
| Rheumatoid disease | 7.4% | 3.1% | 0.21** |
| Parkinsonism | 11.1% | 4.4% | 0.21** |
| History of malignancy | 3.7% | 10.6% | 0.35** |
| Paget’s disease | 0.0% | 0.3% | 1.0** |
| Pathological fracture | 0.0% | 1.3% | 1.0** |
SD = standard deviation
t-test;
chi-squared test
Table 2.
Operative data
| Dislocated hip hemiarthroplasty (n=27) | Uncomplicated hip hemiarthroplasty (n=3,498) | p-value | |
|---|---|---|---|
| Surgery delay >24h | 20 (74.1%) | 850 (24.3%) | <0.0001* |
| Surgery delay >36h | 11 (40.7%) | 78 (2.2%) | <0.0001* |
| Mean operative time in mins | 95 (SD: 30) | 82 (SD: 32) | 0.048** |
SD = standard deviation
chi-squared test;
t-test
Table 3.
Implants used in initial surgery
| Dislocated hip hemiarthroplasty (% of total in group) | Uncomplicated hip hemiarthroplasty (% of total in group) | Dislocated specific to implant | p-value* | |
|---|---|---|---|---|
| Austin Moore | 12 (44.4%) | 2,365 (67.6%) | 0.5% | |
| Thompson | 3 (11.1%) | 189 (5.4%) | 1.6% | |
| Exeter™ Trauma Stem | 4 (14.8%) | 459 (13.1%) | 0.9% | |
| Exeter™ bipolar | 8 (29.6%) | 484 (13.8%) | 1.6% | |
| Cemented | 12 (44.4%) | 2,365 (67.6%) | 0.010 | |
| Uncemented | 15 (55.6%) | 1,132 (32.4%) | ||
| Bipolar | 8 (29.6%) | 484 (13.8%) | 0.027 | |
| Unipolar | 19 (70.4%) | 3,013 (86.2%) |
chi-squared test
Table 4.
Postoperative complications
| Dislocated hip hemiarthroplasty (n=27) | Uncomplicated hip hemiarthroplasty (n=3,498) | p-value* | |
|---|---|---|---|
| Cardiac failure | 0 | 96 (2.7%) | 0.47 |
| Cerebrovascular accident | 0 | 37 (1.1%) | 0.70 |
| Chest infection | 2 (7.4%) | 398 (11.4%) | 0.40 |
| Clostridium difficile | 0 | 19 (0.5%) | 0.86 |
| Deep infection | 2 (7.4%) | 51 (1.5%) | 0.06 |
| Deep vein thrombosis | 1 (3.7%) | 14 (0.4%) | 0.11 |
| Gastrointestinal haemorrhage | 0 | 25 (0.7%) | 0.80 |
| Haematoma | 0 | 57 (1.6%) | 0.64 |
| Myocardial infarction | 0 | 68 (1.9%) | 0.60 |
| Periprosthetic fracture | 0 | 19 (0.5%) | 0.86 |
| Pressure sore: buttock | 0 | 56 (1.6%) | 0.64 |
| Pressure sore: heel | 0 | 48 (1.4%) | 0.69 |
| Pressure sore: other | 0 | 26 (0.7%) | 0.80 |
| Pulmonary embolism | 0 | 31 (0.9%) | 0.78 |
| Renal failure | 0 | 16 (0.5%) | 0.88 |
| Surgical wound infection | 0 | 68 (1.9%) | 0.60 |
| Urinary tract infection | 6 (22.2%) | 213 (6.1%) | 0.005 |
Fisher’s exact test
Predictors of dislocation
In order to investigate predictors of dislocation, factors that have a significant correlation with dislocation were identified using a Pearson correlation coefficient. Significant factors were then fed into a binary logistic regression model to identify significant predictors of dislocation. A significant correlation was established for the factors listed in Table 5 after calculating the Pearson correlation coefficient for all preoperative, intraoperative and postoperative data against dislocation. Binary regression analysis found the delay in surgery to be most significantly associated with an increased risk of dislocation, with a fourfold risk increase if the delay was over 24 hours and a tenfold increase if the delay was over 36 hours from admission. The use of a cemented implant was associated with a more than 50% reduction in the risk of dislocation.
Table 5.
Factors with a significant correlation with dislocation
| Pearson’s correlation coefficient | p-value | |
|---|---|---|
| Patient age | 0.035 | 0.038 |
| Surgery delayed >24h | 0.101 | <0.0001 |
| Surgery delayed >36h | 0.214 | <0.0001 |
| Operative time | -0.033 | 0.048 |
| Cemented hip hemiarthroplasty | -0.043 | 0.010 |
| Bipolar hip hemiarthroplasty | 0.040 | 0.018 |
| Postoperative urinary tract infection | 0.058 | 0.001 |
| Postoperative deep infection | 0.043 | 0.011 |
| Postoperative deep vein thrombosis | 0.044 | 0.009 |
In our sample, sex, place of preadmission residence, mobility prior to fall, past medical history including multiple co-morbidities and Parkinson’s disease, surgical duration, the grade of the operating surgeon and postoperative complications including deep infections were not predictive of postoperative HHA dislocations. The risk of dislocation was doubled in patients who developed a postoperative urinary tract infection but that did not reach statistical significance (Table 6).
Table 6.
Dislocation predictors based on a binary logistic regression analysis model
| OR (95% CI) | p-value | |
|---|---|---|
| Patient age | 1.0 (1.0–1.1) | 0.12 |
| Surgery delayed >24h | 4.2 (1.5–11.4) | 0.005 |
| Surgery delayed >36h | 10.1 (3.9–26.0) | <0.0001 |
| Operative time | 1.0 (1.0–1.0) | 0.21 |
| Cemented hip hemiarthroplasty | 0.4 (0.2–0.9) | 0.027 |
| Bipolar hip hemiarthroplasty | 1.7 (0.7–4.2) | 0.26 |
| Postoperative deep vein thrombosis | 0.1 (0.0–3.5) | 0.23 |
| Postoperative deep infection | 0.3 (0.1–1.9) | 0.22 |
| Postoperative urinary tract infection | 2.5 (0.9–7.2) | 0.09 |
OR = odds ratio; CI = confidence interval
Dislocation treatment outcome
Twenty-six clinical notes were available for review; one was missing. The majority (81%) of the dislocations occurred in the first 6 weeks following surgery at a median of 27 days (interquartile range [IQR]: 3.5–41 days). Figure 1 summarises of the management course for the dislocation group. Although a closed manipulation was successful 65% of the time, it was the definitive treatment in only 6 (23%) of the 26 patients reviewed. Of the remaining 20 patients, all but 2 required further surgery (Table 7). Untoward findings relating to initial surgery were documented for six of the cases: high hip abductor soft tissue tension (due to a miscalculated high offset) (n=2); the neck cut was too low; the proximal femur was fractured; cement retained in the acetabulum; and detached (failed) abductor repair.
Figure 1.
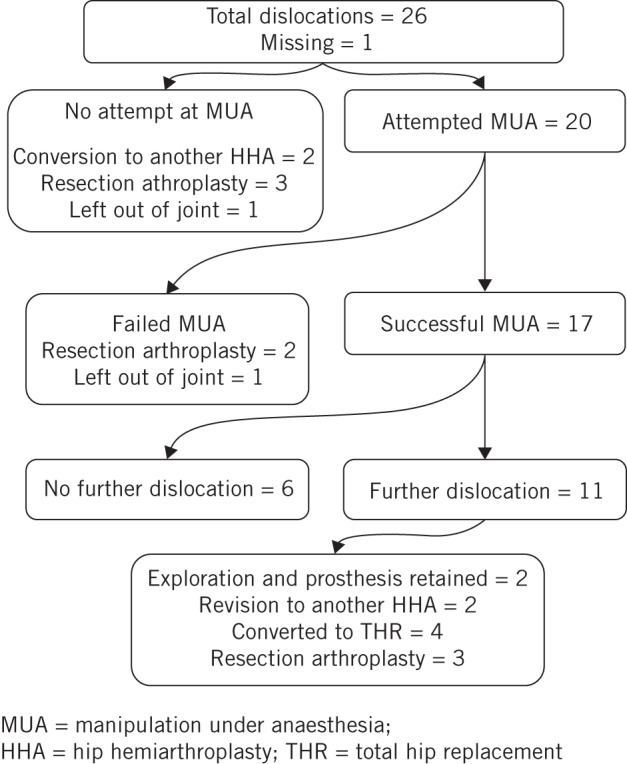
Summary of the management course for the dislocation group
Table 7.
Summary of interventions for the dislocation group
| Intervention | n=26 |
|---|---|
| Resection arthroplasty | 8 (31%) |
| Successful closed manipulation | 6 (23%) |
| Revision to another hemiarthroplasty | 4 (15%) |
| Revision to a total hip replacement | 4 (15%) |
| Left out of joint | 2 (8%) |
| Prosthesis explored and acetabulum cleaned | 2 (8%) |
Survivorship analysis
A significant difference in the mortality could not be identified between the dislocation group and controls at 30 days, 90 days or when the overall mortality rate was calculated at a median follow-up duration of 27 months (IQR: 5–53 months) from the date of the injury (Table 8, Fig 2). Similarly, no significant difference was found when mortality rates for patients who suffered a single dislocation were compared with those who suffered multiple dislocations (62.5% vs 64.7% respectively, p=0.62, chi-squared test).
Table 8.
Mortality at 30 days, 90 days and overall for dislocation versus non-dislocation groups
| Non-dislocation group | Dislocation group | p-value* | |
|---|---|---|---|
| 30-day mortality rate | 8.4% | 3.7% | 0.49 |
| 90-day mortality rate | 19.2% | 25.9% | 0.30 |
| Total mortality rate | 70.0% | 66.7% | 0.42 |
chi-squared test
Figure 2.
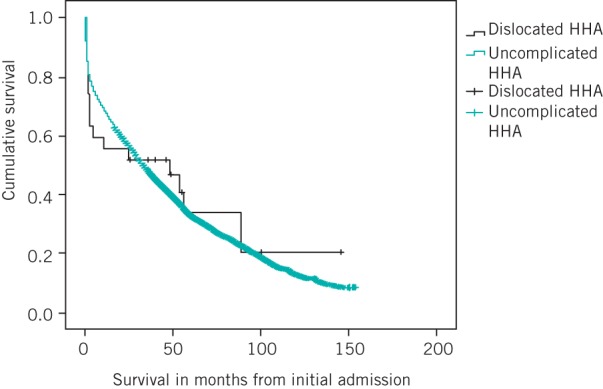
Kaplan–Meier curves demonstrating the survivorship of the dislocated hip hemiarthroplasty (HHA) group against the uncomplicated HHA group
Discussion
The most important predictor of postoperative HHA dislocation is the delay in performing the surgery. The current guidelines for hip fracture management recommend ‘surgery within 36 hours of admission’10 but our findings suggest that the risk of dislocation increases fourfold if the surgery is delayed for more than 24 hours and tenfold if the surgery is delayed for more than 36 hours.
Preoperative patient optimisation should not be understated and might explain the higher delay rate (55.6%) for surgery among patients who underwent uncemented HHA (an implant we have used mainly for the physiologically compromised) compared with those who were managed with cemented HHA (32.4%) but undue delay in surgery must be avoided to minimise further soft tissue swelling and subsequently compromise the exposure and soft tissue repair. Another explanation for the delay (>24 hours) is the lack of theatre time from admission but we prioritise NOF fracture patients in line with the guidelines to perform surgery on the day of or the day after admission.10 We were unable to find any significant preoperative or postoperative predictors for dislocation of a HHA performed for displaced intracapsular NOF fracture. All HHAs in our cohort were performed via an anterolateral approach.10
The grade of operating surgeon and the operating time had no significant impact on the dislocation rate in our study. This might be due to constant senior surgeon supervision of junior surgical trainees. Similarly, Enocson et al described no significant effect of the grade of operating surgeon on HHA dislocation rate in 720 consecutive patients (739 HHA procedures) in Sweden.4 A large review of a cohort of Medicare beneficiaries (n=115,352) who underwent HHA for a NOF fracture revealed a lower dislocation rate following procedures performed by high volume orthopaedic surgeons (25 primary or revision total hip arthroplasties per year),11 emphasising the importance of experience on the rate of dislocation in this group of patients.
The use of cemented HHA was described as a possible cause of increased dislocation risk.6 There is no clear explanation for the effect of cementation on dislocation but cemented implants are technically less forbearing. A substantial component version error and/or high soft tissue tension due to incomplete seating of a cemented implant is unyielding once the cement sets and might significantly compromise the HHA functional motion arc. Minor technical imperfections, on the other hand, are better tolerated in an uncemented implant after hip reduction and mobilisation as the implant shifts slightly through osteoporotic bone in the large medullary canal.
In our study, the risk of dislocation seemed reduced when cemented implants were used. This might be due to a patient selection bias as the Austin Moore uncemented unipolar implant was used for patients with significant co-morbidities and poor mobility. Bipolar HHAs appear to have a lower dislocation rate than unipolar HHAs.8,14 A 2004 meta-analysis of 23,107 patients managed with HHA concluded that after adjustment for the surgical approach and the use of cement, there was no difference in the risk of dislocation between unipolar and bipolar HHAs,6 and our findings support this too. Treatment selection bias might help to explain the insignificant yet high OR for dislocation with bipolar HHA (OR: 1.7) as it is used for the ‘youngest and fittest’ of patients who would, through activity, challenge the implant more frequently at the boundaries of its stability.
A link between neurological conditions and dislocation has yet to be significantly substantiated. In 1,812 primary bipolar HHAs (75% performed for NOF fractures) over a period of 27 years, Sierra et al reported 31 dislocations with 45% suffering from a neurological condition such as senile dementia, Parkinson’s disease, paraplegia, brain tumour or Down’s syndrome but a significant link between any of these factors and HHA dislocation could not be established.8 In another study, Ninh et al reported a 6% dislocation rate in 217 patients following HHA with a follow-up duration of one year, and found male sex and cognitive impairment to have a significant correlation with the dislocation group.9
This is at odds with our findings that Parkinson’s disease was not a predictor for dislocation despite its high prevalence among dislocators, nor was sex. The higher prevalence of urinary tract infections among dislocators is likely to reflect a longer period of recumbency and prolonged catheterisation. In our cohort, deep infection following HHA was not found to be predictive of a dislocation.
On review of the notes, we could not identify a mechanism or a cause for the dislocation in some of the dislocators; where a cause could be identified, however, the findings were in line with previous studies that list one or more of the following factors: an overlooked proximal femoral fracture, gross implant version error, misjudgement of the soft tissue tension (too tight or too lax soft tissues) secondary to offset and/or centre of femoral head miscalculation or retained cement in the acetabulum.6,9,13 HHA dislocation occurred most often in the early postoperative period.8,9 The majority (81%) of the dislocations in our study occurred in the first six weeks following surgery.
A reasonable course of action following the first dislocation is a trial of closed manipulation, keeping in mind the expected high failure rate as shown in our study and others.8,15 We encountered a 23% overall success rate of closed reduction (as a definitive treatment for dislocation), an experience comparable with that of Sierra et al, who reported a 30% success rate with closed manipulation for a dislocated HHA.8 We share the view of Odumala et al that in the event of a further dislocation, early revision surgery or excision arthroplasty should be considered rather than repeat manipulation.15
Our institution published a review of 1,000 NOF fracture cases in the early 1990s, quoting a 2% dislocation rate, a 30-day mortality rate of 10% and a 90-day mortality rate of 50%.7 At present, the accepted figure for overall mortality following a NOF fracture is 10% at 30 days, rising to 30% at one year,10 and our current findings are in line with these rates independent of dislocation or redislocation. This improvement in the medium-term follow-up period is largely the result of advances in therapeutics and the multidisciplinary approach to the management of NOF fracture patients. A review of 2,336 Austin Moore HHAs performed for fracture with a 6-year follow-up period and a 1.9% dislocation rate reported a mortality rate of 24% for non-dislocators and first-time dislocators compared with a 69% mortality rate for redislocators at 6 months.15
Odumala et al reported a sevenfold increase in the risk of redislocation in dementia sufferers that prompted the authors to recommend avoiding closed reduction in favour of an excision arthroplasty procedure in this group of patients.15 Even if the mortality rate was not affected, we expect that the physiological insult secondary to dislocation, subsequent interventions and the prolonged period of recumbency explain Enocson et al’s findings of a significant deterioration in the EQ-5D™ (index) score and a negative effect on the quality of life, which persisted beyond one year following surgery among redislocators.16 This is a limitation in our study as data on dementia and the mini-mental state examination (MMSE) were not collected, and were therefore not included in the data analysis. Over the last four years we have been prospectively collecting MMSE data and will hopefully include this in future publications.
Owing to the retrospective nature of this study, a closer look at the cause of delay to surgery was not possible. A further reflection on our current practice suggests delays to be either due to the lack of theatre time or the physiological instability of the patient prior to surgery (ie severe infections or evidence of severe organ malfunction, mainly cardiac or respiratory) but the details of such information were not recorded for our study sample.
Conclusions
Dislocation is difficult to predict based on preoperative factors but delay to surgery is associated with a significant increase in the risk of postoperative dislocation. We hypothesise that scrupulous surgical technique and implant positioning aided by meticulous preoperative planning and close supervision of junior surgeons may reduce this serious complication. While an initial attempt at closed reduction for a first dislocation is recommended, it is the definitive treatment in only 23% of patients. Patients who suffer a dislocation should be informed that there is a high likelihood that revision surgery will be needed. For redislocators and patients who fail closed reduction, we advocate early exploration and revision surgery as an alternative to repeat manipulations.
References
- 1.Currie C, Partridge M Plant F et al. The National Hip Fracture Database National Report 2011. London: NHFD; 2011. [Google Scholar]
- 2.Bhandari M, Devereaux PJ, Swiontkowski MF et al. Internal fixation compared with arthroplasty for displaced fractures of the femoral neck: a meta-analysis. J Bone Joint Surg Am 2003; 85: 1,673–1,681. [DOI] [PubMed] [Google Scholar]
- 3.Hopley C, Stengel D, Ekkernkamp A, Wich M. Primary total hip arthroplasty versus hemiarthroplasty for displaced intracapsular hip fractures in older patients: systematic review. BMJ 2010; 340: c2332. [DOI] [PubMed] [Google Scholar]
- 4.Enocson A, Tidermark J, Törnkvist H, Lapidus LJ. Dislocation of hemiarthroplasty after femoral neck fracture. Acta Orthop 2008; 79: 211–217. [DOI] [PubMed] [Google Scholar]
- 5.Figved W, Opland V, Frihagen F et al. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures. Clin Orthop Relat Res 2009; 467: 2,426–2,435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Varley J, Parker MJ. Stability of hip hemiarthroplasties. Int Orthop 2004; 28: 274–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blewitt N, Mortimore S. Outcome of dislocation after hemiarthroplasty for fractured neck of the femur. Injury 1992; 23: 320–322. [DOI] [PubMed] [Google Scholar]
- 8.Sierra RJ, Schleck CD, Cabanela ME. Dislocation of bipolar hemiarthroplasty: rate, contributing factors, and outcome. Clin Orthop Relat Res 2006; 442: 230–238. [DOI] [PubMed] [Google Scholar]
- 9.Ninh CC, Sethi A, Hatahet M et al. Hip dislocation after modular unipolar hemiarthroplasty. J Arthroplasty 2009; 24: 768–774. [DOI] [PubMed] [Google Scholar]
- 10.National Institute for Health and Clinical Excellence. Hip Fracture. London: NICE; 2011. [Google Scholar]
- 11.Ames JB, Lurie JD, Tomek IM et al. Does surgeon volume for total hip arthroplasty affect outcomes after hemiarthroplasty for femoral neck fracture? Am J Orthop 2010; 39: E84–E89. [PubMed] [Google Scholar]
- 12.Bush JB, Wilson MR. Dislocation after hip hemiarthroplasty: anterior versus posterior capsular approach. Orthopedics 2007; 30: 138–144. [DOI] [PubMed] [Google Scholar]
- 13.Pajarinen J, Savolainen V, Tulikoura I et al. Factors predisposing to dislocation of the Thompson hemiarthroplasty: 22 dislocations in 338 patients. Acta Orthop Scand 2003; 74: 45–48. [DOI] [PubMed] [Google Scholar]
- 14.Iorio R, Healy WL, Lemos DW et al. Displaced femoral neck fractures in the elderly: outcomes and cost effectiveness. Clin Orthop Relat Res 2001; 383: 229–242. [DOI] [PubMed] [Google Scholar]
- 15.Odumala AO, Iqbal MR, Middleton RG. Failure of closed reduction after dislocation of Austin Moore hemiarthroplasty: an analysis of risk factors. J Arthroplasty 2010; 25: 781–784. [DOI] [PubMed] [Google Scholar]
- 16.Enocson A, Pettersson H, Ponzer S et al. Quality of life after dislocation of hip arthroplasty: a prospective cohort study on 319 patients with femoral neck fractures with a one-year follow-up. Qual Life Res 2009; 18: 1,177–1,184. [DOI] [PubMed] [Google Scholar]


