Abstract
Introduction
The optimal treatment of high energy tibial fractures remains controversial and a challenging orthopaedic problem. The role of external fixators for all these tibial fractures has been shown to be crucial.
Methods
A five-year consecutive series was reviewed retrospectively, identifying two treatment groups: Ilizarov and Taylor Spatial Frame (TSF; Smith & Nephew, Memphis, TN, US). Fracture healing time was the primary outcome measure.
Results
A total of 112 patients (85 Ilizarov, 37 TSF) were identified for the review with a mean age of 45 years. This was higher in women (57 years) than in men (41 years). There was no significant difference between frame types (p=0.83). The median healing time was 163 days in both groups. There was no significant difference in healing time between smokers and non-smokers (180 vs 165 days respectively, p=0.07), open or closed fractures (p=0.13) or age and healing time (Spearman's r=0.12, p=0.18). There was no incidence of non-union or re-fracture following frame removal in either group.
Conclusions
Despite the assumption of the rigid construct of the TSF, the median time to union was similar to that of the Ilizarov frame and the TSF therefore can play a significant role in complex tibial fractures.
Keywords: Tibial fracture, Healing, Ilizarov fixator, Taylor Spatial Frame
The optimal treatment of high energy tibial fractures remains controversial and a challenging orthopaedic problem. The treatment of these severe injuries ranges from non-operative to operative or a combination of these techniques depending on soft tissue damage, anatomical location of the fracture, articular surface involvement and bone defects. 1-13 The role of external fixators is crucial, especially in cases of open fracture, severe soft tissue damage and fracture comminution. 14-18 External fixators have the ability for multilevel tibial fracture stabilisation with minimal disruption of the soft tissue. The Ilizarov apparatus and, more recently, the Taylor Spatial Frame (TSF; Smith & Nephew, Memphis, TN, US) have been used in the treatment of complex high energy tibial fractures. 15,16,19,20,21,22 These ring fixa-tors involve the application of circular rings attached to the limbs by tensioned wires and/or threaded pins. 23
The TSF is a multiplanar external fixator that combines ease of application with computer accuracy in fracture reduction, and allows for residual serial postoperative adjustments and manipulation of fractures into better alignments in an outpatient setting using the frame's web-based software. 20,24 Although the TSF uses the same (slow correction) principles of the Ilizarov system by applying a six-axis deformity analysis in its computer programmes, there is a suggestion that this frame is much more rigid than an Ilizarov frame. No studies have compared the use of TSF or Ilizarov frames in the management of high energy tibial fractures in the adult population. This study aimed to compare the time to union in high energy tibial fractures using Ilizarov or TSF frames in a busy UK trauma setting. The patients were all operated on by a single surgeon.
Methods
A consecutive retrospective review of 122 patients (87 women, 35 men; median age: 45 years) was conducted via a prospective ring external fixator database. Eighty-five patients were treated with an Ilizarov frame while thirty-seven received the TSF (Table 1). The fractures were subdivided depending on anatomical site as well as also into open and closed fractures. Open fractures were classified using the Gustilo and Anderson classification. 25 The mechanisms of injury are reported in Table 1. The mean time period from presentation to application of the circular external fixator was 3.31 days (range: 0-18 days) for the Ilizarov group and 3.79 days (range: 0-28 days) for the TSF group. All patients received a ring fixator at an average of 3.46 days after presentation to our trust.
Table 1.
Patient characteristics
| Total | llizarov frame | TSF | p-value | |
|---|---|---|---|---|
| Number of patients | 122 (100%) | 85 (70%) | 37 (30%) | |
| Median age (years) | 45 (IQR: 31-57) | 44 (IQR: 31-57) | 48 (IQR: 40-57) | 0.36 |
| Median body mass index (kg/m2) | 27 (IQR: 24-30) | 27 (IQR: 24-30) | 27 (IQR: 23-31) | 0.93 |
| Sex | 0.14 | |||
| Male | 35 (29%) | 64 (75%) | 23 (62%) | |
| Female | 87 (71%) | 21 (25%) | 14 (38%) | |
| Side | 0.15 | |||
| Left | 48 (39%) | 37 (44%) | 11 (30%) | |
| Right | 74 (61%) | 48 (56%) | 26 (70%) | |
| Co-morbidity events | 0.86 | |||
| 0 | 61 (50%) | 43 (51%) | 18 (49%) | |
| 1 | 26 (21%) | 17 (20%) | 9 (24%) | |
| >2 | 35 (29%) | 25 (29%) | 10 (27%) | |
| Smoking | 64 (75%) | <0.001 | ||
| No | 78 (64%) | 14 (38%) | ||
| Yes | 25 (20%) | 17 (20%) | 8 (22%) | |
| Unknown | 19 (16%) | 4 (5%) | 15 (41%) | |
| Open/closed fracture | 0.11 | |||
| Closed | 87 (71%) | 62 (73%) | 25 (68%) | |
| Open | 27 (22%) | 20 (24%) | 7 (19%) | |
| Unknown | 8 (7%) | 3 (4%) | 5 (14%) | |
| Injury mechanism | 0.04 | |||
| Fall from height | 34 (28%) | 26 (31%) | 8 (22%) | |
| Road traffic accident | 33 (27%) | 27 (32%) | 6 (16%) | |
| Sports injury | 33 (27%) | 20 (24%) | 13 (35%) | |
| High energy (unspecified) | 13 (11%) | 9 (11%) | 4 (11%) | |
| Unknown | 9 (7%) | 3 (4%) | 6 (16%) | |
| Fracture type | <0.001 | |||
| Tibial shaft | 68 (56%) | 34 (40%) | 34 (92%) | |
| Pilon | 32 (26%) | 31 (36%) | 1 (3%) | |
| Plateau | 20 (16%) | 18 (21%) | 2 (5%) | |
| Segmental | 2 (2%) | 2 (2%) | 0 (0%) |
All fractures had acceptable anatomical reduction on radiography both intraoperatively and postoperatively. All malalignments were corrected during limb reconstruction outpatient follow-up clinics. The first follow-up appointment was at an average of two weeks following frame application. Thereafter, patients were seen every two weeks for the period of correction and every four to six weeks during the non-correction period. Pin site care was performed weekly using alcoholic chlorhexidine according to the modified Royal College of Nursing Consensus Project guidelines. 26 Weight bearing was commenced according to fracture fixation configuration and patient tolerance. All patients received physiotherapy as part of their fracture rehabilitation protocol.
Fracture healing was assessed clinically and radio-graphically. Healing time was defined as length of time in frame. Most patients underwent dynamisation, reloading and frame removal according to the local protocol. Once the fracture had healed, the tibia was reloaded (nuts were loosened and rods left in frame), allowing axial macromotion. One to two weeks later, another x-ray was taken and clinical assessment made. If there were no clinical or radiological concerns, the rods were removed and patients were allowed normal activities for another one to two weeks. At the end of this period, if there were no clinical or radiological concerns, the frame was removed. At union, most of the ring fixator was removed in outpatient clinics with Entonox® (BOC Healthcare, Manchester, UK). No patients required casts or functional braces after frame removal.
The primary outcome was healing time (time in the frame). The following parameters were recorded: patient's baseline characteristics (age, sex, body mass index [BMI], co-morbidities, smoking status), tibial fracture characteristics (location, open/closed) and ring fixator type (Ilizarov or TSF). The influence of patient characteristics on healing was investigated. Complications of ring fixator use were assessed. The types of complications were reviewed and the interventions noted. Complication was defined as pin site infection, infection requiring surgery or admission, neurovascular compromise and compartment syndrome.
Statistical analysis
Analysis of categorical data was performed using the Mann-Whitney U test for two groups and for three groups using the median test for k-samples (k>2). The relationship between variables in combination was considered in a multiple least-squares regression model; residuals were checked for normality. Continuous data were analysed using Spearman's correlation coefficient. A p-value of <0.05 (two-tailed) was considered statistically significant. Stata® (StataCorp, College Station, TX, US) software was used to analyse the data.
Results
Demographic details were available for all patients via the electronic database (Table 1). There was no significant difference between frame types (p=0.83).
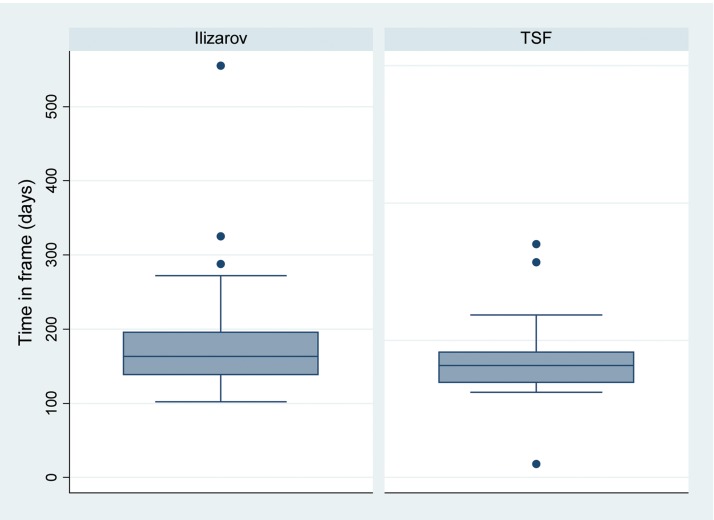
Fracture healing: all patients
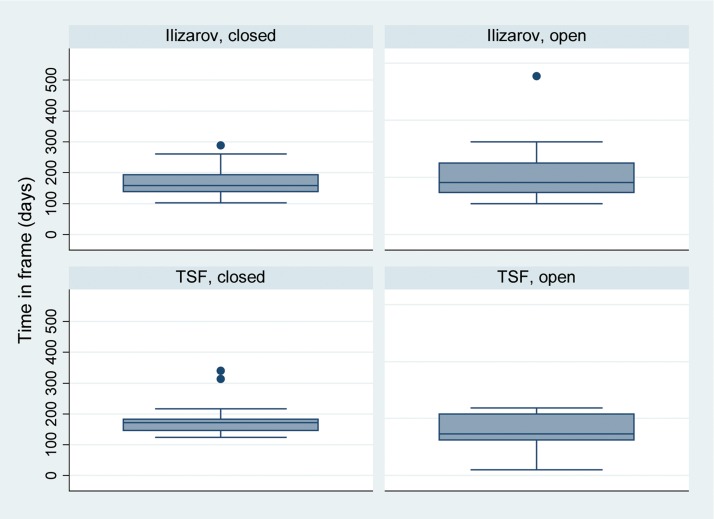
The median fracture healing time was 163 days (Fig 1). Women took longer to heal than men (180 vs 156 days) although this difference was not statistically significant (p=0.21). There was no significant difference in median healing time between smokers and non-smokers (180 vs 165 days respectively, p=0.07) and there was no statistical difference in median healing time between closed or open fractures (p=0.13) (Fig 2). There was no clear relationship between healing time and co-morbid events. The median healing time for patients who sustained a tibial fracture following a road traffic accident was 170 days, 167 days following a sports injury, 158 days following a fall and 146 days following unspecified high energy injuries.
Figure 1.
Overall median healing time. The median is shown as the centre line inside the box with the 25th and 75th centiles shown as the lower and upper hinges respectively. The ‘whiskers’ indicate the lower and upper adjacent values respectively while the circles show extreme values
Figure 2.
Median healing time for closed/open fractures. The median is shown as the centre line inside the box with the 25th and 75th centiles shown as the lower and upper hinges respectively. The ‘whiskers’ indicate the lower and upper adjacent values respectively while the circles show extreme values
There was no significant difference between healing time and sex, co-morbidity, smoking status, injury mechanism or fracture type when these variables were considered together in a multiple regression model. Scatter plots (not shown) indicated a slight downward trend between BMI and fracture healing time (ie as BMI increased, healing time increased). There was no obvious linear relationship between age and healing time. No cases of non-union were documented.
Fracture healing: Ilizarov versus TSF
No significant differences were shown on subgroup analysis (Table 2).
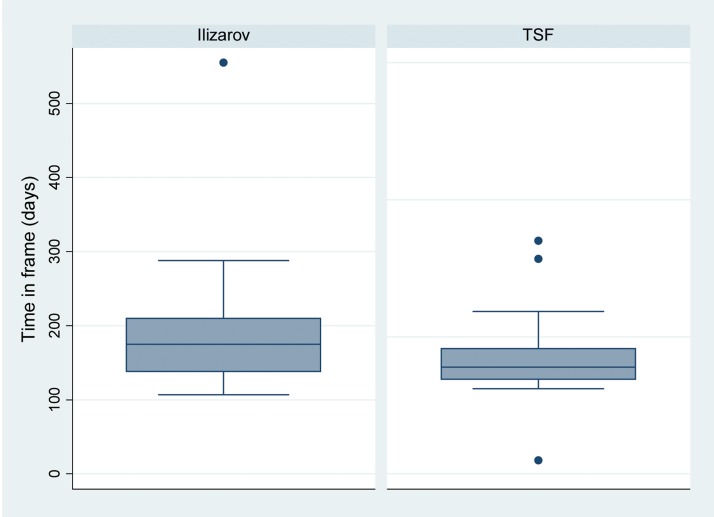
Fracture healing: anatomical site
The median healing times for patients receiving an Ilizarov frame or a TSF were studied according to the anatomical site of the fracture (Table 2). Tibial shaft fractures had a median healing time of 175 days versus 156 days respectively (Fig 3). There was no significant relationship between healing time and diagnosis (%2=4.69, df=3, p=0.19). No patients re-fractured following frame removal.
Table 2.
Median healing time
| Total | Ilizarov frame | TSF | |
|---|---|---|---|
| Median healing time | 163 days | 163 days | 163 days |
| Co-morbidity events | |||
| 0 | 160 days | 154 days | 168 days |
| 1 | 178 days | 187 days | 171 days |
| >2 | 160 days | 163 days | 143 days |
| Smoking | |||
| No | 165 days | 161 days | 177 days |
| Yes | 178 days | 181 days | 173 days |
| Unknown | 147 days | 143 days | |
| Fracture type | |||
| Tibial shaft | 168 days | 175 days | 156 days |
| Pilon | 153 days | 153 days | 181 days* |
| Plateau | 160 days | 158 days | 186 days |
** TSF = Taylor Spatial Frame
Fracture type: TSF pilon*, plateau** and unknown**
Figure 3.
Median healing time for tibial shaft fractures. The median is shown as the centre line inside the box with the 25th and 75th centiles shown as the lower and upper hinges respectively. The ‘whiskers’ indicate the lower and upper adjacent values respectively while the circles show extreme values
Fracture healing: tibial shaft
An equal number of patients received both types of frame for their high energy tibial fractures (n=34). Subgroup analysis of this group showed no significant difference in healing time (p=0.83).
Complications
In the Ilizarov group, 17 patients developed pin site infections (9 treated with oral antibiotics), 3 developed methicil-lin resistant Staphylococcus aureus infections (treated with antibiotics), 2 developed septic knee arthritis and 4 developed cellulitis. Three of these patients had multiple pin site infections with one requiring admission for intravenous antibiotics. Two patients had a pulmonary embolism and two had a fat embolism. Only two patients had their frames adjusted owing to broken wires. One patient developed skin allergy to chlorhexidine. In the TSF group, four patients developed a pin site infection requiring antibiotics, one developed an abscess around the pin sites, two developed a Staphylococcus aureus wound infection while two developed cellulitis. There was no statistical significance between the two groups with regard to pin site infections (p=0.21).
Discussion
High energy tibial injury fractures with associated extensive soft tissue damage pose additional threats to healing and predispose the individual to infections if the fractures are open or if there is suboptimal fracture fixation. Different authors have emphasised that treatment of these fractures should involve multilevel stabilisation and minimal soft tissue disruption, thereby maintaining the biological reserve. 5,8,26,27,28,29,30,31,32,33
The use of external fixators has been shown to provide multilevel stabilisation while limiting soft tissue dissection. The role of fracture stabilisation leading to healing has been demonstrated using Ilizarov frames. 1-9 However, the role of the TSF in these fractures is limited and although there are no studies available in the adult population, there is a general assumption that the TSF is stiffer and can therefore delay healing time. TSF use has been reported in paediatric communities with tibial injuries. 20
Different fracture healing times for the different parts of the tibia have been reported. The mean time to healing for segmental fractures has been reported as 84-217 days, with 98-168 days for high energy pilon fractures, 98-161 days for tibial shaft fractures and 100.8 days for tibial plateau fractures. 1,5,8,13,33,34,35,36 Some studies have reported a longer time to union, with a mean proximal tibia union time of 254 days and 278.6 days for distal tibial fractures. 21
The patients in our study had a median healing time of 163 days in both groups, which compares to the healing time documented in the literature for Ilizarov patients. There was no statistically significant difference between the two groups with regard to fracture healing. Patients with shaft fractures healed at a median of 175 days in an Ilizarov frame and at 156 days in a TSF; the TSF healing time was similar to the reported shaft healing rate in the literature. As is widely reported, closed fractures healed faster than open fractures in the total study population (160 vs 176 days). Our patient numbers in the smoker and open fracture groups were small, and true comparisons for bone healing could therefore not be made but it may suggest a trend.
Infection is a major concern for surgeons, especially pin tract infection following ring fixator use. The overall infection rate following external fixator application is reported at 0-100%. 37 In our study, 16% of the patients developed pin tract infections, with three patients having recurrent multiple pin tract infections requiring antibiotics. This was seen mainly in patients with fractures near the articular surface, which may account for the increased infection rates. According to the literature, the timing of surgery is of the utmost importance. This is said to affect the incidence of soft tissue related infections. Some studies have recommended an average delay of six days prior to fixation of pilon fractures to allow for resolution of soft tissue swelling. 38 Our protocol for pilon and plateau fractures is soft tissue optimisation, usually with a temporary external fixator followed by minimal open reduction internal fixation and a circular frame.
Our study was not a powered study so the lack of significance may reflect inadequate power. The small numbers in anatomical sites led to the inability to compare groups apart from the tibial shaft group, which had similar numbers for Ilizarov and TSF patients. Although fracture healing was achieved at the same time scale for both the TSF and Ilizarov groups, the long-term outcome with regard to functional ability and development of osteoarthritis needs to be studied.
Conclusions
Use of ring fixators plays an important role in the management of high energy tibial fractures. Despite the assumption of the rigid construct of the TSF, the median time to union was similar to that of the Ilizarov frame. Although TSF is more expensive owing to struts, it provides three-dimensional manoeuvrability, quicker application and ease of accurate reduction. It can therefore play a significant role in complex tibial fractures.
References
- 1.Kapoor SK, Kataria H, Patra SR, Boruah T. Capsuloligamentotaxis and definitive fixation by an ankle-spanning Ilizarov fixator in high-energy pilon fractures. J Bone Joint Surg Br. 2010;92:1,100–1,106. doi: 10.1302/0301-620X.92B8.23602. [DOI] [PubMed] [Google Scholar]
- 2.Borrelli J, Ellis E. Pilon fractures: assessment and treatment. Orthop Clin North Am. 2002;33:231–245. doi: 10.1016/s0030-5898(03)00082-8. [DOI] [PubMed] [Google Scholar]
- 3.Helfet DL, Koval K, Pappas J, et al. Intraarticular ‘pilon’ fracture of the tibia. Clin Orthop Relat Res. 1994;298:221–228. [PubMed] [Google Scholar]
- 4.Gaudinez RF, Mallik AR, Szporn M. Hybrid external fixation in tibial plafond fractures. Clin Orthop. 1996;329:223–232. doi: 10.1097/00003086-199608000-00028. [DOI] [PubMed] [Google Scholar]
- 5.Giotakis N, Panchani SK, Narayan B, et al. Segmental fractures of the tibia treated by circular external fixation. J Bone Joint Surg Br. 2010;92:687–692. doi: 10.1302/0301-620X.92B5.22514. [DOI] [PubMed] [Google Scholar]
- 6.Atkins RM, Sudhakar JE, Porteous AJ. Distraction osteogenesis through high energy fractures. Injury. 1998;29:535–537. doi: 10.1016/s0020-1383(98)00128-4. [DOI] [PubMed] [Google Scholar]
- 7.French B, Tornetta P. High-energy tibial shaft fractures. Orthop Clin North Am. 2002;33:211–230. doi: 10.1016/s0030-5898(03)00081-6. [DOI] [PubMed] [Google Scholar]
- 8.Giannoudis PV, Hinsche AF, Cohen A, et al. Segmental tibial fractures: an assessment of procedures in 27 cases. Injury. 2003;34:756–762. doi: 10.1016/s0020-1383(02)00393-5. [DOI] [PubMed] [Google Scholar]
- 9.Huang CK, Cher WM, Chen TH, Lo WH. Segmental tibial fractures treated with interlocking nails. A retrospective study of 33 cases. Acta Orthop Scand. 1997;68:563–566. doi: 10.3109/17453679708999027. [DOI] [PubMed] [Google Scholar]
- 10.Sanders R, Jersinovich I, Anglen J, et al. The treatment of open tibial shaft fractures using an interlocked intramedullary nail without reaming. J Orthop Trauma. 1994;8:504–510. [PubMed] [Google Scholar]
- 11.Stegemann P, Lorio M, Soriano R, Bone L. Management protocol for unreamed interlocking tibial nails for open tibial fractures. J Orthop Trauma. 1995;9:117–120. doi: 10.1097/00005131-199504000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Finkemeier CG, Schmidt AH, Kyle RF, et al. A prospective, randomized study of intramedullary nails inserted with and without reaming for the treatment of open and closed fractures of the tibial shaft. J Orthop Trauma. 2000;14:187–193. doi: 10.1097/00005131-200003000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Inan M, Halici M, Ayan I, et al. Treatment of type IIIA open fractures of tibial shaft with Ilizarov external fixator versus unreamed tibial nailing. Arch Orthop Trauma Surg. 2007;127:617–623. doi: 10.1007/s00402-007-0332-9. [DOI] [PubMed] [Google Scholar]
- 14.Atesalp AS, Yildiz C, Basbozkurt M, Gür E. Treatment of type IIIa open fractures with Ilizarov fixation and delayed primary closure in high-velocity gunshot wounds. Mil Med. 2002;167:56–62. [PubMed] [Google Scholar]
- 15.Hosny G, Fadel M. Ilizarov external fixator for open fractures of the tibial shaft. Int Orthop. 2003;27:303–306. doi: 10.1007/s00264-003-0476-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Inan M, Tuncel M, Karaoglu S, et al. III open tibial fractures with Ilizarov external fixation. Acta Orthop Traumatol Turc. 2002;36:390–396. [PubMed] [Google Scholar]
- 17.Behrens F, Searls K. External fixation of the tibia. J Bone Joint Surg Br. 1986;68:246–254. doi: 10.1302/0301-620X.68B2.3514629. [DOI] [PubMed] [Google Scholar]
- 18.Caudle RJ, Stern PJ. Severe open fractures of the tibia. J Bone Joint Surg Am. 1987;69:801–807. [PubMed] [Google Scholar]
- 19.Edwards CC, Simmons SC, Browner BD, Weigel MC. Severe open tibial fractures. Results treating 202 injuries with external fixation. Clin Orthop Relat Res. 1988;230:98–115. [PubMed] [Google Scholar]
- 20.AL-Sayyad MJ. Taylor Spatial Frame in the treatment of pediatric and adolescent tibial shaft fractures. J Pediatr Orthop. 2006;26:164–170. doi: 10.1097/01.bpo.0000218522.05868.f9. [DOI] [PubMed] [Google Scholar]
- 21.Oztürkmen Y, Karamehmetoglu M, Karadeniz H, et al. Acute treatment of segmental tibial fractures with the Ilizarov method. Injury. 2009;40:321–326. doi: 10.1016/j.injury.2008.07.013. [DOI] [PubMed] [Google Scholar]
- 22.Dagher F, Roukoz S. Compound tibial fractures with bone loss treated by the Ilizarov technique. J Bone Joint Surg Br. 1991;73:316–321. doi: 10.1302/0301-620X.73B2.2005164. [DOI] [PubMed] [Google Scholar]
- 23.Whitehouse MR, Livingstone JA. Taylor Spatial Frame application with the aid of a fine wire half frame. J Orthop Trauma. 2008;22:276–281. doi: 10.1097/BOT.0b013e31815d63ec. [DOI] [PubMed] [Google Scholar]
- 24.Kanellopoulos AD, Mavrogenis AF, Kanellopoulos ND, et al. A guide frame for the Taylor Spatial Frame. J Orthop Trauma. 2009;23:537–540. doi: 10.1097/BOT.0b013e3181a24021. [DOI] [PubMed] [Google Scholar]
- 25.Wood GW. General Principles of Fracture Treatment. In: Canale ST, editor. Campbell's Operative Orthopaedics. 10th edn. Vol 3. Philadelphia: Mosby; 2003. p. p2,671. [Google Scholar]
- 26.Royal College of Nursing London: RCN; 2011. Guidance on Pin Site Care. [Google Scholar]
- 27.Woll TS, Duwelius PJ. The segmental tibial fracture. Clin Orthop Relat Res. 1992;281:204–207. [PubMed] [Google Scholar]
- 28.Fleming B, Paley D, Kristiansen T, Pope M. A biomechanical analysis of the Ilizarov external fixator. Clin Orthop Relat Res. 1989;241:95–105. [PubMed] [Google Scholar]
- 29.Yang L, Saleeh M, Nayagam S. The effects of different wire and screw combinations on the stiffness of a hybrid external fixator. Proc Inst Mech Eng H. 2000;214:669–676. doi: 10.1243/0954411001535697. [DOI] [PubMed] [Google Scholar]
- 30.Merchant TC, Dietz FR. Long-term follow-up after fractures of the tibial and fibular shafts. J Bone Joint Surg Am. 1989;71:599–606. [PubMed] [Google Scholar]
- 31.Rommens PM, Coosemans W, Broos PL. The difficult healing of segmental fractures of the tibial shaft. Arch Orthop Trauma Surg. 1989;108:238–242. doi: 10.1007/BF00936208. [DOI] [PubMed] [Google Scholar]
- 32.Sarmiento A, Latta LL. Functional treatment of closed segmental fractures of the tibia. Acta Chir Orthop Traumatol Cech. 2008;75:325–331. [PubMed] [Google Scholar]
- 33.Kakar S, Tornetta P. Segmental tibial fractures: a prospective evaluation. Clin Orthop Relat Res. 2007;460:196–201. doi: 10.1097/BLO.0b013e318050a3f0. [DOI] [PubMed] [Google Scholar]
- 34.McDonald MG, Burgess RC, Bolano LE, Nicholls PJ. Ilizarov treatment of pilon fractures. Clin Orthop Relat Res. 1996;325:232–238. doi: 10.1097/00003086-199604000-00028. [DOI] [PubMed] [Google Scholar]
- 35.Leung F, Kwok HY, Pun TS, Chow SP. Limited open reduction and Ilizarov external fixation in the treatment of distal tibial fractures. Injury. 2004;35:278–283. doi: 10.1016/s0020-1383(03)00172-4. [DOI] [PubMed] [Google Scholar]
- 36.Dendrinos GK, Kontos S, Katsenis D, Dalas A. Treatment of high-energy tibial plateau fractures by the Ilizarov circular fixator. J Bone Joint Surg Br. 1996;78:710–717. [PubMed] [Google Scholar]
- 37.Henley MB, Chapman JR, Agel J, et al. Treatment of type II. IIIA, and IIIB open fractures of the tibial shaft: a prospective comparison of unreamed interlocking intramedullary nails and half-pin external fixators. J Orthop Trauma. 1998;12:1–7. doi: 10.1097/00005131-199801000-00001. [DOI] [PubMed] [Google Scholar]
- 38.Marsh JL, Bonar S, Nepola JV, et al. Use of an articulated external fixator for fractures of the tibial plafond. J Bone Joint Surg Am. 1995;77:1,498–1,509. doi: 10.2106/00004623-199510000-00004. [DOI] [PubMed] [Google Scholar]