Abstract
Introduction
This study aimed to determine whether ethnic differences show different patterns of arterial disease in the lower limb.
Methods
A prospective analysis of 100 consecutive patients with 160 lower limb arteriograms was performed looking at the pattern of disease with relation to ethnicity in Trinidad and Tobago.
Results
There were 53 male and 47 female patients with an age range of 43–90 years (mean: 66 years). Of the 100 patients, 45 were of East Indian descent, 36 of Afro-Caribbean descent, 14 of mixed descent and 5 had other backgrounds. There were 32 smokers and 69 diabetics.
The most commonly affected artery in East Indians was the anterior tibial artery (ATA, 70%) followed by the peroneal artery (60%), superficial femoral artery (SFA, 60%), posterior tibial artery (PTA, 57%) and tibioperoneal trunk (TPT, 39%). In Afro-Caribbeans, the most commonly affected artery was the ATA (79%) followed by the PTA (74%), peroneal artery (66%) and TPT (55%). The mixed group showed the PTA (85%) to be most diseased followed by the peroneal artery (75%), ATA (70%), SFA (70%), dorsalis pedis artery (DPA, 60%) and TPT (50%). Overall, the most diseased vessel in all groups was the ATA (73%) followed by the PTA (66%), peroneal artery (64%), SFA (59%), TPT (46%), DPA (38%), popliteal artery (31%) and medial plantar artery (MPA, 29%), with the proximal vessels not being affected severely.
Conclusions
Ethnic divisions were only statistically significant (p<0.05) with East Indians showing worse disease in the profunda femoris artery and Afro-Caribbeans showing worse disease in the PTA, DPA and MPA. This suggests that environmental factors may play a significant role in the disease process including smoking and dietary factors rather than purely genetics.
Keywords: Angiographic findings, Arteriosclerotic lesion, Lower limb
Diabetes and peripheral vascular disease are responsible for a significant amount of lower extremity amputations in the Caribbean. 1 Trinidad and Tobago is the southern-most island in the Caribbean, adjacent to the South American continent, and is composed of a diverse population owing to its colourful history of occupation by the French, Spanish and British with indentured labourers being brought here hundreds of years previously from the Indian and African continents. Approximately 40% of the population is of East Indian descent, 38% of African descent and 18% of mixed descent, the remainder being of European, Chinese, Lebanese or Syrian descent. It is with this in mind that a prospective analysis was performed looking at the pattern and distribution of lower limb arterial disease with relation to ethnicity.
Methods
A prospective study was conducted for the period January to November 2010 with four vascular and cardiovascular referral centres in Trinidad and Tobago. The records of all cases admitted to the respective units that required angiographic imaging for lower extremity vascular disease were analysed. Demographic data were collected on age, sex, ethnicity, co-morbidities, diabetic and smoking status.
Regarding the lower extremity, further information was recorded on indication for angiography (rest pain, non-healing ulcers, dry gangrene or claudication), the type of angiography (digital subtraction [DSA], magnetic resonance [MRA] or computed tomography [CTA]) and if any procedures were carried out (including percutaneous angioplasty, bypass or amputation). Findings/occlusions of angiographic patterns were recorded from the common iliac artery (CIA), the internal iliac artery (IIA), the external iliac artery (EIA), the common femoral artery (CFA), the superficial femoral artery (SFA), the profunda femoris artery (PFA), the popliteal artery, the tibioperoneal trunk (TPT), the anterior tibial artery (ATA), the posterior tibial artery (PTA) and the peroneal artery as well as the pedal arteries including the dorsalis pedis artery (DPA) and the medial plantar artery (MPA).
The severity of disease for each vessel was scored using the semiquantitative Bollinger scoring system, 2 with subclassification into two groups: those with a Bollinger score of ≥13 (extensive disease with a complete occlusion of at least half the segment length) and those with a score of <13 (mild to moderate disease with plaques and stenosis encompassing more than half the diameter of the vessel, stenosis narrowing the lumen by more than 25% but less than 50% and plaques stenosing the artery by less than 25%). In the presence of complete occlusions, other plaques and stenosis were not considered, and the score remained 13 even with marked plaque formation in the non-occluded part of the segment. All angiography was reviewed independently and the assessment of occlusive disease standardised.
This was done by classifying the lower limb arterial tree into four segments. Segment I referred to the CIA, the EIA and the IIA; segment II referred to the CFA, the PFA, the SFA and the popliteal artery; segment III referred to the TPT, the ATA, the PTA and the peroneal artery; and segment IV referred to the DPA and the MPA.
Analysis was carried out regarding the pattern of disease in relation to ethnicity. Since there were unequal numbers overall between groups, the percentage of disease of each vessel in each particular ethnic group was calculated, and these percentages were compared (Figs 1–4). Statistical differences were tested with the ‘compare means’ option in SPSS® version 20 (IBM, New York, US) using the independent samples t-test. Type of angiography, amputation rates, intervention rates and diabetic status were calculated, and these were included as demographic data to define the population being studied.
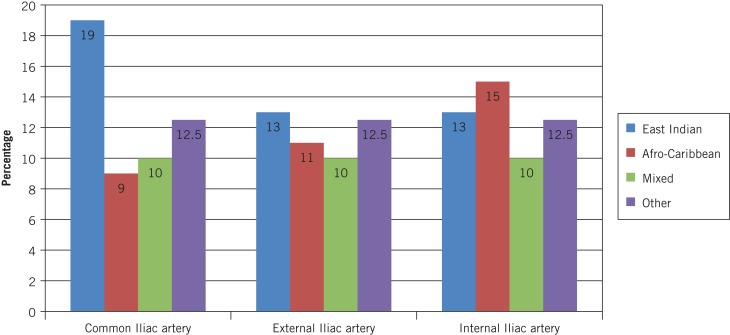
Figure 1.
Comparison of occlusive disease and ethnicity in segment I (common iliac, external iliac and internal iliac arteries).
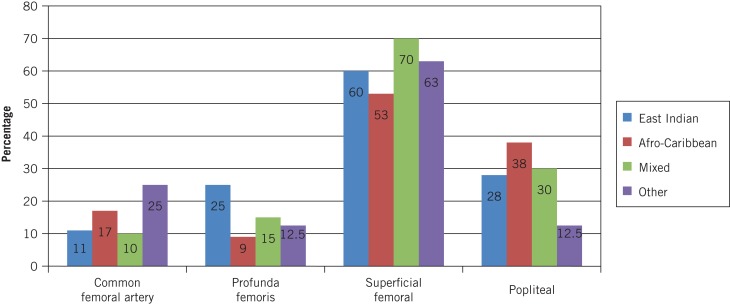
Figure 2.
Comparison of occlusive disease and ethnicity in segment II (common femoral, profunda femoris, superficial femoral and popliteal arteries).
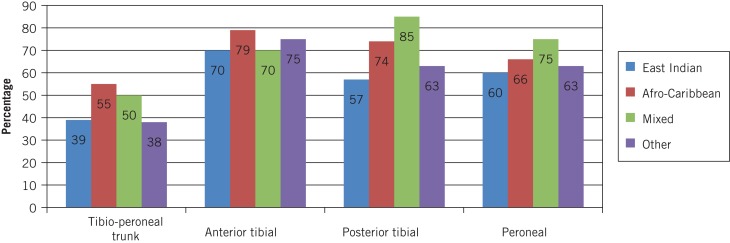
Figure 3.
Comparison of occlusive disease and ethnicity in segment III (tibioperoneal trunk, anterior tibial, posterior tibial and peroneal arteries).
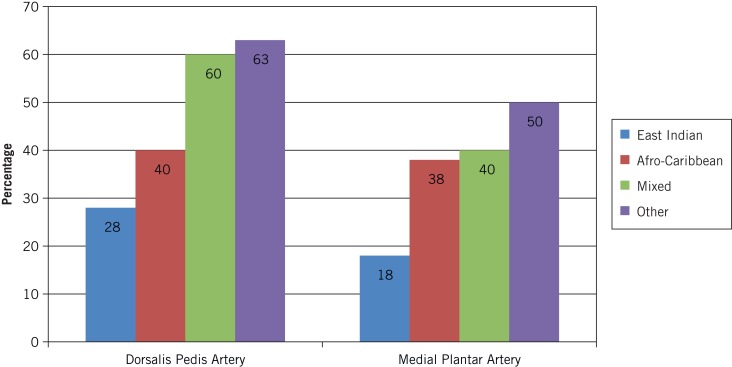
Figure 4.
Comparison of occlusive disease and ethnicity in segment IV (dorsalis pedis and medial plantar arteries).
Results
A total of 100 patients with 160 angiograms of the lower extremity were obtained prospectively (Appendix 1 – available online only). This included 97 MRAs (61%), 53 DSAs (33%) and 10 CTAs (6%). There were 53 male and 47 female patients with an age range of 43–90 years (mean: 66.4 years). There were 45 patients of East Indian descent (79 limbs), 36 of Afro-Caribbean descent (53 limbs), 14 of mixed descent (mixed Chinese, Spanish or African) (20 limbs) and 5 classified as ‘other’ (Chinese, Syrian or Caucasian) (8 limbs). There were 32 smokers, 69 diabetics (56% being East Indian) and 31 non-diabetics.
The main indications for angiography included rest pain (25.0%), dry gangrene (23.8%), claudication (12.5%), non-healing ulcers (11.3%) and wet gangrene (6.9%). Asymptomatic legs that had angiography as part of assessing symptomatic legs accounted for 27.5% and 7% of patients had more than one indication for angiography. There were 72 procedures performed on 160 limbs including 22 major amputations (15 below the knee and 7 above the knee), 15 femoropopliteal bypasses, 13 femorodistal bypasses, 6 popliteal-distal bypasses, 6 digital amputations, 5 transmetatarsal amputations, 4 percutaneous transluminal angioplasties and 1 profundoplasty.
East Indian population
The most commonly affected vessel in East Indian patients was the ATA (70%) followed by the peroneal artery (60%), SFA (60%), PTA (57%), TPA (39%), DPA (28%), popliteal artery (28%) and PFA (25%) with the proximal vessels (CIA, EIA, IIA, CFA) and medial plantar artery (MPA) ranging between 11% and 19%.
Afro-Caribbean population
In Afro-Caribbean patients, the most commonly affected vessel was the ATA (79%) followed by the PTA (74%), peroneal artery (66%), TPT (55%), SFA (53%), DPA (40%), popliteal artery (38%) and MPA (38%) with the proximal vessels (CIA, EIA, IIA, CFA, PFA) ranging between 9% and 17%.
Mixed population
In the mixed population, the most commonly affected vessel was the PTA (85%) followed by the peroneal artery (75%), ATA (70%), SFA (70%), DPA (60%), TPT (50%), MPA (40%) and popliteal artery (30%) with the proximal vessels (CIA, EIA, IIA, PFA) ranging between 10% and 15%.
Other ethnic backgrounds
In the ‘other’ group, the most diseased vessel was the ATA (75%) followed jointly by the SFA, PTA, peroneal artery and DPA (all at 63%), then the MPA (50%) and TPT (38%) with the proximal vessels (CIA, EIA, IIA, CFA, PFA) ranging between 13% and 25% (Figs 1–4).
Overall, the most diseased vessel in all groups was the ATA (73%) followed by the PTA (66%), peroneal artery (64%) and SFA (59%). The TPT (46%) was also significantly diseased, followed by the DPA (38%), popliteal artery (31%) and MPA (29%) with the proximal vessels (CIA, EIA, IIA, CFA, PFA) ranging between 12% and 18%. The Bollinger score generally increased in all categories of patients as the vessels became more distal, with the SFA and crural vessels having the highest scores.
The independent samples t-test was applied between ethnic groups. There was a statistically significant difference between East Indians and Afro-Caribbeans with regard to the PFA, PTA, DPA and MPA with the East Indians having worse disease in the PFA but the Afro-Caribbeans having worse disease in the PTA, DPA and MPA (p<0.05). In terms of East Indians versus those of mixed descent, a similar pattern arose with the mixed group having worse disease (p<0.05) in the PTA, DPA and MPA (Figs 1–4). There were no statistically significant differences with regard to the other vessels including the CIA, IIA, EIA, CFA, SFA, popliteal artery, ATA and peroneal arteries.
Discussion
Haimovici first described patterns of arterial disease in the 1960s with his landmark studies published in the Archives of Surgery and Surgery. 3,4 The analysis performed in our study assesses the distribution of arterial disease based on ethnicity and angiographic findings.
In the UK, Jude et al conducted a study in Manchester to map the distribution of peripheral arterial disease in a mixed diabetic and non-diabetic population. 5 A total of 136 arteriograms were analysed according to the Bollinger system. This showed that diabetic patients had greater severity of arterial disease in the PFA and all arterial segments below the knee. Furthermore, diabetic patients were five times more likely to have an amputation. Conversely, in our series, although the superficial femoral and infrapopliteal vessels were severely diseased, the PFA was one of the least affected after the more proximal limb vessels.
A more recent UK article by Morris-Stiff et al analysed the variations in the anatomical distribution of peripheral vascular disease related to sex. 6 This showed that peripheral arterial disease affects more numerous sites in men, with the difference being greater at the CFA and PFA.
Several studies have also been conducted in the European community. The Italian study by Civarella et al analysed angiography of 150 patients with limb threatening ischaemia (rest pain, non-healing ischaemic ulcers or gangrene). 7 This revealed that diabetic patients demonstrated more occlusive disease in the infrapopliteal vessels than non-diabetic patients, who had more involvement of the aortoiliac and femoropopliteal arteries. Diabetic patients also had a higher prevalence of obstruction in the posterior tibial, peroneal and plantar arteries than non-diabetics. The pattern was similar in our series, with the ATA being the most diseased on angiography in all our ethnic groups, followed by the posterior tibial and peroneal vessels. It seemed that the Afro-Caribbean, mixed and white/Arabic groups also had worse TPT and pedal disease (DPA and MPA) than East Indians (Figs 3 and 4).
With regard to lower extremity disease in the Caribbean community, few data are available, with only two studies. The first paper by Tromp et al showed that limb salvage rates were 74.5% after 1 year and 71.4% after 5 years for a series of 108 patients undergoing infrainguinal arterial reconstructions. 8 Another paper published by Deneuville et al from the French West Indies showed that out of 42 infrapopliteal bypass procedures perfromed for limb salvage in 39 patients (22 diabetics), 87% had tissue loss at admission (8 ulcers, 13 digital gangrene cases and 13 extensive foot infections). 9 Angiographic findings showed involvement of the femoral and crural vessels with outflow anastomotic sites being the popliteal artery in 5, tibial artery in 14, peroneal artery in 14 and the pedal arteries in 9 cases. Autologous vein was suitable in 27 and inadequate in 15 cases, which then required composite or prosthetic grafts.
Conclusions
The most diseased vessel in all groups was the ATA (73%) followed by the PTA (66%), peroneal artery (64%) and SFA (59%). The TPT (46%) was also significantly diseased, followed by the DPA (38%), popliteal artery (31%) and MPA (29%) with the proximal vessels (CIA, EIA, IIA, CFA, PFA) ranging between 12% and 18%.
The Bollinger score generally increased in all categories of patients as the vessels became more distal with the SFA and crural vessels having the highest scores. This is consistent with the majority of patients (69%) being diabetic.
There was a significant difference between East Indians and Afro-Caribbeans with regard to the PFA, PTA, DPA and MPA with the East Indians having worse disease in the PFA but the Afro-Caribbeans having worse disease in the PTA, DPA and MPA (p<0.05). In terms of East Indians versus persons of mixed descent, a similar pattern arose with the mixed group having worse disease (p<0.05) in the PTA, DPA and MPA. There were no statistically significant differences for the other vessels including the CIA, IIA, EIA, CFA, SFA, popliteal artery, ATA and peroneal artery.
This may suggest that Afro-Caribbeans and persons of mixed descent present with pedal disease that is less suitable for distal bypasses if necessary compared with East Indians. These ethnic divisions indicate that environmental factors including smoking and dietary factors may play a significant role in the disease process rather than purely genetics.
We acknowledge two potential areas of bias. Over two-thirds of the study population was diabetic and the data were not separated for analysis. Furthermore, there were not equal numbers in each ethnic group. It seemed that East Indians presented more commonly with peripheral vascular disease than the other races. However, this study provides valuable information regarding the pattern of peripheral vascular disease with the ability to compare the East Indian, Afro-Caribbean, mixed and Caucasian/Chinese/Arabic population groups owing to the diverse population mix that Trinidad and Tobago possesses compared with other countries. This may be relevant in certain countries such as the UK, particularly in the East London communities and communities where there may be a high East Indian, Afro-Caribbean and growing mixed population in the management of peripheral arterial disease. We hope this information is useful for future endeavours.
Appendix 1.
Demographic data
| East Indian (45 patients, 79 limbs) |
Afro-Caribbean (36 patients, 53 limbs) |
Mixed (14 patients, 20 limbs) |
Other (5 patients, 8 limbs) |
Total (100 patients, 160 limbs) |
|
|---|---|---|---|---|---|
| Male Female |
28 17 |
17 19 |
6 8 |
2 3 |
53 47 |
| Mean age (range) in years | 63 (47–83) | 68 (43–90) | 70 (50–90) | 73 (58–89) | 66 (43–90) |
|
Patients in age range
41–50 51–60 61–70 71–80 81–90 |
6 11 19 8 1 |
6 4 8 13 5 |
3 3 5 2 1 |
0 1 1 1 2 |
15 19 33 24 9 |
| Unilateral Bilateral |
11 34 (68 limbs) |
19 17 (34 limbs) |
8 6 (12 limbs) |
2 3 (6 limbs) |
40 60 (120 limbs) |
| Non-diabetic Diabetic only Diabetic and other risk factors |
6 14 25 |
9 5 13 |
2 3 8 |
2 0 1 |
19 22 47 |
| Total diabetic | 39 | 18 | 11 | 1 | 69 |
| Smokers | 16 | 12 | 3 | 1 | 32 |
| Aspirin | 11 | 5 | 3 | 2 | 21 |
|
Indications
Asymptomatic Rest pain Dry gangrene Claudication Non-healing ulcer Wet gangrene |
22 13 18 8 10 8 |
17 19 13 8 5 1 |
4 6 7 1 2 2 |
1 2 0 3 1 0 |
44 40 38 20 18 11 |
|
Type of angiography
Digital subtraction angiography Magnetic resonance angiography Computed tomography angiography |
16 58 5 |
22 25 6 |
8 12 0 |
6 2 0 |
52 97 11 |
|
Procedure
Below-knee amputation Above-knee amputation Femoropopliteal bypass Femorodistal bypass Popliteal-distal bypass Digital amputation Transmetatarsal amputation Percutaneous transluminal angioplasty Profundoplasty |
6 2 9 9 2 3 3 1 1 |
5 2 4 1 1 2 2 2 0 |
4 3 1 3 3 1 0 1 0 |
0 0 1 0 0 0 0 0 0 |
15 7 15 13 6 6 5 4 1 |
References
- 1.Solomon S, Affan AM, Gopie P, et al. Taking the next step in 2005, the year of the diabetic foot. Prim Care Diabetes. 2008;2:175–180. doi: 10.1016/j.pcd.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 2.Bollinger A, Breddin K, Hess H, et al. Semiquantitative assessment of lower limb atherosclerosis from routine angiographic images. Atherosclerosis. 1981;38:339–346. doi: 10.1016/0021-9150(81)90050-2. [DOI] [PubMed] [Google Scholar]
- 3.Haimovici H. Patterns of arteriosclerotic lesions of the lower extremity. Arch Surg. 1967;95:918–933. doi: 10.1001/archsurg.1967.01330180066012. [DOI] [PubMed] [Google Scholar]
- 4.Haimovici H, Steinman C. Aortoiliac angiographic patterns associated with femoropopliteal occlusive disease: significance in reconstructive arterial surgery. Surgery. 1969;65:232–240. [PubMed] [Google Scholar]
- 5.Jude EB, Oyibo SO, Chalmers N, Boulton AJ. Peripheral arterial disease in the diabetic and nondiabetic patients. Diabetes Care. 2001;24:1,433–1,437. doi: 10.2337/diacare.24.8.1433. [DOI] [PubMed] [Google Scholar]
- 6.Morris-Stiff G, Ogunbiyi S, Rees J, et al. Variations in the anatomical distribution of peripheral vascular disease according to gender. Ann R Coll Surg Engl. 2011;93:306–309. doi: 10.1308/003588411X571999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ciavarella A, Silletti A, Mustacchio A, et al. Angiographic evaluation of the anatomic pattern of arterial obstructions in diabetic patients with critical limb ischaemia. Diabete Metab. 1993;19:586–589. [PubMed] [Google Scholar]
- 8.Tromp HR, van Leeuwen JE, Fieuws S. Infra-inguinal arterial reconstruction for peripheral arterial disease: the Curaçao experience. West Indian Med J. 2007;56:439–445. [PubMed] [Google Scholar]
- 9.Deneuville M, Stouff S, N’guyen R. Infrapopliteal bypass for critical limb ischaemia. Early experience in the French West Indies. West Indian Med J. 1996;45:55–59. [PubMed] [Google Scholar]