Abstract
Introduction
Coccygodynia is a condition associated with severe discomfort in the region of the coccyx. While traditional procedures had poor outcomes and high complication rates, recent literature suggests better outcomes and lower complication rates with coccygectomy.
Methods
Data were collected retrospectively from clinical notes. A questionnaire was used to evaluate the outcomes. The outcome measures included pain analogue score (PAS) in sitting and during daily activities as well as patients’ overall pain relief. Overall improvement in pain and complications were documented.
Results
Between 2000 and 2010, 14 patients underwent total coccygectomy for refractory coccygodynia. All patients were available for follow-up appointments and the follow-up duration ranged from 24 to 132 months (mean: 80 months). The aetiology was traumatic in eight patients and non-traumatic in six. The PAS improved from a median of 9 to 4 for sitting and from 7.5 to 2.5 for daily activities. One patient had mild discharge for more than two weeks. No patients required further surgery. Twelve patients (85.7%) had excellent or good pain relief. Only one patient was unsatisfied. A Wilcoxon signed-rank test revealed significant improvement in pain when sitting (p<0.05) and during activities of daily living (p<0.05) at the final follow-up visit. A Mann–Whitney U test did not show a significant difference in improvement in PAS between the traumatic and non-traumatic groups (p=0.282 and 0.755).
Conclusions
In our series, total coccygectomy offered satisfactory relief of pain in the majority of patients with a low wound complication rate.
Keywords: Coccygodynia, Coccygectomy, Aetiology, Traumatic, Non-traumatic, Outcome
The term coccygodynia was coined by Simpson in 1859. 1 The pain is usually provoked by sitting or rising from sitting. 2 Most cases are associated with abnormal mobility of the coccyx, which may trigger a chronic inflammatory process leading to degeneration of this structure. 3 Patients usually present with pain during sitting and defecation. 4 A male-to-female ratio of 1:4 has been reported. 5
The most common aetiological factor for coccygodynia is direct trauma, noted in 40% of the patients in one study. 6 Other proposed aetiological factors include postpartum (20%) and idiopathic (29%) factors, 7 and following spinal fusion. 8 Postacchini and Massobrio suggested that the anatomy of the coccyx might be a causative factor. 4 Coccygodynia has also been reported in people with mental instability and in those suffering from depression or hypochondria. 9,10 Furthermore, tumours and infections have been reported to cause pain arising from the coccyx. 11 Maggiani et al found a glomus coccygeum in 35% of coccygectomy specimens. 12
Conservative management including ring shaped cushions, 7 a hot bath, 13 coccygeal massage, 3 physiotherapy and stretching, 3 manipulation, 3 steroid injections and non-steroidal anti-inflammatory drugs (NSAIDs), 14 and transcutaneous nerve stimulation 15 can be successful in up to 85–90% of patients. 16,17 Surgical treatment for coccygodynia has been viewed with caution historically 2 as it has been associated with high complication rates and variable effectiveness. Better outcomes with coccygectomy have been reported more recently. 6 In our retrospective case series, we report good or excellent outcomes for this operation in 14 patients who underwent this procedure for refractory coccygodynia.
Methods
Fourteen consecutive patients underwent a coccygectomy during 2000–2010 by the senior author (ST). All patients had failed at least six months of conservative treatment before undergoing surgery. The non-operative treatment included cushions, NSAIDs, physiotherapy and steroid injections. The aetiology of the coccygodynia and past medical history of patients (including any spinal operations) were recorded. Tenderness on external/rectal examination prior to surgery confirmed the coccyx as the source of the patients’ discomfort.
Surgery was performed in the prone position under general anaesthesia. No bowel preparation was used preoperatively. Skin preparation was performed using 2% chlorhexidine and subsequently povidone-iodine (Betadine®; Mölnlycke, Dunstable, UK) solution, which was left to dry. Antimicrobial adhesive draping (Ioban™; 3M, Bracknell, UK) was then applied to ensure a complete seal. A posterior midline longitudinal incision was performed, followed by subperiosteal dissection. Disarticulation was performed at the sacrococcygeal joint and the coccyx was removed in one piece. The distal end of the sacrum was chamfered.
Meticulous haemostasis was achieved using bipolar diathermy. The wound was then irrigated with normal saline and a single drain inserted. Closure was performed in layers using Vicryl® sutures (Ethicon, Somerville, NJ, US) for periosteum and subcutaneous tissue, and mattress nylon sutures for the skin. Dermabond® glue (Ethicon) and Mepore® dressings (Mölnlycke) were applied to the skin for protection. Intravenous cefuroxime was given on induction and oral co-amoxiclav continued until the wound was dry. The drain was removed after 24 hours and sutures were removed two weeks following surgery. Patients were allowed to mobilise and sit as tolerated.
All patients were available for follow-up appointments. A questionnaire was used to evaluate the outcomes. The outcome measures included pain analogue score (PAS) in sitting and during activities of daily living (ADLs) as well as patients’ overall satisfaction. Satisfaction was categorised in four groups: unsatisfied, fairly satisfied, good and excellent. Complications were documented. All patients had a minimum follow-up duration of 24 months.
Data were analysed using SPSS® version 15 (SPSS, Chicago, IL, US). As data were not normally distributed, non-parametric tests were used. The Wilcoxon signed-rank test was used to compare the paired samples (ie scores before and after the operation in the same patients) and the Mann-Whitney U test was used to compare the outcomes in independent samples (ie to compare the outcomes in the traumatic vs non-traumatic groups).
Results
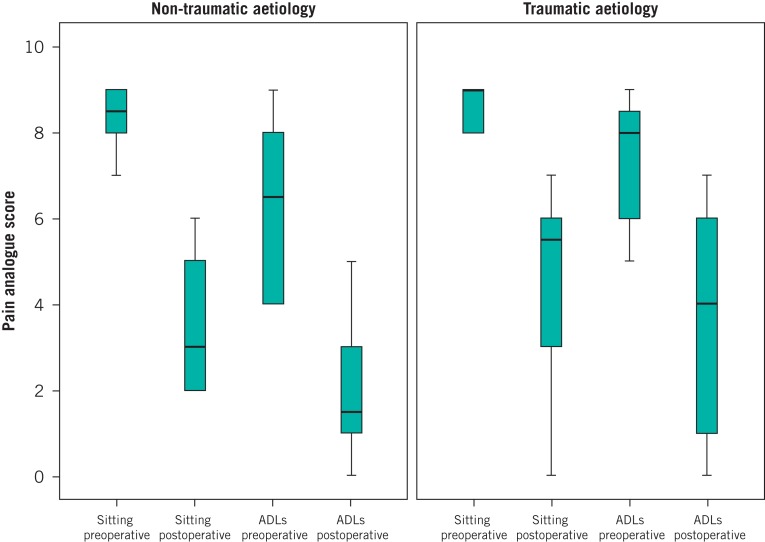
Twelve of the fourteen patients were female. The mean patient age was 39.4 years (standard deviation [SD]: 11.5 years). The cause of pain was traumatic in eight patients and non-traumatic in six patients (one postpartum, two following spinal fusion surgery and three idiopathic). The duration of symptoms was 18–84 months (mean: 30 months, SD: 17.4 months). The follow-up duration ranged from 24 to 132 months (mean: 80 months). The improvements in PAS in both traumatic and non-traumatic groups are shown in Figure 1.
Figure 1.
Improvements in pain analogue score in traumatic and non-traumatic aetiology groups. ADLs = activities of daily living.
The results of the PAS for sitting and during ADLs, and the results of the statistical analysis are summarised in Table 1. A Mann–Whitney U test did not show any significant difference in improvement in PAS between the traumatic and non-traumatic groups (PAS for sitting: p=0.282, PAS during ADLs: p=0.755).
Table 1.
Results and outcomes of operations
| Traumatic aetiology | Non-traumatic aetiology | Total | |
|---|---|---|---|
| Number of patients | 8 | 6 | 14 |
| Median PAS in sitting | |||
| Preoperative | 9 | 8.5 | 9 |
| Postoperative | 5.5 | 3 | 4 |
| p-value* | 0.017 | 0.027 | <0.001 |
| Median PAS during ADLs | |||
| Preoperative | 8 | 6.5 | 7.5 |
| Postoperative | 4 | 1.5 | 2.5 |
| p-value* | 0.017 | 0.027 | <0.001 |
| Overall satisfaction | |||
| Excellent | 3 | 4 | 7 |
| Good | 3 | 2 | 5 |
| Satisfied | 1 | 0 | 1 |
| Unsatisfied | 1 | 0 | 1 |
PAS = pain analogue score; ADLs = activities of daily living
Wilcoxon signed-rank test
Complications included one case (7%) of prolonged wound oozing (more than two weeks), which resolved with dressing change and oral antibiotics. There were no other complications.
Discussion
We report favourable outcomes in 12/14 patients (85.7%) who were treated for refractory coccygodynia. In our series, coccygectomy produced good results for both traumatic and non-traumatic coccygodynia. Our findings are in agreement with the recent literature. While earlier results of coccygectomy were discouraging, more recently, good outcomes for the procedure have been reported.
Patient selection is one of the most important factors for ensuring a good outcome for coccygectomy. Referred pain from a lumbosacral disc prolapse due to irritation of the sacral nerves is an important differential diagnosis that must be excluded. 10 In such cases, coccygectomy is contraindicated. 9,18 We confirmed tenderness of the coccyx by digital rectal examination prior to surgery and ensured that the exact symptoms were reproduced before considering treatment. When necessary, diagnosis was confirmed by injection of local anaesthetic and dye in the sacrococcygeal joint.
Patients with evidence of advanced coccygeal instability (eg subluxation or hypermobility) or spicule formation have been reported to have the greatest improvement postoperatively. 3 Two of our patients developed coccygodynia within six months of lumbar spinal fusion surgery. No other apparent cause was found for pain. They did not have any complaints regarding the previous surgical site. Both patients were in the satisfied group. We do not consider previous uncomplicated lumbar surgical fusion a contraindication to coccygectomy.
There are several limitations to our study. The number of patients was relatively low. It was a retrospective study and so was lacking interim follow-up data. The strength of our study is that all patients were operated on by a single surgeon with identical surgical techniques. We believe that careful preparation and draping, subperiosteal dissection of the bone and meticulous wound closure is an important factor in preventing wound complications, which is the major drawback of this procedure.
A PAS was used for the assessment of outcomes. Patients with coccygodynia complain of localised pain in the area of the coccyx, which does not normally affect activities that are assessed by scoring systems such as the Oswestry Disability Index, which was designed for back pain. 19 For example, localised pain is unlikely to affect personal care or the ability to lift objects. We thought that a general PAS during ADLs would give a better assessment of the effect of this pain on patient perception.
Conclusions
Our results confirm those of the current literature, namely that coccygectomy is a successful treatment for the majority of patients suffering from refractory coccygodynia. Our data suggest that with correct patient selection and meticulous operative technique, good results can be achieved with coccygectomy, with a low complication rate.
Acknowledgement
The authors would like to thank Suzie Cro for her advice and supervision of the statistical analysis.
References
- 1.Powers JA. Coccygectomy. South Med J. 1957;50:675–678. doi: 10.1097/00007611-195705000-00024. [DOI] [PubMed] [Google Scholar]
- 2.Kerr EE, Benson D, Schrot RJ. Coccygectomy for chronic refractory coccygodynia: clinical case series and literature review. J Neurosurg Spine. 2011;14:654–663. doi: 10.3171/2010.12.SPINE10262. [DOI] [PubMed] [Google Scholar]
- 3.Patel R, Appannagari A, Whang PG. Coccydynia. Curr Rev Musculoskelet Med. 2008;1:223–226. doi: 10.1007/s12178-008-9028-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Postacchini F, Massobrio M. Idiopathic coccygodynia. Analysis of fifty-one operative cases and a radiographic study of the normal coccyx. J Bone Joint Surg Am. 1983;65:1,116–1,124. [PubMed] [Google Scholar]
- 5.Balain B, Eisenstein SM, Alo GO, et al. Coccygectomy for coccydynia: case series and review of literature. Spine. 2006;31:E414–E420. doi: 10.1097/01.brs.0000219867.07683.7a. [DOI] [PubMed] [Google Scholar]
- 6.Karadimas EJ, Trypsiannis G, Giannoudis PV. Surgical treatment of coccygodynia: an analytic review of the literature. Eur Spine J. 2011;20:698–705. doi: 10.1007/s00586-010-1617-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Trollegaard AM, Aarby NS, Hellberg S. Coccygectomy: an effective treatment option for chronic coccydynia: retrospective results in 41 consecutive patients. J Bone Joint Surg Br. 2010;92:242–245. doi: 10.1302/0301-620X.92B2.23030. [DOI] [PubMed] [Google Scholar]
- 8.Spence KF. Coccygectomy. Am J Surg. 1961;102:850–853. doi: 10.1016/0002-9610(61)90597-9. [DOI] [PubMed] [Google Scholar]
- 9.Bayne O, Bateman JE, Cameron HU. The influence of etiology on the results of coccygectomy. Clin Orthop Relat Res. 1984;190:266–272. [PubMed] [Google Scholar]
- 10.Pyper JB. Excision of the coccyx for coccydynia. J Bone Joint Surg Br. 1957;39:733–737. doi: 10.1302/0301-620X.39B4.733. [DOI] [PubMed] [Google Scholar]
- 11.Patijn J, Janssen M, Hayek S, et al. Coccygodynia. Pain Pract. 2010;10:554–559. doi: 10.1111/j.1533-2500.2010.00404.x. [DOI] [PubMed] [Google Scholar]
- 12.Maggiani F, Kashima T, Ostlere SJ, Athanasou NA. Immunophenotypic analysis of glomus coccygeum associated with coccygodynia. Skeletal Radiol. 2011;40:1,455–1,459. doi: 10.1007/s00256-011-1128-0. [DOI] [PubMed] [Google Scholar]
- 13.Kotecha AK, Mofidi A, Morgan-Hough C, Trivedi J. Coccygectomy for coccygodynia: do we really have to wait? Injury. 2008;39:816–817. doi: 10.1016/j.injury.2007.12.023. [DOI] [PubMed] [Google Scholar]
- 14.Khan SA, Kumar A, Varshney MK, et al. Dextrose prolotherapy for recalcitrant coccygodynia. J Orthop Surg. 2008;16:27–29. doi: 10.1177/230949900801600107. [DOI] [PubMed] [Google Scholar]
- 15.Zayer M. Coccygodynia. Ulster Med J. 1996;65:58–60. [PMC free article] [PubMed] [Google Scholar]
- 16.Capar B, Akpinar N, Kutluay E, et al. Coccygectomy in patients with coccydynia. Acta Orthop Traumatol Turc. 2007;41:277–280. [PubMed] [Google Scholar]
- 17.Traub S, Glaser J, Manino B. Coccygectomy for the treatment of therapy-resistant coccygodynia. J Surg Orthop Adv. 2009;18:147–149. [PubMed] [Google Scholar]
- 18.Eng JB, Rymaszewski L, Jepson K. Coccygectomy. J R Coll Surg Edinb. 1988;33:202–203. [PubMed] [Google Scholar]
- 19.Fairbank JC, Couper J, Davies JB, O'Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]