Abstract
Introduction
The primary aim of this study was to investigate the relationship between obesity and recurrent intervertebral disc prolapse (IDP) following lumbar microdiscectomy.
Methods
A retrospective review of case notes from 2008 to 2012 was conducted for all patients who underwent single level lumbar microdiscectomy performed by a single surgeon. All patients were followed up at two weeks and six weeks following surgery, and given an open appointment for a further six months.
Results
A total of 283 patients were available for analysis: 190 (67%) were in the non-obese group and 93 (32.9%) in the obese group. There was no statistical difference in postoperative infection, dural tear or length of stay between the non-obese and obese groups. Recurrent symptomatic IDP was seen in 27 patients (9.5%) confirmed by magnetic resonance imaging. Nineteen (10.0%) were in the non-obese group and eight (8.6%) in the obese group (p>0.8).
Conclusions
In our study, obesity was not a predictor of recurrent IDP following lumbar microdiscectomy. Our literature review confirmed that this study reports the largest series to date analysing the relationship between obesity and recurrent IDP following lumbar microdiscectomy in the British population.
Keywords: Intervertebral disc prolapse, Obesity, Recurrence, Microdiscectomy
In the past 25 years, the prevalence of obesity has increased in nearly every country around the world. It is particularly high in England and has more than doubled during this time period. The Health Survey for England report in 2011 confirmed that 62% of adults were overweight or obese in England. 1 This steady rise in obesity causes major public health concern not only because of the association with serious chronic disease related to morbidity and mortality but also the direct financial cost to the National Health Service, which is estimated to be over £5 billion per year. 2 Given the rising incidence of obesity in the adult population, it is inevitable that spinal surgeons will encounter an increasing number of obese patients presenting with lumbar disc herniation.
Single level lumbar discectomy is one of the most common surgical procedures in spinal surgery with good reported patient outcomes. Surgical complications such as surgical site infection, haemorrhage, nerve root injury, recurrence or residual disc, dural tear, discitis and epidural scar formation occur in around 15–30% of cases. 3–6 Recurrent intervertebral disc prolapse (IDP) is a major cause of pain, disability and reoperation with the rate of recurrence after lumbar discectomy reported to be 5–11%. 7 Treatment options for recurrent IDP include conservative management with aggressive pharmacological therapy and physiotherapy or surgical management, which includes revision laminectomy or discectomy. 3
While obesity has been shown in several studies to increase the risk of surgical site infection following orthopaedic spinal surgery, the relationship between obesity as a risk factor for recurrent IDP following lumbar discectomy remains unclear. 8–10 Studies that have looked specifically at whether obesity increases the risk of recurrent IDP are sparse with conflicting data. Meredith et al concluded that obesity was a strong and independent predictor of recurrent IDP after lumbar microdisectomy 7 while Rihn et al found no significant difference between the two groups. 11 The primary aim of our study was to analyse the relationship between obesity and recurrent IDP following single level lumbar discectomy by a single surgeon.
Methods
A retrospective review of case notes from February 2008 to March 2012 was conducted for all patients who underwent single level lumbar discectomy performed by a single surgeon at our institution. The standard criteria for discectomy included significant enduring neurological symptoms that had not been alleviated by non-surgical management and presentation with positive magnetic resonance imaging (MRI) findings within the last six months that correlated with the patient’s level of symptoms. Patients who had previous lumbar spinal surgery and those with cauda equina syndrome were excluded from the study. All patients were followed up at two weeks and six weeks following surgery, and given a further open appointment for six months.
All operations were carried out by the senior author and the surgical technique was standardised. All surgery was performed with the patient in the prone kneeling position and the abdomen hanging freely.
Patient demographics including the body mass index (BMI) were collected from clinical notes. The patients were divided into two cohorts: the non-obese group (BMI <30kg/m2) and the obese group (BMI of ≥30kg/m2). The primary clinical outcome measure was evidence of recurrent IDP on postoperative MRI on the same side and level of the index surgery causing impingement, deviation or compression of nerve tissue (as reported by a musculoskeletal consultant radiologist) that correlated to the patient’s side and level of symptoms. All patients were assessed in the postoperative period at one week and six weeks. Only patients with improved symptoms in this period but who developed new symptoms corresponding to a true recurrence of IDP subsequently were included in this study.
All patients who underwent a discectomy received the standard postoperative advice:
The patient should be mobilised within six to eight hours following surgery (unless contraindicated) while in hospital.
For 6 weeks following surgery, the patient should try not to sit down or lie down for more than 30 minutes during the course of the day in order to avoid irreversible adhesions.
Prolonged bending, stooping or lifting should be avoided for six weeks following surgery.
No physiotherapy was initiated for six weeks after surgery.
Patients should aim to achieve full, unrestricted activities of daily life (including sports) by ten weeks from the time of surgery.
All patients were reviewed at two weeks and at six weeks after surgery. At this last visit, they were referred to the physiotherapist team for a personal trainer spinal rehabilitation programme.
Statistical analysis
Logistic regression analysis was used to analyse the risk of recurrent IDP, BMI, age, length of stay and complications. Fischer’s exact test and the chi-squared test were used to assess the contingency tables with a p-value of <0.05 considered significant. Kaplan–Meier analysis was performed to assess the risk of revision microdiscectomy for recurrence between the two groups and comparison of curves performed with the logrank (Mantel–Cox) test. All analysis was carried out using Prism® version 6 (GraphPad Software, La Jolla, CA, US).
Results
During the 4-year study period, a total of 306 patients underwent single level lumbar discectomy. Only 283 patients were available for analysis as 23 patients did not have their BMI recorded preoperatively or were lost to follow-up. There were 190 patients (67%) in the non-obese group and 93 (33%) in the obese group. The demographic characteristics of the study cohort are presented in Table 1.
Table 1.
Demographics and descriptive characteristics of study cohort (n=283)
| Median age | 48 years (range: 14–83 years) |
|---|---|
| Sex | |
| Male | 44% |
| Female | 56% |
| BMI | |
| Mean | 28.1kg/2 |
| Non-obese group (BMI <30kg/2) | 190 (67%) |
| Obese group (BMI ≥30kg/2) | 93 (33%) |
| Length of stay | |
| Mean | 1.3 days (range: 0–15 days) |
| Non-obese group (BMI <30kg/2) | 1.3 days (range: 0–15 days) |
| Obese group (BMI ≥30kg/2) | 1.1 days (range: 1–7 days) |
| Dural leak | |
| Non-obese group (BMI <30kg/2) | 8 (4.2%) |
| Obese group (BMI ≥30kg/2) | 3 (3.2%) |
| Superficial site infection | |
| Non-obese group (BMI <30kg/2) | 2 (1.1%) |
| Obese group (BMI ≥30kg/2) | 2 (2.2%) |
| MRI for persisting or recurrent symptoms within the first 6 months of index surgery | |
| Total patients scanned | 60 |
| Total patients with recurrent IDP | 27 |
BMI = body mass index; MRI = magnetic resonance imaging; IDP = intervertebral disc prolapse
Recurrent symptomatic IDP was confirmed by MRI in 27 patients (9.5%). There was no statistical difference (p>0.863) between the two groups, with 19 patients (10.0%) in the non-obese group and 8 (8.6%) in the obese group. The mean BMI of patients with recurrence was not significantly higher than that of those without recurrence (29kg/m2 and 28kg/m2 respectively). In the whole study cohort, the mean BMI was 28.1kg/m2 (range: 19–48kg/m2) and the mean length of stay was 1.3 days (range: 0–15 days).
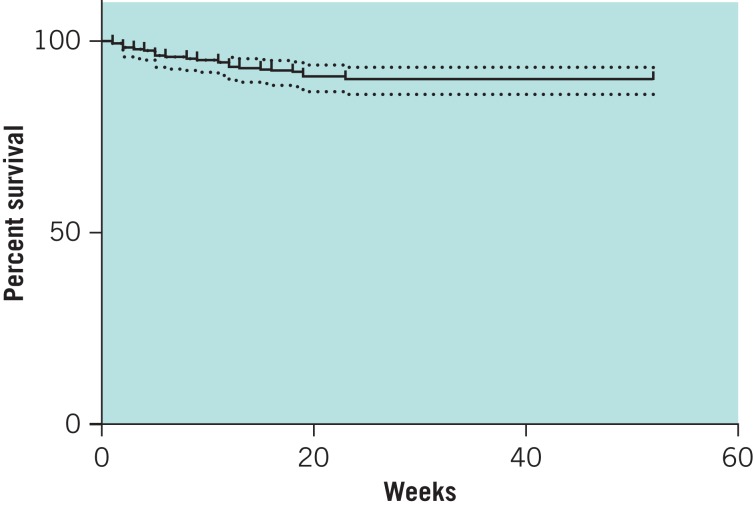
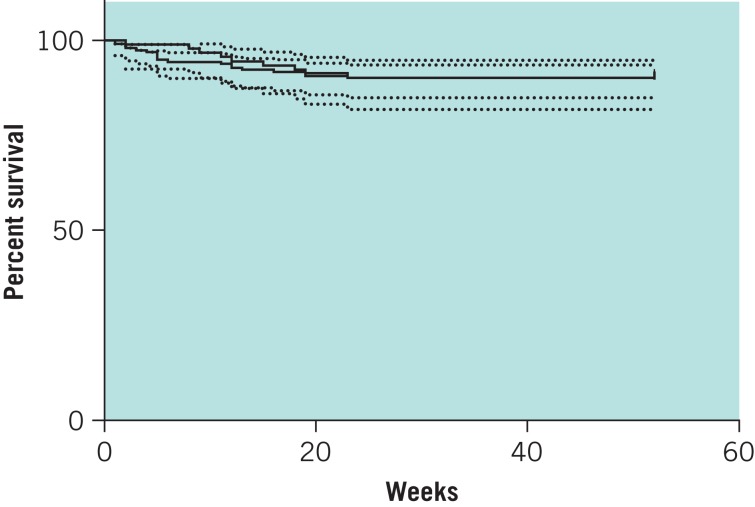
Survival analysis was performed with Kaplan–Meier curves for the two groups with recurrence as an endpoint (Figs 1 and 2). The graphs were compared with logrank regression analysis, which showed no significant difference in the risk of recurrence between the two groups.
Figure 1.
Kaplan–Meier curve for survival with recurrence as an endpoint for all patients with 95% confidence intervals.
Figure 2.
Kaplan–Meier curves for survival with recurrence leading to revision as an endpoint for both the obese and non-obese groups with 95% confidence intervals.
Discussion
Recurrent IDP is a major cause of disability following lumbar discectomy. Controversy still remains regarding the risk factors associated with recurrent disc herniation. Reported risk factors in the literature include male sex, smoking, occupational lifting, diabetes, annular tissue incompetence, preoperative size of the herniation at the time of surgery and high BMI.7,12 Our study did not reveal obesity as a risk factor for recurrent symptomatic disc herniation. The recurrence rate observed in our cohort was 9.5%, which is within the range reported in the literature. 7–11 All patients with recurrence of symptoms had a documented period of resolution of their radicular pain.
There have been only a few of studies that have specifically investigated the relationship between obesity and recurrent disc herniation following lumbar microdiscectomy, with contradicting findings. Meredith et al conducted a retrospective review of 75 patients who underwent 1 or 2-level lumbar microdiscectomy with a minimum follow-up duration of 6 months. 7 The authors concluded that obesity was a strong and independent predictor of recurrent IDP after lumbar microdiscectomy, and that obese patients were 12 times more likely to have recurrent herniated nucleus pulposus than non-obese patients. It is difficult, however, to generalise these findings to the whole population as there were small patient numbers (25 obese patients).
A large prospective study by Rihn et al in 2013 reported different results as no significant difference was found between obese and non-obese patients in the recurrence of disc herniation, need for additional surgical procedures, incidence of nerve root injury, wound haematoma, wound infection or perioperative mortality. 11 Nevertheless, the authors did find that obese patients had significantly longer operating time, more intraoperative blood loss and a longer hospital stay. Although the study was the largest series in the literature specific to lumbar disc herniation, the 854 patients were recruited from 13 multidisciplinary spine practices in 11 states across the US. This could have introduced some bias in terms of patient selection, surgical technique and postoperative rehabilitation.
The study by Rihn et al that looked specifically at outcomes following lumbar discectomy found no significant difference between the obese (2%) and non-obese group (2%). 11 In our study, there was also no significant difference between the two groups although the obese group had a slightly higher infection rate than the non-obese group (2.2% vs 1.1%). Interestingly, when the incidence of dural tear in our study cohort was investigated, the non-obese patients had a significantly higher rate of dural leak than the obese patients. We find this observation difficult to explain although it could possibly be due to the thicker layer of adipose tissue that may have acted as a patch and prevented the obese patients from becoming symptomatic.
To our knowledge, this study is the largest single surgeon series in the literature that has analysed the relationship between obesity and recurrent IDP following lumbar microdiscectomy. Our results suggest that the surgeon can have a non-discriminatory approach when it comes to BMI and patient selection for lumbar disc surgery. The retrospective design is a notable limitation of our study as it was not possible to collect consistent information on other potential risk factors for recurrent IDP such as patient occupation or smoking. In addition, outcome measures (eg SF-36® or Oswestry Disability Index) were recorded inconsistently and were therefore not included for analysis. This, however, was not the aim of our study at the outset.
Conclusions
In our study, obesity was not a predictor of recurrent IDP following lumbar microdiscectomy and did not result in higher complication rates than for the non-obese group. Given the topical nature of obesity in current clinical practice, further studies from multiple centres are recommended to look at the correlation between recurrent disc prolapse and obesity.
References
- 1.Health and Social Care Information Centre Health Survey for England 2011. Leeds: HSCIC; 2011. [Google Scholar]
- 2.Reducing Obesity and Improving Diet Gov.uk. https://www.gov.uk/government/policies/reducing-obesity-and-improving-diet (cited November 2013)
- 3.Swartz KR, Trost GR. Recurrent lumbar disc herniation. Neurosurg Focus. 2003;15:E10. doi: 10.3171/foc.2003.15.3.10. [DOI] [PubMed] [Google Scholar]
- 4.Suk KS, Lee HM, Moon SH, Kim NH. Recurrent lumbar disc herniation: results of operative management. Spine. 2001;26:672–676. doi: 10.1097/00007632-200103150-00024. [DOI] [PubMed] [Google Scholar]
- 5.Mundt DJ, Kelsey JL, Golden AL, et al. An epidemiologic study of non-occupational lifting as a risk factor for herniated lumbar intervertebral disc. Spine. 1993;18:595–602. doi: 10.1097/00007632-199304000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Kelsey JL, Githens PB, O’Connor T, et al. Acute prolapsed lumbar intervertebral disc. An epidemiologic study with special reference to driving automobiles and cigarette smoking. Spine. 1984;9:608–613. doi: 10.1097/00007632-198409000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Meredith DS, Huang RC, Nguyen J, Lyman S. Obesity increases the risk of recurrent herniated nucleus pulposus after lumbar microdiscectomy. Spine J. 2010;10:575–580. doi: 10.1016/j.spinee.2010.02.021. [DOI] [PubMed] [Google Scholar]
- 8.Pull ter Gunne AF, Cohen DB. Incidence, prevalence, and analysis of risk factors for surgical site infection following adult spinal surgery. Spine. 2009;34:1,422–1,428. doi: 10.1097/BRS.0b013e3181a03013. [DOI] [PubMed] [Google Scholar]
- 9.Andreshak TG, An HS, Hall J, Stein B. Lumbar spine surgery in the obese patient. J Spinal Disord. 1997;10:376–379. [PubMed] [Google Scholar]
- 10.Patel N, Bagan B, Vadera S, et al. Obesity and spine surgery: relation to perioperative complications. J Neurosurg Spine. 2007;6:291–297. doi: 10.3171/spi.2007.6.4.1. [DOI] [PubMed] [Google Scholar]
- 11.Rihn JA, Kurd M, Hilibrand AS, et al. The influence of obesity on the outcome of treatment of lumbar disc herniation: analysis of the Spine Patient Outcomes Research Trial (SPORT) J Bone Joint Surg Am. 2013;95:1–8. doi: 10.2106/JBJS.K.01558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cinotti G, Roysam GS, Eisenstein SM, Postacchini F. Ipsilateral recurrent lumbar disc herniation. J Bone Joint Surg Br. 1998;80:825–832. doi: 10.1302/0301-620x.80b5.8540. [DOI] [PubMed] [Google Scholar]