Abstract
We present an unusual case of haematogenous osteomyelitis in the diaphysis of the tibia of an adult leading to a subacute presentation with an extracortical abscess. Fluid from the abscess grew methicillin resistant Staphylococcus aureus (MRSA) on culture; MRSA with the same antibiogram had been grown from the patient’s blood seven years earlier following a bowel resection. Drainage of the abscess and curettage of the bone lesion together with appropriate antibiotic therapy led to resolution of the osteomyelitis.
Keywords: Osteomyelitis, Intracortical, Subperiosteal, Abscess
Osteomyelitis (bacterial infection of bone) occurs either as a result of direct inoculation of the bone following an open fracture or a surgical procedure exposing the bone to infection, or as a result of haematogenous spread. When affecting adults, the latter most commonly affects vertebrae. 1
The term ‘subacute’ has been used to apply to cases with symptoms lasting longer than two weeks; less commonly do patients present with a soft tissue abscess. We present an unusual case of a subacute presentation with a localised intracortical abscess in the distal diaphysis of the tibia of an adult, in association with an extracortical abscess.
Case history
A 31-year-old man presented with a 4-month history of pain, of spontaneous onset, in the left lower leg after exercise and at night. This worsened in the 48 hours prior to presentation, leading him to be unable to weight bear. He also developed numbness on the dorsum of the hallux. He was not taking any medication other than analgesics. There was a history of sepsis following a subtotal colectomy for ulcerative colitis seven years previously, at which time an unusual variant of methicillin resistant Staphylococcus aureus (MRSA) was grown from blood, the central venous pressure line tip, the abdominal wound and urine.
On examination, the patient had a temperature of 37.4°C and was tachycardic (ie heart rate >100bpm) but not hypotensive. An area of erythema (2cm × 1.5cm) was present on the anterior shin compatible with cellulitis. There was tenderness over the anterior and medial aspect of the tibia. The neighbouring fascial compartments were soft. Sensation was decreased in the deep peroneal nerve distribution (assessed using Semmes–Weinstein filament [5.07g; Kom Kare, Carlisle, OH, US]).
Blood tests revealed normal white cell (7.8 × 109/l) and neutrophil (5.8 × 109/l) counts and an elevated C-reactive protein level at 142mg/l. Blood cultures did not reveal any pathological growth. On the basis of the clinical examination and haematological tests, empirical antibiotics were started (intravenous benzylpenicillin and flucloxacillin).
The area of cellulitis improved slightly but the patient remained tachycardic and significantly febrile (>37.5°C). The pain intensified and was not controlled by opiate analgesics. It was exacerbated by active and passive ankle movement but the anterior and posterior compartments remained soft.
Radiological findings
Plain radiography revealed thickening of the lateral cortex of the distal diaphysis with central lucency (Fig 1). Ultrasonography of the left shin revealed no obvious fluid collection. Magnetic resonance imaging (MRI) (1.5T, Symphony Maestro Class; Siemens, Erlangen, Germany) was performed before and after the administration of contrast (Magnevist® 10ml; Bayer, Berlin, Germany). This revealed an intracortical fluid collection (high signal on STIR and proton density fat saturation, Figs 2 and 3) 143mm above the tibial plafond and a fluid collection (41mm × 43mm × 15mm, Fig 4) extending from the lateral aspect of the tibia round to its posterior aspect (high signal on STIR) with an enhancing margin on a T1 weighted image with fat saturation following gadolinium administration (Fig 5). (The posterior location of this fluid collection may explain why it was not detected by ultrasonography of the left shin.)
Figure 1.

Frontal radiography of left lower leg showing focal thickening of the lateral cortex of the tibial lower/mid diaphysis, with intracortical lucency
Figure 2.

Coronal STIR magnetic resonance imaging showing soft tissue and more subtle bone marrow high signal return of oedema and intracortical lesion of high fluid signal return
Figure 3.

Axial fat saturated proton density weighted magnetic resonance imaging showing high fluid signal return in intracortical lesion
Figure 4.

Coronal STIR magnetic resonance imaging showing fluid collection behind and adjacent to tibia
Figure 5.

T1 weighted, fat saturated, gadolinium enhanced, axial magnetic resonance imaging showing enhancing margin of the collection adjacent to the posterior, lateral and medial surfaces of the tibia
Surgical findings
These confirmed the radiological findings of a collection (Fig 6) and a small defect in the cortex with some associated stripping of the periosteum (Fig 7). The abscess collection was drained and the small defect in the cortex enlarged to permit debridement of the underlying intracortical abscess. Samples were sent for microbiological assessment, the wounds left open and closed 48 hours later.
Figure 6.
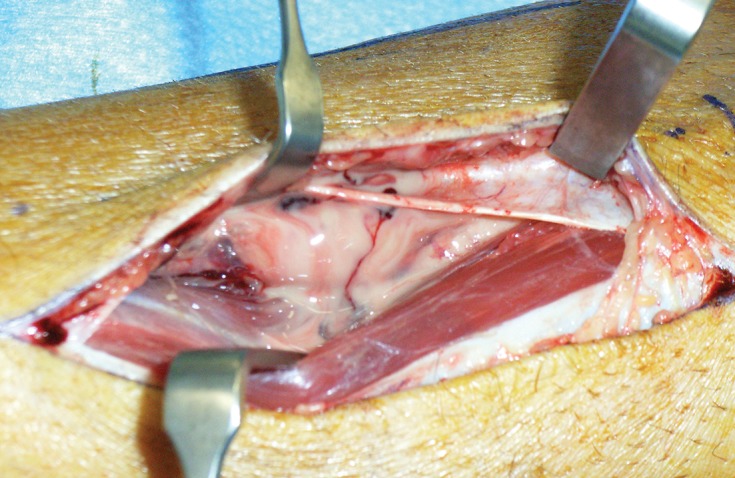
Photograph revealing collection entered and pus exposed between the tibialis anterior (retracted muscle) and the tibia
Figure 7.
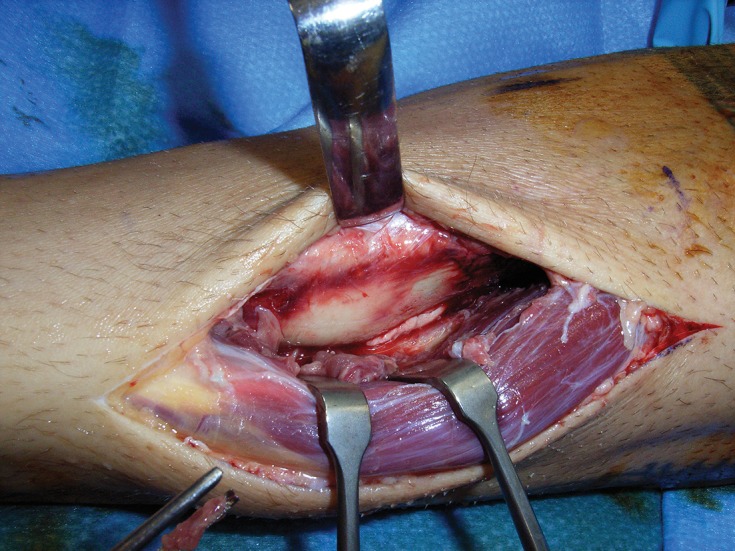
Photograph revealing the area shown in Figure 6 after the collection had been drained, a small defect in the cortex and a small area of stripped periosteum
Pathological findings
Fluid from the abscess and bone from the edge of the intracortical lesion grew MRSA (EMRSA-15). This was resistant to ciprofloxacin, penicillin and flucloxacillin but sensitive to erythromycin. Toxin testing for Panton–Valentine leucocidin was negative.
The patient was commenced on five days of intravenous vancomycin, followed by six weeks of oral clindamycin, on normalisation of inflammatory markers. At thee months, his symptoms had resolved completely.
Discussion
The clinical features of osteomyelitis include:
acute: systemic and local soft tissue signs of sepsis
subacute: pain and radiological signs of infection but little evidence of local or soft tissue signs
chronic: radiological changes, recurring episodes of local soft tissue infection and sinus formation 2
The nature of the presentation in this case (with the soft tissue signs, some systemic disturbance and significant pain, not relieved by opiates) was unusual. Stretching of the periosteum is a potential cause of this pain as this is known to be the most densely innervated tissue related to the skeleton. 5 Pressure on the neighbouring deep peroneal nerve could also lead to discomfort.
Subacute discrete osteomyelitis confined to the diaphysis of long bones is uncommon. 2 The radiological features when this does occur were described by Leveuf in relation to the pathological anatomy with intracortical abscess formation, spreading along Haversian canals leading to streaky loss of density on radiodiographs. 3 Confined intracortical osteomyelitis (ie no changes in the rest of the tibia) in adults, as demonstrated in this case, is very rare. We have only located one case in the literature, which was in the epiphysis/metaphysis junction. 4
EMRSA-15 is the most common healthcare associated epidemic strain of MRSA in the UK. This isolate differed from the more commonly isolated hospital strain in that it was susceptible to erythromycin. Although it was not possible to confirm by typing that the current isolate was identical to that isolated from the patient’s blood seven years previously, the distinctive antibiogram as well as the absence of MRSA from clinical cultures and screening samples in the intervening seven years suggest a haematological spread of the infection.
Conclusions
This case emphasises the usefulness of MRI in distinguishing a cortical bony lesion related to osteomyelitis from an osteoid osteoma, and confirms the importance of a full and detailed history.
References
- 1.Jensen AG, Espersen F, Skinhøj P, et al. Increasing frequency of vertebral osteomyelitis following Staphylococcus aureus bacteraemia in Denmark 1980–1990. J Infect. 1997;34:113–118. doi: 10.1016/s0163-4453(97)92395-1. [DOI] [PubMed] [Google Scholar]
- 2.Bulstrode CJ . Oxford: Oxford University Press; 2002. Oxford Textbook of Orthopaedics and Trauma. [Google Scholar]
- 3.Leveuf J. Treatment of osteomyelitis; anatomical and physiological basis. J Bone Joint Surg Br. 1948;30:207. [PubMed] [Google Scholar]
- 4.Strobel K, Hany TF, Exner GU. PET/CT of a Brodie abscess. Clin Nucl Med. 2006;31:210. doi: 10.1097/01.rlu.0000204125.79919.44. [DOI] [PubMed] [Google Scholar]
- 5.Mach DB, Rogers SD, Sabino MC, et al. Origins of skeletal pain: sensory and sympathetic innervation of the mouse femur. Neuroscience. 2002;113:155–166. doi: 10.1016/s0306-4522(02)00165-3. [DOI] [PubMed] [Google Scholar]


