Abstract
It is well established that angiosarcoma can develop following radiotherapy. We present an unusual case of angiosarcoma of the pharynx that developed three years after treatment with surgery and adjuvant chemoradiotherapy for a T2N2bM0 squamous cell carcinoma of the oropharynx. The patient was tumour free until developing dysphagia, which was found to be caused by an angiosarcoma. The patient underwent surgery of the pharyngeal angiosarcoma by laryngopharyngectomy, tongue base resection, selective neck dissection and radial forearm microvascular free flap reconstruction. Angiosarcoma following head and neck malignancy is rare but must be considered as part of the differential diagnosis in patients with new symptoms after radiotherapy.
Keywords: Squamous cell carcinoma, Angiosarcoma, Pharynx, Radiotherapy, Chemotherapy
Angiosarcomas of the head and neck region are rare tumours. Radiotherapy and lymphoedema are well established risk factors for angiosarcoma. 1 We present a case of angiosarcoma of the pharynx occurring approximately three years after curative multimodal treatment for a T2N2bM0 oropharyngeal squamous cell carcinoma with surgery and chemoradiotherapy. On reviewing the literature, we are not aware of any similar case of post-treatment pharyngeal angiosarcoma.
Case history
A 57-year-old man presented with a right neck lump in June 2008. Examination identified a 4cm cervical lymph node in level II and an enlarged right tonsil. Computed tomography (CT) confirmed this finding and excluded distant metastasis. Examination under anaesthesia revealed a mobile tumour confined clinically in the tonsil. Magnetic resonance imaging (MRI) suggested that the tumour did not extend beyond the tonsil but that level II neck nodes were involved. Histopathological analysis showed poorly differentiated squamous cell carcinoma (Fig 1).
Figure 1.

Initial squamous cell carcinoma: low power view (A, 40x magnification); haematoxylin and eosin staining (B, 100x magnification); and same area with immunostaining for pancytokeratin reacting with both tumour and benign surface epithelium (C, 100x magnification).
The patient was treated by a laser excision of the tonsillar tumour with a right modified radical neck dissection. Histopathological analysis of the specimen confirmed a right tonsillar squamous cell carcinoma 24mm in maximum diameter, with 18mm depth of invasion and four positive level II neck nodes. There was a positive superior margin and close margins of 1mm anteriorly, posteriorly and laterally.
Following a multidisciplinary meeting, the patient received concurrent adjuvant chemoradiotherapy. A total dose of 60Gy in 30 fractions over 39 days was administered to the tonsillar region and right neck field together with docetaxel, cisplatin and fluorouracil chemotherapy. Following his multimodal treatment, he remained tumour free under combined clinical and radiological surveillance.
In March 2011 the patient presented with slowly progressive dysphagia for solids. Fibreoptic nasendoscopy identified a slightly oedematous supraglottis. CT and MRI did not reveal any signs of recurrence. Consequently, a panendoscopy and biopsy was performed (Fig 2). A striking feature at pharyngoscopy was that of very bland, ‘glistening’ mucosa involving multiple sites in the hypopharynx, supraglottic larynx, tongue base and posterior wall of the oropharynx. There was no bulky submucosal disease apparent. Histopathological analysis of multiple biopsy sites confirmed mucosal angiosarcoma (Fig 3).
Figure 2.
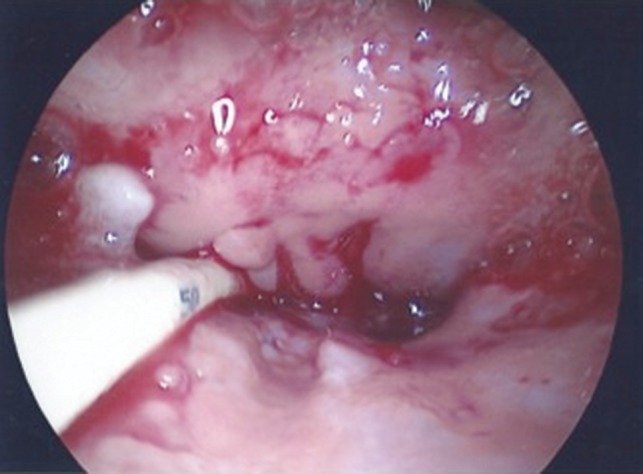
Endoscopic appearance of pharyngeal mucosal angiosarcoma. Nasogastric fine bore feeding tube inserted alongside.
Figure 3.
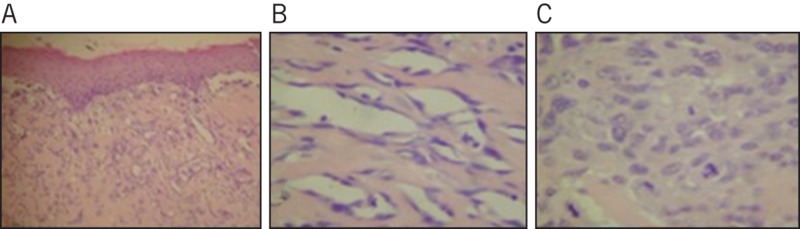
Histological analysis of pharyngeal angiosarcoma with haematoxylin and eosin staining. The presence of abnormal vascular spaces, atypical lining cells and abnormal mitotic figures confirm angiosarcoma: diffuse growth of abnormal vascular spaces (A, 40x magnification); angiosarcoma formation of vascular channels with abnormal lining cells (B, 200x magnification); and solid growth pattern of high grade angiosarcoma (C, 400x magnification).
Laser excision was unsuccessful in obtaining clearance of the tumour. Mapping biopsies demonstrated the tumour extending on to the anterior tongue, up the posterior pharyngeal wall to the level of the soft palate but not extending below the cricopharyngeus. Imaging showed no evidence of metastatic disease. Excision of the recurrent tumour was performed by total pharyngolaryngectomy, excision of tongue base, left selective neck dissection and reconstruction with a tubed radial forearm microvascular free flap. Despite a wide resection, tumour clearance was not obtained and the patient was managed with best supportive care. He died 12 months following diagnosis of the pharyngeal angiosarcoma owing to complications of local disease progression and metastatic disease.
Discussion
We present an unusual post-treatment case of mucosal pharyngeal angiosarcoma. A particular feature was that the angiosarcoma appeared to involve all of the irradiated mucosa with a clear demarcation (at least inferiorly) between normal and abnormal mucosa. Gradual onset of dysphagia was the first presenting symptom, with initial examination and imaging consistent with post-chemoradiotherapy changes. Intractable dysphagia following chemoradiotherapy for head and neck cancer is a well recognised complication of treatment. Recurrent squamous cell carcinoma may present with dysphagia but this will usually be with a more discrete lesion than in this case. The initial clinical appearances of this mucosal pharyngeal angiosarcoma were very similar to the typical post-chemoradiotherapy reaction. Only detailed histopathological analysis after examination under anaesthesia made the diagnosis possible.
To our knowledge, this is the first case of a pharyngeal angiosarcoma following treatment for a squamous carcinoma of the head and neck. An angiosarcoma is a rare malignant neoplasm of endothelial cells and comprises 1–2% of all soft tissue sarcomas. Its tissue of origin typically permits metastasis to distant sites. The exact pathogenesis remains unclear although previous radiotherapy and chronic lymphoedema are two well established risk factors. 1 The relative risk for developing an angiosarcoma is approximately six times higher after radiotherapy 2 and angiosarcomas in irradiated fields represent approximately 3–10% of all angiosarcomas. 3,4 Angiosarcoma following radiotherapy tends to occur within an eight-year window although it is a far more common finding in radiotherapy for breast cancer and lymphoma. 2
Owing to the rarity of the tumour, there are no large case series but the prognosis of head and neck mucosal angiosarcoma is poor. In a series of four intraoral angiosarcomas, none of the patients survived beyond six months from the original diagnosis due to local disease progression or lung metastasis. 5
Conclusions
Although this is a rare tumour, the lesson we have learnt is that dysphagia following treatment is not always due to recurrent squamous cell carcinoma or treatment induced fibrosis. The implications for this in our practice may necessitate a lower threshold for examination under anaesthesia and biopsy following treatment.
References
- 1.Penel N, Marréaud S, Robin YM, Hohenberger P. Angiosarcoma: state of the art and perspectives. Crit Rev Oncol Hematol. 2011;80:257–263. doi: 10.1016/j.critrevonc.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 2.Virtanen A, Pukkala VE, Auvinen A. Angiosarcoma after radiotherapy: a cohort study of 332,163 Finnish cancer patients. Br J Cancer. 2007;97:115–117. doi: 10.1038/sj.bjc.6603805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fury MG, Antonescu CR, Van Zee KJ, et al. A 14-year retrospective review of angiosarcoma: clinical characteristics, prognostic factors, and treatment outcomes with surgery and chemotherapy. Cancer J. 2005;11:241–247. doi: 10.1097/00130404-200505000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Fayette J, Martin E, Piperno-Neumann S, et al. Angiosarcomas, a heterogeneous group of sarcomas with specific behavior depending on primary site: a retrospective study of 161 cases. Ann Oncol. 2007;18:2030–2036. doi: 10.1093/annonc/mdm381. [DOI] [PubMed] [Google Scholar]
- 5.Favia G, Lo Muzio L, Serpico R, Maiorano E. Angiosarcoma of the head and neck with intra-oral presentation. A clinico-pathological study of four cases. Oral Oncol. 2002;38:757–762. doi: 10.1016/s1368-8375(02)00045-3. [DOI] [PubMed] [Google Scholar]


