ABSTRACT
The safety and efficacy of the live-attenuated Japanese encephalitis virus (JEV) SA14-14-2 vaccine are attributed to mutations that accumulated in the viral genome during its derivation. However, little is known about the contribution that is made by most of these mutations to virulence attenuation and vaccine immunogenicity. Here, we generated recombinant JEV (rJEV) strains containing JEV SA14-14-2 vaccine-specific mutations that are located in the untranslated regions (UTRs) and seven protein genes or are introduced from PCR-amplified regions of the JEV SA14-14-2 genome. The resulting mutant viruses were evaluated in tissue culture and in mice. The authentic JEV SA14-14-2 (E) protein, with amino acid substitutions L107F, E138K, I176V, T177A, E244G, Q264H, K279M, A315V, S366A, and K439R relative to the wild-type rJEV clone, was essential and sufficient for complete attenuation of neurovirulence. Individually, the nucleotide substitution T39A in the 5′ UTR (5′-UTR-T39A), the capsid (C) protein amino acid substitution L66S (C-L66S), and the complete NS1/2A genome region containing 10 mutations each significantly reduced virus neuroinvasion but not neurovirulence. The levels of peripheral virulence attenuation imposed by the 5′-UTR-T39A and C-L66S mutations, individually, were somewhat mitigated in combination with other vaccine strain-specific mutations, which might be compensatory, and together did not affect immunogenicity. However, a marked reduction in immunogenicity was observed with the addition of the NS1/2A and NS5 vaccine virus genome regions. These results suggest that a second-generation recombinant vaccine can be rationally engineered to maximize levels of immunogenicity without compromising safety.
IMPORTANCE The live-attenuated JEV SA14-14-2 vaccine has been vital for controlling the incidence of disease caused by JEV, particularly in rural areas of Asia where it is endemic. The vaccine was developed >25 years ago by passaging wild-type JEV strain SA14 in tissue cultures and rodents, with intermittent tissue culture plaque purifications, to produce a virus clone that had adequate levels of attenuation and immunogenicity. The vaccine and parent virus sequences were later compared, and mutations were identified throughout the vaccine virus genome, but their contributions to attenuation were never fully elucidated. Here, using reverse genetics, we comprehensively defined the impact of JEV SA14-14-2 mutations on attenuation of virulence and immunogenicity in mice. These results are relevant for quality control of new lots of the current live-attenuated vaccine and provide insight for the rational design of second-generation, live-attenuated, recombinant JEV vaccine candidates.
INTRODUCTION
Japanese encephalitis virus (JEV) is transmitted in an enzootic cycle between Culex mosquitoes and aquatic birds or domestic pigs and is the leading cause of viral encephalitis in Asia, with >60,000 cases estimated to occur annually (1–4). In areas where the disease is endemic, children are at high risk for disease (5), but all age groups lacking adequate levels of immunity are susceptible to infection, and this is a major concern as the virus continues to expand its geographic range (3). JEV is a member of the genus Flavivirus and has a single-strand, plus-sense RNA genome that is nearly 11 kb in length. The viral genome contains a single open reading frame (ORF) that codes for a polyprotein and is flanked by 5′ and 3′ untranslated regions (UTRs) that are important for virus replication (6). The long viral polyprotein is processed by viral and host cellular proteases into three structural proteins (capsid [C], precursor membrane [prM], and envelope [E]) and at least seven nonstructural proteins (NS1, NS2A, NS2B, NS3, NS4A, NS4B, and NS5) (7). The structural proteins make up the virion, where the C protein binds viral RNA, the prM protein prevents premature viral membrane fusion, and the E protein is responsible for cell binding and entry (8). The nonstructural proteins are produced in infected cells and have multiple functions during the virus life cycle, including virus replication and host immune evasion (7, 9, 10).
Japanese encephalitis is a vaccine-preventable disease, and inactivated vaccines have been available for human use for >50 years (11–13). In developing countries, the use of inactivated vaccines is limited by their relatively high cost and the need for multiple doses in order to achieve adequate levels of immunity (13, 14). In 1988, China's National Institute for the Control of Pharmaceutical and Biological Products approved the use of a novel live-attenuated JEV vaccine (SA14-14-2) produced in primary hamster kidney (PHK) cells (Chengdu Institute of Biological Products). This live-attenuated vaccine gradually replaced the inactivated vaccines used previously in China due to its excellent level of safety and efficacy (12, 15). The JEV SA14-14-2 vaccine has more recently become available in Cambodia, India, South Korea, Laos, Myanmar, Nepal, Sri Lanka, and Thailand, and it has been administered to millions of children, with no reported serious adverse events (12, 16–21). The World Health Organization prequalified the production of the JEV SA14-14-2 vaccine in 2013, which should facilitate its expanded distribution in additional countries.
The live-attenuated JEV SA14-14-2 vaccine strain was derived from wild-type (WT) JEV strain SA14, which was originally isolated from mosquito larvae by several passages in suckling mouse brain (15). The SA14 parent virus strain was passaged 100 times in PHK cells, followed by plaque purifications in primary chicken embryo cells, peripheral passages in mice and hamsters, and additional plaque purifications to generate the stably attenuated and immunogenic SA14-14-2 strain (15). The attenuated phenotype of JEV SA14-14-2 is attributed to a multitude of mutations that accumulated throughout the viral genome during its derivation and have been identified by several different groups that compared the sequence of JEV SA14-14-2 to that of its WT parent virus (15, 22–25). However, the genetic determinants responsible for attenuation of the JEV SA14-14-2 vaccine strain have not been fully elucidated.
A constellation of mutations found in the E protein is considered to be the primary genetic determinant of attenuation of the JEV SA14-14-2 vaccine strain (15), and this assertion is based largely on a study demonstrating that multiple mutations in the E protein are critical for attenuation of neurovirulence for a recombinant, chimeric JEV/yellow fever virus (YFV) 17D vaccine candidate (ChimeriVax-JE) (26). More recent studies support this conclusion and have demonstrated that passage of JEV SA14-14-2 in mouse brain results in amino acid substitutions in the E protein that produce a neurovirulent phenotype (27, 28). However, a recombinant WT JEV Nakayama clone containing prM-E or 5′-UTR-C-prM-E of the JEV SA14-14-2 vaccine strain produced viruses with similar or moderately lower levels of neurovirulence than that of the WT parent virus (29), suggesting that mutations in other regions of the virus genome also contribute to attenuation. One recent study demonstrated that a nucleotide substitution in the JEV SA14-14-2 NS2A gene ablates the formation of NS1′, an elongated form of NS1 produced by a translation frameshift, and confers an attenuation phenotype on WT recombinant JEV (30). The contribution of other JEV SA14-14-2 nonstructural protein mutations to attenuation of virulence has not been evaluated.
The goal of the current study was to comprehensively define the genetic determinants of attenuation of the JEV SA14-14-2 vaccine strain. This was accomplished by introducing vaccine strain-specific mutations or PCR-amplified regions of the vaccine virus genome into a recombinant WT JEV clone. The resulting recombinant JEV (rJEV) mutants were evaluated in vitro and in vivo, revealing that mutations found in multiple regions of the JEV SA14-14-2 genome contribute to its tissue culture phenotype, attenuation, and immunogenicity in mice.
MATERIALS AND METHODS
Cells.
Vero (African green monkey kidney) cells were maintained at 37°C in OptiPRO SFM (serum-free medium) (Gibco) supplemented with 4 mM l-glutamine (Gibco). C6/36 (Aedes albopictus mosquito) cells were maintained at 32°C in Eagle's minimum essential medium (EMEM) (Lonza) supplemented with 10% fetal bovine serum (FBS) (HyClone), 2 mM l-glutamine, and 0.1 mM nonessential amino acids solution (NEAA) (Gibco). HEK-293T (human kidney) cells were maintained at 37°C in EMEM supplemented with 10% FBS, 2 mM l-glutamine, and 100 U/ml penicillin-streptomycin (Gibco). Raji (human B-cell lymphoblast) cells were maintained at 37°C in RPMI 1640 medium supplemented with 10% FBS, 2 mM l-glutamine, and 100 U/ml penicillin-streptomycin.
Viruses.
The rJEV India/78 (genotype III strain 7812474) and rJEV mutant strain 14-14-2 (rJEVmut14-14-2) stocks were derived from cDNA clones that were described previously (31, 32). Our JEV SA14-14-2 laboratory strain was passaged once in Vero cells to obtain a working stock that was characterized in a previous study (32).
Construction and recovery of rJEV mutants.
Synthesized cDNA gene regions encoding point mutations were inserted as cloned fragments into plasmid pJEV India/78 (Fig. 1), which was described previously (31). The T39A (5′-UTR) and T292C (C-L66S amino acid change) nucleotide mutations were inserted as AscI-BstBI cDNA fragments. The C1296T, G1389A, A1503G, A1506G, G1769T, and A1813T nucleotide mutations (E-L107F, -E138K, -I176V, -T177A, -Q264H, and -K279M amino acid substitutions, respectively) were inserted as an XbaI-SacI cDNA fragment. The G3528C nucleotide mutation (NS1-D351H amino acid mutation) was inserted as an MfeI-FseI cDNA fragment. The G4403T (NS2B-E63D), A4408G (NS2B-D65G amino acid mutation), A4782G (NS3-M59V amino acid mutation), and C4921G/T4922C (NS3-A105G amino acid mutation) nucleotide mutations were inserted as an FseI-StuI cDNA fragment. The A7227G nucleotide mutation (NS4B-I106V amino acid change) was inserted as a BclI-XmaI cDNA fragment. The C8832T (NS5-H386Y amino acid change), T9688C (NS5-V671A amino acid change), and T10428C (3′-UTR) nucleotide mutations were inserted as MluI-HpaI cDNA fragments. PCR-amplified cDNA fragments of the E, NS1, NS2A, and NS5 genes of JEV SA14-14-2 were also introduced into pJEV India/78 as described previously (32) (Fig. 1). Recovery of the mutant viruses from in vitro transcripts and by transfection in Vero or C6/36 cells was performed as described previously (31, 32). The recovered viruses were biologically cloned by multiple terminal endpoint dilutions and subsequently amplified in Vero cells prior to sequence analysis.
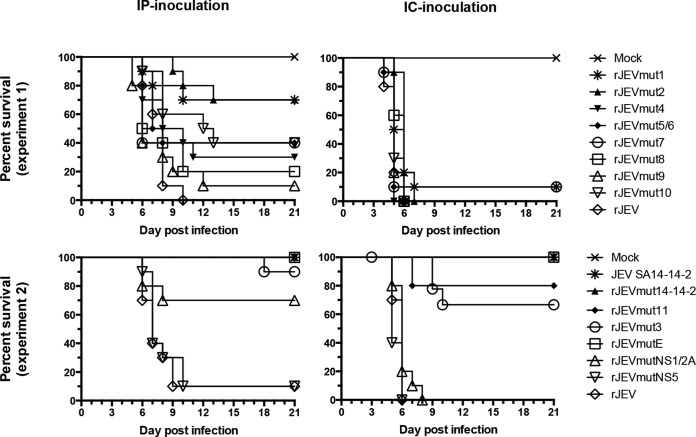
FIG 1.
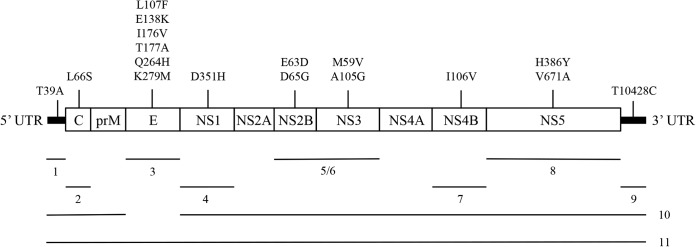
Diagram of rJEV mutants. JEV SA14-14-2 vaccine strain-specific nucleotide substitutions in the UTR and amino acid substitutions in proteins that were introduced into the wild-type rJEV clone are indicated above the molecule. Multiple mutations in the same gene region were introduced together for that region. Regions that were incorporated into rJEV to generate mutants 1 to 11 are indicated below the molecule. Regions 5 and 6 were combined to generate rJEVmut5/6, as all four mutations are located in the NS2B/3 viral protease. Mutant virus 10 contains all of the vaccine strain-specific mutations except for those found in the E protein, and mutant virus 11 contains the entire set of mutations.
Virus replication in Vero cells.
Vero cells were infected with viruses at a multiplicity of infection (MOI) of 0.01 PFU/cell for 1 h and washed twice with phosphate-buffered saline (PBS) (Gibco), followed by the addition of medium. At 3 days postinfection, the medium was harvested, and the virus titer was determined in Vero cells. Plaques were visualized on day 3 by immunostaining, and plaque size was measured.
Mouse studies.
Studies in mice were performed in accordance with the regulations and guidelines of the NIH (Bethesda, MD) and approved by the Animal Care and Use Committee of the NIAID. Viruses were tested for neuroinvasiveness by intraperitoneal (i.p.) inoculation and for neurovirulence by intracerebral (i.c.) inoculation of 3-week-old, weanling, female Swiss Webster mice (Taconic). Groups of 6 or 10 mice were inoculated with a 0.1-ml dose of virus i.p. or a 0.01-ml dose of virus i.c. and monitored for 21 days for signs of encephalitis, which included tremors, seizure, and paralysis. Moribund mice were humanely euthanized to minimize pain and distress. The 50% lethal dose (LD50) values were determined by the method of Reed and Muench (39). Serum was collected from i.p. inoculated mice on study day 21 for neutralization assays.
Production of JEV reporter virus particles.
JEV SA14-14-2 reporter virus particles (RVPs) expressing green fluorescent protein (GFP) were produced in HEK-293T cells, as described previously (32). RVP titers were determined by serial dilution of JEV RVP stocks and infection of Raji cells in 96-well plates. Following 2 days of incubation, the cells were fixed with paraformaldehyde, and the percentage of GFP-expressing cells was determined by flow cytometry.
JEV RVP serum neutralization assay.
The JEV RVP serum neutralization assay was carried out as described previously (31). The data were analyzed by using GraphPad Prism (GraphPad Software, La Jolla, CA) and were fit by a dose-response curve (variable slope) in order to determine the 50% effective neutralization concentration (EC50). Titers are reported as the reciprocal geometric mean EC50 titer (GMT). Seroconversion was indicated for mice with a detectable neutralizing antibody EC50 titer (≥8).
Statistical analysis.
Statistical analyses were performed by using GraphPad Prism. Virus titers were analyzed by using one-way analysis of variance (ANOVA) with Dunnett's test, and a P value of <0.05 was required for significance. Mouse survival analyses were done by using a log rank (Mantel-Cox) test, and a P value of <0.05 was required for significance.
RESULTS
Identification of vaccine strain-specific mutations.
The complete genome sequences contained in GenBank for WT JEV strain SA14 (GenBank accession no. M55506, D90194, and U14163) and vaccine strain JEV SA14-14-2 (accession no. AF315119, D90195, and JN604986) were compared in order to identify nucleotides and amino acids that consistently differed between these viruses. A similar analysis was reported previously by Song and colleagues (33) and yielded results identical to those of our analysis. Table 1 lists only mutations that were consistently found to distinguish the vaccine strain from its WT parent virus. In total, 17 JEV SA14-14-2 vaccine strain-specific mutations were identified. The 5′ and 3′ UTRs each contained a single nucleotide difference, and amino acid differences were identified in the C, E, NS1, NS2B, NS3, NS4B, and NS5 proteins. However, consistent differences were not identified in the prM, NS2A, or NS4A protein. The E protein contained the greatest number of differences, with six amino acid substitutions. The NS2B/3 viral protease had four amino acid differences, while the remaining proteins each had one or two amino acid substitutions.
TABLE 1.
Nucleotide and amino acid residues that are consistently different between consensus genome sequences of the JEV SA14-14-2 vaccine strain and the wild-type JEV SA14 parent virus strain
| Nucleotide position(s) | Region or gene | Amino acid position | Nucleotide or amino acid in JEV strain |
|
|---|---|---|---|---|
| SA14a | SA14-14-2b | |||
| 39 | 5′ UTR | None | T | A |
| 292 | C | 66 | Leu | Ser |
| 1296 | E | 107 | Leu | Phe |
| 1389 | E | 138 | Glu | Lys |
| 1503 | E | 176 | Ile | Val |
| 1506 | E | 177 | Thr | Ala |
| 1769 | E | 264 | Gln | His |
| 1813 | E | 279 | Lys | Met |
| 3528 | NS1 | 351 | Asp | His |
| 4403 | NS2B | 63 | Glu | Asp |
| 4408 | NS2B | 65 | Asp | Gly |
| 4782 | NS3 | 59 | Met | Val |
| 4921 + 4922 | NS3 | 105 | Ala | Gly |
| 7227 | NS4B | 106 | Ile | Val |
| 8832 | NS5 | 386 | His | Tyr |
| 9688 | NS5 | 671 | Val | Ala |
| 10428 | 3′ UTR | None | T | C |
Recovery of recombinant JEV mutants.
The WT rJEV India/78 clone was used as the basis for these reverse-genetics studies because it demonstrates a high level of virulence in weanling mice and allowed us to evaluate the phenotype produced by SA14 parent and vaccine-specific mutations. The JEV SA14-14-2 vaccine strain-specific mutations listed in Table 1 were introduced as point mutations into the cDNA of WT rJEV India/78 to generate rJEV mutant 1 (rJEVmut1) to rJEVmut9 (Fig. 1). rJEV mutant 5/6 combined mutations found in both NS2B and NS3, as they are located in the viral protease. rJEV mutant 10 contained the 11 mutations identified outside the E protein gene, while rJEVmut11 contained all 17 mutations that were specific for JEV SA14-14-2 (Fig. 1). Regions of the JEV SA14-14-2 genome that encoded amino acid residues different from those of WT rJEV India/78, which were not identified as being vaccine strain specific and are likely part of the genetic background of the WT vaccine parent strain JEV SA14, included only E, NS1, NS2A, and NS5. Each of these regions was PCR amplified from JEV SA14-14-2 and used to generate rJEV mutants (Table 2). The rJEV E and NS1/2A mutants each contained 10 mutations compared to WT rJEV India/78, while rJEVmutNS5 had 4 mutations compared to rJEV India/78 (Table 2). rJEV mutant strain 14-14-2 contained the JEV SA14-14-2 PCR-amplified E, NS1/2A, and NS5 gene regions introduced together into the cDNA plasmid of rJEVmut11 and also included one nucleotide change in each UTR and the G3599A nucleotide change in NS2A that ablates NS1′ formation (30). In total, rJEVmut14-14-2 contains 32 mutations relative to rJEV India/78 and comprises 29 amino acid substitutions distributed throughout eight viral proteins (Table 2). All rJEV mutants were recovered in either C6/36 or Vero cells, biologically cloned in Vero cells, and sequenced. Several rJEV mutants contained adventitious silent nucleotide changes, including rJEVmut3 (T1715C and G6575T), rJEVmut5/6 (A1073T, C2567T, and T3431C), rJEVmut7 (G8054A), rJEVmut9 (T5613C, C9500A, and A9602G), rJEVmut10 (T3530C), rJEVmut11 (A3044G and T8747C), rJEVmutE (T2430C and C2963A), and rJEVmutNS1/2A (C1691A). The sequences of rJEV mutants 1, 2, 4, 8, NS5, and 14-14-2 matched their cDNA clones.
TABLE 2.
Recombinant JEV mutants bearing PCR-amplified segments of the JEV SA14-14-2 genome
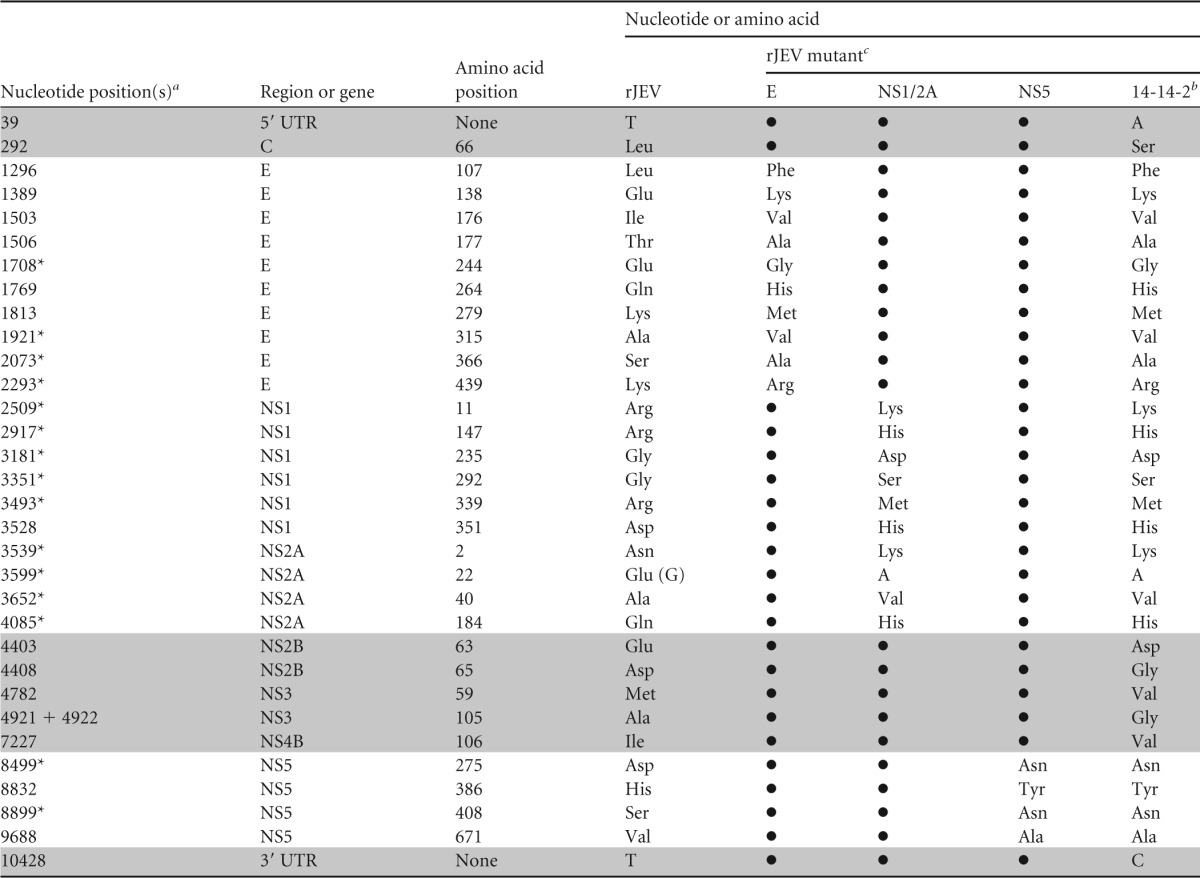
Mutations at nucleotides indicated with an asterisk were not identified as vaccine strain specific and probably represent differences in the genetic backgrounds of the JEV SA14 and rJEV India/78 wild-type strains.
JEV SA14-14-2 PCR-amplified E, NS1/2A, and NS5 gene regions were cloned into the cDNA plasmid of rJEVmut11, which already contained mutations at nucleotides 39, 292, 4403 to 7227, and 10428 (shaded gray), to generate rJEV mutant 14-14-2 (32).
Bullets indicate that the nucleotide or amino acid is the same as that for rJEV.
Phenotype in Vero cells.
The plaque sizes and peak virus titers of the rJEV mutants were measured in Vero cells and compared to those of WT rJEV and the JEV SA14-14-2 laboratory strain. Most of the rJEV mutants had a large plaque size (>2 mm) and mean peak virus titers that were similar to those of WT rJEV, and therefore, many JEV SA14-14-2 mutations do not individually produce a tissue culture phenotype (Table 3). rJEV mutants 2, 3, 10, and E had medium plaque sizes (1 to 2 mm) and significantly lower mean peak virus titers than those of WT rJEV (Table 3). The phenotype of rJEV mutants 2 and 10 or mutants 3 and E were indistinguishable from one another in Vero cells. This indicates that the C-L66S mutation (rJEVmut2 and -10) and at least one of six vaccine strain-specific E protein mutations (rJEVmut3 and -E) were responsible for the observed reductions in plaque size and replicative fitness compared to WT rJEV. Recombinant JEV mutants 11 and 14-14-2 had small plaque sizes (<1 mm), like the JEV SA14-14-2 laboratory strain, and significantly lower mean peak virus titers than those of WT rJEV (Table 3). Thus, the reduction in peak virus titer and small plaque size compared to most WT JEV strains, which are characteristics of JEV SA14-14-2 in tissue culture, are apparently produced by a combination of vaccine strain-specific mutations in multiple genes or UTRs.
TABLE 3.
Phenotype of rJEV mutants in Vero cells
| Virus | Plaque sizea | Mean peak titer (log10 PFU/ml) ± SDb |
|---|---|---|
| rJEV | Large | 8.0 ± 0.3 |
| rJEVmut1 | Large | 7.8 ± 0.4 |
| rJEVmut2 | Medium | 6.7 ± 0.4c |
| rJEVmut3 | Medium | 7.3 ± 0.1c |
| rJEVmut4 | Large | 7.8 ± 0.3 |
| rJEVmut5/6 | Large | 8.1 ± 0.1 |
| rJEVmut7 | Large | 7.8 ± 0.3 |
| rJEVmut8 | Large | 7.8 ± 0.4 |
| rJEVmut9 | Large | 8.0 ± 0.2 |
| rJEVmut10 | Medium | 6.6 ± 0.5c |
| rJEVmut11 | Small | 6.4 ± 0.5c |
| rJEVmutE | Medium | 7.3 ± 0.1c |
| rJEVmutNS1/2A | Large | 7.5 ± 0.2 |
| rJEVmutNS5 | Large | 8.0 ± 0.1 |
| rJEVmut14-14-2 | Small | 6.0 ± 0.4c |
| JEV SA14-14-2 | Small | 7.1 ± 0.3c |
Measured at 3 days postinfection, where small indicates a plaque size of <1 mm, medium indicates a plaque size of 1 to 2 mm, and large indicates a plaque size of >2 mm.
Data were from at least two duplicate experiments per virus.
Significantly different from rJEV by ANOVA with Dunnett's test (P < 0.05).
Virulence phenotype in weanling mice.
Wild-type rJEV and most of the rJEV mutants were screened for virulence in mice by using a dose of 104 PFU i.p. and a dose of 102 PFU i.c. (Table 4 and Fig. 2). JEV SA14-14-2 and rJEVmut14-14-2 were inoculated at a dose of 104 PFU i.p. and i.c. When inoculated by the i.p. route, WT rJEV caused 100% and 90% mortality (95% average) in experiments 1 and 2 and mice had 8- and 7-day (7.5-day average) median survival times, respectively. Mice inoculated i.p. with rJEV mutants 5/6, 7, 8, 9, and NS5 had moderately increased survival (10 to 40%) in comparison, but the survival curves were not significantly different from that for WT rJEV. Thus, NS2B/3, NS4B, NS5, and 3′-UTR vaccine strain-specific mutations, along with mutations in the vaccine virus NS5 genome region, made little or no contribution to attenuation of virus neuroinvasion. In contrast, mice inoculated by the i.p. route with rJEV mutants 1, 2, 3, 10, and NS1/2A had considerably higher rates of survival, 40 to 90%, and the survival curves for these viruses were significantly different from that for WT rJEV. Notably, the nucleotide substitution T39A in the 5′ UTR (rJEVmut1) and the amino acid substitution L66S in the C protein (rJEVmut2) each substantially reduced virus neuroinvasion, with 70% of mice surviving i.p. inoculation. rJEV mutant 10, which contained 11 vaccine strain-specific mutations, including 5′-UTR-T39A and C-L66S, but lacked mutations in E, appeared to be less attenuated, with only 40% of mice surviving i.p. inoculation. However, the mouse survival curves for rJEV mutants 1 and 2 were not significantly different from that of rJEVmut10 (by a log rank test). rJEV mutant 3, which contained the six vaccine strain-specific E protein mutations, demonstrated a significant amount of attenuation but had some residual virulence, with 1 of 10 mice developing signs of encephalitis leading to a moribund state on day 18 following i.p. inoculation. rJEV mutants E, 11, and 14-14-2 behaved like the JEV SA14-14-2 laboratory strain, with i.p. inoculation of mice resulting in no mortality or signs of encephalitis.
TABLE 4.
Virulence screening of rJEV mutants and control viruses in weanling mice
| Virus | i.p. inoculation |
i.c. inoculation |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Dose (PFU) | No. of alive mice/total no. of mice | % survival | Median survival time (days) | Significant difference from rJEVa | Dose (PFU) | No. of alive mice/total no. of mice | % survival | Median survival time (days) | Significant difference from rJEVa | |
| rJEVb | 104 | 1/20 | 5 | 7.5 | NA | 102 | 0/20 | 0 | 5.5 | NA |
| rJEVmut1 | 104 | 7/10 | 70 | >21 | Yes | 102 | 1/10 | 10 | 5.5 | No |
| rJEVmut2 | 104 | 7/10 | 70 | >21 | Yes | 102 | 0/10 | 0 | 6 | Yes |
| rJEVmut3 | 104 | 9/10 | 90 | >21 | Yes | 102 | 6/9c | 67 | >21 | Yes |
| rJEVmut4 | 104 | 3/10 | 30 | 9 | No | 102 | 0/10 | 0 | 5 | No |
| rJEVmut5/6 | 104 | 4/10 | 40 | 7.5 | No | 102 | 0/10 | 0 | 5 | No |
| rJEVmut7 | 104 | 4/10 | 40 | 6 | No | 102 | 1/10 | 10 | 5 | No |
| rJEVmut8 | 104 | 2/10 | 20 | 7 | No | 102 | 0/10 | 0 | 6 | Yes |
| rJEVmut9 | 104 | 1/10 | 10 | 6 | No | 102 | 0/10 | 0 | 5 | No |
| rJEVmut10 | 104 | 4/10 | 40 | 12.5 | Yes | 102 | 0/10 | 0 | 5 | No |
| rJEVmut11 | 104 | 10/10 | 100 | >21 | Yes | 102 | 8/10 | 80 | >21 | Yes |
| rJEVmutE | 104 | 10/10 | 100 | >21 | Yes | 102 | 10/10 | 100 | >21 | Yes |
| rJEVmutNS1/2A | 104 | 7/10 | 70 | >21 | Yes | 102 | 0/10 | 0 | 6 | No |
| rJEVmutNS5 | 104 | 1/10 | 10 | 7 | No | 102 | 0/10 | 0 | 5 | No |
| rJEVmut14-14-2 | 104 | 10/10 | 100 | >21 | Yes | 104 | 10/10 | 100 | >21 | Yes |
| JEV SA14-14-2 | 104 | 10/10 | 100 | >21 | Yes | 104 | 10/10 | 100 | >21 | Yes |
| Mockb | NAd | 20/20 | 100 | >21 | Yes | NA | 20/20 | 100 | >21 | Yes |
Determined by the log rank test, with a P value of <0.05 being required for significance.
Results from two different experiments were combined.
One mouse died from trauma at the injection site.
NA, not applicable.
FIG 2.
Survival of weanling mice inoculated with rJEV mutants and control viruses. Groups of 10 mice were inoculated with virus or mock infected and monitored for 21 days for signs of encephalitis. All viruses were inoculated at a dose of 104 PFU i.p. Most viruses were screened at a dose of 102 PFU i.c., except for rJEVmut14-14-2 and JEV SA14-14-2, which were tested at a dose of 104 PFU i.c. Experiments 1 and 2 were performed independently, and a statistical comparison with wild-type rJEV is shown in Table 4.
For mice inoculated by the i.c. route (Table 4 and Fig. 2), WT rJEV caused 100% mortality, and mice had 5- and 6-day (5.5-day average) median survival times for experiments 1 and 2, respectively. Mice inoculated with rJEV mutants 4, 5/6, 9, 10, NS1/2A, and NS5 had 100% mortality, and the survival curves were not significantly different from that for WT rJEV. Mice inoculated with rJEV mutants 2 and 8 had 100% mortality and very modest but significantly longer 6-day median survival times than mice inoculated with WT rJEV in experiment 1, whereas mice inoculated by the i.c. route with rJEV mutants 1 and 7 had a moderately 10% increased survival rate and 5- to 5.5-day median survival times and were not significantly different from mice inoculated with WT rJEV. Only the rJEV mutants that contained JEV SA14-14-2 E protein amino acid substitutions (rJEVmut3, -11, -E, and -14-14-2) had substantial levels of neurovirulence attenuation. Mice inoculated with rJEV mutants 3 and 11 had 67% and 80% survival rates, respectively, and the survival curves were significantly different from that for WT rJEV but not from each other. Mice inoculated i.c. with rJEV mutants E and 14-14-2 behaved like the JEV SA14-14-2 laboratory strain, causing no mortality or signs of encephalitis.
The i.c. LD50 values in weanling mice were determined for rJEV mutants that caused incomplete or no mortality by the i.c. route in the initial virulence screening (Table 5). Mice inoculated with rJEV mutants 1 and 7 had i.c. LD50 values of <1 PFU, like WT rJEV, and were not attenuated for neurovirulence. Only rJEV mutants bearing JEV SA14-14-2 E protein mutations were attenuated for neurovirulence. Mice inoculated with rJEV mutants 3 and 11 had similar i.c. LD50 values, which were >1,000-fold higher than the LD50 of WT rJEV, but still possessed a residual level of neurovirulence, whereas mice inoculated with rJEVmutE had an i.c. LD50 value of >10,000 PFU, causing no mortality at this dose, similar to rJEVmut14-14-2. The six mice inoculated with rJEVmutE at a dose of 104 PFU i.c. became scruffy and mildly lethargic on day 6, but no other clinical signs were apparent, and they resolved within 24 h, whereas mice inoculated with the same dose of rJEVmut14-14-2 did not show any clinical signs, and this is probably the contribution of attenuating mutations located in regions of the genome outside the E protein gene.
TABLE 5.
Neurovirulence (i.c. LD50) of rJEV mutants in weanling mice
| Virus | Dose (PFU) | No. of alive mice/total no. of mice | Median survival time (days) | LD50 (PFU) |
|---|---|---|---|---|
| rJEVmut14-14-2 | 104 | 6/6 | >21 | >10,000 |
| rJEVmutE | 104 | 6/6 | >21 | >10,000 |
| 103 | 6/6 | >21 | ||
| 102 | 6/6 | >21 | ||
| rJEVmut11 | 104 | 2/6 | 8.5 | 3,162 |
| 103 | 4/6 | >21 | ||
| 102 | 6/6 | >21 | ||
| 101 | 6/6 | >21 | ||
| rJEVmut3 | 104 | 1/6 | 7 | 1,995 |
| 103 | 5/6 | >21 | ||
| 102 | 4/6 | >21 | ||
| 101 | 6/6 | >21 | ||
| rJEVmut1 | 102 | 0/6 | 6 | 0.3 |
| 101 | 1/6 | 8.5 | ||
| 100 | 3/6 | 15.5 | ||
| 10−1 | 5/6 | >21 | ||
| rJEVmut7 | 102 | 0/6 | 5.5 | 0.3 |
| 101 | 0/6 | 6 | ||
| 100 | 1/6 | 6.5 | ||
| 10−1 | 5/6 | >21 | ||
| rJEV | 102 | 0/6 | 6 | 0.7 |
| 101 | 0/6 | 6.5 | ||
| 100 | 3/6 | 17 | ||
| 10−1 | 5/6 | >21 | ||
| Mock | NAa | 6/6 | >21 | NA |
NA, not applicable.
Immunogenicity in weanling mice.
Immunogenicity was evaluated for rJEV mutants that had substantial levels of neurovirulence attenuation (Table 6). Mice immunized with 104 PFU of the JEV SA14-14-2 laboratory strain had 100% seroconversion and a neutralizing antibody GMT of 473. In comparison, rJEVmut14-14-2 administered at the same dose was moderately less immunogenic, with only 70% seroconversion and a neutralizing antibody GMT of 247. rJEVmutE produced 100% seroconversion and a neutralizing antibody GMT that was ∼4-fold higher than that of the JEV SA14-14-2 laboratory strain and 8-fold higher than that of rJEVmut14-14-2 (Table 6). This indicates that mutations located in regions of the virus genome outside the E protein gene moderately reduce immunogenicity. However, underattenuated rJEV mutants 3 and 11 had similar, high levels of immunogenicity, producing 100% seroconversion and neutralizing antibody GMTs <2-fold different from that of rJEVmutE (Table 6). Therefore, the combination of vaccine strain-specific mutations apparently did not affect levels of immunogenicity, suggesting that additional mutations in the JEV SA14-14-2 NS1/2A or NS5 genome region contribute to the reduced immunogenicity of rJEVmut14-14-2.
TABLE 6.
Immunogenicity of rJEV mutants in weanling mice inoculated by the i.p. route
| Virus | Dose (PFU) | No. of mice with seroconversion/total no. of mice | Neutralizing antibody titera (reciprocal EC50) |
|
|---|---|---|---|---|
| GMT | Range | |||
| JEV SA14-14-2 | 104 | 10/10 | 473 | 124–1,026 |
| rJEVmut14-14-2 | 104 | 7/10 | 247 | <8–4,556 |
| rJEVmutE | 104 | 10/10 | 1,857 | 937–3,736 |
| rJEVmut11 | 104 | 10/10 | 1,156 | 496–3,605 |
| rJEVmut3 | 104 | 9/9 | 1,361 | 506–2,521 |
| Mock | NAb | 0/10 | <8 | <8 |
Geometric mean titer calculated only for seroconverted mice.
NA, not applicable.
DISCUSSION
The live-attenuated JEV SA14-14-2 vaccine is safe and effective, but many of the mutations that potentially contribute to its stable attenuation and high level of immunogenicity have not been evaluated. The current study was designed to comprehensively define the genetic determinants of JEV SA14-14-2 that contribute to its attenuation of virulence for mice. Multiple groups have determined the sequence of this vaccine strain and compared it to the sequence of its WT parent virus, JEV SA14, in order to identify mutations that might contribute to virulence attenuation (15, 22–25). However, it has been challenging to decipher the mutations that are truly vaccine strain specific because the nucleotide sequence of the initial JEV SA14 virus stock used to derive the vaccine strain has not been reported. Furthermore, the sequences of both virus strains in GenBank differ considerably because of variable tissue culture passage histories, resulting in previously reported estimates of 57 to 61 nucleotide differences and 24 to 31 amino acid differences between the JEV SA14 and SA14-14-2 strains (15). Here we identified a total of 17 mutations, including nucleotide changes in the UTRs and amino acid substitutions in the polyprotein, that consistently differed between the complete genome sequences of JEV SA14 and SA14-14-2. A similar observation was made previously by Song and colleagues (33).
The vaccine strain-specific mutations or PCR-amplified regions of the JEV SA14-14-2 genome were introduced into a WT rJEV clone, and virus phenotypes were initially studied in Vero cell cultures. Only rJEV mutants containing vaccine strain-specific mutations in the C or E protein had significantly reduced replicative fitness in Vero cells. However, the entire set of vaccine strain-specific mutations was necessary to recapitulate the tissue culture phenotype of JEV SA14-14-2. Surprisingly, this phenotype is not necessarily produced by a combination of vaccine strain-specific C and E protein mutations because previously described JEV SA14-14-2 Vero cell-adapted variants containing a C-S66L reversion mutation retained a small plaque size (32). Furthermore, the combined set of vaccine strain-specific mutations located outside the E gene did not collectively produce a tissue culture phenotype different from that of C-L66S alone. Thus, it appears that vaccine strain-specific mutations found in the E protein coupled with those in the nonstructural protein genes or UTRs produce the small plaque size that is characteristic of JEV SA14-14-2 in tissue culture.
The rJEV mutants were evaluated for neurovirulence attenuation by i.c. inoculation of weanling mice. The only rJEV mutants that had substantial levels of neurovirulence attenuation were those bearing vaccine strain-specific E protein mutations or the authentic JEV SA14-14-2 E protein. This is consistent with the conclusions that were made by Yu and have been drawn based on studies by Arroyo and colleagues using ChimeriVax-JE (15, 26). However, the four reported E protein mutations (L107F, E138K, I176V, and T177A) that, when reverted, were the minimum set of mutations needed to restore a neurovirulent phenotype in mice for ChimeriVax-JE (26) were insufficient to completely attenuate neurovirulence of our WT rJEV. This result indicates that virus chimerization also contributes significantly to the neurovirulence attenuation of ChimeriVax-JE virus. The set of E protein mutations identified as being vaccine strain specific (L107F, E138K, I176V, T177A, Q264H, and K279M) produced rJEV mutants that had residual levels of neurovirulence, while the authentic JEV SA14-14-2 E protein, which also contained the mutations E244G, A315V, S366A, and K439R (Fig. 3), relative to WT rJEV India/78, was critical for complete attenuation of neurovirulence. rJEVmutE caused some mild clinical signs in mice that were inoculated with a high dose by the i.c. route, indicating that attenuating mutations in other regions of the virus genome might minimize vaccine reactogenicity and could be important for overall safety.
FIG 3.
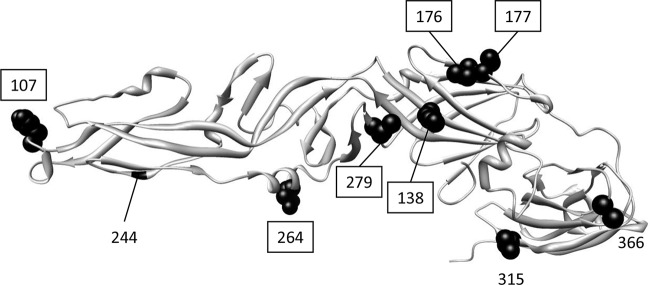
JEV E protein structure (PDB accession no. 3P54) with the location of amino acid differences between JEV SA14-14-2 and wild-type rJEV India/78 indicated. Amino acid substitutions are located in structural domain I (residues 138, 176, 177, and 279), domain II (residues 107, 244, and 264), and domain III (residues 315 and 366). Residue 439 is located in the stem-anchor portion of the E protein and is not pictured here. Boxed residues indicate the locations of amino acids that consistently differed between vaccine virus and parent virus sequences and were considered vaccine strain specific.
Our results deviate from those obtained by Chambers and colleagues, which indicated that the JEV SA14-14-2 E protein was insufficient to attenuate the neurovirulence of WT rJEV Nakayama (29). It is important to note that the virus in their study had acquired mutations relative to the JEV SA14-14-2 sequence, including an E protein reversion mutation, V315A, which could account for the difference in the observed attenuation of neurovirulence demonstrated in our study. Interestingly, Ni and colleagues reported that E protein amino acid substitutions A315V and K439R might in fact be vaccine strain specific and important for attenuation of neurovirulence for JEV SA14-14-2 (23). Furthermore, JEV SA14-14-2 variants described previously are completely attenuated for neurovirulence and lack the E protein mutations T177A and Q264H (15, 23, 24, 32, 34). Taken together, these observations suggest that the collection of the E protein mutations L107F, E138K, I176V, E244G, K279M, A315V, S366A (compared to rJEV India/78), and K439R (Fig. 3) is responsible for complete neurovirulence attenuation of JEV. The location of these mutations in all three E protein structural domains and the stem-anchor region indicates that multiple E protein functions, including cell attachment and entry or virus assembly and release, are probably impaired in neurons of the central nervous system. Reversion of individual or combinations of these JEV SA14-14-2 E protein mutations to the WT amino acid (such as F107L, K138E, G244E, and possibly V315A) is capable of restoring some level of neurovirulence in mice (27–29), emphasizing that their cumulative effect on neurovirulence attenuation is critical for vaccine safety.
i.p. inoculation of mice with JEV is used to evaluate the capacity of the virus to replicate in peripheral tissues and subsequently invade the central nervous system, leading to morbidity and mortality. Wild-type rJEV India/78 has a relatively high potential for neuroinvasion, and this was substantially reduced by the vaccine strain-specific mutations 5′-UTR-T39A and C-L66S, indicating that these mutations probably restrict virus replication in peripheral tissues. For the C-L66S mutation, this phenotype might be related to the significantly reduced levels of virus replication observed in tissue culture. The 5′-UTR-T39A mutation did not affect virus titers in tissue culture, although this nucleotide substitution is located in a region of the 5′ UTR that was previously demonstrated to be important for West Nile virus RNA-dependent RNA polymerase activity (35). Surprisingly, the combined set of vaccine strain-specific mutations found in rJEVmut10, including 5′-UTR-T39A and C-L66S, did not have an additive effect on attenuation of virulence, suggesting that some of these mutations are compensatory. The entire NS1/2A vaccine virus genome region also significantly reduced virus neuroinvasion. This phenotype was apparently produced by at least one of nine mutations that were not identified as vaccine strain specific, including an NS2A nucleotide change previously demonstrated to reduce JEV neuroinvasion (30). It was more difficult to determine the contribution of E protein mutations to the attenuation of virus neuroinvasion, as these mutations were also responsible for substantial levels of neurovirulence attenuation, and these two phenotypes could not be uncoupled.
To better understand the effect of JEV SA14-14-2 mutations on vaccine immunogenicity, neutralizing antibody titers were measured for mice inoculated with mutant viruses that demonstrated a substantial level of attenuation of neurovirulence. rJEVmut14-14-2 was less immunogenic than the JEV SA14-14-2 laboratory strain, and this is likely due to the clonal nature of the recombinant virus stock compared to the mixture of highly immunogenic virus variants that were previously demonstrated to be present in our JEV SA14-14-2 laboratory stock (32). rJEVmutE, bearing the same E protein as that of rJEVmut14-14-2 but no additional mutations, was much more immunogenic. Thus, mutations located outside the E protein gene markedly reduced vaccine immunogenicity. The mutations responsible for this phenotype are likely those that restricted virus replication and dissemination in mouse peripheral tissues and consequently reduced neuroinvasion. It is likely that compensatory vaccine strain-specific mutations mitigated the restricted level of peripheral replication imposed by the 5′-UTR-T39A and C-L66S mutations and in combination did not affect immunogenicity. Furthermore, the collection of E protein mutations that were responsible for complete attenuation of neurovirulence produced a mutant virus that was equally as immunogenic or more immunogenic than underattenuated rJEV mutants, indicating that these mutations do not compromise vaccine immunogenicity. Together, these observations imply that one or more mutations in the NS1/2A genome region substantially reduced the immunogenicity of rJEVmut14-14-2.
The contribution made by most JEV SA14-14-2 vaccine strain mutations to attenuation and immunogenicity had not been previously evaluated. Here, we modified a WT rJEV cDNA clone to contain 17 vaccine strain-specific mutations or PCR-amplified segments of the vaccine virus genome and evaluated their importance for attenuation in mice. The authentic JEV SA14-14-2 E protein was sufficient for complete attenuation of neurovirulence, whereas mutations in other regions of the virus genome predominantly reduced virus neuroinvasion. Recent efforts have been made by others to produce West Nile virus, tick-borne encephalitis virus, and dengue virus prM-E chimeric virus vaccine candidates in an rJEV SA14-14-2 backbone (36–38). In order to achieve adequate levels of attenuation by using this approach, it might be necessary to introduce attenuating mutations in the chimeric virus E proteins, particularly for neurotropic flaviviruses. Additionally, our data indicate that some JEV SA14-14-2 mutations that reduce virus neuroinvasion also reduce vaccine immunogenicity. Therefore, a second-generation rJEV SA14-14-2 vaccine strain variant can be rationally engineered to maximize levels of immunogenicity without affecting vaccine safety.
ACKNOWLEDGMENT
This research was supported by the Intramural Research Program of the National Institute of Allergy and Infectious Diseases, NIH.
REFERENCES
- 1.Rosen L. 1986. The natural history of Japanese encephalitis virus. Annu Rev Microbiol 40:395–414. doi: 10.1146/annurev.mi.40.100186.002143. [DOI] [PubMed] [Google Scholar]
- 2.Buescher EL, Scherer WF. 1959. Ecologic studies of Japanese encephalitis virus in Japan. IX. Epidemiologic correlations and conclusions. Am J Trop Med Hyg 8:719–722. [DOI] [PubMed] [Google Scholar]
- 3.van den Hurk AF, Ritchie SA, Mackenzie JS. 2009. Ecology and geographical expansion of Japanese encephalitis virus. Annu Rev Entomol 54:17–35. doi: 10.1146/annurev.ento.54.110807.090510. [DOI] [PubMed] [Google Scholar]
- 4.Campbell GL, Hills SL, Fischer M, Jacobson JA, Hoke CH, Hombach JM, Marfin AA, Solomon T, Tsai TF, Tsu VD, Ginsburg AS. 2011. Estimated global incidence of Japanese encephalitis: a systematic review. Bull World Health Organ 89:766–774, 774A–774E. doi: 10.2471/BLT.10.085233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vaughn DW, Hoke CH Jr. 1992. The epidemiology of Japanese encephalitis: prospects for prevention. Epidemiol Rev 14:197–221. [DOI] [PubMed] [Google Scholar]
- 6.Villordo SM, Gamarnik AV. 2009. Genome cyclization as strategy for flavivirus RNA replication. Virus Res 139:230–239. doi: 10.1016/j.virusres.2008.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lindenbach BD, Rice CM. 2003. Molecular biology of flaviviruses. Adv Virus Res 59:23–61. doi: 10.1016/S0065-3527(03)59002-9. [DOI] [PubMed] [Google Scholar]
- 8.Mukhopadhyay S, Kuhn RJ, Rossmann MG. 2005. A structural perspective of the flavivirus life cycle. Nat Rev Microbiol 3:13–22. doi: 10.1038/nrmicro1067. [DOI] [PubMed] [Google Scholar]
- 9.Diamond MS. 2009. Mechanisms of evasion of the type I interferon antiviral response by flaviviruses. J Interferon Cytokine Res 29:521–530. doi: 10.1089/jir.2009.0069. [DOI] [PubMed] [Google Scholar]
- 10.Ye J, Zhu B, Fu ZF, Chen H, Cao S. 2013. Immune evasion strategies of flaviviruses. Vaccine 31:461–471. doi: 10.1016/j.vaccine.2012.11.015. [DOI] [PubMed] [Google Scholar]
- 11.Beasley DW, Lewthwaite P, Solomon T. 2008. Current use and development of vaccines for Japanese encephalitis. Expert Opin Biol Ther 8:95–106. doi: 10.1517/14712598.8.1.95. [DOI] [PubMed] [Google Scholar]
- 12.Halstead SB, Thomas SJ. 2011. New Japanese encephalitis vaccines: alternatives to production in mouse brain. Expert Rev Vaccines 10:355–364. doi: 10.1586/erv.11.7. [DOI] [PubMed] [Google Scholar]
- 13.Appaiahgari MB, Vrati S. 2012. Clinical development of IMOJEV—a recombinant Japanese encephalitis chimeric vaccine (JE-CV). Expert Opin Biol Ther 12:1251–1263. doi: 10.1517/14712598.2012.704908. [DOI] [PubMed] [Google Scholar]
- 14.Trent DW, Minor P, Jivapaisarnpong T, Shin J. 2013. WHO working group on the quality, safety and efficacy of Japanese encephalitis vaccines (live attenuated) for human use, Bangkok, Thailand, 21-23 February 2012. Biologicals 41:450–457. doi: 10.1016/j.biologicals.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 15.Yu Y. 2010. Phenotypic and genotypic characteristics of Japanese encephalitis attenuated live vaccine virus SA14-14-2 and their stabilities. Vaccine 28:3635–3641. doi: 10.1016/j.vaccine.2010.02.105. [DOI] [PubMed] [Google Scholar]
- 16.Kumar R, Tripathi P, Rizvi A. 2009. Effectiveness of one dose of SA 14-14-2 vaccine against Japanese encephalitis. N Engl J Med 360:1465–1466. doi: 10.1056/NEJMc0808664. [DOI] [PubMed] [Google Scholar]
- 17.Bista MB, Banerjee MK, Shin SH, Tandan JB, Kim MH, Sohn YM, Ohrr HC, Tang JL, Halstead SB. 2001. Efficacy of single-dose SA 14-14-2 vaccine against Japanese encephalitis: a case control study. Lancet 358:791–795. doi: 10.1016/S0140-6736(01)05967-0. [DOI] [PubMed] [Google Scholar]
- 18.Chotpitayasunondh T, Sohn YM, Yoksan S, Min J, Ohrr H. 2011. Immunizing children aged 9 to 15 months with live attenuated SA14-14-2 Japanese encephalitis vaccine in Thailand. J Med Assoc Thai 94(Suppl 3):S195–S203. [PubMed] [Google Scholar]
- 19.Tandan JB, Ohrr H, Sohn YM, Yoksan S, Ji M, Nam CM, Halstead SB. 2007. Single dose of SA 14-14-2 vaccine provides long-term protection against Japanese encephalitis: a case-control study in Nepalese children 5 years after immunization. Vaccine 25:5041–5045. doi: 10.1016/j.vaccine.2007.04.052. [DOI] [PubMed] [Google Scholar]
- 20.Ohrr H, Tandan JB, Sohn YM, Shin SH, Pradhan DP, Halstead SB. 2005. Effect of single dose of SA 14-14-2 vaccine 1 year after immunisation in Nepalese children with Japanese encephalitis: a case-control study. Lancet 366:1375–1378. doi: 10.1016/S0140-6736(05)67567-8. [DOI] [PubMed] [Google Scholar]
- 21.WHO. 2014. WHO Expert Committee on Biological Standardization, 63rd report, annex 7, recommendations to assure the quality, safety and efficacy of Japanese encephalitis vaccines (live, attenuated) for human use. WHO Press, Geneva, Switzerland. [Google Scholar]
- 22.Aihara S, Rao CM, Yu YX, Lee T, Watanabe K, Komiya T, Sumiyoshi H, Hashimoto H, Nomoto A. 1991. Identification of mutations that occurred on the genome of Japanese encephalitis virus during the attenuation process. Virus Genes 5:95–109. doi: 10.1007/BF00571925. [DOI] [PubMed] [Google Scholar]
- 23.Ni H, Chang GJ, Xie H, Trent DW, Barrett AD. 1995. Molecular basis of attenuation of neurovirulence of wild-type Japanese encephalitis virus strain SA14. J Gen Virol 76(Part 2):409–413. [DOI] [PubMed] [Google Scholar]
- 24.Ni H, Burns NJ, Chang GJ, Zhang MJ, Wills MR, Trent DW, Sanders PG, Barrett AD. 1994. Comparison of nucleotide and deduced amino acid sequence of the 5′ non-coding region and structural protein genes of the wild-type Japanese encephalitis virus strain SA14 and its attenuated vaccine derivatives. J Gen Virol 75(Part 6):1505–1510. [DOI] [PubMed] [Google Scholar]
- 25.Nitayaphan S, Grant JA, Chang GJ, Trent DW. 1990. Nucleotide sequence of the virulent SA-14 strain of Japanese encephalitis virus and its attenuated vaccine derivative, SA-14-14-2. Virology 177:541–552. [DOI] [PubMed] [Google Scholar]
- 26.Arroyo J, Guirakhoo F, Fenner S, Zhang ZX, Monath TP, Chambers TJ. 2001. Molecular basis for attenuation of neurovirulence of a yellow fever virus/Japanese encephalitis virus chimera vaccine (ChimeriVax-JE). J Virol 75:934–942. doi: 10.1128/JVI.75.2.934-942.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yun SI, Song BH, Kim JK, Yun GN, Lee EY, Li L, Kuhn RJ, Rossmann MG, Morrey JD, Lee YM. 2014. A molecularly cloned, live-attenuated Japanese encephalitis vaccine SA14-14-2 virus: a conserved single amino acid in the ij hairpin of the viral E glycoprotein determines neurovirulence in mice. PLoS Pathog 10:e1004290. doi: 10.1371/journal.ppat.1004290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yang D, Li XF, Ye Q, Wang HJ, Deng YQ, Zhu SY, Zhang Y, Li SH, Qin CF. 2014. Characterization of live-attenuated Japanese encephalitis vaccine virus SA14-14-2. Vaccine 32:2675–2681. doi: 10.1016/j.vaccine.2014.03.074. [DOI] [PubMed] [Google Scholar]
- 29.Chambers TJ, Droll DA, Jiang X, Wold WS, Nickells JA. 2007. JE Nakayama/JE SA14-14-2 virus structural region intertypic viruses: biological properties in the mouse model of neuroinvasive disease. Virology 366:51–61. doi: 10.1016/j.virol.2007.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ye Q, Li XF, Zhao H, Li SH, Deng YQ, Cao RY, Song KY, Wang HJ, Hua RH, Yu YX, Zhou X, Qin ED, Qin CF. 2012. A single nucleotide mutation in NS2A of Japanese encephalitis-live vaccine virus (SA14-14-2) ablates NS1′ formation and contributes to attenuation. J Gen Virol 93:1959–1964. doi: 10.1099/vir.0.043844-0. [DOI] [PubMed] [Google Scholar]
- 31.Gromowski GD, Firestone CY, Hanson CT, Whitehead SS. 2014. Japanese encephalitis virus vaccine candidates generated by chimerization with dengue virus type 4. Vaccine 32:3010–3018. doi: 10.1016/j.vaccine.2014.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gromowski GD, Firestone CY, Bustos-Arriaga J, Whitehead SS. 2015. Genetic and phenotypic properties of Vero cell-adapted Japanese encephalitis virus SA14-14-2 vaccine strain variants and a recombinant clone, which demonstrates attenuation and immunogenicity in mice. Am J Trop Med Hyg 92:98–107. doi: 10.4269/ajtmh.14-0427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Song BH, Yun GN, Kim JK, Yun SI, Lee YM. 2012. Biological and genetic properties of SA(1)(4)-14-2, a live-attenuated Japanese encephalitis vaccine that is currently available for humans. J Microbiol 50:698–706. doi: 10.1007/s12275-012-2336-6. [DOI] [PubMed] [Google Scholar]
- 34.Eckels KH, Yu YX, Dubois DR, Marchette NJ, Trent DW, Johnson AJ. 1988. Japanese encephalitis virus live-attenuated vaccine, Chinese strain SA14-14-2; adaptation to primary canine kidney cell cultures and preparation of a vaccine for human use. Vaccine 6:513–518. doi: 10.1016/0264-410X(88)90103-X. [DOI] [PubMed] [Google Scholar]
- 35.Li XF, Jiang T, Yu XD, Deng YQ, Zhao H, Zhu QY, Qin ED, Qin CF. 2010. RNA elements within the 5′ untranslated region of the West Nile virus genome are critical for RNA synthesis and virus replication. J Gen Virol 91:1218–1223. doi: 10.1099/vir.0.013854-0. [DOI] [PubMed] [Google Scholar]
- 36.Li XF, Zhao W, Lin F, Ye Q, Wang HJ, Yang D, Li SH, Zhao H, Xu YP, Ma J, Deng YQ, Zhang Y, Qin ED, Qin CF. 2013. Development of chimaeric West Nile virus attenuated vaccine candidate based on the Japanese encephalitis vaccine strain SA14-14-2. J Gen Virol 94:2700–2709. doi: 10.1099/vir.0.059436-0. [DOI] [PubMed] [Google Scholar]
- 37.Wang HJ, Li XF, Ye Q, Li SH, Deng YQ, Zhao H, Xu YP, Ma J, Qin ED, Qin CF. 2014. Recombinant chimeric Japanese encephalitis virus/tick-borne encephalitis virus is attenuated and protective in mice. Vaccine 32:949–956. doi: 10.1016/j.vaccine.2013.12.050. [DOI] [PubMed] [Google Scholar]
- 38.Li XF, Deng YQ, Yang HQ, Zhao H, Jiang T, Yu XD, Li SH, Ye Q, Zhu SY, Wang HJ, Zhang Y, Ma J, Yu YX, Liu ZY, Li YH, Qin ED, Shi PY, Qin CF. 2013. A chimeric dengue virus vaccine using Japanese encephalitis virus vaccine strain SA14-14-2 as backbone is immunogenic and protective against either parental virus in mice and nonhuman primates. J Virol 87:13694–13705. doi: 10.1128/JVI.00931-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reed LJ, Muench H. 1938. A simple method of estimating fifty per cent endpoints. Am J Hyg 27:493–497. [Google Scholar]