Abstract
In 2009, the General Medical Council UK (GMC) published its updated guidance on medical education for the UK medical schools – Tomorrow’s Doctors 2009. The Council recommended that the UK medical schools introduce, for the first time, a clinical placement in which a senior medical student, “assisting a junior doctor and under supervision, undertakes most of the duties of an F1 doctor”. In the UK, an F1 doctor is a postgraduation year 1 (PGY1) doctor. This new kind of placement was called a student assistantship. The recommendation was considered necessary because conventional UK clinical placements rarely provided medical students with opportunities to take responsibility for patients – even under supervision. This is in spite of good evidence that higher levels of learning, and the acquisition of essential clinical and nontechnical skills, depend on students participating in health care delivery and gradually assuming responsibility under supervision. This review discusses the gap between student and doctor, and the impact of the student assistantship policy. Early evaluation indicates substantial variation in the clarity of purpose, setting, length, and scope of existing assistantships. In particular, few models are explicit on the most critical issue: exactly how the student participates in care and how supervision is deployed to optimize learning and patient safety. Surveys indicate that these issues are central to students’ perceptions of the assistantship. They know when they have experienced real responsibility and when they have not. This lack of clarity and variation has limited the impact of student assistantships. We also consider other important approaches to bridging the gap between student and doctor. These include supporting the development of the student as a whole person, commissioning and developing the right supervision, student-aligned curricula, and challenging the risk assumptions of health care providers.
Keywords: apprenticeship, workplace learning, competency
Introduction
In 2009, the General Medical Council UK (GMC) published its updated guidance on medical education for the UK medical schools – Tomorrow’s Doctors 2009. The Council recommended that medical schools introduce, for the first time, a new kind of clinical placement in which a senior medical student, “assisting a junior doctor and under supervision, undertakes most of the duties of an F1 doctor”. In the UK, an F1 doctor is a postgraduation year 1 (PGY1) doctor. This new kind of placement was called a student assistantship.1
The recommendation was considered necessary because, by 2009, conventional UK clinical placements rarely provided medical students with opportunities to participate in health care provision or to take responsibility for patients – even under supervision. The result was that students graduated from medical school with very limited experience of taking on clinical responsibility or operational work. They had to learn the skills, processes, and disciplines associated with these functions very rapidly from the day of qualification. At this point in their training, following graduation, their performance has a direct impact on clinical services and patient care.
This review explores the unusually wide gap between student and doctor that had grown up over time in the UK and some of its consequences. The assistantship is a policy attempt to bridge the gap, and we discuss the response to and consequences of the policy so far. In addition, we consider other approaches to the same problem – bridging the gap between student and doctor.
The gap between student and doctor
Comparing doctors and students requires a description or taxonomy of what a doctor is or does. Attempting such a description is not a straightforward task. Nevertheless, a range of influential frameworks have attempted to articulate the domains of a contemporary doctor’s practice.1–3 Some common features emerge. In every case, the domains of practice can be mapped to Bloom’s taxonomy of learning (cognitive, psychomotor, and affective). The GMC framework, for example, articulates these domains as “scholar and scientist”, “practitioner”, and “professional”. Similarly, the Association of American Medical Colleges report 1999 sets out four attributes expected of all graduates: “knowledgeable”, “skillful”, “altruistic”, and “dutiful”. Most recent frameworks now expand the scholarly disciplines of a doctor beyond the traditional base of the biomedical scientific disciplines to include “new disciplines” such as psychology, the social sciences, population health, the scientific method, and ethics and the law.
Figure 1 presents a summary of the scope and depth of the UK undergraduate curricula in 2009 based on the authors’ subjective interpretation of publicly available data. The columns (scope) use the GMC domains above (separating the new scholarly disciplines from the traditional disciplines). The rows apply Miller’s taxonomy of “know”, “know how”, “show”, and “do” and expand the top behavioral category to differentiate between activities done on real patients for learning purposes (behavior level 2 – do) and activities done on real patients for real purposes (behavior level 3 – participate).
Figure 1.
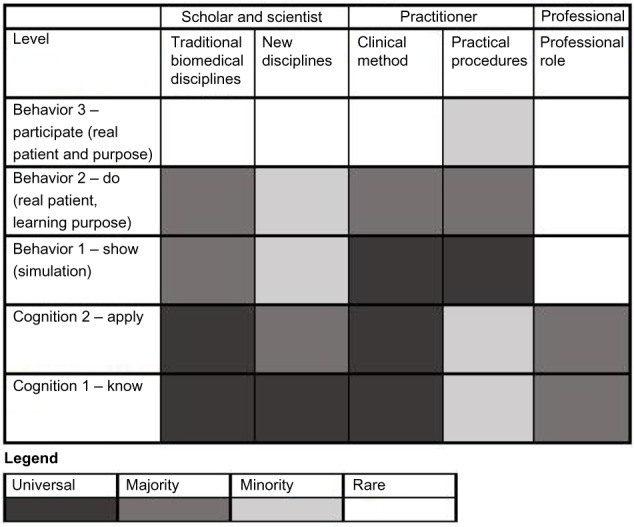
The scope and depth of the UK curricula in 2009.
A number of historical movements have left their fingerprints on this picture. Some of these are itemized below.
The behavioral levels
It has always been essential that medical students progress from understanding things to doing things, but in the past, the behavioral levels of learning were addressed informally through relatively unregulated clinical placements similar to apprenticeships. Only in the last 25 years have these aspects of learning been reflected in the articulated curriculum and in assessment schemes. The competency movement was a key driver of this change.4
Practical procedures
McManus et al drew attention to a diminishing breadth of clinical and practical experience as long ago as the 1980s.5 Most curricula have paid attention to practical skills since the 1990s. The GMC has mentioned clinical skills in its curriculum guidance since 1993;6 however, in 2009, the guidance took the step of setting out 32 specific practical skills that all medical students need to have demonstrated by graduation.1 Frequently, the practical procedures program is delivered according to a “training” model of skills acquisition with relatively little attention to underlying principles.
The new disciplines
Educators with specialist interests and health policymakers have called, and continue to call, for the inclusion of various new disciplines as core to the education of medical students. In the UK, since 1993, GMC guidance has highlighted the importance of communication skills, sociology, public health, and scientific method. These have joined the traditional disciplines of human anatomy, biochemistry, physiology, pathology, and the clinical method. The place of psychology, statistics, evidence-based medicine, ethics, spiritual health, whole-person medicine, the law, etc varies from program to program. Characteristically, however, these newer disciplines are taught by specialists at defined points in the program and fail to be integrated across the curriculum as a whole – not least because clinician teachers may have a limited understanding of the disciplines themselves.
Professionalism
In many ways, the professionalism movement is one of the big themes in contemporary medical education. It is driven for positive reasons by educators with particular convictions and for negative reasons by public lapses in professional conduct.7 Professionalism has been a running theme of most medical education journals and conferences for more than 10 years. However, there is a problem. One core aspect of professionalism is responsibility. As Figure 1 shows, in the UK, by 2009, a graduating medical student may never have participated in patient care or delivering clinical services – even under supervision. As a result, their professionalism is practiced and assessed largely in terms of their contribution to learning groups, their dress and attendance, the handing in assignments, etc.8
The gap then between student and doctor is quite clear. It is participation in health care delivery with a real purpose.
In 2009, few medical students in the UK had experienced these core aspects of the day-to-day work of a clinician: real-world problem-solving; reaching a judgment with consequences; intervening, seeing through, evaluating, and following up consequences; and prioritizing a range of tasks and agendas in a work setting. Newly qualified doctors typically experienced these aspects of working as a clinician for the first time when they began in employment. At that point, their success or failure in acquiring the new skills has a direct impact on clinical services and patient care. There is a supervision structure in place, but the supervision is “hands off”. Almost all new doctors access support only on request, and the more senior staff from whom they access that support have a full diary of service commitments which they must put to one side in order to provide the requested supervision. The tension implicit in this sudden and relatively unsupported learning curve has several negative consequences.
The clinical consequences
Patient care is probably affected. In 2009, investigators from Imperial College used empirical data to confirm a trend in patient mortality that had been perceived for many years. They showed that mortality rates in English hospitals rose by 6% on the first working day of each consecutive cohort of newly qualified doctors. This was observed in historical data when the new doctors started on the 1st of the August. The rise then moved to the first Wednesday of the month when this became the rotation date for newly qualified doctors.9 While debate continues over cause and effect, Sir Bruce Keogh – NHS medical director – was quoted in the lay press (Daily Mail) as saying:
The intention is to end the so-called killing season. This is good news for patients – we recognise the change-over period in August puts patients at risk.10
He also drew a direct link between the perceived risk and the need for junior doctors to adapt to an unfamiliar working environment and role.10
Junior doctors are under stress as they change from being a student to a professional and they need help to adapt to a working environment when they’ve never done a job before.10
The stress he describes is certainly perceived by junior doctors. The following quotes typify the perceptions and advice handed from one generation of newly qualified doctors to the next in the BMJ publication: You will survive: guide for newly qualified doctors:11
Before the ward round: 1) Put all notes where they should be. 2) Check blood/scan results are in the notes. 3) Prepare discharge and phlebotomy forms. 4) Familiarise yourself with new patients. […] It is normal to feel sick the first time you are on call.11
These gems of advice illustrate two main themes. They highlight the importance of knowing how to run relatively mundane operational aspects of the job, and the fear that comes with taking on responsibility.
The gap we are highlighting is not unique to the UK. However, it is particularly intense in the developed western world and at the present time. The previous generation of medical students in the UK were able to participate more fully as legitimate junior members of robust teams. As they approached qualification, it was common for a senior student to cover the work of the most junior doctor when he or she took leave in an arrangement called a house-officer locum. Elsewhere in the world, particularly in resource-poor environments such as remote rural settings and the developing world, medical students are more likely to deliver significant service roles. This is frequently reported by the UK medical students who visit developing countries for the medical elective. The NHS Careers website makes this participation or “hands-on” opportunity explicit:12
Going to a developing country may appeal to you as a chance to do some relief work and you will be likely to have more of an opportunity to have a hands-on experience.12
From a clinical risk perspective then, this lack of supervised participation is a highly undesirable situation. What about the learning perspective?
The educational consequences
The evidence suggests that many medical students are more passive than the “ideal” adult learner, more stressed than reference populations, and that their professional identity develops disappointingly late. Remmen et al, surveying final-year students in Antwerp, Belgium, found that the majority of learners lapsed into passive learning roles during clinical placements.13 In her commentary, Krajic Kachur describes how rapidly even “beginning students” become passive in clinical contexts.14 In both cases, students became passive because they struggled to understand their role in clinical settings.
From a theoretical standpoint, these observations belong with the literature on situated learning or communities of practice. Working in that field, Lave and Wenger collaborated in 1991 to coin a seminal learning concept – learning as “legitimate peripheral participation in communities of practice”.15 Their analysis is thoroughgoing and beyond the scope of this review. However, one of their core critiques of formalized education systems is that they do not nurture or break the relationship between the learner and the master or practitioner. Arguably, that is what the investigators above are observing.
Dornan et al investigated the nature of learning in clinical placements in Manchester, UK.16 They found that one critical cofactor in learning for practice was the development of a professional state of mind. Students developed that state of mind through supported participation in practice:
To reach their ultimate goal of helping patients, medical students must develop two qualities. One is practical competence; the other is a state of mind that includes confidence, motivation and a sense of professional identity.16
In Sheffield, UK, we track the development of students’ professional self-identity.17 We have found that medical students begin to develop a professional identity later than students of other health and social care professions. They attribute the delay to a lack of supported participation in professional activities. The following student quote illustrates the point:
Just watching means you can’t be sure that you can actually do the task or are capable of doing the task. If you work with the people and do things then you can be confident and capable.17
Kavanagh et al, reporting on students’ and supervisors’ perceptions of work shadowing placements immediately ahead of the first F1 post in 2010 before student assistant-ships, summarize these concerns clearly:18
[…] students felt unprepared for commencing work, with particular mention given to medical emergencies, prescribing, and the emotional aspects of the job. […] students should be offered additional supervised responsibility for delivery of patient care […]18
A lack of participation then, holds back active student learning and the development of professional identity, contributes to student stress, delays the meaningful assessment of professionalism, and contributes to clinical risk. In that context, the student assistantship was announced in 2009. It was to be a new kind of clinical placement in which a senior medical student, “assisting a junior doctor and under supervision, undertakes most of the duties of an F1 doctor”. The idea was not new. Similar assistantships in New Zealand have been in place for many years.19
Implementing the policy
In its regulatory role, the GMC mandated all the UK medical schools to respond to the 2009 recommendations by the academic year 2011/2012. Compliance is monitored through the Quality Assurance of Basic Medical Education inspection cycle.
We undertook a questionnaire survey in June 2010 (ahead of the 2011/2012 academic year) exploring the response of the 31 UK medical schools to the policy.20 Defining the “duties of an F1 doctor” by the F1 curriculum competencies, we found that most schools had reservations about some duties – particularly those duties that appeared to present a degree of clinical risk. The following quotes came directly from the responses of participating medical schools:
[Concerns] mostly relate to areas where our teaching trusts are not yet happy to allow students to be involved in these processes.
Patient safety, care standards and trust risk assessment may preclude some elements.20
Other schools were concerned that a brief period of assistantship may not provide the opportunity for the student to undertake many of the duties:
Many are opportunities which may or may not arise ‘by chance’ during such a short period of time.
May not get exposure or time to do all these things within the timescale.20
Still other schools felt confident that their existing final-year placements already provided adequate opportunity for students to take responsibility:
We already have student assistantships in place in the final year: three 10-week placements in medicine, surgery and acute care, plus one 4-week placement in general practice.
Year 5, they are already in existence as part of our curriculum, they just need renaming.
Models of assistantship
Tallentire et al surveyed newly qualified F1 doctors and clinical supervisors in 2011 asking them to rank 16 possible priority areas for development during the student assistantship.21 keeping with the BMJ You will survive guide and Kavanagh’s survey, it was the operational aspects of the role like prescribing, prioritizing, working out of hours, and administrative tasks that were highlighted. The authors suggest that priorities should guide the design of assistantships:
The opportunities considered most important by both FY1s and educational supervisors were prescribing drugs and fluids, providing emergency care and prioritisation of tasks. Free-text responses suggested that experience of out-of-hours working, administrative tasks and the theatre environment were also important.21
In 2011, following a number of implementation workshops, the GMC published supplementary guidance explaining that:22
It became clear that the schools felt that they needed extra advice from the GMC as to how certain requirements in Tomorrow’s Doctors (2009) should be taken forward.22
In their guidance, the GMC gathered and disseminated examples of good practice in implementing the assistantship.22 Three of them are described below:
In secondary care students are allocated a number of in-patients, usually five, for which they have prime responsibility. Students clerk patients, write notes, arrange investigations, visit in-patients and write daily continuation notes on in-patients, liaise with other staff, explain management plans to patients, take part in discharge planning and are present during informed consent, or during procedures which are not within the competence of students. They keep a ‘parallel prescription form’ for their patients that are checked by pharmacists. (Hull York Medical School).
Acting throughout as assistant F1s, they are directly involved (under close supervision) in the assessment and management of patients with a wide range of medical and surgical problems within primary and secondary care. As the year progresses they are expected to take on more responsibility for patient care. The Practical Skills assessment (October) and Therapeutics and Prescribing assessment (March) facilitate the development of the required graduate competencies so they can perform basic procedures during their attachments. The programme also includes seminars and workshops in ‘wardcraft’ including communication skills for multidisciplinary teamwork, an intensive ‘clinical management of acute cases’ small group teaching day in the high fidelity simulator, and the two day ‘Death and Dying’ course. (Cambridge).
During the six week clinical block students gradually assume the majority of the roles of the F1 to whom they are attached. Each student spends time with both F1s in Medicine and Surgery and are involved in significant exposure to acute duties. They access reporting (lab/x-ray) systems that they will use as an F1. They don’t: perform procedures (unless with patient consent and supervised by a competent supervisor), provide signatures for prescriptions, or prescribe x-rays. They are supported by access to Doctor Online Training System (DOTS) F1 materials. This specifies the intended minimum level of training exposure to clinical activities. It covers the six domains of Preparation for Practice (PfP): 1. Prescribing and drug administration, 2. Advanced Clinical Skills, 3. Managing the acutely ill patient, 4. Life skills, 5. Ethics, Law and risk management, and 6. Practical working as a Foundation Year 1 Doctor. (Glasgow). [Quote reproduced with permission from the General Medical Council; Clinical Placements for Medical Students: Advice Supplementary to Tomorrow’s Doctors (2009); Copyright © 2011 General Medical Council.]22
These examples of good practice vary substantially in tone. Only Hull York Medical School specifically mentions students taking responsibility for a group of patients. The Cambridge and Glasgow examples have substantial scaffolding to support the students (“wardcraft” and “DOTS”, respectively) but are not explicit about the way in which they help students to take responsibility for patient care.
Since the academic year 2011–2012, only five UK medical schools with fully operational curricula have been visited by the GMC for evaluation against Tomorrow’s Doctors 2009. These are the first visits to report on the implementation of student assistantships.23 Their findings are summarized below:
The Aberdeen report (2012) indicates that the assistantship is embedded within the second half of otherwise conventional clinical placements (weeks 4–7 in each of four 8-week blocks) covering medicine, surgery, psychiatry, and another specialty. There is relatively little regulation across placements sites, so it is not clear whether students have the same experience wherever they are placed. There is also no explicit assessment of, or feedback about, the student’s performance in the assistantship. Where it occurred, students were glad of night-time work. Both students and supervisors perceived that the assistantship improved readiness for practice.
The Belfast report (2012) indicates that uncertainty over F1 placements makes it difficult to allocate students to an assistantship related to their F1 role. The school plans to reduce its assistantship from 11 weeks to 8 weeks following evaluation. Both students and supervisors perceived that the assistantship improved readiness for practice.
The Keele reports (2012 and 2013) indicate an extensive assistantship program including 15 weeks in primary care, 5 weeks in medicine, and 5 weeks in surgery. The primary care assistantship includes opportunities for students to consult with a minimum of 370 patients “in collaboration with a general practitioner (GP)”. Students and GP teachers reported much increased confidence, efficiency, and skill in consulting and patient management skills. In the secondary care assistantships, students work alongside F1 doctors, but most consult with fewer than ten patients per week. In spite of that, both students and staff spoke of “participation” and “being part of the team” in the hospital assistantships. Despite the strength of the primary care assistantships, some of the students felt that they would prefer longer in secondary care emergency settings (especially A and E) in advance of their F1 role.
The Leeds report (2012) contains very little detail on the assistantships but indicates that staff and students did not all understand the intent of the assistantship and recommended greater clarity in this area.
The Liverpool report (2012) is similarly brief on the assistantship. It describes an 8-week final-year attachment where the students undertake the tasks an F1 would undertake but with supervision and appropriate countersigning of any investigation or treatment. Students enjoyed being part of the team, and both students and F1s perceived that the assistantship improved readiness for practice.
What emerges from these reports, and from the good practice examples, is substantial variation in the clarity of purpose, setting, length, and scope of existing student assistantships in the UK. In particular, most of the reports are not at all explicit on the critical issue: exactly how much does the student participate in the delivery of care, how much responsibility is he or she given, and how is supervision deployed to maximize learning and patient safety? This is usually only clear for prescribing – which is never more than a “simulated” responsibility for legal reasons.
Consequences of the policy
Data on the experience
Almost every one of the GMC visit reports indicates that students, F1s, and supervisors perceived that the assistantship improved readiness for practice. The Keele students and GP supervisors reported greater confidence, skill, and efficiency in consulting and management planning following their 15-week GP student assistantship but would have preferred more time in secondary care emergency settings before starting as F1s.
To date, no peer-reviewed paper has been published reporting the experience of students and staff in relation to student assistantships. However, an extensive report has been prepared by Monrouxe et al based on a program of research commissioned by the GMC.24 The report contains two original datasets. The first dataset comes from multisite (four schools), cross-sectional narrative interviews with a cross-sectional purposive sample of several groups of stakeholders. The second dataset comes from a longitudinal solicited audio diary method drawing on a subgroup of F1 participants from the original sample. Most of the coded narratives expressed a positive view of the student assistantship in smoothing the transition between being a final-year student (sometimes referred to as F0 in the interviews) and becoming an F1. The authors write:
Some […] felt that there was only a ‘slight jump’ from assistantship to their F1 year in terms of respon sibility. [Others] highlighted a lack of responsibility [and were left] feeling sheltered and calm during their F0 year, a far cry from the disturbance of the F1 “ocean”.24
However, a subgroup of the F1 respondents expressed a view that their assistantship experience had not been effective. These respondents typically indicated that they had not really had the chance to take substantial responsibility for patient care or to work out of hours. As the earlier section on “models of assistantship” shows, few assistantships are consistent or specific on these key aspects of their design.
Data on the impact
To our knowledge, there is no peer-reviewed data evaluating the impact of the assistantship on either perceptions or outcomes (efficiency, patient safety, prescribing errors, stress and sickness, etc). The GMC publication Be prepared: are new doctors safe to practice? explains that new graduates have been educated under both the old and the new versions of tomorrow’s doctors and through a period of much change so that it’s difficult to reach firm conclusions about the impact of the new tomorrow’s doctors.25
Nevertheless, the report points to the GMC annual survey which shows a fluctuating but apparently increasing proportion of the UK graduates indicating that they felt prepared for their first F1 post. They also cite a falling proportion of Foundation Doctors being formally identified as “in difficulty”.
Overall perspective on the student assistantship
There is a clear case for interventions that reduce the gap in participation and responsibility between student and doctor in the UK – and probably in many other parts of the developed world. Clinical outcomes may be affected at the time of transition. Senior students are being deactivated as learners. The gap causes significant stress and anxiety at transition.
The student assistantship is one attempt to bridge the gap. However, currently available data from GMC inspection reports indicate substantial variation in the clarity of purpose, setting, length, and scope of existing assistantships in the UK. In particular, most of the reports are not at all explicit on the most critical issues: exactly how much does the student participate in the delivery of care, how much responsibility is he or she given, and how is supervision deployed to maximize learning and patient safety?
This detail is not lost on students. Students who feel that they have had the chance to “step up” and take responsibility have a positive view of assistantships. Those who have not had that opportunity still perceive a big gap.
The variability of assistantship models, proximity of implementation (2011/2012), and the complexity of medical education as a whole preclude any firm conclusions as to the impact of the assistantship. However, it seems likely that lack of clarity over how much participation and responsibility are expected will have reduced the impact of the assistantship policy.
We consider that the move to promote student participation and responsibility is appropriate and important. We would like to see the GMC specify in much more detail how the assistantship is implemented in order to ensure that students are given responsibility and supported in their participation. One obvious option is to disseminate models of good practice. One promising model is described by the Hull York Medical School. Medical students take primary responsibility for a small cohort of in-patients undertaking all the tasks that they are competent to undertake and either observing or simulating the tasks that they are not yet competent to undertake (see “Models of assistantship”). Similarly, the primary care-based assistantships in Keele provide medical students with exceptional participation as they consult with a substantial number of patients in their own right but with immediate access to a GP and a prospective checking mechanism (see “Models of assistantship”).
Complementary approaches to the student–doctor gap
The student assistantship is an attempt to bridge the gap between student and doctor by curriculum policymaking. There is, of course, much more to be done than policymaking. We would like to review a few other important considerations briefly.
Supporting the development of the student as a person
Monrouxe’s interviews and audio diaries make it clear that individual factors are critical in determining both engagement with educational interventions (like the student assistantship) and preparedness for practice.24 Examples from the interviews included: “Students’ confidence, proactivity, [and] resilience […]”.
These personal characteristics are not listed as curricular outcomes for any medical school we know – yet they are pivotal to bridging the gap between student and doctor. Many psychologists would regard them as part of the developmental journey to self-authorship,26 or self-efficacy.27 In their AMEE guide on developmental student support,28 Sandars et al write:
Developmental student support has a focus on developing the whole person, not only academic and clinical competence.28
Their thesis is that medical school is a “nexus” for personal development. Since personal development affects every aspect of performance, the authors rightly draw our attention to it.
Strikingly, the prevailing culture in medicine may even serve to suppress personal development rather than to support it. Kennedy et al write powerfully about strategies that medical trainees use to maintain credibility. They may even consider lying about clinical data to maintain their own credibility.29 This is, at least in part, a product of the learning and practicing culture which they perceive that they are joining.
Speaking of the relationship between undergraduates and the curriculum, one of her co-authors, Glenn Regehr, ask the provocative question: “What if the students are not playing our game, but instead gaming our game?”29
An educational culture which succeeded in promoting the progressive, individual development of the whole person is likely to produce students who seek the opportunity to be active participants as learners, and who are more ready to step into the professional role when their time comes.
A themed issue of the journal Medical Teacher around the subject “Becoming a doctor” explored the possible roles of mentorship,30 feedback,31 and assessment,32 in promoting the development of students as they become doctors.
Commissioning and developing the right supervision
We have argued that the gap between student and doctors is a participation gap. Of course, participation is not a binary state; there are degrees of participation – starting at the most peripheral level. But, as Lave and Wenger point out, participation only begins when the learner is given legitimacy.15 The point we are making is that medical students in the UK have usually experienced very low degrees of participation partly because, in recent times, they have had little or no legitimate role. In that context, students must look to practitioners – in this case clinical supervisors – to give them the gift of a legitimate role.
This perspective provides a powerful interpretation of the students’ perceptions reported in earlier sections. It helps us to understand why a policy mandated by the regulatory body (the GMC), and implemented by a medical school, is only meaningful when it is taken to heart by the particular community of practice that a student wishes to join. Some students spoke of a “lack of clarity about the intent of the assistantship” because there was a gap between what the medical school promised and what their supervisors were willing to offer.23 In Monrouxe’s interviews, the students who had been given the gift of legitimacy used the words “acting up” and “being given responsibility”, while others spoke of “not being given responsibility” and “being sheltered”.24 The clinical supervisor, as a “master practitioner” in the student’s immediate potential community of practice, functions as a key-holder. Officially, in the UK, the medical student’s clinical supervisor is the senior clinician (consultant) who leads the clinical team. In practice, qualified doctors of all grades are key-holders who may give or withhold the gift of a legitimate role. An individual medical student’s experience of participation can be made or broken by the approach of a single doctor on the team. This was frequently reported in Lynn Monrouxe’s interviews and audio diaries.
Tim Dornan’s work also highlights the central role of the supervisor in student learning in practice. He also focuses on the supervisor’s role in enabling participation, but he speaks of the supervisor as an enabler in participation more than a key-holder. His interviews with students highlight the gulf between their abilities and the abilities that they need for participation. He describes the role of the supervisor in the following terms:
Practitioners help students participate by being both supportive and challenging. The presentation of clear learning objectives and continuous periods of attachment that are as personal to the student(s) and practitioner(s) as possible promote workplace learning.16
He describes the partnership between student and supervisor as “supported participation”.
Applying a carefully designed structural equation model to evaluate the impact of clinical experience and teaching time on assessment performance, Wimmers et al showed the same thing. They found that measureable improvements in clinical competence did not depend on the volume of clinical experience, or on the volume of teaching; rather, high-quality supervision in clinical contexts was the vital cofactor for students to unlock learning from experience.33
From either of these perspectives – supervisor as key-holder, or supervisor as enabler – the supervisor has a crucial role in regulating the participation gap. The values and skills of clinical supervisors – which reflect, to some extent, their own community of practice – have the potential to do or to undo any intervention at a policy level.
An educational culture which succeeded in promoting the pivotal and skillful role of clinical supervisors is likely to enable students to be active participants as learners, and to be more ready to step into the professional role when their time comes.
The western world has seen a slow and steady movement to professionalize medical education over the last 25 years. Many medical schools employ staff with educational qualifications and skills. Clinicians who are postgraduate educators are increasingly holding formal qualifications and formal posts. However, the clinicians who supervise medical students are one of the last groups to see change. It is still usual in the UK, for example, for a student clinical supervisor to have no educational qualifications – or only very limited operational-level training – and to have no designated time, remuneration, or recognition for their supervisory work. Given the importance of their task, this seems inappropriate.34 We recommend growing a faculty of permanent senior clinicians with dedicated time to support participation. Most UK models appoint nurses as long-term faculty (eg, clinical skills officers) or training-grade doctors on secondment. It is more difficult for these groups to change the educational culture of the organization.
Student-aligned curricula
Few areas of educational policy have undergone more reform than curricula. In the 1990s, Biggs made the obvious but important point that curricula should be aligned to the desired learning outcomes.35 Consequently, integrated curricula seek to encourage integrated learners, spiral (distributive and progressive) curricula seek to develop meaning-makers, problem-based curricula and student-selected components seek to nurture active learners, and competency-based curricula aspire to produce able practitioners. Each of these developments is rational. However, none of them has had a transferable and measurable impact on learning. In part, this lack of measurable impact may represent type II error. The systems under investigation are extremely complex.36 After all, medical education is not rocket science; it is much more complicated than that.37
Perhaps, however, it is because few if any of the curricular paradigms listed help students in their journey to becoming doctors. The language of these curricula is educators’ language and not students’ language. They do little to help the students understand the world that they are entering. Indeed, they add another barrier; students who have experienced newer curricula meet clinical staff who have experienced more traditional curricula and find themselves negotiating yet another cultural divide.
Glenn Regehr’s question is pertinent here:
What if their goal for themselves in our curriculum is to get through medical school as efficiently as possible and with the best record possible so they can get the residency of their choice and finally learn how to be a doctor?37
Are there curricular innovations that seem authentic to students, that help them to see the way forward, and which they believe will really help them prepare to be doctors? We probably do not yet have the answer to that question. What is clear, however, is that it may not be in the least bit obvious to the students how this new world is relevant to their vocational purpose – to becoming a doctor.
Independent learning requires experience in the domain. Experience provides a framework on which to build and direct future learning efforts. A novice lacks those frameworks. To quote Glenn Regehr again:
“Independent learning” is a luxury of the knowled geable […]. [students] must have a meaningful image of the “big picture” (G Regehr, Faculty of Medicine, The University of British Columbia, email communication, December, 2014).
The same themed issue of Medical Teacher that we mentioned above includes an article arguing for a curriculum that is precisely designed to enable students to construct meaning early by giving them that big picture – a “roadmap curriculum”.38 Perhaps that is a start.
Challenging the risk assumptions of health care provider organizations
If we succeed in supporting students’ developing maturity and independence, and if we can commission and develop clinical supervision that invites and supports appropriate, individualized student participation in practice, and if we can reimagine curricula that make the big picture transparent to students as early as possible, then there is still one obstacle. The health care provider settings where we would like our students to participate are highly risk-averse organizations. Consider the first two quotes from medical schools weighing up the implementation of student assistantships:20
[Concerns] mostly relate to areas where our teaching trusts are not yet happy to allow students to be involved in these processes.
Patient safety, care standards and trust risk assessment may preclude some elements.20
These quotes come from the UK context, but the emphasis on patient safety in all its forms is similar across the whole developed world. Few hospital boards welcome the idea that a learner will be participating in the care of their patients.
Interestingly, those patients do not share the view of their hospital boards. In ambulatory and hospital settings,39 and even in hospices,40 the overwhelming majority of patients in two surveys were strongly positive about medical students participating in their care. One patient statement was so commonly made that, quite independently, it became the title for both papers: “They’ve got to learn”.39,40
This statement is the essence of the case that health care provider boards have to understand. The medical students whose participation makes them anxious today are the junior doctors on whom they will depend for delivering care tomorrow. If they can create the right supervisory conditions for them today, they will both preserve patient safety and optimize learning and development. Through tomorrow’s doctors, they will reap the rewards. This is the risk argument that educators must win with health care providers.
Footnotes
Disclosure
The authors are not aware of any conflicts of interest arising from the publication of this manuscript.
References
- 1.General Medical Council . Tomorrow’s Doctors: Outcomes and Standards for Undergraduate Medical Education. Manchester, UK: General Medical Council; 2009. [Google Scholar]
- 2.Frank JR, Danoff D. The CanMEDS initiative: implementing an outcomes-based framework of physician competencies. Med Teach. 2007;29(7):642–647. doi: 10.1080/01421590701746983. [DOI] [PubMed] [Google Scholar]
- 3.AAMC Learning objectives for medical student education – guidelines for medical schools: report I of the Medical School Objectives Project. Acad Med. 1999;74(1):13–18. doi: 10.1097/00001888-199901000-00010. [DOI] [PubMed] [Google Scholar]
- 4.McClelland DC. Testing for competence rather than for “intelligence”. Am Psychol. 1973;28(1):1–14. doi: 10.1037/h0034092. [DOI] [PubMed] [Google Scholar]
- 5.McManus IC, Richards P, Winder BC, Sproston KA, Vincent CA. The changing clinical experience of British medical students. Lancet. 1993;341(8850):941–944. doi: 10.1016/0140-6736(93)91225-b. [DOI] [PubMed] [Google Scholar]
- 6.General Medical Council . Tomorrow’s Doctors: Recommendations on Undergraduate Medical Education. London: General Medical Council; 1993. [Google Scholar]
- 7.Smith R. All changed, changed utterly. Br Med J. 1998;316(7149):1917–1918. doi: 10.1136/bmj.316.7149.1917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kelly M, O’Flynn S, McLachlan J, Sawdon MA. The clinical conscientiousness index: a valid tool for exploring professionalism in the clinical undergraduate setting. Acad Med. 2012;87(9):1218–1224. doi: 10.1097/ACM.0b013e3182628499. [DOI] [PubMed] [Google Scholar]
- 9.Jen MH, Bottle A, Majeed A, Bell D, Aylin P. Early in-hospital mortality following trainee doctors’ first day at work. PLoS One. 2009;4(9):e7103. doi: 10.1371/journal.pone.0007103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hope J. ‘Killing season’ on NHS wards: Patients at risk when junior doctors start new jobs, says health boss. Daily Mail. 2012 Jun 22; [Google Scholar]
- 11.BMJ . In: You will Survive: BMJ’s Guide for Newly Qualified Doctors. 1st ed. BMJ, editor. London, UK: BMJ publishing; 2013. p. 2. chapter 2. [Google Scholar]
- 12.Medical students: electives. NHS: Medical careers; [Accessed May 20, 2015]. Available from: http://www.medicalcareers.nhs.uk/pdf.aspx?page=7322. [Google Scholar]
- 13.Remmen R, Denekens J, Scherpbier A, et al. An evaluation study of the didactic quality of clerkships. Med Educ. 2000;34(6):460–464. doi: 10.1046/j.1365-2923.2000.00570.x. [DOI] [PubMed] [Google Scholar]
- 14.Krajic Kachur E. Observation during early clinical exposure – an effective instructional tool or a bore? Med Educ. 2003;37(2):88–89. doi: 10.1046/j.1365-2923.2003.01421.x. [DOI] [PubMed] [Google Scholar]
- 15.Lave J, Wenger E. Situated Learning: Legitimate Peripheral Participation. Cambridge, UK/New York: Cambridge University Press; 1991. p. 138. [Google Scholar]
- 16.Dornan T, Boshuizen H, King N, Scherpbier A. Experience-based learning: a model linking the processes and outcomes of medical students’ workplace learning. Med Educ. 2007;41(1):84–91. doi: 10.1111/j.1365-2929.2006.02652.x. [DOI] [PubMed] [Google Scholar]
- 17.Crossley J, Vivekananda-Schmidt P. The development and evaluation of a professional self identity questionnaire to measure evolving professional self-identity in health and social care students. Med Teach. 2009;31(12):e603–e607. doi: 10.3109/01421590903193547. [DOI] [PubMed] [Google Scholar]
- 18.Kavanagh P, Boohan M, Savage M, McCluskey D, McKeown P. Evaluation of a final year work-shadowing attachment. Ulster Med J. 2012;81(2):83–88. [PMC free article] [PubMed] [Google Scholar]
- 19.Collins J. Foundation for Excellence: an Evaluation of the Foundation Programme. London, UK: Medical Education England; 2010. [Google Scholar]
- 20.Vivekananda-Schmidt P, Crossley J, Bax N. Student doctors taking responsibility. Clin Teach. 2011;8(4):267–271. doi: 10.1111/j.1743-498X.2011.00482.x. [DOI] [PubMed] [Google Scholar]
- 21.Tallentire VR, Smith SE, Cameron HS. Designing a purposeful student assistantship. Clin Teach. 2012;9(4):210–215. doi: 10.1111/j.1743-498X.2012.00553.x. [DOI] [PubMed] [Google Scholar]
- 22.General Medical Council . Clinical Placements for Medical Students: Advice Supplementary to Tomorrow’s Doctors (2009) London, UK: General Medical Council; 2011. [Google Scholar]
- 23.General Medical Council UK Medical Schools – Medical school reports. [Accessed May 27, 2015]. Available from: http://www.gmc-uk.org/education/26867.asp.
- 24.Monrouxe LV, Bullock A, Cole J, et al. How Prepared are UK Medical Graduates for Practice? Final report from a programme of research commissioned by the General Medical Council. [Accessed May 14, 2015]. Available from: http://www.gmc-uk.org/How_Prepared_are_UK_Medical_Graduates_for_Practice_SUBMITTED_Revised_140614.pdf_58034815.pdf.
- 25.General Medical Council . Be prepared: Are New Doctors Safe to Practise? London, UK: General Medical Council; 2014. [Google Scholar]
- 26.Baxter Magolda MB. Making Their Own Way: Narratives for Transforming Higher Education to Promote Self-Development. 1st ed. Sterling, VA: Stylus; 2001. p. xxiv.p. 356. [Google Scholar]
- 27.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 28.Sandars J, Patel R, Steele H, McAreavey M. Developmental student support in undergraduate medical education: AMEE Guide No 92. Med Teach. 2014;36(12):1015–1026. doi: 10.3109/0142159X.2014.917166. [DOI] [PubMed] [Google Scholar]
- 29.Kennedy TJ, Regehr G, Baker GR, Lingard L. Preserving professional credibility: grounded theory study of medical trainees’ requests for clinical support. BMJ. 2009;338:b128. doi: 10.1136/bmj.b128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Driessen EW, Overeem K, van der Vleuten CP. Get yourself a mentor. Med Educ. 2011;45(5):438–439. doi: 10.1111/j.1365-2923.2011.03948.x. [DOI] [PubMed] [Google Scholar]
- 31.Watling CJ. Unfulfilled promise, untapped potential: feedback at the crossroads. Med Teach. 2014;36(8):692–697. doi: 10.3109/0142159X.2014.889812. [DOI] [PubMed] [Google Scholar]
- 32.van Loon KA, Driessen EW, Teunissen PW, Scheele F. Experiences with EPAs, potential benefits and pitfalls. Med Teach. 2014;36(8):698–702. doi: 10.3109/0142159X.2014.909588. [DOI] [PubMed] [Google Scholar]
- 33.Wimmers PF, Schmidt HG, Splinter TA. Influence of clerkship experiences on clinical competence. Med Educ. 2006;40(5):450–458. doi: 10.1111/j.1365-2929.2006.02447.x. [DOI] [PubMed] [Google Scholar]
- 34.Crossley J. Do the supervision needs of ‘clerkship students’ change as they become more experienced? Med Educ. 2006;40:1053. doi: 10.1111/j.1365-2929.2006.02617.x. [DOI] [PubMed] [Google Scholar]
- 35.Biggs J. Enhancing teaching through constructive alignment. High Educ. 1996;32(3):347–364. [Google Scholar]
- 36.Brauer DG, Ferguson KJ. The integrated curriculum in medical education: AMEE Guide No 96. Med Teach. 2014;36:1–11. doi: 10.3109/0142159X.2014.970998. [DOI] [PubMed] [Google Scholar]
- 37.Regehr G. It’s NOT rocket science: rethinking our metaphors for research in health professions education. Med Educ. 2010;44(1):31–39. doi: 10.1111/j.1365-2923.2009.03418.x. [DOI] [PubMed] [Google Scholar]
- 38.Crossley JG. Addressing learner disorientation: give them a roadmap. Med Teach. 2014;36(8):685–691. doi: 10.3109/0142159X.2014.889813. [DOI] [PubMed] [Google Scholar]
- 39.Ashley P, Rhodes N, Sari-Kouzel H, Mukherjee A, Dornan T. ‘They’ve all got to learn’. Medical students’ learning from patients in ambulatory (outpatient and general practice) consultations. Med Teach. 2009;31(2):e24–e31. doi: 10.1080/01421590802464445. [DOI] [PubMed] [Google Scholar]
- 40.Arolker M, Barnes J, Gadoud A, Jones L, Barnes L, Johnson MJ. ‘They’ve got to learn’ – a qualitative study exploring the views of patients and staff regarding medical student teaching in a hospice. Palliat Med. 2010;24(4):419–426. doi: 10.1177/0269216310366065. [DOI] [PubMed] [Google Scholar]


