Abstract
Mobility and function are important predictors of survival. However, their combined impact on mortality in adults ≥65 years of age with heart failure (HF) is not well understood. This study examined the role of gait speed and instrumental activities of daily living (IADL) in all-cause mortality in a cohort of 1,119 community-dwelling Cardiovascular Health Study participants ≥65 years of age with incident HF. Data on HF and mortality were collected through annual examinations or contact during the 10-year follow-up period. Slower gait speed (<0.8m/s vs. ≥0.8m/s) and IADL impairment (≥1 vs. 0 areas of dependence) were determined from baseline and follow-up assessments. A total of 740 (66%) of the 1119 participants died during the follow-up period. Multivariate Cox proportional hazards models showed that impairments in either gait speed (hazard ratio 1.37, 95% CI 1.10-1.70; p=0.004) or IADL (HR 1.56, 95% CI 1.29-1.89; p<0.001), measured within 1 year before the diagnosis of incident HF, were independently associated with mortality, adjusting for socio-demographic and clinical characteristics. The combined presence of slower gait speed and IADL impairment was associated with a greater risk of mortality and suggested an additive relationship between gait speed and IADL. In conclusion, gait speed and IADL are important risk factors for mortality in adults ≥65 years of age with HF, but the combined impairments of both gait speed and IADL can have an especially important impact on mortality.
Keywords: Gait speed, IADL, Geriatrics, Heart failure, Mortality
Introduction
Gait speed is an important predictor of mortality,1-3 hospitalization3 and nursing home placement4 in adults 65 years and older, as well as disability5 and mortality6,7 in individuals with cardiovascular disease in particular. A related measure, the 6-minute walk distance is a prognostic marker of mortality in heart failure (HF).8-10 Impairment in gait speed often occurs in the setting of impairments in other geriatric measures, for example, in conjunction with deficits in lower extremity strength and balance as measured by the Short Physical Performance Battery (SPPB),4,11,12 or as a component of frailty in HF.13-15 Instrumental activities of daily living (IADL) is another important geriatric measure in HF given its association with HF incidence and mortality in adults ≥65 years of age.16 Of the available measures of mobility or function, gait speed and IADL are quick and reliable17,18 and may serve as screening tools in the clinical setting to identify adults with HF at increased risk for adverse outcomes. We therefore investigated the impact of gait speed and IADL, separately and combined, on all-cause mortality in adults with incident HF who are ≥65 years of age.
Methods
The Cardiovascular Health Study (CHS) is a prospective, population-based observational cohort study of cardiovascular disease and cardiovascular risk factors in community-dwelling United States adults ≥65 years of age.19 An initial cohort of 5,201 participants was recruited in 1989-1990 and a second cohort of 687 African-Americans was recruited in 1992-1993. All participants underwent health evaluations per standardized protocols, and details of the CHS study methodology including variables collected have been published elsewhere.19,20 There were 1,139 CHS participants ≥65 years of age without prevalent HF at enrollment and who were diagnosed with incident HF during the study. Of these, 1,119 had complete gait speed and IADL data and were included in the current study.
Variables analyzed in this study included socio-demographic characteristics (age, gender, race, marital status, education, income) and past medical history (general health, smoking history, myocardial infarction, coronary artery disease, hypertension, diabetes mellitus, stroke, chronic obstructive pulmonary disease, cancer, kidney disease, depression as measured with the Center for Epidemiologic Studies Depression Scale, and cognitive status as measured by the Mini-Mental State Examination score) collected at baseline. Time to walk 15 feet and IADL were collected at baseline and at annual follow-up assessments. We converted the time to walk 15 feet into gait speed in meters per second and dichotomized into slower (or impaired) (<0.8 m/s) or normal (≥0.8 m/s) based on prior studies.6,21 We defined IADL impairment as dependence in one or more categories among the 8 activity categories. Gait speed measurements were collected from Year 3 (which was the first year of follow-up) through Year 11, but not in Year 10. IADL was measured from Year 3 through Year 11. Of the 1,119 participants meeting inclusion criteria for this study, we identified 815 (73%) participants whose diagnosis of incident HF was at Year 12 or earlier. This subset represented those participants who had either a gait speed or IADL assessment scheduled within one year of their incident HF diagnosis, since neither gait speed nor IADL was assessed beyond Year 11. Among these 815, a total of 606 (74%) had a completed gait speed measurement and 690 (85%) had a completed IADL assessments within 1 year prior to incident HF diagnosis.
Incident HF was diagnosed by central-adjudication by the CHS Events Committee.22 The primary outcome of interest was all-cause mortality, which was adjudicated by reviewing death certificates, autopsy reports, hospital records and interviews with attending physicians, next-of-kin, and witnesses.19
We analyzed cross-sectional associations between socio-demographic and clinical characteristics, and gait speed and IADL, respectively, using chi-square and t-tests. We examined the associations between (1) gait speed impairment and (2) IADL impairment, and all-cause mortality using Cox proportional hazard survival models. Separate models were created for both gait speed and IADL using measurements at baseline and within 1 year of incident HF diagnosis. We further stratified individuals into those with and without preserved ejection fraction (EF) for separate survival analyses. Only 89% of the 1,119 participants had an EF recorded at baseline: 862 (86%) had EF ≥55%, 77 (8%) had EF 45-54% and 60 (6%) had EF <45%. All African-American CHS participants were recruited after the baseline echocardiogram. A second echocardiogram at year 7 was recorded for 687 (61%) of the 1,119; excluding those who died or were lost to follow-up. Among these, 526 (77%) had EF ≥55%, 94 (14%) had EF 45-54% and 68 (10%) had EF <45%. Only 618 participants had EF measurements at baseline and year 7. As the CHS EF categories (≥55% “normal”; 45-54% “mildly reduced” and <45% “moderately or severely reduced”)23 are not concordant with the 2013 American Heart Association guideline EF classifications (≥50% “preserved”; 41-49% “borderline”; ≤40% “reduced” and >40% with previous reduced EF “improved”),24 we incorporated both classifications for this study and defined preserved EF to include any of following criteria: (a) EF ≥55% at Year 7; or (b) EF ≥45% at Year 7 and EF ≥45% at baseline (to exclude individuals with AHA-classified “improved EF”); or (c) EF ≥45% at baseline and died or lost to follow-up before Year 7. Those with EF <45% were defined as “reduced EF”, but their numbers were too small to obtain a meaningful estimate in the Cox model, and so those with no recorded EF were included in this reference group.
We also performed a sensitivity analysis on the subset of participants who did not have impairment with regards to either gait speed or IADL at baseline, in order to examine the impact of acute impairment of gait speed, IADL and both factors combined, in the follow-up period.
Hazard ratios (HR) and 95% confidence intervals (CIs) were used to describe the statistical associations. All statistical tests were 2-tailed, with a p-value <0.05 considered significant. Data analyses were conducted using SPSS statistics software version 21 (IBM Corporation, Somers, NY) and Stata v.12.1 (Stata, Inc. College Station, TX).
Results
The mean age at enrollment for eligible participants in this study was 74 (standard deviation ±6) years, 51% were female and 14% were non-white. The median gait speed at baseline was 0.76 m/s with an inter-quartile range of 0.65-0.91 m/s, and 566 (51%) had a gait speed <0.8 m/s. Males had a significantly faster mean gait speed (0.87 m/s) than females (0.78 m/s; p<0.001). Among the 1,119 participants, 780 (68%) reported no IADL impairments, 270 (24%) reported one and 89 (8%) reported 2 or more impairments. Slower gait speed was positively correlated with age, female sex, non-white race, fewer years of education and lower income, while IADL impairment was more likely to be positively correlated with a number of medical conditions (Table 1).
Table 1.
Baseline characteristics of patients with incident heart failure by instrumental activities of daily living (IADL) impairment and by gait speed impairment.
| Number (%) or mean (±SD) | IADL | P-valuea | Gait Speedb | P-valuea | |||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| IADL=0 (n=780) |
IADL ≥1 (n=359) |
≥ 0.8 m/s (n=553) |
< 0.8 m/s (n=566) |
||||
| Age at study entry (years) | 74 (±6) | 76 (±6) | <0.001 | 73 (±5) | 76 (±6) | <0.001 | |
| Age at the time of incident HF | 81 (±6) | 82 (±4) | 0.04 | 80 (±6) | 82 (±6) | <0.001 | |
| Female | 361 (46%) | 224 (62%) | <0.001 | 224 (41%) | 345 (61%) | <0.001 | |
| Non-white race | 99 (13%) | 64 (18%) | 0.02 | 56 (10%) | 101 (18%) | <0.001 | |
| Married | 513 (66%) | 221 (62%) | 0.18 | 396 (72%) | 328 (58%) | <0.001 | |
| Education (college or higher) | 325 (42%) | 133 (37%) | 0.15 | 264 (48%) | 186 (33%) | <0.001 | |
| Income > $25,000 | 254 (33%) | 99 (28%) | 0.09 | 206 (37%) | 141 (25%) | <0.001 | |
| General health fair to poor | 185 (24%) | 176 (49%) | <0.001 | 125 (23%) | 235 (41%) | <0.001 | |
| Smoking (pack years) | 20 (±28) | 18 (±28) | 0.31 | 17 (±27) | 22 (±28) | 0.002 | |
| Myocardial Infarction | 109 (149%) | 69 (19%) | 0.02 | 94 (17%) | 82 (14%) | 0.25 | |
| Coronary artery disease | 198 (25%) | 126 (35%) | 0.001 | 170 (31%) | 149 (26%) | 0.10 | |
| Hypertension | 421 (54%) | 214 (60%) | 0.08 | 301 (54%) | 324 (57%) | 0.34 | |
| Diabetes mellitus | 187 (24%) | 85 (24%) | 0.90 | 125 (23%) | 142 (25%) | 0.33 | |
| Stroke | 35 (5%) | 27 (8%) | 0.05 | 27 (5%) | 45 (8%) | 0.11 | |
| Chronic obstructive pulmonary disease | 90 (11%) | 74 (21%) | <0.001 | 76 (14%) | 86 (15%) | 0.49 | |
| Cancer | 108 (14%) | 62 (17%) | 0.13 | 90 (16%) | 77 (14%) | 0.21 | |
| Kidney disease | 192 (25%) | 114 (32%) | 0.01 | 138 (25%) | 165 (29%) | 0.11 | |
| Depression score | 4.1 (±4.1) | 6.4 (±5.1) | <0.001 | 3.9 (±3.9) | 5.7 (±5.0) | <0.001 | |
| Mini Mental State Examination score | 28 (±2) | 27 (±3) | 0.001 | 28 (±2) | 27 (±3) | <0.001 | |
P-values are calculated using Pearson Chi-Square tests of association for categorical variables and F tests of equal means for continuous variables.
Twenty participants had missing gait speed data.
Overall, 740 (66%) of the 1,119 participants died. The median time from enrollment to incident HF was 6.4 years and the median time from incident HF to death was 1.7 years. Slower gait speed and IADL impairment, whether assessed at baseline or within 1 year of incident HF, was each independently associated with all-cause mortality (Table 2). The adjusted hazard ratio for IADL was substantially greater, while that for gait speed did not differ meaningfully, for models utilizing assessments within 1e year of incident HF. (Table 2). There was no meaningful difference observed in our stratified analysis of the impact of gait speed in females (HR 1.38, 95% CI 1.09-1.75; p=0.009) and males (HR 1.22, 95% CI 0.99-1.51; p=0.08). Analysis using quartiles of gait speed did not demonstrate a dose-response effect of gait speed on all-cause mortality (Figure 1).
Table 2. Crude and adjusteda models for the effect of gait speed and instrumental activities of daily living (IADL) on all-cause mortality.
| Variables Measured at Baseline (N=1,119) | Variables Measured within One Year of Incident HF (N=606) | |||
|---|---|---|---|---|
|
| ||||
| Model | Hazard Ratio (95% CI) | P-Value | Hazard Ratio (95% CI) | P-Value |
| Gait Speed Impairment (<0.8 m/s vs ≥0.8 m/s) | ||||
| Unadjusted Model | 1.45 (1.25-1.68) | <0.001 | 1.57 (1.29-1.91) | <0.001 |
| Adjusted (all with incident HF) | 1.28 (1.10-1.50) | 0.002 | 1.37 (1.10-1.70) | 0.004 |
| Adjusted (those with preserved ejection fractionb) | 1.36 (1.12-1.65) | 0.002 | 1.45 (1.12-1.86) | 0.004 |
| Adjusted (those with reduced ejection fractionc) | 1.14 (0.87-1.50) | 0.4 | 1.51 (0.98-2.32) | 0.06 |
| IADL Impairment (≥1 Impairments vs. None) | ||||
| Unadjusted Model | 1.23 (1.06-1.43) | 0.006 | 1.69 (1.41-2.02) | <0.001 |
| Adjusted (all with incident HF) | 1.18 (1.01-1.39) | 0.04 | 1.56 (1.29-1.89) | <0.001 |
| Adjusted (those with preserved ejection fractionb) | 1.14 (0.93-1.39) | 0.2 | 1.55 (1.23-1.95) | <0.001 |
| Adjusted (those with reduced ejection fractionc) | 1.28 (0.96-1.69) | 0.09 | 1.53 (1.07-2.20) | 0.02 |
Potential confounding factors included: Age at incident HF, gender (female vs. male), race (non-white vs. white), marital status (married vs. not), education (any college or higher), and income (>$25,000 vs. not), depression score, Mini Mental State Examination Score, hypertension, coronary artery disease, and chronic kidney disease, as determined at study entry.
Sample size for individuals with preserved ejection fraction were 756 (68%) for baseline model and 427 (70%) for the one year prior to HF model.
Sample size for individuals with reduced/unknown ejection fraction were 363 (32%) for baseline model and 179 (30%) for the one year prior to HF model.
Figure 1. Adjusted hazard ratios for all-cause mortality by increasing impairment, based on quartiles of gait speed.
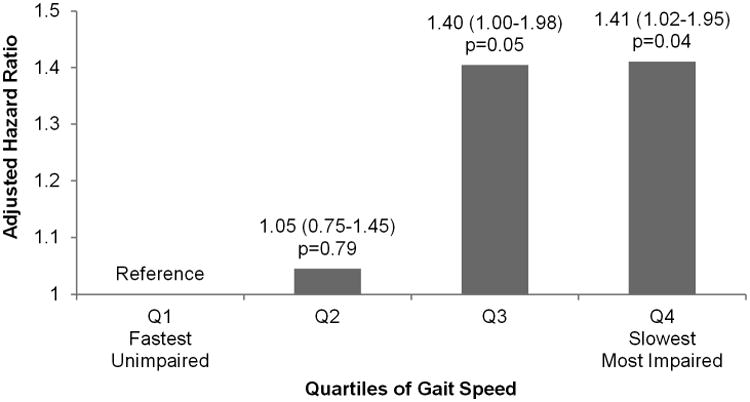
Gait speed measured within one year prior to incident heart failure (HF) in meters per second. Adjusted for age at incident HF, gender (female vs. male), race (non-white vs. white), marital status (married vs. not), education (any college or higher vs. high school graduate or less), and income (>$25,000 vs. not), depression score, Mini Mental State Examination Score, hypertension, coronary artery disease, and chronic kidney disease.
Stratification by ejection fraction showed no significant differences in the effect estimates for gait speed or IADL in individuals with preserved versus reduced EF, but the results were not statistically significant among those with reduced EF due to the small sample size.
A sensitivity analysis of both gait speed and IADL, as measured within 1 year prior to incident HF and restricted to individuals without impairments in either measure at baseline, found only a significantly increased hazard of mortality when impairments in both gait speed and IADL were present (Table 3).
Table 3.
Multivariate survival analysis of the association between gait speed and instrumental activity of daily living (IADL), both measured within one year of HF, and all-cause mortality, restricted to individuals without impairment in either gait speed or IADL at baseline.
| IADL Impairmenta | IADL Impairmenta | |||
|---|---|---|---|---|
|
| ||||
| Dead/Total (%) | Adjustedc Hazard Ratio (95% CI) | |||
|
| ||||
| No (N =151) | Yes (N =65) | No | Yes | |
| Gait Speed Impairmentb | ||||
| No (N = 147) | 67/116 (58%) |
19/31 (61%) |
Reference | 1.30 (0.77-2.20) p=0.33 |
| Yes (N = 69) | 23/35 (66%) |
23/34 (68%) |
1.57 (0.93-2.66) p=0.09 |
1.87 (1.10-3.19) p=0.02 |
IADL impairment is defined as dependence (i.e., impairment) with ≥1 areas of IADL.
Gait speed impairment is defined as a walking speed of <0.8 m/s.
Adjusted for age at incident HF, gender (female vs. male), race (non-white vs. white), marital status (married vs. not), education (any college or higher vs. high school graduate or less), and income (>$25,000 vs. not), depression score, Mini Mental State Examination Score, hypertension, coronary artery disease, and chronic kidney disease, as determined at study entry.
Discussion
This study demonstrates that slower gait speed and IADL impairment are important risk factors for all-cause mortality in adults ≥65 years of age with HF, and that the impact on mortality is greater when both impairments coexist than in the presence of either alone. Our results also show that although other sociodemographic and clinical risk factors for mortality in HF may be associated with mortality in this cohort, none of these variables significantly confounded the association with either gait speed or IADL, as evidenced by the lack of a difference in the crude and adjusted hazard ratios. The observed relationship between gait speed and mortality in this study is supported by previous reports on the prognostic role of gait speed on mortality, whether described alone1,3 or as part of composite measures, such as the SPPB4,11 and frailty.25 Although the relationship was not described in a specific cohort of HF patients, many of the participants in those cohort studies had cardiovascular disease.1 However, the prognostic role of the 6-minute walk distance on mortality has been specifically reported in HF patients in different cohorts.8-10 Our findings add to the body of evidence by characterizing the role of gait speed at or around the time of HF diagnosis and by clarifying its relationship with IADL. It also demonstrates the prognostic role of gait speed in adults ≥65 years of age with HF and preserved EF.
Although gait speed and IADL may change over time, our analysis demonstrated similar risk relationships between gait speed and mortality, and between IADL and mortality, whether using gait speed or IADL assessed at baseline or closer to the time of incident HF. Importantly, gait speed was less likely to change over time than IADL, and the adjusted HR estimates for gait speed were more consistent across models using either baseline or follow-up gait speed, supporting the notion that gait speed may be a more robust predictor of mortality over time.
Both gait speed and IADL predict functional decline26 and mortality,1 but perhaps gait speed is a more sensitive marker of comorbidity and deterioration. Gait speed is more than a simple measure of lower extremity function and has been described as a measure of overall health and physiological reserve in older adults.27 However, it is unclear if the mechanism through which gait speed impacts mortality in HF is a direct one, or through an intermediate conditions, namely frailty.28 While gait speed impairment can be found in pre-frailty states,29 it is unclear if gait speed is a precursor state or an early metric for frailty. Nonetheless, gait speed is more objective than IADL as it is actually measured, while IADL relies on self-report by study participants.19 Additionally, the data in CHS did not allow the determination of which individual IADL was impaired,16 as opposed to gait speed, which serves as an objective assessment of functional status.4 IADL may also be less susceptible to some actual declines in function, for example, using a microwave to prepare frozen meals when one begins losing the physical ability to prepare fresh food prevents identification of the loss in dexterity.
Bowling, et al. showed that IADL predicted HF incidence and all-cause mortality in the same cohort and postulated that IADL indicated difficulties with complex function that adversely affected medication compliance and hindered other healthy practices that ultimately led to increased risk of disease or mortality.16 Perhaps gait speed offers a more accurate metric of the person's underlying overall state of well-being, and IADL is simply the symptomatic manifestation resulting from any insults to this underlying state. Therefore, one could argue that gait speed is superior to IADL in terms of measuring function or mobility, and is a more appropriate indicator for any intervention aimed at preserving mobility.
This study has several limitations. Since time must elapse between baseline and incident HF, it is reasonable to assume that baseline measures may not reflect what these same measures would be at the time of incident HF. We minimized potential misclassification due to changes in either gait speed or IADL in this study with our analysis using only assessments of gait speed and IADL that were within 1 year of the diagnosis of incident HF. IADL data was self-reported and susceptible to misclassification. Data on individual IADLs were not available, thereby limiting our ability to clarify which specific IADL might be associated with outcome.
The sensitivity analyses excluded prevalent cases of impairment involving either gait speed or IADL and provided a subgroup of participants in whom we could investigate the impact of acute impairment. The result of the sensitivity analysis strengthens the findings observed in the larger cohort.
Our results underscore the importance of gait speed on mortality in adults ≥65 years of age with HF. Efforts aimed at improving outcomes and reducing mortality should focus on measures of mobility and function, such as gait speed and IADL respectively, that may serve as useful screening tools in the clinical setting to identify individuals ≥65 years of age with HF who are at increased risk of adverse outcome and who may benefit from interventions aimed at preserving mobility and function.
Acknowledgments
Dr. Brown is supported by a Veterans Administration Rehabilitation Scientific Merit Award (E7036R) and by grants R01 AG16062 and 5UL1 RR025777 from the National Institutes of Health. Dr. Ahmed is supported in part by the NIH through grants (R01-HL085561, R01-HL085561-S and R01-HL097047) from the NHLBI. Mr. Donnelly is supported by a grant from the Agency for Healthcare Research and Quality (T32 HS013852). Dr. Lo is supported by the University of Alabama at Birmingham Lister Hill Center for Health Policy, and the John A. Hartford Foundation. The funding agencies had no role in the design, methods, participant recruitment, data collections, analysis and preparation of the manuscript.
Footnotes
Disclosures: The authors have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, Brach J, Chandler J, Cawthon P, Connor EB, Nevitt M, Visser M, Kritchevsky S, Badinelli S, Harris T, Newman AB, Cauley J, Ferrucci L, Guralnik J. Gait speed and survival in older adults. JAMA. 2011;305:50–58. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ostir GV, Kuo YF, Berges IM, Markides KS, Ottenbacher KJ. Measures of lower body function and risk of mortality over 7 years of follow-up. Am J Epidemiol. 2007;166:599–605. doi: 10.1093/aje/kwm121. [DOI] [PubMed] [Google Scholar]
- 3.Cesari M, Kritchevsky SB, Penninx BW, Nicklas BJ, Simonsick EM, Newman AB, Tylavsky FA, Brach JS, Satterfield S, Bauer DC, Visser M, Rubin SM, Harris TB, Pahor M. Prognostic value of usual gait speed in well-functioning older people--results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005;53:1675–1680. doi: 10.1111/j.1532-5415.2005.53501.x. [DOI] [PubMed] [Google Scholar]
- 4.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Scherr PA, Wallace RB. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 5.Chaudhry SI, McAvay G, Ning Y, Allore HG, Newman AB, Gill TM. Risk factors for onset of disability among older persons newly diagnosed with heart failure: the Cardiovascular Health Study. J Card Fail. 2011;17:764–770. doi: 10.1016/j.cardfail.2011.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Afilalo J, Eisenberg MJ, Morin JF, Bergman H, Monette J, Noiseux N, Perrault LP, Alexander KP, Langlois Y, Dendukuri N, Chamoun P, Kasparian G, Robichaud S, Gharacholou SM, Boivin JF. Gait speed as an incremental predictor of mortality and major morbidity in elderly patients undergoing cardiac surgery. J Am Coll Cardiol. 2010;56:1668–1676. doi: 10.1016/j.jacc.2010.06.039. [DOI] [PubMed] [Google Scholar]
- 7.Dumurgier J, Elbaz A, Ducimetiere P, Tavernier B, Alperovitch A, Tzourio C. Slow walking speed and cardiovascular death in well functioning older adults: prospective cohort study. BMJ. 2009;339:b4460. doi: 10.1136/bmj.b4460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bittner V, Weiner DH, Yusuf S, Rogers WJ, McIntyre KM, Bangdiwala SI, Kronenberg MW, Kostis JB, Kohn RM, Guillotte M, Greenberg B, Woods PA, Bourassa MG. Prediction of mortality and morbidity with a 6-minute walk test in patients with left ventricular dysfunction. SOLVD Investigators. JAMA. 1993;270:1702–1707. [PubMed] [Google Scholar]
- 9.Ingle L, Rigby AS, Carroll S, Butterly R, King RF, Cooke CB, Cleland JG, Clark AL. Prognostic value of the 6 min walk test and self-perceived symptom severity in older patients with chronic heart failure. Eur Heart J. 2007;28:560–568. doi: 10.1093/eurheartj/ehl527. [DOI] [PubMed] [Google Scholar]
- 10.Forman DE, Fleg JL, Kitzman DW, Brawner CA, Swank AM, McKelvie RS, Clare RM, Ellis SJ, Dunlap ME, Bittner V. 6-min walk test provides prognostic utility comparable to cardiopulmonary exercise testing in ambulatory outpatients with systolic heart failure. J Am Coll Cardiol. 2012;60:2653–2661. doi: 10.1016/j.jacc.2012.08.1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Volpato S, Cavalieri M, Sioulis F, Guerra G, Maraldi C, Zuliani G, Fellin R, Guralnik JM. Predictive value of the Short Physical Performance Battery following hospitalization in older patients. J Gerontol A Biol Sci Med Sci. 2011;66:89–96. doi: 10.1093/gerona/glq167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fox KR, Ku PW, Hillsdon M, Davis MG, Simmonds BA, Thompson JL, Stathi A, Gray SF, Sharp DJ, Coulson JC. Objectively assessed physical activity and lower limb function and prospective associations with mortality and newly diagnosed disease in UK older adults: an OPAL four-year follow-up study. Age Ageing. 2014 doi: 10.1093/ageing/afu168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Afilalo J. Frailty in Patients with Cardiovascular Disease: Why, When, and How to Measure. Curr Cardiovasc Risk Rep. 2011;5:467–472. doi: 10.1007/s12170-011-0186-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fried LP, Kronmal RA, Newman AB, Bild DE, Mittelmark MB, Polak JF, Robbins JA, Gardin JM. Risk factors for 5-year mortality in older adults: the Cardiovascular Health Study. JAMA. 1998;279:585–592. doi: 10.1001/jama.279.8.585. [DOI] [PubMed] [Google Scholar]
- 15.Khan H, Kalogeropoulos AP, Georgiopoulou VV, Newman AB, Harris TB, Rodondi N, Bauer DC, Kritchevsky SB, Butler J. Frailty and risk for heart failure in older adults: the health, aging, and body composition study. Am Heart J. 2013;166:887–894. doi: 10.1016/j.ahj.2013.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bowling CB, Fonarow GC, Patel K, Zhang Y, Feller MA, Sui X, Blair SN, Alagiakrishnan K, Aban IB, Love TE, Allman RM, Ahmed A. Impairment of activities of daily living and incident heart failure in community-dwelling older adults. Eur J Heart Fail. 2012;14:581–587. doi: 10.1093/eurjhf/hfs034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, Studenski S, Berkman LF, Wallace RB. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55:M221–231. doi: 10.1093/gerona/55.4.m221. [DOI] [PubMed] [Google Scholar]
- 18.Katz S. Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc. 1983;31:721–727. doi: 10.1111/j.1532-5415.1983.tb03391.x. [DOI] [PubMed] [Google Scholar]
- 19.Fried LP, Borhani NO, Enright P, Furberg CD, Gardin JM, Kronmal RA, Kuller LH, Manolio TA, Mittelmark MB, Newman A, O'Leary DH, Psaty B, Rautaharju P, Tracy RP, Weiler PG. The Cardiovascular Health Study: design and rationale. Ann Epidemiol. 1991;1:263–276. doi: 10.1016/1047-2797(91)90005-w. [DOI] [PubMed] [Google Scholar]
- 20.Arnold AM, Psaty BM, Kuller LH, Burke GL, Manolio TA, Fried LP, Robbins JA, Kronmal RA. Incidence of cardiovascular disease in older Americans: the cardiovascular health study. J Am Geriatr Soc. 2005;53:211–218. doi: 10.1111/j.1532-5415.2005.53105.x. [DOI] [PubMed] [Google Scholar]
- 21.Fritz S, Lusardi M. White paper: “walking speed: the sixth vital sign”. J Geriatr Phys Ther. 2009;32:46–49. [PubMed] [Google Scholar]
- 22.Schellenbaum GD, Heckbert SR, Smith NL, Rea TD, Lumley T, Kitzman DW, Roger VL, Taylor HA, Psaty BM. Congestive heart failure incidence and prognosis: case identification using central adjudication versus hospital discharge diagnoses. Ann Epidemiol. 2006;16:115–122. doi: 10.1016/j.annepidem.2005.02.012. [DOI] [PubMed] [Google Scholar]
- 23.Kitzman DW, Gardin JM, Gottdiener JS, Arnold A, Boineau R, Aurigemma G, Marino EK, Lyles M, Cushman M, Enright PL Cardiovascular Health Study Research G. Importance of heart failure with preserved systolic function in patients > or = 65 years of age. CHS Research Group. Cardiovascular Health Study. Am J Cardiol. 2001;87:413–419. doi: 10.1016/s0002-9149(00)01393-x. [DOI] [PubMed] [Google Scholar]
- 24.Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL. 2013 ACCF/AHA guideline for the management of heart failure: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:1810–1852. doi: 10.1161/CIR.0b013e31829e8807. [DOI] [PubMed] [Google Scholar]
- 25.Cacciatore F, Abete P, Mazzella F, Viati L, Della Morte D, D'Ambrosio D, Gargiulo G, Testa G, Santis D, Galizia G, Ferrara N, Rengo F. Frailty predicts long-term mortality in elderly subjects with chronic heart failure. Eur J Clin Invest. 2005;35:723–730. doi: 10.1111/j.1365-2362.2005.01572.x. [DOI] [PubMed] [Google Scholar]
- 26.Brach JS, Perera S, VanSwearingen JM, Hile ES, Wert DM, Studenski SA. Challenging gait conditions predict 1-year decline in gait speed in older adults with apparently normal gait. Phys Ther. 2011;91:1857–1864. doi: 10.2522/ptj.20100387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cesari M. Role of gait speed in the assessment of older patients. JAMA. 2011;305:93–94. doi: 10.1001/jama.2010.1970. [DOI] [PubMed] [Google Scholar]
- 28.von Haehling S, Anker SD, Doehner W, Morley JE, Vellas B. Frailty and heart disease. Int J Cardiol. 2013;168:1745–1747. doi: 10.1016/j.ijcard.2013.07.068. [DOI] [PubMed] [Google Scholar]
- 29.Morley JE, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R, Cesari M, Chumlea WC, Doehner W, Evans J, Fried LP, Guralnik JM, Katz PR, Malmstrom TK, McCarter RJ, Gutierrez Robledo LM, Rockwood K, von Haehling S, Vandewoude MF, Walston J. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14:392–397. doi: 10.1016/j.jamda.2013.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]


