Abstract
Background
The role of fluorodeoxyglucose (FDG) positron emission tomography (PET/CT) scanning in operable pancreas cancer is unclear. We, therefore, wanted to investigate the impact of PET/CT on management, by incorporating it into routine work-up.
Methods
This was a single-institution prospective study. Patients with suspected and potentially operable pancreas, distal bile duct or ampullary carcinomas underwent PET/CT in addition to routine work-up. The frequency that PET/CT changed the treatment plan or prompted other investigations was determined. The distribution of standard uptake values (SUV) among primary tumours, and adjacent to biliary stents was characterised.
Results
Fifty-six patients were recruited. The surgical plan was abandoned in 9 (16%; 95% CI: 6–26) patients as a result of PET/CT identified metastases. In four patients, metastases were missed and seven were inoperable at surgery, not predicted by PET/CT. Unexpected FDG uptake resulted in seven additional investigations, of which two were useful. Among primary pancreatic cancers, a median SUV was 4.9 (range 2–12.1). SUV was highest around the biliary stent in 17 out of 28 cases. PET/CT detected metastases in five patients whose primary pancreatic tumours demonstrated mild to moderate avidity (SUV < 5).
Conclusions
PET/CT in potentially operable pancreas cancer has limitations. However, as a result of its ability to detect metastases, PET/CT scanning is a useful tool in the selection of such patients for surgery.
Introduction
Adenocarcinoma of the pancreas is a highly malignant disease with a poor prognosis. Currently, in Australia, around 2500 people are diagnosed annually representing around 2.5% of all non-cutaneous cancers. The incidence rate is higher in males than females (1.3:1) and has been approximately stable (12 cases per 100 000 males) from 1980 to 20101. Absolute numbers of patients diagnosed are progressively rising, mainly as a result of an ageing population as well as population growth.
The majority of patients have advanced disease at diagnosis, are treated with palliative intent chemotherapy and/or radiotherapy and have a median survival time measured in months. For the 20% of patients with operable disease, surgery usually involves a Whipple's procedure that carries a morbidity risk and may be associated with a prolonged recovery time. In prospective clinical trials, only around 10–20% of such patients are alive and cancer free 2 years after surgery, with 6 months of adjuvant gemcitabine or 5-fluorouracil associated with a modest survival benefit.2,3
In view of the risks associated with major surgery and the high relapse rate, methods to better select patients most likely to benefit from such curative intent treatment are needed.
Currently, operability assessment is based on high-quality multi-phase CT scanning to assess the tumour relationship with major vascular structures and to look for metastatic disease. Other investigations such as endoscopic ultrasound, ERCP, MRI and laparoscopy are utilized in selected patients. FDG–PET is an established staging tool in many tumours such as non-small cell lung cancer, oesophageal cancer and melanoma,4 where it facilitates more accurate staging, resulting in a proportion of patients being spared futile surgery. The addition of contemporaneous non-enhanced CT (PET/CT) scanning facilitates anatomical localization with resultant increased diagnostic accuracy.5,6 However, the role of PET/CT in staging pancreas cancer is less well defined.7 We postulated that PET/CT may be of a similar clinical value in operable pancreas cancer patients. We also considered PET/CT may detect unrelated and possibly less relevant pathology leading to additional, potentially unnecessary, investigations.8
Tumours resulting from primary pancreatic adenocarcinomas may largely consist of fibrotic stroma rather than malignant cells, and this may impact on their FDG avidity. There are few data detailing the SUV of primary pancreatic adenocarcinomas. Moreover, inflammation is a well-recognized, non-malignant, cause of FDG uptake. We hypothesized that biliary stents might induce an inflammatory response that might result in FDG uptake and confound the interpretation of the scan.
The primary objective of this study was to assess the impact of PET/CT on management decisions, when added to the standard work-up of patients with resectable, pancreas or peri-ampullary cancers. Secondary objectives were to define the FDG avidity of primary pancreatic neoplasms and around indwelling biliary stents (as measured by maximum SUV).
Patients and methods
Study design
This was a prospective, single-institution, observational, cohort study. This manuscript was written with reference to the Strengthening the Reporting of Observational Studies in Clinical Epidemiology (STROBE) statement.9
Patients were recruited between March 2008 and December 2012. All patients referred to the Royal Brisbane and Women's Hospital with a diagnosis of pancreatic cancer received standard work-up consisting of a contrast-enhanced, dual-phase CT scan of the chest, abdomen and pelvis. Other investigations/procedures were performed as deemed clinically appropriate, including ERCP, biliary stenting, Primovist enhanced MRI, endoscopic ultrasound and laparoscopy. Results of these investigations were discussed, and a management plan documented, at a multidisciplinary team (MDT) meeting consisting of hepatobiliary surgeons, medical and radiation oncologists, interventional and diagnostic radiologists and gastroenterologists.
Eligible patients for this study had a clinical diagnosis of resectable pancreas, ampullary or distal bile duct adenocarcinoma, with or without biopsy confirmation, who were fit for, and planned to undergo, surgical resection. Resectability was defined using the criteria of Katz/Varadhachary.10 As such, a normal tissue plane was required between the tumour and the superior mesenteric, coeliac and common hepatic arteries. Surrounding (peri-pancreatic) lymphadenopathy was allowed if the surgeons felt this would be within the resection field. Patients with either no evidence of metastatic disease or indeterminate findings on standard work-up were eligible. Patients were excluded if they had a confirmed or suspected diagnosis of a pancreatic neuroendocrine tumour, would not be available for post-operative follow-up or if they had any contraindications to undergoing a PET/CT scan, such as uncontrolled diabetes. After discussion at the MDT, eligible patients were approached to enrol into the study. Written, informed consent was obtained, after which a PET/CT scan was performed. All patients underwent PET/CT prior to receiving any treatment.
With the results of the PET/CT scan available, the updated management plan was documented, noting whether any change to the pre-PET treatment plan was made. Additionally, any further investigations performed based on the PET/CT findings were recorded, including those performed owing to unexpected FDG uptake. Any independent pathology diagnosed following these investigations was also recorded. The investigators subsequently determined whether any such pathology was clinically relevant in the setting of newly diagnosed pancreatic, ampullary or distal bile duct cancers.
As eligible patients were already diagnosed with operable malignancy, the FDG uptake in the primary tumour or around the biliary stent was not intended to aid in the diagnosis of the primary tumour and had no influence on patient management.
Patients were subsequently followed up by the treating clinicians. No further PET/CT scans were planned. Adjuvant chemotherapy was administered at the discretion of the treating oncologist. If there was no histological verification of foci of abnormal uptake on PET/CT, lesions were followed up by appropriate means over time in order to clarify the aetiology.
The protocol was approved by the Royal Brisbane Hospital Ethics Committee and all patients provided written, informed consent. This research project is registered on the Australia and new Zealand Clinical trials registry: ACTRN12607000604404.
PET/CT imaging protocol
PET/CT scanning followed standard departmental guidelines. Patients fasted for a minimum of 6 h and serum glucose levels were measured on arrival into the department. FDG was injected at a dose of 5–7 MBq/kg. Patients remained in a relaxed position for 1 h before PET emission data were acquired from the base of the skull to the upper thighs. Prior to PET emission data acquisition, non-contrast CT scanning was performed for emission data attenuation correction and anatomical localization. Standard uptakes values (SUV) were measured.
The images were read by a specialist credentialed for PET interpretation by the Joint Nuclear Medicine Credentialling and Accreditation Committee of the Royal Australasian College of Physicians and the Royal Australasian College of Radiologisits.
The PET scans of all patients with a primary pancreatic cancer (patients subsequently found to have benign disease were excluded) were retrospectively analysed by one nuclear medicine physician (DM), who was blinded to clinical outcomes. SUV max values were determined in the region of the tumour, with the assistance of the contemporaneous CT and the contrast enhanced CT scan. In patients with an indwelling biliary stent, the SUV max was also calculated around the stent. In cases where the primary tumour was separate from the stent, two SUV's were calculated.
Statistical analysis
The primary endpoint of the study was to determine the frequency that PET/CT detected occult metastatic disease hence avoiding futile surgery. Secondary endpoints were: (i) to determine the frequency that PET/CT findings led to further investigations, the outcome of these and their contribution to the overall care of the patient; and (ii) to determine the SUV of the primary tumours and, in patients with indwelling biliary stents, determine the SUV around the stent.
The percentage of patients in whom management decisions are changed as a result of the PET/CT scan, with 95% confidence intervals (CIs), were calculated. We aimed to recruit 63 evaluable patients as if PET/CT resulted in 15% of patients avoiding futile surgery, then this number would result in a 95% CI of between 6% and 24%. This was felt to represent a clinically meaningful range, and the recruitment of this number of evaluable patients was deemed feasible for our institution.
The median SUV (and range) was calculated for all patients, those non-stented and around the biliary stent.
Results
Between March 2008 and December 2012, 56 patients were recruited to the study. The study was closed to recruitment at this time as recruitment was slower than expected, and PET/CT scanner availability for research purposes became limited.
Table1 lists the patient characteristics. The majority were male, and the head of the pancreas was the commonest primary site. A biliary stent was placed in 35 patients (63%) prior to the PET/CT scan. In 9% of the patients, the primary tumour was in the distal common bile duct and in a further 4%, the Ampulla. Two patients received neoadjuvant chemotherapy on a separate protocol, and PET/CT did not alter their management. No other patient received any pre-operative therapy. No patients were lost to follow-up.
Table 1.
Patient characteristics (n = 56)
| Number (%) | |
|---|---|
| Age | |
| Median = 64 | |
| Range: 35–84 | |
| Gender | |
| Male | 41 (73) |
| Female | 15 (27) |
| Location of carcinoma | |
| Pancreas | |
| Head | 40 (71) |
| Body | 4 (7) |
| Tail | 2 (4) |
| Distal bile duct | 5 (9) |
| Ampulla | 2 (4) |
| Benign | 3 (5) |
| Stented at time of PET | 35 (63) |
Three patients ultimately turned out to have benign disease. A 65-year-old male presented with obstructive jaundice and a CT cholangiogram suggested a distal common bile duct stricture with a surrounding mass. The PET/CT scan was normal. He underwent a Whipple's operation and grade 2 pancreatic intra-epithelial neoplasia, without invasive carcinoma, was found. The second patient, a 69-year-old male presented with right upper quadrant pain and weight loss. Liver function tests were abnormal but there was no jaundice. A CT scan demonstrated a head of pancreas mass and on PET/CT scan the SUV max was 3.8. At laparotomy, a large unresectable mass was found extending to the liver hilum and surrounding the superior mesenteric vein. Biopsies revealed lymphocytic sclerosing cholangitis. Immunoglobulin G 4 levels were normal. The patient remains well to date. The third patient was a 75-year-old male who presented with obstructive jaundice and imaging consistent with a high-grade distal common bile duct stricture. ERCP failed so he underwent a cholecystojejunostomy. A PET/CT scan was normal. No tissue diagnosis was obtained and the patient refused a Whipple's procedure. The patient remains quite well 3 years later notwithstanding recurrent episodes of cholangitis. A non-malignant stricture was, therefore, presumed.
Patient flow through the study is depicted in the consort diagram (Figure1). In 9 out of 56 patients (16%; 95% CI 6–26) PET/CT scanning resulted in planned surgical treatment being abandoned as a result of detecting unexpected metastatic disease. The details of these nine cases are listed in Table2. They all had pancreatic carcinoma. As expected, metastases were commonly picked up in the liver (5/9 cases). However, in three patients metastases were detected in lymph nodes above the diaphragm (mediastinum/neck), two of which were subsequently biopsy proven. Bone metastases were detected in one patient, in the setting of widespread nodal disease.
Figure 1.
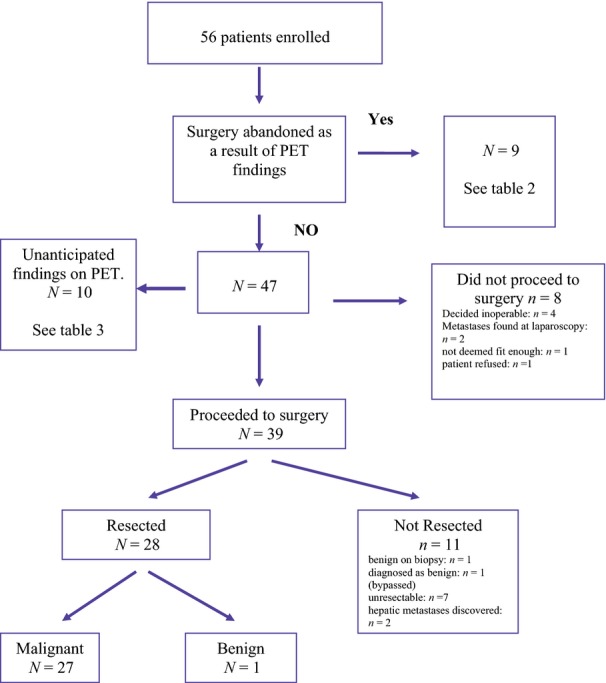
FlowDiagram of the study
Table 2.
Patients in whom surgery was abandoned as a result of PET/CT
| Patient | PET/CT result | CT size*/CA19.9# (other CT findings) | Comments | |
|---|---|---|---|---|
| 1 | 56-year-old female | Low grade uptake in HOP. SUV 3.5. Avid uptake in segment 3 liver metastasis | 48 mm 2200 | Liver metastasis not seen on standard imaging. Lesion became apparent on CT during palliativechemotherapy |
| 2 | 82-year-old male | Mild-moderate uptake HOP. SUV 4.9. Moderate uptake in para-aortic lymph node | 35 mm 660 | Node not seen on prior imaging. Died of metastatic disease 16 months later |
| 3 | 34-year-old male. Swachman diamond syndrome | Moderate uptake in HOP. SUV 4.7. 2 hepatic metastases | 22 mm 140 | Subtly visible on CT but PET/CT confirmed metastases. Patient died 8 months later of metastases |
| 4 | 77-year-old male | Avid uptake HOP. SUV 12.1. 2 peripheral right sided hepatic metastases | 30 mm 360 | No metastases seen on CT. Died 12 months later of metastatic disease |
| 5 | 54-year-old male | Avid uptake body of pancreas. SUV 7.77 Avid mediastinal, cervical nodes and multiple bone metastases | 20 mm 44 000 (Prominent node right of SMA) | Sclerotic lesions seen on CT but metastases confirmed by PET and subsequently by MRI. Patient died 4 months later |
| 6 | 75-year-old male | Mild-moderate uptake HOP. SUV 5. Liver (segment 5), para-aortic node and posterior mediastinal node avid uptake consistent with metastases | 28 mm 110 | Mildly enlarged para-aortic nodes and multiple hepatic cysts seen on CT and MRI. Patient died 2 months later of gastrointestinal haemorrhage |
| 7 | 47-year-old female | Mild- moderate avidity HOP. SUV 4.5 Low to moderate avidity in peri- pancreatic node. Avid posterior mediastinal lymph node 7 mm size | 15 mm 350 (34 mm nodal mass superior to pancreatic head) | Mediastinal node not seen on CT. Thoracoscopic biopsy of node confirmed adenocarcinoma |
| 8 | 58-year-old female | Avid HOP. SUV 11.5 Avid peri-pancreatic nodes. Avid nodes within mediastinum, lung hilar supraclavicular and cervical nodes | 46 mm 10 000 (enlarged 2 cm nodes around pancreas head) | Mildly enlarged nodes in chest/neck on CT (10-13 mm). Excision biopsy of cervical nodes revealed sarcoidosis and adenocarcinoma. Died 4 months later |
| 9 | 65-year-old male | Avid HOP lesion. SUV 8.1 Moderate uptake segment 2/3 lesion consistent with metastasis | No discrete mass identified. 200 (dilated common bile duct) | Liver metastasis not seen on initial CT but developed on subsequent imaging. Alive with disease 18 months later |
HOP = Head of pancreas; SUV = Standard Uptake Value in the primary pancreatic tumour.
Maximum size of the primary tumour.
Ca 19.9 measured in KU/l (normal is <35KU/l).
No cases of peritoneal metastases were detected by PET/CT scanning but two patients were found to have peritoneal metastases at subsequent staging laparoscopy. Two further patients were found to have liver metastases at the time of definitive resection, neither of which were detected on the PET/CT scan.
A total of seven patients were found to have locally advanced/inoperable disease at the time of definitive laparotomy. In none of these cases did the PET/CT scan assist in predicting this eventuality.
Table3 lists the 10 patients in which unexpected uptake was found on the PET/CT scan. In two of these cases, the PET/CT was valuable as possible nodal pathology in the mediastinum/neck was demonstrated which subsequently proved to be metastatic adenocarcinoma (listed also in Table2). Among five patients, unexpected FDG uptake resulted in other investigations which were ultimately considered to have added little or no clinical value, including sigmoidoscopy, colonoscopy, thyroid and axillary node biopsies and excision of a squamous cell carcinoma of the cheek. A further patient required additional history taking to confirm sialadenitis and finally, one patient underwent additional, careful inspection of the pancreatic tail/adjacent small bowel at the time of the Whipple's procedure, with nothing found.
Table 3.
Patients with unexpected FDG uptake
| Site of uptake | Subsequent investigations | Comments/outcome | |
|---|---|---|---|
| 1 | Left parotid and submandibular glands | Nil | Further history revealed known sialadenitis |
| 2 | Ascending colon | Colonoscopy | Tubular adenoma with low grade dysplasia |
| 3 | Mild uptake over left cheek | Excision of skin lesion left cheek | Squamous cell carcinoma left cheek |
| 4 | Mild uptake right upper lobe nodule | Nil | Decided patient unfit for whipples regardless of lung nodule |
| 5 | Abnormal uptake around pancreatic tail. ?Small bowel neoplasia. Primary HOP mass avid | Inspected intraoperatively | Nil found in this region. Proceeded to successful whipples |
| 6 | Left axillary node-moderate uptake | Node biopsied | Normal lymph node |
| 7 | Right thyroid lobe | Biopsied | Benign. Colloid and haemosiderin laden macrophages |
| 8 | Descending colon/sigmoid colon | Sigmoidoscopy | Previous surgery for diverticular disease. Normal anastomosis. No lesion seen |
| 9 | Posterior mediastinal node | Biopsied | Adenocarcinoma |
| 10 | Widespread lung hilar, mediastinal and cervical nodes | Cervical nodes biopsied | Sarcoidosis and adenocarcinoma |
The median SUV of the primary tumour for all patients with pancreatic malignancy (n = 46) was 4.9 (range 2–12.1); for non-stented patients (n = 18) it was 4.2 (range 2.3–11.5) and around the biliary stent (n = 28) it was 3.4 (range 2–11). Among the stented patients, the SUV was highest at the stent in 17 and in three of these, a separate tumour mass with lower SUV was discernable. However, the other 11 stented patients had a discernable, separate tumour mass exhibiting a higher SUV than at the stent.
Among the seven patients with distal common bile duct/ampullary tumours, the SUV max ranged from 1.5 to 6.7. In five cases, uptake was only seen at around the stent whereas in two patients a separate tumour with higher SUV was discernable.
Among the nine patients in which PET/CT scanning resulted in the abandonment of surgical management (by demonstrating metastatic disease), SUV in the primary pancreatic tumours ranged from 3.5 to 12.1 and was five or below (i.e. mild-moderate uptake) in five patients (see table2). Five of the nine patients were stented and in three of these the region with the highest SUV was around the stent.
Discussion
We conducted this prospective study to investigate the role PET/CT scanning in the management of patients with operable pancreas, ampullary or distal bile duct carcinomas. In addition to impact on surgical decision making, we wanted to explore the impact on management more generally, such as any independent, unexpected, pathology detected by PET/CT. As a separate objective, we investigated the SUV characteristics of primary pancreatic tumours. We envisioned that indwelling biliary stents might impact image interpretation, conceivably by inducing an inflammatory response, therefore, we specifically measured SUV's around these stents.
We have shown that PET/CT aided the correct decision to abandon potentially morbid and futile surgery in 9/56 patients (16%). This frequency is similar to that seen in diseases where PET/CT has become part of routine management such as non-small cell lung and oesophageal cancers.4,5 As such, our data support the incorporation of PET/CT scanning into the routine work-up of these patients. The CT or MRI images in some of the 9 patients demonstrated findings that could be construed as suspicious for metastases, such as mildly enlarged nodes, small hepatic hypodensities and sclerotic bone lesions (see Table2) and might have been confirmed using another imaging/investigative modality. This reflects the clinical dilemmas faced by the MDT. In all cases, the scans were reviewed at the MDT meeting, and the patients were declared as being operable. In this setting, the PET/CT was able to clarify the staging and/or direct subsequent confirmatory investigations. In addition to detecting hepatic metastases, PET/CT detected metastases to multiple, disparate nodal groups (retroperitoneal, mediastinal, supraclavicular and cervical) as well as to the bone. As illustrated in Table2, a highly FDG avid primary tumour is not a prerequisite to the detection of metastases, with the primary tumour in five patients exhibiting an SUV of five or less. In all nine patients, the primary tumour was in the pancreas. The number of patients in this study with ampullary or distal bile duct cancers is too low to make any conclusions regarding the relative utility of PET/CT by primary site.
PET/CT scanning, in this clinical scenario, has shortcomings. It was of no use in predicting locally unresectable disease, which was found at the time of surgery in seven patients. In addition, PET/CT missed two cases each of hepatic and peritoneal metastases. Failure to detect inoperable, locally advanced disease is unsurprising given the limited FDG uptake of many primary pancreatic tumours and the inability of PET/CT to accurately define tumour extent relative to surrounding tissues. It is well documented that metastases to the liver and peritoneum, especially when small, can be missed by PET/CT, as has been reported in this specific setting.11,12 It remains to be seen if these shortcomings can be surmounted by contemporaneous contrast enhanced CT and/or MRI scanning, and this should be the subject of future research.
Our findings of the utility of PET/CT scanning are supported by other prospective cohorts; however, some retrospective analyses have found no value of PET in patient management. In a retrospective analysis, but of prospectively collected data, Heinrich et al. found that PET/CT scanning detected metastases in 5/59 pancreatic cancer patients, changed management in 16% and was cost effective. A prospective study by Kauhanen et al. also supports the utility of PET/CT. This group compared PET/CT with MRI and CT scanning. They found that PET/CT was more sensitive in detecting metastases and changed the management strategy in 10 of 38 cases.13 By contrast, Pappas et al.14 found that FDG PET (without concurrent CT) provided no additional information in 98% of 124 patients with resectable, borderline resectable or locally advanced pancreas cancer. Matsumoto et al.7came to a similar conclusion from their retrospective analysis.
Current NCCN guidelines state that the role of PET/CT in the work-up of pancreas cancer patients is unclear but could be considered following a formal pancreas protocol CT in high-risk patients.15 Such patients are defined as having borderline resectable disease, large primary tumours, surrounding lymphadenopathy or markedly elevated Ca 19.9. It would be very useful if a patient subgroup with a higher chance of harbouring detectable metastases at the time of investigative work-up could be identified. While our dataset cannot conclusively identify such a group, all nine patients in whom PET/CT changed the treatment plan and resulted in surgery being abandoned met at least one of these criteria. CA 19.9 was raised by at least three times the upper limit of normal in all nine patients. While biliary obstruction contributes to a raised CA19.9, the bilirubin was normal in four of these patients. However, in three patients the primary tumour was 2 cm or less (T1 according to the 7th edition of the American Joint Committee on Cancer staging) and in six patients no surrounding lymphadenopathy was seen.
In comparison to other tumour sites, the true impact of PET/CT on the treatment of pancreatic cancer might be diluted as patients may not proceed to resection regardless of whether they undergo a PET/CT scan. For example, locally advanced disease or occult peritoneal/hepatic metastatic disease may be discovered intra-operatively. In addition, owing to the morbidity and low cure rates associated with surgery, together with patient co-morbidities surgeons may cogitate on the value of surgery before ultimately deciding not to proceed. In our cohort, 11 patients were subsequently found to harbour occult metastases or be unresectable and a further five were ultimately deemed unsuitable for surgery, in spite of the PET/CT scan being consistent with localized disease.
Unexpected FDG uptake raises the possibility of independent pathology, including second primary neoplasms. This is particularly true for the colon8. We examined this phenomenon in our cohort. PET/CT scanning resulted in several patients undergoing additional investigations (Table3). It can be argued that these ultimately were unnecessary and did not positively contribute to the overall care of these patients, in the setting of a diagnosis of pancreatic cancer. If PET/CT scanning was to be routinely introduced into the work-up, it will be important to bear this in mind and carefully consider the value and appropriate timing of any additional investigations prompted by PET/CT scanning.
Analysis of the SUV range of our cohort demonstrates that it is not uncommon for uptake to be physiologic or only mildly elevated in primary pancreatic carcinomas. Although this did not influence diagnosis or management in our study population, it suggests, in other clinical settings, that PET/CT is not useful for defining the nature of a primary pancreatic mass. This is best achieved using spiral enhanced CT, MRI and/or endoscopic ultrasound. The literature is somewhat conflicting on this issue. The retrospective analysis by Matsumoto et al.14 of the accuracy of FDG-PET in detecting pancreatic cancer found that only 69% of tumours less than 20 mm were detected. Additionally, 79% of focal, mass-forming pancreatitis cases were FDG avid. In contrast, a large meta-analysis of 38 studies found that both FDG PET and PET/CT detected primary pancreatic cancers with high sensitivity of around 90%, but with a somewhat lower specificity, around 80%.16 Sensitivity and specificity values might be misleading as they will be impacted by subjective interpretation of a ‘positive scan’ which might be biased in retrospective analyses, and by the chosen benchmark used to define the true diagnosis (biopsy versus follow-up etc.). It is noteworthy that in five patients in our study with mild to moderately FDG avid primary tumours, PET/CT was still able to detect metastases.
The highest region of FDG uptake may be around the biliary stent. Of course this may be as a result of malignant cells within the tumour but it is conceivable that a stent-induced inflammation/immune reaction may contribute. Of note, 3/28 stented patients had a separate tumour mass exhibiting a lower SUV than was seen around the stent. This concept should be considered when interpreting PET/CT images. Given there is increasing interest in using PET/CT scanning as an early marker of treatment response, perhaps to guide subsequent management17, our data may have implications for pancreatic research protocols investigating PET/CT scanning in the neo-adjuvant or locally advanced settings. Specifically, FDG uptake around the stent may not be due to malignant cells, and hence may not reflect the efficacy of chemo/targeted therapy, thereby confounding data interpretation. It is important to emphasize, however, that our results are not definitive. We did not correlate SUV around stents with histological parameters and we have not assessed the possible confounding effects, if any, of the type of stent or time from stent insertion to PET/CT scanning on SUV uptake.
In conclusion, this prospective study was specifically designed to examine the value of FDG PET/CT in resectable pancreatic cancer, in real world clinical practice. We feel that our study design possesses considerable strengths in comparison to other retrospective analyses. PET/CT, notwithstanding the shortcomings discussed, detects metastatic disease in a significant percentage of patients. Consequently, we intend to incorporate PET/CT into our diagnostic algorithm for these patients. Further research is needed with the aim of refining patient selection for surgery. To this end, we plan on investigating novel gallium-68 labelled PET tracers targeting chemokine receptors.
Acknowledgments
The authors wish to thank Andrea Mckenzie, Annette Cubitt and Louise Campbell for their invaluable support in conducting this study. Above all, we thank the patients and their families for their willing participation in this research.
Conflicts of interest
None declared.
References
- https://www.aihw.gov.au/acim-books/
- Oettle H, Post S, Neuhaus P, Gellert K, Langrehr J, Ridwelski K, et al. Adjuvant chemotherapy with gemcitabine vs observation in patients undergoing curative-intent resection of pancreatic cancer: a randomized controlled trial. JAMA. 2007;297:267–277. doi: 10.1001/jama.297.3.267. [DOI] [PubMed] [Google Scholar]
- Neoptolemos JP, Stocken DD, Bassi C, Ghaneh P, Cunningham D, Goldstein D, et al. Adjuvant chemotherapy with fluorouracil plus folinic acid vs gemcitabine following pancreatic cancer resection: a randomized controlled trial. JAMA. 2010;304:1073–1081. doi: 10.1001/jama.2010.1275. [DOI] [PubMed] [Google Scholar]
- Flamen P, Lerut A, Van Cutsem E, De Wever W, Peeters M, Stroobants S, et al. Utility of positron emission tomography for the staging of patients with potentially operable oesophageal carcinoma. J Clin Oncol. 2000;18:3202–3210. doi: 10.1200/JCO.2000.18.18.3202. [DOI] [PubMed] [Google Scholar]
- Antoch G, Stattaus J, Nemat A, Marnitz S, Beyer T, Kuehl H, et al. Non-small cell lung cancer: dual-modality PET/CT in Preoperative staging. Nucl Med. 2003;229:526–533. doi: 10.1148/radiol.2292021598. [DOI] [PubMed] [Google Scholar]
- De Wever W, Vankan Y, Stroobants S, Verschakelen J. Detection of extrapulmonary lesions with integrated PET/CT in the staging of lung cancer. Eur Respir J. 2007;29:995–1002. doi: 10.1183/09031936.00119106. [DOI] [PubMed] [Google Scholar]
- Matsumoto I, Shirakawa S, Shinzeki M, Asari S, Goto T, Ajiki T, et al. 18-fluorodeoxyglucose positron emission tomography does not aid in diagnosis of pancreatic ductal adenocarcinoma. Clin Gastroenterol Hepatol. 2013;11:712–718. doi: 10.1016/j.cgh.2012.12.033. [DOI] [PubMed] [Google Scholar]
- Lee JC, Hartnett GF, Hughes BGM, Kumar AR. The segmental distribution and clinical significance of colorectal fluorodeoxyglucose uptake incidentally detected on PET-CT. Nucl Med Commun. 2009;30:333–337. doi: 10.1097/MNM.0b013e32832999fa. [DOI] [PubMed] [Google Scholar]
- Vandenbroucke JP. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): elaboration and explanation. PLoS Med. 2007;4:e297. doi: 10.1371/journal.pmed.0040297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans D, Erickson B, Ritch P. Borderline resectable pancreatic cancer: Definitions and the importance of multimodality therapy. Ann Surg Oncol. 2010;17:2803–2805. doi: 10.1245/s10434-010-1285-8. [DOI] [PubMed] [Google Scholar]
- Izuishi K, Yamamoto Y, Sano T, Takebayashi R, Masaki T, Suzuki Y. Impact of 18-fluorodeoxyglucose positron emission tomography on the management of pancreatic cancer. J Gastrointest Surg. 2010;14:1151–1158. doi: 10.1007/s11605-010-1207-x. [DOI] [PubMed] [Google Scholar]
- Heinrich S, Goerres G, Schäfer M, Sagmeister M, Bauerfeind P, Pestalozzi C, et al. Positron emission tomography/computed tomography influences on the management of resectable pancreatic cancer and its cost-effectiveness. Ann Surg. 2005;242:235–243. doi: 10.1097/01.sla.0000172095.97787.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kauhanen S, Komar G, Seppanen M, Dean K, Minn H, Kajander S, et al. A prospective diagnostic accuracy study of (18)F fluorodeoxyglucose positron emission tomography/computed tomography, multidetector row computed tomography, and magnetic resonance imaging in primary diagnosis and staging of pancreatic cancer. Ann Surg. 2009;250:957–963. doi: 10.1097/SLA.0b013e3181b2fafa. [DOI] [PubMed] [Google Scholar]
- Pappas S, Christians K, Tolat P, Mautz A, Lal A, McElroy L, et al. Staging chest computed tomography and positron emission tomography in patients with pancreatic adenocarcinoma: utility or futility? HPB. 2014;16:70–74. doi: 10.1111/hpb.12074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- http://www.nccn.org/professionals/physician_gls/pdf/pancreatic.pdf.
- Liu J, Liu T, Treven L, Song S, Zhang C, Pan L, et al. Usefulness of 18F-FDG PET, combined FDG-PET/CT and EUS in diagnosing primary pancreatic carcinoma: a meta-analysis. Eur J Radiol. 2011;78:142–150. doi: 10.1016/j.ejrad.2009.09.026. [DOI] [PubMed] [Google Scholar]
- Ott K, Weber W, Lordick F, Becker K, Busch R, Herrmann K, et al. Metabolic imaging predicts response, survival, and recurrence in adenocarcinomas of the esophagogastric junction. J Clin Oncol. 2006;24:4692–4698. doi: 10.1200/JCO.2006.06.7801. [DOI] [PubMed] [Google Scholar]


