Abstract
Sepsis is a systemic inflammatory response that follows bacterial infection. Cardiac dysfunction is an important consequence of sepsis that affects mortality and has been attributed to either elevated inflammation or suppression of both fatty acid and glucose oxidation and eventual ATP depletion. Moreover, cardiac adrenergic signaling is compromised in septic patients and this aggravates further heart function. While anti-inflammatory therapies are important for the treatment of the disease, administration of anti-inflammatory drugs did not improve survival in septic patients. This review article summarizes findings on inflammatory and other mechanisms that are triggered in sepsis and affect cardiac function and mortality. Particularly, it focuses on the effects of the disease in metabolic pathways, as well as in adrenergic signaling and the potential interplay of the latter with inflammation. It is suggested that therapeutic approaches should include combination of anti-inflammatory treatments, stimulation of energy production, and restoration of adrenergic signaling in the heart.
Keywords: Sepsis, Heart, Metabolism, Fatty acid oxidation, Adrenergic signaling, Inflammation
Introduction
This review article aims to summarize the effects of sepsis on cardiac function, particularly on cardiac metabolism and adrenergic signaling. Specifically, it aims to describe sepsis-driven suppression of cardiac metabolism and energy production, as well as to indicate the relative contribution of cardiac adrenergic signaling inhibition in heart dysfunction that occurs in septic patients and animal models of sepsis.
Sepsis: an “Inflam-Metabolic” Disease
Sepsis is defined as a systemic inflammatory response. It follows bacterial infection and can lead to severe sepsis and septic shock characterized by hypotension, ischemia, multiple organ failure, and death. Sepsis is a major health complication causing patient mortality and increased health care cost [1]. Approximately 1 million cases are reported annually in the USA and about 50 % of patients with sepsis require intensive care unit (ICU) treatment. Sepsis is responsible for 10 % of all ICU admissions [1, 2]. The incidence of sepsis is expected to increase due to a higher incidence of severe sepsis in older patients, an increased number of people living with chronic diseases and therapies aiming to suppress the native immune system [2].
The exuberant septic inflammatory response in the organism is complicated by secondary end organ damage. In particular, cardiovascular derangements such as decreased peripheral resistance and increased vascular permeability leading to tissue hypoperfusion are of clinical importance in the therapeutic approach of sepsis. Feared complications in severe sepsis and septic shock are multiorgan failure (MOF) and hemostatic derangements leading to disseminated intravascular coagulation (DIC).
Cardiac dysfunction is a consequence of severe sepsis [3–5] and is characterized by impaired contractility [6], diastolic dysfunction, as well as reduced cardiac index and ejection fraction (EF) [7]. Cardiac dysfunction is an important component of multiorgan failure that is caused by severe sepsis [8, 9]. Septic patients with either systolic or diastolic dysfunction or a combination of both have higher mortality than those diagnosed with sepsis but without diastolic or systolic dysfunction [10]. The mechanisms that underlie myocardial depression during septic shock are not well known. Circulating inflammatory cytokines interleukin (IL)-1 [11, 12], IL-8 [12], and tumor necrosis factor (TNF)α [11, 13], which are increased during septic shock, may account for cardiac dysfunction as they have been associated with altered production of nitric oxide [14–16] and altered calcium homeostasis [17, 18]. Impaired β-adrenergic signaling leading to reduced cardiac contractility is also present in sepsis [19]. Moreover, growing evidence associates septic cardiac dysfunction with impaired metabolism and reduced energy production in cardiomyocytes. The heart produces ATP primarily via fatty acid and glucose oxidation, which both are strongly decreased in experimental animal models of sepsis [20, 21]. Despite reduced cardiac lipid uptake, sepsis leads to intracellular lipid accumulation. Lipid accumulation must therefore result from impaired fatty acid oxidation [21, 22•] and conversion of non-oxidized fatty acids into triglycerides.
There are several experimental models [23] that mimic the effects of sepsis. The most common setup includes injection of Escherichia coli lipopolysaccharide (LPS), which is a component of the bacterial cell wall. LPS induces profound inflammation and pathophysiological consequences similar to those found during septic shock. In addition, sepsis can be induced experimentally by cecal ligation and puncture (CLP) or bacterial infusion. Less frequently used sepsis experimental models are based on injection of TNFα or IL-1.
Clinical Facts About Sepsis
Clinical treatment of sepsis is complex with a high mortality of 20–50 % requiring intensive medical treatment. For stage-adapted treatment and estimation of mortality risk, several scoring systems are in use, with the APACHE-II Score (as an outcome score) and the SOFA score (severity of multiorgan failure) among them.
Optimization of management of sepsis is intensively investigated. Cornerstones of the guideline-directed therapy of sepsis are immediate initial volume resuscitation and the identification of the source and causative pathogen allowing a test-appropriate antibiotic therapy, with an initial empiric antibiotic regimen within the first hour after diagnosis. Furthermore, optimization of organ perfusion and tissue oxygen supply are important measures for the management of the septic patient in the intensive care setting.
The high incidence and unsatisfactory therapeutic outcome of sepsis call for new therapeutic approaches and a large number of potential therapies are currently investigated. Among those, strategies to inactivate or remove cytokines and endotoxins by hemabsorption [24] or measures aiming at immunomodulation showed promising results. Immunotherapeutic approaches include administration of interferon (IFN)-γ [25], GM-CSF [26], or IL-7 [27].
Inflammation: a Potential Driving Force of Septic Cardiac Dysfunction
The inflammatory component of the pathophysiology of sepsis is complex, involving the activation of plasmatic (complement activation, coagulation) and cellular (macrophagic, endothelial, thrombocytic, cellular immunity) systems. The innate immune response leads to a strong activation of the cytokine system [28], which has plethoric effects on a variety of organs and the vasculature, leading to changes in vascular permeability, endothelial function, and activation of further mediators such as bradykinin, histamine, the complement, and coagulation system. Cytokines play an important role in the pathology of sepsis: pro-inflammatory mediators such as TNFα, IL-1, IL-6, IL-8, IL-12, and IFN-γ are counteracted by anti-inflammatory cytokines (IL-10, TGF-beta, IL-4) [28]. However, controversies have developed over the role of cytokines as primary target for new therapeutic approaches since a large number of clinical trials investigating anti-inflammatory agents failed [29]. On the other hand, in the process of the disease, a secondary or simultaneously occurring [29] phase of prolonged sepsis-induced immunosuppression can be observed, which further illustrates the complexity of the disease [30, 31].
The production of inflammatory response-related cytokines, such as TNFα and interleukins IL-1 and IL-8, follows association of LPS with plasma LPS-binding protein (LBP). This complex targets CD-14 and TLR4 receptors and turns on signaling mechanisms that finally result in the production of cytokines. LPS-mediated signaling starts from the cytoplasmic portion of TLR4 that is called Toll/IL-1 receptor (TIR) domain and is mediated by several intracellular proteins such as MyD88, IRAK-1, IRAK-4, TNF receptor-associated factor (TRAF)-6, TGF-β-activated kinase 1 (TAK1), TAK1-binding proteins, TAB1, and TAB2. TAK1 phosphorylates either the IKK complex, which leads to activation of the NF-κB pathway, or the MKK7 that activates the c-Jun N-terminal kinase (JNK) signaling pathway [32]. Nevertheless, NF-κB [33] and JNK [34, 35] are well-established targets of LPS stimulus and they induce production of inflammatory response-related cytokines, such as TNFα and IL-1.
TNFα production by macrophages is increased during sepsis and has been considered as a potential target for experimental and clinical therapeutics. Indeed, genetic ablation of TNF receptor 1 (TNFr1−/−) prolonged survival in mice that underwent polymicrobial sepsis with CLP [36]. Accordingly, treatment of BALB/C mice with anti-TNFα antibodies prior to administration of LPS improved survival rate [37]. Interventions aiming to inhibit the TNFα pathway seem to be effective in preventing morbidity and mortality in non-human primates, as well. Treatment of baboons with anti-TNFα antibody that was given either simultaneously or 2 h prior to administration of live E. coli reduced release of cytokines such as IL-1, IL-8, and monocyte chemotactic peptide-1 (MCP-1) [38, 39] and offered complete protection against vital organ dysfunction, stress hormone release, and death [40]. Although anti-TNFα treatment was successful in preventing inflammatory response and improving survival in septic animal models, the use of either anti-TNFα antibodies [41, 42] or soluble TNFr [43, 44] that neutralize circulating TNFα failed to attenuate mortality in septic patients. The discrepancy in efficiency between animal and human studies may pertain to the pretreatment or early treatment of animals with anti-TNFα as opposed to septic patients that received anti-TNFα treatment much later during the progression of the disease. Nevertheless, pretreatment with anti-TNFα reduces the levels of TNFα and IL-8 [39] and attenuates the TNFα-driven effects of sepsis. This suggests that other non-TNF-mediated processes cause much of the mortality in humans.
IL-1 is produced by macrophages, monocytes, and neutrophils in response to TNFα and ignites iNOS production [45], which suppresses cardiac contractility [46]. Human genetic polymorphisms that are associated with reduced levels of IL-1 receptor antagonist (IL-1ra), i.e., enhanced IL-1 signaling, have been associated with increased septic mortality [47]. Thus, IL-1 signaling has been indicated as a potential therapeutic target for treatment of septic patients. This hypothesis was supported by studies in animal models that associated inhibition of IL-1 with improved response in sepsis. Pretreatment of rabbits with IL-1ra resulted in smaller mean arterial pressure decrease and less TNFα and IL-1 increase, following Staphylococcus epidermidis injection [48]. Treatment of mice with combination of IL-1ra and TNFr, which neutralizes circulating TNFα, improved survival following sepsis induction by either LPS administration or CLP [49]. Despite these remarkable protective effects of IL-1 signaling inhibition in the cardiovascular system and survival in sepsis animal models, treatment of septic patients with IL-1ra did not incur any significant improvement [50].
The lack of success of anti-inflammatory therapies in septic patients, such as administration of corticosteroids [51–53], IL-1 receptor antagonist [50, 54], or anti-TNFα [55], despite the significant improvement in cardiac function or survival of septic animal models may be attributed to a number of reasons. Due to advances in intensive medical care, patients survive the initial hyperinflammatory phase, progressing to the fatal state of sepsis-induced immunosuppression. Consequently, recent efforts focus on host innate and adaptive immunity such as T cell exhaustion in sepsis [56] and other mechanisms of cell-mediated immunity [29, 57–59]. Moreover, species differences or the way that anti-inflammatory interventions were applied in animals may explain the failure of anti-inflammatory therapies in septic patients. Most of the animal studies were based on the use of either knockout and transgenic mice or administration of anti-inflammatory treatments prior to or simultaneously with experimental induction of sepsis. This design indicated the importance of the prevention of inflammation as a therapeutic approach in the development of sepsis and subsequent organ dysfunction. As opposed to the animal models, anti-inflammatory treatments were applied in septic patients after diagnosis of the disease, when inflammation and organ failure were already in progress. Other components of the pathophysiology of sepsis, such as energetic starvation of the heart and other organs, might occur later during sepsis and that likely were not corrected with the anti-inflammatory treatments.
Complications of Cardiac β-Adrenergic Signaling in Sepsis
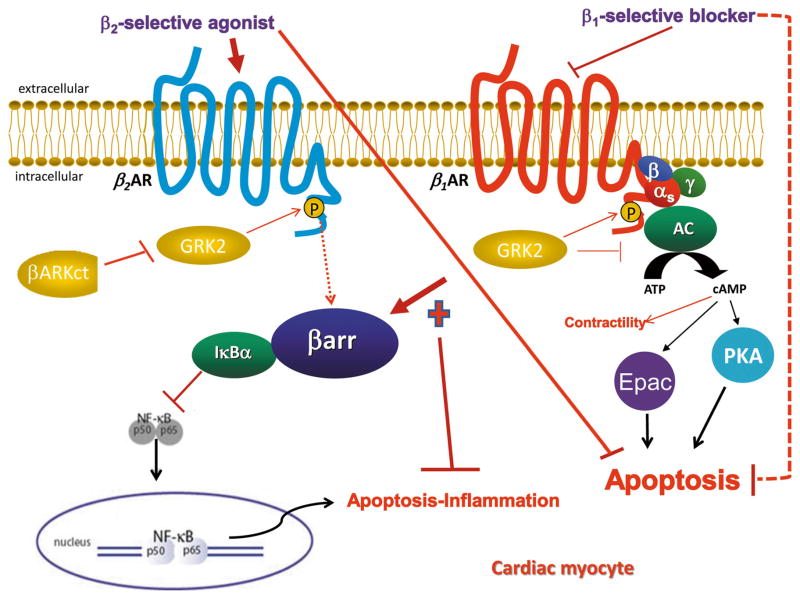
Impaired β-adrenergic signaling is another component of septic cardiac dysfunction and may be due to the pro-inflammatory NF-κB signaling. Cardiac β1- and β2-adrenergic receptors (βARs) are the main stimulatory receptors of cardiac function with distinct and in some cases opposite roles in cardiac physiology and pathology [60–63]. For instance, cardiomyocyte contraction is stimulated by β1ARs but not β2ARs. Cardiac β1AR signaling is generally considered pro-apoptotic via its cAMP signaling pathway that activates both protein kinase A (PKA) and exchange protein directly activated by cAMP (Epac). Conversely, β2AR signaling is anti-apoptotic (Fig. 1) [60–63]. The inhibitory effect of cardiac β2AR in apoptosis is mediated by this subtype’s signal switching from Gs to Gi/o protein-mediated, which is a feature that cardiac β1ARs lack [64–68]. Furthermore, upon agonist-mediated activation and GRK2-mediated phosphorylation β1AR does not readily bind the receptor adapter proteins beta-arrestins (βarrs) following its phosphorylation by G protein-coupled receptor kinases (GRKs) [69–71]. Finally, the interaction of β2AR with βarrs can have pleiotropic effects in cardiac myocytes, such as inhibition of apoptosis and promotion of survival via PI3K activation [64] and NF-κB inhibition (Fig. 1) [72–74].
Fig. 1.
Schematic illustration of the βAR-elicited signaling pathways modulating apoptosis/inflammation in the heart, discussed in the present article. Potential therapeutic strategies for cardiac sepsis are also depicted. See text for details and for molecular acronym descriptions
Early stages of sepsis are characterized by elevated catecholamine levels [75–77], which most likely constitute a compensatory adrenergic response aiming to augment cardiac contractility and heart rate [78, 79]. However, this adaptive response ultimately becomes maladaptive as excessive stimulation of cardiac βARs and particularly of the pro-apoptotic β1AR cause myocardial damage due to intracellular calcium overload and induction of cell death. The sympathetic over-stimulation in critically ill patients—the so-called catecholaminergic storm—is detrimental for the heart in the long run as it can lead to impaired diastolic function, tachycardia and tachyarrhythmias, myocardial ischemia, stunning, apoptosis, and necrosis [80]. In addition, the progression of septic cardiac dysfunction is associated with reduced βAR density [81], and there is evidence for significant cardiac desensitization and downregulation of βARs potentially caused by cytokines [82]. These changes have been observed in the myocardium of patients who survived septic shock [83]. Thus, sympathetic overstimulation appears incapable of stimulating cardiac function any further and the myocardium becomes unresponsive to catecholamines.
The lack of βAR responsiveness during sepsis has been attributed to either auto-oxidation by reactive oxygen species (ROS), as superoxide dismutase (SOD) administration simulated the β-adrenergic responses in an animal model of septic shock [84], or to elevated NO levels [85, 86]. Cardiac GRK2 is the major negative regulator of βAR pro-contractile signaling [87]. Desensitization of βARs and eventual termination of cAMP signaling reduce dramatically cardiac inotropic and adrenergic reserves (Fig. 1). Since GRK2 is markedly elevated in other types of heart failure, such as ischemic cardiomyopathy, its blockade (Fig. 1) has been proposed as an attractive therapeutic strategy for heart disease treatment [87]. The essential role of GRK2 inhibition in maintaining β2AR pro-contractile signaling in the heart was recently uncovered in a murine post-MI heart failure model [88]. In this study, cardiac-specific overexpression of a GRK2 inhibitor, βARKct, in mice with β1AR gene ablation enhanced the pro-contractile signaling of β2AR [88]. The mechanism that underlies this effect includes inhibition of βarr binding. An interesting observation from this study that can be extrapolated in septic cardiac dysfunction was that βarr inhibition was associated with degradation of IκBα, activation of NF-κB, and increased expression of inflammatory markers [88]. The authors suggest that GRK2 inhibition reduces phosphorylation of β2AR and therefore weakens binding of βarr to β2AR. This results in less βarr-dependent scaffolding of IκBα, which normally stabilizes IκBα and prevents NF-κB activation (Fig. 1) [88]. Thus, reduced βarr binding is likely associated with NF-κB activation and inflammation. Accordingly, although there is still no evidence for the role of βarr in septic cardiac inflammation, it has been shown that both βarr1 and βarr2 inhibit NF-κB signaling in vitro [73]. Global βarr2−/− mice with CLP-induced sepsis have elevated plasma IL-6 levels and die faster than septic wild-type mice [89]. These findings indicate βarr activation as an attractive candidate for the alleviation of cardiac inflammation that is elevated in sepsis, when β-AR desensitization and increased binding of βarr to β-ARs occur.
NF-κB has a central role in cardiac inflammation during septic cardiac dysfunction [90]. Also, β1AR- and β2AR-driven signaling pathways induce phenotypically opposing effects on cardiac apoptosis and βarr activation may be a critical switch for that. Therefore, blockade of β1AR signaling [91, 92] or enhancement of cardiac β2AR signaling [93] or βarr-mediated NF-κB inhibition via activation of β2AR [94] may all be valid therapeutic strategies to inhibit NF-κB and inflammation in the septic heart (Fig. 1). Indeed, βAR agonists, such as isoproterenol and dobutamine, β2AR-selective agonists like clenbuterol [95–97], and β1-selective blockers like esmolol [98] are being tested in animal models and in clinical trials of cardiac sepsis. Enhancement of βarr-mediated NF-κB scaffolding/inhibition via β2AR activation could be achieved either with a gene therapy approach aiming to increase cardiac levels of βarrs or with a β2AR ligand capable of acting as βarr-“biased” agonist, e.g., the β-blocker carvedilol [71]. Indirect enhancement of this signaling modality by elevating GRK2 activity is not recommended, as this would severely impair cardiac function [87, 88]. Thus, interventions that augment βarrs during sepsis may lead to combined improvement of β-AR signaling and alleviation of inflammatory pathways in the heart.
Septic Cardiac Dysfunction as a Consequence of Energetic Starvation
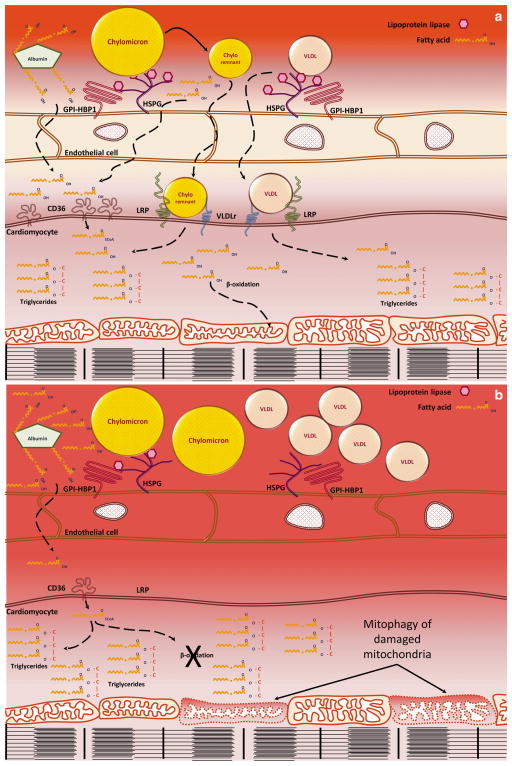
Sepsis is associated with altered lipoprotein metabolism characterized by elevated plasma triglyceride and free fatty acid levels [21, 99–101] and suppression of energy production in several organs, including the heart [20, 21, 22•] (Fig. 2). Increased plasma triglyceride levels are due to compromised intravascular lipolysis and reduced lipid uptake by tissues [102, 103], as hepatic lipoprotein production remains normal [104]. Sepsis-induced energetic deficiency of organs constitutes another critical component of the pathophysiology of the disease. This defect becomes even more important for the heart due to its vast energetic demands. Approximately 70 % of cardiac ATP is produced via lipid oxidation, while the rest is produced primarily via glucose oxidation. Some ATP is also derived from catabolism of lactate and ketone bodies. In pathologic conditions that are characterized by reduced cardiac work such as heart failure, fatty acid oxidation is reduced and glucose oxidation is increased to compensate for ATP production [105, 106]. In contrast, in sepsis, the reduction of cardiac fatty acid oxidation is not compensated by increased glucose catabolism, as insulin resistance and suppressed glucose utilization occur [107–109]. As oxygenation of the heart does not seem to change in sepsis [110], the observed cardiac energetic deficiency is attributed primarily to defective supplementation of the heart with substrates that are used for ATP production.
Fig. 2.
Cardiac fatty acid metabolism in health and in sepsis—a cardiac fatty acid oxidation in normal hearts: fatty acids are taken up by cardiomyocytes via CD36 or with the contribution of lipoprotein remnant receptors, such as VLDLr and LRP. Cardiomyocyte fatty acids can be stored in triglycerides or used for ATP production via β-oxidation in mitochondria. b During sepsis, CD36, lipoprotein lipase, and lipoprotein remnant receptors are downregulated, leading to increased fatty acid and triglyceride-carrying lipoprotein content in the circulation. In addition, cardiac β-oxidation is inhibited and mitochondrial number is reduced via mitophagy, resulting in intracellular accumulation of the unused fatty acids in triglycerides
Septic hearts have reduced expression of a broad range of fatty acid metabolism genes. Moreover, they demonstrate mitochondrial dysfunction. Cardiac supplementation of fatty acids is compromised due to reduced activity of cardiac lipoprotein lipase (LpL) due to lower LpL expression and increased expression of Angptl4, an inhibitor of LpL [21, 111]. Besides reduced LpL activity, sepsis reduces the expression of fatty acid transporter CD36 [112] and the very-low-density lipoprotein receptor (VLDLr) [113], aggravating even further uptake of lipids by the heart (Fig. 2). Efficient lipoprotein clearance from circulation during sepsis can contribute to the removal of bacterial endotoxins, as these stick on lipoproteins [114], particularly chylomicrons [115]. Thus, the observed reduced expression of lipoprotein receptors during sepsis may constitute a defensive mechanism to prevent the delivery of these toxins to the heart.
Intracellular cardiac fatty acid mobilization and oxidation are inhibited due to reduced expression of fatty-acid-binding protein [116], acyl-CoA synthetase [117], and carnitine palmitoyl transferase-1 [112]. Furthermore, cardiac expression of transcriptional factors, which are strongly associated with fatty acid oxidation, such as peroxisome proliferator-activated receptors (PPARs), retinoid-X receptors (RxRs), and thyroid receptors (TRs), as well as their coactivator PPARγ-coactivator-1 (PGC-1) are lower during sepsis [20, 21, 22•, 112]. Accordingly, cardiomyocyte-specific constitutive expression of PGC-1β [22•] or PPARγ [21] as well as pharmacological activation of PPARγ [21] or prevention of cardiac PPARα downregulation [20] induce fatty acid oxidation and correct cardiac function during sepsis. Interestingly, this improvement occurs despite increased expression of cardiac inflammatory markers.
Rosiglitazone-mediated systemic PPARγ activation improves survival in LPS-treated mice [21] or mice with CLP [118]. These results suggest that improved energy production is crucial for several organs during sepsis. As PPARγ activation is also associated with reduced inflammation [119–123], it might also be postulated that the improvement in survival during sepsis is due to alleviation of inflammation. However, when PPARγ activation was applied to mice that do not express adiponectin (APN), an adipocyte-derived protein [124–126] that promotes fatty acid oxidation in peripheral organs, such as the heart [127] and skeletal muscles [128], the survival benefit of this nuclear receptor agonism was blunted [118]. On the other hand, the administration of rosiglitazone in wild-type mice with either polymicrobial sepsis [118] or endotoxemia [21, 129] improved survival. In some studies, the beneficial effect of PPARγ activation in cardiac function [21] or in survival rates [129] was not associated with significant alleviation of inflammation. Another study showed that pharmacological activation of a different inducer of fatty acid oxidation, PPARδ, also protects cardiac function but PPARδ agonist also alleviated inflammation [130]. In accordance with animal studies showing the beneficial effect of fatty acid oxidation, a clinico-metabolomic study that analyzed plasma from septic patients showed that markers of reduced fatty acid utilization in tissues, such as higher concentration of carnitine esters and fatty acids, were associated with increased lethality [131••]. Thus, although inflammation is an important component of sepsis-driven dysfunction of the heart and other organs, improvement in energy production appears to confer survival benefit at least for the early stages of the disease.
The energetic deficiency of septic hearts has also been associated with mitochondrial dysfunction [132, 133]. Mitochondrial dysfunction is triggered by increased production of ROS that occurs in septic hearts, as has been shown in LPS-treated mice [134] and rats [135]. This is associated with reduced levels of complex II and IV of the oxidative phosphorylation machinery and reduced enzymatic activity of several mitochondrial enzymes, such as NADH cytochrome c reductase, succinate cytochrome c reductase, and cytochrome c oxidase [136]. In several cases, mitochondrial dysfunction is paired with autophagy, which is a defensive mechanism for the removal of damaged mitochondria and therefore is called mitophagy. Cardiac mitophagy is induced during sepsis [21, 137]. Accordingly, Park2 deficiency, which compromises autophagic mechanisms in mice, results in impaired recovery of cardiac contractility following administration of a sublethal dose of LPS [137]. The central role of ROS in the impairment of mitochondrial function and eventual induction of mitophagy in sepsis was demonstrated in FVB mice that were treated with LPS and the antioxidant N-acetylcysteine, as well as in LPS-treated mice that overexpress catalase [134]. Both pharmacologic and genetic anti-oxidant interventions prevented LPS-related contractile dysfunction and were associated with reduced levels of autophagy, presumably due to limited ROS accumulation and prevention of mitochondrial damage. In agreement with the studies in animal models, treatment of septic patients with levosimendan, a calcium sensitizer with antioxidant properties, improves cardiac function [138]. Although the beneficial effects of levosimendan on cardiac function could be attributed to its established positive inotropic effects [139], the improvement in mitochondrial number and function that was observed in muscle biopsies from septic patients that were treated with this drug [140] indicates that its beneficial effects in cardiac function may be at least partially accounted for by improved cardiac mitochondrial health.
Conclusion
Sepsis-related cardiac dysfunction is associated with increased inflammation, impaired energetics, and attenuated adrenergic signaling in the heart. While each of these components is important to be resolved in order to correct cardiac function, it seems that therapeutic approaches in septic patients should probably include a combination of anti-inflammatory treatment along with stimulation of energy production in the heart. Moreover, interventions that aim to restore cardiac adrenergic signaling and particularly the function of βarr may have dual effects by improving contractility and reducing cardiac inflammation.
Acknowledgments
Funding Drs. Drosatos, Schulze, and Goldberg are supported by grants through the National Heart, Lung, and Blood Institute (NHLBI) (HL112853, KD; HL114813, PCS; HL45095 and HL73029, IJG). Dr. Lymperopoulos is supported by an AHA Scientist Development Grant (No. 09SDG2010138, National Center).
Footnotes
Conflict of Interest Konstantinos Drosatos, Anastasios Lymperopoulos, Peter Johannes Kennel, Nina Pollak, P. Christian Schulze, and Ira J. Goldberg declare that they have no conflict of interest.
Compliance with Ethics Guidelines
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
Contributor Information
Konstantinos Drosatos, Email: drosatos@temple.edu, Metabolic Biology Laboratory, Center for Translational Medicine, Department of Pharmacology, Temple University School of Medicine, 3500 N. Broad Street, MERB-951, Philadelphia, PA 19140, USA.
Anastasios Lymperopoulos, Email: al806@nova.edu, Neurohormonal Control of the Circulation Lab, Department of Pharmaceutical Sciences, Nova Southeastern University College of Pharmacy, 3200 S. University Dr., Health Professions Division (Terry) Bldg/Room 1338, Fort Lauderdale, FL 33328, USA.
Peter Johannes Kennel, Email: pjk2127@columbia.edu, Division of Cardiology, Columbia University College of Physicians and Surgeons, New York, NY 10032, USA.
Nina Pollak, Email: pcs2121@columbia.edu, Institute of Molecular Biosciences, University of Graz, 8010 Graz, Austria.
P. Christian Schulze, Email: nina.pollak@gmx.at, Division of Cardiology, Columbia University College of Physicians and Surgeons, New York, NY 10032, USA.
Ira J. Goldberg, Email: Ira.Goldberg@NYUMC.org, Division of Endocrinology, Diabetes & Metabolism, NYU-Langone School of Medicine, 522 First Avenue, New York, NY 10016, USA
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Lagu T, Rothberg MB, Shieh MS, et al. Hospitalizations, costs, and outcomes of severe sepsis in the United States 2003 to 2007. Crit Care Med. 2012;40:754–61. doi: 10.1097/CCM.0b013e318232db65. [DOI] [PubMed] [Google Scholar]
- 2.Angus DC, Linde-Zwirble WT, Lidicker J, et al. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–10. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Annane D, Bellissant E, Cavaillon JM. Septic shock. Lancet. 2005;365:63–78. doi: 10.1016/S0140-6736(04)17667-8. [DOI] [PubMed] [Google Scholar]
- 4.Levy MM, Fink MP, Marshall JC, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Crit Care Med. 2003;31:1250–6. doi: 10.1097/01.CCM.0000050454.01978.3B. [DOI] [PubMed] [Google Scholar]
- 5.Zaky A, Deem S, Bendjelid K, Treggiari MM. Characterization of cardiac dysfunction in sepsis: an ongoing challenge. Shock. 2014;41:12–24. doi: 10.1097/SHK.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 6.Ren J, Wu S. A burning issue: do sepsis and systemic inflammatory response syndrome (SIRS) directly contribute to cardiac dysfunction? Front Biosci. 2006;11:15–22. doi: 10.2741/1776. [DOI] [PubMed] [Google Scholar]
- 7.Hunter JD, Doddi M. Sepsis and the heart. Br J Anaesth. 2010;104:3–11. doi: 10.1093/bja/aep339. [DOI] [PubMed] [Google Scholar]
- 8.Court O, Kumar A, Parrillo JE. Clinical review: myocardial depression in sepsis and septic shock. Crit Care. 2002;6:500–8. doi: 10.1186/cc1822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zanotti-Cavazzoni SL, Hollenberg SM. Cardiac dysfunction in severe sepsis and septic shock. Curr Opin Crit Care. 2009;15:392–7. doi: 10.1097/MCC.0b013e3283307a4e. [DOI] [PubMed] [Google Scholar]
- 10.Landesberg G, Gilon D, Meroz Y, et al. Diastolic dysfunction and mortality in severe sepsis and septic shock. Eur Heart J. 2012;33:895–903. doi: 10.1093/eurheartj/ehr351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kumar A, Thota V, Dee L, et al. Tumor necrosis factor alpha and interleukin 1beta are responsible for in vitro myocardial cell depression induced by human septic shock serum. J Exp Med. 1996;183:949–58. doi: 10.1084/jem.183.3.949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hoffmann JN, Werdan K, Hartl WH, et al. Hemofiltrate from patients with severe sepsis and depressed left ventricular contractility contains cardiotoxic compounds. Shock. 1999;12:174–80. doi: 10.1097/00024382-199909000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Natanson C, Eichenholz PW, Danner RL, et al. Endotoxin and tumor necrosis factor challenges in dogs simulate the cardiovascular profile of human septic shock. J Exp Med. 1989;169:823–32. doi: 10.1084/jem.169.3.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Finkel MS, Oddis CV, Jacob TD, et al. Negative inotropic effects of cytokines on the heart mediated by nitric oxide. Science. 1992;257:387–9. doi: 10.1126/science.1631560. [DOI] [PubMed] [Google Scholar]
- 15.Stein B, Frank P, Schmitz W, et al. Endotoxin and cytokines induce direct cardiodepressive effects in mammalian cardiomyocytes via induction of nitric oxide synthase. J Mol Cell Cardiol. 1996;28:1631–9. doi: 10.1006/jmcc.1996.0153. [DOI] [PubMed] [Google Scholar]
- 16.Schulz R, Panas DL, Catena R, et al. The role of nitric oxide in cardiac depression induced by interleukin-1 beta and tumour necrosis factor-alpha. Br J Pharmacol. 1995;114:27–34. doi: 10.1111/j.1476-5381.1995.tb14901.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhong J, Hwang TC, Adams HR, Rubin LJ. Reduced L-type calcium current in ventricular myocytes from endotoxemic guinea pigs. Am J Physiol. 1997;273:H2312–24. doi: 10.1152/ajpheart.1997.273.5.H2312. [DOI] [PubMed] [Google Scholar]
- 18.Goldhaber JI, Kim KH, Natterson PD, et al. Effects of TNF-alpha on [Ca2+]i and contractility in isolated adult rabbit ventricular myocytes. Am J Physiol. 1996;271:H1449–55. doi: 10.1152/ajpheart.1996.271.4.H1449. [DOI] [PubMed] [Google Scholar]
- 19.de Montmollin E, Aboab J, Mansart A, Annane D. Bench-to-bedside review: beta-adrenergic modulation in sepsis. Crit Care. 2009;13:230. doi: 10.1186/cc8026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Drosatos K, Drosatos-Tampakaki Z, Khan R, et al. Inhibition of C-JUN-N-terminal kinase increases cardiac PPAR{alpha} expression and fatty acid oxidation and prevents LPS-induced heart dysfunction. J Biol Chem. 2011;286:36331–9. doi: 10.1074/jbc.M111.272146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Drosatos K, Khan RS, Trent CM, et al. Peroxisome proliferator-activated receptor-gamma activation prevents sepsis-related cardiac dysfunction and mortality in mice. Circ Heart Fail. 2013;6:550–62. doi: 10.1161/CIRCHEARTFAILURE.112.000177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22•.Schilling J, Lai L, Sambandam N, et al. Toll-like receptor-mediated inflammatory signaling reprograms cardiac energy metabolism by repressing peroxisome proliferator-activated receptor {gamma} coactivator-1 signaling. Circ Heart Fail. 2011;4:474–82. doi: 10.1161/CIRCHEARTFAILURE.110.959833. This study showed that activation of PGC-1, a transcriptional co-activator of PPARs, which promotes cardiac fatty acid oxidation and mitochondrial biogenesis, prevents septic cardiac dysfunction. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Doi K, Leelahavanichkul A, Yuen PS, Star RA. Animal models of sepsis and sepsis-induced kidney injury. J Clin Invest. 2009;119:2868–78. doi: 10.1172/JCI39421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cruz DN, Antonelli M, Fumagalli R, et al. Early use of polymyxin B hemoperfusion in abdominal septic shock: the EUPHAS randomized controlled trial. JAMA. 2009;301:2445–52. doi: 10.1001/jama.2009.856. [DOI] [PubMed] [Google Scholar]
- 25.Docke WD, Randow F, Syrbe U, et al. Monocyte deactivation in septic patients: restoration by IFN-gamma treatment. Nat Med. 1997;3:678–81. doi: 10.1038/nm0697-678. [DOI] [PubMed] [Google Scholar]
- 26.Meisel C, Schefold JC, Pschowski R, et al. Granulocyte-macrophage colony-stimulating factor to reverse sepsis-associated immunosuppression: a double-blind, randomized, placebo-controlled multicenter trial. Am J Respir Crit Care Med. 2009;180:640–8. doi: 10.1164/rccm.200903-0363OC. [DOI] [PubMed] [Google Scholar]
- 27.Venet F, Foray AP, Villars-Mechin A, et al. IL-7 restores lymphocyte functions in septic patients. J Immunol. 2012;189:5073–81. doi: 10.4049/jimmunol.1202062. [DOI] [PubMed] [Google Scholar]
- 28.Schulte W, Bernhagen J, Bucala R. Cytokines in sepsis: potent immunoregulators and potential therapeutic targets—an updated view. Mediat Inflamm. 2013;2013:165974. doi: 10.1155/2013/165974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hotchkiss RS, Monneret G, Payen D. Sepsis-induced immunosuppression: from cellular dysfunctions to immunotherapy. Nat Rev Immunol. 2013;13:862–74. doi: 10.1038/nri3552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reddy RC, Chen GH, Tekchandani PK, Standiford TJ. Sepsis-induced immunosuppression: from bad to worse. Immunol Res. 2001;24:273–87. doi: 10.1385/IR:24:3:273. [DOI] [PubMed] [Google Scholar]
- 31.Volk HD, Reinke P, Docke WD. Clinical aspects: from systemic inflammation to ‘immunoparalysis’. Chem Immunol. 2000;74:162–77. doi: 10.1159/000058753. [DOI] [PubMed] [Google Scholar]
- 32.Akira S, Takeda K, Kaisho T. Toll-like receptors: critical proteins linking innate and acquired immunity. Nat Immunol. 2001;2:675–80. doi: 10.1038/90609. [DOI] [PubMed] [Google Scholar]
- 33.Zuckerman SH, Evans GF, Guthrie L. Transcriptional and post-transcriptional mechanisms involved in the differential expression of LPS-induced IL-1 and TNF mRNA. Immunology. 1991;73:460–5. [PMC free article] [PubMed] [Google Scholar]
- 34.Hambleton J, Weinstein SL, Lem L, DeFranco AL. Activation of c-Jun N-terminal kinase in bacterial lipopolysaccharide-stimulated macrophages. Proc Natl Acad Sci U S A. 1996;93:2774–8. doi: 10.1073/pnas.93.7.2774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sanghera JS, Weinstein SL, Aluwalia M, et al. Activation of multiple proline-directed kinases by bacterial lipopolysaccharide in murine macrophages. J Immunol. 1996;156:4457–65. [PubMed] [Google Scholar]
- 36.Ebach DR, Riehl TE, Stenson WF. Opposing effects of tumor necrosis factor receptor 1 and 2 in sepsis due to cecal ligation and puncture. Shock. 2005;23:311–8. doi: 10.1097/01.shk.0000157301.87051.77. [DOI] [PubMed] [Google Scholar]
- 37.Beutler B, Milsark IW, Cerami AC. Passive immunization against cachectin/tumor necrosis factor protects mice from lethal effect of endotoxin. Science. 1985;229:869–71. doi: 10.1126/science.3895437. [DOI] [PubMed] [Google Scholar]
- 38.Redl H, Schlag G, Paul E, et al. Endogenous modulators of TNF and IL-1 response are under partial control of TNF in baboon bacteremia. Am J Physiol. 1996;271:R1193–8. doi: 10.1152/ajpregu.1996.271.5.R1193. [DOI] [PubMed] [Google Scholar]
- 39.Bengtsson A, Redl H, Schlag G, et al. Effects on complement activation and cytokine (TNF-alpha and IL-8) release of infusion of anti-TNF-antibodies or a xanthine derivative (HWA 138) in septic baboons. Acta Anaesthesiol Scand. 1996;40:244–9. doi: 10.1111/j.1399-6576.1996.tb04427.x. [DOI] [PubMed] [Google Scholar]
- 40.Hinshaw LB, Tekamp-Olson P, Chang AC, et al. Survival of primates in LD100 septic shock following therapy with antibody to tumor necrosis factor (TNF alpha) Circ Shock. 1990;30:279–92. [PubMed] [Google Scholar]
- 41.Fisher CJ, Jr, Opal SM, Dhainaut JF, et al. Influence of an anti-tumor necrosis factor monoclonal antibody on cytokine levels in patients with sepsis. The CB0006 sepsis syndrome study group. Crit Care Med. 1993;21:318–27. doi: 10.1097/00003246-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 42.Dhainaut JF, Vincent JL, Richard C, et al. CDP571, a humanized antibody to human tumor necrosis factor-alpha: safety, pharmacokinetics, immune response, and influence of the antibody on cytokine concentrations in patients with septic shock. CPD571 sepsis study group. Crit Care Med. 1995;23:1461–9. doi: 10.1097/00003246-199509000-00004. [DOI] [PubMed] [Google Scholar]
- 43.Fisher CJ, Jr, Agosti JM, Opal SM, et al. Treatment of septic shock with the tumor necrosis factor receptor: Fc fusion protein. The soluble TNF receptor sepsis study group. N Engl J Med. 1996;334:1697–702. doi: 10.1056/NEJM199606273342603. [DOI] [PubMed] [Google Scholar]
- 44.Abraham E, Glauser MP, Butler T, et al. p55 Tumor necrosis factor receptor fusion protein in the treatment of patients with severe sepsis and septic shock. A randomized controlled multicenter trial. Ro 45–2081 study group. JAMA. 1997;277:1531–8. [PubMed] [Google Scholar]
- 45.Tsujino M, Hirata Y, Imai T, et al. Induction of nitric oxide synthase gene by interleukin-1 beta in cultured rat cardiomyocytes. Circulation. 1994;90:375–83. doi: 10.1161/01.cir.90.1.375. [DOI] [PubMed] [Google Scholar]
- 46.Brady AJ, Poole-Wilson PA, Harding SE, Warren JB. Nitric oxide production within cardiac myocytes reduces their contractility in endotoxemia. Am J Physiol. 1992;263:H1963–6. doi: 10.1152/ajpheart.1992.263.6.H1963. [DOI] [PubMed] [Google Scholar]
- 47.Arnalich F, Lopez-Maderuelo D, Codoceo R, et al. Interleukin-1 receptor antagonist gene polymorphism and mortality in patients with severe sepsis. Clin Exp Immunol. 2002;127:331–6. doi: 10.1046/j.1365-2249.2002.01743.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Aiura K, Gelfand JA, Burke JF, et al. Interleukin-1 (IL-1) receptor antagonist prevents Staphylococcus epidermidis-induced hypotension and reduces circulating levels of tumor necrosis factor and IL-1 beta in rabbits. Infect Immun. 1993;61:3342–50. doi: 10.1128/iai.61.8.3342-3350.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Remick DG, Call DR, Ebong SJ, et al. Combination immunotherapy with soluble tumor necrosis factor receptors plus interleukin 1 receptor antagonist decreases sepsis mortality. Crit Care Med. 2001;29:473–81. doi: 10.1097/00003246-200103000-00001. [DOI] [PubMed] [Google Scholar]
- 50.Opal SM, Fisher CJ, Jr, Dhainaut JF, et al. Confirmatory interleukin-1 receptor antagonist trial in severe sepsis: a phase III, randomized, double-blind, placebo-controlled, multicenter trial. The interleukin-1 receptor antagonist sepsis investigator group. Crit Care Med. 1997;25:1115–24. doi: 10.1097/00003246-199707000-00010. [DOI] [PubMed] [Google Scholar]
- 51.Bone RC, Fisher CJ, Jr, Clemmer TP, et al. A controlled clinical trial of high-dose methylprednisolone in the treatment of severe sepsis and septic shock. N Engl J Med. 1987;317:653–8. doi: 10.1056/NEJM198709103171101. [DOI] [PubMed] [Google Scholar]
- 52.Luce JM, Montgomery AB, Marks JD, et al. Ineffectiveness of high-dose methylprednisolone in preventing parenchymal lung injury and improving mortality in patients with septic shock. Am Rev Respir Dis. 1988;138:62–8. doi: 10.1164/ajrccm/138.1.62. [DOI] [PubMed] [Google Scholar]
- 53.Annane D, Bellissant E, Bollaert PE, et al. Corticosteroids in the treatment of severe sepsis and septic shock in adults: a systematic review. JAMA. 2009;301:2362–75. doi: 10.1001/jama.2009.815. [DOI] [PubMed] [Google Scholar]
- 54.Fisher CJ, Jr, Dhainaut JF, Opal SM, et al. Recombinant human interleukin 1 receptor antagonist in the treatment of patients with sepsis syndrome. Results from a randomized, double-blind, placebo-controlled trial. Phase III rhIL-1ra sepsis syndrome study group. JAMA. 1994;271:1836–43. [PubMed] [Google Scholar]
- 55.Reinhart K, Karzai W. Anti-tumor necrosis factor therapy in sepsis: update on clinical trials and lessons learned. Crit Care Med. 2001;29:S121–5. doi: 10.1097/00003246-200107001-00037. [DOI] [PubMed] [Google Scholar]
- 56.Boomer JS, To K, Chang KC, et al. Immunosuppression in patients who die of sepsis and multiple organ failure. JAMA. 2011;306:2594–605. doi: 10.1001/jama.2011.1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Andreu-Ballester JC, Tormo-Calandin C, Garcia-Ballesteros C, et al. Association of gammadelta T cells with disease severity and mortality in septic patients. Clin Vaccine Immunol. 2013;20:738–46. doi: 10.1128/CVI.00752-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Carson WF, Cavassani KA, Dou Y, Kunkel SL. Epigenetic regulation of immune cell functions during post-septic immunosuppression. Epigenetics. 2011;6:273–83. doi: 10.4161/epi.6.3.14017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Monneret G, Lepape A, Voirin N, et al. Persisting low monocyte human leukocyte antigen-DR expression predicts mortality in septic shock. Intensive Care Med. 2006;32:1175–83. doi: 10.1007/s00134-006-0204-8. [DOI] [PubMed] [Google Scholar]
- 60.Xiang Y, Kobilka BK. Myocyte adrenoceptor signaling pathways. Science. 2003;300:1530–2. doi: 10.1126/science.1079206. [DOI] [PubMed] [Google Scholar]
- 61.Xiao RP, Zhu W, Zheng M, et al. Subtype-specific beta-adrenoceptor signaling pathways in the heart and their potential clinical implications. Trends Pharmacol Sci. 2004;25:358–65. doi: 10.1016/j.tips.2004.05.007. [DOI] [PubMed] [Google Scholar]
- 62.Devic E, Xiang Y, Gould D, Kobilka B. Beta-adrenergic receptor subtype-specific signaling in cardiac myocytes from beta(1) and beta(2) adrenoceptor knockout mice. Mol Pharmacol. 2001;60:577–83. [PubMed] [Google Scholar]
- 63.Bernstein D, Fajardo G, Zhao M, et al. Differential cardioprotective/cardiotoxic effects mediated by beta-adrenergic receptor subtypes. Am J Physiol Heart Circ Physiol. 2005;289:H2441–9. doi: 10.1152/ajpheart.00005.2005. [DOI] [PubMed] [Google Scholar]
- 64.Chesley A, Lundberg MS, Asai T, et al. The beta(2)-adrenergic receptor delivers an antiapoptotic signal to cardiac myocytes through G(i)-dependent coupling to phosphatidylinositol 3′-kinase. Circ Res. 2000;87:1172–9. doi: 10.1161/01.res.87.12.1172. [DOI] [PubMed] [Google Scholar]
- 65.Patterson AJ, Zhu W, Chow A, et al. Protecting the myocardium: a role for the beta2 adrenergic receptor in the heart. Crit Care Med. 2004;32:1041–8. doi: 10.1097/01.ccm.0000120049.43113.90. [DOI] [PubMed] [Google Scholar]
- 66.Xiao RP, Avdonin P, Zhou YY, et al. Coupling of beta2-adrenoceptor to Gi proteins and its physiological relevance in murine cardiac myocytes. Circ Res. 1999;84:43–52. doi: 10.1161/01.res.84.1.43. [DOI] [PubMed] [Google Scholar]
- 67.Communal C, Singh K, Sawyer DB, Colucci WS. Opposing effects of beta(1)- and beta(2)-adrenergic receptors on cardiac myocyte apoptosis: role of a pertussis toxin-sensitive G protein. Circulation. 1999;100:2210–2. doi: 10.1161/01.cir.100.22.2210. [DOI] [PubMed] [Google Scholar]
- 68.Zhu WZ, Zheng M, Koch WJ, et al. Dual modulation of cell survival and cell death by beta(2)-adrenergic signaling in adult mouse cardiac myocytes. Proc Natl Acad Sci U S A. 2001;98:1607–12. doi: 10.1073/pnas.98.4.1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Richter W, Day P, Agrawal R, et al. Signaling from beta1- and beta2-adrenergic receptors is defined by differential interactions with PDE4. EMBO J. 2008;27:384–93. doi: 10.1038/sj.emboj.7601968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rengo G, Lymperopoulos A, Koch WJ. Future g protein-coupled receptor targets for treatment of heart failure. Curr Treat Options Cardiovasc Med. 2009;11:328–38. doi: 10.1007/s11936-009-0033-5. [DOI] [PubMed] [Google Scholar]
- 71.Lymperopoulos A, Bathgate A. Arrestins in the cardiovascular system. Prog Mol Biol Transl Sci. 2013;118:297–334. doi: 10.1016/B978-0-12-394440-5.00012-7. [DOI] [PubMed] [Google Scholar]
- 72.DeWire SM, Ahn S, Lefkowitz RJ, Shenoy SK. Beta-arrestins and cell signaling. Annu Rev Physiol. 2007;69:483–510. doi: 10.1146/annurev.physiol.69.022405.154749. [DOI] [PubMed] [Google Scholar]
- 73.Witherow DS, Garrison TR, Miller WE, Lefkowitz RJ. Beta-arrestin inhibits NF-kappaB activity by means of its interaction with the NF-kappaB inhibitor IkappaBalpha. Proc Natl Acad Sci U S A. 2004;101:8603–7. doi: 10.1073/pnas.0402851101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Gao H, Sun Y, Wu Y, et al. Identification of beta-arrestin2 as a G protein-coupled receptor-stimulated regulator of NF-kappaB pathways. Mol Cell. 2004;14:303–17. doi: 10.1016/s1097-2765(04)00216-3. [DOI] [PubMed] [Google Scholar]
- 75.Annane D, Trabold F, Sharshar T, et al. Inappropriate sympathetic activation at onset of septic shock: a spectral analysis approach. Am J Respir Crit Care Med. 1999;160:458–65. doi: 10.1164/ajrccm.160.2.9810073. [DOI] [PubMed] [Google Scholar]
- 76.Kovarik MF, Jones SB, Romano FD. Plasma catecholamines following cecal ligation and puncture in the rat. Circ Shock. 1987;22:281–90. [PubMed] [Google Scholar]
- 77.Boldt J, Menges T, Kuhn D, et al. Alterations in circulating vasoactive substances in the critically ill—a comparison between survivors and non-survivors. Intensive Care Med. 1995;21:218–25. doi: 10.1007/BF01701475. [DOI] [PubMed] [Google Scholar]
- 78.Jones AE, Craddock PA, Tayal VS, Kline JA. Diagnostic accuracy of left ventricular function for identifying sepsis among emergency department patients with nontraumatic symptomatic undifferentiated hypotension. Shock. 2005;24:513–7. doi: 10.1097/01.shk.0000186931.02852.5f. [DOI] [PubMed] [Google Scholar]
- 79.Azimi G, Vincent JL. Ultimate survival from septic shock. Resuscitation. 1986;14:245–53. doi: 10.1016/0300-9572(86)90068-7. [DOI] [PubMed] [Google Scholar]
- 80.Dunser MW, Hasibeder WR. Sympathetic overstimulation during critical illness: adverse effects of adrenergic stress. J Intensive Care Med. 2009;24:293–316. doi: 10.1177/0885066609340519. [DOI] [PubMed] [Google Scholar]
- 81.Hahn PY, Wang P, Tait SM, et al. Sustained elevation in circulating catecholamine levels during polymicrobial sepsis. Shock. 1995;4:269–73. doi: 10.1097/00024382-199510000-00007. [DOI] [PubMed] [Google Scholar]
- 82.Gulick T, Chung MK, Pieper SJ, et al. Interleukin 1 and tumor necrosis factor inhibit cardiac myocyte beta-adrenergic responsiveness. Proc Natl Acad Sci U S A. 1989;86:6753–7. doi: 10.1073/pnas.86.17.6753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bohm M, Kirchmayr R, Gierschik P, Erdmann E. Increase of myocardial inhibitory G-proteins in catecholamine-refractory septic shock or in septic multiorgan failure. Am J Med. 1995;98:183–6. doi: 10.1016/S0002-9343(99)80402-1. [DOI] [PubMed] [Google Scholar]
- 84.Macarthur H, Westfall TC, Riley DP, et al. Inactivation of catecholamines by superoxide gives new insights on the pathogenesis of septic shock. Proc Natl Acad Sci U S A. 2000;97:9753–8. doi: 10.1073/pnas.97.17.9753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Hare JM, Loh E, Creager MA, Colucci WS. Nitric oxide inhibits the positive inotropic response to beta-adrenergic stimulation in humans with left ventricular dysfunction. Circulation. 1995;92:2198–203. doi: 10.1161/01.cir.92.8.2198. [DOI] [PubMed] [Google Scholar]
- 86.Barth E, Radermacher P, Thiemermann C, et al. Role of inducible nitric oxide synthase in the reduced responsiveness of the myocardium to catecholamines in a hyperdynamic, murine model of septic shock. Crit Care Med. 2006;34:307–13. doi: 10.1097/01.ccm.0000199070.46812.21. [DOI] [PubMed] [Google Scholar]
- 87.Lymperopoulos A, Rengo G, Koch WJ. GRK2 inhibition in heart failure: something old, something new. Curr Pharm Des. 2012;18:186–91. doi: 10.2174/138161212799040510. [DOI] [PubMed] [Google Scholar]
- 88.Salazar NC, Vallejos X, Siryk A, et al. GRK2 blockade with betaARKct is essential for cardiac beta2-adrenergic receptor signaling towards increased contractility. Cell Commun Signal. 2013;11:64. doi: 10.1186/1478-811X-11-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Fan H, Bitto A, Zingarelli B, et al. Beta-arrestin 2 negatively regulates sepsis-induced inflammation. Immunology. 2010;130:344–51. doi: 10.1111/j.1365-2567.2009.03185.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Valen G, Yan ZQ, Hansson GK. Nuclear factor kappa-B and the heart. J Am Coll Cardiol. 2001;38:307–14. doi: 10.1016/s0735-1097(01)01377-8. [DOI] [PubMed] [Google Scholar]
- 91.Ibrahim-Zada I, Rhee P, Gomez CT, et al. Inhibition of sepsis-induced inflammatory response by beta1-adrenergic antagonists. J Trauma Acute Care Surg. 2014;76:320–7. doi: 10.1097/TA.0000000000000113. discussion 327–8. [DOI] [PubMed] [Google Scholar]
- 92.Pinsky MR. Is there a role for beta-blockade in septic shock? JAMA. 2013;310:1677–8. doi: 10.1001/jama.2013.278478. [DOI] [PubMed] [Google Scholar]
- 93.Godlewski G, Schlicker E, Baranowska U, Malinowska B. Recruitment of functionally active heart beta2-adrenoceptors in the initial phase of endotoxic shock in pithed rats. Shock. 2006;26:510–5. doi: 10.1097/01.shk.0000228794.95302.c3. [DOI] [PubMed] [Google Scholar]
- 94.Valen G. Innate immunity and remodelling. Heart Fail Rev. 2011;16:71–8. doi: 10.1007/s10741-010-9187-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Leone M, Boyadjiev I, Boulos E, et al. A reappraisal of isoproterenol in goal-directed therapy of septic shock. Shock. 2006;26:353–7. doi: 10.1097/01.shk.0000226345.55657.66. [DOI] [PubMed] [Google Scholar]
- 96.Fink T, Heymann P, Taha-Melitz S, et al. Dobutamine pretreatment improves survival, liver function, and hepatic microcirculation after polymicrobial sepsis in rat. Shock. 2013;40:129–35. doi: 10.1097/SHK.0b013e31829c361d. [DOI] [PubMed] [Google Scholar]
- 97.Cudmore LA, Muurlink T, Whittem T, Bailey SR. Effects of oral clenbuterol on the clinical and inflammatory response to endotoxaemia in the horse. Res Vet Sci. 2013;94:682–6. doi: 10.1016/j.rvsc.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 98.Morelli A, Ertmer C, Westphal M, et al. Effect of heart rate control with esmolol on hemodynamic and clinical outcomes in patients with septic shock: a randomized clinical trial. JAMA. 2013;310:1683–91. doi: 10.1001/jama.2013.278477. [DOI] [PubMed] [Google Scholar]
- 99.Gouni I, Oka K, Etienne J, Chan L. Endotoxin-induced hypertriglyceridemia is mediated by suppression of lipoprotein lipase at a post-transcriptional level. J Lipid Res. 1993;34:139–46. [PubMed] [Google Scholar]
- 100.Kaufmann RL, Matson CF, Beisel WR. Hypertriglyceridemia produced by endotoxin: role of impaired triglyceride disposal mechanisms. J Infect Dis. 1976;133:548–55. doi: 10.1093/infdis/133.5.548. [DOI] [PubMed] [Google Scholar]
- 101.Nogueira AC, Kawabata V, Biselli P, et al. Changes in plasma free fatty acid levels in septic patients are associated with cardiac damage and reduction in heart rate variability. Shock. 2008;29:342–8. doi: 10.1097/shk.0b013e31815abbc6. [DOI] [PubMed] [Google Scholar]
- 102.Bagby GJ, Spitzer JA. Lipoprotein lipase activity in rat heart and adipose tissue during endotoxic shock. Am J Physiol. 1980;238:H325–30. doi: 10.1152/ajpheart.1980.238.3.H325. [DOI] [PubMed] [Google Scholar]
- 103.Scholl RA, Lang CH, Bagby GJ. Hypertriglyceridemia and its relation to tissue lipoprotein lipase activity in endotoxemic, Escherichia coli bacteremic, and polymicrobial septic rats. J Surg Res. 1984;37:394–401. doi: 10.1016/0022-4804(84)90205-1. [DOI] [PubMed] [Google Scholar]
- 104.Bagby GJ, Corll CB, Martinez RR. Triacylglycerol kinetics in endotoxic rats with suppressed lipoprotein lipase activity. Am J Physiol. 1987;253:E59–64. doi: 10.1152/ajpendo.1987.253.1.E59. [DOI] [PubMed] [Google Scholar]
- 105.Neubauer S. The failing heart—an engine out of fuel. N Engl J Med. 2007;356:1140–51. doi: 10.1056/NEJMra063052. [DOI] [PubMed] [Google Scholar]
- 106.Osorio JC, Stanley WC, Linke A, et al. Impaired myocardial fatty acid oxidation and reduced protein expression of retinoid X receptor-alpha in pacing-induced heart failure. Circulation. 2002;106:606–12. doi: 10.1161/01.cir.0000023531.22727.c1. [DOI] [PubMed] [Google Scholar]
- 107.Raymond RM, McLane MP, Law WR, et al. Myocardial insulin resistance during acute endotoxin shock in dogs. Diabetes. 1988;37:1684–8. doi: 10.2337/diab.37.12.1684. [DOI] [PubMed] [Google Scholar]
- 108.Tessier JP, Thurner B, Jungling E, et al. Impairment of glucose metabolism in hearts from rats treated with endotoxin. Cardiovasc Res. 2003;60:119–30. doi: 10.1016/s0008-6363(03)00320-1. [DOI] [PubMed] [Google Scholar]
- 109.Dhainaut JF, Huyghebaert MF, Monsallier JF, et al. Coronary hemodynamics and myocardial metabolism of lactate, free fatty acids, glucose, and ketones in patients with septic shock. Circulation. 1987;75:533–41. doi: 10.1161/01.cir.75.3.533. [DOI] [PubMed] [Google Scholar]
- 110.Hotchkiss RS, Rust RS, Dence CS, et al. Evaluation of the role of cellular hypoxia in sepsis by the hypoxic marker [18F]fluoromisonidazole. Am J Physiol. 1991;261:R965–72. doi: 10.1152/ajpregu.1991.261.4.R965. [DOI] [PubMed] [Google Scholar]
- 111.Lu B, Moser A, Shigenaga JK, et al. The acute phase response stimulates the expression of angiopoietin like protein 4. Biochem Biophys Res Commun. 2010;391:1737–41. doi: 10.1016/j.bbrc.2009.12.145. [DOI] [PubMed] [Google Scholar]
- 112.Feingold K, Kim MS, Shigenaga J, et al. Altered expression of nuclear hormone receptors and coactivators in mouse heart during the acute-phase response. Am J Physiol Endocrinol Metab. 2004;286:E201–7. doi: 10.1152/ajpendo.00205.2003. [DOI] [PubMed] [Google Scholar]
- 113.Jia L, Takahashi M, Morimoto H, et al. Changes in cardiac lipid metabolism during sepsis: the essential role of very low-density lipoprotein receptors. Cardiovasc Res. 2006;69:545–55. doi: 10.1016/j.cardiores.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 114.Read TE, Harris HW, Grunfeld C, et al. The protective effect of serum lipoproteins against bacterial lipopolysaccharide. Eur Heart J. 1993;14(Suppl K):125–9. [PubMed] [Google Scholar]
- 115.Ghoshal S, Witta J, Zhong J, et al. Chylomicrons promote intestinal absorption of lipopolysaccharides. J Lipid Res. 2009;50:90–7. doi: 10.1194/jlr.M800156-JLR200. [DOI] [PubMed] [Google Scholar]
- 116.Memon RA, Bass NM, Moser AH, et al. Down-regulation of liver and heart specific fatty acid binding proteins by endotoxin and cytokines in vivo. Biochim Biophys Acta. 1999;1440:118–26. doi: 10.1016/s1388-1981(99)00120-1. [DOI] [PubMed] [Google Scholar]
- 117.Memon RA, Fuller J, Moser AH, et al. In vivo regulation of acyl-CoA synthetase mRNA and activity by endotoxin and cytokines. Am J Physiol. 1998;275:E64–72. doi: 10.1152/ajpendo.1998.275.1.E64. [DOI] [PubMed] [Google Scholar]
- 118.Uji Y, Yamamoto H, Tsuchihashi H, et al. Adiponectin deficiency is associated with severe polymicrobial sepsis, high inflammatory cytokine levels, and high mortality. Surgery. 2009;145:550–7. doi: 10.1016/j.surg.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 119.Haraguchi G, Kosuge H, Maejima Y, et al. Pioglitazone reduces systematic inflammation and improves mortality in apolipoprotein E knockout mice with sepsis. Intensive Care Med. 2008;34:1304–12. doi: 10.1007/s00134-008-1024-9. [DOI] [PubMed] [Google Scholar]
- 120.Chima RS, Hake PW, Piraino G, et al. Ciglitazone ameliorates lung inflammation by modulating the inhibitor kappaB protein kinase/nuclear factor-kappaB pathway after hemorrhagic shock. Crit Care Med. 2008;36:2849–57. doi: 10.1097/ccm.0b013e318187810e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Siddiqui AM, Cui X, Wu R, et al. The anti-inflammatory effect of curcumin in an experimental model of sepsis is mediated by up-regulation of peroxisome proliferator-activated receptor-gamma. Crit Care Med. 2006;34:1874–82. doi: 10.1097/01.CCM.0000221921.71300.BF. [DOI] [PubMed] [Google Scholar]
- 122.Liu D, Zeng BX, Zhang SH, Yao SL. Rosiglitazone, an agonist of peroxisome proliferator-activated receptor gamma, reduces pulmonary inflammatory response in a rat model of endotoxemia. Inflamm Res. 2005;54:464–70. doi: 10.1007/s00011-005-1379-0. [DOI] [PubMed] [Google Scholar]
- 123.Zingarelli B, Cook JA. Peroxisome proliferator-activated receptor-gamma is a new therapeutic target in sepsis and inflammation. Shock. 2005;23:393–9. doi: 10.1097/01.shk.0000160521.91363.88. [DOI] [PubMed] [Google Scholar]
- 124.Yamauchi T, Kamon J, Waki H, et al. The mechanisms by which both heterozygous peroxisome proliferator-activated receptor gamma (PPARgamma) deficiency and PPARgamma agonist improve insulin resistance. J Biol Chem. 2001;276:41245–54. doi: 10.1074/jbc.M103241200. [DOI] [PubMed] [Google Scholar]
- 125.Yang WS, Jeng CY, Wu TJ, et al. Synthetic peroxisome proliferator-activated receptor-gamma agonist, rosiglitazone, increases plasma levels of adiponectin in type 2 diabetic patients. Diabetes Care. 2002;25:376–80. doi: 10.2337/diacare.25.2.376. [DOI] [PubMed] [Google Scholar]
- 126.Gustafson B, Jack MM, Cushman SW, Smith U. Adiponectin gene activation by thiazolidinediones requires PPAR gamma 2, but not C/EBP alpha-evidence for differential regulation of the aP2 and adiponectin genes. Biochem Biophys Res Commun. 2003;308:933–9. doi: 10.1016/s0006-291x(03)01518-3. [DOI] [PubMed] [Google Scholar]
- 127.Fang X, Palanivel R, Cresser J, et al. An APPL1-AMPK signaling axis mediates beneficial metabolic effects of adiponectin in the heart. Am J Physiol Endocrinol Metab. 2010;299:E721–9. doi: 10.1152/ajpendo.00086.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Yoon MJ, Lee GY, Chung JJ, et al. Adiponectin increases fatty acid oxidation in skeletal muscle cells by sequential activation of AMP-activated protein kinase, p38 mitogen-activated protein kinase, and peroxisome proliferator-activated receptor alpha. Diabetes. 2006;55:2562–70. doi: 10.2337/db05-1322. [DOI] [PubMed] [Google Scholar]
- 129.Reynolds K, Novosad B, Hoffhines A, et al. Pretreatment with troglitazone decreases lethality during endotoxemia in mice. J Endotoxin Res. 2002;8:307–14. doi: 10.1179/096805102125000515. [DOI] [PubMed] [Google Scholar]
- 130.Kapoor A, Shintani Y, Collino M, et al. Protective role of peroxisome proliferator-activated receptor-beta/delta in septic shock. Am J Respir Crit Care Med. 2010;182:1506–15. doi: 10.1164/rccm.201002-0240OC. [DOI] [PubMed] [Google Scholar]
- 131••.Langley RJ, Tsalik EL, Velkinburgh JC, et al. An integrated clinico-metabolomic model improves prediction of death in sepsis. Sci Transl Med. 2013;5:195ra95. doi: 10.1126/scitranslmed.3005893. This study showed that markers of increased tissue fatty acid oxidation detected in plasma of septic patients predict improved survival in sepsis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Watts JA, Kline JA, Thornton LR, et al. Metabolic dysfunction and depletion of mitochondria in hearts of septic rats. J Mol Cell Cardiol. 2004;36:141–50. doi: 10.1016/j.yjmcc.2003.10.015. [DOI] [PubMed] [Google Scholar]
- 133.Levy RJ. Mitochondrial dysfunction, bioenergetic impairment, and metabolic down-regulation in sepsis. Shock. 2007;28:24–8. doi: 10.1097/01.shk.0000235089.30550.2d. [DOI] [PubMed] [Google Scholar]
- 134.Turdi S, Han X, Huff AF, et al. Cardiac-specific overexpression of catalase attenuates lipopolysaccharide-induced myocardial contractile dysfunction: role of autophagy. Free Radic Biol Med. 2012;53:1327–38. doi: 10.1016/j.freeradbiomed.2012.07.084. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 135.Vanasco V, Magnani ND, Cimolai MC, et al. Endotoxemia impairs heart mitochondrial function by decreasing electron transfer, ATP synthesis and ATP content without affecting membrane potential. J Bioenerg Biomembr. 2012;44:243–52. doi: 10.1007/s10863-012-9426-3. [DOI] [PubMed] [Google Scholar]
- 136.Chen HW, Hsu C, Lu TS, et al. Heat shock pretreatment prevents cardiac mitochondrial dysfunction during sepsis. Shock. 2003;20:274–9. doi: 10.1097/00024382-200309000-00013. [DOI] [PubMed] [Google Scholar]
- 137.Piquereau J, Godin R, Deschenes S, et al. Protective role of PARK2/Parkin in sepsis-induced cardiac contractile and mitochondrial dysfunction. Autophagy. 2013;9:1837–51. doi: 10.4161/auto.26502. [DOI] [PubMed] [Google Scholar]
- 138.Noto A, Giacomini M, Palandi A, et al. Levosimendan in septic cardiac failure. Intensive Care Med. 2005;31:164–5. doi: 10.1007/s00134-004-2502-3. [DOI] [PubMed] [Google Scholar]
- 139.Givertz MM, Andreou C, Conrad CH, Colucci WS. Direct myocardial effects of levosimendan in humans with left ventricular dysfunction: alteration of force-frequency and relaxation-frequency relationships. Circulation. 2007;115:1218–24. doi: 10.1161/CIRCULATIONAHA.106.668640. [DOI] [PubMed] [Google Scholar]
- 140.Torraco A, Carrozzo R, Piemonte F, et al. Effects of levosimendan on mitochondrial function in patients with septic shock: a randomized trial. Biochimie. 2014;102:166–73. doi: 10.1016/j.biochi.2014.03.006. [DOI] [PubMed] [Google Scholar]