Abstract
Objective
To examine ADHD symptom persistence and factors associated with elevated symptom counts in a diverse, longitudinal community-based sample.
Method
Parents reported demographics and completed a diagnostic interview repeatedly over a 6-year period. At Time 1, 481 interviews were completed about children (5–13 years); all participants were invited to four annual follow-up interviews, and 379 (79%) completed at least one. Inattentive (IA) and hyperactive-impulsive (HI) symptom counts were modeled with logistic quantile regression, while accounting for study design complexities.
Results
The prevalence of seven IA symptoms remained stable from early childhood through late adolescence. The prevalence of eight HI symptoms decreased by more than half over time. After demographic adjustment, the upper quartile of HI symptom counts decreased with age (p < .01). High HI symptom counts persisted more among those with high IA symptom counts (p = .05).
Conclusion
This study further characterizes and provides insights into ADHD symptom trajectory through adolescence.
Keywords: attention deficit hyperactivity disorder, persistence, development
Introduction
ADHD is one of the most common behavioral disorders of childhood, affecting an estimated 5% to 11% of youth in the community (Akinbami, Liu, Pastor, & Reuben, 2011; Centers for Disease Control and Prevention, 2010; Scahill & Schwab-Stone, 2000; Visser et al., 2014; Wolraich et al., 2012). Although historically considered a disorder of childhood, ADHD research since the 1980s has shown that the disorder often persists into late adolescence and into adulthood (Barbaresi et al., 2013). Clinical guidelines have been adjusted to reflect the persistence of ADHD symptoms and associated impairment (American Academy of Pediatrics’ Subcommittee on Attention-Deficit/Hyperactivity Disorder Steering Committee on Quality Improvement and Management, 2011). Persistent ADHD is associated with negative outcomes including academic underachievement (Barbaresi, Katusic, Colligan, Weaver, & Jacobsen, 2007; Loe & Feldman, 2007), driving violations and motor vehicle collisions (Jerome, Segal, & Habinski, 2006), substance use (Molina et al., 2013), sexual risk behaviors (Flory, Molina, Pelham, Gnagy, & Smith, 2006), and unemployment (Küpper et al., 2012). For this reason, the pattern, timing, and trajectory of ADHD symptoms have important implications for providing guidance and developing treatment, management, and transition plans for children with ADHD and their families.
Prevalence of the disorder and its persistence throughout development are two prominent areas of epidemiologic ADHD research. Prevalence studies utilize data from cross-sectional study designs, and estimates have been reported from a variety of epidemiologic data sources. National surveys include items on the parent report of health-care-provider-diagnosed ADHD (Akinbami et al., 2011; Visser et al., 2014), insurance claims have been mined to create estimates of diagnosed and treated (medicated) ADHD (Getahun et al., 2013), and community-based samples have used epidemiologic screening methods and direct diagnostic interviews to determine which children meet Diagnostic and Statistical Manual of Mental Disorders (DSM) criteria (DSM-IV-TR; 4th ed., text rev.; American Psychiatric Association [APA], 2000; DSM-5; 5th ed., APA 2013; Bird et al., 2006; Wolraich et al., 2012). Although prevalence estimates vary by ascertainment method, assembling results from multiple methodologies creates a more comprehensive picture of the underlying and diagnosed prevalence of ADHD in the United States.
Characterizing ADHD persistence is methodologically more complex than estimating the disorder’s prevalence. One reason is that it requires an appropriate longitudinal data source. As highlighted by Willoughby (2003) and reviewed further by Faraone, Biederman, and Mick (2006), early ADHD persistence studies relied on clinic-based samples; this research methodology continues, likely due to the ease with which these populations are identified (Biederman, Petty, Clarke, Lomedico, & Faraone, 2010). However, findings from clinical samples may not be generalizable to the broader community of interest because those with low access to health care (Eaton et al., 2008; Goldberg, 1995), low levels of impairment (Buitelaar, Kan, & Asherson, 2011; Goodman et al., 1998), and no psychiatric comorbidity (Buitelaar et al., 2011) are less likely to be included in clinical samples. Therefore, persistence estimates from clinic-based samples may suffer selection biases and should be interpreted within the context of research from other population-based studies, when possible.
ADHD persistence can be described at the disorder level (i.e., syndromatic persistence) and symptom level (i.e., symptomatic persistence). Previous estimates of syndromatic persistence have ranged from 33% (Mannuzza & Gittelman, 1984) to 48% (Rasmussen & Gillberg, 2000). Symptomatic persistence has an even larger range in estimates, from 36% (Mannuzza & Gittelman, 1984) to 85% (Biederman et al., 1996). Some of the most comprehensive research on ADHD persistence comes from Biederman et al. (2010) who recently published a thorough report of ADHD persistence patterns using a clinical sample of Caucasian boys followed over 10 years into young adulthood. While 45% of baseline cases continued to meet full DSM-IV criteria (APA, 1994), 78% met at least one of the study’s persistence definitions. This included functional persistence, meaning participants had less than half the symptoms required for a full diagnosis but remained functionally impaired (Biederman et al., 2010).
There is a need for similar research with community samples, especially those that include girls and racial minorities, as very little is known about ADHD persistence patterns among these groups (Bauermeister et al., 2011). We are aware of only one study that has utilized a non-clinical sample and DSM-IV criteria at baseline and follow-up (Todd et al., 2008). This was a twin study focused on ADHD and subtype stability rather than on reporting persistence patterns of the disorder or symptoms.
It is also important that ADHD persistence studies continue to recognize inattention (IA) and hyperactive-impulsive (HI) trajectories separately, as behavior research suggests differing developmental patterns for these sets of behaviors. It is generally understood that disruptive behaviors appear a few years before IA symptoms in development (Loeber, Green, Lahey, Christ, & Frick, 1992) and HI behaviors tend to decline earlier than the decline of IA symptoms in adolescence (Biederman, Mick, & Faraone, 2000; Hart, Lahey, Loeber, Applegate, & Frick, 1995).
The goal of this study is to describe DSM-IV ADHD symptom persistence from early childhood through late adolescence using a diverse community-based epidemiological sample of boys and girls with and without ADHD. Graphics of individual IA and HI symptoms and IA and HI symptom counts will be complemented with advanced modeling to determine statistical significance of symptom decline after accounting for ADHD medication use, psychiatric comorbidity, and other demographic factors.
Method
Sample
This study utilizes data from the Project to Learn about ADHD in Youth (PLAY), a cohort study that included sites in South Carolina (SC) and Oklahoma (OK; Wolraich et al., 2012). Only SC data were included in this analysis because high retention of the cohort over time allowed for an appropriate longitudinal analytic approach. A previous publication which focused on the baseline sample from both sites reported an ADHD prevalence estimate of 8.7% in SC (Wolraich et al., 2012).
In the first stage of a two-stage sampling design, parents and teachers reported history of an ADHD diagnosis and ADHD medication use, and teachers completed the Vanderbilt ADHD Diagnostic Teacher Rating Scale (VADTRS; Wolraich, Feurer, Hannah, Baumgaertel, & Pinnock, 1998). Children with a previous diagnosis, current medication use, or teacher report of ≥6 symptoms and some impairment were categorized as high risk of ADHD. All high screened individuals and their parents were eligible for a second-stage interview, as well as a sample of low-risk peers, frequency-matched on sex. Further details on sampling design have been described previously (Wolraich et al., 2012). All study procedures were approved by the Institutional Review Boards of the Centers for Disease Control and Prevention and University of South Carolina.
At baseline (2003–2005, hereafter referred to as Time 1), 481 children and their parents completed an interview. Beginning 3 years later, all traceable participants were invited for annual interviews; 292, 280, 249, and 294 participants were interviewed at the four follow-up waves, respectively (Times 2–5). In total, 379 participants (79%) were interviewed at least once between 3 and 8 years after Time 1. Most interviews were scheduled 2 to 4 weeks in advance and confirmed a few days beforehand. All interviews were completed in person unless participants had transportation limitations or moved out of the area, in which case interviews were completed via telephone. Participants were compensated for their time upon completion of each interview; the amount varied as procedures were modified to collect age-appropriate data. Written informed consent was obtained before interviews at every wave.
Measures
The Diagnostic Interview Schedule for Children Version IV (DISC-IV) is a standardized interview designed to assess psychiatric disorders in children (Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000). As part of each interview, parents completed 10 DISC-IV modules, each of which asked questions regarding a separate common psychiatric disorder. Questions about inattention, hyperactivity, and impulsivity were asked in the ADHD module, including items on symptoms, time frame, and associated functional impairment. ADHD case criteria required two intermediate or one severe impairment rating. Questions were asked similarly for social phobia, separation anxiety disorder, generalized anxiety disorder, post-traumatic stress disorder (PTSD), obsessive-compulsive disorder (OCD), major depression, mania (and hypomania), oppositional defiant disorder, and conduct disorder. Moderate to strong test–retest agreement (kappa [κ] from 0.5 to 0.8) has been observed for most DISC-IV modules (ADHD module: κ = 0.79; Shaffer et al., 2000). Participants were considered to have a psychiatric condition (other than ADHD) if they met DISC-IV criteria for a condition and had at least intermediate impairment due to the symptoms. The DISC-IV allows for user selection of various impairment thresholds to satisfy DSM’s functional impairment criteria.
In our previously published ADHD prevalence study (Wolraich et al., 2012), we also incorporated teacher-reported data; however, we did not have teacher-reported data from follow-up waves. As a result, prevalence estimates for ADHD are higher in this study than in the previous study (Wolraich et al., 2012).
Information on children’s usage of medication for ADHD was collected as part of each DISC-IV interview, as were data on whether the child lived with two parents. All other demographic data were collected via questionnaire at each data collection wave.
Analytical Approach
IA and HI symptom counts were found to be positively skewed, with increasing skewness from early childhood to late adolescence (IA skewness: 0.50–0.65; HI: 0.71–1.81). The distribution of symptom counts informed the approach of subsequent analyses. All analyses were performed using R Version 2.14.0 (R Core Team, 2012).
To allow for visual interpretation, symptom counts are displayed by categories of developmental stage (early childhood [5–8 years], middle childhood [9–11 years], early adolescence [12–14 years], and late adolescence [15–19 years]). These categories were selected for their applicability to the data while approximating developmental stages in the developmental psychology literature. In this article, developmental stages are only utilized for visualization of basic results; all modeling and resulting test statistics treated participant age (to the 100th of a year) as a continuous variable. Using age in models rather than another time measure yielded estimates whose interpretation directly apply to age itself while precisely accounting for time between each participant’s interviews as well as age difference across participants.
Logistic quantile regression is a procedure that models specified percentiles, rather than the mean, of a dependent variable (Bottai, Cai, & McKeown, 2010). In doing so, no assumptions are made about the scale or the distribution of the variable of interest. This approach has been shown to perform favorably for bounded outcomes with skewed distributions (e.g., symptom counts; Bottai et al., 2010). In this study, logistic quantile regression was used to determine whether age (continuous) was associated with particular percentiles of IA and HI symptom counts.
Other factors considered in models as being associated with symptom count were race, sex, ADHD medication use, presence of psychiatric disorder other than ADHD, and whether two parents lived in the household. Models allowed ADHD medication use, psychiatric comorbidity, and whether two parents lived in the home to vary over time. Potential covariates were removed from all models through a backward stepwise procedure if their elimination did not result in a 10% change in any model’s age-associated estimate. The standard errors of the regression coefficients were estimated with 200 bootstrapped samples, as bootstrapping was shown to outperform other estimators for quantile regression models, especially with heteroskedastic data (i.e., variables that have different variances, such as symptom count by age; Buchinsky, 1995).
In addition, logistic regression modeling was performed to determine whether high (≥6) HI symptom counts were more likely to persist among participants who had high IA symptom counts at Time 1, and whether high IA symptom counts were more likely to persist among those who had high HI symptom counts at Time 1. All analyses accounted for the multistage, stratified study design and the intra-individual correlation between data collection waves. Probability weights used in the analyses reflected differential sampling from the underlying school district population and non-response. When applied to the interview data, they produced demographic estimates that were close to the observed proportions of demographic characteristics in the school district population.
Results
Demographic information of the study sample is displayed in Table 1 by data collection wave using unweighted percentages to allow for inspection of differential attrition. The subsequent table and figures present weighted statistics. Mean participant age at Times 1 to 5 were 9.2, 12.5, 13.6, 14.6, and 15.6 years, respectively. Non-Hispanic Whites and non-Hispanic Blacks were well represented, as were both sexes (67% boys, reflecting a higher prevalence of ADHD symptoms in boys compared with girls in the screened sample). Meeting criteria for other externalizing and internalizing psychiatric conditions were most common at Time 1. At Times 1 to 5, the weighted prevalence estimates and 95% confidence intervals (CI) of DISC-IV-defined ADHD were 12.2% (10.2, 14.5), 11.2% (8.9, 13.8), 12.2% (8.5, 17.1), 6.5% (5.0, 8.4), and 8.4% (6.0, 11.5), respectively. Most demographic groups were retained for follow-up in similar proportions, including non-Hispanic Blacks. Other racial/ethnic minority participants were less likely to be retained, although this difference was not statistically significant.
Table 1.
Frequencies and Unweighted Percentages of Sample Demographics by Data Collection Point.
| Time 1
|
Time 2
|
Time 3
|
Time 4
|
Time 5
|
|
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | |
| Time varying | |||||
| Developmental stage | |||||
| Early childhood (5–8) | 216 (45) | 4 (1) | 1 (0) | 0 (0) | 0 (0) |
| Middle childhood (9–11) | 235 (49) | 110 (38) | 52 (19) | 18 (7) | 3 (1) |
| Early adolescence (12–14) | 30 (6) | 159 (54) | 159 (57) | 128 (51) | 113 (38) |
| Late adolescence (15–19) | 0 (0) | 19 (7) | 68 (24) | 103 (41) | 178 (61) |
| Other psychiatric diagnoses | |||||
| Externalizing disordersa | 89 (19) | 40 (14) | 41 (15) | 29 (12) | 43 (15) |
| Internalizing disordersb | 47 (10) | 26 (9) | 18 (6) | 16 (6) | 17 (6) |
| ADHD medication use | 141 (29) | 92 (32) | 77 (28) | 65 (26) | 73 (25) |
| Live with both parents | 326 (68) | 180 (62) | 171 (61) | 150 (60) | 168 (57) |
| Time invariant | |||||
| Sex | |||||
| Male | 323 (67) | 191 (65) | 188 (67) | 167 (67) | 196 (67) |
| Female | 158 (33) | 101 (35) | 92 (33) | 82 (33) | 98 (33) |
| Race/ethnicity | |||||
| White, non-Hispanic | 269 (56) | 169 (58) | 169 (60) | 154 (62) | 161 (55) |
| Black, non-Hispanic | 184 (38) | 114 (39) | 105 (38) | 90 (36) | 125 (43) |
| Other | 28 (6) | 9 (3) | 6 (2) | 5 (2) | 8 (3) |
| Primary caregiver’s educational attainment | |||||
| No degree beyond high school | 204 (44) | 119 (42) | 115 (41) | 99 (40) | 123 (43) |
| Associate/vocational degree | 69 (15) | 38 (13) | 36 (13) | 32 (13) | 40 (14) |
| ≥ Bachelor’s degree | 192 (41) | 129 (45) | 127 (46) | 115 (47) | 125 (43) |
Conduct disorder and oppositional defiant disorder.
Social phobia, separation anxiety disorder, generalized anxiety disorder, post-traumatic stress disorder, obsessive-compulsive disorder, major depression, and mania.
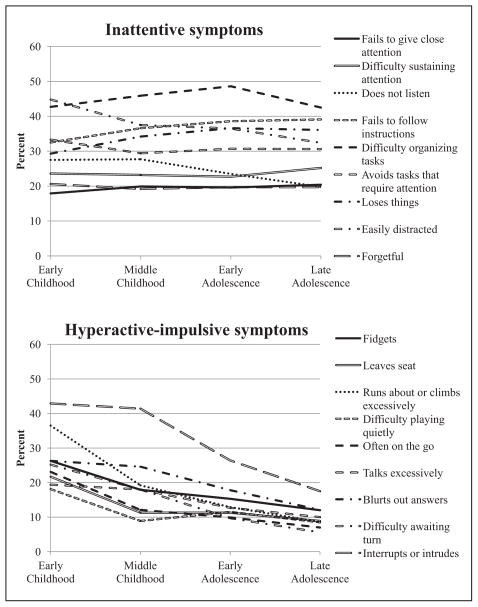
Figure 1 shows the prevalence of each ADHD symptom by developmental stage (early childhood [5–8 years], middle childhood [9–11 years], early adolescence [12–14 years], and late adolescence [15–19 years]). Prevalence of individual IA symptoms ranged from 18% to 45% among early childhood and 20% to 43% among those in late adolescence. Across developmental stages, most symptoms were reported at similar levels. There was a decreasing trend in prevalence of HI symptoms with increasing child age. The prevalence of individual HI symptoms ranged from 18% to 43% among those in early childhood and 6% to 18% among late adolescents. Eight of the nine HI symptoms among participants in late adolescence were at levels less than half the proportions reported in early childhood.
Figure 1.
Prevalence of parent-reported ADHD symptoms by developmental stage.
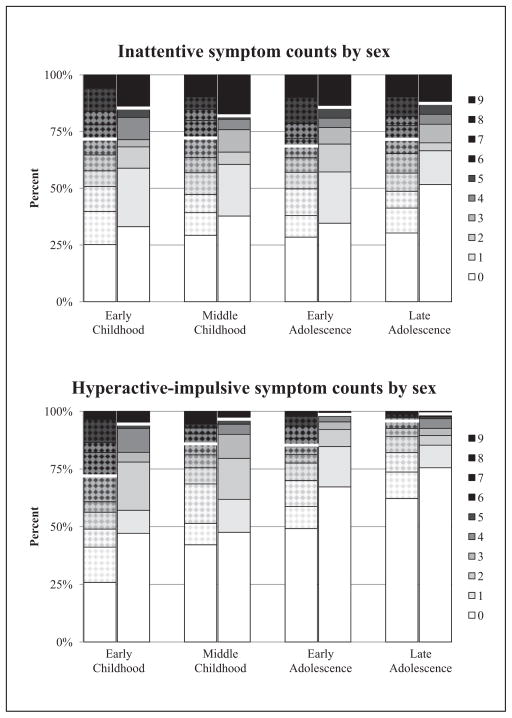
Figure 2 displays the distribution of each symptom count by symptom type, developmental stage, and sex. Cut points are included in the figure to separate those who had six or more symptoms and, therefore, were most likely to meet ADHD diagnostic criteria. Neither sex had a considerable change in IA symptom count distribution over developmental stages. High HI symptom counts appeared to be lower among the older participants, and the rate of this decline was fairly similar across developmental stages (overall, 17%, 10%, 7%, and 3%, respectively). Boys had higher IA and HI symptom counts than girls, although symptom persistence patterns were similar between sexes.
Figure 2.
Distribution of symptom counts by sex (male: textured) and developmental stage.
Note. The white line within each bar separates those who had ≥6 symptoms
Some participants were counted in this figure multiple times within each developmental stage. Therefore, Figure 2 allows for a simple visual inspection of the symptom counts that were later modeled, but does not sufficiently account for the longitudinal characteristic of the data. All models accounted for the correlation between each participant’s symptom counts across data collection points. Median IA and HI symptom counts at Time 1 were similar between those who did and did not participate in follow-up, providing evidence that the apparent patterns over time were not due to cohort attrition.
The top portion of Table 2 shows results of the logistic quantile regression models in which percentiles of IA symptom count were modeled as a function of age (continuous) and adjusted for associated demographic factors. Odds ratios (OR) can be interpreted similarly to those from logistic regression for the probability of binary outcomes, with the probability replaced by the quantile-to-interval-length ratio. For example, the odds of having an IA symptom count in the 80th percentile was 0.25 smaller for females than for males. IA symptom count did not differ independently by age at any fifth percentile (upper quartile shown). Those using ADHD medication, and those with psychiatric disorder other than ADHD, and, to some extent, those living in a single parent household were more likely to have a higher IA symptom count.
Table 2.
Odds Ratios (OR) From Logistic Quantile Regression for Parent-Reported Inattention and Hyperactive-Impulsive Symptom Count Percentiles.
| Inattentive symptom count percentiles
|
Hyperactive-impulsive symptom count percentiles
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 75th
|
80th
|
85th
|
90th
|
95th
|
75th
|
80th
|
85th
|
90th
|
95th
|
|
| OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | |
| Age | 1.00 [0.97, 1.03] | 1.00 [0.97, 1.03] | 1.00 [0.97, 1.03] | 1.00 [0.98, 1.02] | 1.00 [0.99, 1.01] | 0.87 [0.80, 0.95] | 0.89 [0.83, 0.95] | 0.91 [0.85, 0.98] | 0.94 [0.89, 0.99] | 0.93 [0.90, 0.97] |
| Female | 0.61 [0.43, 0.88] | 0.75 [0.52, 1.08] | 0.80 [0.59, 1.08] | 0.94 [0.85, 1.17] | 0.88 [0.76, 1.01] | 0.57 [0.38, 0.86] | 0.55 [0.38, 0.80] | 0.59 [0.43, 0.81] | 0.60 [0.47, 0.78] | 0.63 [0.52, 0.77] |
| On ADHD medication | 2.04 [1.61, 2.58] | 1.88 [1.47, 2.40] | 1.58 [1.25, 2.00] | 1.34 [1.11, 1.60] | 1.25 [1.09, 1.43] | 2.10 [1.42, 3.11] | 1.89 [1.36, 2.62] | 1.81 [1.32, 2.48] | 1.68 [1.33, 2.12] | 1.64 [1.30, 2.07] |
| Psychiatric disordera | 1.63 [1.24, 2.15] | 1.50 [1.14, 1.97] | 1.58 [1.26, 1.99] | 1.36 [1.13, 1.64] | 1.26 [1.11, 1.42] | 2.36 [1.59, 3.51] | 2.24 [1.56, 3.23] | 2.23 [1.55, 3.19] | 1.90 [1.34, 2.70] | 1.98 [1.48, 2.66] |
| Single parent household | 1.42 [1.06, 1.92] | 1.33 [1.02, 1.75] | 1.26 [1.00, 1.59] | 1.25 [1.00, 1.56] | 1.00 [0.83, 1.20] | 1.42 [0.95, 2.13] | 1.41 [1.00, 1.96] | 1.28 [0.95, 1.72] | 1.23 [0.96, 1.59] | 1.35 [1.10, 1.67] |
Note. CI = confidence interval.
Other than ADHD.
This modeling approach was also performed using HI symptom count (bottom of Table 2). The upper quartile of HI symptom count significantly decreased by age after adjustment for associated demographics, although we were unable to detect a significant decrease in any value of HI symptom count below the 75th percentile (data not shown). Demographic factors were similarly associated with high levels of IA and HI symptoms. There was no evidence of a significant interaction between age and sex at any modeled percentile, meaning symptom persistence patterns did not differ between boys and girls in this sample.
The co-existence of IA and HI symptoms were also examined. At Time 1, 41% of children with high (≥6) IA symptom counts also had high HI symptom counts, and 73% of children with high HI symptom counts also had high IA symptom counts. An unadjusted logistic regression model suggested that among those with high HI symptom counts at Time 1, high HI symptom counts were more likely to persist in participants who had high IA symptom counts (OR = 3.3; 95% CI [1.0, 10.7]; p = .05). Although high IA symptom counts more often persisted among participants who had high HI symptom counts, this association was not statistically significant.
Discussion
The data for this study were collected as part of a large community-based project examining the prevalence and correlates of ADHD in school-aged children. The prevalence of parent-reported IA and HI symptoms was similar in early childhood. After adjustment for sex, ADHD medication use, and presence of another psychiatric disorder, IA symptom count did not differ with age, but the highest quartile of HI symptom counts did decrease with age. High HI symptom counts may be more likely to persist among those who also have high IA symptom counts. Symptom counts were positively associated with ADHD medication use and psychiatric comorbidity, although this is likely due to higher likelihood of youth with high ADHD symptom counts and/or a psychiatric disorder other than ADHD being placed on medication.
Building on prior research, this study extends the findings from Todd et al. (2008) who likewise studied a community-based sample, although using data from two time points 5 years apart. Similar to Todd et al., the present study reported inattentive symptoms tended to persist more than HI symptoms, although the present study utilized more frequently collected data over a broader age range to examine detailed patterns from early childhood through late adolescence. Also consistent with prior research, this study shows a higher level of ADHD symptomatology in boys than in girls. However, this study is able to add that the developmental course of the symptoms appears to be similar among boys and girls. Therefore, girls with high levels of symptoms were as likely as boys to show symptom persistence across development in this community-based sample. It is possible that the apparent difference in the developmental trajectory between IA and HI symptom counts partially reflects differences in environmental context. That is, aspects of HI are more apparent at young ages, while the recognition of IA often does not surface until tasks at school or work tax attentional capacity (Faraone et al., 2006; Kessler et al., 2006). In addition, it is possible that a portion of the HI symptom decline is because of the symptom descriptors used in DSM-IV that generally did not apply to adolescent behaviors. This has been addressed in DSM-5 (APA, 2013), as additional examples have been included in DSM-5 to illustrate types of behaviors adolescents and adults with ADHD may exhibit. Findings from this study lend support for recognition of ADHD as a disorder affecting people beyond childhood.
There are at least three important limitations of this study. First, defining remission, relapse, persistence, and desistance is central to both conducting persistence studies and interpreting their findings, particularly in psychiatric research (Eaton, 2002). Because researchers continue to define these measures differently, it is difficult to compare our results with the work of others. Another important limitation is our insufficient power to detect potential differences in symptom persistence patterns by demographic subgroups, such as race/ethnicity. Third, this study relies entirely on parent-reported symptoms because we did not have adequate data from other informants, most notably teachers.
This study also has notable strengths. To build on previous studies (Biederman et al., 2010; Faraone et al., 2006; Hart et al., 1995; Mannuzza, Klein, & Moulton, 2003), this study investigated symptom patterns of inattentive, hyperactive, and impulsive DSM-IV symptoms among both boys and girls from a diverse community-based sample. A second major strength of this study is the novel use of logistic quantile regression, which more appropriately handles dependent variables that are bounded with skewed distributions (i.e., symptom counts), allows for valid interpretation of estimates at extreme ends of the distribution (e.g., the 95th percentile), and makes no assumptions related to scale of the variable itself. This community-based study was also strengthened by the application of sample and non-response weights, which allow estimates to be considered generalizable to the base population, in this case, the school district from which the sample was drawn.
This study’s findings have important clinical implications. Results from this study provide greater context for clinicians who treat children outside of the elementary school age, including adolescents who had not been previously diagnosed (Faraone, Spencer, Montano, & Biederman, 2004). Specifically, this study suggests that HI symptoms often remit but that IA symptoms generally persist into adolescence. Given the negative outcomes associated with adolescent ADHD (Barbaresi et al., 2007; Flory et al., 2006; Jerome et al., 2006; Küpper et al., 2012; Loe & Feldman, 2007; Molina et al., 2013), close clinical attention should be paid to the assessment of inattentive symptoms, in particular, during the evaluation and treatment of adolescent patients, which can be more difficult to identify. Notably, fewer symptoms are now required to meet a diagnosis of ADHD among older adolescents and young adults (17 years of age and older) with ADHD (APA, 2013); therefore, careful assessment of IA symptoms among adolescents may have a measureable impact on the prevalence of ADHD among adolescents. In addition, previous brain imaging research has identified groups of children who appear to have remitting ADHD (Shaw et al., 2006); this study reveals symptom persistence patterns that may further characterize the phenotypes of remitting and persistent childhood ADHD. Finally, this information may be helpful for clinicians who seek to provide anticipatory guidance to parents of children who are newly diagnosed with ADHD and have questions about the persistence of ADHD and its symptoms over time.
Characterizing the course of ADHD symptoms in the community is an important Public Health activity, which leads to greater understanding of this common chronic disorder. Understanding symptom persistence may also inform the development of early prevention and targeted treatment strategies, inform educators on what to expect within the classroom, and inform efforts to educate parents on what to expect from their child’s ADHD symptoms over time. The findings of this study provide support for the importance of ongoing monitoring of ADHD and its symptoms through adolescence. Although ADHD is no longer recognized solely as a childhood disorder, there is very little research on ADHD persistence among older adolescents and young adults, and it is important that future efforts address this gap, particularly as the epidemiology of childhood ADHD continues to evolve (Visser et al., 2014) and the prevalence estimates of adult ADHD increase (Kessler et al., 2006).
Acknowledgments
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Biographies
Joseph R. Holbrook, PhD, is an associate service fellow in the Child Development Studies Team within the Centers for Disease Control and Prevention (CDC). Prior to this position, he was a student, graduate assistant, and data manager for the University of South Carolina Project to Learn about ADHD in Youth (PLAY).
Steven P. Cuffe, MD, is a professor and chair of the Department of Psychiatry at the University of Florida College of Medicine–Jacksonville. He has spent 20 years researching the epidemiology, risk, and protective factors of child and adolescent psychiatric disorders. He was the co-principal investigator of the University of South Carolina PLAY.
Bo Cai, PhD, is an associate professor in the Department of Epidemiology and Biostatistics at the University of South Carolina. His research interests include development of statistical methods in public health, child health, environmental health, and biomedical sciences. He was a statistician for the University of South Carolina PLAY.
Susanna N. Visser, DrPH, is the acting associate director for science within the CDC Division of Human Development and Disability. Her expertise includes the analysis and design of longitudinal and population-based epidemiological studies of neurobehavioral and mental health conditions, including ADHD and Tourette Syndrome. She was the CDC principal investigator for PLAY.
Melinda S. Forthofer, PhD, is an associate professor of epidemiology and biostatistics in the Arnold School of Public Health at the University of South Carolina. She has more than 20 years of experience studying social factors related to health behavior change in children, adolescents, and adults in diverse community settings. Much of her current research is focused on the role of social factors in the promotion of health behaviors, particularly the role of social networks in physical activity.
Matteo Bottai, ScD, is the head of the Unit of Biostatistics, Institute of Environmental Health, Karolinska Institutet, Stockholm, Sweden. He received his Laurea degree in mathematics summa cum laude from University of Pisa, Pisa, Italy, and his doctoral degree in biostatistics from the Harvard School of Public Health, Boston, MA. His current research focuses on statistical methods for modeling and estimation of conditional percentiles. He has served as a statistician for the University of South Carolina PLAY.
Andrew Ortaglia, PhD, is a clinical assistant professor in the Department of Epidemiology and Biostatistics at the University of South Carolina. His primary research interests include semi-parametric models, survival analysis, and health aspects of physical activity.
Robert E. McKeown, PhD, is a Distinguished Professor Emeritus and past chair of the Department of Epidemiology and Biostatistics at the University of South Carolina. He is past president of the American College of Epidemiology and past chair of the epidemiology section of the American Public Health Association. His research focuses on psychiatric epidemiology and public health ethics. He was the University of South Carolina principal investigator for PLAY.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Disclaimer: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- Akinbami LJ, Liu X, Pastor PN, Reuben CA. Attention deficit hyperactivity disorder among children aged 5–17 years in the United States, 1998–2009. NCHS Data Brief. 2011;70:1–8. [PubMed] [Google Scholar]
- American Academy of Pediatrics’ Subcommittee on Attention-Deficit/Hyperactivity Disorder Steering Committee on Quality Improvement and Management. ADHD: Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128:1–16. doi: 10.1542/peds.2011-2654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. text rev. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Washington, DC: Author; 2013. [Google Scholar]
- Barbaresi WJ, Colligan RC, Weaver AL, Voigt RG, Killian JM, Katusic SK. Mortality, ADHD, and psychosocial adversity in adults with childhood ADHD: A prospective study. Pediatrics. 2013;131:637–644. doi: 10.1542/peds.2012-2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbaresi WJ, Katusic SK, Colligan RC, Weaver AL, Jacobsen SJ. Long-term school outcomes for children with attention-deficit/hyperactivity disorder: A population-based perspective. Journal of Developmental & Behavioral Pediatrics. 2007;28:265–273. doi: 10.1097/DBP.0b013e31811ff87d. [DOI] [PubMed] [Google Scholar]
- Bauermeister JJ, Bird HR, Shrout PE, Chavez L, Ramirez R, Canino G. Short-term persistence of DSM-IV ADHD diagnoses: Influence of context, age, and gender. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50:554–562. doi: 10.1016/j.jaac.2011.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biederman J, Faraone S, Milberger S, Curtis S, Chen L, Marrs A, Spencer T. Predictors of persistence and remission of ADHD into adolescence: Results from a four-year prospective follow-up study. Journal of the American Academy of Child Adolescent Psychiatry. 1996;35:343–351. doi: 10.1097/00004583-199603000-00016. [DOI] [PubMed] [Google Scholar]
- Biederman J, Mick M, Faraone SV. Age-dependent decline of symptoms of attention deficit hyperactivity disorder: Impact of remission definition and symptom type. American Journal of Psychiatry. 2000;157:816–818. doi: 10.1176/appi.ajp.157.5.816. [DOI] [PubMed] [Google Scholar]
- Biederman J, Petty CR, Clarke A, Lomedico A, Faraone SV. Predictors of persistent ADHD: An 11-year follow-up study. Journal of Psychiatric Research. 2010;45:150–155. doi: 10.1016/j.jpsychires.2010.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird HR, Canino GJ, Davies M, Duarte CS, Febo V, Ramirez R, Loeber R. A study of disruptive behavior disorders in Puerto Rican youth: I. Background, design, and survey methods. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45:1032–1041. doi: 10.1097/01.chi.0000227878.58027.3d. [DOI] [PubMed] [Google Scholar]
- Bottai M, Cai B, McKeown RE. Logistic quantile regression for bounded outcomes. Statistics in Medicine. 2010;29:309–317. doi: 10.1002/sim.3781. [DOI] [PubMed] [Google Scholar]
- Buchinsky M. Estimating the asymptotic covariance matrix for quantile regression models a Monte Carlo Study. Journal of Econometrics. 1995;68:303–338. [Google Scholar]
- Buitelaar JK, Kan CC, Asherson P. ADHD in adults: Characterization, diagnosis, and treatment. New York, NY: Cambridge University Press; 2011. [Google Scholar]
- Centers for Disease Control and Prevention. Increasing prevalence of parent-reported attention-deficit/hyperactivity disorder among children—United States, 2003 and 2007. Morbidity and Mortality Weekly Report. 2010;59:1439–1443. [PubMed] [Google Scholar]
- Eaton WW. Studying the natural history of psychopathology. In: Tsuang M, Tohen M, editors. Textbook in psychiatric epidemiology. Hoboken, NJ: John Wiley; 2002. [Google Scholar]
- Eaton WW, Martins SS, Nestadt G, Bienvenu OJ, Clarke D, Alexandre P. The burden of mental disorders. Epidemiologic Reviews. 2008;30:1–14. doi: 10.1093/epirev/mxn011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: A meta-analysis of follow-up studies. Psychological Medicine. 2006;36:159–165. doi: 10.1017/S003329170500471X. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Spencer TJ, Montano CB, Biederman J. Attention deficit hyperactivity disorder in adults: A survey of current practice in psychiatry and primary care. Archives of Internal Medicine. 2004;164:1221–1226. doi: 10.1001/archinte.164.11.1221. [DOI] [PubMed] [Google Scholar]
- Flory K, Molina BS, Pelham WE, Jr, Gnagy E, Smith B. Childhood ADHD predicts risky sexual behavior in young adulthood. Journal of Clinical Child & Adolescent Psychology. 2006;35:571–577. doi: 10.1207/s15374424jccp3504_8. [DOI] [PubMed] [Google Scholar]
- Getahun D, Jacobsen SJ, Fassett MJ, Chen W, Demissie K, Rhoads GG. Recent trends in childhood attention-deficit/hyperactivity disorder. JAMA Pediatrics. 2013;167:282–288. doi: 10.1001/2013.jamapediatrics.401. [DOI] [PubMed] [Google Scholar]
- Goldberg D. Epidemiology of mental disorders in primary care settings. Epidemiologic Reviews. 1995;17:182–190. doi: 10.1093/oxfordjournals.epirev.a036174. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Hoven CW, Narrow WE, Cohen P, Fielding B, Alegria M, Dulcan MK. Measurement of risk for mental disorders and competence in a psychiatric epidemiologic community survey: The National Institute of Mental Health Methods for the Epidemiology of Child and Adolescent Mental Disorders (MECA) Study. Social Psychiatry & Psychiatric Epidemiology. 1998;33:162–173. doi: 10.1007/s001270050039. [DOI] [PubMed] [Google Scholar]
- Hart EL, Lahey BB, Loeber R, Applegate B, Frick PJ. Developmental change in attention-deficit hyperactivity disorder in boys: A four-year longitudinal study. Journal of Abnormal Child Psychology. 1995;23:729–749. doi: 10.1007/BF01447474. [DOI] [PubMed] [Google Scholar]
- Jerome L, Segal A, Habinski L. What we know about ADHD and driving risk: A literature review, meta-analysis and critique. Journal of Canadian Academy of Child Adolescent Psychiatry. 2006;15:105–125. [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, Zaslavsky AM. The prevalence and correlates of adult ADHD in the United States: Results from the National Comorbidity Survey Replication. American Journal of Psychiatry. 2006;163:716–723. doi: 10.1176/appi.ajp.163.4.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Küpper T, Haavik J, Drexler H, Ramos-Quiroga JA, Wermelskirchen D, Prutz C, Schauble B. The negative impact of attention-deficit/hyperactivity disorder on occupational health in adults and adolescents. International Archives of Occupational and Environmental Health. 2012;85:837–847. doi: 10.1007/s00420-012-0794-0. [DOI] [PubMed] [Google Scholar]
- Loe I, Feldman H. Academic and educational outcomes of children with ADHD. Journal of Pediatric Psychology. 2007;32:643–654. doi: 10.1093/jpepsy/jsl054. [DOI] [PubMed] [Google Scholar]
- Loeber R, Green SM, Lahey BB, Christ MAG, Frick PJ. Developmental sequences in the age of onset of disruptive child behaviors. Journal of Child and Family Studies. 1992;1:21–41. [Google Scholar]
- Mannuzza S, Gittelman R. The adolescent outcome of hyperactive girls. Psychiatry Research. 1984;13(1):19–29. doi: 10.1016/0165-1781(84)90115-x. [DOI] [PubMed] [Google Scholar]
- Mannuzza S, Klein RG, Moulton JL. Persistence of attention-deficit/hyperactivity disorder into adulthood: What have we learned from the prospective follow-up studies? Journal of Attention Disorders. 2003;7:93–100. doi: 10.1177/108705470300700203. [DOI] [PubMed] [Google Scholar]
- Molina BS, Hinshaw SP, Eugene Arnold L, Swanson JM, Pelham WE, Hechtman L. Adolescent substance use in the multimodal treatment study of attention-deficit/hyperactivity disorder (ADHD) (MTA) as a function of childhood ADHD, random assignment to childhood treatments, and subsequent medication. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52:250–263. doi: 10.1016/j.jaac.2012.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen P, Gillberg C. Natural outcome of ADHD with developmental coordination disorder at age 22 years: A controlled, longitudinal, community-based study. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:1424–1431. doi: 10.1097/00004583-200011000-00017. [DOI] [PubMed] [Google Scholar]
- R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2012. [Google Scholar]
- Scahill L, Schwab-Stone ME. Epidemiology of ADHD in school-age children. Child and Adolescent Psychiatric Clinics of North America. 2000;9:541–555. [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Shaw P, Lerch J, Greenstein D, Sharp W, Clasen L, Evans A, Rapoport J. Longitudinal mapping of cortical thickness and clinical outcome in children and adolescents with attention-deficit/hyperactivity disorder. Archives of General Psychiatry. 2006;63:540–549. doi: 10.1001/archpsyc.63.5.540. [DOI] [PubMed] [Google Scholar]
- Todd RD, Huang H, Todorov AA, Neuman RJ, Reiersen AM, Henderson CA, Reich WC. Predictors of stability of attention-deficit/hyperactivity disorder subtypes from childhood to young adulthood. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47:76–85. doi: 10.1097/chi.0b013e31815a6aca. [DOI] [PubMed] [Google Scholar]
- Visser SN, Danielson ML, Bitsko RH, Holbrook JR, Kogan MD, Ghandour RM, Blumberg SJ. Trends in the parent-report of health care provider-diagnosed and medicated attention-deficit/hyperactivity disorder: United States, 2003–2011. Journal of the American Academy of Child & Adolescent Psychiatry. 2014;53:34–46. e2. doi: 10.1016/j.jaac.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willoughby MT. Developmental course of ADHD symptomatology during the transition from childhood to adolescence: A review with recommendations. Journal of Child Psychology and Psychiatry. 2003;44:88–106. doi: 10.1111/1469-7610.t01-1-00104. [DOI] [PubMed] [Google Scholar]
- Wolraich ML, Feurer ID, Hannah JN, Baumgaertel A, Pinnock TY. Obtaining systematic teacher reports of disruptive behavior disorders utilizing DSM-IV. Journal of Abnormal Child Psychology. 1998;26:141–152. doi: 10.1023/a:1022673906401. [DOI] [PubMed] [Google Scholar]
- Wolraich ML, McKeown RE, Visser SN, Bard D, Cuffe SP, Neas B, Danielson M. The prevalence of attention-deficit/hyperactivity disorder: Its diagnosis and treatment in four school districts. Journal of Attention Disorders. 2012 doi: 10.1177/1087054712453169. Advance online publication. [DOI] [PubMed] [Google Scholar]