Abstract
Objectives
Colorectal cancer (CRC) screening continues to be underused, particularly by Latinos. CRC and colonoscopy fear, worry and fatalism have been identified as screening barriers in Latinos. The study purpose was to examine the relationship of optimism, fatalism, worry, and fear in the context of Latinos referred for CRC screening.
Methods
Our sample included 251 Latinos between the ages of 50 and 83 who had no personal or immediate family history of CRC, no personal history of gastrointestinal disorder, no colonoscopy in the past five years, and received a referral for a colonoscopy. Face-to-face interviews were performed and data were analyzed using regression models.
Results
Greater optimism (β=−1.72, p<0.000), lower fatalism (β=0.29, p<0.01), and absence of family history of cancer (β=1, p<0.01) were associated with decreased worry about the colonoscopy. Being female (β=0.85, p<0.05) and born in the United States (β=1.1, p<0.01) were associated with greater worry about colonoscopy and the possibility of having CRC. Family history of cancer (β=2.6, p<0.01), female gender (β=2.9, p<0.000), not following the doctor’s advice (β=2.7, p<0.01), and putting off medical problems (β=1.9, p<0.05) were associated with greater fear. In the multiple regression model, lower optimism (β=−0.09, p<0.05), higher fatalism (β=0.28, p<0.01), and female gender (β=0.9, p <0.05) were associated with greater worry.
Conclusions
Interventions that address fatalism and promote optimistic beliefs may reduce worry among Latinos referred for colonoscopy. Interventions that alleviate colonoscopy fear due to family history of cancer particularly among Latino women may help improve distress about CRC screening.
Keywords: Cancer, Oncology, Optimism, Fear, Colonoscopy
Introduction
The American Cancer Society (ACS) estimates approximately 136,830 new cases of colorectal cancer (CRC) in 2014 making it the third most common cancer among men and women in the United States. When detected at an early, localized stage, CRC can be prevented and treated effectively as demonstrated by the reported five-year 90% survival rate.[1, 2] However, only 40% of cases of CRC in the United States are detected early. CRC screening continues to be underutilized by Latinos, the minority group that accounts for more than half of the U.S. population growth in the last decade. [2, 3]
Because of its high diagnostic effectiveness, colonoscopy is the gold standard CRC screening test.[4] However, Latinos have one of the lowest screening endoscopy rates (measured as sigmoidoscopy or colonoscopy within the past 5 or 10 years respectively). In 2010, only 45.3% of Latinos over age 50 underwent endoscopic CRC screening vs. 58% Non-Latino whites and 53% African-Americans.[2] This differential is largely explained by lesser access to healthcare [5, 6] and psycho-social barriers [7–12] in which fear of colonoscopy [6, 10, 13, 14] and of cancer diagnosis [6, 14], worry about colonoscopy [10, 15], and fatalism [16, 17] about cancer play a prominent role. Colonoscopy fear and worry have been shown to significantly contribute to cancer anxiety which is a traditional measure of psychological distress [18, 19]. In our study, the fear measure focuses on different aspects of the colonoscopy procedure such as discomfort before and during colonoscopy, while worry assesses feelings of concern about the colonoscopy procedure and potential abnormal results, for example polyp or CRC. [10, 20]. Several studies have identified contributors to cancer worry, among which are family history, perceived presence of symptoms, perceived risk of cancer, and individual personality characteristics.[21–24] In this study we aim to analyze how personality characteristics such as optimism and fatalism are related to colonoscopy worry and fear among Latinos at average risk for CRC. Average risk is characterized by absence of immediate family history of CRC and lack of personal history of other gastrointestinal disorders. This study includes only individuals with access to primary care therefore reducing the need to account for access to care in the analysis.
Optimism is defined as a general expectation of positive events and outcomes in life and is often thought of as a dispositional trait.[25]. It has been shown, however, that level of optimism can change in response to psychosocial interventions.[26, 27] Among patients who are expecting to undergo colonoscopy greater optimism is related to reduced anxiety and distress.[19] This significant negative relationship between optimism and cancer worry has been shown in breast, colorectal, and prostate cancer long-term survivors.[18] In addition, Han and colleagues [28] demonstrated that when people are communicated information about different levels of CRC risk, more optimistic individuals have lower CRC worry.
Similarly, several works showed that optimism may be associated with less fear.[29, 30] However, to our knowledge, no study has looked at the relationship between fear and optimism in the context of CRC.
In addition to optimism, we hypothesize that health-related fatalism, has a positive relationship with worry and fear. Fatalism is the belief that one lacks control of one’s health events and outcomes and has been proposed to be the inverse of optimism [31]. Fatalism has been shown to be negatively related to cancer screening behavior.[17, 32, 33] In addition, Ferrer reported a positive relationship between fatalism and perceived risk.[21] The latter has been proposed as an important factor affecting cancer worry.[23, 34, 35]
We are specifically interested in studying the differences in the relationship of optimism and fatalism with contributors to distress such as worry and fear about colonoscopy because in our past research we have identified fear as a more prominent CRC screening barrier than worry among low-income urban Latinos at average risk for CRC.[10] In addition, when compared to whites, Latinos have been shown to have higher fatalism about CRC.[6, 16] However, less is known about the level of optimism and its relation to colonoscopy fear, worry and fatalism about CRC screening among Latinos. If these relationships are better understood, one can attempt to alleviate CRC-related distress by developing culturally relevant health education interventions that aim to combat fatalistic beliefs and promote optimism about health screening in the Latino population.
In this cross-sectional study we hypothesize that: 1. Optimism is negatively related to colonoscopy worry and fear and 2. Fatalism is positively related to colonoscopy worry and fear and is negatively correlated with optimism.
Methods
Study Sample and Recruitment
Two hundred sixty three individuals were approached to participate between May 2012 – December 2013 in an ongoing IRB-approved parent randomized control trial (NCI R01 CA140737-01A2 “Improving CRC Screening for Diverse Hispanics in an Urban Primary Care Setting”) at the Icahn School of Medicine at Mount Sinai’s primary care facility after receiving a referral for screening colonoscopy from their primary care physician (PCP). Twelve people (5%) refused to participate. Their age, gender, and reason for refusal were recorded. Two hundred fifty one individuals were thus consented in English or Spanish, depending on their choice and subsequently administered the baseline face-to-face interview by a trained bilingual research assistant. Eligibility criteria included: 1) self-identified Latino; 2) ages 50–85; 3) no personal or immediate family history of CRC; 4) no history of gastrointestinal disorder; 5) no colonoscopy procedure in the last five years; 6) referral for screening colonoscopy by PCP; 7) English or Spanish-speaking and; 8) having a telephone. This cross-sectional study analyzed the data obtained during the baseline assessment. Each respondent received $20 in cash for their participation in the interview. IRB approval was gained for this study.
Measures
The following information was collected during the interview: 1) socio-demographic data; 2) personal/family healthcare data and; 3) psychosocial measures. We used the English or Spanish versions of measures depending on participant’s language preference. The Spanish versions of the measures were published in our previous study of 400 Latinos with the exception of the optimism.[10]
The socio-demographic measures included: age, gender, income level, education, marital status, employment status, country of origin, years lived in the US, and language in which the interview was conducted. Additionally, an abbreviated, 9-item Acculturation scale was used which evaluated language preference in social interactions, media use, and healthcare provider communications (1- “only Spanish” to 5 – “only English”) with internal consistency of α=0.94.[36]
In the healthcare section of the interview, we assessed whether participants had a regular PCP and their trust in their physician using a 5-point Likert scale (1- “strongly disagree” to 5 – “strongly agree”). Personal and family history of any cancer diagnosis and cancer-related deaths in family were assessed. Cancer history and deaths were analyzed using dichotomized variables (1 – “yes”; 0 – “no”). Finally, participants were asked to report their perception of their own health on a 5-point scale (1 – “excellent” to 5 – “poor”).
Psychosocial measures assessed: 1) optimism; 2) worry about the colonoscopy; 3) fatalism; 4) and fear of a colonoscopy. Optimism was measured using the Life Orientation Test – Revised (LOT-R).[25] The Spanish version of LOT-R was created by Perzcek and colleagues who showed a high degree of convergence across English and Spanish languages.[37] The Spanish and English versions of LOT-R consisted of nine items (six active and three fillers) with responses recorded using a 5-point Likert scale (1 – “Strongly Agree”; 5 “Strongly Disagree”) with a higher score indicating higher optimism. Example items include: “I rarely count on good things happen to me” or “I’m always optimistic about my future.” The internal consistency of the LOT-R measure in our sample is borderline acceptable (α= 0.59) when using scoring items only; and acceptable (α=0.66) when all scoring and filler items are used. The alpha values are lower than those obtained by Perczek and colleagues [37] in their work comparing reliability of English (α=0.84) and Spanish (α=0.79) LOT-R values. To further investigate the sensitivity of the LOT-R measure in our sample, we performed the analysis for both long and short LOT-R measures (with and without fillers respectively) and noted that the results did not change. Therefore we concluded that using original short LOT-R measure is acceptable because there was no effect on the study results for either scale. The results using the original LOT-R scale are reported in this study.
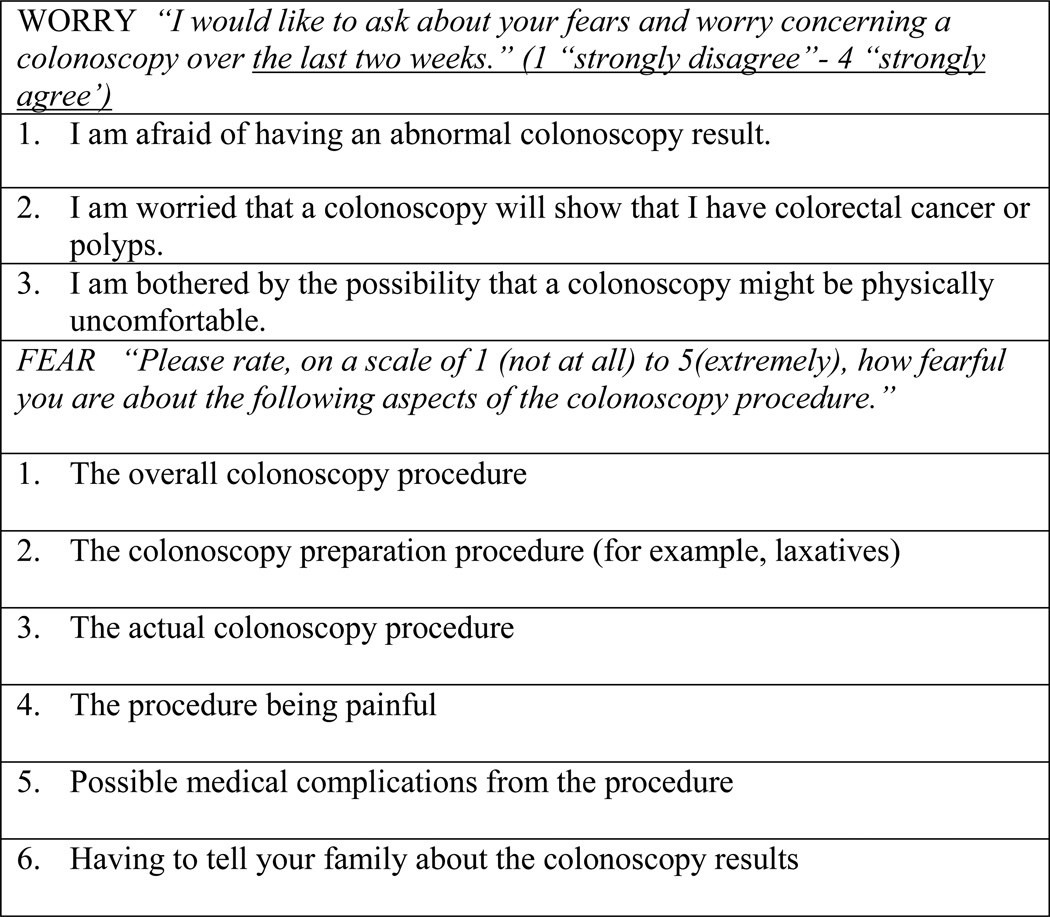
Worry about colonoscopy (Figure 1) was assessed using a 3- item measure that evaluates the participants’ degree of worry and fear about having a colonoscopy during the two weeks prior to the interview. Items included statements such as “I am afraid to have an abnormal colonoscopy result.” The results produce continuous distribution scores using a 4-point Likert scale (1 –“strongly disagree” to 4 “strongly agree”) with good internal consistency (α=0.83).[20]
Figure 1.
Measures of Worry and Fear.
Fatalism was assessed using an abbreviated version of Powe’s measure.[38] Based on our prior research, the originally 15-item inventory was reduced to five items and included statements such as “I believe that if someone has colorectal cancer, it is already too late to do anything about it”. The responses were recorded on a dichotomous scale (1 - “yes” or 0 - “no”). The internal consistency of the abbreviated measure in our sample remained favorable (α=0.84).
Fear of Colonoscopy (Figure 1) was assessed with a 6-item scale used in our previous study. [10] The scale assesses fear of colonoscopy and possible discovery of CRC. The scale produces a continuous score distribution from 1 - “not at all fearful” to 5 - “extremely fearful” and asks participants to rate their level of fear associated with preparation for the colonoscopy, possible medical complications related to the procedure, and having to tell their family about the results. The internal consistency for the measure in our sample is favorable (α=0.85).
Analysis
We first performed descriptive statistics for our sample including socio-demographic, healthcare, and psychosocial variables. We checked model variables for the presence of outliers and internal consistency. Because data were obtained via interview, the amount of missing data was minimized. Summary scores were calculated by adding responses to individual items for measures of fear, worry, optimism, fatalism and acculturation; these scores were used in the regression models. The summary scores for participants who did not answer all individual items were excluded from the analysis. We conducted a simple regression analysis of our model’s dependent variables (fear and worry) with socio-demographic variables (i.e. income, education) and healthcare variables (i.e. personal and family history of cancer, level of physician trust) in order to identify significant relationships. Finally, the significant variables obtained from univariate regressions were included in two multiple regression models that separately analyzed their relationships with worry and fear. Data were analyzed using STATA SE 12 (64-bit) and SPSS 19.0.
Results
Demographic and healthcare characteristics of the sample and mean values for psychometric variables are reported in Table 1. The study sample included 251 participants, all of Latino origin with 69% born outside the United States. The mean age was 60 years. There were 63% females in the sample, and 37% males. Those who refused to participate did not differ by age, however there were more males among refusers than females (67% and 33% respectively). Fifty four percent had less than a high school education. Sixty one percent reported annual household income of less than $10,000, and 86% had income of less than $20,000/year. More than half reported that they had at least one relative affected by cancer (54%). In addition, one fifth of the sample reported putting off medical problems or not following doctor’s advice in the last year (21% and 19% respectively).
Table 1.
Demographics and healthcare characteristics (N=251)
| Variable | N (%) | ||
|---|---|---|---|
| Socio-demographic characteristics | |||
| Age | |||
| 50–60 | 141 (56.2%) | ||
| Over 60 | 110 (43.8%) | ||
| Mean Age 59.9 (SD 7.7) | |||
| Gender | |||
| Male | 92 (36.7%) | ||
| Female | 159 (63.3%) | ||
| US Born Status | |||
| Born in United States | 77 (30.7%) | ||
| Born outside United States | 174 (69.3%) | ||
| Education | |||
| Less than High School | 136 (54.4%) | ||
| High School | 60 (24%) | ||
| Some College | 32 (12.8%) | ||
| College or higher | 22 (8.8%) | ||
| Annual household income | |||
| Less than 10,000/year | 147 (60.7%) | ||
| $10,000 to $19,999 | 60 (24.8%) | ||
| $20,000/year or more | 35 (14.5%) | ||
| Healthcare characteristics | |||
| Family History of Cancer | |||
| Yes | 134 (53.8%) | ||
| No | 115 (46.2%) | ||
| Put Off Medical Problem in the last 12 months | |||
| Yes | 52 (20.8%) | ||
| No | 198 (79.2%) | ||
| Did not follow doctor’s advice in the last 12 months | |||
| Yes | 46 (18.5%) | ||
| No | 202 (81.5%) | ||
| Mean values for psychometric model components | |||
| Measure | Mean Score |
SD | N |
| Optimism (LOT-R) | 22.5 | 3.8 | 250 |
| Fatalism | 1.5 | 1.8 | 239 |
| Fear | 11.8 | 6.1 | 249 |
| Worry | 7.5 | 2.6 | 251 |
Table 2 presents univariate relationships between demographic, psychosocial, and healthcare variables and fear and worry about colonoscopy and CRC. Greater optimism (β=−1.72, p<0.000), lower fatalism (β =0.29, p<0.01), and an absence of family history of cancer (β=1, p<0.01) were associated with less worry. Being a woman (β=0.85, p<0.05) and born in the United States (β =1.1, p<0.01) were associated with greater worry about colonoscopy and the possibility of having CRC. Putting off medical problems (β=1.06, p<0.01) was associated with greater worry. Both age (β=−0.04, p <0.05) and level of acculturation (β =0.04, p<0.01) had minimal, although statistically significant, association with worry which led to their inclusion in multiple regression analysis.
Table 2.
Simple Regression Relationships Between Worry/Fear and Demographic, Healthcare and Psychometric Measures
| Variable | Worry β coefficient |
N | Fear β coefficient |
N |
|---|---|---|---|---|
| Optimism | −1.72*** | 250 | −0.20^ | 248 |
| Fatalism | 0.29** | 239 | .31 | 237 |
| Acculturation | 0.04** | 236 | 0.07^ | 234 |
| Gender | 0.85* | 251 | 2.9*** | 249 |
| Age | −0.04* | 251 | −0.08 | 249 |
| US born status | 1.1** | 251 | 1.1 | 249 |
| Family History of Cancer | 1.0** | 249 | 2.6** | 247 |
| Put off medical problem | 1.06** | 250 | 1.9* | 248 |
| Did not follow doctor’s advice | 0.58 | 248 | 2.7** | 246 |
p<0.000;
P<0.01;
P<0.05;
P=0.053
Presence of a family history of cancer (β =2.6, p<0.01), female gender (β =2.9, p<0.000), not following doctor’s advice (β=2.7, p<0.01), and putting off a medical problem (β =1.9, p<0.05) were associated with greater fear. Interestingly, in contrast to worry, fear was not significantly associated with fatalism, and level of optimism only showed a trend of small negative association with fear (β=−0.2, p=0.053). Finally, income level was not significantly correlated with either fear or worry
In the multiple regression model, lower optimism (β=−0.09, p<0.05), higher fatalism (β=0.28, p<0.01), and female gender (β=0.9, p <0.05) were significantly associated with greater worry although the relationship for optimism was weaker when compared to simple regression analysis. (Adjusted R2 =0.14).
The multiple regression model for fear of colonoscopy demonstrated a positive association of fear with female gender (β=3.1, p<0.000), not following doctor’s advice (β=2.5, p<0.05), and family history of cancer (β =1.96, p <0.05) (Adjusted R2 =0.13). The results are summarized in Tables 2 and 3.
Table 3.
Multiple Regression Relationships Between Worry/Fear and Demographic, Healthcare and Psychometric Measures
| Model 1 Β coefficient |
Model 2 Β coefficient |
|
|---|---|---|
| Worry | Fear | |
| N | 222 | 228 |
| Adjusted R2 | 0.14 | 0.13 |
| Optimism | −0.09* | −0.13 |
| Fatalism | 0.28** | N/A |
| Acculturation | 0.03 | 0.06 |
| Gender | 0.90* | 3.1*** |
| Age | −0.02 | N/A |
| US born status | 0.64 | N/A |
| Family History of Cancer | 0.62 | 1.96* |
| Put off medical problem | 0.47 | 0.88 |
| Did not follow doctor’s advice | N/A | 2.5* |
p<0.000;
P<0.01;
P<0.05;
Discussion
Cancer fear and worry have been shown to act as barriers to colonoscopy screening among Latinos.[6, 10, 11, 13–15] In this study, we investigated how psychosocial, demographic, and healthcare variables relate to measures of fear and worry about colonoscopy procedure and CRC. We found that fatalism and optimism had opposite associations with level of worry about colonoscopy. Previous research identified a negative relationship of optimism with worry and distress in the context of cancer survivors or individuals expecting to undergo the colonoscopy procedure.[18, 19] The studies of the relationship of fatalism and worry are limited and mainly focus on the association of fatalism and perceived risk and the effect of the latter on cancer worry.[21, 23, 34, 35] Our results demonstrate that both lower fatalism and greater optimism were associated with less worry, although the association for optimism was small. Though optimism and fatalism were negatively correlated (β=−0.80, p<0.000), both remained significant in multiple regression models after controlling for demographics, family history of any cancer and health behavior characteristics, and improved the model fit.
Interestingly, colonoscopy fear was not significantly associated with fatalism and showed a trend of negative association with optimism which was not significant in the multiple regression analysis. Greater optimism has been shown to be associated with less fear in the limited number of studies looking at laboratory-induced stress [30] or in the setting of hematopoietic stem cell transplantation. [29] To our knowledge, this is the first study to examine the relationship of fear and optimism in a population of Latinos in primary care setting who had recently been referred for a colonoscopy. Fear has been repeatedly reported as a CRC screening barrier among Latinos [6, 10], which is consistent with our findings that fear was positively associated with putting off medical problem and not following doctor’s advice when controlling for other factors.
One explanation for the observed results could arise from the detailed review of what the worry and fear measures inform us about (Figure 1) the participants’ perceptions. Fear items focus on the colonoscopy procedure: five out of six items inquire about the level of fear of different aspects of colonoscopy while only one item asks about fear of an abnormal result (CRC). Colonoscopy worry is more focused on discovering CRC (two items), with only one question referring to procedure. This may suggest that optimism and fatalism are more associated with participants’ feelings about an abnormal colonoscopy result and have less association with the procedure itself. Furthermore, fear and its significant relationship with health behavior variables (i.e. not following doctor’s advice) may suggest a stronger link between patients’ feelings specifically about the procedure and can affect their adherence to provider’s recommendation for medical interventions. This is consistent with other studies demonstrating that fear was a barrier to colonoscopy.[6, 10, 13]
We also found that female gender was associated with greater worry and fear. This was perhaps due to machismo attitudes among Latino males who may be less willing to report feelings of distress. [6] Nevertheless, female gender was significant for both worry and fear when controlling for other model components. Finally, family history of any cancer had a significant positive association with worry and particularly fear. Consistent with our findings, Ferrer and colleagues reported a positive association between family cancer history and worry.[21] Importantly, over half of our study participants reported a history of cancer in their family. This high prevalence and its association with greater fear suggests that fear of colonoscopy can be quite common among Latinos. This also adds to our understanding of fear as a barrier to CRC screening and contributes to earlier findings of CRC family history as a factor associated with lower screening among Latinos in contrast to Whites.[39]
The results of this study may be utilized in the development of comprehensive health interventions that focus on neutralizing feelings of fear about the colonoscopy and due to family history of cancer, and promoting lower fatalism and higher optimism using increased knowledge of CRC preventability/curability and therapeutic benefits of colonoscopy. One possible intervention can be patient navigation programs that have been shown to improve colonoscopy screening among low-income minority populations. [17, 40]
Limitations
Our study has limitations. First, there is some overlap between the measures of fear and worry as they both include questions about colonoscopy and screening results. In the future, it is advisable to separately analyze worry and fear about the procedure and its results in order to clarify differences between the measures. There is also potential participation bias of less compliant individuals because study eligibility criteria required no colonoscopy in the last 5 years. Given that screening is recommended from age 50, and our sample mean age is 60, it is possible that participants received a colonoscopy referral previously and didn’t adhere to recommendation or had had a previous colonoscopy. In the future it is advisable to check medical records or ask participants about prior colonoscopy referrals and completion to assess their past experience and compliance. In addition, the internal consistency of the optimism measure was low which could have affected our results. The internal consistency, lower than that reported by Perzcek, can be due to differences in sample characteristics and interview methodology. Perzcek interviewed a group of Spanish-English bilingual individuals with a mean age of 19 years. The same bilingual individuals responded to both English and Spanish versions possibly leading to their recall of initial responses and potential bias. Our sample consisted of significantly older individuals and we used one LOT-R version depending on participants’ language preference. This highlights the importance of testing the internal consistency with respect to specific sample and prompts further investigation of LOT-R for other Latino groups. Furthermore, the study sample has more females than males, therefore limiting generalizability to males. Gender is controlled for in the multiple regression analysis in order to address this limitation. Additional limitations include cross-sectional design which doesn’t inform causality; potential recall bias due to self-report nature of questions; low mean income with low variability across the sample which potentially led to no significant correlation between income and fear and worry. This makes results less generalizable to Latinos with higher income levels. Furthermore, the narrow geographic recruitment site – a single primary care clinic in East Harlem New York, poses limitations to generalizability to Latinos in non-urban parts of the country or to those with no access to PCP.
Conclusion
Interventions that address fatalism and promote optimism may help to mildly reduce level of worry among Latinos referred for colonoscopy. Culturally targeted interventions that address colonoscopy fear due to family history of any cancer, particularly among Latino women may be able to alleviate level of distress about CRC screening.
Acknowledgments
Funding: NCI R01 CA140737, Manuscript Preparation: Roxanne Unger
References
- 1.Mandel JS, et al. Reducing mortality from colorectal cancer by screening for fecal occult blood. Minnesota Colon Cancer Control Study. N Engl J Med. 1993;328(19):1365–1371. doi: 10.1056/NEJM199305133281901. [DOI] [PubMed] [Google Scholar]
- 2.Siegel R, Desantis C, Jemal A. Colorectal cancer statistics, 2014. CA Cancer J Clin. 2014;64(2):104–117. doi: 10.3322/caac.21220. [DOI] [PubMed] [Google Scholar]
- 3.Ennis SR, Rios-Vargas M, Albert NG. The Hispanic Population: 2010. [cited 2012 February 10];2010 Census Briefs. 2011 [Google Scholar]
- 4.Rex DK, et al. American College of Gastroenterology guidelines for colorectal cancer screening 2009 [corrected] Am J Gastroenterol. 2009;104(3):739–750. doi: 10.1038/ajg.2009.104. [DOI] [PubMed] [Google Scholar]
- 5.Stimpson JP, Pagan JA, Chen LW. Reducing racial and ethnic disparities in colorectal cancer screening is likely to require more than access to care. Health Aff (Millwood) 2012;31(12):2747–2754. doi: 10.1377/hlthaff.2011.1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang J, et al. Barriers to colorectal cancer screening in Hispanics in the United States: an integrative review. Appl Nurs Res. 2013;26(4):218–224. doi: 10.1016/j.apnr.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 7.Diaz JA, et al. Effect of language on colorectal cancer screening among Latinos and non-Latinos. Cancer Epidemiol Biomarkers Prev. 2008;17(8):2169–2173. doi: 10.1158/1055-9965.EPI-07-2692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ellison J, et al. Screening adherence for colorectal cancer among immigrant Hispanic women. J Natl Med Assoc. 2011;103(8):681–688. doi: 10.1016/s0027-9684(15)30407-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Holden DJ, et al. Systematic review: enhancing the use and quality of colorectal cancer screening. Ann Intern Med. 2010;152(10):668–676. doi: 10.7326/0003-4819-152-10-201005180-00239. [DOI] [PubMed] [Google Scholar]
- 10.Jandorf L, et al. Understanding the barriers and facilitators of colorectal cancer screening among low income immigrant hispanics. J Immigr Minor Health. 2010;12(4):462–469. doi: 10.1007/s10903-009-9274-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shelton RC, et al. The influence of sociocultural factors on colonoscopy and FOBT screening adherence among low-income Hispanics. J Health Care Poor Underserved. 2011;22(3):925–944. doi: 10.1353/hpu.2011.0074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shokar NK, Vernon SW, Weller SC. Cancer and colorectal cancer: knowledge, beliefs, and screening preferences of a diverse patient population. Fam Med. 2005;37(5):341–347. [PubMed] [Google Scholar]
- 13.Bynum SA, et al. Unwillingness to participate in colorectal cancer screening: examining fears, attitudes, and medical mistrust in an ethnically diverse sample of adults 50 years and older. Am J Health Promot. 2012;26(5):295–300. doi: 10.4278/ajhp.110113-QUAN-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Green AR, et al. Barriers to screening colonoscopy for low-income Latino and white patients in an urban community health center. J Gen Intern Med. 2008;23(6):834–840. doi: 10.1007/s11606-008-0572-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Robinson CM, et al. Barriers to colorectal cancer screening among publicly insured urban women: no knowledge of tests and no clinician recommendation. J Natl Med Assoc. 2011;103(8):746–753. doi: 10.1016/s0027-9684(15)30414-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jun J, Oh KM. Asian and Hispanic Americans' cancer fatalism and colon cancer screening. Am J Health Behav. 2013;37(2):145–154. doi: 10.5993/AJHB.37.2.1. [DOI] [PubMed] [Google Scholar]
- 17.Philip EJ, DuHamel K, Jandorf L. Evaluating the impact of an educational intervention to increase CRC screening rates in the African American community: a preliminary study. Cancer Causes Control. 2010;21(10):1685–1691. doi: 10.1007/s10552-010-9597-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deimling GT, et al. Cancer-related health worries and psychological distress among older adult, long-term cancer survivors. Psychooncology. 2006;15(4):306–320. doi: 10.1002/pon.955. [DOI] [PubMed] [Google Scholar]
- 19.Parker J, Kennedy P. Factors predictive of distress in people awaiting a lower gastro-intestinal endoscopy. Psychol Health Med. 2010;15(1):26–33. doi: 10.1080/13548500903440221. [DOI] [PubMed] [Google Scholar]
- 20.Vernon SW, Myers RE, Tilley BC. Development and validation of an instrument to measure factors related to colorectal cancer screening adherence. Cancer Epidemiol Biomarkers Prev. 1997;6(10):825–832. [PubMed] [Google Scholar]
- 21.Ferrer RA, et al. Relationships among health perceptions vary depending on stage of readiness for colorectal cancer screening. Health Psychol. 2011;30(5):525–535. doi: 10.1037/a0023583. [DOI] [PubMed] [Google Scholar]
- 22.McGregor BA, et al. Optimism, perceived risk of breast cancer, and cancer worry among a community-based sample of women. Health Psychol. 2004;23(4):339–344. doi: 10.1037/0278-6133.23.4.339. [DOI] [PubMed] [Google Scholar]
- 23.Moser RP, et al. Associations of perceived risk and worry with cancer health-protective actions: data from the Health Information National Trends Survey (HINTS) J Health Psychol. 2007;12(1):53–65. doi: 10.1177/1359105307071735. [DOI] [PubMed] [Google Scholar]
- 24.Schnur JB, et al. Perceived risk and worry about prostate cancer: a proposed conceptual model. Behav Med. 2006;32(3):89–96. doi: 10.3200/BMED.32.3.89-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J Pers Soc Psychol. 1994;67(6):1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 26.Antoni MH, et al. Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychol. 2001;20(1):20–32. doi: 10.1037//0278-6133.20.1.20. [DOI] [PubMed] [Google Scholar]
- 27.Virginia Lee S, Cohen R. Meaning-making intervention during breast or colorectal cancer treatment improves self-esteem, optimism, and self-efficacy. Social Science & Medicine Volume. 2006:31–33. doi: 10.1016/j.socscimed.2005.11.041. [DOI] [PubMed] [Google Scholar]
- 28.Han PK, et al. Communication of uncertainty regarding individualized cancer risk estimates: effects and influential factors. Med Decis Making. 2011;31(2):354–366. doi: 10.1177/0272989X10371830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DuHamel KN, et al. Optimism and life events as predictors of fear appraisals in mothers of children undergoing hematopoietic stem cell transplantation. Psychooncology. 2007;16(9):821–833. doi: 10.1002/pon.1132. [DOI] [PubMed] [Google Scholar]
- 30.Kimhi S, Eshel Y, Shahar E. Optimism as a predictor of the effects of laboratory-induced stress on fears and hope. Int J Psychol. 2012 doi: 10.1080/00207594.2012.676181. [DOI] [PubMed] [Google Scholar]
- 31.Royse D, Dignan M. Fatalism and cancer screening in Appalachian Kentucky. Fam Community Health. 2011;34(2):126–133. doi: 10.1097/FCH.0b013e31820e0d5d. [DOI] [PubMed] [Google Scholar]
- 32.Niederdeppe J, Levy AG. Fatalistic beliefs about cancer prevention and three prevention behaviors. Cancer Epidemiol Biomarkers Prev. 2007;16(5):998–1003. doi: 10.1158/1055-9965.EPI-06-0608. [DOI] [PubMed] [Google Scholar]
- 33.Powe BD, Finnie R. Cancer fatalism: the state of the science. Cancer Nurs. 2003;26(6):454–465. doi: 10.1097/00002820-200312000-00005. quiz 466–7. [DOI] [PubMed] [Google Scholar]
- 34.Dillard AJ, et al. Risk perception measures' associations with behavior intentions, affect, and cognition following colon cancer screening messages. Health Psychol. 2012;31(1):106–113. doi: 10.1037/a0024787. [DOI] [PubMed] [Google Scholar]
- 35.Price MA, et al. Predictors of cancer worry in unaffected women from high risk breast cancer families: risk perception is not the primary issue. J Genet Couns. 2007;16(5):635–644. doi: 10.1007/s10897-007-9105-4. [DOI] [PubMed] [Google Scholar]
- 36.Marin G, et al. Development of a Short Acculturation Scale for Hispanics. Hispanic Journal of Behavioral Sciences. 1987;9(2):183–205. [Google Scholar]
- 37.Perczek R, et al. Coping, mood, and aspects of personality in Spanish translation and evidence of convergence with English versions. J Pers Assess. 2000;74(1):63–87. doi: 10.1207/S15327752JPA740105. [DOI] [PubMed] [Google Scholar]
- 38.Powe BD. Fatalism among Elderly African-Americans - Effects on Colorectal-Cancer Screening. Cancer Nursing. 1995;18(5):385–392. [PubMed] [Google Scholar]
- 39.Ponce NA, et al. Disparities in cancer screening in individuals with a family history of breast or colorectal cancer. Cancer. 2012;118(6):1656–1663. doi: 10.1002/cncr.26480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Percac-Lima S, et al. A culturally tailored navigator program for colorectal cancer screening in a community health center: a randomized, controlled trial. J Gen Intern Med. 2009;24(2):211–217. doi: 10.1007/s11606-008-0864-x. [DOI] [PMC free article] [PubMed] [Google Scholar]