Abstract
Objective
We prospectively examine evidence for the sustained effects of early intervention based on a follow-up study of 39 children with ASD who began participation in a randomized clinical trial testing the effectiveness of the Early Start Denver Model (ESDM) at age 18–30 months. The intervention, conducted at a high level of intensity in-home for 2 years, showed evidence of efficacy immediately posttreatment.
Method
This group of children was assessed at age 6, two years after the intervention ended, across multiple domains of functioning by clinicians naïve to previous intervention group status.
Results
The ESDM group, on average, maintained gains made in early intervention during the 2-year follow-up period in overall intellectual ability, adaptive behavior, symptom severity, and challenging behavior. No group differences in core autism symptoms were found immediately posttreatment; however, two years later, the ESDM group demonstrated improved core autism symptoms and adaptive behavior as compared with the community-intervention-as-usual (COM) group. The two groups were not significantly different in terms of intellectual functioning at age 6. The two groups received equivalent intervention hours during the original study, but the ESDM group received fewer hours during the follow-up period.
Conclusion
These results provide evidence that gains from early intensive intervention are maintained 2 years later. Notably, core autism symptoms improved in the ESDM group over the follow-up period relative to the COM group. This improvement occurred at the same time the ESDM group received significantly fewer services. This is the first study to examine the role of early ESDM behavioral intervention initiated below 30 months of age in altering the longer term developmental course of autism.
Keywords: early, intervention, autism, long-term, outcomes
INTRODUCTION
Early intensive behavioral intervention is recognized as an efficacious approach for improving outcomes for young children with autism spectrum disorders (ASD). Intellectual ability, communication and language functioning, adaptive behavior, and educational placement and support have all been demonstrated to improve with early intervention.1–3 However, most studies of comprehensive, intensive intervention report only immediate outcomes at the end of intervention, and the degree to which these outcomes are sustained over time is largely unknown.4–6 This is an important question because it is possible that developmental gains achieved with early intervention could diminish after intensive services end. The one long-term outcome study of comprehensive intensive early intervention of which we are aware was published over 20 years ago, and followed 19 children from age 7 to age 11.5 years, all of whom participated in a seminal study of intensive behavioral intervention.1 Results showed that the intervention group maintained gains in IQ and adaptive behavior, suggesting that intervention effects may be long lasting.7
The Early Start Denver Model (ESDM)8 is a naturalistic behavioral intervention that integrates applied behavior analysis (ABA) methods with developmental approaches and parent coaching designed to promote learning, social reciprocity, and affective engagement. It is designed for children with ASD as young as 12 months of age, can be used in a variety of settings,9,10 and intervention goals are set within the context of a specified curriculum.11 In the first randomized clinical trial of the ESDM, children were directly assessed and diagnosed with an autism spectrum disorder at age 18–30 months and randomly assigned to either ESDM intervention or to treatment-as-usual in the greater Seattle-area community (Community; COM). The groups were stratified on sex and developmental quotient. The ESDM group was offered 2-hour intervention sessions twice a day, 5 days per week, for 2 years by trained therapists. The number of hours of therapist-delivered intervention (sum of both individual one-on-one hours and group intervention hours) did not significantly differ between the ESDM and COM group. Results indicated a positive impact of ESDM on child development across a number of domains, including intellectual ability, particularly in the expressive and receptive language domains, adaptive behavior, and less severe autism diagnosis at the end of intervention.3 Significant group differences in social behavior at outcome were also found.12 However, no significant group differences in autism symptom levels were found based on direct observation by examiners blinded to intervention group at the end of the study period.
The present study examined whether early intensive behavioral intervention with the ESDM had sustained effects two years later in this same cohort of children. This will be the first study to our knowledge to examine the role of early intensive behavioral intervention initiated below age 30 months in altering the long-term clinical course of ASD. We hypothesized (1) that children who received 2 years of ESDM in the previous RCT would maintain outcomes for two years after the end of the intervention study across all key developmental domains including IQ, adaptive behavior, autism symptom levels, challenging behavior, and diagnosis by demonstrating the same or better average levels of age-adjusted performance than at the end of study treatment, (2) that at age 6, the ESDM group would continue to show greater intellectual ability, adaptive behavior, and social functioning and less severe ASD diagnoses and challenging behavior levels as compared to children receiving treatment as usual, and that the groups would not differ in terms of core autism symptoms and repetitive behavior, consistent with results reported previously immediately after intervention. We further hypothesized (3) that the gains demonstrated immediately after intervention would generalize to peer relationships, a new domain of functioning that is developmentally relevant at age 6 but was not assessed as part of the original study.
METHOD
Participants
Thirty-nine children who participated in an RCT of early intensive intervention at the University of Washington were assessed at age 6 years. The original RCT study sample consisted of 48 children diagnosed with an ASD at age 18–30 months and randomized into two groups (ESDM n=24; COM n=24) stratified by developmental quotient and sex. Research diagnosis of ASD at baseline was based on direct assessment by expert clinicians with the Autism Diagnostic Interview-Revised (ADI-R),13 Autism Diagnostic Observation Schedule-WPS (ADOS-WPS),14 and clinical judgment using all available information. The ADI-R, a parent interview, and the ADOS-WPS, a semi-structured play observation, are both standardized measures used to diagnose ASD. In addition, information from family history, medical records, cognitive test scores, and clinical observation made during the course of the research assessments were considered when assigning the DSM-IV-TR diagnosis (see3 for details.) The two groups did not differ at baseline in severity of autism symptoms, chronological age, IQ, sex, or adaptive behaviors in the original RCT, nor were there baseline group differences for the subgroup of children who completed the 2-year follow-up assessment (all p’s > .05). All children who at baseline had a history of issues such as significant sensory or motor impairment, serious traumatic brain injury, major physical anomalies, genetic disorders associated with ASD (e.g., Fragile X syndrome), seizure disorder, or prenatal drug exposure were excluded from this study.3 This sample was assessed in the previous study at baseline, one, and two years post-randomization, coinciding with the end of ESDM intervention, and long-term follow-up was conducted at age 6 (hereafter referred to as baseline, 1-year, 2-year, and age-6 assessment, respectively). Attrition rates were equal across groups over the follow-up period (3 lost in each group). In the original RCT, from baseline to the end of the intervention period, the ESDM group lost no children, but the COM group lost 3 (ESDM, 1-year n=24, 2-year n=24, age-6 n=21; COM 1-year n=23, 2-year n=21, age-6 n=18). The age-6 follow-up sample was evaluated with the same diagnostic procedures used at the baseline and 2-year assessments.
Data reported for the current study were obtained when participating children were on average 6 years of age (M=72.9 months, SD=2.6, N=39). In the age-6 sample, 72% were Caucasian, with 9 girls and 30 boys (COM= 4 girls, ESDM=5 girls). Mothers were on average highly educated, with only 13% reporting no college, 23% reporting some college, and 64% reporting college completion. The treatment groups did not differ with regard to maternal education (ESDM: 62% college grad, 28% some college, 10% no college; COM: 70% college grad, 18% some college, 12% no college; Chi-square=0.63, p>.50). Median annual household incomes between the groups also did not differ (ESDM $90,000, COM $85,000; Wilcoxon rank sum test, W=152.5, p > .50).
Parents were interviewed about their children’s service use every 6 months from the end of the intervention study (2 years) to follow-up (age 6.) At each interview, parents were asked to characterize the child’s use of behavioral health treatments and therapy provided by allied health professionals that occurred since the last interview. During the follow-up period, the average amount of ABA-based therapy and other therapies (e.g., speech/language, occupational therapy, physical therapy) received were calculated. Roughly 41% (5 of 18 COM, 11 of 21 ESDM) children received no ABA-based therapy during this period. Given the skewed distributions of treatment hours received, group differences were examined with a nonparametric Wilcoxon rank sum test. The ESDM group received fewer ABA-based therapy hours/week (M=2.40, SD=2.97, range 0 to 8.4) than the COM group (M=4.36, SD=3.56, range 0 to 11.0); however, this was not significant (W=244.5, p=.108). The ESDM group received significantly fewer hours/week of other therapy services (M=1.64, SD=1.73, range 0 to 6.3) than the COM group (M=3.14, SD=2.33, range 0.6 to 7.8; W=2.68.0, p=.027). Interestingly, for the ESDM group, 41.5% of these therapy hours were in a group setting, whereas only 21.7% of these therapy hours in the COM group occurred in a group setting.
Procedures
Intellectual ability and autism symptom level were measured at all time points by a licensed clinical psychologist or doctoral students in clinical psychology under the supervision of a licensed clinical psychologist at the University of Washington. The assessors were naïve to the intervention status of the children at all assessments. Repetitive behavior, challenging behavior, and adaptive behavior were measured by parent-reported questionnaire at all time points. Peer relationships were measured by parent-reported interview at age 6. All study procedures were approved by the University of Washington Institutional Review Board and were conducted with written consent of primary caregivers.
Measures
Intellectual ability
The Differential Ability Scales (DAS)15 School Age Level were used to measure intellectual ability at age 6. This battery is designed and normed for use with children from ages 2 years 6 months to 17 years 11 months. We report a General Conceptual Ability (GCA) score reflecting conceptual and reasoning ability and cluster scores measuring verbal and nonverbal skill areas.
The Mullen Scales of Early Learning (Mullen)16 were used at baseline and 2-year assessments. This battery is a standardized developmental test for children ages birth to 68 months. Standardized t scores from four subscales (Fine Motor, Visual Reception, Expressive Language, Receptive Language) and standard score from the Early Learning Composite (ELC) were assessed at the end of intervention (2-year).
Adaptive behavior
The Vineland Scales of Adaptive Behavior (VABS)17 are a parent interview assessing social, communication, motor, and daily living skills with standard scores based on a large normative sample. We reported overall (Adaptive Behavior Composite; ABC) and subdomain (Socialization, Communication, Daily Living Skills) standard scores at 2-year and age 6.
Autism symptoms
The ADOS-WPS version14 is a semi-structured, standardized interaction and observation tool that measures autism symptoms in social relatedness, communication, play, and repetitive behaviors. At age 6, ADOS Total, Social Affect, Repetitive Behavior, and Severity scores are reported.18 It was administered at baseline, 2-year, and age-6.
The Repetitive Behavior Scale – Revised (RBS-R)19 is a parent questionnaire involving 43 items that characterize severity of repetitive behavior in ASD. It yields six domain scores (e.g., sameness, self-injurious behavior) and a total score. It was administered at age 6 and has been validated for use with children with ASD.20
Challenging behaviors
The Aberrant Behavior Checklist (ABC)21 is a reliable and valid 58-item measure of challenging behaviors known to occur in individuals with moderate to profound developmental disability. The scales were empirically derived by factor analysis. The following scales were used as measures of challenging behavior in this study: (1) Irritability (irritability, agitation, crying) and (2) Hyperactivity (hyperactivity, noncompliance). The child’s primary caregiver, usually the mother, completed this questionnaire at 2-year and age 6.
Peer relationships
The ADI-R13 is a semi-structured parent interview that assesses autism symptoms across three domains: social relatedness, communication, and repetitive behaviors. The mean of current behavior scores on items 61–65 (Imitative social play, Interest in children, Response to approach of other children, Group play with peers, Friendships) was utilized to assess peer relations on a scale from 0 (no concerns) to 3 (serious concerns).
Data Analysis
To examine the children’s long-term course of development following intervention, repeated-measures analyses of variance (ANOVAs) were conducted22 with treatment group as a between-subjects factor, and time point as a within-subjects factor. The results, along with effect sizes calculated using generalized η,2, 23, 24 are presented in Table 1. Group differences in peer relations between the ESDM and COM group at age 6 were assessed using one-tailed t-tests to evaluate whether the ESDM showed improved functioning over the COM group.
Table 1.
Child Outcome Variables: Treatment Group Differences With Time Point as a Repeated Measure
| Variable | Time | Community | ESDM | Effect | F | Gen. η2 | ||||
| M | SD | n | M | SD | n | |||||
|
IQ ELC/GCA |
T3 | 67.28 | 15.91 | 18 | 82.86 | 22.83 | 21 | Timea | 16.96*** | 0.049 |
| T4 | 79.83 | 23.64 | 18 | 90.52 | 26.36 | 21 | Tx Groupb | 3.66 | 0.081 | |
| Tx Group:Timec | 0.99 | 0.003 | ||||||||
| Verbal IQ | T3 | 68.33 | 17.75 | 18 | 81.76 | 23.87 | 21 | Time | 24.03*** | 0.089 |
| T4 | 84.89 | 20.14 | 18 | 91.29 | 22.52 | 21 | Tx Group | 2.45 | 0.053 | |
| Tx Group:Time | 1.75 | 0.007 | ||||||||
| Nonverbal IQ | T3 | 66.50 | 15.63 | 18 | 83.95 | 24.15 | 21 | Time | 11.85** | 0.038 |
| T4 | 78.72 | 27.56 | 18 | 90.33 | 26.38 | 21 | Tx Group Tx Group:Time |
4.05 1.17 |
0.088 0.004 |
|
| Vineland | ||||||||||
| Adapt Behavior | T3 | 59.00 | 9.46 | 16 | 69.35 | 13.94 | 17 | Time | 47.46*** | 0.177 |
| Composite | T4 | 72.06 | 13.86 | 16 | 81.41 | 17.27 | 17 | Tx Group | 4.77* | 0.117 |
| Tx Group:Time | 0.08 | 0.000 | ||||||||
| Communication | T3 | 69.71 | 15.53 | 17 | 83.06 | 20.61 | 17 | Time | 11.37** | 0.043 |
| T4 | 79.71 | 18.53 | 17 | 88.35 | 19.76 | 17 | Tx Group | 3.36 | 0.084 | |
| Tx Group:Time | 1.08 | 0.004 | ||||||||
| Daily Living | T3 | 58.76 | 8.67 | 17 | 66.06 | 11.83 | 17 | Time | 50.03*** | 0.266 |
| Skills | T4 | 77.71 | 16.40 | 17 | 83.06 | 21.56 | 17 | Tx Group | 1.86 | 0.043 |
| Tx Group:Time | 0.15 | 0.001 | ||||||||
| Socialization | T3 | 63.19 | 8.63 | 16 | 70.47 | 10.34 | 17 | Time | 17.97*** | 0.087 |
| T4 | 69.44 | 13.81 | 16 | 79.24 | 16.03 | 17 | Tx Group Tx Group:Time |
4.55* 0.50 |
0.109 0.003 |
|
| ADOS | ||||||||||
| Restricted/ | T3 | 4.00 | 2.14 | 18 | 3.24 | 1.79 | 21 | Time | 0.75 | 0.005 |
| Repetitive | T4 | 4.17 | 2.46 | 18 | 2.48 | 1.97 | 21 | Tx Group | 4.54* | 0.083 |
| Tx Group:Time | 1.84 | 0.013 | ||||||||
| Social Affect | T3 | 12.94 | 4.04 | 18 | 11.24 | 4.00 | 21 | Time | 6.66* | 0.038 |
| T4 | 11.83 | 4.85 | 18 | 8.76 | 5.47 | 21 | Tx Group | 3.28 | 0.065 | |
| Tx Group:Time | 0.96 | 0.006 | ||||||||
| Total | T3 | 16.94 | 4.50 | 18 | 14.48 | 5.31 | 21 | Time | 6.86* | 0.032 |
| T4 | 16.00 | 6.57 | 18 | 11.24 | 6.87 | 21 | Tx Group | 4.40* | 0.089 | |
| Tx Group:Time | 2.06 | 0.010 | ||||||||
| ABC | ||||||||||
| Hyperactivity | T3 | 16.40 | 10.03 | 15 | 13.00 | 8.46 | 17 | Time | 0.24 | 0.002 |
| T4 | 17.07 | 9.56 | 15 | 13.76 | 9.33 | 17 | Tx Group | 1.28 | 0.033 | |
| Tx Group:Time | 0.00 | 0.000 | ||||||||
| Irritability | T3 | 10.87 | 8.96 | 15 | 7.12 | 6.46 | 17 | Time | 0.05 | 0.000 |
| T4 | 12.13 | 10.42 | 15 | 6.47 | 6.67 | 17 | Tx Group | 3.35 | 0.081 | |
| Tx Group:Time | 0.51 | 0.004 | ||||||||
| RBS | ||||||||||
| Total score | T3 | 21.94 | 14.60 | 17 | 16.53 | 13.95 | 17 | Time | 2.23 | 0.009 |
| T4 | 26.76 | 17.65 | 17 | 17.35 | 12.84 | 17 | Tx Group | 2.45 | 0.062 | |
| Tx Group:Time | 1.12 | 0.005 | ||||||||
Note: ABC = Adaptive Behavior Composite; ADOS = Autism Diagnostic Observation Schedule; ELC = Early Learning Composite; ESDM = Early Start Denver Model; GCA = General Conceptual Ability; RBS = Repetitive Behavior Scale; Tx = treatment.
Time = Main effect for time point.
Tx Group= Main effect for treatment group.
Tx Group:Time = Treatment group by time point interaction.
p <.05;
p <.01;
p <.001
RESULTS
Developmental Outcomes Following Early Intervention
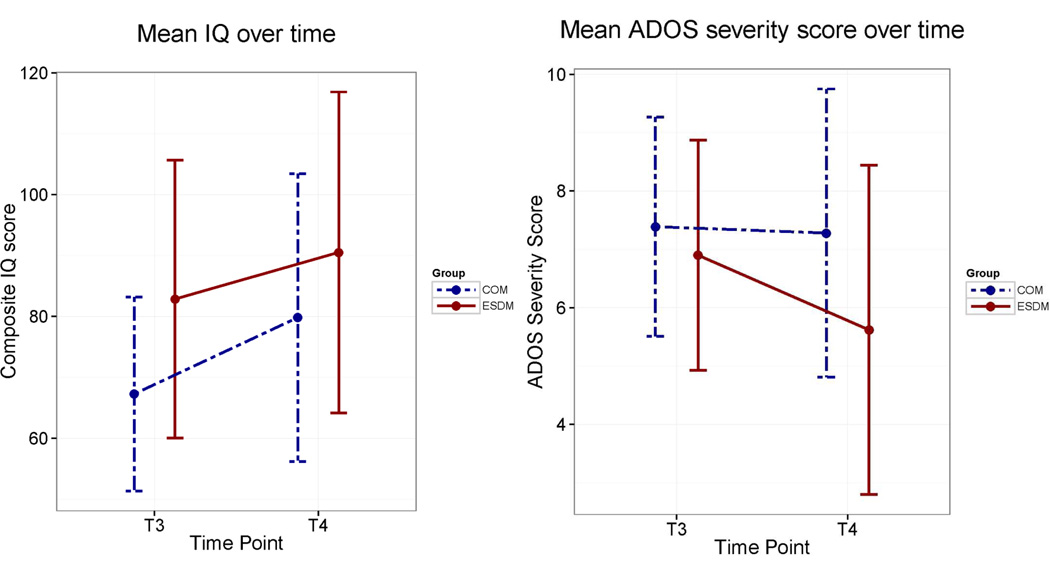
For all IQ and Vineland domains, there was a significant main effect of time, demonstrating continued improvement in intellectual and adaptive functioning for both treatment groups. There were no significant treatment group effects nor a treatment group-by-time interaction for the IQ variables. The ESDM group’s composite and nonverbal IQ scores remained 10 points higher at age 6; however, the treatment group effect fell short of significance (p = .063 and .051, respectively). A non-significant verbal IQ advantage for the ESDM group of 6.4 was observed (see Figure 1).
Figure 1.
IQ and Autism Diagnostic Observation Schedule (ADOS) severity by group and time point. Note: Error bars ± 1 SD. COM = community; ESDM = Early Start Denver Model.
Standard scores on the Vineland remained 5 to 10 points higher for the ESDM group at age 6. Significant group effects were present for the Vineland Adaptive Behavior Composite and Socialization scores. No significant group-by-time interactions were observed.
Core Symptom Outcomes Following Early Intervention
Significant treatment group effects were seen on ADOS Total and Restricted and Repetitive Behavior scores as the ESDM group showed lower overall scores. The ESDM group also had lower Social Affect scores; however, this difference fell short of significance (p = .078). There were significant time effects on the Social affect and Total scores, as overall age 6 scores were lower than those at age 4. There were no significant group-by-time interactions on any of the ADOS variables (see Figure 1).
Scores on the RBS were similar between ages 4 and 6 for both groups, with no significant effect of time. The Composite score was not significantly different between groups. The group-by-time interaction term was not significant.
Diagnostic Outcomes Following Early Intervention
There was no statistically significant difference in diagnostic categorization in the two groups at age 6 (Fishers exact probability test; p=.27; ESDM 57%, n=12 Autistic Disorder, 33% n=7 PDD, 10%, n=2 no diagnosis; COM 78% n=14 Autistic Disorder, 22% n=4 PDD). The two children in the ESDM group were classified as “no diagnosis” according to the clinical judgment of 2 expert clinicians blind to prior intervention group at age 6. At age 6, these two children obtained composite IQ scores of 92 and 110 and ADOS module 3 calibrated severity scores of 2 and 1, well short of the symptom levels for ASD classification. One child received an average of 4.50 hrs/wk of 1:1 ABA therapy and 0.32 hrs/wk of other group-based treatment between study completion and the 2-year follow-up assessment, with all education hours occurring in general education contexts. The second child received an average of 0.13 of other (non-ABA) treatment between study completion and the 2-year follow-up assessment, with 58% of educational hours occurring in a general education context and 42% in special education.
Challenging Behavior Outcomes
The Irritability and Hyperactivity subdomain scores were not significantly different, and there were no significant time effects, nor any group-by-time interactions.
Peer Relationship Outcomes
We hypothesized that the gains demonstrated immediately after intervention would generalize to improved peer relationships at age 6. There was a non-significant trend for the ESDM group to have more positive peer relationships than the COM group (COM M=1.37, SD=0.60; ESDM M=1.03, SD=0.57 [t, 1.84, p=.0741, ES=.57]).
DISCUSSION
The current study prospectively examined evidence for the sustained effects of early intensive behavioral intervention initiated between 18 and 30 months of age for children with ASD at age 6. Children in the ESDM group maintained the gains they made in early intervention 2 years later in all areas, including intellectual ability, adaptive behavior, autism symptoms, and challenging behaviors. This provides direct evidence these children did not exhibit a developmental regression, lose skills, or, in the case of standardized tests, slow their rate of development after withdrawal of early intensive services. Furthermore, at age 6, in comparison to the COM group, the ESDM group demonstrated better adaptive behavior and socialization ability and less severe overall ASD symptoms. The reduction in ASD symptom severity, revealed in direct assessments conducted by expert clinicians naive to intervention group (ADOS total and repetitive behavior), and parent report of improved socialization (VABS-II), was striking. We did not hypothesize this would be the case at age 6 because the ESDM group did not demonstrate this advantage at the end of the original RCT at age 4. Two children in the ESDM group, but not the COM group, no longer met criteria for ASD according to two expert clinicians naive to intervention group. The ESDM group demonstrated a non-significant trend toward better peer relations, a new domain of functioning assessed at age 6, compared to the COM group. Although both the ESDM and COM groups showed improvements in intellectual ability across the follow-up period there were no longer significant group differences at age 6, contrary to our hypothesis. This is the first report of long-term outcomes of a comprehensive intervention begun prior to 30 months of age in children with ASD and demonstrates continued positive impacts on development. Two years later, these children maintained the gains achieved over the course of the intervention period and long-term outcome data revealed improvement during follow-up in the ESDM group compared with the COM group in areas not seen at the end of the original RCT.
This convergence of evidence, from both parents and clinicians naïve to intervention group, suggests the possibility that the significant IQ, language, and social ability gains made by the end of the early intervention period were not just maintained, but had generalized to new areas of functioning. This was particularly notable because core ASD symptoms are one of the most difficult areas for demonstrating improvement. If replicated, these results could suggest a particular benefit of ESDM relative to other intervention options. It was also notable that group differences in intellectual ability seen at the end of early intervention were no longer present at age 6. Both groups increased standardized intellectual ability scores over the follow-up period, with the COM group increasing 12.55 points and the ESDM group increasing 7.66 points. Thus, the lack of statistically significant group differences was due to variability (i.e., large standard deviations in scores) and a larger mean increase in scores in the COM group rather than a loss of skills in the ESDM group.
The observed developmental gains in intellectual ability for both groups and decreased symptom severity for the ESDM group occurred in the context of community intervention and educational services. During the follow-up period, we assessed the number of hours of intervention that parents spontaneously sought for their children after completion of the RCT. The ESDM and COM groups significantly differed in the number of hours of ABA-based and other intervention they received. Parents of children in the ESDM group reported a reduction in one-on-one intervention hours from 15.2 hours per week during the study period to 4.04 hours per week during the follow-up period. Parents of children in the COM group reported one-on-one intervention hours were reduced from 9.1 hours per week during the study period to 7.5 hours per week during follow-up. The ESDM group increased their performance during a period of substantially reduced one-on-one services, suggesting that they may have increased their ability to learn from less restrictive, more naturalistic environments as a result of early intervention.
It is important to consider characteristics of this study that may limit the generalizability of these findings. The COM group received a similar number of intervention hours as the ESDM group during the initial study period. Although this was a strength of the study in terms of making valid group comparisons, it may suggest that the COM group had greater access to intervention than is typical. One effect of enrollment was that each family received early diagnosis and referrals to community services by a team of expert clinicians. In addition, this sample was recruited from a geographically constrained area, 30 minutes from an urban university. This was necessary in order for the university-based intervention team to be able to carry out high-intensity, in-home services without incurring extraordinary transportation expenses. But this meant that families from the COM group lived in close proximity to a number of excellent private intervention providers. Families that participated in this longitudinal study may differ from other families who did not participate in terms of ability and motivation to obtain high levels of early behavioral intervention for their children. We also observed high numbers of intervention hours in the comparison group from an RCT of a low-intensity, parent coaching intervention that we conducted with a different sample.25 In that study, the groups had received equivalent intervention hours up until randomization. But in a very short time, by the end of the twelve-week intervention period, there was a significant difference in the number of treatment hours children (aged 12–24 months) were receiving weekly, with the comparison group receiving more intervention (P-ESDM 1.48 [1.96]; community group 3.68 [3.91], p<.05.) It is possible that families who enroll in an RCT and are randomized to the control group might make even more effort to obtain intervention when they are not assigned to the intervention group. Thus, participating families, even those who are randomized to community intervention, may receive more and earlier intervention than other families in the same community.
Mothers in this study were on average highly educated, with only 13% reporting no college, 23% reporting some college, and 64% reporting college completion. In contrast, educational attainment among US women nationally is estimated as 32% no college; 33.6% some college; and 34.5% college completion or higher.26 Importantly for the purposes of this efficacy study, the two groups (ESDM and COM) had equivalent maternal education levels and were comparable to other groups of mothers who participate in research on child development at this university (e.g.,27). However, there is a critical need to evaluate the effectiveness of this and other early autism intervention programs in culturally diverse populations, less-educated families, and lower resource, rural, or military communities.
Measurement issues may also constrain the types of observations we are able to make. For example, our measure of symptom severity, the ADOS, has four different modules based on the verbal ability of the participant, ranging from Module 1 for non-verbal individuals to Module 4 for highly verbal adults. These modules contain a number of different activities and reflect qualitative differences in the expectations for a non-verbal individual as compared with individuals with more advanced communication abilities. Thus, individuals who have better verbal abilities have to meet higher expectations for social interaction. Thus, differences in symptom severity as measured by the ADOS should be interpreted cautiously.
This is a follow-up to a randomized trial of a manualized intervention with measured fidelity to the intervention model, clearly described inclusion criteria, well-matched groups prior to randomization, and assessment by clinicians who were naïve to intervention group. Attrition during the follow-up period was minimal and balanced across groups (3 in each), but should be noted. An inherent weakness in the community intervention-as-usual study design is the impossibility of adequately describing and quantifying the intervention received in community settings. This difficulty is amplified in the follow-up study period when children in both groups receive non-randomly assigned intervention of differing types and intensities. Although we carefully assessed the hours of intervention and general categories of intervention received, we were not able to create a single metric to directly compare community-delivered interventions due to unmeasured differences in implementation and practices. Thus, the impact of intervention received after the study period is unknown. However, we can observe that the comparison group in the present study appeared to have more positive outcomes than the comparison group in the only other long-term follow-up study of a comprehensive, intensive intervention.7 It is not unreasonable to speculate that one contributor to the positive outcomes in the COM group we report here is the availability and high quality of intervention in the greater Seattle area. We suspect that services for individuals with autism have greatly improved across many communities in the 20 years since the first long-term follow-up study7 was conducted. Future studies are needed to replicate these findings in independent samples, extend these findings to older ages, and investigate other styles and approaches to intervention.
These results demonstrate that significant, longer-term gains are possible with early, comprehensive, intensive intervention, and that these gains are evident not only in intellectual ability, language, and social behavior, but also in reductions in ASD symptoms. In two cases, children who received ESDM no longer met criteria for an ASD diagnosis. This study replicates the results of McEachin et al.7 but also extends those findings to intervention begun with children under 30 months of age and provided at less than half the number of hours per week, in a developmental style of delivery. A recent cost-comparison study of early intensive behavioral intervention in the Netherlands suggests that lifetime cost savings could be over one million Euros per individual.28 These findings demonstrate how early identification and intensive, early, ASD-specific intervention can improve long-term outcomes for children with ASD; they also suggest the need to extend this work into lower-resourced community settings to work toward improving outcomes for all children with ASD.
CLINICAL GUIDANCE.
Early intensive behavioral intervention has been found efficacious in improving developmental outcomes for young children with autism spectrum disorder.
Children were able to maintain the developmental gains they made in early, intensive, in-home intervention over a two-year follow-up period. These children did not exhibit developmental regression or lose skills, even after substantial reductions in services.
Intellectual, language, and adaptive functioning gains made as a result of early intervention may generalize to new domains of functioning, such as reduced ASD symptom severity, two years later.
Research is needed to extend these results to a more diverse range of families and communities to assess the effectiveness of early autism intervention.
Acknowledgments
This research was supported by grants from the National Institute of Mental Health, the National Institute of Child Health and Human Development (U19HD34565, P50HD066782, R01HD-55741), and the National Institute of Mental Health (U54MH066399).
Dr. Munson served as the statistical expert for this research.
The authors wish to thank the children and parents who participated in this study and Lena Tsui, MS, of the University of Washington Autism Center, for her devotion to keeping in touch with these children and parents.
Dr. Estes has received grant or research funding from the Simons Foundation, the National Institutes of Health, the National Institute of Mental Health, and the Autism Speaks Foundation. Dr. Rogers has received royalty payments and material fees related to the Early Start Denver Model (ESDM). She has also received occasional honoraria from Guilford Press for ESDM materials. She is a co-author of two books on early intervention: The Early Start Denver Model for Young Children With Autism: Promoting Language, Learning, and Engagement and An Early Start for Your Child With Autism from which she has received royalties (Guilford Press). Dr. Dawson is a co-author of two books on early intervention: The Early Start Denver Model for Young Children With Autism: Promoting Language, Learning, and Engagement and An Early Start for Your Child With Autism from which she has received royalties (Guilford Press).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure: Drs. Munson, Greenson, and Winter report no biomedical financial interests or potential conflicts of interest.
Contributor Information
Annette Estes, University of Washington Autism Center and University of Washington, Seattle..
Jeffrey Munson, University of Washington Autism Center and University of Washington, Seattle..
Sally J. Rogers, University of California, Davis..
Jessica Greenson, University of Washington Autism Center and University of Washington, Seattle..
Jamie Winter, Weill-Cornell Medical College, New York City..
Geraldine Dawson, Duke University, Durham, NC..
REFERENCES
- 1.Lovaas O. Behavioral treatment and normal educational and intellectual functioning in young autistic children. Journal of Consulting and Clinical Psychology. 1987;55(1):3–9. doi: 10.1037//0022-006x.55.1.3. [DOI] [PubMed] [Google Scholar]
- 2.Smith T, Groen A, Wynn J. Randomized trial of intensive early intervention for children with pervasive developmental disorder. American Journal on Mental Retardation. 2000;105(4):269–285. doi: 10.1352/0895-8017(2000)105<0269:RTOIEI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 3.Dawson G, Rogers S, Munson J, et al. Randomized, controlled trial of an intervention for toddlers with autism: the Early Start Denver Model. Pediatrics. 2010;125(1):e17–e23. doi: 10.1542/peds.2009-0958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tonge B, Bull K, Brereton A, Wilson R. A review of evidence-based early intervention for behavioural problems in children with autism spectrum disorder: the core components of effective programs, child-focused interventions and comprehensive treatment models. Current Opinion in Psychiatry. 2014;27(2):158–165. doi: 10.1097/YCO.0000000000000043. [DOI] [PubMed] [Google Scholar]
- 5.Magiati I, Tay XW, Howlin P. Early comprehensive behaviorally based interventions for children with autism spectrum disorders: a summary of findings from recent reviews and meta-analyses. Neuropsychiatry. 2012;2:543–570. [Google Scholar]
- 6.Matson JL, Konst MJ. What is the evidence for long term effects of early autism intervention? Research in Autism Spectrum Disorders. 2013;7:475–479. [Google Scholar]
- 7.McEachin J, Smith T, Lovaas O. Long-term outcome for children with autism who received early intensive behavioral treatment. American Journal of Mental Retardation: AJMR. 1993;97(4):359–372. [PubMed] [Google Scholar]
- 8.Rogers SJ, Dawson G. The Early Start Denver Model for Young Children with Autism: Promoting Language, Learning, and Engagement. New York: Guilford Press; [Google Scholar]
- 9.Rogers S, Lewis H. An effective day treatment model for young children with pervasive developmental disorders. Journal of the American Academy of Child and Adolescent Psychiatry. 1989;28(2):207–214. doi: 10.1097/00004583-198903000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Rogers S. Interventions that facilitate socialization in children with autism. Journal of Autism and Developmental Disorders. 2000;30(5):399–409. doi: 10.1023/a:1005543321840. [DOI] [PubMed] [Google Scholar]
- 11.Rogers SJ, Dawson G. The Early Start Denver Model for Young Children with Autism: The Curriculum. New York: Guilford Press; 2010. [Google Scholar]
- 12.Dawson G, Jones EJH, Merkle K, et al. Early behavioral intervention is associated with normalized brain activity in young children with autism. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51(11):1150–1159. doi: 10.1016/j.jaac.2012.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rutter M, LeCouteur A, Lord C. Autism diagnostic interview revised: WPS edition manual. Los Angeles: Western Psychological Services; 2003. [Google Scholar]
- 14.Lord C, Rutter M, DiLavore PC, Risi S. Autism diagnostic observation schedule manual. Los Angeles: Western Psychological Services; 2003. [Google Scholar]
- 15.Elliott CD. Differential Ability Scales: Introductory and Technical Handbook. San Antonio, TX: The Psychological Corporation; 1990. [Google Scholar]
- 16.Mullen EM. Mullen Scales of Early Learning: AGS edition. Circle Pines, MN: American Guidance Service Publishing; 1995. [Google Scholar]
- 17.Sparrow S, Balla D, Cicchetti D. Vineland Adaptive Behavior Scales. second edition. Shoreview, MN: American Guidance Service; 2005. [Google Scholar]
- 18.Gotham K, Risi S, Pickles A, Lord C. The Autism Diagnostic Observation Schedule: revised algorithms for improved diagnostic validity. Journal of Autism and Developmental Disorders. 2007;37(4):613–627. doi: 10.1007/s10803-006-0280-1. [DOI] [PubMed] [Google Scholar]
- 19.Bodfish J, Symons F, Parker D, Lewis M. Varieties of repetitive behavior in autism: comparisons to mental retardation. Journal of Autism and Developmental Disorders. 2000;30(3):237–243. doi: 10.1023/a:1005596502855. [DOI] [PubMed] [Google Scholar]
- 20.Lam K, Aman M. The Repetitive Behavior Scale-Revised: independent validation in individuals with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2007;37(5):855–866. doi: 10.1007/s10803-006-0213-z. [DOI] [PubMed] [Google Scholar]
- 21.Aman MG, Singh NN. Aberrant Behavior Checklist (abc) East Aurora, NY: Slosson Educational Publications, Inc; 1986. [Google Scholar]
- 22.Lawrence MA. ez: Easy analysis and visualization of factorial experiments. [Accessed March 1 2015];R package version 4.2-2. 2013 Available at http://CRAN.R-project.org/package=ez. [Google Scholar]
- 23.Bakeman R. Recommended effect size statistics for repeated measures designs. Behavioral Research Methods. 2005;37(3):379–384. doi: 10.3758/bf03192707. [DOI] [PubMed] [Google Scholar]
- 24.Olejnik S, Algina J. Generalized eta and omega squared statistics: measures of effect size for some common research designs. Psychological Methods. 2003;8(4):434–47. doi: 10.1037/1082-989X.8.4.434. [DOI] [PubMed] [Google Scholar]
- 25.Rogers SJ, Estes A, Lord C, et al. Effects of a brief ESDM-based parent intervention on toddlers at risk for ASD: A randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51:1052–1065. doi: 10.1016/j.jaac.2012.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.US Department of Health and Human Services Health Resources and Services Administration. Maternal and Child Health. [Accessed March 27, 2015];2013 Available at: www.mchb.hrsa.gov/whusa12/more/downloads/pdf/whousa12.pdf.
- 27.Brooks R, Meltzoff AN. Connecting the dots from infancy to childhood: A longitudinal study connecting gaze following, language, and explicit theory of mind. Journal of Experimental Child Psychology. 2015;130:67–78. doi: 10.1016/j.jecp.2014.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peters-Scheffer N, Didden R, Korzilius H, Matson J. Cost comparison of early intensive behavioral intervention and treatment as usual for children with autism spectrum disorder in The Netherlands. Research in Developmental Disabilities. 2012;33(6):1763–1772. doi: 10.1016/j.ridd.2012.04.006. [DOI] [PubMed] [Google Scholar]