Abstract
Background:
Volar locking plate fixation has become the gold standard in the treatment of unstable distal radius fractures. Juxta-articular screws should be placed as close as possible to the subchondral zone, in an optimized length to buttress the articular surface and address the contralateral cortical bone. On the other hand, intra-articular screw misplacements will promote osteoarthritis, while the penetration of the contralateral bone surface may result in tendon irritations and ruptures. The intraoperative control of fracture reduction and implant positioning is limited in the common postero-anterior and true lateral two-dimensional (2D)-fluoroscopic views. Therefore, additional 2D-fluoroscopic views in different projections and intraoperative three-dimensional (3D) fluoroscopy were recently reported. Nevertheless, their utility has issued controversies.
Objectives:
The following questions should be answered in this study; 1) Are the additional tangential view and the intraoperative 3D fluoroscopy useful in the clinical routine to detect persistent fracture dislocations and screw misplacements, to prevent revision surgery? 2) Which is the most dangerous plate hole for screw misplacement?
Patients and Methods:
A total of 48 patients (36 females and 13 males) with 49 unstable distal radius fractures (22 x 23 A; 2 x 23 B, and 25 x 23 C) were treated with a 2.4 mm variable angle LCP Two-Column volar distal radius plate (Synthes GmbH, Oberdorf, Switzerland) during a 10-month period. After final fixation, according to the manufactures' technique guide and control of implant placement in the two common perpendicular 2D-fluoroscopic images (postero-anterior and true lateral), an additional tangential view and intraoperative 3D fluoroscopic scan were performed to control the anatomic fracture reduction and screw placements. Intraoperative revision rates due to screw misplacements (intra-articular or overlength) were evaluated. Additionally, the number of surgeons, time and radiation-exposure, for each step of the operating procedure, were recorded.
Results:
In the standard 2D-fluoroscopic views (postero-anterior and true lateral projection), 22 screw misplacements of 232 inserted screws were not detected. Based on the additional tangential view, 12 screws were exchanged, followed by further 10 screws after performing the 3D fluoroscopic scan. The most lateral screw position had the highest risk for screw misplacement (accounting for 45.5% of all exchanged screws). The mean number of images for the tangential view was 3 ± 2.5 images. The mean surgical time was extended by 10.02 ± 3.82 minutes for the 3D fluoroscopic scan. An additional radiation exposure of 4.4 ± 4.5seconds, with a dose area product of 39.2 ± 14.5 cGy/cm2 were necessary for the tangential view and 54.4 ± 20.9 seconds with a dose area product of 2.1 ± 2.2 cGy/cm2, for the 3D fluoroscopic scan.
Conclusions:
We recommend the additional 2D-fluoroscopic tangential view for detection of screw misplacements caused by overlength, with penetration on the dorsal cortical surface of the distal radius, predominantly observed for the most lateral screw position. The use of intraoperative 3D fluoroscopy did not become accepted in our clinical routine, due to the technical demanding and time consuming procedure, with a limited image quality so far.
Keywords: Distal Radius Fracture, Intraoperative, Imaging, Screw Penetration, Doenicke View
1. Background
Volar locking plate fixation became the gold standard in operative treatment of unstable distal radius fractures (1-3). Juxta-articular screws should to be placed as close as possible to the subchondral zone, in an optimized length to buttress the articular surface and address the contralateral cortical bone, to prevent a fragment dislocation under early postoperative functional physiotherapy, especially in dorsal comminuted fractures (4-6). These demands, together with the use of variable angle stable plates, are associated with an increased risk of screw misplacements. Nevertheless, intra-articular screw placements will promote osteoarthritis, while the penetration of the contralateral bone surface may result in extensor tendon irritations and ruptures (7-9). If screw misplacement is confirmed postoperatively, revision surgery is required to avoid such iatrogenic complications. Therefore, conclusive intraoperative detection of screw misplacements is mandatory. The standard intraoperative control of anatomic fracture reduction and implant placement is the 2D-fluoroscopic view, in two perpendicular planes (postero-anterior and true lateral). These projection images are not sufficient to securely detect screw misplacements, due to the complex shaped distal radius, especially on the dorsal side (10-18). To the best of our knowledge, Doenicke et al. (19) were the first who described an additional 2D fluoroscopic tangential view to detect screw penetrations on the dorsal distal radius, due to screw overlength.
2. Objectives
In recent years, intraoperative 3D fluoroscopy was introduced to acquire CT-like images for the control of anatomic fracture reduction and prevention of implant misplacements, predominantly in articular fractures (20-23). The following two questions should be answered in this study:
Are the additional tangential view and the intraoperative 3D fluoroscopy useful in the clinical routine to detect persistent fracture dislocations and screw misplacements to prevent revision surgery?
Which is the most dangerous plate hole for screw misplacement?
3. Patients and Methods
Between February and November 2013, all patients with unstable distal radius fractures, treated with a polyaxial locking plate fixation [2.4 mm variable angle LCP Two-Column volar distal radius plate (Synthes GmbH, Oberdorf, Switzerland)], were prospectively included. Exclusion criteria were: I, patient’s age under 18 years; II, refusal of participation; or III, need for a dorsal approach or use of other implants. Surgical procedure: The operation was performed according to the manufactures technique guide. After final fixation of the distal radius fracture including the intraoperative control of fracture reduction and implant placement in the standard 2D fluoroscopy (postero-anterior and true lateral), the additional 2D fluoroscopic tangential view was performed first, followed by the final intraoperative 3D fluoroscopic scan. If any screw misplacement was detected, an exchange of screws was performed immediately after each image control (tangential view or 3D fluoroscopy). The senior consultant classified the fracture types according to the AO-Müller (AO) classification system and analyzed all intraoperative control images. The number and cause for screw exchanges, as well as procedure time (in minutes) and radiation exposure (no. of fluoroscopic images, fluoroscopy time and dose area product) were recorded for each step. Additionally, the number of surgeons and their level of education were documented.
3.1. Performing the 2D-Fluoroscopic Tangential View
The patient’s arm is placed on a radiolucent hand table, in 90° abduction, in the glenohumeral joint. The forearm is 70° flexed in the elbow, with a maximum volar tilt in the wrist joint to get a central fluoroscopic beam path perpendicular to the dorsal surface of the distal radius (Figures 1 and 2).
Figure 1. Image of an Intraoperative Two-Dimensional Fluoroscopic Tangential View (Doenicke View).
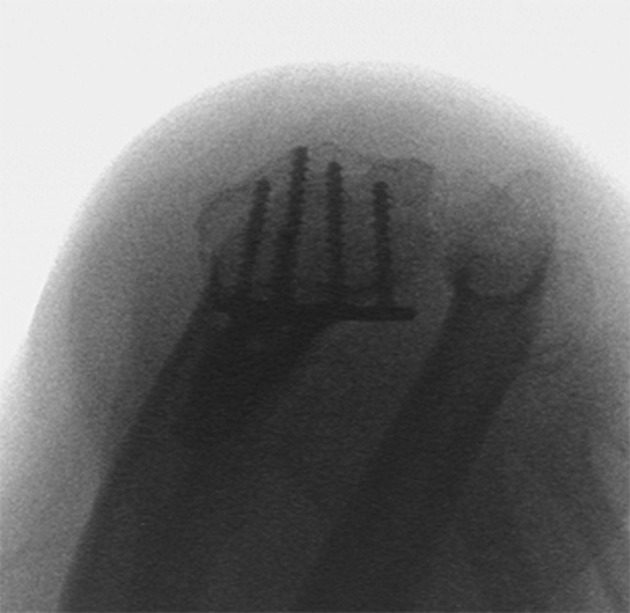
Figure 2. Two-Dimensional Reformation Images of the Intraoperative Three-Dimensional Fluoroscopic Scan After Volar Distal Radius Plating.

In the sagittal plane, perfect juxta-articular screw placements are displayed. In the coronal plane, a screw tip perforation was detected (the image quality in the axial plane is limited).
3.2. Performing the Intraoperative Three-Dimensional Fluoroscopic Scan
The patient’s arm is placed on a radiolucent hand-table in 90° abduction in the glenohumeral joint, with extension in the elbow and neutral position in the wrist. The c-arm (Ziehm Vario 3D, Ziehm Imaging GmbH, Nuremberg, Germany) is placed in a cephalad position, parallel to the patient’s body axis (Figure 3). After adjusting for the exact isocenter, focused on the wrist joint, a manual orbital rotation of 136°, without radiation, is performed as control-scan, to exclude a collision of the c-arm with the hand table. Finally, the operating team leaves the operating room for the automatic scan for image acquisition. Out of one hundred 2D-fluoroscopic images, a computed tomography like 3D data-set will be reconstructed, covering a cube dimension of approximately 12 × 12 × 12 cm. In reformatted 2D-slice imaging, the anatomic reduction and save screw placement were evaluated (Figure 4), while the second surgeon closed the wound.
Figure 3. Intraoperative Set-up and Patients’ Arm Position for the Acquisition of a 2D-Fluoroscopic Tangential View (Doenicke View).

Figure 4. Intraoperative Set-up and Patients’ Arm Position for a Correctly Performed Three-Dimensional Fluoroscopic Scan.

3.3. Statistical Analysis
A pre-hoc power analysis for an estimated screw misplacement rate of 20%, revealed a minimum study sample size of 46 patients (α-value of 0.05, power 0.8). The descriptive statistical analysis was performed using SPSS 20 (SPSS Inc., Chicago, IL, USA). The study was approved by the institutional ethics committee (No. 3630-12/2012).
4. Results
The study included 48 patients (37 women, 11 men) with 49 distal radius fractures (22 right wrist, 25 left wrist, and one, both wrists). The patient’s characteristics are displayed in Table 1. The most common fracture type, according to the AO classification system, was the A3 fracture. Of the total, 15 radius fracture diagnoses were performed by senior consultants while 34 radius fractures by residents under supervision. The mean procedure time was 79 ± 20 minutes. A total of 7.3 fluoroscopic images (14.1 ± 8.2 seconds fluoroscopic time, and 10.0 ± 19.7 cGy/cm2 dose area product) were necessary for the standard operating procedure.
Table 1. Patients’ Characteristics.
| Variables | Fracture Type Distribution Due to AO Classification | Wrist | Mean Age in Years ± SD (Range) | ||||
|---|---|---|---|---|---|---|---|
| A | B | C | Left Side | Right Side | Both Sides | ||
| All patients | 22 | 2 | 15 | 25 | 22 | 1 | 62.1 ± 16.3 (22 - 84) |
| Female | 17 | 2 | 18 | 20 | 17 | 0 | 66.7 ± 11.8 (45 - 84) |
| Male | 5 | 0 | 7 | 5 | 5 | 1 | 47.9 ± 16.7 (22 - 72) |
4.1. Two-Dimensional Fluoroscopic Tangential View
The additional images were 3 ± 2.5 fluoroscopic images (4.4 ± 4.5 seconds fluoroscopy time, 2.12 ± 2.21 cGy/cm2 dose area product), which were necessary to obtain a tangential view in an analyzable projection. Twelve of 232 screws in the distal plate-hole row had an overlength not suspicious in the standard fluoroscopic images (postero-anterior and true lateral) and were exchanged intraoperatively.
4.2. Intraoperative Three-Dimensional Fluoroscopy
The additional procedure time for the intraoperative 3D-fluoroscopic scan was 10.02 ± 3.82 minutes. Totally, 3 ± 2.5 fluoroscopic images (54.4 ± 20.9 seconds fluoroscopy time, 39.2 ± 14.5 cGy/cm2 dose area product) were necessary to obtain a tangential view in an analyzable projection. In four patients (8.2%) the 3D-fluoroscopic scan could not be finished due to technical errors. Further, 10 of 232 screws (nine penetrating and one intra-articular screw) in the distal fragments were replaced after the 3D-fluoroscopic scan, not identified as suspicious in the three previous 2D-fluoroscopic control views (in postero-anterior, true lateral and tangential projections).
4.3. Most Dangerous Screw Position for Misplacement
In 10 cases (45.5% of all screw misplacements), the screws in the most radial plate hole position had to be exchanged. In five patients, more than one screw had to be replaced. The overall intraoperative revision rate for all 49 distal radius fractures was 34.7%.
5. Discussion
The anatomy of the distal radius is complex and difficult to visualize intraoperatively (14, 24, 25). The articular surface of the radius is biconcave and tilted in different planes. Further, the commonly used volar plating technique does not allow joint visualization and therefore, the intra-articular fracture reduction can be controlled by fluoroscopy, only (2). Extensive experience and detailed knowledge of the anatomy are necessary to restore the anatomical alignment, without articular steps or gaps, and to ensure an adequate screw length, leading to reliable retention of individual fragments. Standard intraoperative postero-anterior and true lateral fluoroscopic views cannot adequately visualize the correct extra-articular subchondral screw position and length (9, 14, 17, 25). Several additional 2D-fluoroscopic projection images have been described to solve this problem (13, 15-18, 25). To the best of our knowledge, Doenicke et al. (19) were the first in 2006, who described the tangential view as a reliable image modality for the detection of screw overlength (12 penetrating screws in nine patients followed by intraoperative replacement). The postoperative CT scans revealed no residual screw penetration. Modified fluoroscopic techniques were published as “dorsal horizon view” or “dorsal tangential view” with conclusive results (15, 16, 18). In a recent experimental cadaveric study by Haug et al. (11), the validity of such tangential fluoroscopic imaging was corroborated by comparison with CT imaging and direct visual control. Maschke et al. (13) described oblique pronosupination fluoroscopic imaging for enhanced detection of dorsal screw prominence. A screw prominence of at least 2 to 4 mm is required, however, to achieve reproducible results. Several authors reported the use of oblique images to rule out intra-articular screw penetration (10, 12). Alternatively, intraoperative 3D imaging of articular fracture has become an integrated part of several surgical procedures (20, 21, 23, 26). Different studies described an intraoperative screw replacement rate of 10% to 20% in the treatment of distal radial fractures, which, in the authors’ opinion, spared the patients from further revision surgery (20, 21, 27). Multi-slice imaging allows for precise detection of screw misplacements, poor reduction results due to persistent articular steps and gaps. A common limitation of most of these techniques, however, is the lack of standardization, as well as missing proof of clinical relevance in a large patients population provided in this study. Our findings demonstrate that the additional tangential view (Doenicke view) is a helpful 2D-fluoroscopic image projection for the detection of screw-overlength, with penetration of the dorsal cortical surface in the distal radius. The easy and fast acquisition, with neglectible increase of radiation exposure, justifies the application in our routine clinical setting. In contrast, the intraoperative 3D-fluoroscopic scan did not become accepted due to the technical demands, as well as time and cost-intensive procedure, despite the further detection of 10 additional screw misplacements. Important to mention is the fact that no revision was performed to increase the reduction quality after the intraoperative 3D-fluoroscopic control scan, due to persistent steps or gaps. Erroneous interpretations, however, may arise from a limited image quality of the 3D-fluoroscopy. The high intraoperative rate for screw revisions in our study may be attributed to the large number of operations performed by inexperienced surgeons (34 by residents and 15 by senior consultants). In a level 1 trauma center, most distal radius fractures are a typical training operation for residents supervised by the trauma-surgeons on call. The lack of tactile feed-back for the supervised surgeon makes an adequate intraoperative imaging necessary to avoid revision surgery. The study has several limitations:
A direct comparison of both image modalities was not possible, due to the study design that primarily focused on the clinical algorithm, with stepwise exchange of screws after each image acquisition (tangential view and 3D-fluoroscopic scan).
The detected screw misplacements could not be verified by direct visualization after soft tissue dissection or by postoperative computed tomography.
The observed misplacement rate due to overlength screw cannot be directly extrapolated to potential clinical complications, like tendon synovitis and ruptures.
In conclusion, the additional tangential view (Doenicke view) is recommended for the routine detection of screw overlength, penetrating the posterior cortical surface of the distal radius, which may lead to postoperative tendon irritations and ruptures. The use of the intraoperative 3D-fluoroscopy is subject for selected cases only, due to the limitations discussed above.
Footnotes
Authors’ Contributions:All authors have participated in the design, coordination and execution of the study and helped to draft the manuscript. All authors read and approved the final manuscript.
References
- 1.Simic PM, Weiland AJ. Fractures of the distal aspect of the radius: changes in treatment over the past two decades. Instr Course Lect. 2003;52:185–95. [PubMed] [Google Scholar]
- 2.Orbay J. Volar plate fixation of distal radius fractures. Hand Clin. 2005;21(3):347–54. doi: 10.1016/j.hcl.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 3.Lichtman DM, Bindra RR, Boyer MI, Putnam MD, Ring D, Slutsky DJ, et al. Treatment of distal radius fractures. J Am Acad Orthop Surg. 2010;18(3):180–9. doi: 10.5435/00124635-201003000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Drobetz H, Kutscha-Lissberg E. Osteosynthesis of distal radial fractures with a volar locking screw plate system. Int Orthop. 2003;27(1):1–6. doi: 10.1007/s00264-002-0393-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Drobetz H, Bryant AL, Pokorny T, Spitaler R, Leixnering M, Jupiter JB. Volar fixed-angle plating of distal radius extension fractures: influence of plate position on secondary loss of reduction--a biomechanic study in a cadaveric model. J Hand Surg Am. 2006;31(4):615–22. doi: 10.1016/j.jhsa.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 6.Shin EK, Jupiter JB. Current concepts in the management of distal radius fractures. Acta Chir Orthop Traumatol Cech. 2007;74(4):233–46. [PubMed] [Google Scholar]
- 7.Freeland AE, Luber KT. Biomechanics and biology of plate fixation of distal radius fractures. Hand Clin. 2005;21(3):329–39. doi: 10.1016/j.hcl.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 8.Al-Rashid M, Theivendran K, Craigen MA. Delayed ruptures of the extensor tendon secondary to the use of volar locking compression plates for distal radial fractures. J Bone Joint Surg Br. 2006;88(12):1610–2. doi: 10.1302/0301-620X.88B12.17696. [DOI] [PubMed] [Google Scholar]
- 9.Tarallo L, Mugnai R, Zambianchi F, Adani R, Catani F. Volar plate fixation for the treatment of distal radius fractures: analysis of adverse events. J Orthop Trauma. 2013;27(12):740–5. doi: 10.1097/BOT.0b013e3182913fc5. [DOI] [PubMed] [Google Scholar]
- 10.Pace A, Cresswell T. Use of articular wrist views to assess intra-articular screw penetration in surgical fixation of distal radius fractures. J Hand Surg Am. 2010;35(6):1015–8. doi: 10.1016/j.jhsa.2010.03.041. [DOI] [PubMed] [Google Scholar]
- 11.Haug LC, Glodny B, Deml C, Lutz M, Attal R. A new radiological method to detect dorsally penetrating screws when using volar locking plates in distal radial fractures. The dorsal horizon view. Bone Joint J. 2013;95-B(8):1101–5. doi: 10.1302/0301-620X.95B8.31301. [DOI] [PubMed] [Google Scholar]
- 12.Soong M, Got C, Katarincic J, Akelman E. Fluoroscopic evaluation of intra-articular screw placement during locked volar plating of the distal radius: a cadaveric study. J Hand Surg Am. 2008;33(10):1720–3. doi: 10.1016/j.jhsa.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 13.Maschke SD, Evans PJ, Schub D, Drake R, Lawton JN. Radiographic evaluation of dorsal screw penetration after volar fixed-angle plating of the distal radius: a cadaveric study. Hand (N Y). 2007;2(3):144–50. doi: 10.1007/s11552-007-9038-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Park DH, Goldie BS. Volar plating for distal radius fractures--do not trust the image intensifier when judging distal subchondral screw length. Tech Hand Up Extrem Surg. 2012;16(3):169–72. doi: 10.1097/BTH.0b013e31825f7c5a. [DOI] [PubMed] [Google Scholar]
- 15.Thomas AD, Greenberg JA. Use of fluoroscopy in determining screw overshoot in the dorsal distal radius: a cadaveric study. J Hand Surg Am. 2009;34(2):258–61. doi: 10.1016/j.jhsa.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 16.Ozer K, Wolf JM, Watkins B, Hak DJ. Comparison of 4 fluoroscopic views for dorsal cortex screw penetration after volar plating of the distal radius. J Hand Surg Am. 2012;37(5):963–7. doi: 10.1016/j.jhsa.2012.02.026. [DOI] [PubMed] [Google Scholar]
- 17.Lee SK, Bae KW, Choy WS. Use of the radial groove view intra-operatively to prevent damage to the extensor pollicis longus tendon by protruding screws during volar plating of a distal radial fracture. Bone Joint J. 2013;95-B(10):1372–6. doi: 10.1302/0301-620X.95B10.31453. [DOI] [PubMed] [Google Scholar]
- 18.Joseph SJ, Harvey JN. The dorsal horizon view: detecting screw protrusion at the distal radius. J Hand Surg Am. 2011;36(10):1691–3. doi: 10.1016/j.jhsa.2011.07.020. [DOI] [PubMed] [Google Scholar]
- 19.Dönicke T, Petrovitch A, Grubert S, Friedel R, Hofmann. Deutscher Kongress für Orthopädie und Unfallchirurgie 70. Jahrestagung der Deutschen Gesellschaft für Unfallchirurgie. 2006 Available from: http://www.egms.de/static/de/meetings/dgu2006/06dgu0249.shtml.
- 20.Mehling I, Rittstieg P, Mehling AP, Kuchle R, Muller LP, Rommens PM. Intraoperative C-arm CT imaging in angular stable plate osteosynthesis of distal radius fractures. J Hand Surg Eur Vol. 2013;38(7):751–7. doi: 10.1177/1753193413476418. [DOI] [PubMed] [Google Scholar]
- 21.Atesok K, Finkelstein J, Khoury A, Peyser A, Weil Y, Liebergall M, et al. The use of intraoperative three-dimensional imaging (ISO-C-3D) in fixation of intraarticular fractures. Injury. 2007;38(10):1163–9. doi: 10.1016/j.injury.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 22.Carelsen B, Haverlag R, Ubbink DT, Luitse JS, Goslings JC. Does intraoperative fluoroscopic 3D imaging provide extra information for fracture surgery? Arch Orthop Trauma Surg. 2008;128(12):1419–24. doi: 10.1007/s00402-008-0740-5. [DOI] [PubMed] [Google Scholar]
- 23.Carelsen B, van Loon J, Streekstra GJ, Maas M, van Kemenade P, Strackee SD. First experiences with the use of intraoperative 3D-RX for wrist surgery. Minim Invasive Ther Allied Technol. 2011;20(3):160–6. doi: 10.3109/13645706.2010.518807. [DOI] [PubMed] [Google Scholar]
- 24.Clement H, Pichler W, Nelson D, Hausleitner L, Tesch NP, Grechenig W. Morphometric analysis of lister's tubercle and its consequences on volar plate fixation of distal radius fractures. J Hand Surg Am. 2008;33(10):1716–9. doi: 10.1016/j.jhsa.2008.08.012. [DOI] [PubMed] [Google Scholar]
- 25.Tweet ML, Calfee RP, Stern PJ. Rotational fluoroscopy assists in detection of intra-articular screw penetration during volar plating of the distal radius. J Hand Surg Am. 2010;35(4):619–27. doi: 10.1016/j.jhsa.2009.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stubig T, Kendoff D, Citak M, Geerling J, Khalafi A, Krettek C, et al. Comparative study of different intraoperative 3-D image intensifiers in orthopedic trauma care. J Trauma. 2009;66(3):821–30. doi: 10.1097/TA.0b013e31815edf34. [DOI] [PubMed] [Google Scholar]
- 27.Hufner T, Stubig T, Gosling T, Kendoff D, Geerling J, Krettek C. [Cost-benefit analysis of intraoperative 3D imaging]. Unfallchirurg. 2007;110(1):14–21. doi: 10.1007/s00113-006-1202-6. [DOI] [PubMed] [Google Scholar]


