Abstract
Acute respiratory distress syndrome (ARDS) is a devastating disorder characterized by increased alveolar permeability with no effective treatment beyond supportive care. Current mechanisms underlying ARDS focus on alveolar endothelial and epithelial injury caused by products of innate immune cells and platelets. However, the role of adaptive immune cells in ARDS remains largely unknown. Here we report that expansion of antigen-specific αβT helper 17 (αβTH17) cells contribute to ARDS by local secretion of IL-17A, which in turn directly increases alveolar epithelial permeability. Mice with a highly restrictive defect in antigen-specific αβTH17 cells were protected from experimental ARDS induced by a single dose of endotracheal lipopolysaccharide (LPS). Loss of IL-17 receptor C or antibody blockade of IL-17A was similarly protective, further suggesting that IL-17A released by these cells was responsible for this effect. LPS induced a rapid and specific clonal expansion of αβTH17 cells in the lung, as determined by deep sequencing of the hypervariable CD3RβVJ region of the T cell receptor. Our findings could be relevant to ARDS in humans, since we found significant elevation of IL-17A in bronchoalveolar lavage (BAL) fluid from patients with ARDS and recombinant IL-17A directly increased permeability across cultured human alveolar epithelial monolayers. These results reveal a previously unexpected role for adaptive immune responses that increase alveolar permeability in ARDS and suggest that αβTH17 cells and IL-17A could be novel therapeutic targets for this currently untreatable disease.
Keywords: TH17, IL-17, Acute Respiratory Distress Syndrome, TH17 Clonal Expansion
Introduction
Acute respiratory distress syndrome (ARDS), a frequent cause for respiratory failure in patients admitted to intensive care units, is characterized by diffuse alveolar filling with protein-rich fluid as a consequence of increased permeability of the alveolar-capillary barrier(1). ARDS can be a consequence of trauma, hemorrhagic shock or toxic inhalation, but the most common cause is bacterial sepsis(2). The prevailing explanation is that the increase in permeability that underlies this disorder is a consequence of direct injury to the alveolar epithelium and endothelium. It is widely recognized that innate immune cells, principally neutrophils, are rapidly recruited to lung alveoli in response to injury or bacterial products, such as lipopolysaccharide (LPS). These neutrophils contribute to alveolar injury by secreting oxidants and proteases, and by promoting the formation of neutrophil extracellular traps (NETs)(3, 4). However, until now there has been little evidence implicating direct effects of the adaptive immune system in the development of ARDS.
The time course of increased alveolar permeability in response to sepsis or experimental exposure to LPS calls into question the simple explanation of direct injury by neutrophils. For example, neutrophil recruitment peaks within the first few days after a single dose of endotracheal LPS, whereas the peak increase in alveolar permeability does not occur until four to five days later, at a time when lymphocytes are replacing neutrophils as the prominent hematopoietic cell in the airspaces(5). Recent work suggests that regulatory T cells (Tregs) contribute to the resolution phase of ARDS, but it is not clear whether this effect is antigen dependent(6). We hypothesized that antigen-specific adaptive immune cells contribute to the induction of increased permeability in ARDS.
αβ T helper 17 (αβTH17) cells are T helper cells that secrete a distinct subset of T cell cytokines, including IL-17A and F, IL-21 and IL-22(7). IL-17A and F, in particular, are released in the setting of bacterial infections and have specific roles in response to bacterial and fungal pathogens(7). Nearly all cells express members of the IL-17 receptor family; therefore, IL-17, once released, can affect tissue injury by directly modulating the behavior of a variety of tissue cells (8, 9). IL-17 has been shown to have important roles in numerous models of inflammatory diseases, including experimental autoimmune encephalomyelitis, psoriasis, inflammatory arthritis and allergic asthma(10-16). Most of these experimental models are driven by introducing known specific antigens, suggesting that the IL-17-dependent effects are a consequence of clonal expansion of antigen-specific αβTH17 cells. Current understanding of IL-17 mediated pathways in experimental ARDS is much more limited. In models of influenza and LPS induced lung injury, IL-17 was linked to neutrophil recruitment (17, 18). The potential roles of pulmonary antigens driving an IL-17-mediated adaptive immune response or direct effects of IL-17 on alveolar epithelial barrier function that is independent of neutrophil recruitment have not been previously examined. We took advantage of mice we have developed with a specific defect in antigen-dependent αβTh17 cells to address these issues.
Materials and Methods
Animals
Mice were bred and maintained according to approved protocols by the University of California, San Francisco, Institutional Animal Care and Use Committee. Itgb8fl/flxCD11c-cre mice were bred on a C57Bl/6 background has been previously described(19). IL-17 receptor C knock-out (IL-17RC KO) mice were generated as previously described in C57Bl/6 background(20). IL-17A eGFP knock-in reporter mice were obtained from Jackson Laboratory (#018472, JAX®Mice).
Human BAL Studies
Human BAL fluid was collected with informed consent and analyzed in accordance to guidelines and approval by the Office of Research Ethics Committees, Northern Ireland. Details of patient demographics and inclusion criteria for developing the sample repository have been previously published(21).
LPS lung injury studies
Itgb8fl/flxCD11c-cre and littermate control mice were used for the Itgb8fl/flxCD11c-cre LPS-induced ARDS studies. C57Bl/6 mice were used for the IL-17A blocking antibody studies. C57Bl/6 mice were used for controls in IL-17RC KO lung injury studies. Mice were randomly assigned 4-digit ear tag numbers and the operator was blinded to the genotype or treatment received prior to initiation of ARDS. Male and female mice between 8 to 12-weeks of age, weighing 20 to 25 grams, were used for the lung injury studies. Sample size was selected based on previous lung injury studies using similar models. The inclusion/exclusion criteria were based on age, weight, and genotype of the mice. Mice were anesthetized with inhaled isofluorane and placed in a supine position at 60-degree incline. Endotracheal LPS (List Biological Laboratories, Inc. #201) 100 μg dissolved in 100 μl of distilled water was administered via direct endotracheal intubation of the trachea using P-10 polyethylene tubing (Becton Dickinson Co. #427400) attached to a 28 gauge insulin syringe (Becton Dickinson Co. #329461) followed by 150 μl of air to improve distribution. In the IL-17A blocking antibody experiments, IL-17A antibody (eBioscience #16-7173-85) or isotype control IgG1K antibody (eBioscience #16-4714-85) was administered intravenously at a dose of 100 μg per mouse two days after treatment with LPS or H2O. Lung injury was measured by permeability of Evan’s Blue labeled serum albumin as previously described in detail(22). In brief, Evan’s Blue (Sigma-Aldrich Co. #E2129) was injected intravenously at a dose of 25 μg/g via retro-orbital injection 96 hours after endotracheal LPS instillation. Mice were euthanized two hours after Evan’s Blue administration, and serum was collected for total serum Evan’s Blue measurement. The lungs were perfused free of blood with 10 ml of PBS with heparin 10 unit/ml (Sigma-Aldrich Co. #078K1610) under 20 cm H2O of pressure by direct cannulation of the pulmonary artery via right ventriculotomy. Lungs were harvested and Evan’s Blue was extracted by incubation in 1 ml of formamide (Fisher Scientific #BP228-100) at 65°C for 48 hours. Evan’s blue concentration was determined by measurement at 620 nm (Beckman Coulter Spectrophotometer DU 800) and corrected for minor blood contamination by using a formula previously described(23). The Evan’s Blue extravasation is reported as lung divided by serum Evan’s Blue.
Flow cytometry
Whole lungs were isolated and minced with blunt scissors. Minced lung was passed through a 70 μm mesh strainer (BD Falcon #352350) in RPMI (Cellgro Mediatech Inc. #10-040CV). Red cell lysis was performed with red cell lysis buffer (Sigma-Aldrich Co. #R7757). Isolated lung cells were incubated in the presence of ionomycin 1 μM (Sigma-Aldrich Co. #I9657), PMA 50 μM (Sigma-Aldrich Co. #P8139) and monensin 2 uM (eBioscience #00-4505-51) at 37°C for 4 hours. Fc receptor and non-specific binding were blocked with anti-CD16/30 (eBioscience #14061) and 10% rat serum (Sigma-Aldrich Co. #R9759) for 20 minutes at 4°C. Live/dead staining was performed with Aqua Live/Dead stain (Invitrogen #L34957) in PBS for 30 minutes at 4°C. Single cell suspension was stained with anti-CD4 (eBioscience #48-0041-82), anti γδ TCR (eBioscience #12-5711-82), anti-CD44 (eBioscience #12-04441-81), and anti-CD62L (eBioscience #17-0621-81). Cells were fixed and permeabilized with Fix/Perm kit per manufacturer instructions (eBioscience #00-5523-00). Intracellular staining was performed with anti-IL-17 antibody (eBioscience #17-7177-81). Flow cytometry was performed using an LSRII (BD Biosciences) and analyzed using FlowJo (Tree Star Inc.). The isolated cells were gated for live cells from live-dead staining and these live cells were gated for CD4+ and γδ TCR+ cells. The CD4+ and γδ TCR+ were then gated for cells that stained for intracellular IL-17.
Cell count
BAL was performed by cannulating the trachea using a 20-gauge Intramedic Luer Stub Adapter (Becton Dickinson #427564), and lungs were lavaged twice with 0.8 ml of PBS. Cell pellets were collected and resuspended in 1 ml of PBS. Cells were counted using a Bright-Line Hemocytometer (Hausser Scientific). Differential cell count was performed manually on cells harvested by cytospin using Diff/Quick staining kit per manufacturer’s instructions (Andwin Scientific #NC9943455).
IL-17A Cytokine Studies
For lung injury induced by LPS in mice, BAL fluid was collected in ice-cold PBS with Halt Protease Inhibitor Cocktail (Thermo Scientific #78430). Mouse IL-17A cytokine levels were measured using mouse IL-17A Duoset kits according to manufacturer’s protocol (R&D Systems #DY421). Human IL-17A cytokine levels were measured using cytometric bead arrays per manufacturer’s recommendations (R&D Systems Europe).
Epithelial cell culture
Rat type II alveolar epithelial cells were isolated from male Sprague-Dawley rats weighing between 150 to 200 grams as previously described(24, 25). Isolated rat type II epithelial cells were cultured on 96-well 0.4 μm pore size polycarbonate cell culture insert plates with receiver plate (Millipore #PSHT004R1) in DMEM/Ham’s F12 50/50 media with 10% FBS at a density of 1.5 × 106 cells/cm2. Human type II alveolar epithelial cells were isolated from human donor lungs declined for transplantation as previously described(25). Isolated human type II epithelial cells were cultured on 24-well 0.4 μm pore size transwell plates (Corning #3495) in DMEM/Ham’s F12 50/50 media with 10% FBS at density of 1 × 106 cells/ cm2. Cells were cultured for 5 days until confluent monolayer could maintain an air-liquid interface.
Epithelial barrier injury
Serum-starved cultured rat type II alveolar epithelial monolayers were stimulated with recombinant rat IL-17A 100 ng/mL (Prospec #CYT-542) for 24 hours. Serum starved human type II alveolar epithelial cells were stimulated with recombinant human IL-17A 100 ng/mL (Cell Signaling #8928). Transepithelial electrical resistance (TER) was measured using a STX100 electrode and ohm-meter (World Precision Instruments). Permeability across transwell was measured by diffusion of FITC-dextran 4 kD 1 mg/mL (Sigma #FD4) over 2 hours from top to bottom well. Concentration of FITC-dextran was measured using top-plate counter with excitation of 488 nm and emission was detected at 520 nm (Tecan GENios Pro).
Survival studies
IL-17RC KO and C57Bl6 wild type mice were treated with 100 μl of endotracheal H2O or 125 μg of LPS in the same volume. Mice were between 8 to 12 weeks old weighing between 20 to 25 grams. Mouse weights are reported as percentage weight change based on baseline body weight determined prior to treatment.
High-throughput T-cell receptor deep sequencing
CDR3β regions were amplified and sequenced by Adaptive Biotechnologies Corporation (Seattle, WA) using the ImmunoSEQ™ assay. In brief, a multiplex PCR system was used to amplify CDR3β sequences from DNA samples. The ImmunoSEQ™ assay can amplify all 35 V segments, both D genes and the 14 functional J segments. This approach generates an 87 base-pair fragment capable of identifying the VDJ region spanning each unique CDR3β(26). Amplicons were sequenced using the Illumina HiSeq™ platform. Using a baseline developed from a suite of synthetic templates, primer concentrations and computational corrections were used to correct for the primer bias common to multiplex PCR reactions. Raw sequence data was filtered based on the TCRβ V, D and J gene definitions provided by the IMGT database (www.imgt.org) and binned using a modified nearest-neighbor algorithm to closely merge related sequences and remove both PCR and sequencing errors. Data was analyzed using the ImmunoSEQ™ analyzer tool.
Statistical analysis
Experimental ARDS studies
Lung permeability, lung cytokine and BAL cell count studies are reported as mean ± standard error of the mean (SEM). One-way ANOVA was applied to compare three or more groups and post-hoc Tukey-Kramer tests were used to identify specific differences.
Barrier integrity studies
For alveolar epithelial barrier transwell studies, unpaired two-tailed Student’s t-test was applied.
Survival studies
Sample size for survival study was determined by sample size calculations for time to an event to detect a difference in survival of over 30%(27). n = C [(pcqc + peqe)/d2] + 2/d + 2. pc = proportion of control group exhibiting event. Pe = desired proportion of experimental group exhibiting event. qc = 1 − pc and qe = 1 − pe. d = |pc − pe| C = constant of 7.85 was used in our calculations as determined by α and 1 − β for power of 80% and significance level of 5%. Comparison of survival curves were calculated based on Log-rank Mantel-Cox test.
Weight change
The percent weight change relative to initial weight was calculated for each mouse. Mean values ± SEM for each group of mice was plotted against the number of days after endotracheal LPS instillation. One-way ANOVA and Bonferroni multiple comparison test were applied to determine differences between means on each day after endotracheal LPS instillation.
Clonality
The degree of clonal expansion within a sample and a direct measure of sample diversity is calculated as the inverse of normalized H, the Shannon-Weiner index. The Shannon-Weiner index is normalized by dividing H by the log2 of the number of elements being measured (Pielou’s evenness). The inverse of this result is a metric that varies between 0 and 1 where 0 is equal to all sequences being equally abundant and 1 when a single sequence makes up the entire sample.
Top 10 clones and pairwise sharing
Two-tailed Wilcoxon rank sum test was used to compare the sums of the average frequencies for the top 10 clones and fraction of shared sequences in pairwise sharing analysis.
Statistical Software
Statistical analysis was performed using GraphPad Prism 5.0, GraphPad Software, San Diego California, USA and the R statistical programing language 3.0.2 (10/31/2013).
Results
Itgb8fl/flxCD11c-cre mice are protected from experimental ARDS
IL-17 can be released by a number of immune cells, including γδ T cells and natural killer T (NKT) cells, and there is no specific genetically altered knockout (KO) model in which IL-17 deletion is restricted to antigen-specific αβTh17 cells. However, we previously reported that mice deficient in the integrin-β8-subunit in CD11c-expressing cells (Itgb8fl/flxCD11c-cre) have a remarkably specific defect in αβTH17 cells due to inability to activate TGF-β during antigen presentation by dendritic cells(28, 29). We used these mice as the best available model of αβTH17 deficient mice, since mice lacking IL-17A and/or F and mice lacking IL-17 receptors have defects in responses to IL-17 cytokines from all cellular sources (both innate and adaptive). Itgb8fl/flxCD11c-cre allowed us to determine the specific importance of αβTH17 cells in ARDS. We assessed the peak increase in alveolar permeability in a model of ARDS (determined by extravasation of albumin-binding Evan’s blue dye) four days after endotracheal instillation of LPS into control or Itgb8fl/flxCD11c-cre mice. There was no baseline difference in permeability between Itgb8fl/flxCD11c-cre mice and littermate control mice treated with vehicle (H2O), but Itgb8fl/flxCD11c-cre mice had a significantly reduced increase in Evans blue extravasation after treatment with LPS (figure 1a).
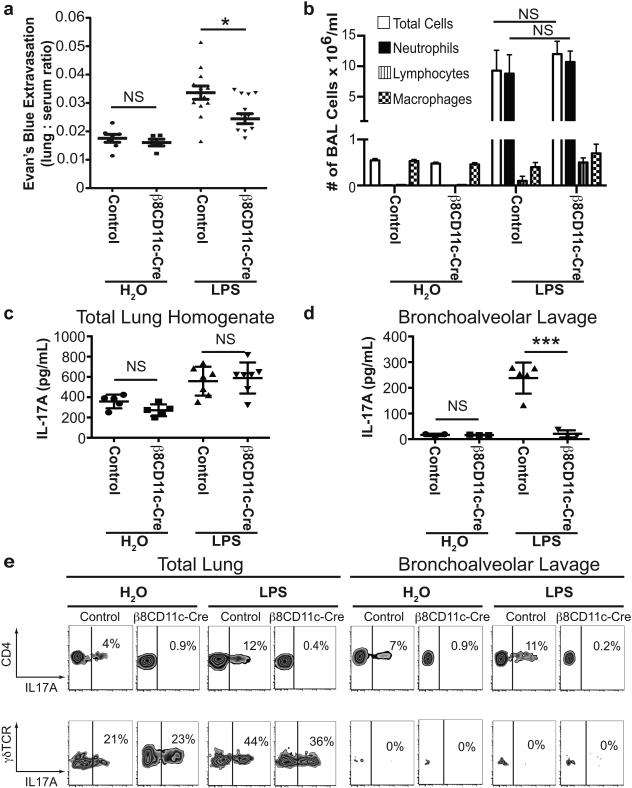
Figure 1. Itgb8fl/flxCD11c-cre mice that fail to differentiate αβTH17 cells are protected from LPS-induced increases in lung permeability.
(a) Endotracheal LPS (100 μg/mouse) or vehicle control (H2O) was administered to Itgb8fl/flxCD11c-cre and littermate control mice. Lung permeability was measured by extravasation of intravascular albumin labeled with Evan’s blue dye into the lung alveolar space and parenchyma. n=12 in Itgb8fl/flxCD11c-cre LPS group, n=13 in littermate control LPS group, n=5 in H2O groups. *p<0.05, no statistical significance (NS) = p>0.05 by one-way ANOVA and Tukey-Kramer test. (b) Total cell count and differential analysis of BAL fluid showed no difference in total cell count and neutrophil count 2 days after administration of H2O or LPS (the peak time for neutrophil influx) between Itgb8fl/flxCD11c-cre and littermate control mice. n=5 per group. NS = p>0.05, by student t-test. (c) IL-17A protein levels measured by ELISA in total lung homogenates 4 days after treatment with LPS or H2O. n=5 per group. (d) IL-17A protein levels in BAL fluid 4 days after treatment with LPS or H2O. n=3-5 per group. ***p<0.001, NS = p>0.05 by student t-test. (e) Flow cytometry analysis of total lung isolates and BAL fluid obtained 4 days after treatment with LPS or H2O. PMA and ionomycin stimulated and monensin treated cells were stained for anti-CD4, anti-γδTCR and anti-IL-17A. Top row are CD4+ gated cells and the bottom row are γδTCR+ gated cells. Data are representative flow cytometry plots with percentage of IL-17A+ cells from 4 per group. Data reported as mean ± SEM for figures a-d.
Previous studies identified an important function of IL-17A in host defense against various pathogens that was due to IL-17A-mediated neutrophil recruitment(30). Since neutrophils contribute to the pathogenesis of ARDS, we wanted to determine if the protective effect observed in Itgb8fl/flxCD11c-cre mice could be secondary to a defect in neutrophil recruitment. The total cell count and neutrophil count in BAL fluid were similar in Itgb8fl/flxCD11c-cre mice and littermate control mice, suggesting that protection from increased lung permeability was not a consequence of reduced neutrophil recruitment (figure 1b).
Both αβTH17 and γδ T cells are important sources of IL-17A in the lung. We previously reported that Itgb8fl/flxCD11c-cre mice have a dramatic defect in pulmonary αβTH17 cells, but no defect in IL-17 producing γδ T cells in a model of allergic airway inflammation(29). Interestingly, there was no difference in IL-17A protein concentration in whole lung lysates from LPS-challenged Itgb8fl/flxCD11c-cre mice (figure 1c), but a dramatic decrease in IL-17A protein concentration in BAL fluid (figures 1d). After treatment with endotracheal LPS, we also found a dramatic defect in whole lung αβTH17 cells in Itgb8fl/flxCD11c-cre mice, but normal numbers of IL-17 producing γδ T cells (figure 1e). αβTH17 cells were easily detected in BAL fluid from LPS-treated control mice, but were absent from BAL fluid of Itgb8fl/flxCD11c-cre mice. IL-17 producing γδ T cells were not detected in BAL fluid (figure 1e). These results suggest tight spatial control of IL-17A production from distinct populations of T cells in the lung and raise the possibility that local alveolar production of IL-17A by αβTH17 cells could play an important role in the induction of lung permeability in response to LPS.
Disruption of IL-17A signaling protects against experimental ARDS
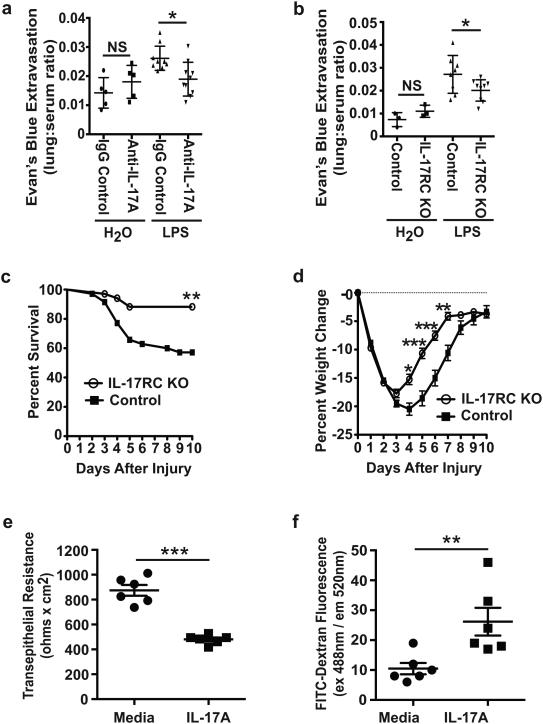
To determine whether the protection seen in mice with a defect in αβTH17 cells was due to reduced levels of locally secreted IL-17A, we evaluated the effects of an IL-17A blocking antibody in wild type C57BL/6 mice in the same model(31). Anti-IL17A blocking antibody was delivered intravenously two days after treatment with LPS to circumvent concerns of blocking IL-17A during the early phase of injury and affecting neutrophil recruitment. IL-17A blocking antibody protected mice from LPS-induced ARDS to a similar degree to that seen for Itgb8fl/flxCD11c-cre mice (figure 2a). To further evaluate the role of IL-17A in ARDS, we examined the effects of LPS in mice deficient in IL-17 receptor C (IL-17RC KO), the component of heterodimeric IL-17 receptors that is most specific for responses to IL-17A and F(32). IL-17RC KO mice were also protected against LPS-induced ARDS (figure 2b). Furthermore, when the LPS dose was increased to a dose that caused significant lethality in control mice, IL-17RC KO mice had a significant improvement in survival (figure 2c). Weight loss was similar during the first three days after initiation of injury, but IL-17RC KO mice had a significant decrease in severity of weight loss from four to seven days (figure 2d).
Figure 2. IL-17A inhibition and loss of IL-17 receptor C protect mice against LPS-induced increased lung permeability.
(a) Anti-IL17A antibody or control IgG was administered intravenously 2 days after endotracheal administration of H2O or LPS (100 μg/mouse) to C57Bl/6 wild type mice. Permeability was measured by leakage of Evan’s blue-labeled intravascular albumin into the lung at 4 days after LPS or H2O administration. Data reported as mean ± SEM, n=10 in LPS groups and n=5 in H2O groups. *p<0.05 by one-way ANOVA and Tukey-Kramer test. (b) LPS or H2O was administered to control or IL-17 receptor C knock-out (IL-17RC KO) mice and permeability was assessed at 4 days, as in figure 2a. Data reported as mean ± SEM, n=9 in LPS groups and n=3 in H2O groups. *p<0.05 by one-way ANOVA and Tukey-Kramer test. (c) Higher dose LPS (125 μg per mouse) was administered endotracheally to control or IL-17 receptor C knockout mice and survival was assessed over the next 10 days. Data reported as percent survival, n=35 in each group. **p<0.01 by log-rank Mantel-Cox test. (d) Body weight was measured daily in all surviving high-dose LPS-treated control and IL-17 receptor C knockout mice for 10 days. Data reported as percent weight change from initial weight. *p<0.05, **p<0.01, ***p<0.001 by one-way ANOVA and Bonferroni multiple comparison test. Confluent rat type II alveolar epithelial monolayers were cultured on collagen-impregnated semi-permeable membrane inserts in the presence of serum-free media with and without recombinant rat IL-17A for 24 hours. (e) Transepithelial electrical resistance and (f) permeability to FITC-dextran were measured. Data reported as mean ± SEM, n=6 per group. **p<0.01,***p<0.001 by student t-test.
Disruption of the alveolar epithelial barrier is a hallmark of ARDS. The direct effect of IL-17A on alveolar epithelial barrier function is unknown. We modeled the alveolar epithelial barrier by culturing primary rat type II epithelial cells in an air-liquid interface to form monolayers on semi-permeable membrane filters. We examined the in vitro effects of IL-17A on the barrier integrity of the alveolar epithelial cell monolayers. Recombinant rat IL-17A disrupted the alveolar epithelial barrier as determined by decreased transepithelial resistance across confluent monolayers and increased permeability to FITC-dextran (figures 2e and 2f).
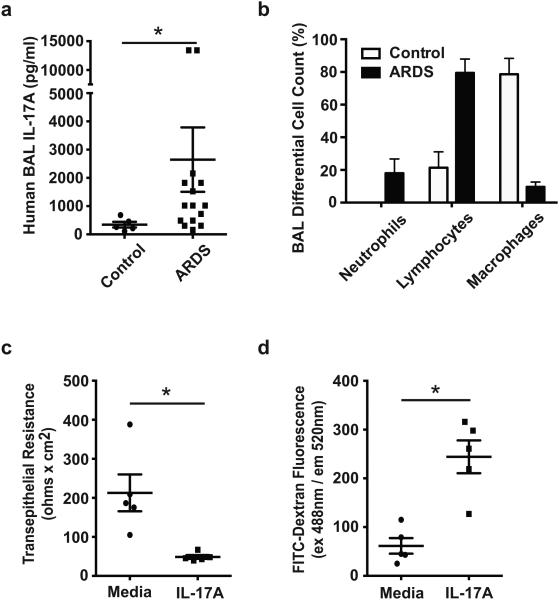
IL-17A levels are elevated in patients with ARDS and IL-17A directly disrupts human alveolar epithelial barrier integrity
In human ARDS patients, very little has been reported related to IL-17A. During the H1N1 influenza outbreak, there were reports of elevated IL-17 levels in BAL fluid, but this was not a direct report of patients diagnosed with ARDS (33). To determine the relevance of our findings to humans, we measured IL-17A levels in BAL fluid samples collected two to five days after initial diagnosis of ARDS. IL-17A levels increased significantly in patients with ARDS (figure 3a). Similar to our findings in experimental ARDS, lymphocytes were readily detected in human BAL fluid samples from patients with ARDS. Human BAL fluid samples from control patients had a predominance of macrophages (figure 3b). Next, we sought to model the human alveolar epithelial barrier. Commercially available immortalized human lung epithelial cells derived from lung carcinoma cells do not provide the best model for alveolar epithelial cell barrier studies. Due to this limitation, we undertook the task of isolating primary human alveolar epithelial cells from cadaveric donor lungs. Primary human alveolar epithelial cells were cultured in an air-liquid interface to form monolayer barriers on semi-permeable membranes. Recombinant human IL-17A decreased transepithelial resistance of primary human alveolar epithelial monolayers and increased permeability to FITC dextran (figure 3c and 3d).
Figure 3. IL-17A levels are significantly elevated in patients with ARDS and IL-17A increases permeability across human alveolar epithelial cell monolayers.
(a) BAL fluid was collected by bronchoscopy in patients diagnosed with ARDS at 2 to 5 days after initial diagnosis, n=15. Control patients were healthy volunteers, n=5. *p<0.05 by student t-test. (b) Cell differential from BAL fluid collected in the same patients diagnosed with ARDS demonstrated readily detectable lymphocytes (74 ± 8.8), neutrophils (18 ± 8.7) and macrophages (9.6 ± 3.0). Control patients had lymphocytes (21 ± 9.7), no detectable neutrophils, and macrophages (79 ± 10). n=5 patients per group. Data for absolute cell counts were not available. (c) Primary isolated human alveolar type II cells from cadaveric lungs were cultured to confluency on semi-permeable membrane inserts. Transepithelial resistance was measured after 24 hours of incubation in the presence of serum-free media with and without recombinant human IL-17A. n=5 per group. *p<0.05 by student t-test. (d) Permeability to FITC-dextran was measured in confluent monolayers of primary cultured human alveolar type II cells after 24 hours incubation with recombinant human IL-17A or vehicle. n=5 per group. *p<0.05 by student t-test. All data reported as mean ± SEM.
Clonal expansion of αβTH17 in experimental ARDS
The contribution of αβTH17 cells to LPS-induced ARDS raised the possibility that this could be an antigen driven process. Because this is a new line of investigation and without a priori knowledge of the pulmonary antigens associated with ARDS, we sought to determine if there is evidence suggesting that specific antigens could contribute to expansion of pathogenic αβTH17 cells in in response to a single dose of endotracheal LPS. We employed high throughput sequencing to characterize the diversity of αβTH17 cells based on the unique VDJ sequences of each T cell receptor (TCR). Quantitative sequencing of the diverse hypervariable region of the beta chain V and J regions of the TCR (CD3RβVJ) allows determination of whether the increase in αβTH17 cells that we found in response to a single dose of endotracheal LPS was due, at least in part, to clonal expansion. We performed TCR sequencing on genomic DNA derived from either αβTH17 cells (identified by knock-in of GFP into the IL-17A locus in CD4+ cells) or non-IL17A expressing CD4+ T cells, isolated from lungs and spleens of mice treated with endotracheal LPS or H2O. An average of 137,940 sequencing reads and 15,636 unique TCR sequences were obtained for each sample. Average V, J gene usage and the distribution of CDR3 lengths were calculated. To characterize the degree of oligoclonality for each sample, we calculated H, the Shannon-Weiner index for each sample based on the frequency of each unique CD3RβVJ sequence(34). The results represent both a diversity metric and a quantification of the degree of clonal expansion within each sample. H is normalized by the log of the number of unique TCR sequences observed by Pielou’s evenness index to produce a metric that varies between 1 for an oligoclonal sample to 0 for a fully polyclonal sample(35). Clonality calculated in this manner is independent of number of T cells sequenced and sampling depth.
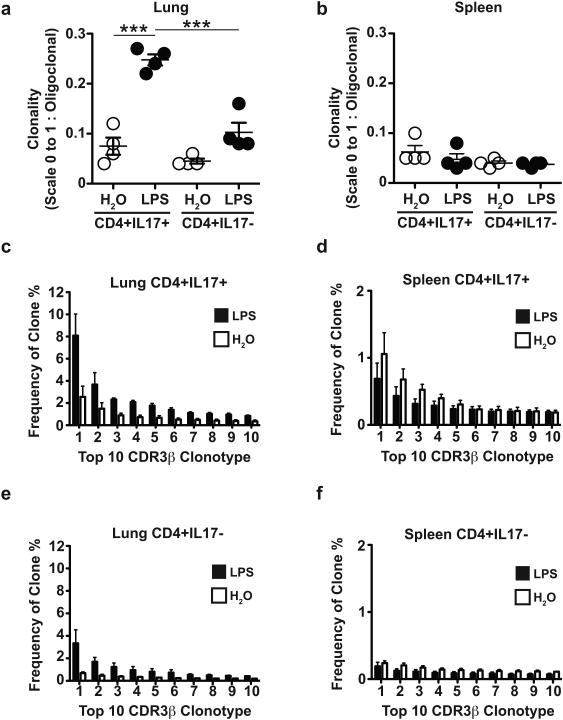
Our results show that clonal expansion was significantly greater in αβTH17 (CD4+IL17+) cells isolated from the lungs of mice treated with LPS. We also sought to determine if clonal expansion was restricted to αβTH17 cells or if this phenomenon would be observed in CD4+ T cells that do not express IL-17A (CD4+IL17−). Endotracheal LPS slightly increased clonal expansion of CD4+IL17− T cells isolated from the lungs, but the increase was significantly less than that seen for αβTH17 cells. There was no detectable clonal expansion in both αβTH17 and CD4+IL17− T cells isolated from the lungs of mice treated with endotracheal H2O (figure 4a).
Figure 4. αβTH17 are clonally expanded in experimental ARDS.
(a) Deep sequencing of the hypervariable CDR3βVJ region of αβTH17 cells (CD4+IL17+) and non-IL-17 producing CD4+ T cells (CD4+IL17−) isolated from lungs 4 days after endotracheal LPS (100μg/mouse) or H2O. To characterize the polyclonal vs. oligoclonal nature of the samples, we calculated the inverse of the normalized Shannon-Weiner index for each sample. This clonality metric varies from 0 to 1, with 1 being a completely monoclonal population. ***p<0.001 by one-way ANOVA and Tukey-Kramer test. (b) Clonality of CD4+IL17+ and CD4+IL17− T cells isolated from the spleens 4 days after endotracheal LPS or H2O. n=4 per group, p>0.05 by one-way ANOVA and Tukey-Kramer test. (c) To further characterize the difference in clonal expansions between the two treatment groups, the frequency of the top 10 individual clones was summed and compared to determine if the difference in clonality between groups was due largely to the expansion of high frequency clones. The 10 highest frequency CD4+IL17+ T cell clones isolated from the lungs of mice 4 days after endotracheal LPS averaged 23% of the total repertoire compared to an average of 7.9% in the H2O treatment group. n=4 per group, **p<0.01 by two-tailed Wilcoxon sum rank test. There were no significant differences in the 10 highest frequency clones isolated from (d) splenic CD4+IL17+ T cells after treatment with LPS (average 1.0%) vs. H2O (average 1.3%); (e) lung CD4+IL17− T cells after treatment with LPS (average 11%) vs. H2O (average 3.1%); (f) splenic CD4+IL17− T cells after treatment with LPS (average 2.9%) vs. H2O (average 3.9%). n=4 per group, p>0.05 by two-tailed Wilcoxon sum rank test. All data reported as mean ± SEM.
In the same mice treated with endotracheal LPS or H2O, we measured the CD3RβVJ sequences of αβTH17 and CD4+IL17− T cells isolated from the spleens. There were no significant differences in clonal expansion of either αβTH17 or CD4+IL17− T cells isolated from the spleens (figure 4b).
To determine the differences in αβTH17 cells in ARDS, we examined a subset of the T cell repertoire from individual samples. A comparison of the fraction of each sample comprised of the 10 most frequent clones isolated from lungs of mice treated with either LPS or H2O revealed a nearly three-fold higher frequency in αβTH17 cells isolated from mice treated with endotracheal LPS (figure 4c). The fraction of the top 10 most frequent clones from CD4+IL17− T cells showed a non-significant increase in mice treated with LPS compared to those treated with H2O (figure 4e). Furthermore, the fraction of each sample comprising the top 10 most frequent clones was notably lower in both αβTH17 and CD4+IL17− T cells obtained from the spleens and was not different between mice treated with LPS or H2O (figures 4d and 4f).
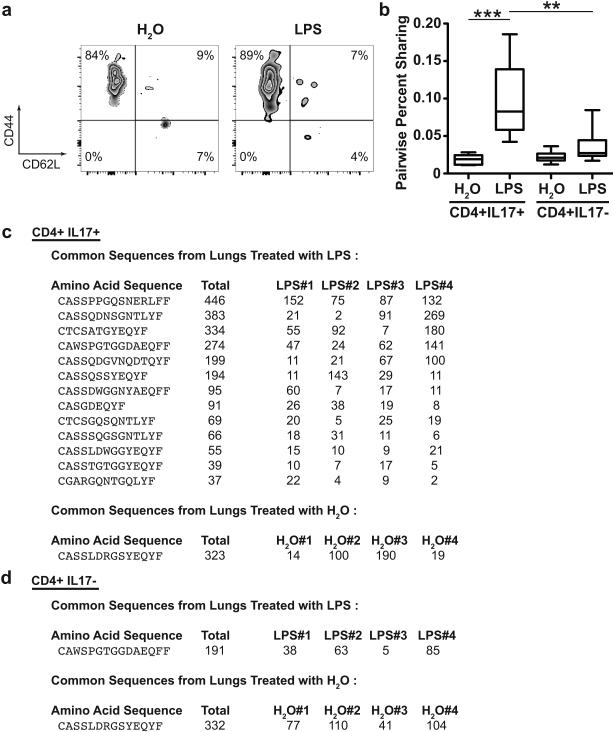
The αβTH17 cells isolated from the lungs of mice treated with LPS or H2O showed a predominantly memory T cell phenotype of CD44highCD62Llow (figure 5a). To assess the likelihood that a common antigen or restricted number of antigens might drive the convergence of the immune repertoire of individual mice after experimental ARDS, the degree of sample similarity amongst different mice was measured by calculating the fraction of pairwise sequences shared between all pairwise combinations of samples. αβTH17 cells isolated from the lungs of mice treated with LPS showed significantly more sharing than αβTH17 cells isolated from mice treated with H2O. Furthermore, pairwise sharing was lower and not significantly different in CD4+IL17− T cells isolated from the lungs of mice treated with LPS or H2O (figure 5b).
Figure 5. Expansion of common sequences of the hypervariable CDR3βVJ regions from predominantly memory αβTH17 cells isolated from the lung in experimental ARDS.
(a) Flow cytometry analysis of CD4+IL17+ T cells isolated from the lung stained for memory T cell markers CD44 and CD62L (memory T cell defined by CD44highCD62Llow). Representative flow cytometry plots from mice treated with LPS or H2O. n=3 per group. (b) Percent pairwise sharing of all CDR3βVJ sequences between different mice in each treatment group was calculated as the number of shared sequences in each sample divided by the total number of sequences for both samples. The TCR sequences among αβTH17 cells (CD4+IL17+) were significantly more shared among lung samples treated with LPS. The mean fraction of shared sequences was 0.097 for CD4+IL17+ T cells from mice treated with LPS compared to 0.018 for CD4+IL17+ T cells from mice treated with H2O, 0.035 for CD4+IL17− T cells from mice treated with LPS, or 0.022 from mice treated with H2O. Data reported as mean ± SEM, n=4 mice per group with 6 unique pairwise comparisons between mice of each group. **p<0.01, ***p<0.001 by Kruskal-Wallis rank sum test. (c) The list of common amino acid sequences from the CDR3βVJ region of CD4+IL17+ T cells isolated from the lungs of mice treated with LPS or H2O. n=4 per group. (d) The list of the common amino acid sequences from the CDR3βVJ region of CD4+IL17− T cells isolated from the lungs of mice treated with LPS or H2O. n=4 per group.
We also evaluated CD3RβVJ sequences shared by all mice in a given treatment group and found 13 such sequences in αβTH17 cells isolated from the lungs of LPS-treated mice but only a single and unique shared sequence in αβTH17 cells from the lungs of H2O treated mice (figure 5c). There were no common sequences in αβTH17 cells isolated from the spleens of mice treated with either LPS or H2O. There was only one common sequence in the CD4+IL17− T cells isolated from the lungs of mice treated with LPS and one common sequence from mice treated with H2O (figure 5d). These results suggest the possibility of clonal expansion of αβTH17 cells in response to common endogenous or exogenous pulmonary antigens.
Discussion
In this study, we found an important contribution of αβTH17 cells to an intermediate phase of ARDS that begins a few days after initial injury. Mice lacking αβTH17 cells, IL-17 receptor C knockout mice and mice treated with antibody blocking IL-17A were all similarly protected from experimental lung injury. IL-17A was readily detectible in the BAL fluid of LPS-treated mice. These experimental findings appear to translate into patients with ARDS where IL-17A was elevated in BAL fluid collected 2-5 days after initial diagnosis of ARDS. We also found that IL-17A directly increased the permeability of human alveolar epithelial cells, suggesting a possible mechanism for the effects of IL-17 in ARDS. This finding extends the role of IL-17A beyond tissue injury caused by neutrophil related pathways. Because αβTH17 cells are known to expand and release IL-17A and other cytokines in response to specific antigens, we sought evidence of clonal expansion. We found a marked increase in oligoclonality and an expansion of shared CD3RβVJ sequences specifically in αβTH17 cells in the lungs (but not the spleens) of LPS-treated mice. Together these results reveal an unexpected contribution of an adaptive immune response involving αβTH17 cells and IL-17A that develops within a few days in response to a single treatment with an activator of innate immunity (LPS).
It is well recognized that αβTH17 cells are important in host response to extracellular pathogens and play a key role in maintaining the integrity of the intestinal mucosa(30, 36). Our data suggest that αβTH17 cells in the alveoli contribute to barrier disruption, perhaps as a consequence of direct effects of IL-17A on alveolar epithelial cells. However, our data do not provide direct proof that the in vivo protection we observed was due to prevention of direct effects on the epithelium. This question would cells, but unfortunately, no such mice have yet been described. In future work, it will also be important to identify the molecular mechanisms by which IL-17A increases alveolar epithelial permeability.
Furthermore, our findings that in lung digests there were large numbers of γδ T cells but that IL-17 expressing cells in the BAL fluid were all αβTH17 cells suggests that there could be spatial differences in the location of IL-17A secreting cells in the lung. The paucity of γδ T cells in the BAL fluid is consistent with the possibility that γδ T cells are immobile around the conducting airways of the lung where they play a key role in innate host-defense functions as previously described (37, 38). An increase in αβTH17 cells in the BAL fluid suggests that αβTH17 cells are recruited to the alveolar space in response to LPS-induced lung injury and the likely source of tissue injurious IL-17A.. The predominance of memory αβTH17 in the lung raises the question of the origin of the αβTH17 cells in lung injury. Our data do not directly prove whether expansion of αβTH17 cells in response to LPS is a result of differentiation of naïve T cells or expansion of pre-existing memory αβTH17 cells. However, the short time frame of our study (four days after initiation of injury) seems more consistent with expansion of pre-existing memory αβTH17 cells. Vital imaging αβTH17 and γδ T cells in experimental lung injury could help us better understand their trafficking patterns in ARDS.
Our study used Itgb8fl/flxCD11c-cre mice to examine the role of αβTH17 cells. We used this strategy instead of CD4-depleted mice because both beneficial and harmful effects of CD4+ T cells have been described in ARDS. For example, CD4+ T regulatory cells have been shown to be important in the resolution phase of ARDS and in mitigating injury to the alveolar-capillary barrier induced by LPS (6). Nakajima et al. found that CD4+ cells could be injurious in experimental ARDS and blockade of CTLA-4 increased IL-17A levels, but this study did not directly test αβTH17 cells (5). Studying Rag−/− mice could have limitations where various CD4+ T cell subsets may have different effects of protection and injury that nullify each other. Our Itgb8fl/flxCD11c-cre mice are the only line of genetically manipulated mice we are aware of that specifically lacks antigen-dependent αβTH17 cells while all other sources of IL-17 remain intact.
Our findings of oligoclonality of sequences in the hypervariable CD3RβVJ region and the presence of a number of sequences shared in αβTH17 cells from all of the mice treated with a single dose of LPS strongly suggest that this clonal expansion is antigen-driven. However, we cannot rule out the possibility that LPS could drive antigen-presenting cells to secrete inflammatory cytokines that stimulate αβTH17 proliferation (39). LPS could also serve as an adjuvant to stimulate αβTH17 response to peptides, such as previously described with myelin oligodendrocyte glycoprotein (MOG) in experimental autoimmune encephalitis(40). MHCII dependent and independent pathways have been previously explored in a mouse Klebsiella Pneumoniae pneumonia model (41). In a MHCII dependent pathway, outer membrane proteins of Klebsiella Pneumoniae were capable of stimulating memory αβTH17 cells (41). In the same study, a smaller percentage of αβTH17 cells were capable of being stimulated by MHCII deficient cells that implied an antigen independent pathway driven by IL-1β could also exist (41). Our finding that the increase in αβTH17 cells in response to LPS was associated with a marked reduction in TCR sequence diversity leads us to favor the possibility that specific antigens, as yet unidentified, drive this expansion process.
This is one of the first studies to our knowledge that suggests pulmonary antigens could drive an injurious adaptive immune response in the devastating lung disorder of ARDS. However, this conclusion must remain speculative until we or others identify specific exogenous or endogenous antigens that drive this response. We hope our study will spawn future research to identify one or more relevant antigens that has the potential to shed new light on the link between innate and adaptive immunity in driving the pathogenic contributions of αβTH17 cells to ARDS, and could also be relevant to other IL-17 dependent pathologies.
Acknowledgements
Supplies
IL-17RC KO mice were kindly provided by W. Ouyang (Genentech).
Special Thanks
Julie Yabu for intellectual contribution and editing the manuscript. Roger Chang for isolating cells for deep sequencing.
Footnotes
This work was supported by the US National Institute of Health (NIH) grants R37HL53949 (D.S.), NIH K08HL111208 (J.T.L.), NIH R37HL51856 (M.A.M.), HSC R&D Division, Public Health Agency Northern Ireland (C.M.O. and D.A.M.). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or other funders.
Bibliography
- 1.Ashbaugh DG, Bigelow DB, Petty TL, Levine BE. Acute respiratory distress in adults. Lancet. 1967;2:319–323. [Google Scholar]
- 2.Ware LB, Matthay MA. The acute respiratory distress syndrome. The New England journal of medicine. 2000;342:1334–1349. doi: 10.1056/NEJM200005043421806. [DOI] [PubMed] [Google Scholar]
- 3.Abraham E. Neutrophils and acute lung injury. Critical care medicine. 2003;31:S195–199. doi: 10.1097/01.CCM.0000057843.47705.E8. [DOI] [PubMed] [Google Scholar]
- 4.Caudrillier A, Kessenbrock K, Gilliss BM, Nguyen JX, Marques MB, Monestier M, Toy P, Werb Z, Looney MR. Platelets induce neutrophil extracellular traps in transfusion-related acute lung injury. The Journal of clinical investigation. 2012;122:2661–2671. doi: 10.1172/JCI61303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nakajima T, Suarez CJ, Lin KW, Jen KY, Schnitzer JE, Makani SS, Parker N, Perkins DL, Finn PW. T cell pathways involving CTLA4 contribute to a model of acute lung injury. Journal of immunology. 2010;184:5835–5841. doi: 10.4049/jimmunol.0903238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.D'Alessio FR, Tsushima K, Aggarwal NR, West EE, Willett MH, Britos MF, Pipeling MR, Brower RG, Tuder RM, McDyer JF, King LS. CD4+CD25+Foxp3+ Tregs resolve experimental lung injury in mice and are present in humans with acute lung injury. The Journal of clinical investigation. 2009;119:2898–2913. doi: 10.1172/JCI36498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gaffen SL. Structure and signalling in the IL-17 receptor family. Nature reviews. Immunology. 2009;9:556–567. doi: 10.1038/nri2586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yao Z, Painter SL, Fanslow WC, Ulrich D, Macduff BM, Spriggs MK, Armitage RJ. Human IL-17: a novel cytokine derived from T cells. Journal of immunology. 1995;155:5483–5486. [PubMed] [Google Scholar]
- 9.Haudenschild D, Moseley T, Rose L, Reddi AH. Soluble and transmembrane isoforms of novel interleukin-17 receptor-like protein by RNA splicing and expression in prostate cancer. The Journal of biological chemistry. 2002;277:4309–4316. doi: 10.1074/jbc.M109372200. [DOI] [PubMed] [Google Scholar]
- 10.Cua DJ, Sherlock J, Chen Y, Murphy CA, Joyce B, Seymour B, Lucian L, To W, Kwan S, Churakova T, Zurawski S, Wiekowski M, Lira SA, Gorman D, Kastelein RA, Sedgwick JD. Interleukin-23 rather than interleukin-12 is the critical cytokine for autoimmune inflammation of the brain. Nature. 2003;421:744–748. doi: 10.1038/nature01355. [DOI] [PubMed] [Google Scholar]
- 11.Park H, Li Z, Yang XO, Chang SH, Nurieva R, Wang YH, Wang Y, Hood L, Zhu Z, Tian Q, Dong C. A distinct lineage of CD4 T cells regulates tissue inflammation by producing interleukin 17. Nature immunology. 2005;6:1133–1141. doi: 10.1038/ni1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nakae S, Nambu A, Sudo K, Iwakura Y. Suppression of immune induction of collagen-induced arthritis in IL-17-deficient mice. Journal of immunology. 2003;171:6173–6177. doi: 10.4049/jimmunol.171.11.6173. [DOI] [PubMed] [Google Scholar]
- 13.Korn T, Bettelli E, Oukka M, Kuchroo VK. IL-17 and Th17 Cells. Annual review of immunology. 2009;27:485–517. doi: 10.1146/annurev.immunol.021908.132710. [DOI] [PubMed] [Google Scholar]
- 14.Zaba LC, Cardinale I, Gilleaudeau P, Sullivan-Whalen M, Suarez-Farinas M, Fuentes-Duculan J, Novitskaya I, Khatcherian A, Bluth MJ, Lowes MA, Krueger JG. Amelioration of epidermal hyperplasia by TNF inhibition is associated with reduced Th17 responses. The Journal of experimental medicine. 2007;204:3183–3194. doi: 10.1084/jem.20071094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Molet S, Hamid Q, Davoine F, Nutku E, Taha R, Page N, Olivenstein R, Elias J, Chakir J. IL-17 is increased in asthmatic airways and induces human bronchial fibroblasts to produce cytokines. The Journal of allergy and clinical immunology. 2001;108:430–438. doi: 10.1067/mai.2001.117929. [DOI] [PubMed] [Google Scholar]
- 16.Alcorn JF, Crowe CR, Kolls JK. TH17 cells in asthma and COPD. Annual review of physiology. 2010;72:495–516. doi: 10.1146/annurev-physiol-021909-135926. [DOI] [PubMed] [Google Scholar]
- 17.Crowe CR, Chen K, Pociask DA, Alcorn JF, Krivich C, Enelow RI, Ross TM, Witztum JL, Kolls JK. Critical role of IL-17RA in immunopathology of influenza infection. Journal of immunology. 2009;183:5301–5310. doi: 10.4049/jimmunol.0900995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ferretti S, Bonneau O, Dubois GR, Jones CE, Trifilieff A. IL-17, produced by lymphocytes and neutrophils, is necessary for lipopolysaccharide-induced airway neutrophilia: IL-15 as a possible trigger. Journal of immunology. 2003;170:2106–2112. doi: 10.4049/jimmunol.170.4.2106. [DOI] [PubMed] [Google Scholar]
- 19.Travis MA, Reizis B, Melton AC, Masteller E, Tang Q, Proctor JM, Wang Y, Bernstein X, Huang X, Reichardt LF, Bluestone JA, Sheppard D. Loss of integrin alpha(v)beta8 on dendritic cells causes autoimmunity and colitis in mice. Nature. 2007;449:361–365. doi: 10.1038/nature06110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zheng Y, Valdez PA, Danilenko DM, Hu Y, Sa SM, Gong Q, Abbas AR, Modrusan Z, Ghilardi N, de Sauvage FJ, Ouyang W. Interleukin-22 mediates early host defense against attaching and effacing bacterial pathogens. Nature medicine. 2008;14:282–289. doi: 10.1038/nm1720. [DOI] [PubMed] [Google Scholar]
- 21.Craig TR, Duffy MJ, Shyamsundar M, McDowell C, O'Kane CM, Elborn JS, McAuley DF. A randomized clinical trial of hydroxymethylglutaryl- coenzyme a reductase inhibition for acute lung injury (The HARP Study) American journal of respiratory and critical care medicine. 2011;183:620–626. doi: 10.1164/rccm.201003-0423OC. [DOI] [PubMed] [Google Scholar]
- 22.Patterson CE, Rhoades RA, Garcia JG. Evans blue dye as a marker of albumin clearance in cultured endothelial monolayer and isolated lung. Journal of applied physiology. 1992;72:865–873. doi: 10.1152/jappl.1992.72.3.865. [DOI] [PubMed] [Google Scholar]
- 23.Moitra J, Sammani S, Garcia JG. Re-evaluation of Evans Blue dye as a marker of albumin clearance in murine models of acute lung injury. Translational research : the journal of laboratory and clinical medicine. 2007;150:253–265. doi: 10.1016/j.trsl.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 24.Johnson MD, Widdicombe JH, Allen L, Barbry P, Dobbs LG. Alveolar epithelial type I cells contain transport proteins and transport sodium, supporting an active role for type I cells in regulation of lung liquid homeostasis. Proceedings of the National Academy of Sciences of the United States of America. 2002;99:1966–1971. doi: 10.1073/pnas.042689399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee JW, Fang X, Dolganov G, Fremont RD, Bastarache JA, Ware LB, Matthay MA. Acute lung injury edema fluid decreases net fluid transport across human alveolar epithelial type II cells. The Journal of biological chemistry. 2007;282:24109–24119. doi: 10.1074/jbc.M700821200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Robins HS, Campregher PV, Srivastava SK, Wacher A, Turtle CJ, Kahsai O, Riddell SR, Warren EH, Carlson CS. Comprehensive assessment of T-cell receptor beta-chain diversity in alphabeta T cells. Blood. 2009;114:4099–4107. doi: 10.1182/blood-2009-04-217604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guidelines for the Care and Use of Mammals in Neuroscience and Behavioral Research. The National Academies Press; 2003. [PubMed] [Google Scholar]
- 28.Melton AC, Bailey-Bucktrout SL, Travis MA, Fife BT, Bluestone JA, Sheppard D. Expression of alphavbeta8 integrin on dendritic cells regulates Th17 cell development and experimental autoimmune encephalomyelitis in mice. The Journal of clinical investigation. 2010;120:4436–4444. doi: 10.1172/JCI43786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kudo M, Melton AC, Chen C, Engler MB, Huang KE, Ren X, Wang Y, Bernstein X, Li JT, Atabai K, Huang X, Sheppard D. IL-17A produced by alphabeta T cells drives airway hyper-responsiveness in mice and enhances mouse and human airway smooth muscle contraction. Nature medicine. 2012;18:547–554. doi: 10.1038/nm.2684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ye P, Garvey PB, Zhang P, Nelson S, Bagby G, Summer WR, Schwarzenberger P, Shellito JE, Kolls JK. Interleukin-17 and lung host defense against Klebsiella pneumoniae infection. American journal of respiratory cell and molecular biology. 2001;25:335–340. doi: 10.1165/ajrcmb.25.3.4424. [DOI] [PubMed] [Google Scholar]
- 31.Hou W, Kang HS, Kim BS. Th17 cells enhance viral persistence and inhibit T cell cytotoxicity in a model of chronic virus infection. The Journal of experimental medicine. 2009;206:313–328. doi: 10.1084/jem.20082030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hu Y, Ota N, Peng I, Refino CJ, Danilenko DM, Caplazi P, Ouyang W. IL-17RC is required for IL-17A- and IL-17F-dependent signaling and the pathogenesis of experimental autoimmune encephalomyelitis. Journal of immunology. 2010;184:4307–4316. doi: 10.4049/jimmunol.0903614. [DOI] [PubMed] [Google Scholar]
- 33.Li C, Yang P, Sun Y, Li T, Wang C, Wang Z, Zou Z, Yan Y, Wang W, Wang C, Chen Z, Xing L, Tang C, Ju X, Guo F, Deng J, Zhao Y, Yang P, Tang J, Wang H, Zhao Z, Yin Z, Cao B, Wang X, Jiang C. IL-17 response mediates acute lung injury induced by the 2009 pandemic influenza A (H1N1) virus. Cell research. 2012;22:528–538. doi: 10.1038/cr.2011.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shannon CE, Weaver W. The mathematical theory of communication. University of Illinois Press; Urbana: 1949. [Google Scholar]
- 35.Pielou EC. An introduction to mathematical ecology. Wiley-Interscience; New York: 1969. [Google Scholar]
- 36.Ivanov, Atarashi K, Manel N, Brodie EL, Shima T, Karaoz U, Wei D, Goldfarb KC, Santee CA, Lynch SV, Tanoue T, Imaoka A, Itoh K, Takeda K, Umesaki Y, Honda K, Littman DR. Induction of intestinal Th17 cells by segmented filamentous bacteria. Cell. 2009;139:485–498. doi: 10.1016/j.cell.2009.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.King DP, Hyde DM, Jackson KA, Novosad DM, Ellis TN, Putney L, Stovall MY, Van Winkle LS, Beaman BL, Ferrick DA. Cutting edge: protective response to pulmonary injury requires gamma delta T lymphocytes. Journal of immunology. 1999;162:5033–5036. [PubMed] [Google Scholar]
- 38.Moore TA, Moore BB, Newstead MW, Standiford TJ. Gamma delta-T cells are critical for survival and early proinflammatory cytokine gene expression during murine Klebsiella pneumonia. Journal of immunology. 2000;165:2643–2650. doi: 10.4049/jimmunol.165.5.2643. [DOI] [PubMed] [Google Scholar]
- 39.Veldhoen M, Hocking RJ, Atkins CJ, Locksley RM, Stockinger B. TGFbeta in the context of an inflammatory cytokine milieu supports de novo differentiation of IL-17-producing T cells. Immunity. 2006;24:179–189. doi: 10.1016/j.immuni.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 40.Bettelli E, Carrier Y, Gao W, Korn T, Strom TB, Oukka M, Weiner HL, Kuchroo VK. Reciprocal developmental pathways for the generation of pathogenic effector TH17 and regulatory T cells. Nature. 2006;441:235–238. doi: 10.1038/nature04753. [DOI] [PubMed] [Google Scholar]
- 41.Chen K, McAleer JP, Lin Y, Paterson DL, Zheng M, Alcorn JF, Weaver CT, Kolls JK. Th17 cells mediate clade-specific, serotype-independent mucosal immunity. Immunity. 2011;35:997–1009. doi: 10.1016/j.immuni.2011.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]