Abstract
Objectives
By summarizing the value adults place on child health and functional status, this study provides a new quantitative tool that enhances our understanding of the benefits of new health technologies and illustrates the potential contributions of existing datasets for comparative effectiveness research in pediatrics.
Methods
Respondents, ages 18 and older, were recruited from a nationally representative panel between August 2012 and February 2013 to complete an online survey. The survey included a series of paired comparisons that asked respondents to choose between child health and functional status outcomes, which were described using the National Survey of Children with Special Health Care Needs, a 14-item descriptive system of child health outcomes. Using respondent choices regarding an unnamed 7- or 10-year-old child, generalized linear model analyses estimated the value of child health and functional status on a quality-adjusted life year scale.
Results
Across the domains of health and functional status, repeated or chronic physical pain, feeling anxious or depressed, and behavioral problems (such as acting out, fighting, bullying, or arguing) were most valuable, as indicated by adult respondents’ preference of other health problems to avoid outcomes along these domains.
Discussion
These findings may inform comparative effectiveness research, health technology assessments, clinical practice guidelines, and public resource allocation decisions by enhancing understanding of the value adults place on health and functional status of children. Improved measurement of public priorities can promote national child health by drawing attention to what adults value most and complementing conventional measures of public health surveillance.
Keywords: QALY, discrete choice experiments, patient-reported outcomes, NS-CSHCN
Introduction
A quality-adjusted life year (QALY) is an idealized year of life with no health problems and serves as a common preference-based metric in comparative effectiveness research (CER), health technology assessment, and the allocation of communal resources.1 Health problems for a given duration may be summarized by their equivalence in lost QALYs using a variety of methods. Although standard gamble (SG) and time-tradeoff (TTO) responses were commonly used in the past,1 these methods have serious limitations, including cognitive difficulty, scaling biases, and practical considerations.2–5 A recent alternative that addresses these limitations and facilitates the measurement across a much wider domain of problems is to use preference questions on a health valuation survey, such as paired comparisons. For example, the survey might ask a participant, “Which do you prefer: a year in mild pain or a 6-month loss in lifespan with no health problems?” Responses to such questions help us understand the value placed on a year of pain without referencing money, which may be a less reliable and ethical metric. If, for example, half of the respondents prefer the six-month loss in lifespan, this empirical result (i.e., median respondent) suggests that a year in mild pain is worth six quality-adjusted months (i.e., 0.5 QALYs). This study examines the value adults place on child health and functional status and provides a new quantitative tool that enhances our understanding of the benefits of new health technologies. Specifically, this tool applies preference weights to existing data on child health outcomes, such as the National Survey of Children with Special Health Care Needs (NS-CSHCN), summarizing these outcomes to better inform CER in pediatrics.
Faced with a wealth of evidence on child health outcomes, translation and summary of such measures into values that can be used for analysis in medical decision-making (e.g., Markov models) requires tools. Multiple studies have examined the value adults place on child health;6–10 however, few studies have targeted outcomes measured by a child-specific health questionnaire or attempted to summarize value on a QALY scale. Valuation on a QALY scale requires including a description of lifespan or risk of death as an attribute in the alternatives, which can be difficult. An Australian study assessed adult preferences for health scenarios as described by the Child Health Utility 9D (CHU9D), but did not include a lifespan attribute so the study does not report QALYs.11 This limits its value for formal decision analyses. More recently, a United Kingdom study assessed QALY values for the CHU9D by eliciting adult preferences on adult outcomes (not child outcomes).12
To date, only two health valuation studies both 1) utilize a child-specific health-related quality of life (HRQoL) instrument and 2) translate instrument responses to the QALY scale. Both studies valued the Pediatric Asthma Health Outcome Measure (PAHOM) using an SG technique with samples of adults from Seattle, Washington (N=94) and Birmingham, Alabama (N=261).13,14 Furthermore, the Health Utilities Index Mark-2 represents a noteworthy general health instrument marketed largely for adults, yet originally developed for adolescents using preferences from parents in the general population.15,16
Our expanding technology to systematically collect real-time data can potentially advance our understanding of children’s health-related experiences for CER and public health surveillance. Formally weighing evidence on child health outcomes in decision analyses informs clinical guidelines, resource allocations, and policy decisions; yet, only the PAHOM studies summarized child outcomes on a QALY scale. The passing of the 2010 US Patient Protection and Affordable Care Act and the formation of the Patient-Centered Outcomes Research Institute have strengthened the importance of HRQoL as a patient-centered outcome.17,18 Still, tools are needed to summarize quantitatively the evidence in a manner that accounts for the priorities of stakeholders.
Due to the paucity of child health valuation studies in the literature, many comparative studies have used adult measures of HRQOL—the Health Utilities Index (HUI)19 and the EQ-5D9—and applied the same values to both child health outcomes and adult outcomes, as if their experiences were interchangeable. We know from other literature, however,10 that adults often express preferences about health care differently for children than for adults, especially when resources may be limited. In this study, we take the perspective of US adults and examine the values they place on child health outcomes; however, future studies may focus on the values of children, parents, caregivers, or other stakeholder populations.
The purpose of this study is to be the first to assess the value adults place on child health and functional status as described by NS-CSHCN. The NS-CSHCN items measure the health and functional status of US children with special health care needs and gathers critical information on access to quality health care, care coordination of services, access to a medical home, transition services for youth, and the impact of chronic condition(s) on the child’s family.20,21 A multitude of studies have examined NS-CSHCN to assess: a) the roles of medical homes;22–25 b) medical transitioning to adult services health care;26–30 c) impact on the family;28,31–37 and d) health care services and disparities.24,34,36,38–42 Moreover, the NS-CSHCN is a tool to monitor service systems for these children and their families in order to comply with Healthy People 2000 and 2010.23 By summarizing the child health and functional status items in the NS-CSHCN on a QALY scale, this study provides a new tool that extends its use for comparative studies and public health surveillance.
Methods
Participants
To inform medical decision-making and health policy, CER requires measurement and valuation.43 Measurement typically involves surveys of health outcomes completed by patients (e.g., children) or their proxies (e.g., parents, caregivers). The currently available NS-CSHCN data are one source of such measurement. Valuation requires surveys of preferences from the perspective of decision makers (e.g., general population). For this valuation study, we surveyed adults (instead of children) ages 18 years or older who resided in the US because adults typically make health care decisions for children. We recruited respondents from a pre-existing national panel of US adults, and to promote concordance with the 2010 US Census, we used 18 demographic quotas (all combinations of 2 genders, 3 age groups, 3 race/ethnicity groups). Once filled, the survey admitted no additional respondents belonging to that quota. The survey was administered online between August 7, 2012 and February 5, 2013. The protocol, including its sampling design and survey instrument, was adapted from the PROMIS-29 valuation study (1R01CA160104)44 and approved by the University of South Florida Institutional Review Board (USF IRB #8236).
Survey
After consenting, respondents completed a screener in which they reported their current US state of residence, ZIP code, birthdate, race, and Hispanic ethnicity, educational attainment, and household income. After the screener, respondents proceeded to the survey, which was composed of health, paired comparisons (below), and follow-up components. The health component included the PROMIS-29, a validated measure supported by a National Institutes of Health initiative, as a measure of adult HRQoL.44 The follow-up component asked about the respondent’s experience with parenting, selected childhood health conditions, and provided an open text box for opportunity to leave survey feedback.
Paired comparisons
Due to space constraints, this section summarizes the preference elicitation task. The Appendix includes a more didactic overview of paired comparisons, adjectival statements, and the results of each pair as well as a more comprehensive econometric discussion.
A paired comparison is a choice-based question that asks a respondent about his/her preference between two alternatives (e.g., orange vs. apple). Responses show how choices change with different combinations of alternatives. Each respondent first completed three example paired comparison questions: “Which do you prefer?” (1: Apple or Orange); (2: Good Health or Poor Health); and (3: Bad Health or Poor Health). The “Bad Health” vs. “Poor Health” question was included to prepare respondents for potentially more challenging descriptions of health and functional status problems later on the survey. Next, respondents received a randomly assigned base scenario and completed a series of paired comparisons building from this base scenario. The base scenario described the age of an unnamed child (7 or 10 years old) and health-problem duration (1 or 2 years). Each respondent completed up to 40-paired comparisons.
Initial pairs asked respondents to choose between a health problem and a loss in lifespan given the assigned base scenario. For example, the paired comparison in Figure 1 has a base scenario for a 10-year-old child. In this task, the respondents must choose between a reduction in child lifespan of 3 years (i.e., loss of 3 QALYs) and an increase in feeling anxious and depressed for 1 year. For these initial pairs, the loss in lifespan occurred 10 years after the problem, which follows common practice in TTO tasks and allows for sufficient range in loss of lifespan.45 Remaining pairs asked respondents to choose between two problems. All health problems were described using statements derived from the NS-CSHCN. To strengthen concordance with the 2010 US Census at the pair-level, all pairs were assigned and sequenced following the 18 demographic quotas.
Figure 1.

Example of a Paired Comparison
Econometric Analysis
Screener responses of those who dropped out, were terminated, and completed the survey were compared using chi-squared tests and shown alongside the US 2010 Census results. Responses to the 147 pairs were stratified by 4 base scenarios. Figure 2 illustrates the relationship between choices and losses in lifespan. The NS-CSHCN has 14 three-level items and captures up to 28 problems (scale shifts). To assess the 28 problems, all 588 pair-specific probabilities (4 base scenarios × 147 pairs) were included in a generalized linear model.2 Furthermore, the model was re-estimated after stratifying the pairs by base-scenario. Significance level was set at 0.05, and 95% bootstrapped confidence intervals were computed for all parameters.
Figure 2.
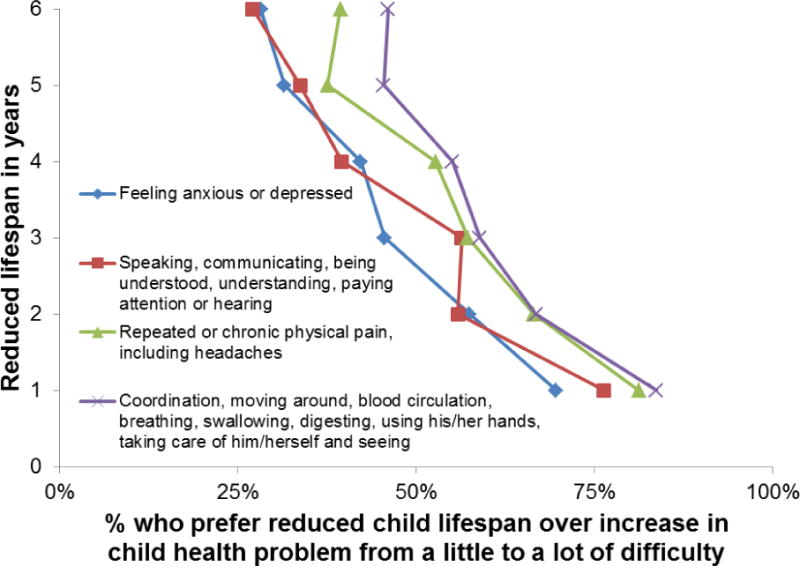
Percentage of adult respondents who preferred reducing the child’s lifespan over the health problem by length of reduction and health problem
Results
Survey Participation
Of the 11,496 respondents recruited for this study, 1075 (9.35%) visited only the consent page, 190 (1.65%) reported non-consent, and 408 (3.55%) dropped out during the screener. Among the 9823 respondents who completed the screener, 2669 (27.17%) belonged to a filled quota, and 1947 (19.82%) failed the screener requirements. As shown in Table 1, among the 5207 respondents who were allowed to enter the survey, 805 (15.46%) dropped out during the survey, and 247 (4.74%) were terminated due to technical requirements (e.g., JavaScript not enabled). The 4155 respondents who completed the survey were younger than those who dropped out, older than those who were terminated, and better educated than those who did not complete the survey (Table 1). Compared to the 2010 US Census, the analytical sample was demographically similar, but better educated, with small differences at the extremes in annual household incomes (less than $15,000 and greater than $150,000). The sample sizes of the 844-paired comparisons ranged from 45 to 69 respondents per comparison. The median survey duration was 25.2 minutes (interquartile range 19.5–34.2 minutes). Most participants reported that the survey was easy to understand (71%) and navigate (87%).
Table 1.
Respondent characteristics by completion and compared to 2010 United States Census*
| Dropout | Terminated | Completed | p-value | US 2010 Census/American Community Survey % | |
|---|---|---|---|---|---|
| N=805 % (#) | N=247 % (#) | N=4155 % (#) | |||
| Age in years | |||||
| 18 to 34 | 23.85 (192) | 31.17 (77) | 27.34 (1136) | 0.017 | 30.58 |
| 35 to 54 | 33.66 (271) | 35.22 (87) | 35.64 (1481) | 36.70 | |
| 55 and older | 42.48 (342) | 33.6 (83) | 37.02 (1538) | 32.72 | |
| Sex | |||||
| Male | 49.32 (397) | 49.8 (123) | 48.45 (2013) | 0.843 | 48.53 |
| Female | 50.68 (408) | 50.2 (124) | 51.55 (2142) | 51.47 | |
| Race | |||||
| White | 80.87 (651) | 76.92 (190) | 81.68 (3394) | 0.337 | 74.66 |
| Black or African American | 13.04 (105) | 17.41 (43) | 11.87 (493) | 11.97 | |
| American Indian or Alaska Native | 0.62 (5) | 0 (0) | 0.55 (23) | 0.87 | |
| Asian | 2.61 (21) | 3.24 (8) | 2.74 (114) | 4.87 | |
| Native Hawaiian or other Pacific Islander | 1.24 (10) | 0.40 (1) | 0.94 (39) | 0.16 | |
| Some other race | – | – | – | 5.39 | |
| Two or more races | 1.61 (13) | 2.02 (5) | 2.21 (92) | 2.06 | |
| Hispanic ethnicity | |||||
| Hispanic or Latino | 12.05 (97) | 13.36 (33) | 11.65 (484) | 0.699 | 14.22 |
| Not Hispanic or Latino | 87.95 (708) | 86.64 (214) | 88.35 (3671) | 85.78 | |
| Educational attainment among age 25 or older | |||||
| Less than high school | 10.68 (86) | 12.55 (31) | 9.24 (384) | 0.001 | 14.42 |
| High school graduate | 26.21 (211) | 23.89 (59) | 20.39 (847) | 28.50 | |
| Some college, no degree | 18.26 (147) | 21.86 (54) | 18.29 (760) | 21.28 | |
| Associate’s degree | 8.2 (66) | 5.67 (14) | 9.92 (412) | 7.61 | |
| Bachelor’s degree | 26.83 (216) | 24.29 (60) | 31.14 (1294) | 17.74 | |
| Graduate or professional degree | 2.73 (22) | 2.43 (6) | 3.44 (143) | 10.44 | |
| Refused/Don’t know | 0.50 (4) | 0 (0) | 0.26 (11) | – | |
| Household income | |||||
| $14,999 or less | 9.57 (77) | 11.74 (29) | 10.35 (430) | 0.129 | 13.46 |
| $15,000 to $24,999 | 15.28 (123) | 14.57 (36) | 14.22 (591) | 11.49 | |
| $25,000 to $34,999 | 13.04 (105) | 14.98 (37) | 12.90 (536) | 10.76 | |
| $35,000 to $49,999 | 18.14 (146) | 14.17 (35) | 18.00 (748) | 14.24 | |
| $50,000 to $74,999 | 11.43 (92) | 14.98 (37) | 14.10 (586) | 18.28 | |
| $75,000 to $99,999 | 10.68 (86) | 4.45 (11) | 8.98 (373) | 11.81 | |
| $100,000 to $149,999 | 6.09 (49) | 8.50 (21) | 7.75 (322) | 11.82 | |
| $150,000 or more | 5.47 (44) | 6.48 (16) | 4.96 (206) | 8.14 | |
| Refused/Don’t know | 10.31 (83) | 10.12 (25) | 8.74 (363) | – |
Age, sex, race, and ethnicity estimates for the US are based on 2010 Census Summary File 1. Educational attainment and household income are based on 2010 American Community Survey 1-Year Estimates. Unlike the US Census, the American Community Survey excluded adults not in the community (e.g., institutionalized) and describes income by the proportion of households, not adults.
Choices
Figure 2 illustrates the percentage of respondents who preferred reducing the child’s lifespan to the health problem, combining responses across the 4 base scenarios. As expected, the percentages form lines that are largely parallel and decreasing (i.e., law of demand). To summarize its demand, the value of a problem is defined by where its line crosses 50% on the x-axis (i.e., median respondent), because this is the point where exactly half of respondents prefer -reduced lifespan over the problem. For example, (Fig. 1), if half of adults choose reduced lifespan by 3 years and half choose a year with increased anxiety and depression, such a result implies that this problem equals a loss of three QALYs.
Respondents’ willingness to sacrifice lifespan (i.e., place a higher value on the problem) increases with the height of the line (y-axis) in Figure 2. The topmost line (in this case, denoted with X) indicates the most valuable problem compared to the lines below it. Interestingly, respondents rated the accumulative problems within physical health (X line) more valuable than repeated or chronic pain (triangle line). Feeling anxious and depressed (diamond line) and communication and learning disorders (square line) were similarly the least valuable of the 4 problems. The results for all paired comparisons are included in the Appendix.
The Value Adults Place on Child Health and Functional Status
The third column of Table 2 describes the value of child health and functional status on a QALY scale, assuming that the base scenario has no effect on the result (i.e., problems for 2 years has twice the value as problems for 1 year, and the value for a 7-year-old child is the same as for a 10-year-old child). Figure 3 shows the sum of the values from Table 2 by their rank from most (top) to least (bottom) valuable. For all items, the value of the shift from “none” to “a little difficulty” (shown in black) was less than the value of the shift from “a little” to “a lot of difficulty” (shown in white); however, “a little difficulty” making friends seems to have larger proportion of the total value.
Table 2.
The Value Adults Place on Child Health and Functional Status
| Base Scenario | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | 10-year-old child with 1-year health problem | 7-year-old child with 1-year health problem | 10-year-old child with 2-year health problem | 7-year-old child with 2-year health problem | ||||||||||||
| Problem | Difficulty | QALY | 95% CI | QALY | 95% CI | QALY | 95% CI | QALY | 95% CI | QALY | 95% CI | |||||
| Breathing | None to little | 0.160 | 0.125 | 0.192 | 0.215 | 0.146 | 0.308 | 0.233 | 0.153 | 0.332 | 0.112 | 0.071 | 0.162 | 0.106 | 0.067 | 0.157 |
| Little to a lot | 0.611 | 0.532 | 0.811 | 0.869 | 0.633 | 1.320 | 0.752 | 0.528 | 1.116 | 0.419 | 0.293 | 0.662 | 0.423 | 0.307 | 0.659 | |
| Swallowing | None to little | 0.191 | 0.159 | 0.226 | 0.219 | 0.155 | 0.295 | 0.284 | 0.203 | 0.379 | 0.119 | 0.083 | 0.168 | 0.169 | 0.120 | 0.232 |
| Little to a lot | 0.831 | 0.780 | 1.103 | 1.051 | 0.842 | 1.534 | 1.116 | 0.876 | 1.663 | 0.523 | 0.404 | 0.831 | 0.665 | 0.536 | 0.983 | |
| Blood circulation | None to little | 0.123 | 0.093 | 0.146 | 0.142t | 0.089 | 0.200 | 0.138 | 0.083 | 0.194 | 0.099 | 0.064 | 0.143 | 0.112 | 0.071 | 0.167 |
| Little to a lot | 0.393 | 0.325 | 0.512 | 0.384 | 0.236 | 0.629 | 0.449 | 0.300 | 0.693 | 0.339 | 0.224 | 0.579 | 0.356 | 0.231 | 0.571 | |
| Chronic pain | None to little | 0.553 | 0.440 | 0.607 | 0.665 | 0.468 | 0.840 | 0.660 | 0.477 | 0.825 | 0.400 | 0.257 | 0.521 | 0.504 | 0.362 | 0.660 |
| Little to a lot | 2.877 | 2.763 | 3.335 | 3.213 | 2.809 | 4.019 | 3.438 | 3.013 | 4.158 | 2.037 | 1.802 | 2.587 | 2.777 | 2.484 | 3.647 | |
| Seeing | None to little | 0.059 | 0.042 | 0.067 | 0.065 | 0.039 | 0.091 | 0.080 | 0.048 | 0.107 | 0.036 | 0.020 | 0.051 | 0.057 | 0.035 | 0.078 |
| Little to a lot | 0.300 | 0.256 | 0.364 | 0.389 | 0.274 | 0.555 | 0.337 | 0.243 | 0.478 | 0.192 | 0.135 | 0.284 | 0.293 | 0.209 | 0.422 | |
| Hearing | None to little | 0.116 | 0.084 | 0.132 | 0.125 | 0.073 | 0.179 | 0.149 | 0.086 | 0.208 | 0.072 | 0.040 | 0.104 | 0.116 | 0.075 | 0.158 |
| Little to a lot | 0.297 | 0.234 | 0.356 | 0.389 | 0.260 | 0.530 | 0.387 | 0.261 | 0.535 | 0.234 | 0.160 | 0.327 | 0.211 | 0.117 | 0.311 | |
| Taking care of self | None to little | 0.111 | 0.086 | 0.129 | 0.147 | 0.100 | 0.203 | 0.130 | 0.080 | 0.176 | 0.083 | r0.054 | 0.117 | 0.086 | 0.057 | 0.119 |
| Little to a lot | 0.476 | 0.417 | 0.605 | 0.689 | 0.501 | 0.998 | 0.566 | 0.417 | 0.805 | 0.399 | 0.294 | 0.625 | 0.300 | 0.218 | 0.432 | |
| Coordinatior | None to little | 0.088 | 0.062 | 0.106 | 0.141 | 0.084 | 0.207 | 0.071 | 0.037 | 0.104 | 0.087 | 0.054 | 0.126 | 0.068 | 0.040 | 0.105 |
| Little to a lot | 0.329 | 0.273 | 0.411 | 0.409 | 0.277 | 0.595 | 0.417 | 0.287 | 0.608 | 0.287 | 0.196 | 0.444 | 0.215 | 0.148 | 0.322 | |
| Using hands | None to little | 0.065 | 0.047 | 0.074 | 0.118 | 0.073 | 0.164 | 0.078 | 0.046 | 0.108 | 0.036 | 0.020 | 0.051 | 0.051 | 0.030 | 0.071 |
| Little to a lot | 0.281 | 0.235 | 0.345 | 0.312 | 0.218 | 0.449 | 0.290 | 0.200 | 0.402 | 0.218 | 0.155 | 0.329 | 0.288 | 0.207 | 0.413 | |
| Learning | None to little | 0.167 | 0.124 | 0.192 | 0.187 | 0.114 | 0.260 | 0.243 | 0.152 | 0.324 | 0.111 | 0.063 | 0.159 | 0.136 | 0.082 | 0.194 |
| Little to a lot | 0.783 | 0.713 | 0.921 | 0.875 | 0.684 | 1.160 | 1.045 | 0.823 | 1.362 | 0.579 | 0.462 | 0.766 | 0.675 | 0.544 | 0.934 | |
| Speaking | None to little | 0.197 | 0.149 | 0.229 | 0.325 | 0.211 | 0.439 | 0.175 | 0.104 | 0.243 | 0.131 | 0.081 | 0.179 | 0.184 | 0.115 | 0.261 |
| Little to a lot | 0.734 | 0.646 | 0.873 | 0.832 | 0.632 | 1.115 | 0.995 | 0.778 | 1.316 | 0.520 | 0.395 | 0.687 | 0.620 | 0.471 | 0.858 | |
| Anxious or depressed | None to little | 0.267 | 0.184 | 0.288 | 0.333 | 0.206 | 0.417 | 0.376 | 0.233 | 0.475 | 0.158 | 0.085 | 0.200 | 0.253 | 0.157 | 0.332 |
| Little to a lot | 1.428 | 1.325 | 1.575 | 1.817 | 1.520 | 2.161 | 1.729 | 1.500 | 2.030 | 1.045 | 0.899 | 1.261 | 1.213 | 1.061 | 1.502 | |
| Behavior problems | None to little | 0.558 | 0.453 | 0.663 | 0.907 | 0.646 | 1.247 | 0.554 | 0.366 | 0.742 | 0.318 | 0.212 | 0.437 | 0.556 | 0.401 | 0.762 |
| Little to a lot | 1.302 | 1.161 | 1.565 | 1.457 | 1.083 | 2.046 | 1.559 | 1.238 | 2.012 | 0.981 | 0.753 | 1.348 | 1.101 | 0.864 | 1.519 | |
| Making friends | None to little | 0.270 | 0.193 | 0.328 | 0.298 | 0.143 | 0.466 | 0.314 | 0.189 | 0.461 | 0.221 | 0.136 | 0.321 | 0.238 | 0.137 | 0.367 |
| Little to a lot | 0.362 | 0.242 | 0.460 | 0.628 | 0.375 | 0.940 | 0.288 | 0.124 | 0.476 | 0.375 | 0.229 | 0.580 | 0.246 | 0.118 | 0.398 | |
Figure 3.
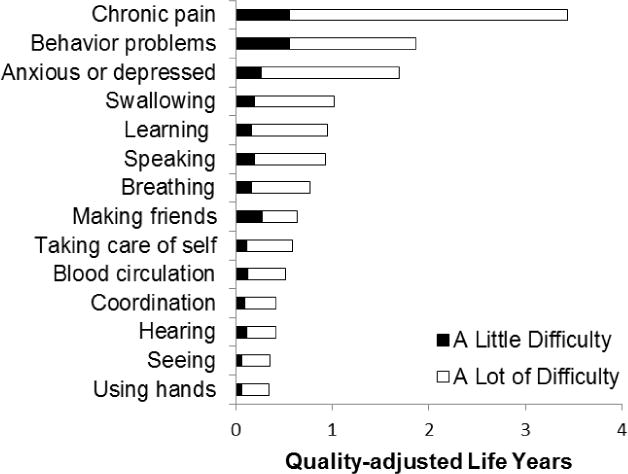
The Value Adults Place on 1 Year of Child Health and Functional Status
As shown by the first bar (Fig. 3), adults value 1 year with “a lot” of chronic pain equal to a loss of 3.43 QALYs (0.553+2.877; Table 2). This implies that when given a choice between a child in “a lot” of chronic pain and one with “a lot” of behavioral problems (1.86 QALYs), 65% of adults prefer the child with “a lot” of behavioral problems (3.43/(1.86+3.43)). Across the 14 problems, chronic pain, behavioral problems, and anxious or depressed are the most valuable, and their rank is the same regardless of base scenario. Hearing, seeing, and using hands were the 3 least valuable problems; however, this result varies by base scenario described later.
Differences in Value by Child Age and Problem Duration
The remaining columns of Table 2 show QALY values for the different base scenarios in this study. Based on 95% significance level, we tested for differences by child age and problem duration. By in large, increasing the health-problem duration from 1 year to 2 years decreases value (up to 69%), regardless of age and possibly attributable to adaptation (i.e., perception that a second year is less valuable than the first). At first glance, the differences by age appear small, but four 1-year problems are significantly more valuable at age 10 than at age 7: “none” to “a little difficulty” with coordination, speaking and behavioral problems and “a little” to “a lot of difficulty” making friends. As for the 2-year problems, we found no significant evidence that problems at age 10 are more valuable that at age 7. On the contrary, 2 years of “a little” to “a lot” of chronic pain is more valuable at age 7 than 10 as was “none” to “a little difficulty” with behavioral problems, suggesting some age-duration interactions in the values adults place on child health and functional status.
Discussion
This study is among the first to value child health for medical decision-making and policy analysis using a set of child-specific HRQoL measures—the NS-CSHCN. To date, most medical decision-making models have had two serious limitations with their health valuation or QALY measures. Previously, health valuation studies estimated QALY values by assessing preferences between health outcomes occurring in adults (not children), and these outcomes were described based on adult-specific instruments, such as the EQ-5D or the HUI. This study expands the small set of child-specific measures available, which now include QALY valuations of the EQ-5D-Y46 and the PAHOM.13,14
This study expands the set of available analysis tools to address the unique and specific needs of the population of children with special health care needs. This is the first study to value the health and functional status domains measured by the NS-CSHCN. Completed by the parents/guardians of children with special needs, the data from the NS-CSHCN provides critical information for decision makers on the health and functioning of special needs children, access to care and services, and impact of the condition on the child’s family. This valuation study, integrating the perspectives of adults from the US general population, enhances the usefulness of the NS-CSHCN data by prioritizing those health problems and functional limitations to inform resource allocations for decision-making. This is important because general HRQoL instruments (e.g., EQ-5D) are known to have many limitations in capturing the full burden of health for specific groups; indeed, this is why hundreds of “disease-specific” HRQoL instruments exist.47,48
Chronic pain, behavior problems (such as acting out, fighting, bullying, or arguing), and mental health (anxiety and depression) were rated as the most valuable domains regardless of the child’s age (7 or 10 years old) or the duration of problem (1 or 2 years). Hearing, seeing, and using hands received the lowest values relative to the other conditions, but varied in their ranking based on child’s age and/or duration of problem.
There are several limitations to this study, particularly concerning questions about the effects of using unnamed children and 10-year time horizons in the valuation of child health. Usually, adult participants are asked to value their own health, not the health of an unnamed child. The results might differ with a familial or named description of the child (e.g. by gender, socio-economic status, or disease), particularly among parents or survivors of childhood diseases. In addition, the preferences may change if the reductions in lifespan occurred later in the child’s life (as an older adult), instead of 10 years later when the child becomes a young adult. Although 10 years is the most common time horizon, a wide range of lifespans have been incorporated in TTO studies.49 The use of 10-year time horizon may be particularly problematic when applied to the valuation of child health. For example, the child in Figure 1 has a tragically short lifespan regardless of the choice (18 and 21 years, respectively), which may confound the preference elicitation task. A longer horizon, however, would likely increase willingness to reduce adult lifespan to prevent child behavioral problems, further inflate the seemingly high estimates (i.e., 7-to-1 ratio). Other health valuation literature raises the issues of unnamed children, “fair innings,” and the 10-year time horizon, but represents an unresolved area for which there is no standard.45,50 The present paper adds to the sparse literature on adult valuations of child health outcomes, but the novelty of this study suggests approaching results with caution. As this literature grows over time, these issues and their effect on valuation may be tested further.
This study used paired comparisons, which is a necessary component of a TTO task; however, the TTO employs an adaptive series of paired comparisons to identify an indifference point.50–53 Unlike TTO-based studies, this preference study is based solely on non-adaptive paired comparisons, which simplifies the task, reduces cognitive burden, expedites response, and reduces the use of heuristics.54 The primary limitation of non-adaptive paired comparisons is that the data are less descriptive (i.e., representing inequalities, not point estimates). This trade-off between adaption and bias will be examined in future work on study design efficiency, well beyond the topic of child health valuation.
The NS-CSHCN clearly covers important child health and functional problems, but does not capture all domains of child health and functional problems or the impact of such problems on the HRQoL of others (e.g., caregivers). It focuses on child functional status and is not a “generic” measure of broader aspects of HRQoL, such as the HUI19 or the EQ-5D.9 This valuation study used data from a national online panel that is similar to, but not perfectly representative of, the US population. For example, there were slightly more educated and non-Hispanic Whites in the panel data.
Conclusions
Understanding the values adults place on child health and functional status is critical for the interpretation of comparative evidence on the effectiveness of new health technologies and public health initiatives in pediatrics. The NS-CSHCN is a valuable resource that is available to parents, researchers, community health providers and anyone interested in maternal and child health. This study enhances the NS-CSHCN by providing a tool that summarizes child health outcomes from the perspective of the general population of US adults.
For the scenarios used in this study, the suffering occurred in childhood (7 or 10 years old), and the losses in lifespan occurred in early adulthood. Keeping that in mind, the prevention of poor child health may be worth the seemingly high loss in adult lifespan from the perspective of US adults, possibly due to perceived long-term and communal consequences or to the fact that adults have had their “fair innings.”45,55 More research is needed on the effects of using unnamed children and 10-year time horizons in the valuation of child health. Furthermore, future analyses will examine differences in health preferences among adults, particularly differences based on experience with children (e.g., parent vs. non-parents), and poor health during their childhood (e.g., survivors of childhood conditions, such as leukemia). Nevertheless, the fundamental results of this study provide a basis for the comparison of perspectives in the promotion of national child health by drawing attention to what adults value most of all.
Supplementary Material
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Drummond M, Brixner D, Gold M, et al. Toward a Consensus on the QALY. Value Health. 2009 Mar-Apr;12:S31–S35. doi: 10.1111/j.1524-4733.2009.00522.x. [DOI] [PubMed] [Google Scholar]
- 2.Craig BM, Busschbach JJ. The episodic random utility model unifies time trade-off and discrete choice approaches in health state valuation. Popul Health Metr. 2009;7:3. doi: 10.1186/1478-7954-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Craig BM, Oppe M. From a different angle: A novel approach to health valuation. Soc Sci Med. 2010 Jan;70(2):169–174. doi: 10.1016/j.socscimed.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Craig BM, Busschbach JJV. Revisiting United States valuation of EQ-5D states. Journal of Health Economics. 2011 Sep;30(5):1057–1063. doi: 10.1016/j.jhealeco.2011.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Craig BM, Busschbach JJV. Toward a More Universal Approach in Health Valuation. Health Economics. 2011 Jul;20(7):864–875. doi: 10.1002/hec.1650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carroll AE, Downs SM. Improving Decision Analyses: Parent Preferences (Utility Values) for Pediatric Health Outcomes. Journal of Pediatrics. 2009 Jul;155(1):21–25. doi: 10.1016/j.jpeds.2009.01.040. [DOI] [PubMed] [Google Scholar]
- 7.Friedman JY, Reed SD, Weinfurt KP, Kahler KH, Walter EB, Schulman KA. Parents’ reported preference scores for childhood atopic dermatitis disease states. BMC pediatrics. 2004 Oct 18;4(1):21. doi: 10.1186/1471-2431-4-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hauber AB, Itzler R, Johnson FR, et al. Healthy-days time equivalents for outcomes of acute rotavirus infections. Vaccine. 2011 Oct;29(45):8086–8093. doi: 10.1016/j.vaccine.2011.08.041. [DOI] [PubMed] [Google Scholar]
- 9.Secnik K, Matza LS, Cottrell S, Edgell E, Tilden D, Mannix S. Health state utilities for childhood attention-deficit/hyperactivity-disorder based on parent preferences in the United Kingdom. Med Decis Mak. 2005 Jan-Feb;25(1):56–70. doi: 10.1177/0272989X04273140. [DOI] [PubMed] [Google Scholar]
- 10.Ungar W. Economic evaluation in child health. Oxford: Oxford University Press; 2010. [Google Scholar]
- 11.Ratcliffe J, Couzner L, Flynn T, et al. Valuing Child Health Utility 9D health states with a young adolescent sample: a feasibility study to compare best-worst scaling discrete-choice experiment, standard gamble and time trade-off methods. Applied health economics and health policy. 2011;9(1):15–27. doi: 10.2165/11536960-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 12.Stevens K. Valuation of the Child Health Utility 9D Index. Pharmacoeconomics. 2012;30(8):729–747. doi: 10.2165/11599120-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 13.Chiou CF, Weaver MR, Bell MA, Lee TA, Krieger JW. Development of the multi-attribute Pediatric Asthma Health Outcome Measure (PAHOM) Int J Qual Health Care. 2005 Feb;17(1):23–30. doi: 10.1093/intqhc/mzh086. [DOI] [PubMed] [Google Scholar]
- 14.Gerald JK, McClure LA, Harrington KF, Moore T, Hernandez-Martinez AC, Gerald LB. Measurement Characteristics of the Pediatric Asthma Health Outcome Measure. J Asthma. 2012 Apr;49(3):260–266. doi: 10.3109/02770903.2012.656863. [DOI] [PubMed] [Google Scholar]
- 15.McCabe CJ, Stevens KJ, Brazier JE. Utility scores for the health utilities index mark 2 – An empirical assessment of alternative mapping functions. Med Care. 2005 Jun;43(6):627–635. doi: 10.1097/01.mlr.0000163666.00471.8e. [DOI] [PubMed] [Google Scholar]
- 16.Torrance GW, Feeny DH, Furlong WJ, Barr RD, Zhang YM, Wang QN. Multiattribute utility function for a comprehensive health status classification system – Health Utilities Index Mark 2. Med Care. 1996 Jul;34(7):702–722. doi: 10.1097/00005650-199607000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Patient Protection and Affordable Care Act, Pub. L. 111–148, 124 Stat. 119, (as amended by the Health and Education Reconciliation Act Pub. L. 111–152, 124 Stat. 1029. Subtitle D–Patient Centered Outcomes Research. In: Office UGP, ed2010.
- 18.Selby JV, Beal AC, Frank L. The Patient-Centered Outcomes Research Institute (PCORI) National Priorities for Research and Initial Research Agenda. JAMA-J Am Med Assoc. 2012 Apr;307(15):1583–1584. doi: 10.1001/jama.2012.500. [DOI] [PubMed] [Google Scholar]
- 19.Petrou S, Kupek E. Estimating Preference-Based Health Utilities Index Mark 3 Utility Scores for Childhood Conditions in England and Scotland. Med Decis Mak. 2009 May;29(3):291–303. doi: 10.1177/0272989X08327398. [DOI] [PubMed] [Google Scholar]
- 20.Craig BM, Pickard AS, Lubetkin EI. Health problems are more common, but less severe when measured using newer EQ-5D versions. J Clin Epidemiol. 2014 Jan;67(1):93–99. doi: 10.1016/j.jclinepi.2013.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.The Child and Adolescent Health Measurement Initiative. Children with Special Health Care Needs (CSHCN) http://www.cahmi.org/pages/Topics.aspx?section=10&topic=65. Accessed Nov. 11, 2013.
- 22.Diedhiou A, Probst JC, Hardin JW, Martin AB, Xirasagar S. Relationship Between Presence of a Reported Medical Home and Emergency Department Use Among Children With Asthma. Medical Care Research and Review. 2010 Aug;67(4):450–475. doi: 10.1177/1077558710367735. [DOI] [PubMed] [Google Scholar]
- 23.Ghandour RM, Perry DF, Kogan MD, Strickland BB. The Medical Home as a Mediator of the Relation Between Mental Health Symptoms and Family Burden Among Children With Special Health Care Needs. Academic Pediatrics. 2011 Mar-Apr;11(2):161–169. doi: 10.1016/j.acap.2010.12.015. [DOI] [PubMed] [Google Scholar]
- 24.Raphael JL, Zhang YQ, Liu H, Tapia CD, Giardino AP. Association of Medical Home Care and Disparities in Emergency Care Utilization Among Children With Special Health Care Needs. Academic Pediatrics. 2009 Jul-Aug;9(4):242–248. doi: 10.1016/j.acap.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 25.Toomey SL, Homer CJ, Finkelstein JA. Comparing Medical Homes for Children with ADHD and Asthma. Academic Pediatrics. 2010 Jan-Feb;10(1):56–63. doi: 10.1016/j.acap.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 26.Lotstein DS, Ghandour R, Cash A, McGuire E, Strickland B, Newacheck P. Planning for Health Care Transitions: Results From the 2005–2006 National Survey of Children With Special Health Care Needs. Pediatrics. 2009 Jan;123(1):E145–E152. doi: 10.1542/peds.2008-1298. [DOI] [PubMed] [Google Scholar]
- 27.Kane DJ, Kasehagen L, Punyko J, Carle AC, Penziner A, Thorson S. What factors are associated with state performance on provision of transition services to CSHCN? Pediatrics. 2009;124(Supplement 4):S375–S383. doi: 10.1542/peds.2009-1255H. [DOI] [PubMed] [Google Scholar]
- 28.Knapp CA, Madden VL, Marcu MI. Factors that Affect Parent Perceptions of Provider-Family Partnership for Children with Special Health Care Needs. Maternal and Child Health Journal. 2010 Sep;14(5):742–750. doi: 10.1007/s10995-009-0503-0. [DOI] [PubMed] [Google Scholar]
- 29.Park MJ, Adams SH, Irwin CE. Health Care Services and the Transition to Young Adulthood: Challenges and Opportunities. Academic Pediatrics. 2011 Mar-Apr;11(2):115–122. doi: 10.1016/j.acap.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 30.Sawicki GS, Whitworth R, Gunn L, Butterfield R, Lukens-Bull K, Wood D. Receipt of Health Care Transition Counseling in the National Survey of Adult Transition and Health. Pediatrics. 2011 Sep;128(3):E521–E529. doi: 10.1542/peds.2010-3017. [DOI] [PubMed] [Google Scholar]
- 31.Bumbalo J, Ustinich L, Ramcharran D, Schwalberg R. Economic impact on families caring for children with special health care needs in New Hampshire: The effect of socioeconomic and health-related factors. Maternal and Child Health Journal. 2005 Jun;9(2):S3–S11. doi: 10.1007/s10995-005-4350-3. [DOI] [PubMed] [Google Scholar]
- 32.Viner-Brown SI, Kim HK. Impact of caring for children with special health care needs on the family: Rhode Island’s experience. Maternal and Child Health Journal. 2005 Jun;9(2):S59–S66. doi: 10.1007/s10995-005-4483-4. [DOI] [PubMed] [Google Scholar]
- 33.Ganz ML, Tendulkar SA. Mental health care services for children with special health care needs and their family members: Prevalence and correlates of unmet needs. Pediatrics. 2006 Jun;117(6):2138–2148. doi: 10.1542/peds.2005-1531. [DOI] [PubMed] [Google Scholar]
- 34.Kenney MK, Kogan MD, Crall JJ. Parental perceptions of dental/oral health among children with and without special health care needs. Ambulatory Pediatrics. 2008 Sep-Oct;8(5):312–320. doi: 10.1016/j.ambp.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 35.Churchill SS, Villareale NL, Monaghan TA, Sharp VL, Kieckhefer GM. Parents of Children with Special Health Care Needs Who have Better Coping Skills have Fewer Depressive Symptoms. Maternal and Child Health Journal. 2010 Jan;14(1):47–57. doi: 10.1007/s10995-008-0435-0. [DOI] [PubMed] [Google Scholar]
- 36.Coker TR, Rodriguez MA, Flores G. Family-Centered Care for US Children With Special Health Care Needs: Who Gets It and Why? Pediatrics. 2010 Jun;125(6):1159–1167. doi: 10.1542/peds.2009-1994. [DOI] [PubMed] [Google Scholar]
- 37.Lindley LC, Mark BA. Children with Special Health Care Needs: Impact of Health Care Expenditures on Family Financial Burden. Journal of Child and Family Studies. 2010 Feb;19(1):79–89. doi: 10.1007/s10826-009-9286-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ngui EM, Flores G. Satisfaction with care and ease of using health care services among parents of children with special health care needs: The roles of race/ethnicity, insurance, language, and adequacy of family-centered care. Pediatrics. 2006 Apr;117(4):1184–1196. doi: 10.1542/peds.2005-1088. [DOI] [PubMed] [Google Scholar]
- 39.Ngui EM, Flores G. Unmet needs for specialty, dental, mental, and allied health care among children with special health care needs: Are there racial/ethnic disparities? Journal of Health Care for the Poor and Underserved. 2007 Nov;18(4):931–949. doi: 10.1353/hpu.2007.0102. [DOI] [PubMed] [Google Scholar]
- 40.Honberg LE, Kogan MD, Allen D, Strickland BB, Newacheck PW. Progress in Ensuring Adequate Health Insurance for Children With Special Health Care Needs. Pediatrics. 2009 Nov;124(5):1273–1280. doi: 10.1542/peds.2009-0372. [DOI] [PubMed] [Google Scholar]
- 41.Montes G, Halterman JS. White-Black Disparities in Family-Centered Care Among Children with Autism in the United States: Evidence From the NS-CSHCN 2005–2006. Academic Pediatrics. 2011 Jul-Aug;11(4):297–304. doi: 10.1016/j.acap.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 42.Chiri G, Warfield ME. Unmet Need and Problems Accessing Core Health Care Services for Children with Autism Spectrum Disorder. Maternal and Child Health Journal. 2012 Jul;16(5):1081–1091. doi: 10.1007/s10995-011-0833-6. [DOI] [PubMed] [Google Scholar]
- 43.Craig B, Reeve B. Patient-Reported Outcomes and Preference Research: Igniting the Candle at Both Ends and the Middle. ISPOR Connections – Uniting Research and Practice. 2012;18(5) [Google Scholar]
- 44.PROMIS-29 Profile v1.0. 2008–2012. https://www.assessmentcenter.net/ac1//files/pdf/44b7636201a34267a9213db7f69f2c6d.pdf. Accessed June 06, 2012.
- 45.Feeny D. Standardization and regulatory guidelines may inhibit science and reduce the usefulness of analyses based on the application of preference-based measures for policy decisions. Medical decision making : an international journal of the Society for Medical Decision Making. 2013 Apr;33(3):316–319. doi: 10.1177/0272989X12468793. [DOI] [PubMed] [Google Scholar]
- 46.Craig B, Greiner W, Brown D, Reeve B. Valuation of Child Health-Related Quality of Life in the United States. Under Review. doi: 10.1002/hec.3184. [DOI] [PubMed] [Google Scholar]
- 47.Eiser C. Children with Cancer: The Quality of Life. Mahwah, New Jersey: Lawrence Erlbaum Associates, Inc; 2004. Vol isb. [Google Scholar]
- 48.Finley GA, McGrath PJ. Measurement of pain in infants and children. Journal of Pediatric Hematology/Oncology. 1998;20(4):364. [Google Scholar]
- 49.Arnesen T, Trommald M. Are QALYs based on time trade-off comparable? – A systematic review of TTO methodologies. Health Economics. 2005 Jan;14(1):39–53. doi: 10.1002/hec.895. [DOI] [PubMed] [Google Scholar]
- 50.Eidt-Koch D, Mittendorf T, Greiner W. Cross-sectional validity of the EQ-5D-Y as a generic health outcome instrument in children and adolescents with cystic fibrosis in Germany. BMC pediatrics. 2009;9:55. doi: 10.1186/1471-2431-9-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jelsma J. A comparison of the performance of the EQ-5D and the EQ-5D-Y health-related quality of life instruments in South African children. International journal of rehabilitation research. Internationale Zeitschrift fur Rehabilitationsforschung. Revue internationale de recherches de readaptation. 2010 Jun;33(2):172–177. doi: 10.1097/MRR.0b013e32832bb0f7. [DOI] [PubMed] [Google Scholar]
- 52.Ravens-Sieberer U, Wille N, Badia X, et al. Feasibility, reliability, and validity of the EQ-5D-Y: results from a multinational study. Quality of life research : an international journal of quality of life aspects of treatment, care and rehabilitation. 2010 Aug;19(6):887–897. doi: 10.1007/s11136-010-9649-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wille N, Badia X, Bonsel G, et al. Development of the EQ-5D-Y: a child-friendly version of the EQ-5D. Quality of Life Research. 2010 Aug;19(6):875–886. doi: 10.1007/s11136-010-9648-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Craig B, Runge S, Rand-Hendriksen K, Ramos-Goñi J, Oppe M. Learning and Satisficing: An Analysis of Sequence Effects in Health Valuation. Value Health. doi: 10.1016/j.jval.2014.11.005. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Harris J. The Value of Life. New York: Routledge & Kegan Paul; 1985. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


