Abstract
Objective
To determine whether optimism about HAART is associated with sexual risk behavior among young adult HIV-negative gay and bisexual men, and to test two alternative explanations for this association: (1) that treatment optimism leads to increased sexual risk or (2) that treatment optimism is the result of previous sexual risk.
Methods
Data on sexual risk behavior, treatment optimism, and perceived susceptibility to HIV infection were obtained from a sample of 538 HIV-negative or untested gay and bisexual men (ages 18 – 30) who were not in monogamous relationships. Follow-up data were collected eighteen months later.
Results
In the cross sectional data, treatment optimism was associated with the 2-month cumulative incidence of unprotected anal intercourse (UAI) with non-primary partners; however, this effect was observed only among men who felt highly susceptible to HIV infection. Longitudinal analyses revealed that treatment optimism did not predict subsequent UAI, but UAI did predict later treatment optimism.
Conclusion
Treatment optimism is associated with sexual risk behavior among young adult gay and bisexual men. However, these data suggest that optimism may result from, rather than precede, sexual risk.
Keywords: Human Immunodeficiency Virus, Sexual behavior, Gay men, Bisexual men, Treatment optimism
Introduction
In the past several years the incidence of unprotected anal intercourse (1–3), sexually transmitted infections (1, 2, 4–6), and HIV (7) has risen among men who have sex with men (MSM) in the United States and some other countries. Consequently, researchers and prevention advocates have begun searching for explanations for these alarming trends. Given the coincidence of increases in risk behaviors with the development of highly active antiretroviral therapy (HAART), some have speculated that optimism about the availability and efficacy of new HIV treatments is leading to decreased vigilance about precautionary behavior (8, 9).
Shortly after the development of HAART, studies began documenting that MSM did hold a variety of optimistic attitudes and beliefs about new HIV treatments (10, 11). Specifically, this optimism was manifest in both beliefs about how HIV/AIDS might be less serious or less infectious and attitudes reflecting less concern about the importance of safe sex. Since this early work, multiple cross-sectional studies have further demonstrated that treatment optimism is associated with sexual risk behavior (12–16).
Some investigators have implied a causal relationship between treatment optimism and risk behavior; however, reports of longitudinal data supporting this assumption are extremely limited. While a causal path from optimism to risk behavior is certainly plausible, it is also possible that following risky encounters, individuals increase their optimism about treatments as a form of post-hoc rationalization (17). An abundance of theoretical and empirical work from the behavioral sciences supports the notion that when individuals behave in a certain way, their attitudes and beliefs change as a result (18–24). At least one study on beliefs about HAART has found data consistent with this alternate explanation that treatment optimism may result, in part, from past risky behavior (25).
Despite the lack of longitudinal data to support causal hypotheses, two studies have been conducted that utilize cross-sectional samples taken at several points over time. A study of MSM attending gyms in London found cross-sectional associations between optimism and risk, but failed to show evidence across time for a causal link between optimism and risk behavior (26). Another study conducted with MSM in Sydney indicated that optimism about the efficacy of HAART for improving health increased between 1997 and 1999; however, men sampled in 1999 were no less worried about HIV than those sampled in 1997, and the belief in HAART’s ability to render sexual partners less infectious actually decreased over time (27). Thus, it did not appear as if optimism was increasing during the years in which increases in sexual risk and disease were observed.
Current Study
Although many studies have documented an association between risk and optimism, few have been able to inform the causal question. Emerging evidence suggests that the causal link between treatment optimism and risk may be more complex than previously assumed (25–27). We aimed to further explore the possibility that treatment optimism does not exclusively precede risk, but rather, may also result from past risky sexual behavior. To do this, we extended analyses that have been conducted in previous publications in two ways.
First, we aimed to examine in greater detail the cross sectional associations between risk and optimism. One possible method for informing the question of causality in cross sectional data on this topic is to examine associations between risk and optimism among individuals who differ in how susceptible they feel to HIV infection. Perceived susceptibility refers to an individual’s assessment of how vulnerable he is to a disease, given his levels of risk and precautionary behaviors (28). If individuals use optimism to rationalize their past risky behaviors, we would expect the association between risk and optimism to be most pronounced among individuals who feel highly susceptible to infection. Presumably, people who have unprotected sex and who feel highly susceptible to HIV infection are those who most need to find relief by rationalizing their past risk behavior with treatment optimism. In contrast, if treatment optimism truly precedes sexual risk behavior, the association between optimism and risk should hold, regardless of how susceptible individuals feel.
In addition to this cross sectional analysis, we conducted longitudinal analyses, examining the two competing causal hypotheses. The traditional hypothesis implied by some existing research is that treatment optimism precedes increases in sexual risk behavior. The competing hypothesis is that risk behavior precedes treatment optimism. Thus, we tested both models to determine which had greater support in our longitudinal data.
Presently, few studies have examined the association between optimism about HAART and sexual risk behavior in young adult gay and bisexual men. It is especially important that the phenomenon be understood among younger adults, given that they are at high risk for HIV infection in some parts of the world (29–31). Furthermore, many of these men came of age during the era of HAART, have not witnessed the devastating effects of AIDS, and thereby may be most prone to the effects of treatment optimism. Therefore, we sought to test the association between risk and optimism in a sample of relatively younger gay and bisexual male adults.
Methods
Study Population
A cohort of 1248 gay and bisexual men between the ages of 18 and 27 was recruited from Phoenix, AZ, Albuquerque, NM, and Austin, TX for participation in the “Young Men’s Survey,” a longitudinal study designed to test the effectiveness of a community-based HIV-preventive intervention. Participants were recruited independently of the intervention by peers who sought out eligible men through venues, organizations, and social networks. Detailed descriptions of the sampling methods can be found elsewhere (32, 33). Data were collected at three points in time; each collection was separated by approximately 18 months.
Treatment optimism was first assessed in the cohort during Wave 2. Therefore, data from the present study come from Waves 2 and 3, collected in 1998/1999 and 2000/2001 respectively. Table 1 displays the demographic characteristics of the samples at Waves 2 and 3. The sample included 837 men at Wave 2. Between Wave 2 and Wave 3, 67% (n = 561) of the sample was retained. Relative to men who were lost, men retained from Waves 2 to 3 were older, more educated, and less likely to be African-American. However, Hispanic, Native American, and Asian/Pacific Islander men were all proportionally retained between Waves 2 and 3. Men retained also did not differ in their levels of sexual risk behavior, treatment optimism, or the extent to which they were “out” about their sexual orientation.
Table 1.
Demographic Characteristics
| Wave 2 | Wave 3 | |
|---|---|---|
| n | 837 | 561 |
| Mean age | 24.8 years | 27.0 years |
| Mean outness score (range=1–5) | 4.2 | 4.3 |
| Education | ||
| Less than High School | 2.0% | 0.5% |
| High School Grad | 61.2% | 50.6% |
| College Grad | 36.8% | 48.8% |
| Ethnicity | ||
| African American | 4.7% | 3.2% |
| Asian / Pacific Islander | 3.7% | 3.7% |
| European American | 65.0% | 66.8% |
| Latino | 23.7% | 24.2% |
| Native American | 3.0% | 2.0% |
| Sexual Identity | ||
| Gay | 89.6% | 91.4% |
| Bisexual | 8.2% | 7.0% |
| Self-Reported HIV Status | ||
| Negative | 76.2% | 80.3% |
| Positive* | 5.9% | 7.5% |
| Untested | 17.8% | 12.3% |
HIV-positive men were excluded from the present analyses.
Men who reported that they were HIV-positive were excluded from the present analyses, as were men who failed to report their HIV-testing status (n = 72 at Wave 2 and n = 62 at Wave 3). For cross-sectional analyses, we utilized only men who were not in monogamous relationships at Wave 2 (n = 538), and for longitudinal analyses, we utilized only men who were not in monogamous relationships at both Waves 2 and 3 (n = 275). When Wave 2 to Wave 3 attrition analyses were repeated using only this subset of men eligible for the present study, no new differences were identified. Unless otherwise specified, variable n’s across analyses are the result of missing data.
Research Instrument
Participants indicated how frequently in the previous two months they had engaged in insertive and receptive anal intercourse: (1) with a condom, (2) without a condom – without ejaculating in their partner, and (3) without a condom – ejaculating in their partner. These behaviors were reported separately for non-primary partners and boyfriends/lovers. We created a dichotomous risk variable reflecting whether or not the participant reported any unprotected anal intercourse in the previous two months with any non-primary partner.
Treatment optimism was measured using two moderately correlated items (r = .43): “With all the new AIDS drugs, I’m not that concerned about getting HIV,” and “I’m not that concerned about catching HIV since there will probably be a cure by the time I get sick.” These items closely resemble items from more elaborate scales of treatment optimism that have been developed since these data were collected (34, 35). Participants responded to these items using a six-point Likert scale ranging from “Disagree strongly” to “Agree Strongly.” The mean of these two items was used in subsequent analyses. Perceived susceptibility to HIV infection was measured with the following item: “My sexual behavior is risky for catching or spreading HIV.” Participants responded to this item using a six-point Likert scale, ranging from “Disagree strongly” to “Agree Strongly.”
Results1
Descriptive Statistics and Correlation Analyses
Table 2 displays descriptive statistics for and correlations among the primary study variables. Participant age, education, and ethnicity were not consistently associated with either sexual risk behavior or treatment optimism, and therefore they were not included as covariates in subsequent analyses. Notably, levels of treatment optimism were low at both study waves, with the majority of respondents disagreeing moderately or strongly with the optimistic attitudes.
Table 2.
Descriptive Statistics and Intercorrelations for Primary Study Variables
| Variable (study wave) | Possible Range |
Mean | SD | 2. | 3. | 4. | 5. | 6. | 7. |
|---|---|---|---|---|---|---|---|---|---|
| 1. Age (2) | 18–30 | 24.70 | 2.98 | .34*** | −.05 | .06 | .01 | .04 | −.18** |
| 2. Education (2) | 1–7 | 4.31 | 1.22 | -- | −.06 | −.06 | −.09* | −.05 | −.01 |
| 3. Perceived Susceptibility (2) | 1–6 | 2.73 | 1.60 | -- | .22*** | .44*** | .16** | .14* | |
| 4. Treatment Optimism (2) | 1–6 | 1.48 | .84 | -- | .13** | .48*** | .01 | ||
| 5. Sexual Risk (2) | 0–1 | 0.31 | 0.46 | -- | .15* | .18** | |||
| 6. Treatment Optimism (3) | 1–6 | 1.47 | 0.75 | -- | .13* | ||||
| 7. Sexual Risk (3) | 0–1 | 0.31 | 0.47 | -- |
Note. Correlations among Wave 2 variables have n = 525. Correlations including Wave 3 variables have n = 268.
p < .05,
p < .01,
p < .001, two-tailed
Cross Sectional Analyses from Wave 2
A t-test was conducted to determine whether levels of treatment optimism were greater among men reporting any versus no sexual risk behavior in the previous two months. Levine’s test for equality of variances indicated unequal variances across groups, and so an adjusted value for degrees of freedom was used. Men reporting unprotected anal intercourse (UAI) with a non-primary partner were significantly more optimistic than men not reporting this behavior (UAI: M = 1.65, SD = 0.97, No UAI: M = 1.40, SD = 0.77), t (259.46) = −2.89, p < .01.2
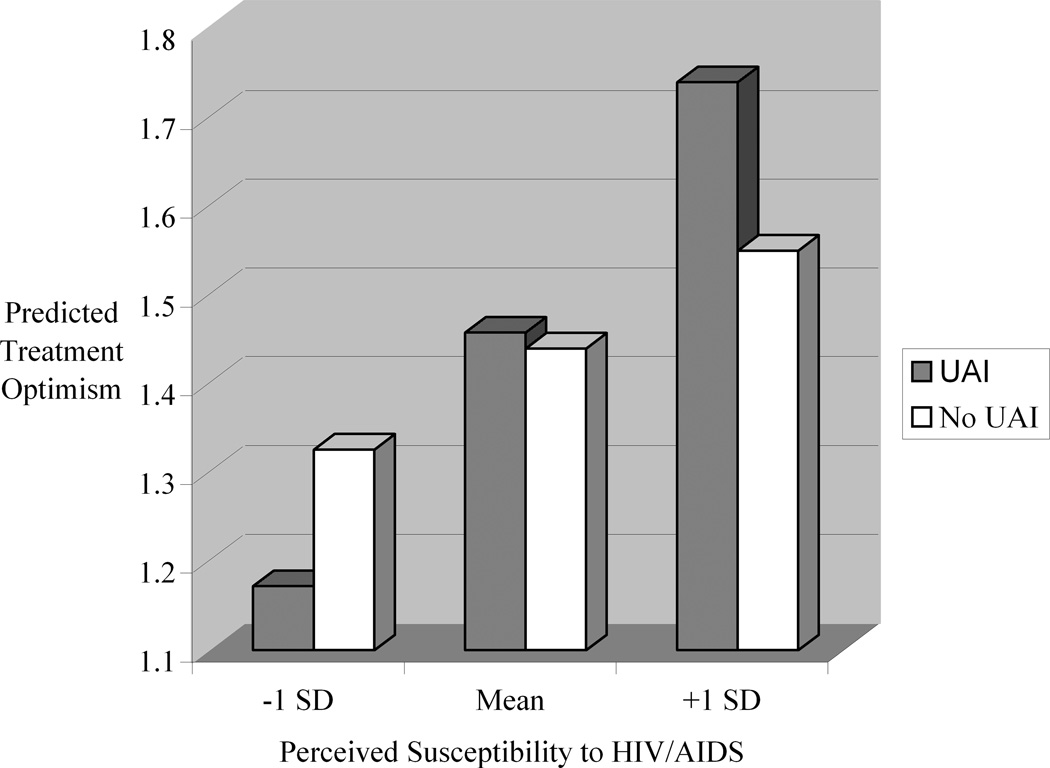
To determine whether this difference occurred at all levels of perceived susceptibility, an ordinary least squares (OLS) regression analysis was conducted in which treatment optimism was predicted from sexual risk behavior in the previous two months, perceived susceptibility, and the interaction of susceptibility and risk. The results presented in Table 3 reveal that susceptibility was a significant moderator of the association between risk and treatment optimism. Because a significant interaction was present, the simple associations between risk and treatment optimism were estimated at varying levels of perceived susceptibility (36). These associations are depicted in Figure 1, which illustrates how the previously observed cross-sectional association between treatment optimism and sexual risk behavior is actually only seen among men with relatively higher levels of perceived susceptibility.
Table 3.
Ordinary Least Squares Regression Analysis of Cross Sectional Data Predicting Treatment Optimism from Perceived Susceptibility and Past Unprotected Anal Intercourse
Figure 1.
Association between Unprotected Anal Intercourse in the Previous Two Months and Treatment Optimism at Varying Levels of Perceived Susceptibility
Longitudinal Analyses
We next tested two models using longitudinal data from Waves 2 to 3 to further examine whether treatment optimism precedes risk behavior or whether the opposite was true. For the first model, we conducted a logistic regression analysis in which sexual risk behavior at Wave 3 was predicted from Wave 2 treatment optimism, controlling for Wave 2 risk behavior. In this model, Wave 2 treatment optimism was not associated with Wave 3 risk behavior (B = −0.05, SE B = 0.17, OR = 0.95, ns). Wave 2 risk behavior did predict Wave 3 risk behavior (B = 0.88, SE B = 0.29, OR = 2.42, p < .01). In the second model we utilized OLS regression to predict Wave 3 treatment optimism from Wave 2 risk behavior, controlling for Wave 2 treatment optimism. In this model Wave 2 risk behavior significantly predicted Wave 3 treatment optimism (B = 0.18, SE B = 0.08, β = 0.11, p < .05). Wave 2 treatment optimism was also associated with Wave 3 treatment optimism (B = 0.36, SE B = 0.04, β = 0.41, p < .001). Thus, in testing these two models we found no evidence that treatment optimism predicts risk behavior at the subsequent wave of data collection. However, sexual risk behavior was a significant predictor of subsequent treatment optimism.
Discussion
The present study identified an association between treatment optimism and sexual risk behavior in a sample of young adult gay and bisexual men. Our findings are consistent with data from other samples of men showing similar relations between optimism and risk (12–15). However, this study was also the first to test a priori the theoretical possibility that treatment optimism does not precede sexual risk behavior in a standard, causal manner. Our data suggest that sexual risk behavior may proceed and lead to subsequent treatment optimism. This is in contrast to some empirical work and much of the public discourse on the topic that has implied that optimism surrounding new treatments has caused the recent increases in sexual risk behavior.
When men reported feeling only moderately or mildly susceptible to HIV-infection, optimism and sexual risk behavior were unrelated. Only among the men who reported feeling most susceptible to HIV-infection was there any association between optimism and risk behavior. One explanation for this finding is that higher levels of treatment optimism are, in part, a result of previous risk behavior. Men who engage in risk behavior and who feel susceptible to infection may have the greatest incentive to rationalize their behavior after the fact. They may do this by increasing their optimism related to new HIV treatments. In contrast, men who engage in risk behavior but are unconcerned have less need to rationalize their behavior, and thus have less need to feel optimistic about new treatments. Our longitudinal data further support the hypothesis that sexual risk behavior precedes treatment optimism, rather than the reverse. In our statistical models, treatment optimism did not predict subsequent risk behavior. However, risk behavior was a significant predictor of later treatment optimism.
Together, these findings suggesting that optimism may not lead to subsequent risk behavior are consistent with post hoc findings from one previous cross sectional study (25), as well as with other research that failed to show evidence for an association between optimism and risk over time (26). However, our results stand in contrast to recently reported findings from the only other longitudinal study on this topic of which we are aware. Stolte and colleagues (37) analyzed data from a sample of 146 young adult MSM from Amsterdam who reported no sexual risk behavior at an initial assessment; of these men reporting no initial risk, the 28 men who subsequently reported UAR at a later assessment also reported relatively more treatment optimism than the men who remained risk free. Their study did not report analyses that might examine the alternative hypothesis tested in the present paper – that optimism results from past risk behavior.
It is important to note that even if the direction of causality between treatment optimism and risk behavior is reversed, as we suggest is possible, this does not imply that treatment optimism is unimportant to address in prevention efforts. If treatment optimism is in part a cognitive mechanism to reduce post risk behavior anxiety, then treatment optimism may make sexual risk behavior more reinforcing and more likely to be sustained through subsequent sexual encounters. That is, if men feel less anxiety following sexual risk behavior, they may have fewer disincentives to engaging in those behaviors again in the future.
A further qualification of the traditional treatment optimism hypothesis is the fact that the men in our sample largely disagreed with the optimistic statements with which they were presented. This is consistent with recent findings obtained in Vancouver, Sydney, Paris, Melbourne and London (35). Given the fact that new treatments for HIV have clearly lead to dramatic decreases in HIV-related morbidity and mortality, it is surprising that treatment optimism is not more widespread. Nevertheless, current empirical data suggest that most men are unwilling to endorse optimistic statements. This further argues against the idea that reckless optimism about HIV has lead to increases in risk behavior.
Limitations
The findings of this study must be qualified by several limitations. First, our measure of treatment optimism consisted only of two items. While use of only two or three items to assess treatment optimism is not uncommon in the literature (13, 17, 26, 38), more complete measures of treatment related beliefs and attitudes do exist (15, 25, 34). These longer measures were not published when we constructed our survey. Our use of just two, only modestly correlated items to assess optimism most likely increased the unreliability of the measure, making tests of our hypotheses more conservative. In addition, because these data come from a convenience sample, the results may not be generalizable to the larger population of young American gay and bisexual men. This is a limitation our study shares with the existing literature on treatment optimism. Finally, the longitudinal analyses presented in this paper must be qualified by the fact that we experienced differential attrition in our cohort. We lost men who were younger and African-American, and therefore caution must be exercised in generalizing the longitudinal findings to these groups.
Conclusions
Treatment optimism remains among the most common hypotheses cited to explain the recently documented increases in risk behavior among MSM. This attention to treatment optimism has somewhat eclipsed research into other potential causes for these increases. For example, while HAART may have fueled optimism among MSM, it also fueled optimism among contributors to HIV/AIDS charities more generally, resulting in dramatic decreases in donations to these organizations (39). Thus, prevention efforts have been less well funded in the post HAART era, which may also contribute to increases in risk. Furthermore, HAART was not the only development to alter the landscape of sexual behavior and prevention in the mid 1990’s. Internet use exploded during this time as well, making available an efficient means for individuals to arrange casual sexual encounters. Recent findings document an association between Internet use and sexual risk (40, 41). Finally, methamphetamine use remains widespread among MSM in parts of the United States (42). Although it is unclear from existing data whether changes in the prevalence of methamphetamine use have occurred, this may be another reason for increased risk. Even with steady rates of amphetamine use, it is possible that the release of Viagra in 1998 has facilitated risk among men whose substance use would make them otherwise unable to perform sexually. Emerging data has linked Viagra use to risky sexual behavior (43, 44). Ultimately, it is unlikely that any one explanation can completely account for the recent increases in sexual risk behavior. Rather multiple factors are likely operating in a complex and dynamic manner to affect gay men’s sexual risk behavior.
This study adds to a growing body of work that attempts to explain the recent increases in sexual risk behavior among MSM. Our findings suggest that although risk and treatment optimism are related, the association may be more complex than previously thought. Whereas some prior research has implied that optimism drives subsequent risky sexual behavior, our data indicate that optimism is just as likely to follow from past risk behavior. As emerging studies show the limitations of the traditional treatment optimism hypothesis, researchers must continue to explore additional reasons for this resurgence in sexual risk behavior and disease.
Acknowledgments
This research was supported by grant MH46816 and grant MH19105-14 from the National Institute for Mental Health. The authors would also like to acknowledge Robert Hays, PhD, for his contributions to all aspects of this study and to Ben Zovod for his efforts in the data collection for this study. This study was approved by the Committee on the Use of Human Subjects in Research of the University of California, San Francisco.
Footnotes
Because these data were collected during the course of a trail of an HIV-prevention intervention, it is possible that exposure to the intervention might affect the results of the present analyses. While the intervention did not contain components specifically addressing treatment optimism or its potential effect on sexual risk behavior, we nevertheless conducted analyses to ensure that the intervention did not have an impact on our findings. After the primary data analyses were conducted on the full sample, analyses were re-run using only the subsample of men from our control city (Phoenix). When only those data were utilized, the effects were not substantively different from those obtained in the full sample.
Similar effects were obtained when only the subset of men (n = 275) providing data at both waves 2 and 3 were analyzed, as well as when data from Wave 3 only were analyzed cross-sectionally.
References
- 1.US Centers for Disease Control and Prevention. Increases in unsafe sex and rectal gonorrhea among men who have sex with men -- San Francisco, CA, 1994–1997. Morbidity and Mortality Weekly Report. 1999;48:45–58. [PubMed] [Google Scholar]
- 2.Chen SY, Gibson S, Katz MH, et al. Continuing increases in sexual risk behavior and sexually transmitted diseases among men who have sex with men: San Francisco, Calif, 1999–2001, USA. Am. J. Public Health. 2002;92:1387–1388. [PMC free article] [PubMed] [Google Scholar]
- 3.Van de Ven P, Prestage G, Crawford J, Grulich A, Kippax S. Sexual risk behaviour increases and is associated with HIV optimism among HIV-negative and HIV-positive gay men in Sydney over the 4 year period to February 2000. AIDS. 2000;14:2951–2953. doi: 10.1097/00002030-200012220-00023. [DOI] [PubMed] [Google Scholar]
- 4.US Centers for Disease Control and Prevention. Resurgent bacterial sexually transmitted disease among men who have sex with men -- King County, Washington, 1997–1999. Morbidity and Mortality Weekly Report. 1999;48:773–777. [PubMed] [Google Scholar]
- 5.Stolte IG, Dukers NH, de Wit JB, Fennema JS, Coutinho RA. Increase in sexually transmitted infections among homosexual men in Amsterdam in relation to HAART. Sex. Transm. Infect. 2001;77:184–186. doi: 10.1136/sti.77.3.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dupin N, Jdid R, N'Guyen YT, Gorin I, Franck N, Escande JP. Syphilis and gonorrhoea in Paris: the return. AIDS. 2001;15:814–815. doi: 10.1097/00002030-200104130-00026. [DOI] [PubMed] [Google Scholar]
- 7.Katz MH, Schwarcz SK, Kellogg TA, et al. Impact of highly active antiretroviral treatment on HIV seroincidence among men who have sex with men: San Francisco. Am. J. Public Health. 2002;92:388–394. doi: 10.2105/ajph.92.3.388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kelly JA, Otto-Salaj LL, Sikkema KJ, Pinkerton SD, Bloom F. Implications of HIV treatment advances for behavioral research on AIDS: Protease inhibitors and new challenges in HIV secondary prevention. Health Psychol. 1998;17:310–319. doi: 10.1037//0278-6133.17.4.310. [DOI] [PubMed] [Google Scholar]
- 9.Signorile M. Bareback and restless. Out. 1997 Jul;:36–37. [Google Scholar]
- 10.Kelly JA, Hoffmann RG, Rompa D, Gray M. Protease inhibitor combination therapies and perceptions of gay men regarding AIDS severity and the need to maintain safer sex. AIDS. 1998;12:F91–F95. doi: 10.1097/00002030-199810000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Dilley JW, Woods WJ, McFarland W. Are advances in treatment changing views about high-risk sex? N. Engl. J. Med. 1997;337:501–502. doi: 10.1056/NEJM199708143370715. [DOI] [PubMed] [Google Scholar]
- 12.Van de Ven P, Kippax S, Knox S, Prestage G, Crawford J. HIV treatments optimism and sexual behaviour among gay men in Sydney and Melbourne. AIDS. 1999;13:2289–2294. doi: 10.1097/00002030-199911120-00011. [DOI] [PubMed] [Google Scholar]
- 13.Van de Ven P, Rawstorne P, Nakamura T, Crawford J, Kippax S. HIV treatments optimism is associated with unprotected anal intercourse with regular and with casual partners among Australian gay and homosexually active men. Int. J. STD AIDS. 2002;13:181–183. doi: 10.1258/0956462021924884. [DOI] [PubMed] [Google Scholar]
- 14.Kalichman SC, Nachimson D, Cherry C, Williams E. AIDS treatment advances and behavioral prevention setbacks: preliminary assessment of reduced perceived threat of HIV-AIDS. Health Psychol. 1998;17:546–550. doi: 10.1037//0278-6133.17.6.546. [DOI] [PubMed] [Google Scholar]
- 15.Ostrow DE, Fox KJ, Chmiel JS, et al. Attitudes towards highly active antiretroviral therapy are associated with sexual risk taking among HIV-infected and uninfected homosexual men. AIDS. 2002;16:775–780. doi: 10.1097/00002030-200203290-00013. [DOI] [PubMed] [Google Scholar]
- 16.Vanable PA, Ostrow DG, McKirnan DJ, Taywaditep KJ, Hope B. Impact of combination therapies on HIV risk perceptions and sexual risk among HIV-positive and HIV-negative gay and bisexual men. Health Psychol. 2000;19:134–145. doi: 10.1037//0278-6133.19.2.134. [DOI] [PubMed] [Google Scholar]
- 17.Elford J, Bolding G, Maguire M, Sherr L. Combination therapies for HIV and sexual risk behavior among gay men. Journal of Acquired Immunodeficiency Syndrome. 2000;23:266–271. doi: 10.1097/00126334-200003010-00010. [DOI] [PubMed] [Google Scholar]
- 18.DeRubeis RJ, Crits-Christoph P. Empirically supported individual and group psychological treatments for adult mental disorders. Journal of Consulting & Clinical Psychology. 1998;66:37–52. doi: 10.1037//0022-006x.66.1.37. [DOI] [PubMed] [Google Scholar]
- 19.Aronson E. Berkowitz L. Advances in experimental social psychology. San Diego, CA: Academic Press; 1969. The theory of cognitive dissonance: A current perspective; pp. 1–34. [Google Scholar]
- 20.Festinger LA. A theory of cognitive dissonance. Evanston, IL: Row, Peterson; 1957. [Google Scholar]
- 21.Craighead WE, Craighead LW, Ilardi SS. Psychosocial treatments for major depressive disorder. In: Nathan PE, Gorman JM, editors. A guide to treatments that work. 1998. pp. 226–239. [Google Scholar]
- 22.Emmelkamp PMG. Behavior therapy with adults. In: Bergin AE, Garfield SL, editors. Handbook of psychotherapy and behavior change. 4th ed. Oxford, England: John Wiley & Sons; 1994. pp. 379–427. [Google Scholar]
- 23.Cooper J, Croyle RT. Attitudes and attitude change. Annu. Rev. Psychol. 1984;35:395–426. doi: 10.1146/annurev.ps.35.020184.002143. [DOI] [PubMed] [Google Scholar]
- 24.Kiesler CA, Pallak MS. Arousal properties of dissonance manipulations. Psychol. Bull. 1976;83:1014–1025. [PubMed] [Google Scholar]
- 25.Huebner DM, Gerend MA. The relation between beliefs about drug treatments for HIV and sexual risk behavior in gay and bisexual men. Ann. Behav. Med. 2001;23:304–312. doi: 10.1207/S15324796ABM2304_10. [DOI] [PubMed] [Google Scholar]
- 26.Elford J, Bolding G, Sherr L. High-risk sexual behaviour increases among London gay men between 1998 and 2001: What is the role of HIV optimism? AIDS. 2002;16:1537–1544. doi: 10.1097/00002030-200207260-00011. [DOI] [PubMed] [Google Scholar]
- 27.Knox S, Van De Ven P, Prestage G, Crawford J, Grulich A, Kippax S. Increasing realism among gay men in Sydney about HIV treatments: Changes in attitudes over time. Int. J. STD AIDS. 2001;12:310–314. doi: 10.1258/0956462011923147. [DOI] [PubMed] [Google Scholar]
- 28.Gerrard M, Gibbons FX, Bushman BJ. Relation between perceived vulnerability to HIV and precautionary sexual behavior. Psychol. Bull. 1996;19:390–409. doi: 10.1037/0033-2909.119.3.390. [DOI] [PubMed] [Google Scholar]
- 29.Koblin BA, Torian LV, Guilin V, Ren L, MacKellar DA, Valleroy LA. High prevalence of HIV infection among young men who have sex with men in New York City. AIDS. 2000;14:1793–1800. doi: 10.1097/00002030-200008180-00015. [DOI] [PubMed] [Google Scholar]
- 30.Mansergh G, Marks G. Age and risk of HIV infection in men who have sex with men. AIDS. 1998;12:1119–1128. doi: 10.1097/00002030-199810000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Valleroy L, MacKellar D, Karon J, et al. HIV Prevalence and Associated Risks in Young Men Who Have Sex With Men. JAMA. 2000;284:198–204. doi: 10.1001/jama.284.2.198. [DOI] [PubMed] [Google Scholar]
- 32.Kegeles SM, Hays RB, Pollack LM, Coates TJ. Mobilizing young gay and bisexual men for HIV prevention: A two-community study. AIDS. 1999;13:1753–1762. doi: 10.1097/00002030-199909100-00020. [DOI] [PubMed] [Google Scholar]
- 33.Kegeles SM, Hays RB, Coates TJ. The Mpowerment Project: A community-level HIV prevention intervention for young gay men. Am. J. Public Health. 1996;86:1129–1136. doi: 10.2105/ajph.86.8_pt_1.1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Van de Ven P, Crawford J, Kippax S, Knox S, Prestage G. A scale of optimism-scepticism in the context of HIV treatments. AIDS-Care. 2000;12:171–176. doi: 10.1080/09540120050001841. [DOI] [PubMed] [Google Scholar]
- 35.International Collaboration on HIV Optimism. HIV treatments optimism among gay men: An international perspective. J. Acquir. Immune Defic. Syndr. 2003;32:545–550. doi: 10.1097/00126334-200304150-00013. [DOI] [PubMed] [Google Scholar]
- 36.Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- 37.Stolte IG, Dukers NH, Geskus RB, Coutinho RA, de Wit JB. Homosexual men change to risky sex when perceiving less threat of HIV/AIDS since availability of highly active antiretroviral therapy: a longitudinal study. AIDS. 2004;18:303–309. doi: 10.1097/00002030-200401230-00021. [DOI] [PubMed] [Google Scholar]
- 38.Remien RH, Wagner G, Carballo-Diéguez A, Dolezal C. Who may be engaging in high-risk sex due to medical treatment advances? AIDS. 1998;12:1560–1561. doi: 10.1097/00002030-199812000-00025. [DOI] [PubMed] [Google Scholar]
- 39.Private donations tumble as funders lose interest in HIV. AIDS Policy Law. 1999;14:1, 6. [PubMed] [Google Scholar]
- 40.Benotsch EG, Kalichman S, Cage M. Men who have met sex partners via the Internet: Prevalence, predictors, and implications for HIV prevention. Arch. Sex. Behav. 2002;31:177–183. doi: 10.1023/a:1014739203657. [DOI] [PubMed] [Google Scholar]
- 41.Elford J, Bolding G, Sherr L. Seeking sex on the Internet and sexual risk behaviour among gay men using London gyms. AIDS. 2001;15:1409–1415. doi: 10.1097/00002030-200107270-00010. [DOI] [PubMed] [Google Scholar]
- 42.Mansergh G, Colfax GN, Marks G, Rader M, Guzman R, Buchbinder S. The Circuit Party Men's Health Survey: Findings and implications for gay and bisexual men. Am. J. Public Health. 2001;91:953–958. doi: 10.2105/ajph.91.6.953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Colfax GN, Mansergh G, Guzman R, et al. Drug use and sexual risk behavior among gay and bisexual men who attend circuit parties: A venue-based comparison. J. Acquir. Immune Defic. Syndr. 2001;28:373–379. doi: 10.1097/00126334-200112010-00011. [DOI] [PubMed] [Google Scholar]
- 44.Sherr L, Bolding G, Maguire M, Elford J. Viagra use and sexual risk behaviour among gay men in London. AIDS. 2000;14:2051–2053. doi: 10.1097/00002030-200009080-00024. [DOI] [PubMed] [Google Scholar]