Abstract
Background
It is recommended that general practitioners (GPs) offer cessation advice and pharmacological interventions to smokers with acute coronary syndrome (ACS). The study objective was to describe the extent to which this is done, and to describe outcomes by smoking status.
Design
Patients aged 30+ hospitalised for troponin-positive ACS from 2002 to 2009, discharged home alive, were identified in the Myocardial Ischaemia National Audit Project registry. Patient data were linked to the General Practice Research Database, Hospital Episode Statistics, and Office of National Statistics mortality data, enabling a unique perspective of longitudinal smoking data. Patients who smoked prior to the hospitalisation had GP interventions and quitting status established in the 3 months following discharge, and were followed up for major clinical outcomes.
Methods
The outcomes evaluated included death, repeat ACS, stroke, heart failure, and major adverse cardiac events (MACE).
Results
Of the 4834 patients included, 965 (20%) were smokers at the time of their ACS. After the ACS event, only 225 (24%) received any GP smoking intervention within 3 months, with 82 (9%) receiving advice only, and 143 (15%) receiving a pharmacological intervention. Patients who quit (320; 33%) were at a decreased risk of mortality (relative risk (RR) 0.49; 95% confidence interval (CI) 0.35–0.69) and MACE (RR 0.61; 0.46–0.80) compared with patients who did not.
Conclusions
Whilst a high proportion of patients with ACS are smokers, there is a low level of GP cessation intervention following hospital discharge. This missed opportunity of patient care is important given the decreased risk of mortality and MACE found amongst those who quit.
Keywords: Smoking, cessation, acute coronary syndrome, mortality, stroke, heart failure, general practice
Introduction
Acute coronary syndrome (ACS) occurs in around 130,000 patients in England and Wales each year. Smoking is a major risk factor for ACS, whilst quitting smoking is associated with a 36% reduction in risk of all-cause mortality and a 32% reduction in non-fatal myocardial infarction among patients with coronary heart disease.1 A recent study found that smoking relapse after ACS is associated with a significant increase in all-cause mortality in these patients and that an earlier resumption of smoking is associated with a greater risk of death compared with a later relapse.2
It is recommended internationally that general practitioners (GPs) offer smoking cessation advice and treatment to smokers who have ACS.3 Smoking cessation advice from GPs, given during routine consultations, encourages patients to stop smoking and pharmacological interventions may double the effectiveness of advice alone.4–6 A Cochrane review states that, for cardiovascular inpatients, intensive counselling intervention begun in hospital and continued with supportive contacts for at least 1 month after discharge is the only non-pharmacological intervention that delivers an increase in smoking cessation rates. Less intensive counselling intervention has no influence on cessation rates.7
The Myocardial Ischaemia National Audit Project (MINAP) registry has collected data on patients with myocardial infarction since 1998 and more recently collects information on the treatment of patients who have been admitted to hospital with ACS.8 However, no information on the treatment of these patients once they have been discharged into primary care is collected.
The General Practice Research Database (GPRD) collates the computerised medical records of GPs. GPs play a key role in the UK healthcare system as they are responsible for primary healthcare and specialist referrals. Patients are semi-permanently affiliated with a practice that centralises the medical information from the GPs, specialist referrals and hospitalisations. The data recorded in the GPRD include demographic information, prescription details, clinical events, preventative care, specialist referrals, hospital admissions and major outcomes.9 However, in-depth information on events occurring in secondary care is not comprehensively recorded.
GPRD can now be linked individually and anonymously to other National Health Service (NHS) datasets in England, including MINAP. When this study was conducted 224 GP practices in England were participating in the linkage (approximately 45% of all GPRD practices). The linkage between the secondary care data within MINAP and the primary care data in the GPRD allows studies that follow patients throughout their NHS care to give a more complete picture of the treatment and outcomes of patients in England, such as those with ACS. Of particular interest is the unique perspective this linkage provides on longitudinal smoking status.
The objective of this study was to utilise the linked GPRD-MINAP record to describe the extent of smoking cessation advice and pharmaceutical interventions for smoking cessation provided by GPs following ACS and to describe patient outcomes stratified by smoking status.
Methods
This retrospective observational study utilised linked data from the MINAP, GPRD, Hospital Episode Statistics (HES) and Office of National Statistics (ONS) mortality datasets. Linkage between participating GPRD practices and MINAP required both to send information on patient identifiers, including NHS number, to a trusted third party. The linkage was done in two passes. The first pass matched patients on NHS number, sex and partial date of birth. The second pass matched patients on sex, date of birth and postcode. After matching, the patient identifiers were removed. The study protocol was reviewed and approved by independent scientific committees with experience in GPRD and MINAP studies.
The study population included patients aged 30 years and over who were hospitalised for troponin-positive ACS in the period between 1 January 2002 and 30 September 2009. Patients who were discharged alive from the hospital to home were followed from the date of hospital discharge to death, transfer out of the general practice, or the last data collection date. In case of repeat ACS admissions in MINAP, one record was randomly selected.
The characteristics of the ACS cases, as recorded in MINAP and GPRD, were described. Mean and median troponin levels were taken from the MINAP data, whilst all other variables were taken from GPRD. These included age, gender, alcohol use, socioeconomic status, systolic blood pressure, and the ratio of total cholesterol to high-density lipoprotein cholesterol. In addition, smoking status and the extent of smoking cessation interventions provided by the GP prior to the ACS were described. Interventions were classified into the following three groups:
prescribed pharmacological interventions for smoking cessation;
GP smoking cessation advice or referral to stop-smoking clinic (without pharmaceutical interventions);
no GP intervention.
Counts and percentages and means and medians were calculated as appropriate.
GPRD records of patients who smoked prior to their ACS were searched for evidence of GP interventions for smoking cessation in the 3 months following discharge. This included events recorded using Read codes (the coded thesaurus of clinical terms used by GPs in primary care), prescriptions and information recorded in the free text. Evidence of quitting was also recorded.
Major clinical outcomes were explored in patients who smoked prior to their ACS, stratified by quitting status. The outcomes included death (as recorded in the ONS mortality data), repeat ACS (as recorded in MINAP or GPRD), stroke (as recorded in GPRD or HES), heart failure (as recorded in GPRD or HES) and major adverse cardiac events (MACEs), defined as death, recurrent ACS, coronary artery bypass grafting or target lesion revascularisation (defined as percutaneous intervention or bypass surgery). GPRD and HES were used to identify the cardiac procedures. Cox proportional hazards regression was used to estimate the absolute incidence and relative rates.
Results
Table 1 shows the characteristics of the 4834 patients with ACS included in the study. Smoking status was recorded for almost all patients, with approximately 20% classified as current smokers at the time of the ACS event. Approximately 65% of patients were aged 70 or older at the time of the ACS and 61% were men. However, amongst smokers, only 33% were aged 70 or older and a higher proportion were men. The mean systolic blood pressure, as recorded prior to the ACS in GPRD, was elevated above normal, but not to the level considered to be hypertensive. The median peak troponin concentration during the hospitalisation, as recorded in MINAP, was consistent with the diagnosis of ACS.
Table 1.
Characteristics of 4834 patients with acute coronary syndrome (ACS) by smoking status measured prior to hospitalisation.
| Characteristics | Non-smokers (1611) | Ex-smokers (2122) | Smokers (965) | Unknown (136) | Total (4834) |
|---|---|---|---|---|---|
| Men | 743 (46.1%) | 1437 (67.7%) | 690 (71.5%) | 81 (59.6%) | 2951 (61.0%) |
| Age at ACS hospitalisation | |||||
| 30–39 | 6 (0.4%) | 6 (0.3%) | 23 (2.4%) | 4 (2.9%) | 39 (0.8%) |
| 40–49 | 42 (2.6%) | 41 (1.9%) | 139 (14.4%) | 9 (6.6%) | 231 (4.8%) |
| 50–59 | 149 (9.2%) | 145 (6.8%) | 248 (25.7%) | 19 (14.0%) | 561 (11.6%) |
| 60–69 | 214 (13.3%) | 395 (18.6%) | 233 (24.1%) | 20 (14.7%) | 862 (17.8%) |
| 70–79 | 468 (29.1%) | 700 (33.0%) | 204 (21.1%) | 24 (17.6%) | 1396 (28.9%) |
| 80+ | 732 (45.4%) | 835 (39.3%) | 118 (12.2%) | 60 (44.1%) | 1745 (36.1%) |
| Drinking status: | |||||
| Non-drinker | 310 (19.2%) | 214 (10.1%) | 109 (11.3%) | 1 (0.7%) | 634 (13.1%) |
| Ex-drinker | 164 (10.2%) | 244 (11.5%) | 96 (9.9%) | 1 (0.7%) | 505 (10.4%) |
| Drinker | 955 (59.3%) | 1527 (72.0%) | 657 (68.1%) | 6 (4.4%) | 3145 (65.1%) |
| Unknown | 182 (11.3%) | 137 (6.5%) | 103 (10.7%) | 128 (94.1%) | 550 (11.4%) |
| Systolic BP: mean, median | 139.1, 140.0 | 138.3, 139.0 | 137.8, 138.0 | 143.1, 140.0 | 138.6, 139.0 |
| Total/HDL cholesterol: | |||||
| ≤7 | 971 (60.3%) | 1530 (72.1%) | 498 (51.6%) | 19 (14.0%) | 3018 (62.4%) |
| >7 | 29 (1.8%) | 25 (1.2%) | 39 (4.0%) | 0 (0.0%) | 93 (1.9%) |
| Unknown | 611 (37.9%) | 567 (26.7%) | 428 (44.4%) | 117 (86.0%) | 1723 (35.6%) |
| Deprivation (IMD) quintile | |||||
| 0 (least deprived) | 287 (17.8%) | 328 (15.5%) | 84 (8.7%) | 17 (12.5%) | 716 (14.8%) |
| 1 | 378 (23.5%) | 465 (21.9%) | 158 (16.4%) | 32 (23.5%) | 1033 (21.4%) |
| 2 | 351 (21.8%) | 444 (20.9%) | 203 (21.0%) | 31 (22.8%) | 1029 (21.3%) |
| 3 | 317 (19.7%) | 441 (20.8%) | 237 (24.6%) | 30 (22.1%) | 1025 (21.2%) |
| 4 (most deprived) | 278 (17.3%) | 444 (20.9%) | 283 (29.3%) | 26 (19.1%) | 1031 (21.3%) |
| Peak troponin: mean, median | 5.3, 0.8 | 6.8, 0.8 | 6.6, 0.8 | 5.0, 0.9 | 6.2, 0.8 |
BP: blood pressure; HDL: high-density lipoprotein; IMD: Index of Multiple Deprivation.
Table 2 shows the concordance between smoking status recorded prior to the admission by GPs (from GPRD) and smoking status recorded on admission to hospital for the ACS (from MINAP). Whilst smoking status was more complete in the GPRD record, the concordance between GPRD and MINAP data was strong.
Table 2.
Concordance between primary care (General Practice Research Database (GPRD)) and hospital registry (Myocardial Ischaemia National Audit Project (MINAP)) records of smoking status prior to admission.
| Smoking status recorded in MINAP | Smoking status recorded in GPRD |
|||
|---|---|---|---|---|
| Non-smoker | Ex-smoker | Smoker | Unknown | |
| Non-smoker | 837 | 263 | 32 | 35 |
| Ex-smoker | 227 | 1311 | 123 | 46 |
| Smoker | 34 | 150 | 729 | 25 |
| Unknown | 513 | 398 | 81 | 30 |
Tables 3 and 4 show the extent of GP smoking cessation interventions amongst smokers prior to and after the ACS hospitalisation, both overall (Table 3) and by gender and age (Table 4). Prior to hospitalisation, almost half of smokers had received no intervention, and this proportion was higher amongst those aged at least 80 years. In the 3 months following discharge, over three-quarters received no intervention, despite 99% of patients having had some contact with their GP. Again, the proportion of patients who received no intervention in the 3 months following discharge was higher amongst those aged at least 80 years.
Table 3.
Patterns of smoking cessation interventions in primary care amongst 965 people who were current smokers at the time of admission with acute coronary syndrome (ACS).
| Coded data, n (%) | Free text, n (%) | Combined, n (%) | |
|---|---|---|---|
| Intervention prior to ACS | |||
| Pharmacological | 262 (27.1) | 80 (8.3) | 272 (28.2) |
| Advice/referral | 7 (0.7) | 374 (38.8) | 262 (27.2) |
| None | 696 (72.1) | 511 (53.0) | 431 (44.7) |
| 3 months following ACS | |||
| Pharmacological | 141 (14.6) | 42 (4.4) | 143 (14.8) |
| Advice/referral | 4 (0.4) | 107 (11.1) | 82 (8.5) |
| None | 820 (85.0) | 816 (84.6) | 740 (76.7) |
Table 4.
Patterns of smoking cessation interventions in primary care by age and gender.
| Pre-ACS intervention (ever) |
Post-ACS intervention (in 3 months following discharge) |
|||||
|---|---|---|---|---|---|---|
| Pharmacological | Advice/referral | None | Pharmacological | Advice/referral | None | |
| Men | 175 (25.4) | 192 (27.8) | 323 (46.8) | 102 (14.8) | 69 (10.0) | 519 (75.2) |
| Women | 97 (35.3) | 70 (25.5) | 108 (39.3) | 41 (14.9) | 13 (4.7) | 221 (80.4) |
| 30–39 | 7 (30.4) | 10 (43.5) | 6 (26.1) | 10 (43.5) | 2 (8.7) | 11 (47.8) |
| 40–49 | 40 (28.8) | 34 (24.5) | 65 (46.8) | 27 (19.4) | 21 (15.1) | 91 (65.5) |
| 50–59 | 72 (29.0) | 70 (28.2) | 106 (42.7) | 57 (23.0) | 27 (10.9) | 164 (66.1) |
| 60–69 | 78 (33.5) | 56 (24.0) | 99 (42.5) | 34 (14.6) | 17 (7.3) | 182 (78.1) |
| 70–79 | 58 (28.4) | 57 (27.9) | 89 (43.6) | 12 (5.9) | 12 (5.9) | 180 (88.2) |
| 80+ | 17 (14.4) | 35 (29.7) | 66 (55.9) | 3 (2.5) | 3 (2.5) | 112 (94.9) |
ACS: acute coronary syndrome.
Table 5 shows the change in smoking status and number of cigarettes smoked per day from the last GP record prior to hospitalisation to the first GP record in the three months after hospitalisation. The number of cigarettes smoked per day was recorded for 92% of smokers prior to hospitalisation. Of these, approximately half (56%) had no change in smoking status or number of cigarettes smoked per day, whilst 32% were recorded as “ex-smoker”. A small proportion had evidence of a decrease in the extent of smoking recorded (9%) whilst a minority increased their consumption (4%).
Table 5.
Change in status and number of cigarettes smoked a day from last record pre-acute coronary syndrome (ACS) to first record within 3 months of ACS.
| Post-ACS (first record within 3 months of ACS) |
|||||||
|---|---|---|---|---|---|---|---|
| Pre-ACS | Ex-smoker | Up to 5 a day | 6–10 a day | 11–15 a day | 16–20 a day | Over 20 a day | Unknown no. |
| Up to 5 a day | 60 | 134 | 7 | 1 | 2 | 1 | N/A |
| 6–10 a day | 76 | 22 | 126 | 5 | 7 | 0 | N/A |
| 11–15 a day | 46 | 7 | 10 | 64 | 3 | 1 | N/A |
| 16–20 a day | 76 | 9 | 9 | 7 | 112 | 5 | N/A |
| Over 20 a day | 22 | 4 | 4 | 3 | 5 | 55 | N/A |
| Unknown no. | 18 | 4 | 4 | 0 | 1 | 2 | 53 |
N/A: not applicable.
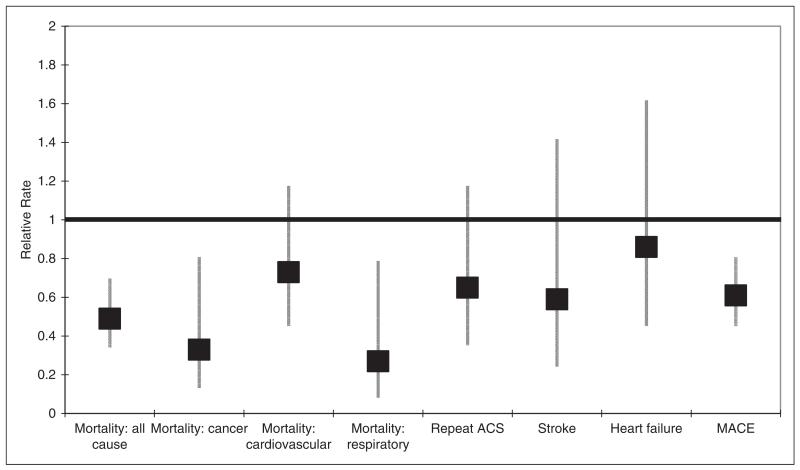
In total, 320 (33%) smokers quit within the first 3 months following the ACS hospitalisation. Table 6 and Figure 1 show the incidence (per 1000 patient years) and relative rate of major clinical outcomes in ACS smokers by quitting status. The relative rate of all-cause mortality, mortality due to neoplasms and mortality due to diseases of the respiratory system were significantly lower in smokers who quit within 3 months of discharge compared with those who remained smokers. There was also a significantly lower rate of MACE in smokers who quit. Other clinical outcomes, including repeat ACS, stroke and heart failure, tended to be lower in smokers who quit compared with those who remained smokers but the difference was not significant.
Table 6.
Incidence (per 1000 patient years) and relative rate of major clinical outcomes in smokers with acute coronary syndrome (ACS) by quitting status.
| Outcome | Smokers n=645 | Incidence in smokers | Quitters n=320 | Incidence in quitters | Relative rate |
|---|---|---|---|---|---|
| Mortality | |||||
| All cause | 149 | 105.1 (89.5–123.5) | 43 | 50.2 (37.3–67.7) | 0.49 (0.35–0.69) |
| Cancer | 30 | 21.2 (14.8–30.3) | 6 | 7.0 (3.2–15.6) | 0.33 (0.14–0.80) |
| Cardiovascular | 58 | 40.9 (31.6–52.9) | 25 | 29.2 (19.7–43.2) | 0.73 (0.46–1.17) |
| Respiratory | 25 | 17.6 (11.9–26.11) | 4 | 4.7 (1.8–12.5) | 0.27 (0.09–0.78) |
| Repeat ACS | 44 | 22.5 (16.7–30.2) | 15 | 14.1 (8.5–23.4) | 0.65 (0.36–1.17) |
| Stroke | 19 | 15.1 (9.6–23.6) | 7 | 8.9 (4.2–18.7) | 0.59 (0.25–1.41) |
| Heart failure | 28 | 22.8 (15.7 – 33.0) | 15 | 19.2 (11.6–31.8) | 0.86 (0.46–1.61) |
| MACE | 185 | 167.8 (145.3–193.8) | 69 | 98.0 (77.4–124.0) | 0.61 (0.46–0.80) |
MACE: major adverse cardiac event.
Figure 1.
Relative rate of major clinical outcomes in smokers with acute coronary syndrome (ACS) by quitting status. MACE: major adverse cardiac event.
Discussion
This study of linked primary and secondary care databases provides a unique longitudinal perspective on smoking status and cessation interventions before and after hospitalisation for ACS. The results show that a minority of patients discharged from hospital after ACS receive interventions for smoking and a large number continue to smoke. This missed opportunity for care is important because patients who continued to smoke had a significantly worse prognosis than those who quit.
The use of linked GPRD and MINAP registry data in this study provided a unique longitudinal perspective on smoking patterns in patients before, during, and after hospital admission with ACS. In the period before presentation with ACS only 54% of smokers received smoking cessation interventions, while in the 3 months after discharge, when motivation to stop was likely much higher, only 23% of smokers received smoking cessation interventions. The benefits of smoking cessation interventions are well established4–7 and the demonstrated failure of adherence to guideline recommendations for smoking cessation interventions no doubt contributed to the high proportion of smokers who failed to quit after ACS and who were thereby exposed to an increased risk of adverse outcomes.
The failure of adherence to guideline recommendations was particularly marked in older patients, consistent with previous reports of systematic under-treatment in this high-risk group.10–16 Whist some pharmacological interventions should be used with caution in older people, it is widely accepted that there are no circumstances in which it is safer to smoke than to use nicotine replacement therapy.17 Smoking cessation has been shown to increase the life expectancy of older patients with cardiovascular disease, and is more effective than most other interventions.18
This study has important limitations which are inherent in any epidemiological study utilising databases. Smoking status was derived from GP records, was not validated, and may only have been recorded if the patient visited the practice. Smoking cessation advice may have been provided without being recorded in the patient record; a recent pan-European cross-sectional study found smoking cessation advice was not recorded in a third of cases.19 GP recording of smoking status and of advice against smoking may have changed following the introduction in 2004 of the Quality and Outcomes Framework contract which offers financial incentives for the recording of smoking status and advice.20,21 This is a descriptive observational study and hence confounding may be present. Patients were not randomised to GP interventions, possibly leading to bias in the comparison of rates of clinical outcomes.
As this study is descriptive and retrospective, its findings are not definitive. However, the results do support future research, both in larger prospective epidemiological studies and randomised controlled trials, of the promotion of GP smoking cessation interventions, the association between interventions and cessation and the effects on long-term clinical outcomes.
This descriptive study, utilising four linked datasets, provides evidence that smoking is common amongst those hospitalised for ACS. However, despite the National Institute for Health and Clinical Excellence guidelines, few GPs offer smoking cessation advice, referral to smoking clinics, or pharmacological intervention in the 3 months following ACS discharge. Given the lower rates of major clinical outcomes, including mortality and MACE, amongst those who quit smoking following ACS, there remains a significant opportunity for GPs to actively engage smokers in cessation interventions.
Acknowledgments
Funding
This study was supported Pfizer Ltd, employees of whom were involved in the study protocol and analysis specification, interpreting the results, and drafting the manuscript.
Harry Hemingway and Adam Timmis are supported by grants from the Wellcome Trust [086091/Z/08/Z] and the National Institute for Health Research (NIHR PHR) Programme (RP-PG-0407-10314). The views and opinions expressed in this paper are those of the authors and do not necessarily reflect those of the NIHR PHR Programme or the Department of Health.
Footnotes
Conflict of interest
GPRD is owned by the UK Department of Health and operates within the Medicines and Healthcare products Regulatory Agency (MHRA). GPRD has received funding from the MHRA, Wellcome Trust, Medical Research Council, NIHR Health Technology Assessment programme, Innovative Medicine Initiative, UK Department of Health, Technology Strategy Board, Seventh Framework Programme EU, various universities, contract research organisations and pharmaceutical companies. GPRD received financial support from Pfizer in connection with the development of this manuscript.
AT and HH are committee members of the National Institute of Cardiac Outcomes Research and sit on the MINAP Advisory Group.
References
- 1.Critchley J, Capewell D. Mortality risk reduction associated with smoking cessation in patients with coronary artery disease – a systematic review. JAMA. 2003;290:86–97. doi: 10.1001/jama.290.1.86. [DOI] [PubMed] [Google Scholar]
- 2.Colivicchi F, Mocini D, Tubaro M, et al. Effect of smoking relapse on outcome after acute coronary syndromes. Am J Cardiol. 2011;108:804–808. doi: 10.1016/j.amjcard.2011.04.033. [DOI] [PubMed] [Google Scholar]
- 3.National Institute for Health and Clinical Excellence . MI: secondary prevention. 2007. (NICE clinical guideline 48). [Google Scholar]
- 4.Ashenden R, Silagy C, Weller D. A systematic review of the effectiveness of promoting lifestyle change in general practice. Fam Pract. 1997;14:160–176. doi: 10.1093/fampra/14.2.160. [DOI] [PubMed] [Google Scholar]
- 5.Silagy C. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev. 2000;(3) doi: 10.1002/14651858.CD000146. CD000146. [DOI] [PubMed] [Google Scholar]
- 6.Hughes J, Stead L, Lancaster T. Antidepressants for smoking cessation. Cochrane Database Syst Rev. 2007;(1) doi: 10.1002/14651858.CD000031.pub3. CD000031. [DOI] [PubMed] [Google Scholar]
- 7.Rigotti N, Munafo M, Stead L. Interventions for smoking cessation in hospitalised patients – review. Cochrane Database Syst Rev. 2007;(3) doi: 10.1002/14651858.CD001837.pub2. CD001837. [DOI] [PubMed] [Google Scholar]
- 8.Herrett E, Smeeth L, Walker L, et al. The Myocardial Ischaemia National Audit Project (MINAP) Heart. 2010;96:1264–1267. doi: 10.1136/hrt.2009.192328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. [accessed 22 August 2012];General Practice Research Database. gprd.com.
- 10.Kerr S, Watson H, Tolson D, et al. Smoking after the age of 65 years: a qualitative exploration of older current and former smokers’ views on smoking, stopping smoking, and smoking cessation resources and services. Health Soc Care Community. 2006;14:572–582. doi: 10.1111/j.1365-2524.2006.00659.x. [DOI] [PubMed] [Google Scholar]
- 11.Ruchlin H. An analysis of smoking patterns among older adults. Med Care. 1999;37:615–619. doi: 10.1097/00005650-199906000-00010. [DOI] [PubMed] [Google Scholar]
- 12.Kerr S, Watson H, Tolson D, et al. Developing evidence-based smoking cessation training/education initiatives in partnership with older people and health professionals. ASH; Scotland: [accessed 22 August 2012]. 2004. www.ashscotland.org.uk. [Google Scholar]
- 13.Kerr S, Watson H, Tolson D. Older people who smoke: Why nurses should help them to stop. Br J Nurs. 2002;11:1012–1020. doi: 10.12968/bjon.2002.11.15.10528. [DOI] [PubMed] [Google Scholar]
- 14.Maguire C, Ryan J, Kelly A, et al. Do patient age and medical condition influence medical advice to stop smoking? Age Ageing. 2000;29:264–266. doi: 10.1093/ageing/29.3.264. [DOI] [PubMed] [Google Scholar]
- 15.Williams D, Bennett K, Heery A, et al. Initial uptake and evidence of safe prescribing practice with Buproprion (Zyban) Pharmacoepidemiol Drug Saf. 2004;13:411–415. doi: 10.1002/pds.906. [DOI] [PubMed] [Google Scholar]
- 16.Steinberg M, Akincigil A, Delnevo C, et al. Gender and age disparities for smoking-cessation treatment. Am J Prev Med. 2006;20:405–412. doi: 10.1016/j.amepre.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 17.Joint Formulary Committee . British National Formulary. 63rd ed BMJ Group and Pharmaceutical Press; London: 2012. [Google Scholar]
- 18.Gohlke H. Is it worth offering cardiovascular disease prevention to the elderly? Eur J Cardiovasc Prev Rehabil. 2013;20:121–126. doi: 10.1177/1741826711430384. [DOI] [PubMed] [Google Scholar]
- 19.Ludt S, Petek D, Laux G, et al. Recording of risk-factors and lifestyle counselling in patients at high risk for cardiovascular diseases in European primary care. Eur J Cardiovasc Prev Rehabil. 2012;19:258–266. doi: 10.1177/1741826711400510. [DOI] [PubMed] [Google Scholar]
- 20.Department of Health . Investing in General Practice: The New General Medical Services Contract. Department of Health; London: 2004. [Google Scholar]
- 21.Coleman T, Lewis S, Hubbard R, et al. Impact of contractual financial incentives on the ascertainment and management of smoking in primary care. Addiction. 2007;102:803–808. doi: 10.1111/j.1360-0443.2007.01766.x. [DOI] [PubMed] [Google Scholar]