Abstract
Background
Recent attention to health of people with intellectual disabilities has used a health disparities framework. Building on historical context, the paper summarizes what is known about health disparities from reports and research and provide direction on what to do to reduce these disparities among adults with intellectual disabilities.
Methods
The present authors examined literature from 2002 to 2011 on health disparities and people with disabilities looking for broad themes on documenting disparities and on research approaches and methods.
Results
Multiple countries published reports on health of people with intellectual disabilities. Researchers summarized existing research within a health disparities framework. A number of promising methodologies are identified such as health services research, health indicators, enhanced surveillance and mixed-methods.
Conclusions
Strategies to reduce health disparities include use of data to educate decision makers, attention to social determinants and a life-course model and emphasis on leveraging inclusion in mainstream services where possible.
Keywords: disparities, life-course model, social determinants
Introduction
This article summarizes what is known through recent research on health disparities of people with intellectual disabilities, examines the methodological advances in recent years that are regarded as particularly promising and draws on the literature to project future directions for action to reduce these disparities. The purpose of this invited review is to reflect findings from the literature as a broad overview of the field of health disparities and intellectual disabilities in themes of research and emerging topics and methodologies; it is not a systematic review intended to answer specific questions.
What do We Know about Health Disparities of People With Intellectual Disabilities?
The health of people with intellectual disabilities has been of long-standing concern (Beange et al. 1995; Beange 1996; Kerr et al. 1996; Hand 1999; Lennox et al. 2003; van Schrojenstein Lantman-de Valk 2005), but only recently has it been cast within the framework of health disparities and inequities. For more than a century, people with disabilities were increasingly institutionalized and their medical care provided within the institution’s specialty settings (Braddock & Parish 2001). With the increase in deinstitutionalization beginning in the 1950s (Braddock & Parish 2001), responsibility for medical care of people with more severe disabilities was increasingly transferred to the community. These transfers were not always well planned and placed great pressure on community practitioners to integrate this complex population into their clinical practice, bringing their needs to the attention of public health (McGilloway & Donnelly 1999; Nottestad & Linaker 1999; Lewis et al. 2002; Cooper 2003; Lennox et al. 2003; Cornwell 2004; Janicki et al. 2004; Jansen et al. 2004).
By the early 1980s, there was a shifting in the perception of disability and health from one that was more focused on medical care to a view that was more grounded in the social context, incorporating evolving views of the role of environment in the disabling process (WHO 2001; Iezzoni & Freedman 2008; Drum 2009). Consequently, public health was recognized as central to the ongoing dialogue on disability and health (Marge 1988; Lollar & Crews 2003; Fujiura et al. 2010). In both the United States and European Union, the health of people with disabilities was formally brought to the attention of public health through national and international reports or resolutions (Degener 2005; U.S. National Council on Disability, 1986; U.N. General Assembly 1982). In 1988, the US Congress appropriated funds to the Centers for Disease Control and Prevention to improve the health of people with disabilities (Houk & Thacker 1989). During the 1990s, the international community vigorously debated the conceptualization of disability, resulting in the WHO’s International Classification of Functioning, Disability and Health (ICF) (2001). The ICF framework laid the foundation to understand ‘health condition’ as distinct from ‘disability’, to recognize the environment’s role and that of social exclusion in the disabling process and to assess health of people with disabilities using indicators that allowed comparison with the health of the general population.
Health disparities and inequities
Health disparity is essentially a public health concept. While there are multiple perspectives and definitions (Whitehead 1992; Braveman 2006; US DHHS, 2010), health disparities are frequently defined as differences in health outcomes and their determinants between segments of the population as defined by social, demographic, environmental and geographical attributes (Carter-Pokras & Baquet 2002). Health disparities exist at the population level, and their links to a history of discrimination and socio-economic or environmental disadvantage led to their being seen as avoidable and unjust (Krieger 1999). Health inequalities are a broad term used in the scientific and economic literature to refer to summary measures of population health associated with individual- or group-specific attributes (e.g. income, education or race/ethnicity) (Asada 2010). Health inequities are considered a subset of health inequalities, modifiable, but still associated with social disadvantage and concerns related to ethical justice (Braveman & Gruskin 2003). Health disparity is the term more frequently used in the United States while health inequity is used more frequently in Europe and internationally to identify preventable health inequality. Throughout this document, the present authors use the term health disparity to refer to health inequities.
In considering health disparities, the scope of health is extended beyond medical care to include health promotion and the multiple social determinants that influence health outcomes. When measuring health disparities in the context of disability, there is also a need, conceptually or statistically, to avoid including differences that are an unavoidable consequence of the primary disabling health condition (Krahn et al. 2006; Turk 2006). As examples, there are clearly established relationships between Down syndrome and early onset dementia, and between uncontrolled epilepsy and intellectual disability. At present, the higher rates of dementia or epilepsy within these populations should not be regarded as disparities. However, if health technology in the future is capable of preventing dementia or improving control of epilepsy, and these technologies are not provided to this population, then these conditions could be considered health disparities.
Intellectual disabilities
The definitions of intellectual disabilities and methods to measure its prevalence vary across countries. The most widely recognized definition of intellectual disabilities in use in the United States (AAIDD, 2010) characterizes intellectual disability as significant limitations both in intellectual functioning and adaptive behaviour as expressed in conceptual, social and practical skills that are apparent before the age of 18. Further, it requires consideration of the context of community environments typical of the individual’s age peers and culture; and cultural and linguistic diversity as well as differences in communication, sensory, motor and behavioural factors. Documentation of limitation in adaptive functioning is not required for diagnosis in many other countries (WHO, 2012).
Prevalence of intellectual disability is generally regarded as between 1 and 2% of the general population, but with considerable variability in estimates of prevalence. A recent meta-analysis of studies across 52 countries yielded a prevalence estimate of 10.37/1000, with estimates varying across income group of the country, age group of the study population and study design (Maulik et al., 2011). Variability in prevalence estimates within countries across time is also noted, attesting to the importance of study design. Based on a rigorous survey design in the United States in 1994–1995, the estimated prevalence of intellectual disability in the community dwelling population was .78% (Larson et al. 2001) to 1.27% (Fujiura & Taylor 2003)
Prevalence of intellectual disabilities in Europe has been estimated at or below 1% using variations of these definitions, with variability across countries (European Intellectual Disability Research Network, 2003). For the 15 European Union countries, this translates to between 1.1 and 1.5 million people with severe intellectual disability (IQ < 50) and an additional 2.3–2.7 million people with mild intellectual disability (IQ approximately 50–70). More recent estimates for the general population in England are closer to 2% (Emerson et al. 2012), while 2003 estimates in Australia are 3% (AIHW, 2008).
Attention to prevalence rates is important from a public health perspective, although may be less significant for research or clinical treatment. Increases in prevalence rates raise concerns about underlying environmental or societal contributors to a condition (e.g. current debate about increasing rates of diagnosed autism) or improved case ascertainment; decreases can relate to environmental improvements or diagnostic changes (e.g. revised diagnostic criteria, diagnostic substitution).
Methods
To determine what is currently known about health disparities of adults with intellectual disabilities, the present authors reviewed articles identified through a literature search to identify themes in research and reports covering the years 2002–2011. Boolean search strategies were used to look for articles of interest with the search terms: intellectual disabilities, mental retardation, developmental disabilities, access to healthcare services, utilization of healthcare services and intellectual disability surveillance. Databases accessed for these search terms were PubMed, Academic Search Premier, ProQuest, CINAHL Plus, PsycARTICLES (2005–2010 only) and PsycINFO. To ensure that key literature in the area of intellectual disabilities and healthcare services was captured, the reference lists of the leading studies were reviewed for additional articles. Further, Google and Google Scholar were used to search the internet for related government and non-governmental agency reports. Identified titles and articles were reviewed for relevance to the current topic, and selected articles were reviewed in full. Our intent was to provide a broad perspective on themes and trends relating to health disparities and intellectual disabilities and not to present a focused systematic review designed to answer one or more specific questions.
Findings
National reports
In the past decade, there was a near simultaneous emergence of reports from multiple countries on the health of people with intellectual disabilities. In 2001, the United Kingdom published ‘Valuing People’ as a comprehensive plan to improve the health and well-being of people with learning disabilities and their caregivers (UK DOH, 2001). In 2002, the US Surgeon General published ‘Closing the Gap: A National Blueprint to Improve the Health of Persons with Mental Retardation’ (US DHHS, 2002); and, in that same year, Scotland released ‘Promoting Health, Supporting Inclusion: The National Review of the Contribution of all Nurses and Midwives to the Care and Support of People with Learning Disabilities’ (SEHD 2002). Through government support, the New South Wales Council for Intellectual Disability in Australia published ‘Health and People with Intellectual Disability’ in 2003 (NSWCID 2003), and in 2004, a workgroup in Canada published ‘Addressing Health Disparities through Promoting Equity for Individuals with Intellectual Disability’ (Ouellette-Kuntz et al. 2005).
This confluence of governmental attention to the health of people with disabilities in such a short time period is noteworthy. These reports used differing frameworks but yielded similar core recommendations. These recommendations can be summarized as follows: (i) promote early identification, inclusion and self-determination of people with intellectual disability; (ii) prevent and manage the occurrence and impact of health conditions; (iii) empower caregivers and family members to adequately meet the needs of persons with intellectual disabilities in their care; and (iv) promote healthy behaviours in people with intellectual disabilities (see Krahn et al. 2006). This work occurred in the context of considerable attention to reducing health inequalities for populations identified by race/ethnicity or geographical regions. However, people with disabilities, particularly intellectual disabilities, have generally not been the focus of attention, nor explicitly included in these health disparity efforts (e.g. Emerson et al. 2011).
Research literature
From approximately 2004 onward, the professional literature reflects a series of scholarly articles that summarizes research on health disparities of people with intellectual disabilities, demonstrating the wealth of valuable literature on health status and need for improved health care. There were at least seven review papers that relate to a health disparities framework (Fisher 2004; Graham 2005; Ouellette-Kuntz 2005; Scheepers et al. 2005; Krahn et al. 2006; Shogren et al. 2006), including the Journal of Applied Research on Intellectual Disabilities’ special issue on this topic in 2005 (e.g. Emerson & Durvasula 2005). One paper was published in 2004, four in 2005 and two in 2006. The publication from the workgroup of the International Association for the Scientific Study of Intellectual Disabilities (IASSID) (Scheepers et al. 2005) outlined the steps needed to reduce health disparities, and Shogren et al. (2006) emphasized the importance of maintaining self-determination in efforts to reduce health disparities. The other papers provide extensive summaries of previous studies, each paper reflecting different breadth or focus, but all demonstrating the complexities of considering health disparities within the context of pre-existing disability. Their findings, not surprisingly, reached similar conclusions of significant health differences and disparities, with recommendations for research, practice and training.
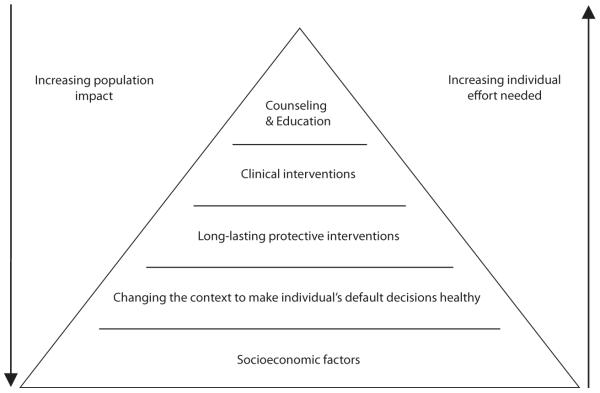
In the review paper the first author wrote with colleagues in 2006, findings of previous studies until that time were summarized as representing a ‘cascade of disparities’ (Figure 1).
Figure 1.
“Cascade of Disparities” leading to poor health outcomes in adults with intellectual disabilities.
At the top of this cascade is the finding that people with intellectual disabilities as a group have higher rates of adverse health conditions such as epilepsy and neurological disorders, gastrointestinal disorders and behavioural/psychiatric problems. These conditions put people’s health at greater risk. Some of these conditions may not be preventable but, instead, relate to the primary health condition that results in the disability; others likely are preventable or amenable to improved care. This distinction about the aetiology of the difference is an important one to make to avoid confusing observed health differences with preventable health disparities. All the rest of the differences that follow in the cascade, however, are presumed to be preventable. This includes the problem that people with intellectual disabilities or their caregivers are not sufficiently communicative or attentive to problems with their health. For example, systematic health checks showed high rates of undetected vision or hearing loss among adults with intellectual disabilities (Kerr et al. 2003; Woodhouse et al. 2004). These disparities are compounded with disparities in use of preventive care and engaging in healthy behaviours such as physical activity and good oral hygiene practices. Collectively, these problems add to disparities in equitable access to health care, like management of chronic conditions such as hypertension and diabetes (Janicki et al. 2002). Living situation was also observed to have an important effect throughout this cascade, as indicated in the attention of carers to health status (Lewis et al. 2002). The end result of these cascading disparities is poor health outcomes observed in people with intellectual disabilities.
A major shortcoming of the earlier research is that most, if not all, of these ‘disparity’ findings were not based on true population data—they were typically based on convenience samples. Sometimes these were very large samples, such as the Special Olympics Healthy Athletes, but they were not based on data that are known to be representative of the population of all people with intellectual disabilities. As a result, while these findings brought attention to the dire health problems of this population, they were often not sufficiently compelling to make the case for sustained attention by policymakers.
Promising strategies to improve data
The literature from the past 5 to 7 years demonstrates substantial efforts to improve the data. The present authors highlight four of these strategies that appear particularly promising: health services research, population health indicators, health surveys and mixed-methods approaches.
Expanding health services research
Health services research is an important methodological advance for the study of the health of people with intellectual disabilities. It is the multidisciplinary investigation of how social factors, financing systems, organizational structures and processes, health technologies and personal behaviours affect access to health care, the quality and cost of health care, and ultimately health and well-being (Lohr & Steinwachs 2002). Health services research includes analyses of administrative data of entire health systems to understand service utilization patterns and outcomes—who is using what services? at what cost? and where possible, to what effect? The advantages of using administrative data are that they are typically collected in an ongoing way, and they encompass a defined population, even if not the entire population of interest. The utility of health services research is very dependent on the variables in the data sets, how readily the data systems can be manipulated, and whether the sets contain the codes needed to identify the population of interest. There are unique complexities relating to whether and how the data systems identify intellectual disabilities. People with intellectual disabilities may be difficult to differentiate from people with emotional problems or those with traumatic brain injury or dementia.
Health services research has been used effectively by researchers in documenting disparities in breast cancer treatment and survival in women with disabilities (McCarthy et al. 2006). Lin et al. (2003, 2004) were early users of health services research with people with intellectual disabilities specifically, reporting on service utilization of people with intellectual disabilities in Taiwan. They continue to use this methodology to publish on a series of topics such as dual diagnosis (Lai et al. 2011), prescription drug use (Yen et al. 2009) and elder healthcare use (Hsu et al. 2012). Balogh et al. (2010) used health services research methods to examine access to quality health care for people with intellectual disabilities. Using the linked data sets from the Manitoba data repository, their analyses showed that adults with intellectual disabilities were more likely to be hospitalized for conditions that should be manageable on an outpatient basis—ambulatory care sensitive conditions. By demonstrating higher rates of hospitalization for asthma and diabetes, even when rates were adjusted for prevalence of those conditions in the respective populations, they argued this was a disparity that indicated poorer access to quality primary care. Related work has compared algorithms for identifying individuals with intellectual disabilities using administrative data (Lin et al. 2012). In two studies, Reichard & Stolzle (2011), Reichard et al. (2011) identified significantly higher rates of diabetes among people with cognitive limitations compared with those without, additionally demonstrating a strong link to other and multiple chronic conditions. Health services research provides fundamental data on service use that can identify where to take action to improve primary health care for people with intellectual disabilities. As cost-effectiveness and improvements in quality of care are demonstrated for subsets of people with disabilities using electronic health records with more widespread interoperability (Gilmer et al. 2012), the present authors anticipate that health services research will increasingly provide a means of conducting surveillance and epidemiological research through its analysis of secondary data.
Improving health indicators
A second important development in improving health disparities data is the use of health indicators. Broadly considered, a health indicator is a variable that reflects or indicates the state of health of persons in a defined population that can be used to monitor progress or assess what works and what does not (Murray 2007). Ideally, health indicators are reliably measureable (e.g. body mass index), population relevant (e.g. vaccination rates) and sensitive to change (e.g. mammogram in past 2 years). Using carefully selected variables, these health indicators can provide a good reflection of population overall health, without requiring more comprehensive assessment of health or health care. To demonstrate health disparities, the variables selected as health indicators for special populations should be relevant for general populations (e.g. vaccination rates) and not unique to the special population (e.g. rehabilitation treatment). Different health indicator sets have been proposed for different purposes (IOM 2009; Butler et al. 2012). Two major initiatives determined health indicators for intellectual disability populations: the National Core Indicators (NCI) project in the United States and the Pomona project in Europe. Both are based on surveys of populations and are described in greater detail.
National Core Indicators Project (United States)
NCI (Smith & Ashbaugh 2001) was begun in 1997 to establish a performance measurement framework for state developmental disabilities services. The framework addresses a number of major domains (individual outcomes; health, welfare and rights; system performance; staff stability; family indicators), each with subdomains and corresponding indicators, measures and data sources. The health, welfare and rights domain addresses healthcare services, health behaviours, medication rates, safety considerations, rights protection and use of restraints. Participation in the National Core Indicators system is voluntary by states and has varied somewhat across the years, but as of January 2012, up to 35 states had participated in this ongoing indicators programme (NCI 2012).
Pomona project (Europe)
Pomona (Walsh et al. 2003) was begun prior to 2002 through collaboration among 13 European countries to identify health indicators for people with intellectual disabilities (van Schrojenstein Lantman-de Valk et al. 2007; Walsh 2008; Haveman et al. 2011). Importantly, they worked within an established indicators framework, the European Community Health Indicators. The Pomona collaborators agreed on 18 health indicators: demographics (prevalence of intellectual disability, living arrangements, daily occupation, income/SES, life expectancy); health status (epilepsy, oral health, body mass index, mental health/psychiatric disorder, sensory capacities, mobility); determinants of health (physical activity, challenging behaviours, psychotropic medications); and health systems (hospitalization and contact with healthcare professionals, health checks, health promotion, specific training for physicians). Teams then demonstrated the feasibility of implementing the indicators framework across these countries, laying the groundwork for a potentially sustainable system in the future.
Table 1 presents a crosswalk of these two indicator sets with the framework and indicator set proposed by the Institute of Medicine (2009) to demonstrate their comparability (adapted from Krahn et al. 2010). The domains in the framework consider indicators of mortality, health-related quality of life, outcomes, behaviours, systems and environment. The present authors observe reasonably comparable weighting across frameworks on many of the categories of indicators. NCI indicators are less focused on health outcomes, while providing more information about systems performance. The IOM framework acknowledges the importance of environmental factors, but it did not provide indicators for that domain, while both the Pomona and the NCI frameworks provide three and five indicators, respectively.
Table 1.
Cross-walk of health indicators across Institute of Medicine, Pomona project, and National Core Indicators
| Health indicators – Crosswalk of measures |
|||
|---|---|---|---|
| Indicator set | Institute of Medicine (U.S.) |
Pomona (Europe) |
National Core Indicators |
| Domain | |||
| Mortality | 2 | 1 | 2 |
| HRQOL | 2 | 2 | 1 |
| Outcomes | 7 | 6 | 1 |
| Behaviours | 6 | 6 | 6 |
| Systems | 7 | 4 | 12 |
| Environment | – | 3 | 5 |
|
| |||
| Unique to ID | Secondary conditions Under/over-medication Access to advocacy Communication supports |
||
Enhancing health surveillance
The third strategy in improving data collection is population surveillance as a means of obtaining population-level data on health of people with intellectual disabilities. Health surveillance differs from clinical or convenience sampling where the method used to identify participants introduces bias in who will participate. In population surveillance, every person in the category under study ideally would have an equal opportunity to provide data, with the sample drawn randomly from that population. Two strategies are evident in the recent literature:
Special disability surveys
Several countries have conducted population-level surveys specific to disabilities (see Fujiura et al. 2010). Of note, these surveys typically do not sample from institutionalized populations. The surveys include as follows: in the USA, the 1994–1995 National Health Interview Survey—Disability Supplement; in Australia, the Survey of Disability, Ageing and Carers in 1998 and 2003; in China, the National Sample Survey on Disability in 2006; and in Ireland, the National Disability Survey in 2006. These surveys measure variables of targeted relevance for people with disabilities. Unfortunately, unless these special surveys are repeated regularly, they do not provide current data or trend-line data. An exception to this is the UK Life Opportunities Survey, a longitudinal cross-disability survey initiated in 2009. It has recently collected the second wave of data from a representative sample of people with disabilities that documents the dynamic nature of disability (Office of National Statistics 2012) and allows analyses for specific topics such as barriers to health care (Allerton & Emerson 2012). WHO is currently developing a disability module and UNICEF in conjunction with the Washington Group are working to improve disability identification in children; both activities hold promise for better surveillance in the future (WHO 2013).
Disability inclusion in public health surveys
An alternative survey approach is to include intellectual disability identifiers in general health surveys that contain variables relevant to people with disabilities. Two papers recently reviewed this approach. Linehan and others from the Pomona-1 Group (2009) reviewed 123 European health surveys. They found that 16 of 18 Pomona indicators were represented in the surveys. However, only 8% of the surveys clearly identified respondents with intellectual disability. Fujiura et al. (2010) reviewed 131 national systems from 12 countries in eight global regions. They found that about 25% of the data systems coded for intellectual disability. However, the authors cautioned about quality of the data and the use of differing definitions of disability across surveys. A major limitation of most US public health surveillance systems is that they gather information on household or non-institutionalized populations. This sampling frame excludes people living in institutions as well as group residential settings, affecting many adults with significant intellectual disabilities. A recent development of interest for the United States is the legislatively mandated development of standard disability identifier questions for use in public health surveys (Madans et al. 2011). This 6-question set will include the question: ‘Because of a physical, mental or emotional condition, do you have serious difficulty concentrating, remembering or making decisions?’ for respondents 5 years old or older. While this question will capture persons with intellectual disabilities, it will not distinguish intellectual disabilities from other conditions like dementia, traumatic brain injury or mental health problems.
Developing mixed-methods approaches
In a recent effort in the United States, the Centers for Disease Control and Prevention partnered with the Association of University Centers for Disability to identify methods to improve the health surveillance data for people with intellectual disabilities (Krahn et al. 2010). With input from international colleagues, the present authors developed a five-step process to operationally define intellectual disabilities for use with administrative data sets, test its implementation, summarize current knowledge and extend analyses of extant data sets to determine methods and gaps that future surveillance systems can use and address. Initial progress has included establishing conceptual and operational definitions for administrative data sets and recommended procedures for finding people with intellectual disabilities in data sets (Bonardi et al. 2011).
In the United Kingdom, researchers affiliated with the Improving Health and Lives: Learning Disabilities Observatory (2012) have used mixed-methods, combining administrative data with census data and statistical forecasting to project prevalence for adults with profound multiple learning disabilities (PMLD) (Emerson 2009). The steps required were identifying number of children with special educational needs associated with PMLD, estimating number of children with PMLD in England who would reach 18 years of age between prescribed years, estimating number and age profile of adults with PMLD in England in a given year, adjusting the population of adults with PMLD for the expected effects of mortality over the projected time period and combining data with estimated inflows from child services to estimate net changes over the period 2009–2026. Using these techniques, projected annual increases by 1.8% were identified over this time period.
Emerging and re-emerging issues
Ageing and transition
Ageing of persons with intellectual disabilities has been an area of study for many years and is re-emerging as a topic of increased focus in recent years (Innes et al. 2012). The increasing lifespan of people with disabilities is putting significant pressure on service delivery systems to accommodate a growing number of older people with disabilities. Projections indicate that the current shortfalls in service delivery systems will be greatly magnified without systemic changes. In addition to unique needs, the ageing population of people with disabilities also experiences the typical health concerns of the general ageing population, with growing rates of obesity and other chronic conditions. A review by a study group of the IASSID’s Ageing Special Interest Group considered the range of issues that need to be addressed to promote healthy ageing for this population and serves as an excellent resource for future planning (Haveman et al. 2010).
Chronic conditions
Chronic conditions are now the major threat to health of the general population in terms of morbidity, mortality and cost. The emerging morbidity of multiple chronic conditions is anticipated to account for up to 80% of healthcare expenditures in developed countries by 2020 (WHO 2002). Chronic conditions include noncommunicable diseases (NCDs), mental disorders and certain communicable diseases such as HIV/AIDS that are of long duration (WHO 2002, 2011a,b). The World Health Organization reports that 63% of global deaths in 2008 were due to NCDs, primarily cardiovascular diseases, diabetes, cancers and chronic respiratory diseases (WHO 2011a,b), with the impact of NCDs felt disproportionately in low- and middle-resourced populations. In the United States, a recently published government report for the Medicare programme [public funding for the over age 65 population and for some people with significant disabilities (dual eligibles)] determined that the 15 top chronic conditions accounted for $260 billion of the total $280 billion spent in 2008 (US DHHS CMS 2011). Major behavioural contributors to these conditions are tobacco use, harmful use of alcohol, physical inactivity and unhealthy diet, the effects of which are also reflected in high rates of obesity.
People with disabilities, including intellectual disabilities, are at substantially higher risk for obesity and other chronic conditions and may be experiencing them at younger ages. As in the general population, the occurrence of multiple chronic conditions compounds the impact on health status. Reichard & Stolzle (2011) illustrated this using the Medical Expenditure Panel Survey, a nationally representative sample in the United States. Their findings show that adults with cognitive disabilities have dramatically higher rates of chronic conditions than adults without disabilities. Notably, they are almost five times more likely to have diabetes, almost three times more likely to have arthritis and more than twice as likely to have cardiovascular disease and asthma. These are not conditions that have an obvious causal relationship with cognitive disability, suggesting that poor health behaviours (e.g. sedentary lifestyles, poor nutrition), inadequate attention by carers and healthcare providers (e.g. obesity, poor management of chronic conditions), and other underlying health-influencing factors (e.g. prenatal influences, chronic lifelong stress) are underlying these seriously elevated rates of chronic conditions.
As the population of people with intellectual disabilities ages, the present authors anticipate seeing a substantial increase in the rates of chronic conditions and their relative impact on health. While management of conditions more unique to intellectual disabilities (e.g. epilepsy) will continue to be important, the successful prevention and management of conditions such as diabetes, hypertension and cardiovascular disease will represent the major avenues for improving health of people with intellectual disabilities across their life course.
What Can We Do to Reduce These Health Disparities?
In 1958, Sir Charles Geoffrey Vickers stated: ‘The landmarks of political, economic and social history are the moment when some condition passed from the category of the given into the category of the intolerable. I believe that the history of public health might well be written as a record of successive redefining of the unacceptable’.
The present authors contend that we are in the midst of just such a time of redefinition: the governments of many countries recognize the need to improve the health of people with intellectual disabilities; the research literature documents the poor health status and health disparities of people with intellectual disabilities; efforts are underway to improve surveillance of the health of people with intellectual disabilities; and heightened awareness to issues like ageing, obesity and chronic conditions are extended to people with intellectual disabilities. These combined forces are demanding a change from accepting the poor health of people with intellectual disabilities as a given, to regarding these health disparities as intolerable.
Earlier recommendations from previous governmental reports as summarized above outline the general issues to address and can be used as a road map for future actions. In this section of the article, the present authors focus on the methods for how to approach these actions. To undertake these activities, the present authors propose researchers and policy-makers use data to drive action; address health determinants as well as disparities; regard health across the life course; and use mainstream inclusion approaches where possible.
Data to drive action
The successes of the past decade are the prologue to future approaches. Using science to shape practice and policy underlies much of the work in medicine and public health over the past decades. The evidence base for practices is a standard that is increasingly expected, and emphasis on evidence will likely continue to be a major requirement, particularly in the United States, while a rights-based approach incorporating improved data collection may continue to drive more of the global work on equity for persons with disabilities. The present authors also anticipate ongoing efforts to improve surveillance, so that resulting data can be used to monitor status and measure intervention effectiveness. Health indicators have proven a useful means of documenting value, and more pressure to strategically select existing indicators or develop new ones that can demonstrate the effect of interventions is anticipated. Equally important are developing new surveillance and sampling strategies that can be used to more inclusively identify people with intellectual disabilities across the life course. Researchers have perhaps been most effective when they have anticipated where policy opportunities will arise in the future and have framed their research to provide the data in a timely way.
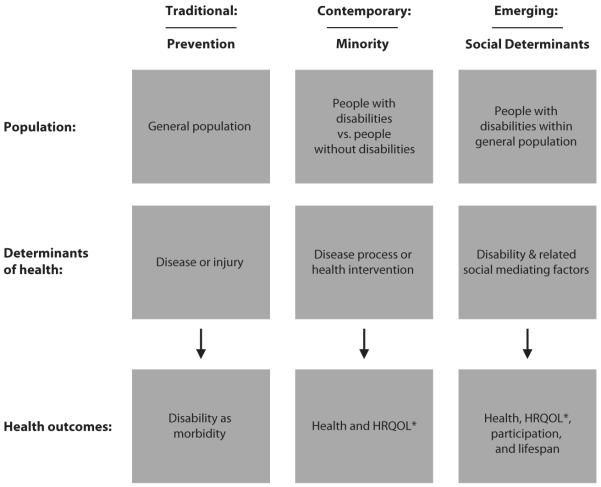
Increased reliance on data provides opportunities to measure and maximize impact of interventions. Frieden (2010) proposed the health impact pyramid (see Figure 2). As applied to this population, it indicates greatest impact when intervention focuses on the bottom of the pyramid on socio-economic factors (e.g. equitable access to health care), changing the context so that people’s default decisions are healthy ones (e.g. improving nutrition for group home menus) and investing in protective interventions that have long-lasting outcomes (e.g. immunizations). On the contrary, most effort is required with least impact when efforts focus on counselling and education methods or on individual clinical interventions.
Figure 2.
Health impact pyramid for public health.
Addressing health determinants and disparities
Health determinants are the personal, social, economic and environmental factors that influence population health status. Determinants include gender and genetics; individual behaviours; social circumstances, supports and opportunities; the economic situation broadly and people’s place within the economic strata, including poverty; and the environment as reflected in natural, interpersonal and architectural, barriers and exposures (McGinnis et al. 2002; U.S. Department of Health & Human Services 2010). Emerson & Hatton (2007) and Graham (2005) have informed the field on health determinants and intellectual disabilities for more than a decade. Further, the recently released report from the UK Observatory on Health Inequities provides an excellent summary of recent research findings on many chronic conditions and social determinants for persons with intellectual disabilities. In the United States, the Healthy People 2020 document published in 2010 frames public health outcomes for the coming decade within a determinants framework, departing from the disparities framework of a decade ago (U.S. Department of Health & Human Services 2010).
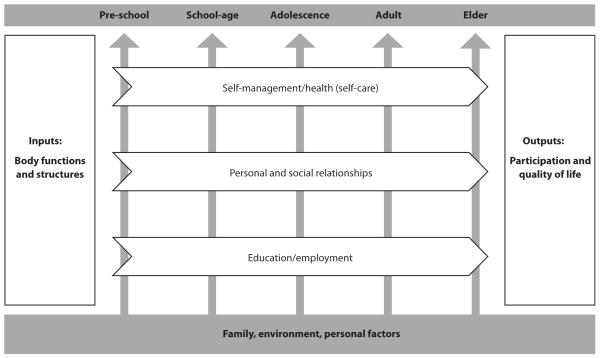
A health determinants perspective has important implications for how disability is viewed within public health. Figure 3 presents three historical views of disability within public health, with the latter representing a social determinants view (Drum et al. 2009; Krahn & Campbell 2011). While a traditional public health approach focuses on primary prevention of disability and a minority model looks for disparities between people with and without disabilities, a determinants view regards people with disabilities as part of the general population. Disability is one of multiple risk factors for poor outcomes, much like poverty and social isolation. This reflects a shift from dichotomizing a population into people with and without disabilities and documenting differences, to considering the population as a whole and examining the influence of multiple determinants—including disability status—on health outcomes such as health, health-related quality of life (HRQOL) and social participation in addition to traditional morbidity and mortality measures. A social determinants perspective supports analyses that examine the association of disability as an independent variable on various health outcomes. Rather than controlling for factors like age or income, this approach would expand our ability to examine the unique and interactive role that disability contributes to various health outcomes. The implications of this are in a broader systemic ability to more effectively target public health interventions around the needs of disability populations in general and intellectual disability subpopulations in particular.
Figure 3.
Three views of disability within public health: traditional, contemporary, emerging.
* HRQOL = health-related quality of life.
Life-course model of health and disability
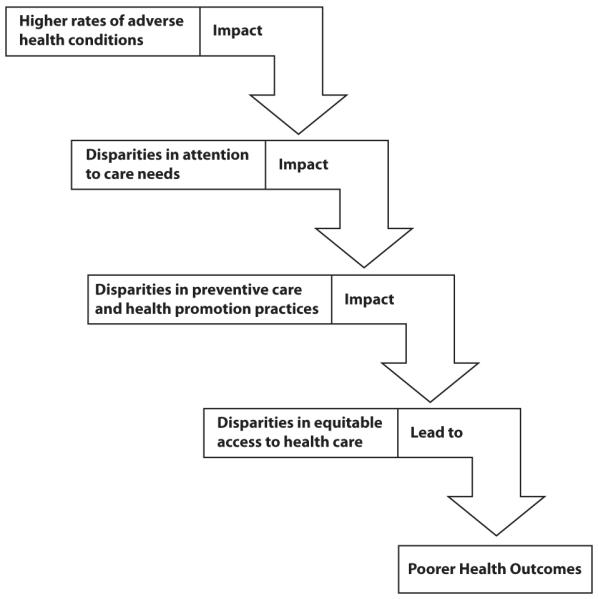
A life-course perspective of health inequities has been reflected in the literature for a long time (e.g. Graham 1982), but the past decade has witnessed a resurgence of interest as applied to current health issues (e.g. WHO 2000; Ben-Shlomo 2002). A life-course perspective recognizes that health trajectories are particularly affected at certain times in life, that health disparities result from the cumulative impact of experiences in the past and the present, that the environment affects the capacity to be healthy and function effectively in society and that health disparities reflect inequities that go beyond genetics and personal choice (US DHHS HRSA/MCH, 2010). Environment is broadly considered to include not only the physical environment, but also social factors that shape our experiences such as culture, geography, family, economics and policies. Environmental factors significantly affect health-related and functional outcomes and can foster or impede good health and high quality of life (World Health Organization 2001). Moreover, the earlier the onset of disability, the more likely it will affect a person’s health and development across their life course. Using a life-course perspective, Swanson (2010) has explicated the developmental tasks for persons with disabling conditions to achieve successful transition to adulthood. An adaptation of this life-course model is presented in Figure 4.
Figure 4.
Life-course model of disabilities.
This model is based on the ICF framework (World Health Organization 2001) and considers the core domains of self-management/health, personal and social relationships, education and employment for different life phases, including elders. The model considers the inputs of body functions and structures, the context of family, environment and personal factors, and promotes attention to the outcomes of participation and quality of life. Emphasis has been on the experiences and competencies acquired in these different life stages that support successful transitioning to the next life stage. Examples include as follows: health self-care such as toothbrushing or capacity to manage medication; adequate nutrition among people with intellectual disabilities at different stages of life, factoring in functionality and capacity to select and prepare food; capacity to develop and maintain friendships; how one is able to move about and use transportation; use of telephone and electronic messaging; and meaningful life activities such as education, recreation, employment and volunteering.
Mainstream inclusion
When do planners and interventionists use a mainstream inclusion approach, a cross-disability approach, or an intellectual disability-specific approach? This is an important strategic question. By some definitions of disability, about 85% of the population does not report a disability, with 15% of the population reporting some functional limitation. Only about 1–2% of the general population has an intellectual disability, and approximately one-half per cent are known by administrative systems to have significant intellectual disability and need for supports (e.g. Ouellette-Kuntz et al. 2009; Sondenaa et al. 2010). Policymakers across the board are faced with the dual challenges of decreasing resources and increasing service demands. Current circumstances press the questions: When can intellectual disability stakeholders leverage the resources of the generic systems? When do they partner with the broader, cross-disability community to have their needs met? And when are the issues of intellectual disabilities so unique that they need to be addressed specially?
The World Health Organization, in its in World Report on Disability (2011b), advocates for a ‘mainstream’ approach where possible, recognizing that disability-specific services will also be necessary. Strategic actions can use inclusion in the mainstream services where possible, to promote a cross-disabilities approach where necessary and only to use a condition-specific approach where that is essential. There are needs and situations where the approach needs to be specific to persons with intellectual disabilities, but disability advocates can seek opportunities to ally with other initiatives for the general population and for other disability groups that will advance the health and reduce the health disparities of people with intellectual disabilities. The present authors encourage researchers, policymakers and programme planners to adopt approaches that use science to direct action, recognize the multiple determinants of health and health disparities, understand health from a life-course perspective and strategically leverage inclusion and cross-disability approaches where possible.
Summary
This article is intended to provide a broad understanding of the contemporary and emerging views and approaches to health and health disparities, of the contribution that public health is making to identify and address health disparities, to note the progress made through government reports and professional literature on health disparities, to recognize some of the emerging methodologies to improve health surveillance data and to acknowledge the important concerns of ageing and of chronic conditions.
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. The authors are grateful to Ismaila Ramon who conducted the literature search and to Eric Emerson and Helene Ouellette-Kuntz who provided comments to an earlier draft of this article.
References
- Allerton L, Emerson E. [accessed on 10 November 2012];Individuals With Impairments Face Significant Barriers to Accessing Health Services in the United Kingdom. Public Health. 2012 doi: 10.1016/j.puhe.2012.08.003. Available at: http://dx.doi.org/10.1016/j.puhe.2012.08.003) [DOI] [PubMed]
- American Association on Intellectual and Developmental Disabilities (AAIDD) Intellectual disability: Definition, classification, and systems of supports. American Association on Intellectual and Developmental Disabilities; Washington, DC: 2010. [Google Scholar]
- Asada Y. [accessed on 15 December 2012];A summary measure of health inequalities for a pay-for-population performance system. Preventing Chronic Disease. 2010 7 http://www.cdc.gov/pcd/issues/2010/jul/09_0250.htm. [PMC free article] [PubMed] [Google Scholar]
- Australian Institute of Health and Welfare . Disability in Australia: Intellectual Disability. AIHW; Canberra: 2008. AIHW bulletin no. 67. Cat. no. AUS 110. [Google Scholar]
- Balogh R, Brownell M, Ouellette-Kuntz H, Colantonio A. Hospitalization rates for ambulatory care sensitive conditions for persons with and without an intellectual disability –a population perspective. Journal of Intellectual Disability Research. 2010;54:820–832. doi: 10.1111/j.1365-2788.2010.01311.x. [DOI] [PubMed] [Google Scholar]
- Beange H. Caring for a vulnerable population: Who will take responsibility for those getting a raw deal from the health care system? Medical Journal of Australia. 1996;164:159–160. doi: 10.5694/j.1326-5377.1996.tb122016.x. [DOI] [PubMed] [Google Scholar]
- Beange H, McElduff A, Baker W. Medical disorders of adults with mental retardation: A population study. American Journal on Mental Retardation. 1995;99:595–604. [PubMed] [Google Scholar]
- Ben-Shlomo Y. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. International Journal of Epidemiology. 2002;32:285–293. [PubMed] [Google Scholar]
- Bonardi A, Lauer E, Mitra M, Bershadsky J, Taub S, Noblett C. Expanding Surveillance of Adults with Intellectual Disability in the US. Center for Developmental Disabilities Evaluation and Research (CDDER), E.K. Shriver Center University of Massachusetts Medical School. A technical report submitted to the U.S. Centers for Disease Control and Prevention; 2011. [Google Scholar]
- Braddock DL, Parish SL. An institutional history of disability. In: Albrecht GL, Seelman KD, Bury M, editors. Handbook of Disability Studies. Sage Publications; Thousand Oaks, CA: 2001. pp. 11–68. [Google Scholar]
- Braveman P. Health disparities and health equity: Concepts and measurement. Annual Review of Public Health. 2006;27:176–194. doi: 10.1146/annurev.publhealth.27.021405.102103. [DOI] [PubMed] [Google Scholar]
- Braveman P, Gruskin S. Defining equity in health. Journal of Epidemiology and Community Health. 2003;57:254–258. doi: 10.1136/jech.57.4.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler M, Kane RL, Larson S, Jeffery MM, Grove M. Quality Improvement Measurement of Outcomes for People With Disabilities. Closing the Quality Gap: Revisiting the State of the Science. Agency for Healthcare Research and Quality; Rockville, MD: [October 2012]. 2012. Evidence Report/Technology Assessment No. 208. (Prepared by the Minnesota Evidence-based Practice Center under Contract No. 290-2007-10064-I.) AHRQ Publication No. 12(13)-E013-EF. www.effectivehealthcare.gov/reports/final.cfm. [PMC free article] [PubMed] [Google Scholar]
- Carter-Pokras O, Baquet C. What is a “health disparity”? Public Health Reports. 2002;117:426–434. doi: 10.1093/phr/117.5.426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper SA. Meeting the mental health needs of older adults with intellectual disabilities. Aging and Mental Health. 2003;7:411–412. doi: 10.1080/13607860310001594646. [DOI] [PubMed] [Google Scholar]
- Cornwell KL. People with intellectual disabilities: People registered disabled with learning difficulties tend to fall through the net.[comment] British Medical Journal. 2004;329:917. doi: 10.1136/bmj.329.7471.917-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degener T. Disability discrimination law: A global comparative approach. In: Lawson A, Gooding C, editors. Disability Rights in Europe: From Theory to Practice. Hart Publishing; Portland: 2005. pp. 87–106. [Google Scholar]
- Drum CE. Models and approaches to disability. In: Drum CE, Krahn GL, Bersani H, editors. Disability and Public Health. American Public Health Association & American Association on Intellectual and Developmental Disabilities; Washington, DC: 2009. pp. 27–44. [Google Scholar]
- Drum CE, Krahn GL, Peterson JJ, Horner-Johnson W, Newton K. Health of people with disabilities: Determinants and disparities. In: Drum CE, Krahn GL, Bersani H, editors. Disability and Public Health. American Public Health Association & American Association on Intellectual and Developmental Disabilities; Washington, DC: 2009. pp. 125–144. [Google Scholar]
- Emerson E. Estimating Future Numbers of Adults with Profound Multiple Learning Disabilities in England: CeDR Research Report 2009(1) Centre for Disability Research, Lancaster University; Lancaster: 2009. Working Paper. [Google Scholar]
- Emerson E, Durvasula S. Health inequalities and people with intellectual disabilities: An introduction to the special issue. Journal of Applied Research in Intellectual Disabilities. 2005;18:95–96. [Google Scholar]
- Emerson E, Hatton C. Contribution of socioeconomic position to health inequalities of British children and adolescents with intellectual disabilities. American Journal on Mental Retardation. 2007;112:140–150. doi: 10.1352/0895-8017(2007)112[140:COSPTH]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Emerson E, Madden R, Graham H, Llewellyn G, Hatton C, Robertson J. The health of disabled people and the social determinants of health. Public Health. 2011;125:145–147. doi: 10.1016/j.puhe.2010.11.003. [DOI] [PubMed] [Google Scholar]
- Emerson E, Hatton C, Robertson J, Roberts H, Baines S, Evison F, Glover G. Learning Disabilities Observatory. Improving Health and Lives (IHAL); UK: 2012. People with Learning Disabilities in England 2011. [Google Scholar]
- European Intellectual Disability Research Network . Intellectual Disability in Europe: Working Papers. Tizard Center, University of Kent at Canterbury; Canterbury: 2003. [Google Scholar]
- Fisher K. Health disparities and mental retardation. Journal of Nursing Scholarship. 2004;36:48–53. doi: 10.1111/j.1547-5069.2004.04010.x. [DOI] [PubMed] [Google Scholar]
- Frieden T. A framework for public health action: The health impact pyramid. American Journal of Public Health. 2010;100:590–595. doi: 10.2105/AJPH.2009.185652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fujiura GT, Taylor SJ. Continuum of intellectual disability: demographic evidence for the “Forgotten Generation”. Mental Retardation. 2003;41:420–429. doi: 10.1352/0047-6765(2003)41<420:COIDDE>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Fujiura GT, Rutkowski-Kmitta V, Owen R. Make measurable what is not so: National monitoring of the status of persons with intellectual disability. American Journal of Intellectual and Developmental Disabilities. 2010;35:244–258. doi: 10.3109/13668250.2010.519330. [DOI] [PubMed] [Google Scholar]
- Gilmer TP, O’Connor PJ, Sperl-Hillen JM, Rush WA, Johnson PE, Amundson GH, Asche SE, Ekstrom HL. Cost-effectiveness of an electronic medical record based clinical decision support system. Health Services Research. 2012;47:2137–2158. doi: 10.1111/j.1475-6773.2012.01427.x. doi:10.1111/j.1475-6773.2012.01427.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham H. Building an inter-disciplinary science of health inequalities: The example of lifecourse research. Social Science and Medicine. 1982;55:2006–2016. doi: 10.1016/s0277-9536(01)00343-4. [DOI] [PubMed] [Google Scholar]
- Graham H. Intellectual disabilities and socioeconomic inequalities in health: an overview of research. Journal of Applied Research in Intellectual Disabilities. 2005;18:101–111. [Google Scholar]
- Hand J. The care of individuals with mental retardation: lessons from the New Zealand experience. International Review of Psychology. 1999;11:68–75. [Google Scholar]
- Haveman M, Heller T, Lee L, Maaskant M, Shooshtari S, Strydom A. Major health risks in aging persons with intellectual disabilities: an overview of recent studies. Journal of Policy and Practice in Intellectual Disabilities. 2010;7:59–69. [Google Scholar]
- Haveman M, Perry J, Salvador-Carulla L, Walsh PN, Kerr M, Van Schrojenstein Lantman-de Valk H, Van Hove G, Berger DM, Azema B, Buono S, Cara AC, Germanavicius A, Linehan C, Määttä T, Tossebro J, Weber G. Ageing and health status in adults with intellectual disabilities: results of the European POMONA II study. Journal of Intellectual and Developmental Disability. 2011;36:49–60. doi: 10.3109/13668250.2010.549464. [DOI] [PubMed] [Google Scholar]
- Houk V, Thacker SB. The Centers for Disease Control program to prevent primary and secondary disabilities in the United States. Public Health Reports. 1989;104:226–231. [PMC free article] [PubMed] [Google Scholar]
- Hsu S-W, Lin J-D, Chiang P-H, Chang Y-C, Tung H-J. Comparison of outpatient services between elderly people with intellectual disabilities and the general elderly population in Taiwan. Research in Developmental Disabilities. 2012;33:1429–1436. doi: 10.1016/j.ridd.2012.03.014. [DOI] [PubMed] [Google Scholar]
- Iezzoni LI, Freedman VA. Turning the tide: the importance of definitions. Journal of the American Medical Association. 2008;299:332–334. doi: 10.1001/jama.299.3.332. [DOI] [PubMed] [Google Scholar]
- Improving Health and Lives (IHAL) [accessed on 20 December 2012];Learning Disabilities Observatory. Available at: http://www.improvinghealthandlives.org.uk/
- Innes A, McCabe L, Watchman K. Caring for older people with an intellectual disability: a systematic review. Maturitas. 2012;72:286–295. doi: 10.1016/j.maturitas.2012.05.008. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (IOM) State of the USA health indicators: Letter report. The National Academies Press; Washington, DC: 2009. [PubMed] [Google Scholar]
- Janicki MP, Davidson PW, Henderson CM, McCallion P, Taets JD, Force LT, Sulkes SB, Frangenberg E, Ladrigan PM. Health characteristics and health services utilization in older adults with intellectual disability living in community residences. Journal of Intellectual Disability Research. 2002;46:287–298. doi: 10.1046/j.1365-2788.2002.00385.x. [DOI] [PubMed] [Google Scholar]
- Janicki MP, Davidson PW, Henderson CM, McCallion P, Taets J, Jansen DE, Krol B, Groothoff JW, Post D. People with intellectual disability and their health problems: a review of comparative studies. Journal of Intellectual Disability Research. 2004;48:93–102. doi: 10.1111/j.1365-2788.2004.00483.x. [DOI] [PubMed] [Google Scholar]
- Jansen D, Krol B, Groothoff J, Post D. People with intellectual disability and their health problems: a review of comparative studies. Journal of Intellectual Disability Research. 2004;48:93–102. doi: 10.1111/j.1365-2788.2004.00483.x. [DOI] [PubMed] [Google Scholar]
- Kerr M, Fraser W, Felce D. Primary health care for people with a learning disability: a keynote review. British Journal of Learning Disabilities. 1996;24:2–8. [Google Scholar]
- Kerr AM, McCulloch D, Oliver K, McLean B, Coleman E, Law T, Beaton P, Wallace S, Newell E, Eccles T, Prescott RJ. Medical needs of people with intellectual disability require regular reassessment, and the provision of client- and carer-held reports. Journal of Intellectual Disability Research. 2003;47:134–145. doi: 10.1046/j.1365-2788.2003.00453.x. [DOI] [PubMed] [Google Scholar]
- Krahn G, Campbell VA. Evolving views of disability and public health: the roles of advocacy and public health. Disability and Health Journal. 2011;4:12–18. doi: 10.1016/j.dhjo.2010.05.005. [DOI] [PubMed] [Google Scholar]
- Krahn GL, Hammond L, Turner A. A cascade of disparities: Health and health care access for people with intellectual disabilities. Mental Retardation and Developmental Disabilities Research Review. 2006;12:70–82. doi: 10.1002/mrdd.20098. [DOI] [PubMed] [Google Scholar]
- Krahn G, Fox MH, Campbell VA, Ramon I, Jesien G. Developing a health surveillance system for people with intellectual disabilities in the United States. Journal of Policy and Practice in Intellectual Disabilities. 2010;7:155–166. [Google Scholar]
- Krieger N. Embodying inequality: a review of concepts, measures, and methods for studying health consequences of discrimination. International Journal of Health Services. 1999;29:295–352. doi: 10.2190/M11W-VWXE-KQM9-G97Q. [DOI] [PubMed] [Google Scholar]
- Lai C-L, Hung W-J, Lin L-P, Chien W-C, Lin J-D. A retrospective population-based data analyses of inpatient care use and medical expenditure in people with intellectual disability co-occurring schizophrenia. Research in Developmental Disabilities. 2011;32:1226–1231. doi: 10.1016/j.ridd.2010.12.024. [DOI] [PubMed] [Google Scholar]
- Larson SA, Lakin KC, Anderson L, Kwak N, Lee JH, Anderson D. Prevalence of mental retardation and developmental disabilities: Estimates from the 1994/1995 National Health Interview Survey Disability Supplements. American Journal of Mental Retardation. 2001;106:231–252. [PubMed] [Google Scholar]
- Lennox TN, Nadkarni J, Moffat P, Robertson C. Access to services and meeting the needs of people with learning disabilities. Journal of Intellectual Disabilities. 2003;7:34–50. [Google Scholar]
- Lewis MA, Lewis CE, Leake B, King BH, Lindemann R. The quality of health care for adults with developmental disabilities. Public Health Reports. 2002;117:174–184. doi: 10.1016/S0033-3549(04)50124-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J-D, Wu JL, Lee PN. Healthcare needs of people with intellectual disability in institutions in Taiwan: outpatient care utilization and implications. Journal of Intellectual Disability Research. 2003;47:169–180. doi: 10.1046/j.1365-2788.2003.00454.x. [DOI] [PubMed] [Google Scholar]
- Lin J-D, Wu JL, Lee PN. Utilization of inpatient care and its determinants among persons with intellectual disabilities in day care centres in Taiwan. Journal of Intellectual Disability Research. 2004;48:655–662. doi: 10.1111/j.1365-2788.2003.00572.x. [DOI] [PubMed] [Google Scholar]
- Lin E, Balogh R, Cobigo V, Ouellette-Kuntz H, Wilton AS, Lunsky Y. Using administrative health data to identify individuals with intellectual and developmental disabilities: a comparison of algorithms. Journal of Intellectual Disability Research. 2012 doi: 10.1111/jir.12002. doi:10.1111/jir.12002. [DOI] [PubMed] [Google Scholar]
- Linehan C, Walsh PN, Van Schrojenstein Lantman-deValk H, Kerr MP, Dawson F, Pomona-I Group Are people with intellectual disabilities represented in European public health surveys? Journal of Applied Research in Intellectual Disabilities. 2009;22:409–420. [Google Scholar]
- Lohr KN, Steinwachs DM. Health services research: an evolving definition of the field. Health Services Research. 2002;37:15–17. [PubMed] [Google Scholar]
- Lollar DJ, Crews JE. Redefining the role of public health in disability. Annual Review of Public Health. 2003;24:195–208. doi: 10.1146/annurev.publhealth.24.100901.140844. [DOI] [PubMed] [Google Scholar]
- Madans JH, Loeb ME, Altman BM. Measuring disability and monitoring the UN convention on the rights of persons with disabilities: The work of the Washington group on disability statistics. BMC Public Health. 2011;11(Suppl 4):S4. doi: 10.1186/1471-2458-11-S4-S4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marge M. Health promotion for persons with disabilities: moving beyond rehabilitation. American Journal of Health Promotion. 1988;2:29–35. doi: 10.4278/0890-1171-2.4.29. [DOI] [PubMed] [Google Scholar]
- Maulik PK, Mascarenhas MN, Mathers CD, Dua T, Saxena S. Prevalence of intellectual disability: a meta-analysis of population-based studies. Research in Developmental Disabilities. 2011;32:419–436. doi: 10.1016/j.ridd.2010.12.018. [DOI] [PubMed] [Google Scholar]
- McCarthy EP, Ngo LN, Roetzheim RG, Chirikos TN, Li D, Drews RE, Iezzoni LI. Disparities in breast cancer treatment and survival for women with disabilities. Annals of Internal Medicine. 2006;145:637–645. doi: 10.7326/0003-4819-145-9-200611070-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGilloway S, Donnelly M. Patterns of service use among people with learning disabilities discharged from long-stay hospital care in Northern Ireland. Irish Journal of Psychological Medicine. 1999;16:109–113. [Google Scholar]
- McGinnis JM, Williams-Russo P, Knickman JR. The case for more active policy attention to health promotion. Health Affairs. 2002;21:78–93. doi: 10.1377/hlthaff.21.2.78. [DOI] [PubMed] [Google Scholar]
- Murray CJ. Towards good practice for health statistics: lessons from the Millennium Development Goal health indicators. Lancet. 2007;369:862–867. doi: 10.1016/S0140-6736(07)60415-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Core Indicators [accessed on 2 July 2012];2012 Available at: http://www.nationalcoreindicators.org.
- New South Wales Council on Intellectual Disability [accessed on 20 December 2012];Health and People With Intellectual Disability. NSW Council for Intellectual Disability. 2003 Available at: http://www.nswcid.or.au/systemic/position/health.html.
- Nottestad JA, Linaker OM. Psychiatric health needs and services before and after complete deinstitutionalization of people with intellectual disability. Journal of Intellectual Disability Research. 1999;43:523–530. doi: 10.1046/j.1365-2788.1999.00236.x. [DOI] [PubMed] [Google Scholar]
- Office for National Statistics [accessed on 19 December 2012];An Executive Summary, Life Opportunities Survey – Wave Two Report, Part 1. 2012 Available at: http://www.ons.gov.uk/ons/dcp171776_287077.pdf.
- Ouellette-Kuntz H. Understanding health disparities and inequities faced by individuals with intellectual disabilities. Journal of Applied Research in Intellectual Disabilities. 2005;18:113–121. [Google Scholar]
- Ouellette-Kuntz H, Garcin N, Lewis ME, Minnes P, Martin C, Holden JJ. Addressing health disparities through promoting equity for individuals with intellectual disability. Canadian Journal of Public Health. 2005;96(S2):S8–S22. doi: 10.1007/BF03403699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouellette-Kuntz H, Shooshtari B, Temple B, Brownell M, Burchill C, Yu CT, Holden J, Hennen B. Estimating administrative prevalence of intellectual disabilities in Manitoba. Journal on Developmental Disabilities. 2009;15:69–80. [Google Scholar]
- Reichard A, Stolzle H. Diabetes among adults with cognitive limitations compared to individuals with no cognitive disabilities. Intellectual and Developmental Disabilities. 2011;49:141–154. doi: 10.1352/1934-9556-49.2.141. [DOI] [PubMed] [Google Scholar]
- Reichard A, Stolzle H, Fox M. Health disparities among adults with physical disabilities or cognitive limitations compared to individuals with no disabilities in the United States. Disability and Health Journal. 2011;4:59–67. doi: 10.1016/j.dhjo.2010.05.003. [DOI] [PubMed] [Google Scholar]
- Scheepers M, Kerr M, O’Hara D, Bainbridge D, Cooper SA, Davis R, Fujiura G, Heller T, Holland A, Krahn G. Reducing health disparity in people with intellectual disabilities: a report from the Health Issues Special Interest Research Group of the International Association for the Scientific Study of Intellectual Disabilities. Journal of Policy and Practice in Intellectual Disabilities. 2005;2:249–255. [Google Scholar]
- van Schrojenstein Lantman-de Valk H. Health in people with intellectual disabilities: current knowledge and gaps in knowledge. Journal of Applied Research in Intellectual Disabilities. 2005;18:325–333. [Google Scholar]
- van Schrojenstein Lantman-de Valk H, Linehan C, Kerr M, Walsh PN. Developing health indicators for people with intellectual disabilities. The method of the Pomona project. Journal of Intellectual Disability Research. 2007;51:427–434. doi: 10.1111/j.1365-2788.2006.00890.x. [DOI] [PubMed] [Google Scholar]
- Scottish Executive Health Department [accessed on 20 June 2012];Promoting Health, Supporting Inclusion: The National Review of the Contribution of All Nurses and Midwives to the Care and Support of People With Learning Disabilities. 2002 Available at: http://www.scotland.gov.uk/Publications/2002/07/15072/8573.
- Shogren KA, Wehmeyer ML, Reese RM, O’Hara D. Promoting self-determination in health and medical care: a critical component of addressing health disparities in people with intellectual disabilities. Journal of Policy and Practice in Intellectual Disabilities. 2006;3:105–113. [Google Scholar]
- Smith G, Ashbaugh J. [accessed on 20 June 2012];National Core Indicators Project: Phase II Consumer Survey Technical Report. 2001 Available at: http://www.hsri.org.
- Sondenaa E, Rasmussen K, Nottestad JA, Lauvrud C. Prevalence of intellectual disabilities in Norway: domestic variance. Journal of Intellectual Disability Research. 2010;54:161–167. doi: 10.1111/j.1365-2788.2009.01230.x. [DOI] [PubMed] [Google Scholar]
- Swanson ME. Need for the life course model for spina bifida. Pediatric Clinics of North America. 2010;57:893–901. doi: 10.1016/j.pcl.2010.08.001. [DOI] [PubMed] [Google Scholar]
- Turk MA. Appendix J: Secondary conditions and disability. In: Institute of Medicine, editor. Workshop on Disability in America: A New Look - Summary and Background Papers. The National Academies Press; Washington, DC: 2006. pp. 185–193. [Google Scholar]
- U.K. Department of Health . Valuing People: A New Strategy for Learning Disability for the 21st century. The Stationery Office Limited; London: 2001. [PMC free article] [PubMed] [Google Scholar]
- U.N. General Assembly World Programme of Action Concerning Disabled Persons. 1982. United Nations document A/37/51, Official Records of the General Assembly, Thirty-seventh Session Supplement No. 51.
- U.S. Department of Health and Human Services Closing the Gap: A National Blueprint for Improving the Health of Individuals with Mental Retardation. Report of the Surgeon General’s Conference on Health Disparities and Mental Retardation; Washington, DC: U.S. Public Health Service; 2002. [Google Scholar]
- U.S. Department of Health and Human Services [accessed on 20 June 2012];The Secretary’s Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020. Phase I Report: Recommendations for the framework and format of Healthy People 2020. Section IV. Advisory Committee Findings and Recommendations. 2010 Available at: http://www.healthypeople.gov/hp2020/advisory/PhaseI/sec4.htm#_Toc211942917.
- U.S. Department of Health and Human Services. Centers for Medicare & Medicaid Services . Chronic Conditions Among Medicare Beneficiaries, Chart Book. Baltimore, MD: [accessed 20 June 2012]. 2011. Available at: http://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Chronic-Conditions/Downloads/2011Chartbook.pdf. [Google Scholar]
- U.S. Department of Health and Human Services. Health Resources and Services Administration. Maternal and Child Health Bureau [accessed 10 November 2012];Rethinking MCH: The Life Course Model as an Organizing Framework Concept Paper. (Version 1.1). 2010 Nov; Available at: http://mchb.hrsa.gov/lifecourse/rethinkingmchlifecourse.pdf.
- U.S. National Council on Disability (formerly National Council on the Handicapped) Toward Independence: An Assessment of Federal Laws and Programs Affecting Persons with Disabilities–With Legislative Recommendations. A report to the President and to the Congress of the United States; Washington, DC: [accessed on 10 February 2012]. 1986. [document on the internet] Available at: http://www.ncd.gov/newsroom/publications/1986/toward.htm. [Google Scholar]
- Vickers G. What sets the goals of public health? Lancet. 1958;1:599–604. doi: 10.1056/NEJM195803202581205. [DOI] [PubMed] [Google Scholar]
- Walsh PN. Applying an indicator set to survey the health of people with intellectual disabilities in Europe. Journal of Policy and Practice in Intellectual Disabilities. 2008;5:211–213. [Google Scholar]
- Walsh PN, Kerr M, van Schrojenstein Lantman-de Valk HM. Health indicators for people with intellectual disabilities: a European perspective. European Journal of Public Health. 2003;13(3 Suppl.):47–50. doi: 10.1093/eurpub/13.suppl_1.47. [DOI] [PubMed] [Google Scholar]
- Whitehead M. The concepts and principles of equity in health. International Journal of Health Services. 1992;22:429–445. doi: 10.2190/986L-LHQ6-2VTE-YRRN. [DOI] [PubMed] [Google Scholar]
- Woodhouse JM, Adler P, Duignan A. Vision in athletes with intellectual disabilities: the need for improved eyecare. Journal of Intellectual Disability Research. 2004;48:736–745. doi: 10.1111/j.1365-2788.2004.00595.x. [DOI] [PubMed] [Google Scholar]
- World Health Organization . International Classification of Functioning, Disability and Health. WHO; Geneva, Switzerland: 2001. [Google Scholar]
- World Health Organization [accessed on 18 October 2012];Innovative Care for Chronic Conditions: Building Blocks for Action. 2002 Available at: http://www.who.int/chp/knowledge/publications/icccreport/en/
- World Health Organization [accessed on 18 October 2012];Health Topics: Chronic Diseases. 2011a Available at http://www.who.int/topics/chronic_diseases/en/
- World Health Organization . World Report on Disability. WHO; Geneva, Switzerland: [accessed on 20 June 2012]. 2011b. Available at: http://www.who.int/disabilities/world_report/2011/en/index.html. [Google Scholar]
- World Health Organization [accessed on 20 December 2012];Definition: Intellectual Disability. 2012 Available at http://www.euro.who.int/en/what-we-do/health-topics/noncommunicable-diseases/mental-health/news/news/2010/15/childrens-right-to-family-life/definition-intellectual-disability.
- World Health Organization [accessed on 3 April 2013];Washington Group on Disability Statistics. 2013 Available at: http://unstats.un.org/unsd/methods/citygroup/washington.htm.
- World Health Organization. International Longevity Centre-UK . The Implications for Training of Embracing a Life Course Approach to Health. World Health Organization; Geneva: [accessed 10 November 2012]. 2000. Available at: http://www.who.int/ageing/publications/lifecourse/alc_lifecourse_training_en.pdf. [Google Scholar]
- Yen CF, Lin JD, Loh CH, Shi L, Hsu SW. Determinants of prescription drug use by adolescents with intellectual disabilities in Taiwan. Research in Developmental Disabilities. 2009;30:1354–1366. doi: 10.1016/j.ridd.2009.06.002. [DOI] [PubMed] [Google Scholar]