Summary
Aim
To evaluate the impact of smoking and previous periodontal disease on peri-implant microbiota and health in medium to long-term maintained patients.
Methods
A retrospective evaluation of partial edentulous patients restored with dental implants and enrolled in a regular supportive therapy was performed. Inclusion criteria were: medium to long-term periodontal and implant maintenance (at least 5 years), a minimum of 2 implants placed in each patient, absence of systemic diseases that may affect osseointegration. 30 implants in 15 patients were included in the study. Subjects were divided in smokers or non-smokers and between patients previously affected by periodontal disease and periodontally healthy. Peri-implant and periodontal parameters were assessed (PD,BoP, mPI). Microbiological samples were collected around implant and an adjacent tooth. Real- Time Polymerase Chain Reaction (RT-PCR) analysis was performed.
Results
In all the three groups no differences in bacterial counts between dental and implant sites were observed. Non smoker, healthy patients: healthy clinical parameters, significant counts of spirochetes in isolated patients. Non smokers with previous periodontal disease: occasional positive BoP values, significant high counts of pathogenic bacteria. Smokers with previous periodontal disease: clinical signs of inflammation including deep pockets and slight bone resorption, significant counts of pathogenic bacteria.
Conclusions
Over a follow-up of 5 to 7 years, it is possible to state that the absence of smoking habit and previous periodontal disease positively influences the peri-implant microbiological and clinical conditions in partial edentulous patients restored with dental implants and enrolled in a strict regular supportive therapy.
Keywords: microbiota, periodontal disease, smoking, dental implants, long-term maintenance
Introduction
The development of biofilm on implant surfaces
The introduction of dental implants as surgical and-prosthetic procedures to replace lost natural teeth, due to dental caries, trauma or periodontal disease, has been a major advance in the management of fully and partially edentulous individuals. The surfaces of the inserted implants represent a new opportunity for bacterial colonization and lead to a microbial profile that might be substantially different from the one found on natural teeth. The immune-blot technique, used for the study of bacterial colonization in osseointegrated implants, has led to the recognition of five different species: Porphyromonas gingivalis, Prevotella intermedia, Actinomycesnaes lundii, Fusobacterium nucleatum, Treponemasocranskii (1). The results showed that implants in partially edentulous subjects were colonized by periodontal pathogens as early as 14 days after the exposure to the oral environment and that the establishment of a complex subgingival microbiota occurred as early as 28 days after exposure. Biofilm development on teeth and implants was also compared during a 3-week study of experimental gingivitis and peri-implant mucositis using phase contrast microscopy (2). It was evident that the biofilm revealed similar proportions of coccoid cells, motile rods, and spirochetes (spp) on both teeth and implants at baseline and after three weeks of plaque accumulation. The development of biofilms on titanium surfaces was also examined in partially edentulous subjects who required implants (3). Higher counts of complex species were detected on the tooth surfaces at all time points, particularly at 2 weeks. At later time points, the differences between the sampled sites were less marked, although complex species were still at higher levels in the dental sites compared to implant ones. The above studies indicate that the early development of biofilms on implant surfaces is similar to the one observed on natural teeth. Studies about the development of biofilms on natural teeth showed that attachment of bacterial occurred within minutes and that the increase in specific species could be detected in a time period as short as 2–6 hours. It is likely that biofilm development on the implant follows a similar course and that maturation is well under way by 2 weeks as provided by Quirynen et al. (4).
The microbiological pattern in partially edentulous subjects
The literature comparing the bacterial profile around implants in fully edentulous subjects with the microbiota in partially edentulous subjects confirms the role of the remaining dentition as a major source for colonization. Studies comparing the peri-implant microbiota with the bacteria of adjacent teeth described several similar aspects in the two sites. In partial edentulous subjects, bacterial counts did not significantly differ between subgingival dental and implant samples (5). Moreover, the bacteria around healthy implant and dental sites were extremely similar. This observation suggests that the major influence on the peri-implant microbiota was the bacteria present on the remaining teeth.
The association between periodontal and peri-implant conditions
It may be assumed that the peri-implant tissue response to the bacterial challenge may follow patterns similar to that of the periodontal tissues in a susceptible host (6, 7). So far, it has not yet been clarified whether a host susceptible for periodontitis will also be susceptible for peri-implantitis. However, there is evidence for the association between periodontitis and peri-implantitis (8). It is sure also that smoke, local and systemic conditions and the presence of subgingival pathogenic bacteria play an important role in the occurrence of complications. However, the biological impact of these factors on the long-term prognosis of oral implant is still to be defined. Karoussis et al. (9) compared in a prospective study the clinical and radiographic changes in periodontal and peri-implant conditions in a population susceptible to periodontal diseases. This study investigated the association of changes in periodontal parameters and periimplant conditions over a mean observation period of 10 years (8–12 years) following implant installation. The results of this study indicated that after a period of 10 years, statistically significant differences existed between implants and matching control teeth with regard to most of the clinical and radiographic parameters with the exception of plaque index and recession. Marginal bone level at implants at 10 years was also associated to smoking and general health condition.
Dental implant prognosis in periodontally compromised partially edentulous patients
The outcome of implant treatment in periodontally compromised partially edentulous patients has not been completely clarified. In this regard, it is significant a recent review from Karoussis et al. (10). The Authors completed a comprehensive and critical review of all the studies regarding the short-term and long-term prognosis of osseointegrated implants placed in periodontally compromised patients. 15 prospective studies were selected, including seven short-term and eight long-term studies. The results of this review revealed that no statistically significant differences in both short-term and long-term implant survival exist between patients with a history of chronic periodontitis and periodontally healthy individuals. However, patients with a previous history of chronic periodontitis may exhibit significantly greater long-term probing pocket depths, peri-implant marginal bone loss and incidence of peri-implantitis compared with periodontally healthy subjects. Alterations in clinical parameters around implants and teeth in aggressive periodontitis patients may not follow the same pattern, in contrast to what has been reported for chronic periodontitis patients. Therefore, more studies are required to evaluate implant prognosis in this form of periodontitis. Other systematic reviews (11–13) have provided the highest level of evidence supporting the favorable long-term prognosis of implant therapy in the general population. However, fewer data seem to be available concerning the prognosis of implants placed in periodontally compromised patients and the incidence of implant biological complications appear to be higher in patients previously affected by periodontitis.
Smoking and dental implant failure
Cigarette smoking has been related with an increased risk for peri-implantitis, marginal bone loss around implants, and loss of implants (14–16).
It is therefore essential that the dental team explain the patient that smoking can contribute to complications following implant insertion.
Several historical follow-up studies have shown that cigarette smoking is a significant risk factor from implant failure (17, 18).
Smokers are more susceptible to both periodontitis and peri-implantitis because of impairment of immune response (19) and compromised wound healing (20). Increased probing depths, plaque indices and bleeding on probing values have been observed in smoker subjects restored with dental implants. A systematic review of the literature that assessed implant loss, bone loss greater than 50%, implant mobility, persistent pain, or peri-implantitis, reported that smokers had a significantly enhanced risk of peri-implantitis (21).
The aim of the present study was to evaluate the impact of smoking and previous periodontal disease on the microbiota and peri-implant health in a group of partial edentulous patients restored with dental implants. All the subjects included in this retrospective study had been enrolled in a regular supportive therapy program fora medium to long term period (5–7 years of restoration function).
Materials and methods
Selection of patients:
Patients were enrolled during January to February 2014 in a private dental practice (B.A.) in Milan, Italy. A retrospective search for patients restored with fixed partial dentures supported by dental implants and enrolled in regular supportive periodontal therapy (at least four times per year) was performed. The study was conducted in compliance with the “Ethical principles for medical research involving human subjects” of Helsinki Declaration.
Inclusion criteria were the following:
- medium to long-term implant and periodontal maintenance (at least 60 months after the delivery of the final implant supported restoration)
- 2 to 3 dental implants (Bone System, Milan, Italy) previously inserted in each partial edentulous patient
- no uncontrolled diabetes
- no pregnancy and lactation
- no use of antibiotic or corticosteroids in the last three months
- no active, untreated periodontal infection of the natural dentition assessed at the clinical evaluation.
A total of 15 patients and 30 implants have been selected. Patients were subdivided in the following three subgroups according to previous periodontal disease and smoking habit:
- Group 1: Non smoker, periodontally healthy patients.
- Group 2: Non smoker subjects previously affected by periodontitis.
- Group 3: Smokers, previously affected by periodontitis.
Periodontally healthy smoker patients that fulfill the inclusion criteria were not found within the entire population of the dental practice.
Clinical and microbiological procedures
All the patients were recalled for supportive therapy and the following procedures were carried out:
first, on each implant site, the following biometric parameters were evaluated: probing depth (PD), bleeding on probing (BoP), modified plaque index (mPI), the presence of keratinized tissue (KT).
Reproducibility of probing procedure was evaluated by clinical assessment in 9 implants in 5 patients during two separate sessions 1 week apart and linear weighted kappa (κ) score was calculated.
Later, microbiological samples of the subgingival biofilm were collected by carefully removing supra gingival plaque and inserting five paper points in each implant site and an adjacent tooth. The samples were then analyzed by Carpegen© Perio Diagnostics, Munster, Germany. This analysis is based on a Real-time PCR procedure that detects and quantifies the presence of the following bacterial species: Aggregati bacter Actinomycetem comitans (A.a.), Fusobacterium nucleatum (F.n.), Porphyromonas gingivalis (P.g.), Prevotella intermedia (P.i.), Treponemadenticola (T.d.), Tannerella forsythia (T.f.). The PCR-Real Time parameters were the following:
- a detection limit for each of the five pathogens of 100 bacteria within a patient’s sample;
- a linear range for quantification that comprehends seven orders of magnitude for each pathogen;
- a coefficient of variation is 15%.
The bacterial genomic DNA was isolated and purified with the AGOWAs mag DNA Isolation Kit Sputum (AGOWA GmbH, Berlin, Germany). Primers and probes for Carpagen Perio Diagnostics were designed to match highly specifically to ribosomal DNA (rDNA) of the five bacterial pathogens. The exact primer and probe sequences were selected with the Primer Express software (Applied Biosystems, Foster City, CA, USA), which checks the primer and probesets for matching the guidelines that are recommended for real-time PCR with TaqMan’s probes. The primers and probes were obtained from Applied Biosystems. Real-time PCR was carried out with 2 ml of the isolated DNA as template in a reaction mixture containing the appropriate primer probesets and the TaqMans Universal PCR Mastermix. The PCR was carried out in a real time PCR cycler (LightCycler® 480 II” Roche Diagnostics Ltd., Rotkreuz, Switzerland). A laboratory code has been assigned to each patient (Tab. 1).
Table 1.
Biometric parameters and microbiological profile of all the patients included in the study.
| name | smoking habit | sex | age | biotype | position | mes pd | dist pd | cent pd | ml pd | dl pd | l pd | bop v | bopl | mPI | keratinized tissue | previous period disease | Lab.-No. | A.a. | F.n. | P.g. | P.i. | T.d. | T.f. | Total bacterial load |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BA | 0 | m | 59 | T | #20 | 3 | 3 | 3 | 2 | 2 | 2 | 1 | 0 | 0 | 1 | N | 1084749 | <100 | <100 | <100 | <100 | <100 | <100 | 3,4E+06 |
| BA | 0 | m | 59 | T | #21 | 2 | 2 | 2 | 2 | 2 | 3 | 0 | 0 | 0 | 1 | N | 1084750 | <100 | 5,0E+02 | <100 | <100 | <100 | <250 | 1,7E+07 |
| AG | 0 | f | 70 | T | #25 | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 0 | 0 | 1 | y | 1084751 | <100 | <100 | <100 | <100 | 1,5E+04 | 4,6E+04 | 2,4E+07 |
|
| ||||||||||||||||||||||||
| AG | 0 | f | 70 | T | #23 | 3 | 4 | 3 | 3 | 4 | 3 | 0 | 0 | 0 | 1 | y | 1084752 | <100 | <250 | <100 | <100 | 2,2E+04 | 1,2E+04 | 1,1E+06 |
| GM | 1 | m | 48 | T | #24 | 2 | 2 | 1 | 2 | 2 | 1 | 0 | 0 | 0 | 1 | y | 1084753 | <100 | <250 | 3,4E+03 | <250 | <250 | 1,5E+03 | 5,0E+05 |
|
| ||||||||||||||||||||||||
| GM | 1 | m | 48 | T | #12 | 3 | 3 | 2 | 3 | 3 | 2 | 0 | 1 | 1 | 1 | y | 1084754 | <100 | 2,5E+03 | 2,7E+04 | <100 | 2,8E+03 | 2,9E+03 | 3,0E+06 |
| FR | 0 | f | 45 | T | #29 | 3 | 3 | 2 | 3 | 3 | 2 | 0 | 0 | 1 | 1 | N | 1084755 | <100 | <100 | <100 | <100 | <100 | <100 | 4,5E+07 |
| FR | 0 | f | 45 | T | #14 | 3 | 3 | 2 | 3 | 3 | 2 | 0 | 0 | 0 | 1 | N | 1084756 | <100 | <100 | <100 | <100 | <100 | 5,0E+02 | 2,0E+06 |
|
| ||||||||||||||||||||||||
| FR | 0 | m | 45 | T | #10 | 3 | 2 | 3 | 2 | 2 | 2 | 0 | 0 | 0 | 1 | N | 1084757 | <100 | <100 | <100 | <100 | <100 | <100 | 1,6E+06 |
| MV | 0 | m | 66 | T | #10 | 2 | 4 | 4 | 4 | 2 | 2 | 2 | 1 | 1 | 1 | Y | 1084758 | <100 | 3,8E+04 | 2,9E+06 | 3,2E+05 | 8,2E+06 | 1,6E+06 | 7,6E+07 |
| MV | 0 | m | 66 | T | #9 | 3 | 3 | 2 | 3 | 3 | 2 | 1 | 1 | 1 | 1 | Y | 1084759 | <100 | <100 | 1,8E+03 | <100 | 2,6E+03 | 9,4E+02 | 1,7E+06 |
|
| ||||||||||||||||||||||||
| FG | 1 | m | 50 | t | #13 | 3 | 3 | 2 | 3 | 3 | 2 | 0 | 0 | 0 | 1 | y | 1084760 | <100 | <100 | <100 | <100 | <100 | <100 | 6,1E+04 |
| FG | 1 | m | 50 | t | #12 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 0 | 0 | 1 | y | 1084761 | <100 | 1,2E+03 | <100 | <100 | <100 | <100 | 5,6E+05 |
|
| ||||||||||||||||||||||||
| T | 1 | f | 50 | t | #2 | 4 | 3 | 3 | 4 | 4 | 3 | 0 | 0 | 1 | 0 | y | 1084762 | <100 | <100 | <100 | <100 | <100 | <250 | 2,5E+07 |
| T | 1 | f | 50 | t | #3 | 3 | 3 | 2 | 3 | 3 | 2 | 0 | 0 | 0 | 0 | y | 1084763 | <100 | <100 | <100 | <100 | <100 | 3,6E+02 | 2,0E+06 |
| Y | 0 | f | 27 | t | #3 | 3 | 3 | 2 | 3 | 3 | 2 | 0 | 0 | 0 | 0 | y | 1084764 | <100 | <100 | <100 | <100 | <100 | <100 | 1,3E+06 |
|
| ||||||||||||||||||||||||
| Y | 0 | f | 27 | t | #5 | 3 | 3 | 3 | 3 | 3 | 2 | 0 | 0 | 0 | 0 | y | 1084765 | <100 | <100 | <100 | <100 | <100 | <100 | 2,0E+06 |
| MS | 0 | m | 37 | T | #30 | 3 | 3 | 2 | 3 | 3 | 2 | 0 | 0 | 0 | 0 | N | 1084766 | <100 | 2,2E+05 | <100 | <100 | <100 | 8,1E+04 | 1,3E+07 |
|
| ||||||||||||||||||||||||
| MS | 0 | m | 37 | T | #18 | 2 | 2 | 3 | 2 | 2 | 3 | 0 | 0 | 0 | 0 | N | 1084767 | <100 | 3,7E+03 | <100 | <100 | <100 | <250 | 1,7E+06 |
| CG | 0 | m | 66 | T | #30 | 1 | 1 | 0 | y | 1084768 | <100 | <100 | 4,0E+03 | 2,3E+03 | <100 | 4,6E+02 | 6,6E+06 | |||||||
|
| ||||||||||||||||||||||||
| CG | 0 | m | 66 | T | #28 | 3 | 3 | 2 | 4 | 3 | 2 | 0 | 0 | 0 | 1 | y | 1084769 | <100 | 4,0E+03 | 4,0E+02 | <100 | <250 | <100 | 4,3E+06 |
| AG | 1 | m | 66 | T | #20 | 4 | 7 | 3 | 4 | 7 | 3 | 1 | 1 | 0 | 1 | y | 1084770 | <100 | <100 | 3,3E+04 | 1,2E+04 | 3,7E+03 | 2,0E+03 | 9,4E+05 |
| AG | 1 | m | 66 | T | #21 | 3 | 3 | 2 | 3 | 3 | 2 | 0 | 0 | 1 | 0 | y | 1084771 | <100 | <100 | 4,3E+02 | 2,9E+02 | <250 | <100 | 3,0E+06 |
|
| ||||||||||||||||||||||||
| LGB | 1 | m | 68 | T | #3 | 3 | 3 | 2 | 4 | 4 | 2 | 0 | 0 | 1 | 0 | y | 1084772 | <100 | 2,3E+04 | 3,8E+04 | 1,4E+04 | 5,4E+04 | 6,0E+03 | 3,9E+07 |
| LGB | 1 | m | 68 | T | #6 | 3 | 3 | 2 | 3 | 3 | 2 | 0 | 0 | 1 | 0 | y | 1084773 | <100 | 6,2E+04 | <100 | <100 | <100 | <100 | 2,6E+06 |
| VC | 1 | f | 75 | T | #12 | 3 | 3 | 2 | 3 | 3 | 2 | 0 | 0 | 1 | 0 | y | 1084774 | 1,3E+03 | <100 | 1,6E+04 | <100 | <100 | 3,1E+03 | 1,0E+05 |
| VC | 1 | f | 75 | T | #11 | 4 | 4 | 3 | 2 | 3 | 2 | 3 | 2 | 3 | 0 | y | 1084775 | 3,7E+04 | <100 | 9,1E+03 | <100 | 2,0E+03 | 8,6E+04 | 5,6E+06 |
|
| ||||||||||||||||||||||||
| CR | 0 | m | 53 | T | #5 | 3 | 3 | 2 | 4 | 4 | 3 | 0 | 0 | 0 | 0 | y | 1084776 | <100 | <100 | 7,0E+03 | <100 | <100 | 2,8E+03 | 2,5E+06 |
| CR | 0 | m | 53 | T | #28 | 4 | 4 | 3 | 3 | 3 | 2 | 0 | 0 | 0 | 0 | y | 1084777 | <100 | <100 | <100 | <100 | <100 | <100 | 1,1E+06 |
|
| ||||||||||||||||||||||||
| CC | 0 | f | 21 | T | #19 | 3 | 2 | 3 | 3 | 2 | 3 | 0 | 0 | 0 | 1 | N | 2014028 | <100 | 1,8E+03 | 4,8E+04 | 3,1E+03 | 1,2E+04 | 9,2E+03 | 1,7E+06 |
| CC | 0 | f | 21 | T | #8 | 3 | 3 | 3 | 3 | 2 | 3 | 0 | 0 | 0 | 1 | N | 2014029 | <100 | <100 | <100 | <100 | <100 | <100 | 5,9E+04 |
0=NO (Under the columns “smoking habits” and “keratinized tissue”); 1=YES (Under the columns “smoking habits” and “keratinized tissue”); Y=yes; NA=not assigned; f=female; t=thin; m=male; T=thick; N=no
A.a., T.f., P.g., P.i., T.d., F.n.: bacterial species as described in the section “Materials and methods”
Note: Implant positions are reported according to the universal numbering system (also known as the “american dental numbering system”)
All the data were assembled, results analyzed and manuscript written by first author (A.Q.) from August to December 2014 at the Department of Oral Sciences, Faculty of Dentistry, University of Otago, New Zealand.
Results
A total of 15 patients (9 males-6 females) was enrolled in the present study. The average age of male patients was 53.3 years; the average age of female patients was 53.4 years, the mean patients’ follow-up was 60.5 months (range 5 to 12 years).
Microbiological results described the counts for each pathogenic species and its proportion compared to the total bacterial load found in the analyzed sites. In all the three groups, no significant differences in proportions of bacterial species were observed between dental and implant sites.
Intra-examiner reproducibility regarding the collection of clinical parameters was good with a linear weighted kappa (κ) score of 0.85.
GROUP 1) Non-smoker patients with healthy periodontal tissues; (Tab. 2)
Table 2.
Clinical parameters and microbiological profile in non-smoker, periodontally healthy patients.
| NO SMOKERS-NO PREVIOUS PERIODONTAL DESEASE | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||
| PZ | Implant position | BOP | PD | mPI | K tissue | Lab.-No. | A.a. | F.n. | P.g. | P.i. | T.d. | T.f. | Total bacterial load |
| B.A. | #20 | vest | + | 1084749 | <100 | <100 | <100 | <100 | <100 | <100 | 3,4E+06 | ||
| #21 | + | 1084750 | <100 | 5,0E+02 | <100 | <100 | <100 | <250 | 1,7E+07 | ||||
|
| |||||||||||||
| F.R. | #19 | + | + | 1084755 | <100 | <100 | <100 | <100 | <100 | <100 | 4,5E+07 | ||
| #14 | + | 1084756 | <100 | <100 | <100 | <100 | <100 | 5,0E+02 | 2,0E+06 | ||||
| #10 | + | 1084757 | <100 | <100 | <100 | <100 | <100 | <100 | 1,6E+06 | ||||
|
| |||||||||||||
| M.S. | #18 | − | 1084766 | <100 | 2,2E+05 | <100 | <100 | <100 | 8,1E+04 | 1,3E+07 | |||
| #30 | − | 1084767 | <100 | 3,7E+03 | <100 | <100 | <100 | <250 | 1,7E+06 | ||||
|
| |||||||||||||
| C.C. | #19 | + | 2014028 | <100 | 1,8E+03 | 4,8E+04 | 3,1E+03 | 1,2E+04 | 9,2E+03 | 1,7E+06 | |||
| #8 | + | 2014029 | <100 | <100 | <100 | <100 | <100 | <100 | 5,9E+04 | ||||
vest= buccal side; +=present; - =absent
A.a., T.f., P.g., P.i., T.d., F.n.: bacterial species as described in the section “Materials and methods”
Note: Implant positions are reported according to the universal numbering system (also known as the “american dental numbering system”)
Significant counts of isolated red complex species were observed in all the patients (Fig. 1).
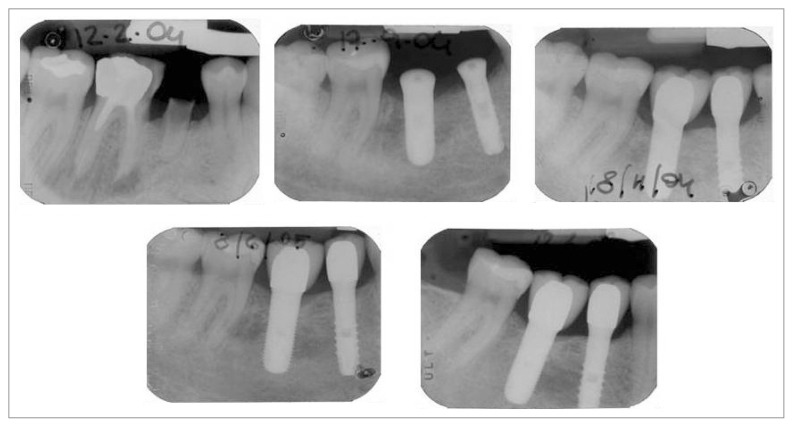
Figure 1.
Peri-apical x-rays of a non-smoker, periodontally healthy patient over a period of 7 years.
However, this observation was not related to pathological PD values or peri-implant inflammation. Only 1 patient showed BOP+, but this clinical observation did not correspond to a high total bacterial load nor significant single pathogenic counts. mPI values were considered satisfactory in all the subjects and ranged from 0 to 1. The presence of keratinized tissue did not correspond with healthier biometric parameters.
GROUP 2) Non-smoker patients previously affected by chronic periodontal disease (Tab. 3)
Table 3.
Clinical parameters and microbiological profile in non-smoker patients with previous periodontal disease.
| NO SMOKERS-PREVIOUS PERIODONTAL DESEASE | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||
| PZ | Implant position | BOP | PD | mPI | k tissue | Lab.-No. | A.a. | F.n. | P.g. | P.i. | T.d. | T.f. | Total bacterial load |
| A.G. | #25 | + | + | 1084751 | <100 | <100 | <100 | <100 | 1,5E+04 | 4,6E+04 | 2,4E+07 | ||
| #23 | + | 1084752 | <100 | <250 | <100 | <100 | 2,2E+04 | 1,2E+04 | 1,1E+06 | ||||
|
| |||||||||||||
| M.V | #10 | vest-ling | + | + | + | 1084758 | <100 | 3,8E+04 | 2,9E+06 | 3,2E+05 | 8,2E+06 | 1,6E+06 | 7,6E+07 |
| #9 | vest-ling | + | 1084759 | <100 | <100 | 1,8E+03 | <100 | 2,6E+03 | 9,4E+02 | 1,7E+06 | |||
|
| |||||||||||||
| Y | #3 | − | 1084764 | <100 | <100 | <100 | <100 | <100 | <100 | 1,3E+06 | |||
| #5 | − | 1084765 | <100 | <100 | <100 | <100 | <100 | <100 | 2,0E+06 | ||||
|
| |||||||||||||
| C.G. | #30 | − | 1084768 | <100 | <100 | 4,0E+03 | 2,3E+03 | <100 | 4,6E+02 | 6,6E+06 | |||
| #28 | + | 1084769 | <100 | 4,0E+03 | 4,0E+02 | <100 | <250 | <100 | 4,3E+06 | ||||
|
| |||||||||||||
| C.R. | #5 | − | 1084776 | <100 | <100 | 7,0E+03 | <100 | <100 | 2,8E+03 | 2,5E+06 | |||
| #28 | − | 1084777 | <100 | <100 | <100 | <100 | <100 | <100 | 1,1E+06 | ||||
vest=buccal side; ling=lingual side; +=positive; - =negative
A.a., T.f., P.g., P.i., T.d., F.n.: bacterial species as described in the section “Materials and methods”
Note: Implant positions are reported according to the universal numbering system (also known as the “american dental numbering system”)
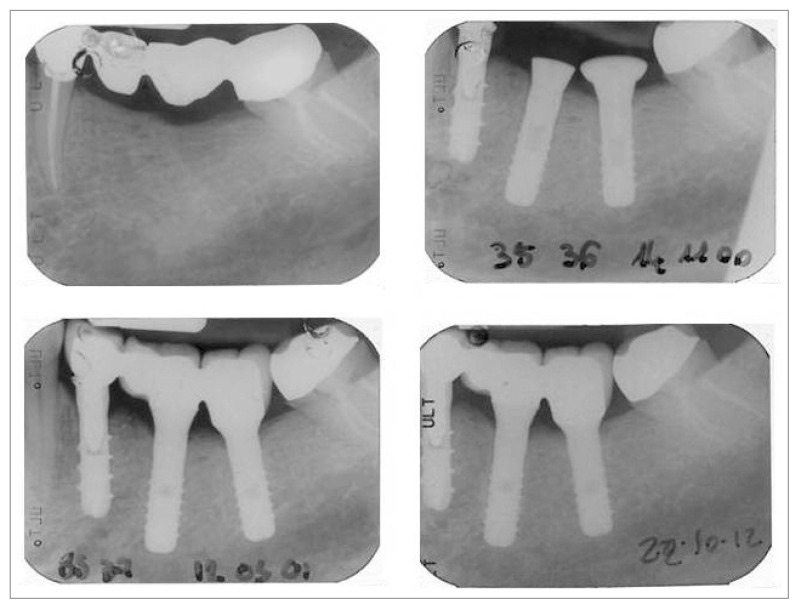
Seven implant sites in four patients showed significant counts of all the pathogenic species. The implant site with the most severe biometric parameters was also characterized by the highest total bacterial load and number of single pathogenic bacterial counts. In only 1 patient no significant presence of pathogenic species was observed around an implant site.
Bleeding on probing was positive and profuse in 3 implants in 2 different patients. In both the patients, this clinical observation corresponded to a microbiological profile with an extremely high total bacterial load. mPI values were considered relatively satisfactory in all the subjects and ranged from 0 to 2. The presence of keratinized tissue was not related to healthier biometric parameters (Fig. 2).
Figure 2.
Peri-apical x-rays of asmoker, periodontally healthy patient over a period of 6 years.
GROUP 3) Smoker patients previously affected by chronic periodontitis (Tab. 4)
Table 4.
Clinical parameters and microbiological profile in smoker patients with previous periodontal disease.
| SMOKERS-PREVIOUS PERIODONTAL DISEASE | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||||
| PZ | Implant position | BOP | PPD | mPI | K tissue | Lab.-No. | A.a. | F.n. | P.g. | P.i. | T.d. | T.f. | Total bacterial load |
| G.M. | #24 | + | 1084753 | <100 | <250 | 3,4E+03 | <250 | <250 | 1,5E+03 | 5,0E+05 | |||
| #12 | ling | + | 1084754 | <100 | 2,5E+03 | 2,7E+04 | <100 | 2,8E+03 | 2,9E+03 | 3,0E+06 | |||
|
| |||||||||||||
| F.G. | #13 | + | 1084760 | <100 | <100 | <100 | <100 | <100 | <100 | 6,1E+04 | |||
| #12 | + | 1084761 | <100 | 1,2E+03 | <100 | <100 | <100 | <100 | 5,6E+05 | ||||
|
| |||||||||||||
| T.M. | #2 | + | + | − | 1084762 | <100 | <100 | <100 | <100 | <100 | <250 | 2,5E+07 | |
| #3 | − | 1084763 | <100 | <100 | <100 | <100 | <100 | 3,6E+02 | 2,0E+06 | ||||
|
| |||||||||||||
| A.G | #21 | vest-ling | + | + | 1084770 | <100 | <100 | 3,3E+04 | 1,2E+04 | 3,7E+03 | 2,0E+03 | 9,4E+05 | |
| #22 | + | − | 1084771 | <100 | <100 | 4,3E+02 | 2,9E+02 | <250 | <100 | 3,0E+06 | |||
|
| |||||||||||||
| V.C. | #5 | − | 1084774 | 1,3E+03 | <100 | 1,6E+04 | <100 | <100 | 3,1E+03 | 1,0E+05 | |||
| #28 | + | − | 1084775 | 3,7E+04 | <100 | 9,1E+03 | <100 | 2,0E+03 | 8,6E+04 | 5,6E+06 | |||
|
| |||||||||||||
| L.G.B. | #3 | + | − | 1084772 | <100 | 2,3E+04 | 3,8E+04 | 1,4E+04 | 5,4E+04 | 6,0E+03 | 3,9E+07 | ||
| #6 | − | 1084773 | <100 | 6,2E+04 | <100 | <100 | <100 | <100 | 2,6E+06 | ||||
vest=buccal side; ling=lingual side; +=positive; - =negative
A.a., T.f., P.g., P.i., T.d., F.n.: bacterial species as described in the section “Materials and methods”
Note: Implant positions are reported according to the universal numbering system (also known as the “american dental numbering system”)
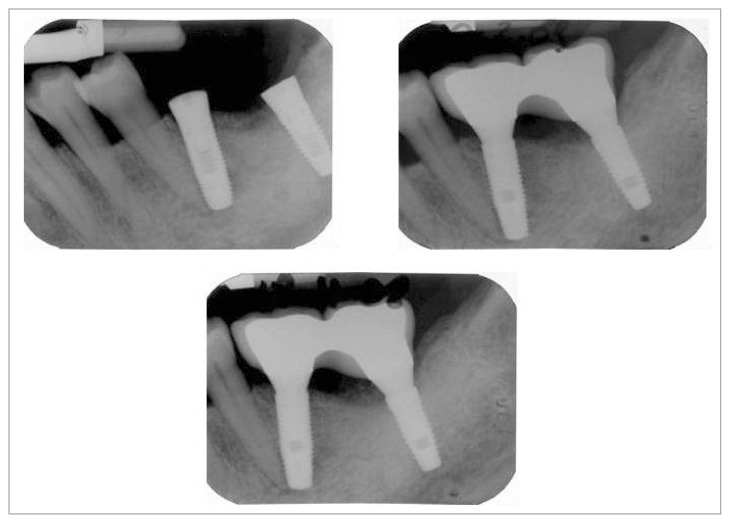
The microbiological analysis of peri-implant sites showed significant pathogenic counts in all the patients (Tab. 4). T.f. morphotype was the bacterial specie with the greatest counts in most of thesites. Four implant sites in four different patients showed deep PD values.
Two implant sites in two patients were characterized by high mPI values (3) and two additional implant sites in two subjects showed profuse bleeding on probing. The implant site with the most severe biometric parameters was characterized by a microbial profile with the highest total and pathogenic bacterial counts. The presence of keratinized tissue was not related to healthier biometric parameters (Fig. 3).
Figure 3.
Peri-apical x-rays of a smoker patient previously affected by periodontitis over a period of 7 years.
Discussion
It is well known that the peri-implant tissue response to the bacterial challenge may follow patterns similar to that of the periodontal tissues in a susceptible host, although it has not yet been clarified whether or not a host susceptible for periodontitis will also be susceptible for peri-implantitis. Nowadays there is scientific evidence about the association between periodontitis and peri-implantitis (8). It is also possible to state that smoke, local and systemic conditions and the presence of subgingival, pathogenic bacteria, play an important role in the occurrence of implant complications, although the biological impact of these factors on the long-term prognosis of oral implant is still to be defined. In the present study, the absence of deep PDs around implants in non-smoker patients with healthy periodontal tissues, seems to validate the positive role that the absence of modifying factors plays in peri-implant health. The results of the present study shows that previous periodontal disease has a role similar to smoking as risk factor for implant complications. The presence of both these factors do not make peri-implant clinical conditions worse. Unfortunately, no data about the number of cigarettes smoked per day were collected and this may be a confounding factor.
The total bacterial load was not always related to the presence of significant pathogenic counts.
T.f. was the bacterial specie with the highest number of counts in each group but it was not associated to significant counts of the other assessed bacteria.
On the other hand, the inverse assumption resulted consistently valid: a greater count of pathological species was found in patients with a greater total bacterial load.
In general, the total bacterial load was not related to pathological biometric parameters nor presence or absence of keratinized tissue.
However, the implant site with the worst biometric parameters was characterized by the greatest total bacterial load and the larger number of single pathogenic species counts.
Finally, in the present study significant pathogenic counts were observed in both smoker and non smoker subjects previously affected by periodontitis.
Conclusions
Within the limits of the present study it is possible to state that the absence of smoking habit and previous periodontal disease positively influences the medium to long-term microbiological profile and peri-implant health in partial edentulous patients. Further studies on a larger number of patients and paying special attention to the number of cigarettes smoked per day would be necessary in order to confirm our conclusions.
References
- 1.Koka S, Razzog ME, Bloem TJ, Syed S. Microbial colonization of dental implant in partially edentulous subjects. J Prosthet Dent. 1993;70:141–144. doi: 10.1016/0022-3913(93)90009-d. [DOI] [PubMed] [Google Scholar]
- 2.Pontoriero R, Tonelli MP, Carnevale G, Mombelli A, Nyman SR, Lang NP. Experimentally induced peri-implant mucositis. A clinical study in humans. Clin Oral Implants Res. 1994;5:254–259. doi: 10.1034/j.1600-0501.1994.050409.x. [DOI] [PubMed] [Google Scholar]
- 3.Quyrinen M, Vogels R, Peeters W, van Steenberghe D, Naert I, Haffajee A. Dynamics of initial subgingival colonization of “pristine” peri-implant pokets. Clin Oral Implants Res. 2006;17:25–37. doi: 10.1111/j.1600-0501.2005.01194.x. [DOI] [PubMed] [Google Scholar]
- 4.Quyrinen M, Vogels R, Pauwels M, Haffajeed C, Socransky SS, Uzel NG, van Steenberghe D. Initial subgingival colonization of “pristine” pokets. J Dent Research. 2005b;84:340–344. doi: 10.1177/154405910508400409. [DOI] [PubMed] [Google Scholar]
- 5.Quyrinen M, Listgarten MA. Distribution of bacterial morphotypes around natural teeth and titanium implants ad modum Branemark. Clin Oral Implants Res. 1990;1:8–12. doi: 10.1034/j.1600-0501.1990.010102.x. [DOI] [PubMed] [Google Scholar]
- 6.Seymour GJ, Gemmell E, Lenz LJ, Henry P, Bower R, Yamazaki K. Immunohistologic analysis of the inflammatory infiltrates associated with osseointegrated implants. Int J Oral Maxillofac Implants. 1989;4:191–8. [PubMed] [Google Scholar]
- 7.Liljenberg B, Gualini F, Berglundh T, Tonetti M, Lindhe J. Composition of plaque-associated lesions in the gingiva and the peri-implant mucosa in partially edentulous subjects. Clin Periodontol. 1997;24:119–23. doi: 10.1111/j.1600-051x.1997.tb00477.x. [DOI] [PubMed] [Google Scholar]
- 8.Karoussis IK, Salvi GE, Heitz-Mayfield LJ. Long-term implant prognosis in patients with and without a history of chronic periodontitis: a 10-year prospective cohort study of the ITI Dental Implant System. Clin Oral Implants Res. 2003;14:329–39. doi: 10.1034/j.1600-0501.000.00934.x. [DOI] [PubMed] [Google Scholar]
- 9.Karoussis IK, Müller S, Salvi GE, Heitz-Mayfield LJ, Brägger U, Lang NP. Association between periodontal and peri-implant conditions: a 10-year prospective study. Clin Oral Implants Res. 2004;15:1–7. doi: 10.1111/j.1600-0501.2004.00982.x. [DOI] [PubMed] [Google Scholar]
- 10.Karoussis IK, Kotsovilis S, Fourmousis A comprehensive and critical review of dental implant prognosis in periodontally compromised partially edentulous patients I. Clin Oral Implants Res. 2007;18:669–79. doi: 10.1111/j.1600-0501.2007.01406.x. [DOI] [PubMed] [Google Scholar]
- 11.Berglundh T, Persson L, Klinge B. A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. J Clin Periodontol. 2002;29:197–212. doi: 10.1034/j.1600-051x.29.s3.12.x. [DOI] [PubMed] [Google Scholar]
- 12.Lang NP, Pjetursson BE, Tan K, Brägger U, Egger M, Zwahlen M. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. II. Combined tooth-implant-supported FPDs. Clin Oral Implants Res. 2004;15:643–53. doi: 10.1111/j.1600-0501.2004.01118.x. [DOI] [PubMed] [Google Scholar]
- 13.Pjetursson BE, Tan K, Lang NP, Brägger U, Egger M, Zwahlen M. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. M Clin Oral Implants Res. 2004;15:625–42. doi: 10.1111/j.1600-0501.2004.01117.x. [DOI] [PubMed] [Google Scholar]
- 14.Rinke S, Ohl S, Ziebolz D, Lange K, Eikholz P. Prevalence of peri-implant disease in partially edentulous patients: A practice- based cross-sectional study. Clin Oral Implants Res. 2011;22:826–833. doi: 10.1111/j.1600-0501.2010.02061.x. [DOI] [PubMed] [Google Scholar]
- 15.Heitz-Mayfield LJ. Peri-implant diseases: Diagnosis and risk indicators. J Clin Periodontol. 2008;35(suppl 8):292–304. doi: 10.1111/j.1600-051X.2008.01275.x. [DOI] [PubMed] [Google Scholar]
- 16.Strietzel FP, Reichart PA, Kale A, Kulkarni M, Wegner B, Kuchler I. Smoking interferes with the prognosis of dental implant treatment: A systematic review and meta-analysis. J Clin Periodontol. 2007;34:523–544. doi: 10.1111/j.1600-051X.2007.01083.x. [DOI] [PubMed] [Google Scholar]
- 17.Bain CA, Moy PK. The association between the failure of dental implants and cigarette smoking. Int J Oral Maxillofac Implants. 1993;8(6):609–15. [PubMed] [Google Scholar]
- 18.Lindquist LW, Carlsson GE, Jemt T. Association between marginal bone loss around osseointegrated mandibular implants and smoking habits: a 10-year follow-up study. J Dent Res. 1997 Oct;76(10):1667–74. doi: 10.1177/00220345970760100801. [DOI] [PubMed] [Google Scholar]
- 19.Johnson GK, Hill M. Cigarette smoking and the periodontal patient. Periodontol. 2004 Feb;75(2):196–209. doi: 10.1902/jop.2004.75.2.196. [DOI] [PubMed] [Google Scholar]
- 20.Labriola A, Needleman I, Moles DR. Systematic review of the effect of smoking on nonsurgical periodontal therapy. Periodontol. 2000. 2005;37:124–37. doi: 10.1111/j.1600-0757.2004.03793.x. [DOI] [PubMed] [Google Scholar]
- 21.Roos-Jansåker AM, Renvert H, Lindahl C, Renvert S. Nine- to fourteen-year follow-up of implant treatment. Part III: Factors associated with peri-implant lesions. J Clin Periodontol. 2006;33:296–301. doi: 10.1111/j.1600-051X.2006.00908.x. [DOI] [PubMed] [Google Scholar]