Significance
Nature threads the very fabric of human lives in remote forest areas of developing countries. Unfortunately, we do not fully understand how ecosystem services (such as human health benefits) could be secured by conserving natural capital. Thus, we analyze a rich dataset on disease, climate, demography, land uses, and conservation policies in the Brazilian Amazon. Unsurprisingly, we find that the health dividends vary across conservation policies and are small relative to the overall burden of these diseases. However, interventions targeted specifically at preserving biodiversity (strict protected areas) generate health cobenefits. Thus, given a chance, nature does its part for human (health) capital, especially for the poor and politically voiceless.
Keywords: infectious diseases, roads, mining, protected areas, Amazon forest
Abstract
The claim that nature delivers health benefits rests on a thin empirical evidence base. Even less evidence exists on how specific conservation policies affect multiple health outcomes. We address these gaps in knowledge by combining municipal-level panel data on diseases, public health services, climatic factors, demographics, conservation policies, and other drivers of land-use change in the Brazilian Amazon. To fully exploit this dataset, we estimate random-effects and quantile regression models of disease incidence. We find that malaria, acute respiratory infection (ARI), and diarrhea incidence are significantly and negatively correlated with the area under strict environmental protection. Results vary by disease for other types of protected areas (PAs), roads, and mining. The relationships between diseases and land-use change drivers also vary by quantile of the disease distribution. Conservation scenarios based on estimated regression results suggest that malaria, ARI, and diarrhea incidence would be reduced by expanding strict PAs, and malaria could be further reduced by restricting roads and mining. Although these relationships are complex, we conclude that interventions to preserve natural capital can deliver cobenefits by also increasing human (health) capital.
The natural environment threads the very fabric of human lives in remote forest areas of developing countries, yet the local costs of conserving forest ecosystems are far better recognized than the local benefits. This contributes to conflict over conservation efforts because of the perception that they impose only costs on local populations by constraining their economic activities to benefit the rest of the globe by preserving biodiversity and mitigating climate change (1–4). However, it is difficult to judge the local effects of conservation without better evidence on the magnitude and multitude of ecosystem services that can be secured. A good example is the incomplete and insufficient evidence on whether and how ecosystem degradation harms human health (5–8). Health is a universal development concern (one of three components of human development indices) and very likely to be directly affected by land use and land-use policy (3).
Recent approximations attribute as much as 24% of the global burden of disease (GBD) to poor environmental quality, including land-use patterns (9, 10). Ecosystem degradation and infectious diseases are central elements of a vicious cycle of rural poverty traps in the developing topics (11–13). Although these problems are not new, they continue to be of global concern and significance, especially in the context of climate change. Thus, there is renewed attention to the environmental drivers of health (2, 6, 14, 15), which requires stepping back from a purely biomedical and molecular view of health to examine community and environmental drivers using a landscape epidemiology or ecoepidemiology perspective (16, 17). The desire to make the case for conservation has led to broad claims regarding the benefits of nature conservation for human health; these claims must be tested and substantiated with rigorous empirical analysis (3, 8, 18–20).
Consider the biggest environmental contributors to the GBD: diarrheal diseases, respiratory infections, and malaria, which have all featured prominently in the global appraisal because of their large environmental component and disproportionate impact on children (9, 10). The thin evidence base focuses on specific drivers of specific diseases (6), typically climate (20–25), biodemography and migration (13, 26–30), or land-use change (20, 31–33). Expanding this literature into multifactorial analyses could provide a more comprehensive picture of the human ecology of these diseases, including the role of specific behaviors and policies (8, 34). For example, behaviors such as migration and use of treated bednets and improved cookstoves are classic confounders because they muddle the links between disease reduction (in the environment) and disease exposure (in the human host), especially for infectious diseases (34). In such population–health–environment settings, environmental changes could trigger a dynamic set of behavioral interactions between families and the community that play out at multiple scales and, in turn, degrade the natural environment (35). In the Amazon, key policies include establishment of protected areas (PAs), investments in road construction, and regulation of mining (36, 37). This emphasis on behaviors and policies echoes calls in public health for translation or implementation science to address the unacceptable gap between our knowledge of diseases and the implementation of that knowledge in poor areas of developing countries, plagued by inadequate policies and insufficient prevention behaviors (38).
We help address these gaps in knowledge by building a comprehensive panel dataset containing information on disease, climate, sociodemographic factors, and drivers of land-use change in the Brazilian Amazon. Further, we develop hypotheses about how alternative conservation actions might affect disease incidence, through their influence on both ecosystem processes and exposure (SI Appendix, Table S1). The data are then used to test these hypotheses by estimating models that link disease incidence to drivers of ecosystem change. We also test whether and how these ecosystem services vary with different levels of disease incidence. The Brazilian Amazon is an appropriate setting to explore the health impacts of ecosystem changes because it has undergone both rapid land-use change, including conversion of nearly a fifth of the original forest cover to other land uses, and significant conservation efforts, including establishment of PAs covering 44% of the region (39). Further, data on other sociodemographic, climatic, and policy drivers are available at the municipal level (SI Appendix).
Our research responds to recent calls for policy driven studies that examine (i) multiple health outcomes, (ii) multiple ecosystem changes, (iii) human behaviors and policies, and (iv) differences across populations and places, to fill in key gaps in our understanding of ecosystem change and human health (6). Specifically, we examine policies that have been demonstrated to induce or prevent deforestation in the Amazon—roads, mines, and PAs—assessing the plausibility of their links with disease incidence. All of these policies can be manipulated to reduce deforestation, which in turn reduces air and water pollution from forest fires, erosion, and agriculture. Reduced deforestation can also prevent the proliferation of mosquito breeding sites and microclimates conducive to anopheline development and growth, and conserve biodiversity including mosquito predators and species that dilute the transmission of malaria itself (13, 40). However, as summarized in SI Appendix, Table S1, different policies for reducing deforestation could have very different effects on human exposure to disease, separate from any disease regulation resulting from ecosystem conservation. For example, strict PAs are likely to decrease exposure more than sustainable-use PAs (31). Roads increase mobility and hence both the spread of disease and access to medical services. Informal mining is associated with water pollution as well as working and living conditions that increase exposure to mosquitos. Thus, it is important to model the effects of real world conservation policies and not just the effects of ecosystem protection itself.
We expect PAs to be negatively related and roads and mines to be positively related to respiratory and diarrheal disease and malaria through their impacts on ecosystem processes, although their net effects will depend on all impact channels including exposure change (SI Appendix, Table S1). In addition, we model four diseases that serve as negative controls for the link between PAs and disease because they are not theoretically related to landscape level ecological changes: AIDS, dengue, arthritis, and leukemia (Materials and Methods).
Empirical examination of policies associated with ecosystem change poses two complications. First, there are clearly multiple factors that drive public health outcomes (19, 20). To estimate the effects of land-use change drivers, we need to control for factors such as sociodemographics, local climate, and healthcare. Second, some factors are time varying whereas others are time invariant. Panel estimation techniques take advantage of both types of data while estimating SEs consistent with the data structure. Thus, by estimating multivariate panel models, we can assess the importance of conservation policy levers for public health outcomes. For example, our results suggest that the expansion of the strict PAs between 1990 and 2010 reduced the incidence of all diseases considered, most notably malaria. Although the relationships are complex, we conclude that interventions to preserve natural capital can deliver cobenefits by also increasing human (health) capital.
Results
As described in Materials and Methods, we (i) assemble a comprehensive panel dataset on disease, demographic, socioeconomic, climatic, and land-use factors; and (ii) use rigorous statistical methods to isolate the links between potential policy levers for reducing deforestation and key disease outcomes. All data are collected at the level of a municipality in the Brazilian Amazon, which serves as the unit of analysis for our empirical work.
Land Uses.
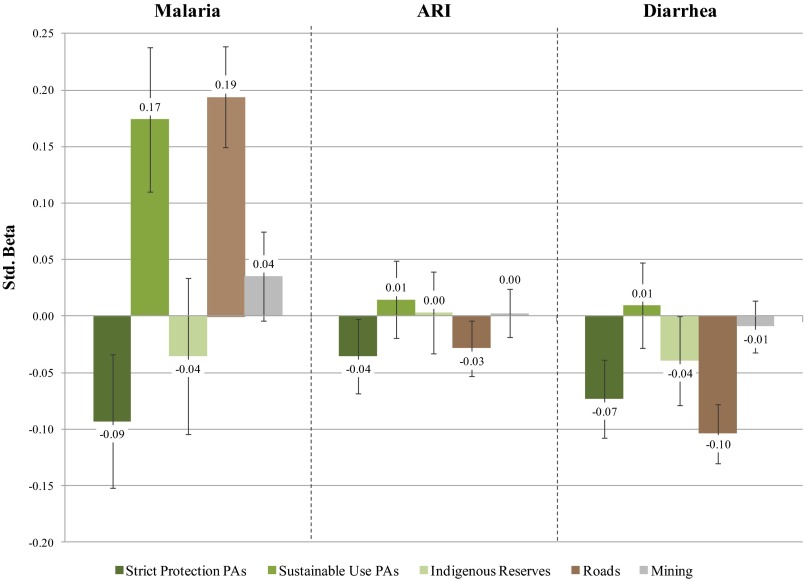
Fig. 1 shows that the type of PAs matter. We find that strict PAs are negatively correlated with the three major diseases: malaria, diarrhea, and acute respiratory infection (ARI). This may be because of the combined effects of reduced deforestation and reduced exposure, which mean that strict PAs can serve as a barrier to disease transmission (SI Appendix, Table S1). In support of that argument, we find that sustainable-use PAs, which allow for human use and/or occupation, are not associated with diarrhea and ARI and are positively correlated with malaria. We also find that indigenous reserves are negatively correlated only with diarrhea, possibly reflecting differences in health outcomes among the indigenous populations who live in those reserves. Turning to our negative controls, we find that as expected, strict PAs are not correlated with AIDS, dengue, arthritis, or leukemia.
Fig. 1.
Effects of land-use drivers on various diseases, based on random-effects regression results reported in SI Appendix, Table S6 and calculated as standardized coefficients, which offer a quick way to assess the relative importance of different predictors within a model. Whiskers depict 90% confidence intervals: If they cross 0, we cannot reject the null that there is no relationship between land-use drivers and disease.
Fig. 1 also shows that municipalities with more roads have higher rates of malaria but lower rates of diarrhea and ARI. This supports the contention that roads can plausibly both damage ecosystems and improve access to formal health services.
Other Covariates.
The full set of analyses is in SI Appendix, Table S6, including controls for the usual suspects correlated with prevention and treatment such as income, population, health services, remoteness (e.g., distance to capital), and climate. Here we briefly comment on select covariates. The number of migrants is positively correlated with each disease, which was expected because many of those migrants had little previous exposure and therefore lower natural immunity (41). Migrants often settle in frontier areas well before public health services are established, and migration can also lead to ecosystem degradation (35). Population is negatively correlated with diseases because it partly reflects the protective effect of urban services (public health, sewage, piped water, electricity) and partly the effect of wealth and education, over and above our other proxies for these factors. If we reestimate all models by dropping the most urban municipios, we find the population coefficient to be either statistically insignificant or positive and significant. Turning to bioclimatic factors, natural water bodies are positively correlated with all three diseases, altitude is negatively correlated with malaria, and in the summer higher temperature and rainfall (which could, for example, flush pathogens down river) are negatively correlated with all three diseases (23, 42, 43).
Level Matters (Quantile Regressions).
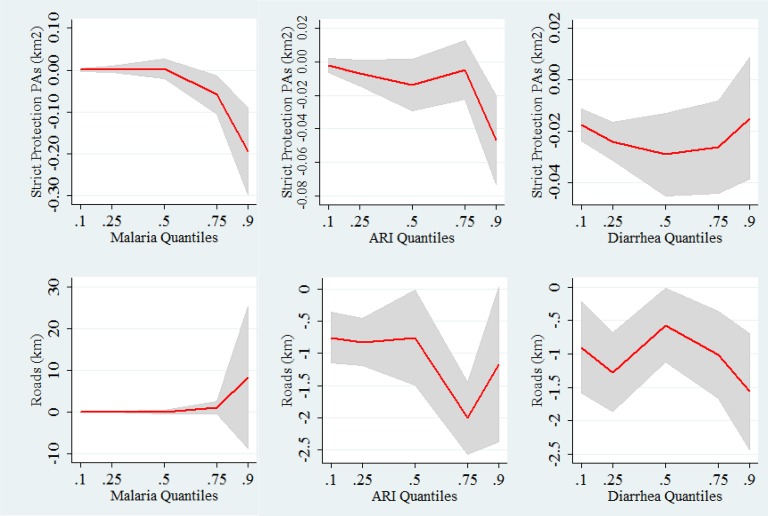
SI Appendix, Tables S8–S10 show quantile regression results, with model specifications identical to the random-effects models. These results show that at different levels of disease incidence, there are different associations: the size, sign, and significance of the estimated coefficients vary. We illustrate with two key variables—strict PAs and roads—in Fig. 2 and observe several patterns. First, quantile regression coefficients vary by quantiles. Second, strict PAs are negatively correlated with malaria in the 75th and 90th quantiles but with ARI only in the 90th quantile. In contrast, we see that strict PAs are negatively correlated with diarrhea at all points of the distribution, except at the 90th quantile. Third, roads are positively correlated with malaria only at the upper end of the distribution, whereas roads are positively correlated with diarrhea and ARI at all levels of the distribution. Thus, ecosystem mediation of health outcomes depends on not only the disease type but also its population incidence.
Fig. 2.
Comparison of coefficients and confidence intervals of quantile and random effects regressions for malaria, ARI, and diarrhea for strict PAs (1,000s of kilometers squared) and roads (kilometers). The red lines and gray-shaded areas depict quantile regression coefficients and 90% confidence intervals, respectively. Quantile regressions use bootstrapped SEs.
Discussion
Increasingly, the popular media and gray literature assert that human health depends on ecosystem health, despite the limited scientific evidence on the health benefits of ecosystem protection. There is even less evidence on the net effects of conservation policies (e.g., PAs) on human health (2, 18). We contribute to this thin literature by compiling a rich panel dataset on key diseases and potential contributing factors in the Brazilian Amazon. The data cover 4 years and 700 municipalities. Variables include demographic, socioeconomic, and bioclimatic factors, as well as deforestation drivers that are potential policy levers. Many of these have previously appeared separately in disease models but not all together in one model. With our more complete specification, we can evaluate the separate effects of land-use drivers on malaria, diarrhea, and ARI with greater confidence. Furthermore, we confirm these effects by finding no evidence of such links between ecosystem change and negative control diseases.
It is always possible that regression results are biased by omitted confounders, whether observed or unobserved. However, we consider it unlikely that the unexplained variation in public health (the statistical error) is meaningfully related to land-use factors such as placement of PAs and roads. More rigorous causal impact analysis could potentially generate precise estimates of how much a specific potential cause impacts a specific disease. However, the causal chain of environmental health is neither short nor simple (19, 20). Thus, more precise identification will require longer time series data on diseases, sociodemographic factors, and policies that vary over space as well as time. Our analysis of conservation health links should encourage future researchers to invest in building databases that can generate causal impact estimates to compare with our first-order estimates of the links between multiple health outcomes and multiple ecosystem changes.
In responding to calls for more research on the multiplicity of links between health and ecosystem changes, we focus on the policy drivers of those ecosystem changes (6): roads, mining, and three distinct types of PAs. We find statistically significant relationships with strict PAs and roads, even while controlling for a range of covariates that capture the influences of rural population, migration, rainfall, and temperature. The rainfall and temperature findings are important in and of themselves because regional climate change represents another long-term, large-scale feedback from deforestation and other ecosystem disturbances (44, 45). Malaria, diarrhea, and ARI are positively related to the number of migrants, likely through both the indirect link from migration to deforestation to diseases and the direct link of migrants being particularly vulnerable and infectious.
We also find that different policy levers for reducing deforestation have different net effects on disease, suggesting a variety of impact channels worthy of further investigation. First, we find mixed evidence on the influence of roads: They are associated with increases in malaria and decreases in diarrhea and ARI cases. This likely reflects their dual impacts on access to healthcare (manifested in reduced diarrhea and ARI) and disturbance of the natural ecosystem (manifested in increased malaria). Note that this is after controlling for income and for coverage of the Brazil’s Family Health Program [Programa Saúde da Familia (PSF)], two factors that are expected to increase with roads and improve health. Second, we find that only strict PAs reduce the incidence of all three diseases, probably because, in addition to slowing deforestation, they effectively discourage interaction between forest and susceptible people. A more complete list of potential mechanisms is summarized in SI Appendix, Table S1.
We can use the estimated coefficients from SI Appendix, Table S7 to evaluate policy scenarios, such as the expansion of strict PAs between 1990 and 2010 by 63%, for example. Our estimates suggest that this expansion reduced ARI, diarrhea, and malaria by 1.5%, 2%, and 6%, respectively, in an average municipality. It is difficult to benchmark these findings against (i) other conservation actions because the empirical evidence does not exist and (ii) public health interventions because they have different designs and contexts (e.g., targeting specific groups, not general populations). Nonetheless, our modeling of multiple drivers would also allow conservation planners to consider scenarios such as combining strict PAs with the complementary strategy of reducing roads, which together would have a much larger impact on malaria, for example.
In sum, we find evidence of health cobenefits from strict PAs that have been implemented for the primary purpose of preserving ecosystems but also have statistically significant negative correlations with malaria, ARI, and diarrhea. Other policies associated with land-use change—including roads, sustainable-use PAs, and mines—have mixed effects, perhaps because those policies influence health through many channels other than land use. For example, roads may reduce ARI and diarrhea because they improve access to healthcare, and sustainable-use PAs may increase malaria because they increase exposure to anopheline mosquitos. We caution that our analysis does not consider the full range of benefits or costs of different types of PAs, mining, or roads (18). However, from the perspectives of malaria, ARI, and diarrhea, our results suggest that the public health benefits of strict PAs may offset some of their local costs. Our takeaway is that nature is doing its part by providing a form of (human) capital for the rural poor and the politically voiceless.
Materials and Methods
Rich panel datasets are required to overcome the limitations of prior research identified by a recent review (6). We have compiled such a dataset on municipalities in the Brazilian Amazon, allowing us to estimate panel and quantile regressions with controls for many potential confounders. The dataset used in the analysis comprises 4 years (2003–2006) of annual municipality-level observations on cases of malaria, dengue, AIDS, arthritis, and leukemia in the population and cases of diarrhea and ARI in children under 2 years of age; health program coverage; and weather (rainfall and temperature). In addition, we compiled cross-sectional data for three categories of PAs, the presence of mining, official (planned) roads, population density, proportion of population living in rural areas, proportion of population that migrated to the municipality, gross domestic product (GDP), and extent of water bodies (rivers, lakes, wetlands) for about 700 municipalities in the Brazilian Amazon. Most data are available from the statistics department of the Brazilian public healthcare system DATASUS, the Brazilian Institute of Geography and Statistics (Rio de Janeiro), and Ministry of the Environment (Brasília, Brazil). Data on length of roads in each municipality were provided by the Amazon Institute of People and the Environment (IMAZON). The primary goal for building this dataset with multiple indicators for multiple cross-sectional units at multiple points in time is to identify the effects of deforestation drivers on health.
Descriptive Statistics.
In SI Appendix, Table S2, we report descriptive statistics for all 25 variables used in this analysis. Below we provide a brief narrative, beginning with the outcome variables and continuing with variables typically included in statistical models of health outcomes: (i) climate and biophysical characteristics (temperature, precipitation, altitude, and water bodies) and (ii) demographic and socioeconomic characteristics (population, health services, and income). While controlling for these factors, we focus on the influence of land-use drivers, including roads, mining, and three types of PAs.
Public health outcomes.
Malaria has been at the center of the debate over the relationship between public health and tropical deforestation. The Brazilian Ministry of Health (Brasília, Brazil) tracks the number of cases confirmed in each municipality in each year in the Sistema de Informação de Vigilânica Epidemiológica database. In the Amazon region as a whole, there were between 19 and 47 positive tests for every 1,000 people in the years from 1990 to 2010 (46). Malaria cases are unevenly distributed in the region, with about 60 municipalities accounting for 80% of all cases (47). Among the five major regions of Brazil, the Amazon (the North) has the highest proportion of deaths of children under five due to ARI (6.8% in 2005) and the second highest proportion due to diarrhea (6.2% in 2005) (46). The PSF has been credited with improving the quality of data available on these types of public health problems in the mostly poor, rural municipalities of the Amazon (48). We use data on cases in children under 2 years of age, as recorded in the Sistema de Informação de Atenção Básica database. The spatial patterns of these diseases are depicted in SI Appendix, Fig. S3.
Negative controls.
To check whether the estimated coefficients in models of malaria, ARI, and diarrhea could reflect underlying correlations between public health and placement of PAs, we also estimate models of dengue, AIDS, arthritis, and leukemia as negative controls that theory suggests are not related to landscape-level ecosystem change. Dengue is transmitted primarily in urban areas, where it has expanded rapidly in Brazil (49). Likewise, AIDS is a significant and growing public health concern in Brazil, including the Amazon. Arthritis and leukemia have no known conceptual or empirical links to conservation actions. However, because the land-use drivers have multiple impact channels, these negative controls may not be valid for all of them. For example, expansion of roads could increase AIDS because of the combination of long-distance truck drivers, susceptible migrants, and sex workers mixing along a dynamic frontier highway. Thus, these negative controls are best viewed as falsification tests only for the health impacts of PAs.
Climate.
There are two seasons, rainy (winter, defined as October to March) and dry (summer) in the Amazon. Average rainfall is 113 mm per month during winter and 64 mm per month during summer. Over one-third of municipalities have total annual rainfall over 2,300 mm. Average temperatures are approximately 27 °C. We also include a measure of altitude at the centroid and hectares covered in water in each municipality.
Demographics.
We include data on municipal population, percent of the population that migrated to the municipality, and percent of the population living in rural areas. On average, each municipality has 27,000 inhabitants, with 47% living in rural areas. There are 24,000 migrants on average in each municipality. The population of the Amazon includes a small fraction of indigenous people, a large traditional population (descended from earlier migrants to the region and of mixed indigenous, African, and European heritage), and people who were born in other parts of Brazil but moved to the Amazon in pursuit of economic opportunity. In most municipalities the migrant population is dominated by people who came from other parts of Brazil.
Socioeconomics.
The bidirectional relationship between health and wealth or income operates through many different channels. For example, the rich are better able to prevent and treat diseases. To control for the influence of income on health, we include municipal GDP in 2000, which averaged R$3,300 (∼US$1,200) per capita for the Brazilian Amazon as a whole. We measure the population’s access to healthcare with two variables. First is number of families served by the PSF, which was launched in 1994 as a strategy to expand healthcare coverage in underserved areas, including rural communities. During the time period of this study, the PSF rapidly expanded its coverage. In 2006, the PSF served 2,000 families per municipality on average in the Amazon region. Prior research has found the PSF to be effective at decreasing mortality rates among infants and children (50–52). The PSF could also be positively correlated with disease outcomes, as it might reflect the government’s response to high disease rates in some regions. Additionally, whereas the PSF provides basic healthcare through teams operating directly in the communities, more advanced medical care is available in regional cities. We control for variation in access to advanced healthcare, as well as markets, with distance (kilometers) from the municipality centroid to the state capital.
Land-use drivers.
The average size of the municipalities in our sample is 6,800 km2, with an average of 136 km2 in water. During the 4 years included in our sample, 40 km2 were deforested per year per municipality on average. Underlying drivers of deforestation and land use more generally include mining (36), roads (53), and PAs (54). Eleven percent of the municipalities have mineral-extraction activities, including both legal and informal mining activities. On average, each municipality has 21 km of official (paved) roads (SI Appendix, Fig. S4). We calculate the areas of each municipality in various categories of protection (SI Appendix, Fig. S5). The Brazilian National System of Conservation Units includes two broad categories: (i) sustainable-use PAs that allow people to live within their borders and harvest forest products sustainably; and (ii) strict PAs that have the primary objective of preserving biodiversity, allowing only indirect uses such as research. Indigenous reserves can also be considered PAs in that they encompass large tracts of forest where indigenous groups reside and use the forest for their livelihoods. More than 40% of an average municipality in the Brazilian Amazon were in PAs in 2006, including 14% in sustainable-use PAs, 7.5% in strict-protection PAs, and 21% in indigenous reserves (SI Appendix, Table S2). We include both state and federal PAs. There is considerable variation in the percent of municipalities in PAs. At the extremes, some municipalities have no PAs, whereas other municipalities are essentially contained entirely within PAs.
Statistical Methods.
Panel data expand both the sample size and the range of variation in key variables, which in our case are public health and land-use drivers. However, observations on the same municipality over the 4 years in our panel are clearly correlated and thus provide less “additional” information than simply more cross-sectional units. We therefore estimate an error components model that partitions the error into two independently and identically distributed random variables, one specific to the municipality and the other to the observation, in addition to a set of fixed municipality characteristics as covariates. This estimation approach is labeled multilevel, hierarchical, or random effects in different fields. The key results of interest are the coefficients (SI Appendix, Table S6) on the PAs (strict, sustainable use, and indigenous), roads (kilometers), and mining (presence or absence). To facilitate interpretation, in Fig. 1 we present standardized coefficients, which offer a quick way to assess the relative importance of different predictors within a model. Standardized coefficients have been more widely used in other social sciences (55) and recommended for use in ecology (56).
Our estimation procedure employs the variation both between and within municipalities over time to estimate the relationship between public health outcomes and land-use change drivers. We assume that the unexplained residual variation in the health outcome (the error) is unrelated to the land-use drivers, which largely reflect federal government decisions (about placement of roads and PAs) and the distribution of mineral resources. To assess whether our results could be due to some omitted variables that influence both land-use policies and public health, we estimate models of negative controls that have no theoretical relationship with rural ecosystems: dengue, arthritis, leukemia, and AIDS. As reported in Results, we do not identify spurious relationships between PAs and these health outcomes, confirming that our strategy is reasonable.
The error components (or random-effects) model estimates the relationship between mean health outcomes and climate, demography, income, and land use. However, these relationships may vary at different levels of health or disease (3). To assess whether the influence of land-use drivers varies with the level of disease, we estimate quantile regressions (57–59). In SI Appendix, Tables S8–S10, we report the marginal impacts of covariates on different points (10th, 25th, 50th, 75th, and 90th quantiles) of the conditional distribution of diseases. In Fig. 2, we show the quantile plots of these marginal effects for two key covariates (strict PAs and roads) for malaria, ARI, and diarrhea.
Supplementary Material
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1406495111/-/DCSupplemental.
References
- 1.Foley JA, et al. Global consequences of land use. Science. 2005;309(5734):570–574. doi: 10.1126/science.1111772. [DOI] [PubMed] [Google Scholar]
- 2.Locatelli B, et al. Facing an Uncertain Future: How Forest and People Can Adapt to Climate Change. Center for International Forestry Research; Bogor, Indonesia: 2008. [Google Scholar]
- 3.Pattanayak SK, et al. Evaluating the health impacts of climate change and conservation policies using applied CGE. BE J Econ Anal Poli. 2009;9(2):6. [Google Scholar]
- 4.Sachs J, Malaney P. The economic and social burden of malaria. Nature. 2002;415(6872):680–685. doi: 10.1038/415680a. [DOI] [PubMed] [Google Scholar]
- 5.Ezenwa VO, et al. Biodiversity loss affects global disease ecology. Bioscience. 2009;59(11):945–954. [Google Scholar]
- 6.Myers SS, et al. Human health impacts of ecosystem alteration. Proc Natl Acad Sci USA. 2013;110(47):18753–18760. doi: 10.1073/pnas.1218656110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pattanayak SK, Wendland KJ. Nature’s care: Diarrhea, watershed protection, and biodiversity conservation in Flores, Indonesia. Biodivers Conserv. 2007;16(1):2801–2819. [Google Scholar]
- 8.Pattanayak SK, Yasuoka J. Deforestation and Malaria: Revisiting the Human Ecology Perspective. Human Health and Forests: A Global Overview of Issues, Practice and Policy. Earthscan; Sterling, VA: 2008. pp. 197–217. [Google Scholar]
- 9.Prüss-Ustün A, Bonjour S, Corvalán C. The impact of the environment on health by country: A meta-synthesis. Environ Health. 2008;7(1):7. doi: 10.1186/1476-069X-7-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prüss-Ustün A, Corvalán C. How much disease burden can be prevented by environmental interventions? Epidemiology. 2007;18(1):167–178. doi: 10.1097/01.ede.0000239647.26389.80. [DOI] [PubMed] [Google Scholar]
- 11.Barrett CB, Travis AJ, Dasgupta P. On biodiversity conservation and poverty traps. Proc Natl Acad Sci USA. 2011;108(34):13907–13912. doi: 10.1073/pnas.1011521108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dasgupta P. 2013. Personal histories and poverty traps. Development Challenges in a Post-Crisis World, Annual Bank Conference on Development Economics 2011, eds Sepulveda C, Harrison A, Lin JY (World Bank, Washington, DC), pp 103–126.
- 13.Pattanayak S, et al. Deforestation, malaria, and poverty: A call for transdisciplinary research to support the design of cross-sectoral policies. Sustain Sci Pract Policy. 2006;2(2) [Google Scholar]
- 14.Confalonieri U, et al. 2007. Human health. Climate Change 2007: Impacts, Adaptation and Vulnerability, Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change, eds Parry ML, Canziani OF, Palutikof JP, van der Linden PJ, Hanson CE (Cambridge Univ Press, Cambridge, UK), pp 391–431.
- 15.Daily GC, Ehrlich PR. Global change and human susceptibility to disease. Annu Rev Energy Environ. 1996;21(1):125–144. [Google Scholar]
- 16.McMichael AJ. Prisoners of the proximate: Loosening the constraints on epidemiology in an age of change. Am J Epidemiol. 1999;149(10):887–897. doi: 10.1093/oxfordjournals.aje.a009732. [DOI] [PubMed] [Google Scholar]
- 17.Parkes M, Panelli R, Weinstein P. Converging paradigms for environmental health theory and practice. Environ Health Perspect. 2003;111(5):669–675. doi: 10.1289/ehp.5332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ferraro PJ, Lawlor K, Mullan KL, Pattanayak SK. Forest figures: Ecosystem services valuation and policy evaluation in developing countries. Rev Environ Econ Policy. 2012;6(1):20–44. [Google Scholar]
- 19.McMichael AJ. Environmental change, climate and population health: A challenge for inter-disciplinary research. Environ Health Prev Med. 2008;13(4):183–186. doi: 10.1007/s12199-008-0031-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McMichael AJ, et al. Globalization and the sustainability of human health. Bioscience. 1999;49(3):205–210. [Google Scholar]
- 21.Colwell RR. Global climate and infectious disease: The cholera paradigm. Science. 1996;274(5295):2025–2031. doi: 10.1126/science.274.5295.2025. [DOI] [PubMed] [Google Scholar]
- 22.McMichael AJ, Woodruff RE, Hales S. Climate change and human health: Present and future risks. Lancet. 2006;367(9513):859–869. doi: 10.1016/S0140-6736(06)68079-3. [DOI] [PubMed] [Google Scholar]
- 23.Olson SH, et al. Links between climate, malaria, and wetlands in the Amazon Basin. Emerg Infect Dis. 2009;15(4):659–662. doi: 10.3201/eid1504.080822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Paaijmans KP, Read AF, Thomas MB. Understanding the link between malaria risk and climate. Proc Natl Acad Sci USA. 2009;106(33):13844–13849. doi: 10.1073/pnas.0903423106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pascual M, Ahumada JA, Chaves LF, Rodó X, Bouma M. Malaria resurgence in the East African highlands: Temperature trends revisited. Proc Natl Acad Sci USA. 2006;103(15):5829–5834. doi: 10.1073/pnas.0508929103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Alisson FB, Sawyer DO, Soares-Filho BS. Population and land use effects on malaria prevalence in the southern Brazilian Amazon. Hum Ecol. 2005;33(6):847–874. [Google Scholar]
- 27.de Castro MC, Monte-Mór RL, Sawyer DO, Singer BH. Malaria risk on the Amazon frontier. Proc Natl Acad Sci USA. 2006;103(7):2452–2457. doi: 10.1073/pnas.0510576103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gushulak BD, MacPherson DW. Globalization of infectious diseases: The impact of migration. Clin Infect Dis. 2004;38(12):1742–1748. doi: 10.1086/421268. [DOI] [PubMed] [Google Scholar]
- 29.Haines A, Kovats RS, Campbell-Lendrum D, Corvalan C. Climate change and human health: Impacts, vulnerability and public health. Public Health. 2006;120(7):585–596. doi: 10.1016/j.puhe.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 30.Zelner JL, et al. Social connectedness and disease transmission: Social organization, cohesion, village context, and infection risk in rural Ecuador. Am J Public Health. 2012;102(12):2233–2239. doi: 10.2105/AJPH.2012.300795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hahn MB, et al. Conservation efforts and malaria in the Brazilian Amazon. Am J Trop Med Hyg. 2014;90(4):591–594. doi: 10.4269/ajtmh.13-0323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vittor AY, et al. Linking deforestation to malaria in the Amazon: Characterization of the breeding habitat of the principal malaria vector, Anopheles darlingi. Am J Trop Med Hyg. 2009;81(1):5–12. [PMC free article] [PubMed] [Google Scholar]
- 33.Yasuoka J, Levins R. Impact of deforestation and agricultural development on anopheline ecology and malaria epidemiology. Am J Trop Med Hyg. 2007;76(3):450–460. [PubMed] [Google Scholar]
- 34.Pattanayak SK, Pfaff A. Behavior, environment, and health in developing countries: Evaluation and valuation. Annu Rev Resour Econ. 2009;1(1):183–217. [Google Scholar]
- 35.Messina JP, Pan WK. Different ontologies: Land change science and health research. Curr Opin Environ Sustain. 2013;5(5):515–521. doi: 10.1016/j.cosust.2013.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Laurance WF, et al. Environment. The future of the Brazilian Amazon. Science. 2001;291(5503):438–439. doi: 10.1126/science.291.5503.438. [DOI] [PubMed] [Google Scholar]
- 37.Pfaff A, Amacher GS, Sills EO. Realistic REDD: Improving the forest impacts of domestic policies in different settings. Rev Environ Econ Policy. 2013;7(1):114–135. [Google Scholar]
- 38.Sanders D, Haines A. Implementation research is needed to achieve international health goals. PLoS Med. 2006;3(6):e186. doi: 10.1371/journal.pmed.0030186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Veríssimo A, Rolla A, Vedoveto M, Futada SdM. 2011. Protected Areas in the Brazilian Amazon: Challenges & Opportunities (Imazon, Belém, Brazil)
- 40.Laporta GZ, Lopez de Prado PI, Kraenkel RA, Coutinho RM, Sallum MA. Biodiversity can help prevent malaria outbreaks in tropical forests. PLoS Negl Trop Dis. 2013;7(3):e2139. doi: 10.1371/journal.pntd.0002139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ladeia-Andrade S, Ferreira MU, de Carvalho ME, Curado I, Coura JR. Age-dependent acquisition of protective immunity to malaria in riverine populations of the Amazon Basin of Brazil. Am J Trop Med Hyg. 2009;80(3):452–459. [PubMed] [Google Scholar]
- 42.Hoshen MB, Morse AP. A weather-driven model of malaria transmission. Malar J. 2004;3(1):32. doi: 10.1186/1475-2875-3-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pascual M, Dobson A. Seasonal patterns of infectious diseases. PLoS Med. 2005;2(1):e5. doi: 10.1371/journal.pmed.0020005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Myers SS, Patz JA. Emerging threats to human health from global environmental change. Annu Rev Environ Resour. 2009;34(1):223–252. [Google Scholar]
- 45.Patz JA, Campbell-Lendrum D, Holloway T, Foley JA. Impact of regional climate change on human health. Nature. 2005;438(7066):310–317. doi: 10.1038/nature04188. [DOI] [PubMed] [Google Scholar]
- 46. Rede Interagencial de Informações Para a Saúde. (2012) Basic Data and Indicators - Brazil. Available at tabnet.datasus.gov.br/cgi/idb2012/matriz.htm. Accessed May 9, 2014. [Google Scholar]
- 47.Pant K, Pattanayak S, Thakuri M. Climate change, cook stoves, and coughs and colds: Thinking global and acting local in rural Nepal. In: Barrett S, Mäler K, Maskin E, editors. Environment and Development Economics: Essays in Honor of Sir Partha Dasgupta. Oxford Univ Press; New York: 2014. pp. 145–168. [Google Scholar]
- 48.Rasella D, Aquino R, Barreto ML. Impact of the Family Health Program on the quality of vital information and reduction of child unattended deaths in Brazil: An ecological longitudinal study. BMC Public Health. 2010;10:380. doi: 10.1186/1471-2458-10-380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Teixeira MG, Costa MdaC, Barreto F, Barreto ML. Dengue: Twenty-five years since reemergence in Brazil. Cad Saude Publica. 2009;25(Suppl 1):S7–S18. doi: 10.1590/s0102-311x2009001300002. [DOI] [PubMed] [Google Scholar]
- 50.Aquino R, de Oliveira NFP, Barreto MLMDP. Impact of the family health program on infant mortality in Brazilian municipalities. Am J Public Health. 2009;99(1):87–93. doi: 10.2105/AJPH.2007.127480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Macinko J, Marinho de Souza MdeF, Guanais FC, da Silva Simões CC. Going to scale with community-based primary care: An analysis of the family health program and infant mortality in Brazil, 1999-2004. Soc Sci Med. 2007;65(10):2070–2080. doi: 10.1016/j.socscimed.2007.06.028. [DOI] [PubMed] [Google Scholar]
- 52.Rocha R, Soares RR. Evaluating the impact of community-based health interventions: Evidence from Brazil’s Family Health Program. Health Econ. 2010;19(Suppl):126–158. doi: 10.1002/hec.1607. [DOI] [PubMed] [Google Scholar]
- 53.Pfaff A, et al. Road investments, spatial spillovers, and deforestation in the Brazilian Amazon. J Reg Sci. 2007;47(1):109–123. [Google Scholar]
- 54.Miteva DA, Pattanayak SK, Ferraro PJ. Evaluation of biodiversity policy instruments: What works and what doesn’t? Oxf Rev Econ Policy. 2012;28(1):69–92. [Google Scholar]
- 55.Gelman A, Pardoe I. Average predictive comparison for models with nonlinearity, interactions and variance components. Sociol Methodol. 2007;37(1):23–51. [Google Scholar]
- 56.Schielzeth H. Simple means to improve the interpretability of regression coefficients. Method Ecol Evol. 2010;1(2):103–113. [Google Scholar]
- 57.Borooah VK. The height-for-age of Indian children. Econ Hum Biol. 2005;3(1):45–65. doi: 10.1016/j.ehb.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 58.Koenker R, Hallock KF. Quantile Regression. J Econ Perspect. 2001;15(4):143–156. [Google Scholar]
- 59.Rivera B, Currais L. 2005. Individual returns to health in Brazil: A quantile regression analysis. Health and Economic Growth: Findings and Policy Implications, eds Lopez-Casasnovas G, Rivera B, Currais L (MIT Press, Cambridge, MA) [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.