Abstract
Objectives
To estimate age-related changes for serum concentration of non–high-density lipoprotein cholesterol (HDL-C), describe non-HDL-C distribution, and examine the prevalence of high non-HDL-C levels in children and adolescents by demographic characteristics and weight status.
Study design
Data from 7058 participants ages 6–19 years in the 2005–2010 National Health and Nutrition Examination Surveys were analyzed. A high level of non-HDL-C was defined as a non-HDL-C value ≥145mg/dL.
Results
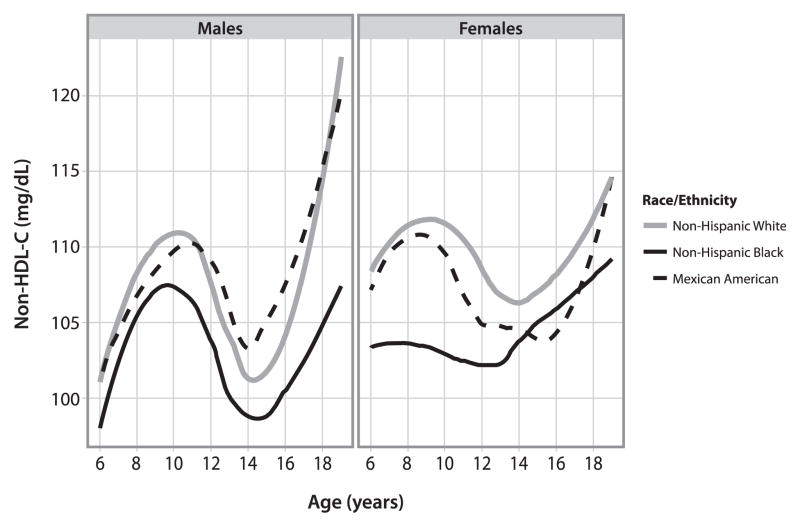
Locally weighted scatterplot smoothing–smoothed curves showed that non-HDL-C levels increased from 101 mg/dL at age 6 to 111 mg/dL at age 10, decreased to 101 mg/dL at age 14, and then increased to 122 mg/dL at age 19 in non-Hispanic white males. Non-HDL-C levels generally were greater in female than male subjects, lower in non-Hispanic black subjects, and similar in male and slightly lower in female Mexican American subjects, compared with non-Hispanic white subjects. The overall mean was 108 (SE 0.5), and the percentiles were 67 (5th), 74 (10th), 87 (25th), 104 (50th), 123 (75th), 145 (90th), and 158 (95th) mg/dL. Mean and percentiles were greater among age groups 9–11 and 17–19 years than others and greater among non-Hispanic white than non-Hispanic black subjects. The prevalence of high non-HDL-C was 11.8% (95% CI 9.9%–14.0%) and 15.0% (95% CI 12.9%–17.3%) for the age groups 9–11 and 17–19, respectively. It varied significantly by race/ethnicity and overweight/obesity status.
Conclusion
Non-HDL-C levels vary by age, sex, race/ethnicity, and weight classification status. Evaluation of non-HDL-C in youth should account for its normal physiologic patterns and variations in demographic characteristics and weight classification.
Non–high-density lipoprotein cholesterol (HDL-C) is a combined measure of the cholesterol content of all atherogenic apolipoprotein B–containing lipoproteins.1,2 Childhood non-HDL-C is considered as good as or better than other lipid measures, including low-density lipoprotein cholesterol (LDL-C), in predicting adult dyslipidemia and subclinical atherosclerosis.3,4 Recently, on the basis of a comprehensive evidence review, the Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents concluded that early identification and control of dyslipidemia throughout youth and into adulthood would substantially reduce the risk of clinical cardiovascular disease beginning in young adult life.5 The guidelines recommended universal screening with nonfasting non-HDL-C among children and adolescents, first at ages 9–11 years and again at ages 17–21 years, as the first step in identifying children and adolescents with lipid disorders that predispose them to accelerated atherosclerosis.5 This approach has a major advantage in that, unlike calculated LDL-C, which is influenced by the presence of postprandial hypertriglyceridemia, non-HDL-C can be accurately determined by subtracting high-density lipoprotein cholesterol (HDL-C) from total cholesterol (TC) in a nonfasting state and is therefore practical in a clinical setting.2
A non-HDL-C value of ≥145 mg/dL is used to identify a dyslipidemic state in children and adolescents up to 19 years of age.5 Although the cut points for evaluation of TC and LDL-C are based on the 75th and 95th percentile estimates from the Lipid Research Clinics Prevalence Study data,6 the definition for non-HDL-C is derived from the Bogalusa Heart Study.7 Non-HDL-C cut points from a local biracial community study, although useful in isolation, would most likely not represent the intended percentile values of non-HDL-C for the US population, resulting in uncertainty about positive screening results in the population. Nationally representative data on the detailed distribution of non-HDL-C have been scant with respect to their age-related changes, mean, median, and percentile values by sex, race/ethnicity, and other correlates.8
Using data from the National Health and Nutrition Examination Survey (NHANES), we sought to estimate changes related to age in serum concentrations of non-HDL-C by sex and race/ethnicity for children and adolescents aged 6–19 years; to describe the distribution of non-HDL-C in terms of mean and percentile by age, sex, and race/ethnicity; and to examine the prevalence of high non-HDL-C levels in children and adolescents by demographic characteristics, weight status, and socioeconomic status (family income).
Methods
NHANES is designed to assess the health and nutritional status of the civilian, noninstitutionalized US population and collects data from a nationally representative sample of survey participants via household interviews and physical examinations in a mobile examination center. Survey protocol was reviewed and approved by the National Center for Health Statistics ethics review board. Participants provided written informed consent before participation. Detailed information about NHANES procedures is available elsewhere.9 For our analyses, we used data collected from participants ages 6–19 years during the 2005–2006, 2007–2008, and 2009–2010 cycles of NHANES. Of the 8275 6- to 19-year-old respondents examined, we excluded 1217 with missing TC or HDL-C, leaving 7058 children and adolescents, representing 85.3% of the total available sample size.
Blood specimens provided by participants during the physical examination were stored at –20°C and shipped weekly for laboratory analyses. TC and HDL-C levels were based on samples taken regardless of fasting state. For NHANES 2005–2006, TC and HDL-C were measured enzymatically in serum with Hitachi 717 and Hitachi 912 (Roche Diagnostics, Indianapolis, Indiana) at Johns Hopkins University. For NHANES 2007–2008 and 2009–2010, the testing was performed at the University of Minnesota, and the equipment used was the Roche Modular P chemistry analyzer (Roche Diagnostics). Despite changes in equipment and laboratory sites, laboratory method was essentially the same, and both laboratories participated in the Centers for Disease Control and Prevention’s (CDC) Lipid Standardization Program (http://www.cdc.gov/labstandards/lsp.html). We calculated non-HDL-C as (TC – HDL-C) and defined a high non-HDL-C as a non-HDL-C value ≥145mg/dL.
To describe the distribution of non-HDL-C by demographic characters and explore the difference in prevalence of high non-HDL-C by weight and socioeconomic status, age, sex, race/ethnicity, body mass index (BMI), waist circumference, and poverty index were included in the analysis as covariates. Race/ethnicity was classified as non-Hispanic white, non-Hispanic black, Mexican American, or other. The group indicated as “other” was included in overall estimates, but, because it is a heterogeneous group with a limited sample size, results for this group are not separately reported. BMI was calculated as weight in kilograms divided by height in meters squared (kg/m2). To account for variability by age and sex, all BMI measures were compared with age- and sex-specific reference values from the 2000 CDC growth charts to define the weight status.10 Normal weight was defined as a BMI-for-age-sex of <85th percentile, overweight as a BMI-for-age-sex of the 85th to <95th percentile, and obesity as a BMI-for-age-sex of ≥95th percentile.11 In our analysis, we collapsed the overweight and obese categories into a single weight-status category, “overweight/obese.”
Waist circumference was measured to the nearest 0.1 cm at the high point of the iliac crest at minimal respiration while in a standing position. It was compared with reference data for the US population and categorized in the current analysis into 2 groups: those ≥90th percentile and those <90th percentile for sex and age.12
Poverty index is a ratio measuring the household income to the poverty threshold after accounting for inflation and family size. For example, the poverty threshold for a family of 4 with 2 children younger than 18 years of age in 2010 was $22 113. Therefore, a poverty index of 200% (2.0) for a family of 4 in 2010 was equivalent to approximately $44 000 annual household income. We categorized the poverty index to <200% (2.0) vs≥200% (2.0) in our analysis. In 2010, 31.3% of children and adolescents <18 years had a poverty index <200% (2.0) in the US.13
Statistical Analyses
Locally weighted scatterplot smoothing (Lowess), a robust smoothing technique, was used to graphically examine levels of non-HDL-C by age.14 These curves were constructed within each race-sex group with the ggplot2 package [Wickham’12] in R.15
We calculated the weighted means (±SE) and percentiles of non-HDL-C by age, sex and race/ethnicity and used LOGISTIC procedure in SUDAAN to estimate the unadjusted prevalence, prevalence ratio of high non-HDL-C, and their 95% CIs16 in each of the strata defined by age, sex, race/ethnicity, weight status, and poverty index. Examination sample weights were used in all analyses to adjust for unequal sampling probabilities and SAS-callable SUDAAN, version 9.2 (RTI International, Research Triangle Park, North Carolina) was used for the analyses taking into account for the complex sampling design.
Results
Lowess-smoothed curves for non-HDL-C levels vs age are plotted and presented in the Figure. In non-Hispanic white males, non-HDL-C level increased from 101 mg/dL at age 6 years to 111 mg/dL at age 10 years, decreased to 101 mg/dL at age 14 years, and then increased sharply to approximately 122 mg/dL at age 19 years. Non-HDL-C levels fluctuated similarly, although to a lesser degree, in non-Hispanic white females; however, it appeared generally greater than in non-Hispanic white males, except for those aged 17 years and older. In both males and females, the non-HDL-C curve was about 5 mg/dL or more lower in non-Hispanic blacks than in non-Hispanic whites. It was also lower in female Mexican Americans than in female non-Hispanic whites.
Figure.
Lowess-smoothed curves for serum non-HDL-C levels vs age, by sex, and race/ethnicity—NHANES, 2005–2010.
The overall mean non-HDL-C level was 108 (SE 0.5) and the percentiles were 67 (5th), 74 (10th), 87 (25th), 104 (50th), 123 (75th), 145 (90th), and 158 (95th) mg/dL (Table I). With a few exceptions, means and percentiles of non-HDL-C were greater among those aged 9–11 and 17–19 than among other age groups. Age- and sex-specific mean and percentile values of non-HDL-C generally were greater in female than in male subjects except for those aged 17–19 years and for the 90th and 95th percentiles, where non-HDL-C values generally were greater in male than in female subjects. The mean value of non-HDL-C was 5 mg/dL lower in non-Hispanic blacks than in non-Hispanic whites. Age-specific means and percentiles were also lower in non-Hispanic blacks than in non-Hispanic whites, with rare exceptions. The overall mean of non-HDL-C was 108 mg/dL in Mexican Americans, 1 mg/dL lower than that in non-Hispanic whites. However, we observed no consistent pattern in age-specific mean and percentile values of non-HDL-C between these 2 racial/ethnic groups. Among non-Hispanic whites and non-Hispanic blacks, means and percentiles were greater in female than in male subjects, except for the 90th and 95th percentiles. Among Mexican Americans, the 5th percentile of non-HDL-C was greater, and the 75th through 95th percentiles were lower in female than in male subjects.
Table I.
Serum non-HDL-C levels among US children ages 6–19 years by age, sex, and race/ethnicity—NHANES, 2005–2010
| Characteristics | n* | Mean (SE), mg/dL | Percentiles, mg/dL
|
||||||
|---|---|---|---|---|---|---|---|---|---|
| 5 | 10 | 25 | 50 | 75 | 90 | 95 | |||
| Age, y | |||||||||
| 6–8 | 1326 | 107 (1.2) | 69 | 76 | 89 | 104 | 121 | 142 | 152 |
| 9–11 | 1502 | 110 (0.8) | 68 | 75 | 89 | 107 | 127 | 146 | 160 |
| 12–14 | 1539 | 105 (1.2) | 65 | 72 | 85 | 102 | 120 | 139 | 154 |
| 15–16 | 1090 | 104 (1.2) | 68 | 75 | 84 | 99 | 120 | 140 | 154 |
| 17–19 | 1601 | 112 (1.1) | 68 | 77 | 89 | 107 | 128 | 154 | 171 |
| Total (6–19) | 7058 | 108 (0.5) | 67 | 74 | 87 | 104 | 123 | 145 | 158 |
| Sex and age, y | |||||||||
| Male | |||||||||
| 6–8 | 686 | 105 (1.5) | 65 | 73 | 87 | 102 | 117 | 138 | 152 |
| 9–11 | 742 | 110 (1.2) | 67 | 74 | 89 | 107 | 127 | 147 | 162 |
| 12–14 | 779 | 104 (1.7) | 62 | 69 | 84 | 99 | 119 | 143 | 157 |
| 15–16 | 572 | 102 (1.9) | 65 | 74 | 83 | 96 | 117 | 140 | 155 |
| 17–19 | 841 | 113 (1.7) | 68 | 78 | 89 | 107 | 131 | 157 | 174 |
| Total (6–19) | 3620 | 107 (0.7) | 65 | 73 | 86 | 102 | 123 | 146 | 161 |
| Female | |||||||||
| 6–8 | 640 | 110 (1.4) | 72 | 80 | 91 | 107 | 125 | 145 | 152 |
| 9–11 | 760 | 110 (1.5) | 69 | 77 | 90 | 107 | 127 | 145 | 157 |
| 12–14 | 760 | 106 (1.3) | 69 | 73 | 87 | 104 | 121 | 138 | 149 |
| 15–16 | 518 | 106 (1.2) | 69 | 76 | 85 | 102 | 122 | 140 | 152 |
| 17–19 | 760 | 111 (1.4) | 68 | 76 | 89 | 107 | 125 | 149 | 166 |
| Total (6–19) | 3438 | 109 (0.8) | 70 | 76 | 88 | 105 | 123 | 144 | 156 |
| Race/ethnicity and age, y | |||||||||
| Non-Hispanic white | |||||||||
| 6–8 | 383 | 107 (1.9) | 67 | 75 | 88 | 104 | 121 | 143 | 152 |
| 9–11 | 433 | 111 (1.5) | 67 | 75 | 89 | 107 | 129 | 148 | 160 |
| 12–14 | 420 | 106 (1.9) | 67 | 72 | 86 | 103 | 121 | 140 | 157 |
| 15–16 | 347 | 104 (1.7) | 69 | 76 | 84 | 99 | 120 | 140 | 151 |
| 17–19 | 458 | 114 (1.7) | 69 | 79 | 90 | 108 | 130 | 157 | 174 |
| Total (6–19) | 2041 | 109 (0.8) | 68 | 75 | 88 | 104 | 124 | 147 | 160 |
| Non-Hispanic black | |||||||||
| 6–8 | 316 | 103 (1.2) | 68 | 73 | 86 | 101 | 118 | 135 | 144 |
| 9–11 | 366 | 106 (1.4) | 67 | 74 | 85 | 104 | 122 | 140 | 150 |
| 12–14 | 426 | 102 (1.7) | 61 | 70 | 81 | 98 | 118 | 137 | 149 |
| 15–16 | 291 | 103 (1.7) | 61 | 71 | 83 | 97 | 120 | 139 | 151 |
| 17–19 | 471 | 106 (1.6) | 62 | 71 | 86 | 103 | 123 | 144 | 156 |
| Total (6–19) | 1870 | 104 (0.8) | 63 | 72 | 84 | 101 | 120 | 139 | 151 |
| Mexican American | |||||||||
| 6–8 | 410 | 107 (2.0) | 68 | 76 | 87 | 104 | 121 | 142 | 157 |
| 9–11 | 468 | 109 (1.1) | 69 | 75 | 91 | 106 | 122 | 144 | 160 |
| 12–14 | 483 | 105 (1.5) | 67 | 73 | 86 | 102 | 121 | 141 | 153 |
| 15–16 | 299 | 105 (1.4) | 65 | 72 | 84 | 99 | 123 | 142 | 156 |
| 17–19 | 467 | 112 (1.8) | 68 | 75 | 91 | 109 | 128 | 153 | 168 |
| Total (6–19) | 2127 | 108 (0.9) | 68 | 74 | 88 | 104 | 123 | 144 | 159 |
| Sex and race/ethnicity | |||||||||
| Non-Hispanic white | |||||||||
| Male | 1069 | 108 (1.1) | 66 | 74 | 86 | 102 | 123 | 147 | 163 |
| Female | 972 | 110 (1.2) | 70 | 77 | 89 | 107 | 125 | 146 | 157 |
| Non-Hispanic black | |||||||||
| Male | 950 | 103 (1.1) | 61 | 71 | 83 | 100 | 119 | 140 | 153 |
| Female | 920 | 105 (1.0) | 66 | 73 | 86 | 103 | 121 | 138 | 147 |
| Mexican American | |||||||||
| Male | 1081 | 108 (0.9) | 67 | 74 | 88 | 104 | 125 | 146 | 161 |
| Female | 1046 | 107 (1.4) | 69 | 74 | 87 | 104 | 122 | 142 | 157 |
Sample size.
The overall prevalence of high non-HDL-C was 10.7% (95% CI 9.6%-11.9%) (Table II). The prevalence was greater among those 9–11 years of age (11.8%; 95% CI 9.9%–14.0%) and 17–19 years old (15.0%; 95% CI 12.9%–17.3%) than in other age groups. It was similar among male (11.2%) and female (10.1%) subjects. The prevalence of high non-HDL-C was significantly lower among non-Hispanic blacks overall (7.7%; 95% CI: 6.7%, 8.9%) and among those aged 9–11 years (6.9%; 95% CI 4.8%–9.8%) and 17–19 years (10.3%; 95% CI 7.9%–13.2%) than among non-Hispanic whites (11.5% [95% CI 9.9%–13.4%] overall; 13.5% [95% CI 10.5%–17.1%] for those ages 9–11 years; and 17.0% [95% CI 13.8%–20.8%] for those ages 17–19 years, respectively). When we compared the prevalence ratio of high non-HDL-C in non-Hispanic blacks with non-Hispanic whites in the overall group and in those ages 9–11 years and 17–19 years, the results were 0.67 (95% CI 0.54–0.82), 0.51 (95% CI 0.33–0.79), and 0.60 (95% CI 0.44–0.83), respectively.
Table II.
Prevalence and prevalence ratio of high serum non-HDL-C levels* among US children ages 6–19 years by age, sex, and race/ethnicity—NHANES, 2005–2010
| Characteristics | Prevalence
|
Prevalence ratio
|
|
|---|---|---|---|
| n† | % (95% CI) | (95% CI) | |
| Age, y | |||
| 6–8 | 106 | 9.0 (7.3–11.0) | 1.00 |
| 9–11 | 153 | 11.8 (9.9–14.0) | 1.31 (1.03–1.66) |
| 12–16 | 228 | 8.4 (6.9–10.2) | 0.93 (0.71–1.21) |
| 17–19 | 224 | 15.0 (12.9–17.3) | 1.66 (1.33–2.08) |
| Total (6–19) | 711 | 10.7 (9.6–11.9) | |
| Sex and age, y | |||
| 6–8 | |||
| Male | 46 | 7.3 (5.0–10.4) | 1.00 |
| Female | 60 | 11.0 (8.2–14.6) | 1.51 (0.91–2.5) |
| 9–11 | |||
| Male | 82 | 12.8 (10.1–16.1) | 1.00 |
| Female | 71 | 10.8 (7.7–14.8) | 0.84 (0.54–1.31) |
| 12–16 | |||
| Male | 133 | 9.3 (7.2–12.0) | 1.00 |
| Female | 95 | 7.5 (5.5–10.1) | 0.80 (0.54–1.19) |
| 17–19 | |||
| Male | 124 | 16.4 (13.0–20.5) | 1.00 |
| Female | 100 | 13.4 (10.6–16.7) | 0.81 (0.57–1.15) |
| Total (6–19 | |||
| Male | 385 | 11.2 (9.7–12.9) | 1.00 |
| Female | 326 | 10.1 (8.6–11.8) | 0.90 (0.73–1.11) |
| Race/ethnicity and age, y | |||
| 6–8 | |||
| Non-Hispanic white | 35 | 9.1 (6.7–12.4) | 1.00 |
| Non-Hispanic black | 17 | 5.5 (3.1–9.4) | 0.60 (0.29–1.22) |
| Mexican American | 34 | 8.8 (5.5–13.8) | 0.96 (0.58–1.59) |
| 9–11 | |||
| Non-Hispanic white | 55 | 13.5 (10.5–17.1) | 1.00 |
| Non-Hispanic black | 25 | 6.9 (4.8–9.8) | 0.51 (0.33–0.79) |
| Mexican American | 45 | 9.8 (7.6–12.6) | 0.73 (0.52–1.04) |
| 12–16 | |||
| Non-Hispanic white | 69 | 8.5 (6.2–11.5) | 1.00 |
| Non-Hispanic black | 52 | 7.6 (6.1–9.5) | 0.90 (0.63–1.28) |
| Mexican American | 78 | 9.0 (6.9–11.6) | 1.06 (0.70–1.60) |
| 17–19 | |||
| Non-Hispanic white | 84 | 17.0 (13.8–20.8) | 1.00 |
| Non-Hispanic black | 53 | 10.3 (7.9–13.2) | 0.60 (0.44–0.83) |
| Mexican American | 62 | 12.9 (9.9–16.6) | 0.76 (0.55–1.05) |
| Total (6–19) | |||
| Non-Hispanic white | 243 | 11.5 (9.9–13.4) | 1.00 |
| Non-Hispanic black | 147 | 7.7 (6.7–8.9) | 0.67 (0.54–0.82) |
| Mexican American | 219 | 9.9 (8.6–11.5) | 0.86 (0.70–1.06) |
A high level of non-HDL-C was defined as serum non-HDL-C concentration ≥145 mg/dL.
Number of subjects with high level of non-HDL-C.
The prevalence of high non-HDL-C consistently was greater in overweight/obese groups than in normal-weight groups in overall comparisons and in age-specific subgroups, with prevalence ratios ranging from 2.50 (95% CI 1.86–3.37) among those aged 17–19 years to 3.27 (95% CI 2.28–4.71) among those aged 9–11 years (Table III). The prevalence of high non-HDL-C was also consistently greater in those with a waist circumference ≥90th percentile than those with a waist circumference <90th percentile in each of the age groups, with prevalence ratios ranging from 2.58 (95% CI 1.94–3.42) among those aged 17–19 years to 3.59 (95% CI 2.56–5.03) among those ages 12–16 years. The prevalence ratios for low poverty index groups were not significantly different from that for the high poverty index groups in any age strata, as indicated by the 95% CIs of corresponding prevalence ratios.
Table III.
Prevalence and prevalence ratio of high serum non-HDL-C levels* among US children ages 6–19 years by weight status, waist circumference category, and poverty index—NHANES, 2005–2010
| Characteristics | Prevalence
|
Prevalence ratio
|
|
|---|---|---|---|
| n† | % (95% CI) | (95% CI) | |
| Age, y | |||
| Overweight/obesity‡ status | |||
| 6–8 | |||
| Normal weight | 44 | 6.2 (4.4–8.5) | 1.00 |
| Overweight/obese | 62 | 16.1 (12.0–21.4) | 2.62 (1.65–4.17) |
| 9–11 | |||
| Normal weight | 52 | 6.5 (4.6–9.1) | 1.00 |
| Overweight/obese | 101 | 21.3 (17.5–25.7) | 3.27 (2.28–4.71) |
| 12–16 | |||
| Normal weight | 72 | 4.9 (3.4–7.1) | 1.00 |
| Overweight/obese | 151 | 14.4 (11.7–17.5) | 2.93 (1.99–4.32) |
| 17–19 | |||
| Normal weight | 81 | 9.7 (7.5–12.4) | 1.00 |
| Overweight/obese | 135 | 24.2 (20.1–29.0) | 2.50 (1.86–3.37) |
| Total (6–19) | |||
| Normal weight | 249 | 6.5 (5.5–7.8) | 1.00 |
| Overweight/obese | 449 | 18.3 (16.3–20.5) | 2.80 (2.32–3.39) |
| Waist circumference | |||
| 6–8 y | |||
| <90th percentile | 73 | 7.5 (5.8–9.6) | 1.00 |
| ≥90th percentile | 32 | 21.1 (14.4–30.0) | 2.83 (1.82–4.39) |
| 9–11 y | |||
| <90th percentile | 99 | 9.2 (7.2–11.5) | 1.00 |
| ≥90th percentile | 53 | 30.3 (23.6–38.0) | 3.31 (2.37–4.62) |
| 12–16 y | |||
| <90th percentile | 139 | 6.3 (4.8–8.3) | 1.00 |
| ≥90th percentile | 80 | 22.7 (18.3–27.9) | 3.59 (2.56–5.03) |
| 17–19 y | |||
| <90th percentile | 142 | 11.7 (9.4–14.4) | 1.00 |
| ≥90th percentile | 71 | 30.1 (23.9–37.2) | 2.58 (1.94–3.42) |
| Total (6–19 y) | |||
| <90th percentile | 453 | 8.3 (7.1–9.6) | 1.00 |
| ≥90th percentile | 236 | 26.0 (22.7–29.7) | 3.14 (2.59–3.81) |
| Poverty index§ | |||
| 6–8 y | |||
| Poverty index <2 | 58 | 8.2 (5.8–11.5) | 0.85 (0.48–1.50) |
| Poverty index ≥2 | 41 | 9.6 (6.7–13.6) | 1.00 |
| 9–11 y | |||
| Poverty index <2 | 86 | 11.7 (9.0–15.1) | 0.99 (0.69–1.41) |
| Poverty index ≥2 | 59 | 11.8 (9.3–14.9) | 1.00 |
| 12–16 y | |||
| Poverty index <2 | 134 | 9.9 (7.9–12.3) | 1.27 (0.98–1.65) |
| Poverty index ≥2 | 84 | 7.7 (6.0–9.9) | 1.00 |
| 17–19 y | |||
| Poverty index <2 | 125 | 14.4 (11.9–17.3) | 0.92 (0.67–1.27) |
| Poverty index ≥2 | 78 | 15.6 (12.1–19.9) | 1.00 |
| Total (6–19 y) | |||
| Poverty index <2 | 403 | 10.9 (9.6–12.4) | 1.04 (0.86–1.24) |
| Poverty Index ≥2 | 262 | 10.6 (9.0–12.3) | 1.00 |
A high level of non-HDL-C was defined as serum non-HDL-C concentration ≥145 mg/dL.
Number of subjects with a high level of non-HDL-C.
Normal weight defined as age- and sex-specific BMI of <85th percentile of CDC BMI-for-age growth charts (http://www.cdc.gov/growthcharts), overweight as age- and sex-specific BMI of 85th to <95th percentile of CDC BMI-for-age growth charts, and obesity as age- and sex-specific BMI of ≥95th percentile of the CDC BMI-for-age growth charts.
Poverty index is the ratio of a family’s income to the poverty threshold defined by the US Census Bureau (www.census.gov/hhes/www/poverty/data/threshld/index.html), appropriate to the family’s composition.
Discussion
In the current study we examine the natural development with age of non-HDL-C levels in children and adolescents by using the latest nationally representative data, demonstrate smoothed non-HDL-C curves by age for sex and racial/ethnic subgroups, and provide reference values on non-HDL-C distribution among children and adolescents in the US. The analysis further estimates the prevalence of high non-HDL-C in US children and adolescents according to the definition set by the Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents. Our findings demonstrate that non-HDL-C levels in children and adolescents vary with age, sex, and race/ethnicity and that the prevalence of high non-HDL-C in overweight/obese youth is nearly 3 times that of those with normal weight.
Data from NHANES and other population studies have been used previously to document the detailed distribution of lipid components, including TC, LDL-C, HDL-C, and triglycerides, with respect to their age-related mean, median, and percentile values by sex and race/ethnicity.17–19 However, data on the distribution of non-HDL-C in children and adolescents are limited.8 The distribution data are critical for establishing diagnostic criteria to identify children with adverse non-HDL-C levels and for monitoring the effectiveness of interventions to improve blood lipid profiles in the community.
On the basis of data collected between 1992 and 1994 from 2843 5- to 17-year-old Bogalusa Heart Study participants that characterized non-HDL-C levels by broad age categories (5–11 and 12–17 years) and by sex and race (white and black),7 the Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents recently defined non-HDL-C values for children of <120, 120–144, and ≥145 mg/dL as acceptable, borderline high, and high, respectively.5 These values are similar to the National Cholesterol Education Program Pediatric Panel definitions for LDL-C (<110, 110–129, and ≥130 mg/dL, respectively).6
It is well known that TC and LDL-C decrease during early teen years and increase again steadily in late adolescence and that HDL-C decreases during the first one-half of teen years in male, but not in female subjects.17–20 For example, Dai et al20 found that HDL-C increased sharply from age 14 years to age 18 years in female but to a lesser degree in male subjects from ages 16–18 years. Also, non-HDL-C levels generally were lower in 12- to 17-year-olds than in 5- to 11-year-olds in sex-and race-specific subgroups in the Bogalusa Heart Study.7 A recent report from NHANES 2007–2010 found mean non-HDL-C levels of 105, 109, 102, and 112 mg/dL among those aged 6–8, 9–11, 12–15, and 16–19 years, respectively.8 Findings in the current analysis, shown both as age-related curves of non-HDL-C and as the means and percentiles within sex- or racial/ethnic-specific age groups, demonstrated similar age-related changes in non-HDL-C: a decrease during early teen years of life and an increase afterwards. This finding adds to the concept that 9–11 years of age is the best age range for universal lipid screening in childhood. Non-HDL-C was generally, although only slightly, lower in male than in female subjects in our study, which is consistent with previous reports.7,8 However, the mean level in males exceeded that in females during ages 17–19 years in our study. The changes in sex-related difference in non-HDL-C levels reflect the changes reported earlier in both TC and HDL-C during the teen years of life, especially the steady increase in HDL-C in the late teen years among females.20
It is of interest to note that the current study, based on recent NHANES data, found non-HDL-C levels in non-Hispanic blacks were approximately 5 mg/dL lower than in non-Hispanic whites. Earlier reports have been inconsistent in racial comparisons of non-HDL-C in children. Data from the NHANES III and the Bogalusa Heart Study showed no black-white differences in non-HDL-C levels,7,21 and findings from Project HeartBeat! found a 9 mg/dL lower non-HDL-C in black children than in whites aged 8–18 years.22 Geographic differences and differential secular changes in non-HDL-C level among different racial/ethnic groups may account for the inconsistent findings.
According to the latest recommendations,5 12.4 million children aged 9–11 years and 13.5 million adolescents aged 17–19 years in 2010 would need to be screened for non-HDL-C levels. According to our findings, when they are screened, 11.8% in the 9- to 11-year age group and 15.0% in the 17- to 19-year age group—a total of about 3.5 million children and adolescents—would be found to have high non-HDL-C and would need further evaluation with a fasting lipid profile. The variation in mean and percentile values of non-HDL-C by age, sex, and race/ethnicity with a fixed cut point, that is, ≥145 mg/dL, for the diagnosis of high level of non-HDL-C would result in various proportions of positives in population subgroups.
The prevalence of high non-HDL-C is found to be greater in non-Hispanic white than in non-Hispanic black subjects within the recommended-for-screening age groups, greater in those 9–11 and 17–19 years of age than in other age groups, and, although not statistically significant, slightly greater in male than in female subjects within each age group except for those 6–8 years of age. This finding is consistent with the shape of non-HDL-C curves and percentile distributions of non-HDL-C by age, sex, and race/ethnicity in our results. The mean non-HDL-C was slightly greater in female compared with male subjects. However, there was a greater prevalence of high non-HDL-C in male subjects because there were more male than female subjects in the upper 90th percentile of the distribution.
The current data show a consistently greater prevalence of non-HDL-C in overweight/obese groups than in normal-weight groups, and in those with a waist circumference ≥90th percentile for sex and age than in those with a lower waist circumference percentile, stratified by age. This finding underscores the fact that obesity in childhood is associated with an increase in apolipoprotein B–containing atherogenic particles. Earlier studies have demonstrated the association between adiposity and atherogenic blood lipid levels in children and adolescents.23–29 A dose–response relationship between the prevalence of abnormal lipid levels—including high LDL-C, low HDL-C, and high triglycerides—and weight classification (ie, normal weight, overweight, and obese) among adolescents was reported using recent NHANES data.30,31 Non-HDL-C has also been shown to be independently associated with obesity measures, including BMI, percent body fat, waist circumference, abdominal circumference, and measures of skinfold thickness.7,22
One of the limitations in the current study is the potential selection bias because of the relatively high proportion of the study sample (14.7%) with missing values for TC and HDL-C. The proportions of missing values are greater among younger study participants and lower among Mexican Americans compared with other groups, although they are not significantly different by sex, body weight, waist circumference, and poverty index. Missing values in Mexican Americans should have only a minor effect on overall estimates of non-HDL-C levels, because non-HDL-C levels among Mexican Americans are mostly between that of non-Hispanic whites and non-Hispanic blacks. The proportion of missing by age may have a slight effect on the overall estimates of non-HDL-C levels. However, it should not affect the age-specific estimation of non-HDL-C in our analysis. Another limitation is the change in equipment and laboratory sites for TC and HDL-C testing between the NHANES 2005–2006 and NHANES 2007–2008/2009–2010. However, both Johns Hopkins University and the University of Minnesota laboratories participated in CDC’s Lipid Standardization Program. Adherence to the standardization criteria should make testing results from these 2 laboratories comparable. The main strengths of the current study include the use of nationally representative data and NHANES’ sampling approach that allow comparisons across racial/ethnic groups.
The current analysis provides detailed data on the distribution of non-HDL-C in children and adolescents. Non-HDL-C levels and the prevalence of high non-HDL-C vary by age, sex, race/ethnicity, and overweight/obesity status. Following the most recent expert panel recommendations, approximately 1 in 9 children aged 9–11 years and 1 in 7 adolescents aged 17–19 years will be identified as having high non-HDL-C level and will require further evaluation. The numbers change to 1 in 5 and 1 in 4 among overweight/obese children and adolescents, respectively. These findings have important public health implications. Age- and sex-specific cut points for acceptable, borderline-high, and high non-HDL-C levels should be determined on the basis of available population data so that evaluation of non-HDL-C could account for normal physiologic developmental patterns and for variations in demographic characteristics. Non-HDL-C is a useful measure of atherogenic particles and may be especially helpful in children who are overweight and obese in whom LDL-C levels alone may not be the best measure of risk of atherosclerosis. Children with overweight and obesity should be evaluated with non-HDL-C, and those with increased levels should be targeted for lipid-lowering interventions.
Acknowledgments
We acknowledge David S. Freedman, PhD (Division of Nutrition, Physical Activity, and Obesity, CDC), for his insightful review of the report and help with the Lowess-smoothed curves.
Glossary
- BMI
Body mass index
- CDC
Centers for Disease Control and Prevention
- HDL-C
High-density lipoprotein cholesterol
- LDL-C
Low-density lipoprotein cholesterol
- Lowess
Locally weighted scatterplot smoothing
- NHANES
National Health and Nutrition Examination Survey
- TC
Total cholesterol
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. The authors declare no conflicts of interest.
References
- 1.Miller M, Ginsberg HN, Schaefer EJ. Relative atherogenicity and predictive value of non-high-density lipoprotein cholesterol for coronary heart disease. Am J Cardiol. 2008;101:1003–8. doi: 10.1016/j.amjcard.2007.11.046. [DOI] [PubMed] [Google Scholar]
- 2.National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–421. [PubMed] [Google Scholar]
- 3.Frontini MG, Srinivasan SR, Xu J, Tang R, Bond MG, Berenson GS. Usefulness of childhood non-high density lipoprotein cholesterol levels versus other lipoprotein measures in predicting adult subclinical atherosclerosis: The Bogalusa Heart Study. Pediatrics. 2008;121:924–9. doi: 10.1542/peds.2007-1472. [DOI] [PubMed] [Google Scholar]
- 4.Srinivasan SR, Frontini MG, Xu J, Berenson GS. Utility of childhood non-high-density lipoprotein cholesterol levels in predicting adult dyslipidemia and other cardiovascular risks: The Bogalusa Heart Study. Pediatrics. 2006;118:201–6. doi: 10.1542/peds.2005-1856. [DOI] [PubMed] [Google Scholar]
- 5.Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents. Expert Panel on Integrated Guidelines for Cardiovascular Health and Risk Reduction in Children and Adolescents: Summary report. Pediatrics. 2011;128(Suppl 5):S213–56. doi: 10.1542/peds.2009-2107C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Cholesterol Education Program. . Report of the Expert Panel on Blood Cholesterol Levels in Children and Adolescents. Pediatrics. 1992;89:525–84. [PubMed] [Google Scholar]
- 7.Srinivasan SR, Myers L, Berenson GS. Distribution and correlates of non-high-density lipoprotein cholesterol in children: The Bogalusa Heart Study. Pediatrics. 2002;110:e29. doi: 10.1542/peds.110.3.e29. [DOI] [PubMed] [Google Scholar]
- 8.Kit BK, Carroll MD, Lacher DA, Sorlie PD, DeJesus JM, Ogden CL. Trends in serum lipids among US youths aged 6 to 19 years, 1988–2010. JAMA. 2012;308:591–600. doi: 10.1001/jama.2012.9136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.National Center for Health Statistics. National Health and Nutrition Examination Survey. [August 2012];Questionnaires, Datasets, and Related Documentation. Accessed, http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm.
- 10.Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat. 2002;11:1–190. [PubMed] [Google Scholar]
- 11.Ogden CL, Flegal KM. Changes in terminology for childhood overweight and obesity. Natl Health Stat Report. 2010:1–5. [PubMed] [Google Scholar]
- 12.McDowell MA, Fryar CD, Hirsch R, Ogden CL. Anthropometric reference data for children and adults: U.S. population, 1999–2002. Adv Data. 2005:1–5. [PubMed] [Google Scholar]
- 13.US Census Bureau. [August 2012];Poverty thresholds. Assessed http://www.census.gov/hhes/www/poverty/data/threshld/index.html.
- 14.Cleveland W. The elements of graphing data. Belmont (CA): Wadsworth Publ Co; 1985. [Google Scholar]
- 15.Wickham H, Chang C. ggplot2: An implementation of the Grammar of Graphics. http://cran.r-project.org/web/packages/ggplot2/index.html.
- 16.Bieler GS, Brown GG, Williams RL, Brogan DJ. Estimating model-adjusted risks, risk differences, and risk ratios from complex survey data. Am J Epidemiol. 2010;171:618–23. doi: 10.1093/aje/kwp440. [DOI] [PubMed] [Google Scholar]
- 17.Hickman TB, Briefel RR, Carroll MD, Rifkind BM, Cleeman JI, Maurer KR, et al. Distributions and trends of serum lipid levels among United States children and adolescents ages 4–19 years: data from the Third National Health and Nutrition Examination Survey. Prev Med. 1998;27:879–90. doi: 10.1006/pmed.1998.0376. [DOI] [PubMed] [Google Scholar]
- 18.Jolliffe CJ, Janssen I. Distribution of lipoproteins by age and gender in adolescents. Circulation. 2006;114:1056–62. doi: 10.1161/CIRCULATIONAHA.106.620864. [DOI] [PubMed] [Google Scholar]
- 19.Tamir I, Heiss G, Glueck CJ, Christensen B, Kwiterovich P, Rifkind BM. Lipid and lipoprotein distributions in white children ages 6–19 yr. The Lipid Research Clinics Program Prevalence Study. J Chronic Dis. 1981;34:27–39. doi: 10.1016/0021-9681(81)90079-5. [DOI] [PubMed] [Google Scholar]
- 20.Dai S, Fulton JE, Harrist RB, Grunbaum JA, Steffen LM, Labarthe DR. Blood lipids in children: age-related patterns and association with body-fat indices: Project HeartBeat! Am J Prev Med. 2009;37:S56–64. doi: 10.1016/j.amepre.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 21.Winkleby MA, Robinson TN, Sundquist J, Kraemer HC. Ethnic variation in cardiovascular disease risk factors among children and young adults: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. JAMA. 1999;281:1006–13. doi: 10.1001/jama.281.11.1006. [DOI] [PubMed] [Google Scholar]
- 22.Dai S, Steffen M, Mihalopoulos N, Labarthe DR. Non-HDL Cholesterol in children: age-related patterns and association with body fat indices, Project Heartbeat! (abstract) Circulation. 2011;124:A15802. [Google Scholar]
- 23.Freedman DS, Dietz WH, Srinivasan SR, Berenson GS. The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa Heart Study. Pediatrics. 1999;103:1175–82. doi: 10.1542/peds.103.6.1175. [DOI] [PubMed] [Google Scholar]
- 24.Friedland O, Nemet D, Gorodnitsky N, Wolach B, Eliakim A. Obesity and lipid profiles in children and adolescents. J Pediatr Endocrinol Metab. 2002;15:1011–6. doi: 10.1515/JPEM.2002.15.7.1011. [DOI] [PubMed] [Google Scholar]
- 25.Morrison JA, Barton BA, Biro FM, Daniels SR, Sprecher DL. Overweight, fat patterning, and cardiovascular disease risk factors in black and white boys. J Pediatr. 1999;135:451–7. doi: 10.1016/s0022-3476(99)70167-8. [DOI] [PubMed] [Google Scholar]
- 26.Morrison JA, Sprecher DL, Barton BA, Waclawiw MA, Daniels SR. Overweight, fat patterning, and cardiovascular disease risk factors in black and white girls: the National Heart, Lung, and Blood Institute Growth and Health Study. J Pediatr. 1999;135:458–64. doi: 10.1016/s0022-3476(99)70168-x. [DOI] [PubMed] [Google Scholar]
- 27.Srinivasan SR, Myers L, Berenson GS. Rate of change in adiposity and its relationship to concomitant changes in cardiovascular risk variables among biracial (black-white) children and young adults: the Bogalusa Heart Study. Metabolism. 2001;50:299–305. doi: 10.1053/meta.2001.21019. [DOI] [PubMed] [Google Scholar]
- 28.Thompson DR, Obarzanek E, Franko DL, Barton BA, Morrison J, Biro FM, et al. Childhood overweight and cardiovascular disease risk factors: the National Heart, Lung, and Blood Institute Growth and Health Study. J Pediatr. 2007;150:18–25. doi: 10.1016/j.jpeds.2006.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Venegas HL, Perez CM, Suarez EL, Guzman M. Prevalence of obesity and its association with blood pressure, serum lipids and selected lifestyles in a Puerto Rican population of adolescents 12–16 years of age. Puerto Rico Health Sci J. 2003;22:137–43. [PubMed] [Google Scholar]
- 30.May AL, Kuklina EV, Yoon PW. Prevalence of cardiovascular disease risk factors among US adolescents, 1999–2008. Pediatrics. 2012;129:1035–41. doi: 10.1542/peds.2011-1082. [DOI] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention. Prevalence of abnormal lipid levels among youths—United States, 1999–2006. MMWR. 2010;59:29–33. [PubMed] [Google Scholar]