Abstract
Background
The incidence of adverse events with non-cardiac procedures (NCP) after the use of drug eluting stents (DES) is not well studied. We sought to determine the incidence and temporal trends of adverse events in patients undergoing NCP after coronary DES.
Methods
We performed a retrospective review of patients receiving DES during percutaneous coronary intervention (PCI) in the Lexington VAMC between 1/1/04 and 12/31/10 to determine the circumstances and the results of their NCP.
Results
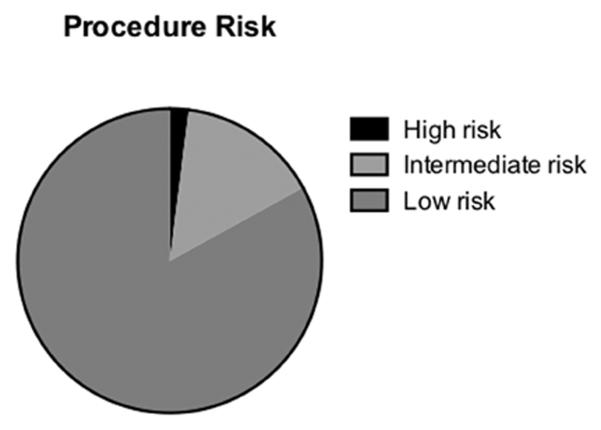
We identified 1092 patients who underwent at least 1 PCI with DES who were followed for at least 3 years. Of those, 452 patients (41%) had a NCP at a median of 534 days after PCI with 1081 procedures (894 low-, 160 Intermediate- and 27 high-risk) performed. Clinically relevant NCP-related complications were defined as significant bleeding or stent thrombosis and occurred in 13 individuals (9 peri-operative bleeding and 4 probable/possible stent thrombosis including 2 mortalities). Five adverse events occurred within the first year at a rate of 0.014 event/patient-year. During the remainder of follow up (up to 9 years), 8 events were documented at a rate of 0.0004 event/patient-years. During the first year of follow-up, there was no significant increase in risk of recurrent myocardial infarction (MI) or target vessel revascularization (TVR) in patients undergoing NCP but higher risk of all cause mortality in those who did not undergo NCP. However, in patients who underwent NCP, there was a statistically significant increase in myocardial infarction (MI), target vessel revascularization (TVR), and rehospitalization for cardiac reasons compared to those without NCP during long term follow up (median of 5.6 years).
Conclusion
NCP after DES requiring management of DAT are relatively common among veterans following PCI using DES. The risk of bleeding and stent thrombosis is concentrated in the first year but remains very low.
Keywords: non-cardiac procedures, drug eluting stents, dual antiplatelet therapy, percutaneous coronary intervention, adverse events
Introduction
In 2003, the FDA approved the use of the first generation of Drug Eluting Stents (DES) which significantly reduced the rate of restenosis and need for repeat revascularization (1). However, DES use was associated with a small but statistically significant increased risk of stent thrombosis when dual antiplatelet therapy (DAT) with aspirin and a P2Y12 inhibitor is prematurely discontinued. Acknowledging this risk, the FDA and the national practice guidelines recommended the continuation of DAT for at least one year in patients who are revascularized with DES as opposed to 30 days for bare metal stents (2-6).
It is not infrequent that patients require a non-cardiac surgery or procedure (NCP) within the timeframe for which DAT is recommended after DES. The incidence of surgical intervention has been reported as high as 9.2% within 1 year, 15.2% to 18% within 2 years, 22% at 3 years, and 26% at 5 years in prior studies (7-10). The performance of NCP while the patient is on DAT increases the risk of perioperative bleeding. In addition, the surgical condition represents a procoagulant state due to activation of tissue factor with endothelial damage and if DAT is held there is concern for increased risk of stent thrombosis (11,12). Thus, optimal management of these patients is required to balance the risk of stent thrombosis while holding DAT with the increased bleeding risks associated with continuation of DAT. Recent data suggest that the temporary interruption of DAT (particularly clopidogrel) may be safe after the first to sixth months following PCI (13,14). To improve our understanding of how to treat these patients, we performed a large retrospective analysis of all veterans needing NCP after having DES placed in a tertiary Veterans Affairs Medical Center. We examined the rates of perioperative complications such as bleeding and stent thrombosis. We also examined the short- and long-term incidence of other major cardiac complications such as all cause mortality, recurrent myocardial infarction, repeat revascularization, need for target vessel revascularization and rehospitalizations for cardiac indications.
Methods
All patients who received at least one drug eluting stent (DES) during percutaneous coronary artery intervention between January 1, 2004 and December 31, 2010 at the VA Medical Center in Lexington, KY were enrolled. Using the VA’s computerized patient record system (CPRS) a “Health Summary” document was created that compiled information for procedures performed at the VA Medical Center since 2004. This document was reviewed to identify patients who had undergone any procedures since their initial percutaneous interventions, allowing the target sample to be identified. The charts of those who had procedures were then reviewed to determine the circumstances, results and peri-operative complications of their non-cardiac surgeries or procedures. We examined the charts for patients who suffered major complications for DAT in the perioperative/peri-procedure period.
We categorized NCP based on the current ACC/AHA guidelines for perioperative cardiovascular evaluation into high- (aortic, major vascular surgery, and peripheral vascular surgery), intermediate- (intrathoracic, intraperitoneal, orthopedic, head and neck surgery, carotid endarterectomy and prostate surgery) and low-risk (ambulatory, breast, cataract surgeries as well as superficial and endoscopic procedures) categories (15). Operative reports and progress notes during the perioperative period were reviewed to identify complications. Clinically relevant NCP-related complications were defined as significant bleeding or stent thrombosis. In addition, major cardiovascular adverse outcomes (death, recurrent myocardial infarction [MI], repeat revascularization, cardiac rehospitalization and target vessel revascularization [TVR]) were noted for all included patients. A bleeding complication was defined as a decrease in hemoglobin of ≥ 3g/dL in the setting of clinical concern for bleeding or transfusion requirement. Stent thrombosis was classified into possible, probably and definite events reported according to ARC criteria (16).
Numerical data are presented as mean ± standard error and compared between two groups using student T test. Categorical data are presented as number (percent) or as percent ± standard error and compared between two groups using a chi-square test or Fisher’s exact test. Kaplan-Meier analyses were performed to explore the associations between NCP and cardiac mortality, TVR, and recurrent myocardial infarction (MI) regarded as time-to-event endpoints. We also fit Cox proportional hazards regression models for these three endpoints in which NCP was treated as a time-dependent dichotomous covariate; hence, not only ‘whether’ but also ‘when’ a person transitioned from not undergoing NCP to undergoing NCP was taken into account, mitigating the crossover bias inherent to Kaplan-Meier analyses. In addition, we fit versions of the Cox models in which we adjusted for potential confounding factors such as stent type, diabetes mellitus, hypertension, hyperlipidemia, chronic kidney disease and tobacco use. A P value < 0.05 was used as a cutoff for statistical significance throughout the analyses.
Results
We identified 1092 patients who underwent at least 1 PCI with DES between January 1, 2004 and December 31, 2010. Patients were followed up for a median duration of 5.6 years (interquartile range 3.3-7.3 years). Of those, 452 patients (41%) underwent 1081 non-cardiac procedures (894 low-, 160 Intermediate- and 27 high-risk) (Figure 1) with a median duration of 523 days between the index PCI and NCP (interquartile range 243-1064 days). 118 of these patients (11%) underwent NCP in the first year following PCI. When comparing patients who underwent NCP versus those who did not, there were significantly larger fractions of patients with diabetes mellitus (DM), chronic kidney disease (CKD), and first generation stents among those who underwent NCP; otherwise, there were no significant differences in the baseline characteristics of those who underwent NCP and those who did not (Table 1). The majority of NCP were performed during the first 3 years after the index PCI (Suppl. Figure 1).
Figure 1. The distribution of patients among the various risk non-cardiac procedures.
Pie graph demonstrating the distribution of patients among the various risk procedures. Most of the patients underwent low risk procedures (see methods for details).
Table 1.
Baseline characteristics of study population.
| Non-cardiac procedures N=449 |
No procedures N=634 |
P
value |
|
|---|---|---|---|
| Age | 65.9±0.5 | 65.7±0.4 | 0.66 |
| HTN (%) | 403 (90) | 565 (90) | 0.9 |
| Tobacco use (%) |
169 (38) | 219 (35) | 0.31 |
| Chronic kidney disease (%) |
105 (23) | 84 (13) | <0.001 |
| Statin use (%) | 400 (89) | 568 (90) | 0.66 |
| Hyperlipidemia (%) |
395 (88) | 567 (90) | 0.33 |
| DM (%) | 244 (54) | 296 (47) | 0.02 |
| First generation DES (%) |
369 (82) | 384 (61) | <0.001 |
| Second generation DES (%) |
80 (18) | 247 (39) | <0.001 |
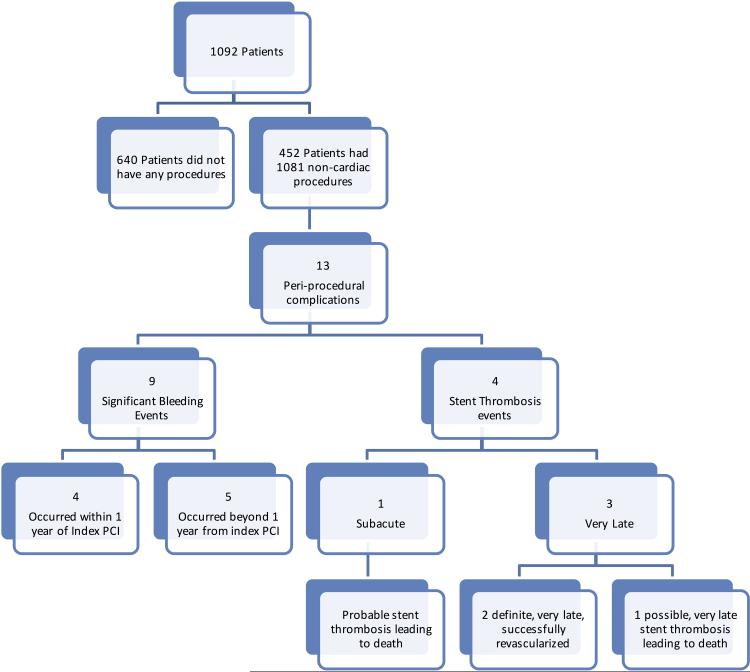
Major complications during follow up, defined as peri-operative significant bleeding or stent thrombosis, occurred in 13 individuals. Supplemental Table 1 details the major complications and the circumstances that could be obtained from the medical records. Five of the major complications occurred within the first year at a rate of 0.014 events/patient-year. Nine patients experienced peri-operative bleeding events (4 within one year of DES placement and 5 beyond the first year after DES PCI) (Figure 2). There were no mortality events in patients who had bleeding complications. Overall, all bleeding events occurred in patients were at least one antiplatelet agent was continued perioperatively. On the other hand, all stent thrombosis events occurred in patients with both antiplatelet agents being discontinued.
Figure 2.
Flow chart summarizing the incidence of complications in the study sample.
Four patients had events of probable/possible stent thrombosis; among them there were two mortalities (Figure 2). One mortality occurred early after DES placement when the patient developed serious post-operative complications requiring placement of a feeding tube. Prior to that procedure, DAT was stopped and vitamin K was given to reverse the effects of concomitant warfarin therapy. The patient developed cardiac arrest and died after 24 hours. The second mortality event occurred as a possible very late stent thrombosis in a patient who underwent hip surgery and had a NSTEMI on recovering from anesthesia with chest pain and positive biomarkers. Medical therapy for the NSTEMI was initiated but the patient developed cardiac arrest and died on the 4th postoperative day. Stent thrombosis occurred mostly in patients treated with first generation DES (3 out of 4) and all of them interrupted their DAT for their planned procedure.
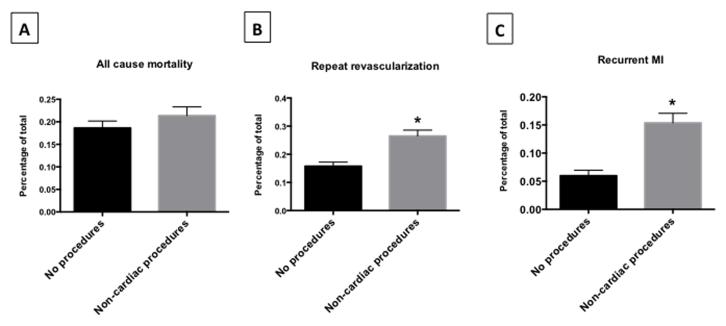
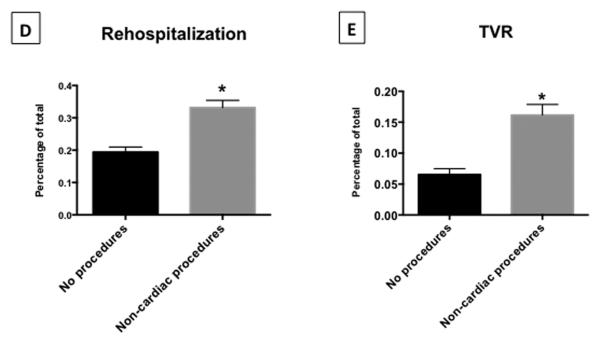
During the remainder of follow up (up to 8.8 years), 8 events were documented at a rate of 0.0004 events/patient-year. During the long-term follow-up, there was no significant difference in unadjusted overall mortality between patients with and without NCP (Table 2 and Figure 3). However, in patients who underwent NCP, there was a significantly higher incidence of repeat revascularization, myocardial infarction (MI), target vessel revascularization (TVR), and rehospitalization for cardiac reasons (Table 2 and Figure 3).
Table 2.
Clinical outcomes at longest follow up.
| Non-cardiac procedures N=449 |
No procedures N=634 |
P
value |
|
|---|---|---|---|
| All cause mortality: N (%) |
90 (20) | 120 (19) | 0.5 |
| Repeat revascularization: N (%) |
119 (27) | 100 (16) | <0.001 |
| Rehospitalization: N (%) |
149 (33) | 123 (19) | <0.001 |
| TVR: N (%) | 74 (17) | 43 (7) | <0.001 |
| Recurrent MI: N (%) |
72 (16) | 38 (6) | <0.001 |
Patients were followed up for a median duration of 5.6 years (interquartile range 3.3-7.3 years of follow up).
Figure 3.
Bar graphs demonstrating the rates of clinically important adverse events in patients who underwent non-cardiac procedures vs. those who did not The rate of all cause mortality (Panel A) did not differ significantly among the study groups. However, the rates of repeat revascularization (Panel B), recurrent myocardial infarction (Panel C), rehospitalizations (Panel D) and target vessel revascularization (Panel E) were higher in patients who underwent non-cardiac procedures.
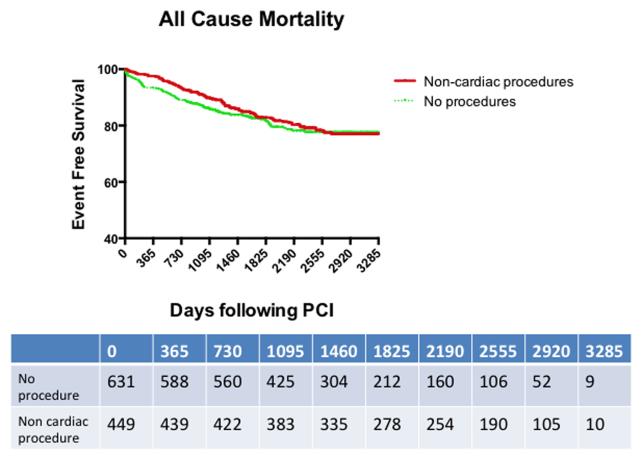
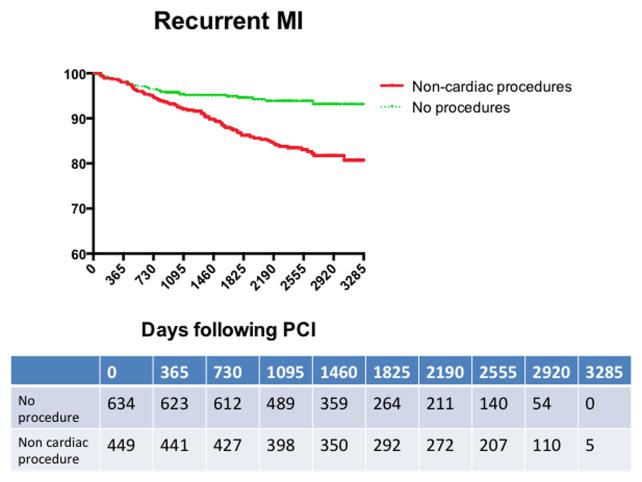
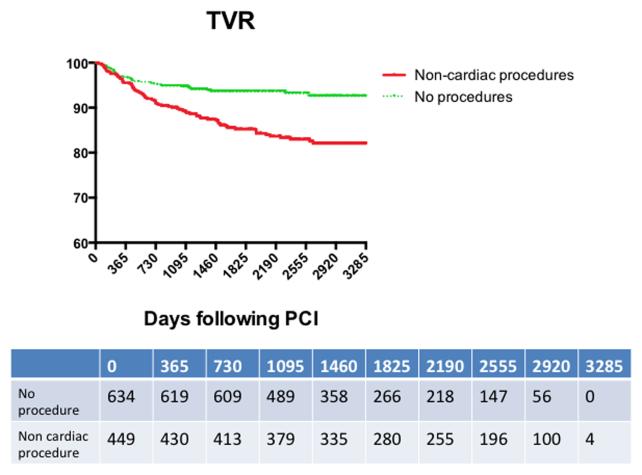
Kaplan-Meier curves were created to depict event free survival after the index PCI for all cause mortality, recurrent myocardial infraction (MI) and target vessel revascularization (TVR) among patients who underwent NCP and those who did not. The unadjusted all cause mortality curves were similar for both groups (Figure 4). On the other hand, unadjusted event free survival for recurrent MI and TVR was significantly worse in the patients who underwent NCP. Upon visual inspection of the Kaplan-Meier curves, the initial separations occurred at least 1 year after the index PCI (Figures 5 and 6). Most patients who underwent NCP did so within 2 years after DES implantation. Most adverse events occurred within the first 3 years following NCP (Suppl. Figure 2).
Figure 4. Kaplan-Meier curves demonstrating the event free survival from all cause mortality throughout the follow up duration.
The rates of all cause mortality were higher in patients who did not undergo non-cardiac procedures for the first 4 years following their index PCI. However, the curves overlapped after the fourth year and there was no statistically significant difference in the overall analysis. The numbers in the table represent the numbers still at risk for the endpoint at the indicated time points.
Figure 5. Kaplan-Meier curves demonstrating the event free survival from recurrent myocardial infarction throughout the follow up duration.
The overall rates of recurrent myocardial infarction were higher in patients who underwent non-cardiac procedures at the end of study follow-up. However, the curves did not start separating until after the first year after the index percutaneous coronary intervention. The numbers in the table represent the numbers still at risk for the endpoint at the indicated time points.
Figure 6. Kaplan-Meier curves demonstrating the event free survival from target vessel revascularization throughout the follow up duration.
The overall rates of target vessel revascularization were higher in patients who underwent non-cardiac procedures at the end of study follow-up. However, the curves did not start separating until after the first year after the index percutaneous coronary intervention. The numbers in the table represent the numbers still at risk for the endpoint at the indicated time points.
We elected to examine the data for the first year following PCI since this is the time period currently recommended for DAT. The rates of TVR and recurrent MI during the first year after deploying DES were similar between patients who underwent NCP and those who did not (Table 3). On the other hand, all cause mortality was higher among patients who did not undergo NCP (Table 3).
Table 3.
Clinical outcomes at 1 year.
| Non-cardiac procedures N=449 |
No procedures N=634 |
P
value |
|
|---|---|---|---|
| All cause mortality: N (%) |
11 (2) | 46 (7) | <0.001 |
| TVR: N (%) | 19 (4) | 20 (3) | 0.4 |
| Recurrent MI: N (%) |
9 (2) | 12 (2) | 1 |
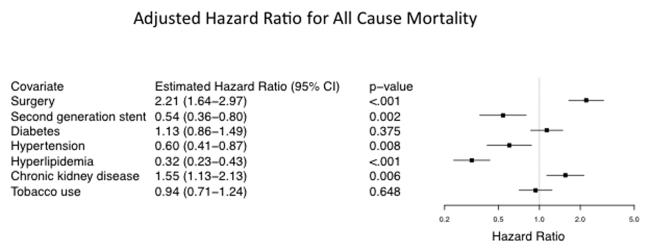
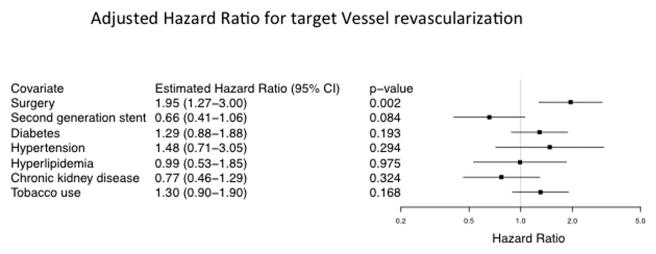
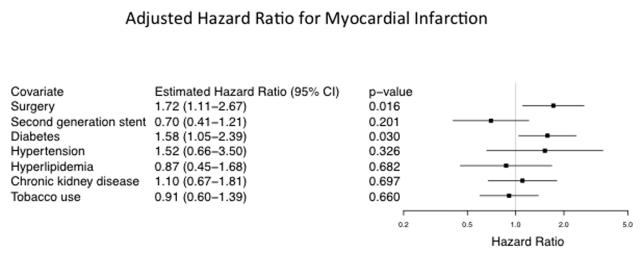
We then conducted a Cox model, which allowed NCP to be expressed as a time-dependent covariate, to adjust for comorbidities and differences in baseline characteristics. While the unadjusted hazard of all cause mortality was not significantly higher or lower with NCP, the unadjusted hazards for TVR and recurrent MI were significantly higher (in fact, estimated to be more than double) with NCP (Table 4). When we modified the Cox models to adjust for potential clinical confounders such as stent type, diabetes mellitus, hypertension, hyperlipidemia, chronic kidney disease and tobacco use, we found significantly greater adjusted hazards with NCP for all three endpoints (Figures 7-9). However, while the adjusted hazard of all cause mortality was estimated to be more than double with NCP, the adjusted hazard ratio estimates for TVR and recurrent MI were somewhat lower than the corresponding unadjusted hazard ratio estimates. Having a second generation DES was significantly protective against all cause mortality and exhibited a favorable trend in protecting against TVR. Chronic kidney disease was a significant risk factor for all cause mortality, while diabetes significantly elevated risk for recurrent MI.
Table 4.
Hazard ratios for major clinical outcomes.
| Unadjusted Hazard Ratio Estimate (95% CI) |
Adjusted Hazard Ratio#
Estimate (95% CI) |
|
|---|---|---|
| All cause mortality | 0.89 (0.68-1.68) | 2.18 (1.63-2.93)** |
| TVR | 2.36 (1.63-3.43)** | 1.89 (1.23-2.89)** |
| Recurrent MI | 2.41 (1.64-3.49)** | 1.66 (1.08-2.58)* |
P value < 0.05,
P value < 0.01
Cox proportional hazards regression modeling adjusted for confounding baseline characteristics such as diabetes, hypertension, hyperlipidemia, chronic kidney disease and tobacco abuse.
Figure 7.
Forest plot demonstrating the adjusted hazard ratio of all cause mortality in the study population. Chronic kidney disease was statistically associated with higher risk for all cause mortality. Diabetes showed a trend towards higher risk of all cause mortality. On the other hand, second generation drug eluting stents were protective.
Figure 9.
Forest plot demonstrating the adjusted hazard ratio of target vessel revascularization in the study population. Diabetes, hypertension and tobacco use showed trends towards higher risk of target vessel revascularization. On the other hand, second generation drug eluting stents showed trends for being protective.
Discussion
The introduction of DES has revolutionized the field of interventional cardiology and the management of coronary artery disease. However, recent doubts about the duration of DAT and stent thrombosis (ST) have slightly reduced the reliance on DES in patients anticipating non-cardiac surgical procedures requiring temporary interruption of DAT. This study is one of the largest and longest follow-up studies of patients treated with DES who subsequently underwent non-cardiac procedures in a real-world setting. We demonstrate the safety of using DES in patients who subsequently underwent NCP in terms of risk of bleeding and ST during short- and long-term follow-up. While patients undergoing NCP suffered more cardiac events such as TVR and myocardial infarctions, these events often happened more than 1 year after their DES and beyond the recommended duration of DAT.
Interruption of DAT early after DES can carry deleterious consequences, particularly the risk of stent thrombosis, a rare but potentially fatal complication (13,17,18). However, the risk decreases after the first 6 months, especially with the introduction of second and third generation DES (19-21). Schouten et al (22) studied 192 patients who underwent NCP up to 2 years after PCI using BMS or DES and demonstrated 30.7% major adverse cardiac events (MACE) in patients undergoing NCP within 30 days from their PCI. Anwaruddin et al (11) examined 481 patients undergoing 606 cardiac and non-cardiac procedures with a mean duration of 1.1 years after PCI using BMS or DES. The authors noted increased risk of MACE in the first 30 days after the index PCI but the risk decreased at 1 and 6 months afterwards. Interestingly, aspirin and/or clopidogrel use within 24 hours of NCP was not a significant predictor of outcomes in the multivariate analysis. Our data suggests that the risk of major clinical complications, such as bleeding and stent thrombosis, is low with the temporary interruption of DAT in patients who received DES followed by NCP. This was evident both at 1 year and long-term follow-up. Nonetheless, and in contrast to the study by Anwaruddin et al, all patients who suffered stent thrombosis had their DAT interrupted for their procedure. It is important to note that the risk of ST with DAT interruption is higher in the first 30 days after DES implantation (22,23) and with early generation DES (13,18). In our study, among the 4 patients who suffered stent thrombosis, three of them were treated with first generation DES while the fourth one was treated with second generation DES. Furthermore, all patients who suffered bleeding complications were on at least one antiplatelet agent perioperatively.
When we analyzed the major cardiac events data during the first year after PCI, we did not observe increased risk of TVR or recurrent myocardial infarction in patients who underwent NCP at 1 year of follow-up compared to those who did not undergo NCP (Table 3). Furthermore, mortality was actually higher among patients who did not undergo procedures. Since this data was not randomized, we cannot role out selection bias by the operators treating these patients. Our data is in agreement with the available literature as well as recent data proposing shorter DAT duration in patients treated with second generation DES (20). Ferreira-Gonzalez et al examined the risk of discontinuing one or both antiplatelet agents during the first year after DES implantation (24). In this cohort, almost all of the discontinuation occurred after the first month after PCI and most of the interruption was temporary (median of 7 days). The risk of acute coronary syndrome or major cardiac adverse events was low (4.4% and 5.5% respectively) and interrupting DAT was not an independent predictor of major cardiac events at 1 year of follow up. Other studies have demonstrated the rate of stent thrombosis to be significantly higher among the first 6 months after DES in patients who discontinued thienopyridines (13). The median time between discontinuing thienopyridines and ST was 13.5 days, and this duration increased to 90 days after the first 6 months after PCI, suggesting that temporary discontinuation of less than 7 days for NCP may be safe.
The need for non-cardiac procedures was common in patients after DES occurring in 41% of our patients especially in those with DM and CKD. There was no significant increase in stent thrombosis or bleeding associated with non-cardiac procedures in patients who had placement of DES when analyzed using the Fisher’s exact test. Our data is in agreement with others’ showing the safety of temporary discontinuing of DAT in patients undergoing NCP after DES implantation. However, these patients were more likely to have cardiac events and this could be explained, at least in part, by the higher preponderance of risk factors in this group. These data are meant to be hypothesis generating and future prospective trials are needed to clarify the safety of discontinuing DAT or undergoing NCP following PCI with DES. Given the relatively common need for NCP in this cohort, preoperative risk stratifications remains of utmost importance. Based on our study and available data, delaying the procedure for at least 6 months remains reasonable understanding that the risk persists but is reduced significantly after 1 year of PCI (11).
The literature is conflicting regarding the safety of NCP, and the associated temporary discontinuation of DAT, following DES placement. Our study, among others, highlights the safety of temporary discontinuation of DAT in the first year following DES in patients undergoing mostly low risk procedures. Furthermore, newer generation of DES have been shown in smaller studies to provide better safety profile with shorter DAT duration (19,20). Our data is in agreement with others regarding the low risk of bleeding and stent thrombosis with NCP performed greater than 1 month after treatment with DES (11,25). The implications of this data are significant given that NCP after PCI is unpredictable and appears to be common (11% in the first year alone). Given the lack of concrete data, the American College of Cardiology/American Heart Association maintains its advisory cautioning from the discontinuation of DAT in the first year after DES (26). The European Society of Cardiology’s most recent guidelines recommend postponing elective NCP for 6-12 weeks following BMS and 1 year following DES (27). We believe that based on our and other reports as well as the recent data with the newer generation of DES and antiplatelet therapies, these recommendations are due for an update.
This study has several limitations. We collected our data using a retrospective chart review and as such the study is limited by all the inherit limitations of the design such as referral bias. One of the major limitations of these analyses is the crossover bias, however, we conducted cox regression analysis models to mitigate this limitation. Using Cox regression modeling, we accounted only for events that occurred after NCP. We also did not have complete data regarding patients who stopped either or both of the antiplatelet therapies prior to their NCP and the duration of discontinuation. As a VA study, this study looked almost exclusively at male patients. Although the VA system is the primary healthcare provider for these patients, it is possible that a number of events were missed if the patients elected to utilize a non-VA hospital or provider. Furthermore, examining cardiac enzymes following NCP is subjective and some subclinical ischemic events may have gone undetected. Finally, the majority of procedures performed were low risk procedures and while this is a real life scenario, the results may be different if there was more higher risk procedures included (11,12).
Conclusions
Non-cardiac Procedures are common after placement of DES for the treatment of CAD. This retrospective study demonstrates no significant increase in peri-operative bleeding or stent thrombosis in patients who underwent NCP following DES implantation. There was, however, increased mortality, MI, hospitalization for cardiac causes, and target vessel revascularization following the first year after DES placement in the NCP cohort. Future prospective studies examining the safety of temporary interruption of DAT in patients treated with newer generation of DES and antiplatelet therapies will be important in updating the current recommendations and guidelines.
Supplementary Material
Supplemental Figure 1. Bar graph illustrating the time between the index percutaneous coronary intervention and non-cardiac procedure in the study sample. The majority of non-cardiac procedures were performed in the first 2 years following the index percutaneous coronary intervention (PCI).
Supplemental Figure 2. Bar graph illustrating the time between the index non-cardiac procedure and all cause mortality (Panel A), recurrent myocardial infarction (Panel B) and target vessel revascularization (Panel C). The majority of cardiac adverse events occurred in the first 4 years following the index non-cardiac procedure.
Figure 8.
Forest plot demonstrating the adjusted hazard ratio of recurrent myocardial infarction in the study population. Diabetes was statistically associated with higher risk for recurrent myocardial infarction. Hypertension and chronic kidney disease showed trends towards higher risk of recurrent myocardial infarction. On the other hand, second generation drug eluting stents showed trends for being protective.
Acknowledgments
Drs. Abdel-Latif and Ziada are supported by the University of Kentucky Clinical and Translational Science Pilot Award (UL1TR000117).
Dr. Abdel-Latif is supported by the UK COBRE Early Career Program (P20 GM103527).
Footnotes
The authors have no conflict of interest to report in relation to this manuscript
References
- 1.Takayama T, Hiro T, Hirayama A. Stent thrombosis and drug-eluting stents. Journal of cardiology. 2011;58:92–98. doi: 10.1016/j.jjcc.2011.07.003. [DOI] [PubMed] [Google Scholar]
- 2.Iakovou I, Schmidt T, Bonizzoni E, et al. INcidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA. 2005;293:2126–2130. doi: 10.1001/jama.293.17.2126. [DOI] [PubMed] [Google Scholar]
- 3.Jeremias A, Sylvia B, Bridges J, et al. Stent Thrombosis After Successful Sirolimus-Eluting Stent Implantation. Circulation. 2004;109:1930–1932. doi: 10.1161/01.CIR.0000127105.99982.21. [DOI] [PubMed] [Google Scholar]
- 4.Spertus JA, Kettelkamp R, Vance C, et al. Prevalence, Predictors, and Outcomes of Premature Discontinuation of Thienopyridine Therapy After Drug-Eluting Stent Placement: Results From the PREMIER Registry. Circulation. 2006;113:2803–2809. doi: 10.1161/CIRCULATIONAHA.106.618066. [DOI] [PubMed] [Google Scholar]
- 5.Airoldi F, Colombo A, Morici N, et al. Incidence and Predictors of Drug-Eluting Stent Thrombosis During and After Discontinuation of Thienopyridine Treatment. Circulation. 2007;116:745–754. doi: 10.1161/CIRCULATIONAHA.106.686048. [DOI] [PubMed] [Google Scholar]
- 6.Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58:e44–122. doi: 10.1016/j.jacc.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 7.Berger PB, Kleiman NS, Pencina MJ, et al. Frequency of Major Noncardiac Surgery and Subsequent Adverse Events in the Year After Drug-Eluting Stent Placement: Results From the EVENT (Evaluation of Drug-Eluting Stents and Ischemic Events) Registry. JACC: Cardiovascular Interventions. 2010;3:920–927. doi: 10.1016/j.jcin.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 8.Gandhi NK, Abdel-Karim A-RR, Banerjee S, Brilakis ES. Frequency and risk of noncardiac surgery after drug-eluting stent implantation. Catheterization and Cardiovascular Interventions. 2011;77:972–976. doi: 10.1002/ccd.22744. [DOI] [PubMed] [Google Scholar]
- 9.Hawn MT, Graham LA, Richman JR, et al. The Incidence and Timing of Noncardiac Surgery after Cardiac Stent Implantation. Journal of the American College of Surgeons. 2012;214:658–666. doi: 10.1016/j.jamcollsurg.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 10.To ACY, Armstrong G, Zeng I, Webster MWI. Noncardiac Surgery and Bleeding After Percutaneous Coronary Intervention. Circulation: Cardiovascular Interventions. 2009;2:213–221. doi: 10.1161/CIRCINTERVENTIONS.108.830158. [DOI] [PubMed] [Google Scholar]
- 11.Anwaruddin S, Askari AT, Saudye H, et al. Characterization of post-operative risk associated with prior drug-eluting stent use. JACC Cardiovasc Interv. 2009;2:542–9. doi: 10.1016/j.jcin.2009.03.014. [DOI] [PubMed] [Google Scholar]
- 12.Riddell JW, Chiche L, Plaud B, Hamon M. Coronary stents and noncardiac surgery. Circulation. 2007;116:e378–82. doi: 10.1161/CIRCULATIONAHA.107.726992. [DOI] [PubMed] [Google Scholar]
- 13.Airoldi F, Colombo A, Morici N, et al. Incidence and predictors of drug-eluting stent thrombosis during and after discontinuation of thienopyridine treatment. Circulation. 2007;116:745–54. doi: 10.1161/CIRCULATIONAHA.106.686048. [DOI] [PubMed] [Google Scholar]
- 14.Kimura T, Morimoto T, Nakagawa Y, et al. Antiplatelet therapy and stent thrombosis after sirolimus-eluting stent implantation. Circulation. 2009;119:987–95. doi: 10.1161/CIRCULATIONAHA.108.808311. [DOI] [PubMed] [Google Scholar]
- 15.Fleisher LA, Beckman JA, Brown KA, et al. ACC/AHA 2007 Guidelines on Perioperative Cardiovascular Evaluation and Care for Noncardiac Surgery: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines on Perioperative Cardiovascular Evaluation for Noncardiac Surgery) Developed in Collaboration With the American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, and Society for Vascular Surgery. Journal of the American College of Cardiology. 2007;50:1707–1732. doi: 10.1016/j.jacc.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 16.Cutlip DE, Windecker S, Mehran R, et al. Clinical End Points in Coronary Stent Trials: A Case for Standardized Definitions. Circulation. 2007;115:2344–2351. doi: 10.1161/CIRCULATIONAHA.106.685313. [DOI] [PubMed] [Google Scholar]
- 17.Park DW, Park SW, Park KH, et al. Frequency of and risk factors for stent thrombosis after drug-eluting stent implantation during long-term follow-up. Am J Cardiol. 2006;98:352–6. doi: 10.1016/j.amjcard.2006.02.039. [DOI] [PubMed] [Google Scholar]
- 18.Iakovou I, Schmidt T, Bonizzoni E, et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA. 2005;293:2126–30. doi: 10.1001/jama.293.17.2126. [DOI] [PubMed] [Google Scholar]
- 19.Valgimigli M, Campo G, Monti M, et al. Short-versus long-term duration of dual-antiplatelet therapy after coronary stenting: a randomized multicenter trial. Circulation. 2012;125:2015–26. doi: 10.1161/CIRCULATIONAHA.111.071589. [DOI] [PubMed] [Google Scholar]
- 20.Kim BK, Hong MK, Shin DH, et al. A new strategy for discontinuation of dual antiplatelet therapy: the RESET Trial (REal Safety and Efficacy of 3-month dual antiplatelet Therapy following Endeavor zotarolimus-eluting stent implantation) J Am Coll Cardiol. 2012;60:1340–8. doi: 10.1016/j.jacc.2012.06.043. [DOI] [PubMed] [Google Scholar]
- 21.Gwon HC, Hahn JY, Park KW, et al. Six-month versus 12-month dual antiplatelet therapy after implantation of drug-eluting stents: the Efficacy of Xience/Promus Versus Cypher to Reduce Late Loss After Stenting (EXCELLENT) randomized, multicenter study. Circulation. 2012;125:505–13. doi: 10.1161/CIRCULATIONAHA.111.059022. [DOI] [PubMed] [Google Scholar]
- 22.Schouten O, van Domburg RT, Bax JJ, et al. Noncardiac surgery after coronary stenting: early surgery and interruption of antiplatelet therapy are associated with an increase in major adverse cardiac events. J Am Coll Cardiol. 2007;49:122–4. doi: 10.1016/j.jacc.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 23.Reddy PR, Vaitkus PT. Risks of noncardiac surgery after coronary stenting. Am J Cardiol. 2005;95:755–7. doi: 10.1016/j.amjcard.2004.11.029. [DOI] [PubMed] [Google Scholar]
- 24.Ferreira-Gonzalez I, Marsal JR, Ribera A, et al. Double antiplatelet therapy after drug-eluting stent implantation: risk associated with discontinuation within the first year. J Am Coll Cardiol. 2012;60:1333–9. doi: 10.1016/j.jacc.2012.04.057. [DOI] [PubMed] [Google Scholar]
- 25.Rabbitts JA, Nuttall GA, Brown MJ, et al. Cardiac risk of noncardiac surgery after percutaneous coronary intervention with drug-eluting stents. Anesthesiology. 2008;109:596–604. doi: 10.1097/ALN.0b013e318186de1c. [DOI] [PubMed] [Google Scholar]
- 26.Grines CL, Bonow RO, Casey DE, Jr., et al. Prevention of premature discontinuation of dual antiplatelet therapy in patients with coronary artery stents: a science advisory from the American Heart Association, American College of Cardiology, Society for Cardiovascular Angiography and Interventions, American College of Surgeons, and American Dental Association, with representation from the American College of Physicians. J Am Coll Cardiol. 2007;49:734–9. doi: 10.1016/j.jacc.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 27.Task Force for Preoperative Cardiac Risk A. Perioperative Cardiac Management in Non-cardiac S. European Society of C et al. Guidelines for pre-operative cardiac risk assessment and perioperative cardiac management in non-cardiac surgery. Eur Heart J. 2009;30:2769–812. doi: 10.1093/eurheartj/ehp337. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1. Bar graph illustrating the time between the index percutaneous coronary intervention and non-cardiac procedure in the study sample. The majority of non-cardiac procedures were performed in the first 2 years following the index percutaneous coronary intervention (PCI).
Supplemental Figure 2. Bar graph illustrating the time between the index non-cardiac procedure and all cause mortality (Panel A), recurrent myocardial infarction (Panel B) and target vessel revascularization (Panel C). The majority of cardiac adverse events occurred in the first 4 years following the index non-cardiac procedure.